Submitted:
30 March 2024
Posted:
01 April 2024
You are already at the latest version
Abstract
Keywords:
Introduction
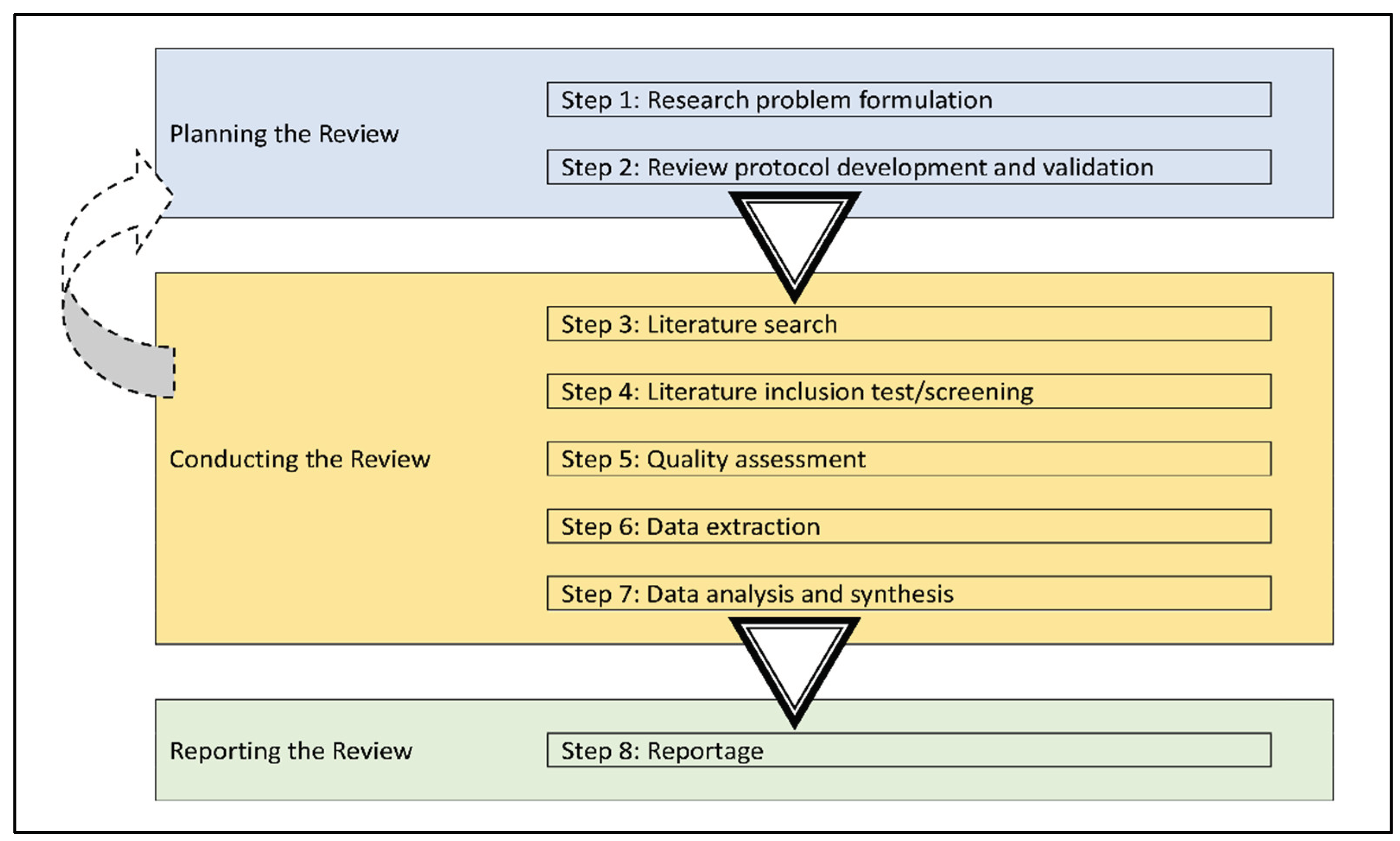
Methods
| S/N | CODE | SQL |
|---|---|---|
| 1. | A | Healthy Built Environment |
| 2. | B | Technology in/and the Built Environment |
| 3. | C | QoL and Technology |
| 4. | D | QoL and the Built Environment |
| Health | Technology | Built Environment | QoL(Quality of Life) | |
|---|---|---|---|---|
| Health | Healthy Built Environment | |||
| Technology | Technology in/and the Built Environment | QoL and Technology | ||
| Built Environment | Healthy Built Environment | Technology in/and the Built Environment | QoL and Built Environment | |
| QoL(Quality of Life) | QoL and Technology | QoL and Built Environment |

Results
Conclusion
References
- Abbasi, G.A.; Jagaveeran, M.; Goh, Y.-N.; Tariq, B. The impact of type of content use on smartphone addiction and academic performance: Physical activity as moderator. Technol. Soc. 2021, 64, 101521. [Google Scholar] [CrossRef]
- Agboola, O.P.; Tunay, M. Urban resilience in the digital age: The influence of Information-Communication Technology for sustainability. J. Clean. Prod. 2023, 428, 139304. [Google Scholar] [CrossRef]
- Agost-Felip, R.; Ruá, M.J.; Kouidmi, F. An Inclusive Model for Assessing Age-Friendly Urban Environments in Vulnerable Areas. Sustainability 2021, 13, 8352. [Google Scholar] [CrossRef]
- Ahad, M.A.; Paiva, S.; Tripathi, G.; Feroz, N. Enabling technologies and sustainable smart cities. Sustain. Cities Soc. 2020, 61, 102301. [Google Scholar] [CrossRef]
- Lee, C.; Ahmed, G. Improving IoT Privacy, Data Protection and Security Concerns. Int. J. Technol. Innov. Manag. (IJTIM) 2021, 1, 18–33. [Google Scholar] [CrossRef]
- Albahri, A.; Duhaim, A.M.; Fadhel, M.A.; Alnoor, A.; Baqer, N.S.; Alzubaidi, L.; Albahri, O.; Alamoodi, A.; Bai, J.; Salhi, A.; et al. A systematic review of trustworthy and explainable artificial intelligence in healthcare: Assessment of quality, bias risk, and data fusion. Inf. Fusion 2023, 96, 156–191. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ. 2023, 23, 1–15. [Google Scholar] [CrossRef]
- Alruwaili, M.M.; Shaban, M.; Ramadan, O.M.E. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability 2023, 15, 16503. [Google Scholar] [CrossRef]
- Antonishak, J.; Suellentrop, K.; Steiner, R.J.; Lloyd, L.; Axelson, S.M. Catalyzing Technology-Based Innovation in Teen Pregnancy Prevention: an Implementation Model and Findings from a Human-Centered Design Initiative. Prev. Sci. 2023, 24, 185–195. [Google Scholar] [CrossRef]
- Gabbiadini, A.; Baldissarri, C.; Durante, F.; Valtorta, R.R.; De Rosa, M.; Gallucci, M. Together Apart: The Mitigating Role of Digital Communication Technologies on Negative Affect During the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11, 554678. [Google Scholar] [CrossRef]
- Ben Atitallah, S.; Driss, M.; Boulila, W.; Ben Ghézala, H. Leveraging Deep Learning and IoT big data analytics to support the smart cities development: Review and future directions. Comput. Sci. Rev. 2020, 38, 100303. [Google Scholar] [CrossRef]
- Balcetis, E.; Cole, S.; Duncan, D.T. How Walkable Neighborhoods Promote Physical Activity: Policy Implications for Development and Renewal. Policy Insights Behav. Brain Sci. 2020, 7, 173–180. [Google Scholar] [CrossRef]
- Baobeid, A.; Koç, M.; Al-Ghamdi, S.G. Walkability and Its Relationships With Health, Sustainability, and Livability: Elements of Physical Environment and Evaluation Frameworks. Front. Built Environ. 2021, 7, 721218. [Google Scholar] [CrossRef]
- Becerik-Gerber, B.; Lucas, G.; Aryal, A.; Awada, M.; Bergés, M.; Billington, S.L.; Boric-Lubecke, O.; Ghahramani, A.; Heydarian, A.; Jazizadeh, F.; et al. Ten questions concerning human-building interaction research for improving the quality of life. J. Affect. Disord. 2022, 226, 109681. [Google Scholar] [CrossRef]
- Bell, I.H.; Nicholas, J.; Alvarez-Jimenez, M.; Thompson, A.; Valmaggia, L. Virtual reality as a clinical tool in mental health research and practice. Dialog- Clin. Neurosci. 2020, 22, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Bibri, S.E.; Krogstie, J. Data-driven smart sustainable cities of the future: An evidence synthesis approach to a comprehensive state-of-the-art literature review. Sustain. Futur. 2021, 3, 100047. [Google Scholar] [CrossRef]
- Bibri, S.E.; Krogstie, J.; Kaboli, A.; Alahi, A. Smarter eco-cities and their leading-edge artificial intelligence of things solutions for environmental sustainability: A comprehensive systematic review. Environ. Sci. Ecotechnology 2024, 19, 100330. [Google Scholar] [CrossRef] [PubMed]
- Bitar, H.; Alismail, S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit. Heal. 2021, 7. [Google Scholar] [CrossRef] [PubMed]
- Bogdandy, B.; Tamas, J.; Toth, Z. Digital transformation in education during COVID-19: A case study. 11th IEEE International Conference on Cognitive Infocommunications, CogInfoCom 2020 - Proceedings; 2020; pp. 173–178. [Google Scholar] [CrossRef]
- Borghouts, J.; Eikey, E.; Mark, G.; De Leon, C.; Schueller, S.M.; Schneider, M.; Stadnick, N.; Zheng, K.; Mukamel, D.; Sorkin, D.H. Barriers to and Facilitators of User Engagement With Digital Mental Health Interventions: Systematic Review. J. Med Internet Res. 2021, 23, e24387. [Google Scholar] [CrossRef]
- Bricout, J.; Baker, P. M. A.; Moon, N. W.; Sharma, B. Exploring the Smart Future of Participation: Community, Inclusivity, and People With Disabilities. International Journal of E-Planning Research (IJEPR) 2021, 10, 94–108. [Google Scholar] [CrossRef]
- Browne, D.T.; May, S.S.; Colucci, L.; Pietra, P.H.-D.; Christakis, D.; Asamoah, T.; Hale, L.; Delrahim-Howlett, K.; A Emond, J.; Fiks, A.G.; et al. From screen time to the digital level of analysis: a scoping review of measures for digital media use in children and adolescents. BMJ Open 2021, 11, e046367. [Google Scholar] [CrossRef]
- Campos-Castillo, C.; Mayberry, L. S. Disparities in digital health in underserved populations. Diabetes Digital Health and Telehealth 2022, 269–280. [Google Scholar] [CrossRef]
- Cayla, K.; Eithan, M.; Macie, C. The Impact of Social Media on Body Image and Self-esteem: A Comparative Study of Adolescent Girls in United States and South Korea. Stud. Soc. Sci. Humanit. 2023, 2, 30–37. [Google Scholar] [CrossRef]
- Cerritelli, F.; Chiera, M.; Abbro, M.; Megale, V.; Esteves, J.; Gallace, A.; Manzotti, A. The Challenges and Perspectives of the Integration Between Virtual and Augmented Reality and Manual Therapies. Front. Neurol. 2021, 12, 700211. [Google Scholar] [CrossRef] [PubMed]
- Chau, H.-W.; Jamei, E. Age-Friendly Built Environment. Encyclopedia 2021, 1, 781–791. [Google Scholar] [CrossRef]
- Chen, E.; Leos, C.; Kowitt, S.D.; Moracco, K.E. Enhancing Community-Based Participatory Research Through Human-Centered Design Strategies. Heal. Promot. Pr. 2020, 21, 37–48. [Google Scholar] [CrossRef]
- Chennamaneni, A.; Gupta, B. The privacy protection behaviours of the mobile app users: exploring the role of neuroticism and protection motivation theory. Behav. Inf. Technol. 2023, 42, 2011–2029. [Google Scholar] [CrossRef]
- Cho, Y.; Egan, T. The changing landscape of action learning research and practice. Hum. Resour. Dev. Int. 2023, 26, 378–404. [Google Scholar] [CrossRef]
- Copp, J.E.; Mumford, E.A.; Taylor, B.G. Online sexual harassment and cyberbullying in a nationally representative sample of teens: Prevalence, predictors, and consequences. J. Adolesc. 2021, 93, 202–211. [Google Scholar] [CrossRef]
- Craig, K.J.T.; Fusco, N.; Gunnarsdottir, T.; Chamberland, L.; Snowdon, J.; Kassler, W. Leveraging data and digital health technologies to assess and impact social determinants of health (SDoH). Online J. Public Heal. Informatics 2021, 13, E14. [Google Scholar] [CrossRef]
- Craig, S.; McPeak, K.E.; Madu, C.; Dalembert, G.; Madu, N.; Wasserman, R.C. Health information technology and equity: Applying history's lessons to tomorrow's innovations. Curr. Probl. Pediatr. Adolesc. Heal. Care 2022, 52, 101110. [Google Scholar] [CrossRef]
- Creed, C.; Al-Kalbani, M.; Theil, A.; Sarcar, S.; Williams, I. Inclusive Augmented and Virtual Reality: A Research Agenda. Int. J. Human–Computer Interact. 2023. [Google Scholar] [CrossRef]
- Dhagarra, D.; Goswami, M.; Kumar, G. Impact of Trust and Privacy Concerns on Technology Acceptance in Healthcare: An Indian Perspective. Int. J. Med Informatics 2020, 141, 104164–104164. [Google Scholar] [CrossRef]
- Egan, K. Digital Technology, Health and Well-Being and the Covid-19 Pandemic: It's Time to Call Forward Informal Carers from the Back of the Queue. Semin. Oncol. Nurs. 2020, 36, 151088. [Google Scholar] [CrossRef]
- Eisenberg, Y.; Maisel, J. Environmental Contexts Shaping Disability and Health. Public Health Perspectives on Disability: Science, Social Justice, Ethics, and Beyond, Second Edition, 2020; 107–128. [Google Scholar] [CrossRef]
- Emmelkamp, P.M.; Meyerbröker, K. Virtual Reality Therapy in Mental Health. Annu. Rev. Clin. Psychol. 2021, 17, 495–519. [Google Scholar] [CrossRef] [PubMed]
- Eshuis, L.; van Gelderen, M.; van Zuiden, M.; Nijdam, M.; Vermetten, E.; Olff, M.; Bakker, A. Efficacy of immersive PTSD treatments: A systematic review of virtual and augmented reality exposure therapy and a meta-analysis of virtual reality exposure therapy. J. Psychiatr. Res. 2021, 143, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Smith, A. P. Information overload, well-being and COVID-19: A survey in China. Behavioral Sciences 2021, 11, 62. [Google Scholar] [CrossRef]
- Ferreira, J.J.; Fernandes, C.I.; Rammal, H.G.; Veiga, P.M. Wearable technology and consumer interaction: A systematic review and research agenda. Comput. Hum. Behav. 2021, 118, 106710. [Google Scholar] [CrossRef]
- Ferrer, R. L. Social Determinants of Health. Chronic Illness Care: Principles and Practice, 2nd ed. Springer International Publishing, 2023; 527–545. [Google Scholar] [CrossRef]
- Fu, S.; Li, H.; Liu, Y.; Pirkkalainen, H.; Salo, M. Social media overload, exhaustion, and use discontinuance: Examining the effects of information overload, system feature overload, and social overload. Inf. Process. Manag. 2020, 57, 102307. [Google Scholar] [CrossRef]
- Ghazal, T.M.; Hasan, M.K.; Alshurideh, M.T.; Alzoubi, H.M.; Ahmad, M.; Akbar, S.S.; Al Kurdi, B.; Akour, I.A. IoT for Smart Cities: Machine Learning Approaches in Smart Healthcare—A Review. Futur. Internet 2021, 13, 218. [Google Scholar] [CrossRef]
- Goldstein, S.P.; Tovar, A.; Espel-Huynh, H.M.; Stowers, K.C. Applying a Social Determinants of Health Framework to Guide Digital Innovations That Reduce Disparities in Chronic Disease. Psychosom. Med. 2023, 85, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Gómez, C.A.; Kleinman, D.V.D.; Pronk, N.P.; Gordon, G.L.M.W.; Ochiai, E.; Blakey, C.B.; Johnson, A.M.; Brewer, K.H. Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. J. Public Heal. Manag. Pr. 2021, 27, S249–S257. [Google Scholar] [CrossRef] [PubMed]
- Göttgens, I.; Oertelt-Prigione, S. The Application of Human-Centered Design Approaches in Health Research and Innovation: A Narrative Review of Current Practices. JMIR mHealth uHealth 2021, 9, e28102. [Google Scholar] [CrossRef]
- Gracias, J.S.; Parnell, G.S.; Specking, E.; Pohl, E.A.; Buchanan, R. Smart Cities—A Structured Literature Review. Smart Cities 2023, 6, 1719–1743. [Google Scholar] [CrossRef]
- Harry, A. The Future of Medicine: Harnessing the Power of AI for Revolutionizing Healthcare. Int. J. Multidiscip. Sci. Arts 2023, 2, 36–47. [Google Scholar] [CrossRef]
- Hjetland, G.J.; Skogen, J.C.; Hysing, M.; Sivertsen, B. The Association Between Self-Reported Screen Time, Social Media Addiction, and Sleep Among Norwegian University Students. Front. Public Heal. 2021, 9, 794307. [Google Scholar] [CrossRef] [PubMed]
- Hui, C.X.; Dan, G.; Alamri, S.; Toghraie, D. Greening smart cities: An investigation of the integration of urban natural resources and smart city technologies for promoting environmental sustainability. Sustain. Cities Soc. 2023, 99, 104985. [Google Scholar] [CrossRef]
- Iyamu, I.; Gómez-Ramírez, O.; Xu, A.X.; Chang, H.-J.; Watt, S.; Mckee, G.; Gilbert, M. Challenges in the development of digital public health interventions and mapped solutions: Findings from a scoping review. Digit. Heal. 2022, 8. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Ngien, A. The Effects of Instagram Use, Social Comparison, and Self-Esteem on Social Anxiety: A Survey Study in Singapore. Soc. Media + Soc. 2020, 6. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Tosevska, A.; Klager, E.; Eibensteiner, F.; Laxar, D.; Stoyanov, J.; Glisic, M.; Zeiner, S.; Kulnik, S.T.; Crutzen, R.; et al. Virtual and Augmented Reality Applications in Medicine: Analysis of the Scientific Literature. J. Med Internet Res. 2021, 23, e25499. [Google Scholar] [CrossRef]
- Kasula, B. Y. Harnessing Machine Learning for Personalized Patient Care. Transactions on Latest Trends in Artificial Intelligence 2023, 4. [Google Scholar]
- Kemp, A.H.; Fisher, Z. Wellbeing, Whole Health and Societal Transformation: Theoretical Insights and Practical Applications. Glob. Adv. Heal. Med. 2022, 11. [Google Scholar] [CrossRef]
- Khan, M.; McNally, C. A holistic review on the contribution of civil engineers for driving sustainable concrete construction in the built environment. Dev. Built Environ. 2023, 16. [Google Scholar] [CrossRef]
- Kim, H.-J.; Lee, S.; Jung, D.; Hur, J.-W.; Lee, H.-J.; Lee, S.; Kim, G.J.; Cho, C.-Y.; Choi, S.; Lee, S.-M.; et al. Effectiveness of a participatory and interactive virtual reality intervention in patients with social anxiety disorder: Longitudinal questionnaire study. J. Med Internet Res. 2020, 22, e23024. [Google Scholar] [CrossRef]
- Kılıç, A.; Brown, A.; Aras, I.; Hui, R.; Hare, J.; Hughes, L.D.; McCracken, L.M. Using Virtual Technology for Fear of Medical Procedures: A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions. Ann. Behav. Med. 2021, 55, 1062–1079. [Google Scholar] [CrossRef]
- Kumari, J.; Das, K.; Babaei, M.; Rokni, G.R.; Goldust, M. The impact of blue light and digital screens on the skin. J. Cosmet. Dermatol. 2023, 22, 1185–1190. [Google Scholar] [CrossRef]
- Kwan, I.; Dickson, K.; Richardson, M.; MacDowall, W.; Burchett, H.; Stansfield, C.; Brunton, G.; Sutcliffe, K.; Thomas, J. Cyberbullying and Children and Young People's Mental Health: A Systematic Map of Systematic Reviews. Cyberpsychology, Behav. Soc. Netw. 2020, 23, 72–82. [Google Scholar] [CrossRef]
- Albreht, T. Challenges to Global Health Emerging from the COVID-19 Pandemic. Sustainability 2023, 15, 7633. [Google Scholar] [CrossRef]
- Lattie, E.G.; Stiles-Shields, C.; Graham, A.K. An overview of and recommendations for more accessible digital mental health services. Nat. Rev. Psychol. 2022, 1, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Lau, P.L.; Nandy, M.; Chakraborty, S. Accelerating UN Sustainable Development Goals with AI-Driven Technologies: A Systematic Literature Review of Women’s Healthcare. Healthcare 2023, 11, 401. [Google Scholar] [CrossRef] [PubMed]
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R: Rep. 2020, 140, 100523. [Google Scholar] [CrossRef]
- Lythreatis, S.; Singh, S.K.; El-Kassar, A.-N. The digital divide: A review and future research agenda. Technol. Forecast. Soc. Chang. 2022, 175, 121359. [Google Scholar] [CrossRef]
- Malik, A.; Dadure, P. Cyberbullying in the Digital Age. In Empowering Low-Resource Languages With NLP SolutionsEmpowering Low-Resource Languages With NLP Solutions; IGI Global, 2024; pp. 247–273. [Google Scholar] [CrossRef]
- Mann, R.B.; Blumberg, F. Adolescents and social media: The effects of frequency of use, self-presentation, social comparison, and self esteem on possible self imagery. Acta Psychol. 2022, 228, 103629. [Google Scholar] [CrossRef]
- Melles, M.; Albayrak, A.; Goossens, R. Innovating health care: key characteristics of human-centered design. Int. J. Qual. Heal. Care 2020, 33, 37–44. [Google Scholar] [CrossRef]
- Misra, S.; Roberts, P.; Rhodes, M. Information overload, stress, and emergency managerial thinking. Int. J. Disaster Risk Reduct. 2020, 51, 101762. [Google Scholar] [CrossRef]
- Moore, A.; Boyle, B.; Lynch, H. Designing for inclusion in public playgrounds: a scoping review of definitions, and utilization of universal design. Disabil. Rehabilitation: Assist. Technol. 2023, 18, 1453–1465. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.; Machado, C.C.; Burr, C.; Cowls, J.; Joshi, I.; Taddeo, M.; Floridi, L. The ethics of AI in health care: A mapping review. Soc. Sci. Med. 2020, 260, 113172. [Google Scholar] [CrossRef] [PubMed]
- Morrow, E.; Zidaru, T.; Ross, F.; Mason, C.; Patel, K.D.; Ream, M.; Stockley, R. Artificial intelligence technologies and compassion in healthcare: A systematic scoping review. Front. Psychol. 2023, 13, 971044. [Google Scholar] [CrossRef] [PubMed]
- Mouratidis, K. Urban planning and quality of life: A review of pathways linking the built environment to subjective well-being. Cities 2021, 115, 103229. [Google Scholar] [CrossRef]
- Nah, S.; Kwon, H.K.; Liu, W.; McNealy, J.E. Communication Infrastructure, Social Media, and Civic Participation across Geographically Diverse Communities in the United States. Commun. Stud. 2021, 72, 437–455. [Google Scholar] [CrossRef]
- Nah, S.; Lee, S.; Liu, W. Community Storytelling Network, Expressive Digital Media Use, and Civic Engagement. Commun. Res. 2021, 49, 327–352. [Google Scholar] [CrossRef]
- Nawaz, S. Rethinking classifications and metrics for problematic smartphone use and dependence: Addressing the call for reassessment. Comput. Hum. Behav. Rep. 2023, 12, 100327. [Google Scholar] [CrossRef]
- Neal Joshua, E. S.; Rao, N. T.; Bhattacharyya, D. Managing information security risk and Internet of Things (IoT) impact on challenges of medicinal problems with complex settings. In Multi-Chaos, Fractal and Multi-Fractional Artificial Intelligence of Different Complex Systems; Academic Press, 2022; pp. 291–310. [Google Scholar] [CrossRef]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. e-Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- Akindote, O.J.; Adegbite, A.O.; Dawodu, S.O.; Omotosho, A.; Anyanwu, A.; Maduka, C.P. Comparative review of big data analytics and GIS in healthcare decision-making. World J. Adv. Res. Rev. 2023, 20, 1293–1302. [Google Scholar] [CrossRef]
- Olaniyi, O.O.; Okunleye, O.J.; Olabanji, S.O. Advancing Data-Driven Decision-Making in Smart Cities through Big Data Analytics: A Comprehensive Review of Existing Literature. Curr. J. Appl. Sci. Technol. 2023, 42, 10–18. [Google Scholar] [CrossRef]
- Olliaro, P.; Torreele, E. Global challenges in preparedness and response to epidemic infectious diseases. Mol. Ther. 2022, 30, 1801–1809. [Google Scholar] [CrossRef] [PubMed]
- Olsson, T.; Jarusriboonchai, P.; Woźniak, P.; Paasovaara, S.; Väänänen, K.; Lucero, A. Technologies for Enhancing Collocated Social Interaction: Review of Design Solutions and Approaches. Comput. Support. Cooperative Work. (CSCW) 2020, 29, 29–83. [Google Scholar] [CrossRef]
- Opoku, A.; Bondinuba, F. K.; Manaphraim, N. Y. B.; Kugblenu, G. Advancing the sustainable development goals through the promotion of health and well-being in the built environment; Edward Elgar Publishing, 2024; Available online: https://www.elgaronline.com/edcollchap/book/9781035300037/book-part-9781035300037-17.xml.
- Pang, H. How compulsive WeChat use and information overload affect social media fatigue and well-being during the COVID-19 pandemic? A stressor-strain-outcome perspective. Telematics Informatics 2021, 64, 101690–101690. [Google Scholar] [CrossRef]
- Partarakis, N.; Zabulis, X. A Review of Immersive Technologies, Knowledge Representation, and AI for Human-Centered Digital Experiences. Electronics 2024, 13, 269. [Google Scholar] [CrossRef]
- Phillips-Wren, G.; Adya, M. Decision making under stress: the role of information overload, time pressure, complexity, and uncertainty. J. Decis. Syst. 2020, 29, 213–225. [Google Scholar] [CrossRef]
- Phuong, J.; Ordóñez, P.; Cao, J.; Moukheiber, M.; Moukheiber, L.; Caspi, A.; Swenor, B.K.; Naawu, D.K.N.; Mankoff, J. Telehealth and digital health innovations: A mixed landscape of access. PLOS Digit. Heal. 2023, 2, e0000401. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, B.; Bhattacharyya, S.; Pal, K. IoT-Based Applications in Healthcare Devices. J. Heal. Eng. 2021, 2021, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Raja, R. V.; Soundarapandian, K. Impact of Factors on Work Life Balance Due to Technology Transformation with Respect to Information Technology Employees. Webology 2022, 19, 5487–5496. [Google Scholar] [CrossRef]
- Rana, S.; Shuford, J. AI in Healthcare: Transforming Patient Care through Predictive Analytics and Decision Support Systems. J. Artif. Intell. Gen. Sci. (JAIGS) ISSN:3006-4023 2024, 1. [Google Scholar] [CrossRef]
- Rasool, S.; Husnain, A.; Saeed, A.; Gill, A. Y.; Hussain, H. K. Harnessing Predictive Power: Exploring the Crucial Role of Machine Learning in Early Disease Detection. JURIHUM : Jurnal Inovasi Dan Humaniora 2023, 1, 302–315. [Google Scholar]
- Ratta, P.; Kaur, A.; Sharma, S.; Shabaz, M.; Dhiman, G. Application of Blockchain and Internet of Things in Healthcare and Medical Sector: Applications, Challenges, and Future Perspectives. J. Food Qual. 2021, 2021, 1–20. [Google Scholar] [CrossRef]
- Rizzo, A.; Shilling, R. Herramientas de realidad virtual clínica para avanzar en la prevención, la evaluación y el tratamiento del TEPT. Eur. J. Psychotraumatology 2017, 8, 1414560. [Google Scholar] [CrossRef]
- Rounsefell, K.; Gibson, S.; McLean, S.; Blair, M.; Molenaar, A.; Brennan, L.; Truby, H.; McCaffrey, T.A. Social media, body image and food choices in healthy young adults: A mixed methods systematic review. Nutr. Diet. 2020, 77, 19–40. [Google Scholar] [CrossRef] [PubMed]
- Seixas, A. A.; Olaye, I. M.; Wall, S. P.; Dunn, P. Optimising Healthcare Through Digital Health and Wellness Solutions to Meet the Needs of Patients With Chronic Disease During the COVID-19 Era. Frontiers in Public Health, 2021; 9, 667654. [Google Scholar] [CrossRef]
- Sembiring, T.B.; Mokodenseho, S. The Impact of Online Interactions on Mental Health among Adolescents in West Java. Eastasouth J. Soc. Sci. Humanit. 2023, 1, 1–9. [Google Scholar] [CrossRef]
- Sen, K.; Prybutok, G.; Prybutok, V. The use of digital technology for social wellbeing reduces social isolation in older adults: A systematic review. SSM - Popul. Heal. 2022, 17, 101020. [Google Scholar] [CrossRef]
- Shirmohammadi, M.; Au, W.C.; Beigi, M. Remote work and work-life balance: Lessons learned from the covid-19 pandemic and suggestions for HRD practitioners. Hum. Resour. Dev. Int. 2022, 25, 163–181. [Google Scholar] [CrossRef]
- Slater, M.; Gonzalez-Liencres, C.; Haggard, P.; Vinkers, C.; Gregory-Clarke, R.; Jelley, S.; Watson, Z.; Breen, G.; Schwarz, R.; Steptoe, W.; et al. The Ethics of Realism in Virtual and Augmented Reality. Front. Virtual Real. 2020, 1. [Google Scholar] [CrossRef]
- Slaughter, A.; Newman, E. New Frontiers. J. Online Trust. Saf. 2022, 1. [Google Scholar] [CrossRef]
- Stępniak, C.; Jelonek, D.; Wyrwicka, M.; Chomiak-Orsa, I. Integration of the Infrastructure of Systems Used in Smart Cities for the Planning of Transport and Communication Systems in Cities. Energies 2021, 14, 3069. [Google Scholar] [CrossRef]
- Sun, J.; Lee, S.K. Flooded with too many messages? Predictors and consequences of instant messaging fatigue. Inf. Technol. People 2022, 35, 2026–2042. [Google Scholar] [CrossRef]
- Sunday, O.J.; Adesope, O.O.; Maarhuis, P.L. The effects of smartphone addiction on learning: A meta-analysis. Comput. Hum. Behav. Rep. 2021, 4, 100114. [Google Scholar] [CrossRef]
- Tiggemann, M.; Anderberg, I. Social media is not real: The effect of ‘Instagram vs reality’ images on women’s social comparison and body image. 2019, 22, 2183–2199. [Google Scholar] [CrossRef]
- Torous, J.; Bucci, S.; Bell, I.H.; Kessing, L.V.; Faurholt-Jepsen, M.; Whelan, P.; Carvalho, A.F.; Keshavan, M.; Linardon, J.; Firth, J. The growing field of digital psychiatry: current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 2021, 20, 318–335. [Google Scholar] [CrossRef] [PubMed]
- Townsend, B.; Schram, A.; Baum, F.; Labonté, R.; Friel, S. How does policy framing enable or constrain inclusion of social determinants of health and health equity on trade policy agendas? Crit. Public Heal. 2020, 30, 115–126. [Google Scholar] [CrossRef]
- Vandemeulebroucke, T.; Denier, Y.; Gastmans, C. The Need for a Global Approach to the Ethical Evaluation of Healthcare Machine Learning. Am. J. Bioeth. 2022, 22, 33–35. [Google Scholar] [CrossRef]
- Velmovitsky, P.E.; Bevilacqua, T.; Alencar, P.; Cowan, D.; Morita, P.P. Convergence of Precision Medicine and Public Health Into Precision Public Health: Toward a Big Data Perspective. Front. Public Heal. 2021, 9, 561873. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhu, T.; Zhang, T.; Zhang, J.; Yu, S.; Zhou, W. Security and privacy in 6G networks: New areas and new challenges. Digit. Commun. Networks 2020, 6, 281–291. [Google Scholar] [CrossRef]
- Woodward, E.N.; Singh, R.S.; Ndebele-Ngwenya, P.; Castillo, A.M.; Dickson, K.S.; Kirchner, J.E. A more practical guide to incorporating health equity domains in implementation determinant frameworks. Implement. Sci. Commun. 2021, 2, 1–16. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Operational Framework for Primary Health Care: Transforming Vision into Action; World Health Organization, 2020; Available online: https://www.who.int/publications/i/item/9789240017832.
- World Health Organisation. Ethics and governance of artificial intelligence for health: WHO guidance; 2021; pp. 3–22. [Google Scholar] [CrossRef]
- World Health Organization. Health and well-being and the 2030 agenda for sustainable development in the WHO European region: an analysis of policy development and implementation. In the Report of the first survey to assess Member States’ activities in relation to the WHO European Region Roadmap to Implement the 2030 Agenda for Sustainable Development; https://iris.who.int/handle/10665/339795; 2021. [Google Scholar]
- Wu, Z.; Jiang, M.; Li, H.; Zhang, X. Mapping the Knowledge Domain of Smart City Development to Urban Sustainability: A Scientometric Study. Sustainable Smart City Transitions 2022, 28–52. [Google Scholar] [CrossRef]
- Xiao, Y.; Watson, M. Guidance on Conducting a Systematic Literature Review. J. Plan. Educ. Res. 2019, 39, 93–112. [Google Scholar] [CrossRef]
- Young, J.F.; Jones, J.D.; Gallop, R.; Benas, J.S.; Schueler, C.M.; Garber, J.; Hankin, B.L. Personalized Depression Prevention: A Randomized Controlled Trial to Optimize Effects Through Risk-Informed Personalization. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 1116–1126. [Google Scholar] [CrossRef]
- Zahlan, A.; Ranjan, R.P.; Hayes, D. Artificial intelligence innovation in healthcare: Literature review, exploratory analysis, and future research. Technol. Soc. 2023, 74, 102321. [Google Scholar] [CrossRef]
| DATABASE | SUBJECT AREAS | ||
|---|---|---|---|
| Health | Technology | BuiltEnvironment | |
| Scopus | Medicine; Nursing; Biochemistry, Genetics and Molecular Biology; Health Professions; Psychology; Agricultural and Biological Sciences; Neuroscience; Decision Science; Immunology and microbiology. | Engineering; Energy; Computer Science; Mathematics; Physics & Astronomy. | Environmental Science; Social Sciences; Arts & Humanities; Earth & Planetary Sciences; Business Management & Accounting. |
| Google Scholar | |||
| DOAJ | |||
| JSTOR | Psychology; Public Health. | Computer Science; Engineering; Technology. | Architecture/Architectural History; Environmental Science/Studies; Garden & Landscape; Sustainability. |
| ProQuest | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




