1. Introduction
Ureteral obstruction is a common cause of urinary dysfunction in cats, with increasing incidence in recent years. A major cause of feline urinary obstruction is urolithiasis, with calcium oxalate uroliths accounting for 98% of cases [
1,
2]. Urinary obstruction due to urolithiasis often results in inflammation and dilation of the ureter which progresses from the obstruction site, and is a potentially life-threatening condition requiring immediate relief of obstruction. Due to their narrow ureters, many cats are forced to undergo surgical treatment, such as ureterotomy, ureteronephrectomy and neoureterocystotomy. However, the clinical outcome after surgery is not always favorable, and various postoperative complications such as persistent or recurrent ureteral obstruction and urine leakage are known to occur [
2,
3,
4]. For cases that suffer irreversible dysfunction following surgery, surgical reconstruction of the ureter is necessary.
Recently, Nakayama et al. developed a novel
in vivo tissue engineering technology, called in body tissue architecture (iBTA), which is based on the tissue-encapsulation phenomenon of foreign material in living bodies [
5,
6]. A mold consisting of a silicone tube with a stainless-steel rod placed inside, enclosed in a cylindrical plastic cage with linear windows, is first embedded into the subcutaneous tissue. After a few months, collagenous connective tissue forms around the silicone tube [
7]. The resulting tubular tissue, called a “biotube”, consists of an abundant extracellular matrix, and its utility as a graft for the reconstruction of collapsed blood vessels has been evaluated for human patients suffering from cardiovascular and angiopathic diseases [
8,
9,
10]. Watanabe et al. also reported that, in rabbits, a biotube implanted into the carotid artery successfully functioned as a scaffold for cells, including endothelial cells, fibroblast cells and myocytes. After 6 months of implantation, reconstruction of the layered structure of the blood vessel wall, including the endothelial layer, submucosal layer, smooth muscle layer, and serosa was achieved [
8]. Grafts engineered using iBTA technology have also been reported to have the following advantages: no immunological rejection (autologously engineered grafts), no toxicity, high biocompatibility, as well as being able to adapt to the growth of the recipient [
5]. Moreover, the grafts can be engineered into a wide range of shapes and sizes to suit the recipient by adjusting the shape and size of the molds. Most importantly, this technique does not require expensive or time-consuming procedures such as complex cell management or exceptionally clean laboratory facilities. Based on these results, biotube implantation has recently been applied to hemodialysis patients for the reconstruction of collapsed shunt vessels [
11].
The wall of the urinary tract has a layered structure, consisting of a urothelium layer at the luminal surface, a submucosal layer, and a smooth muscle layer. This layered structure closely resembles that of blood vessels. The structural similarity between blood vessels and the urinary tract suggests the possibility that iBTA can also be applied to not only the vascular system but also to the urinary tract, and offers a promising method for ureteral reconstruction. Another study using dogs demonstrated that bladder wall reconstruction could be achieved by transplanting autologous collagen connective tissue membrane (biosheet) fabricated using iBTA technology, suggesting that biosheets also have the potential to reconstruct the urinary tract [
12]. However, so far, there have been no reports of graft fabrication, such as biotubes and biosheets, using iBTA technology in cats, or the utilization of these grafts in the reconstruction of the feline urinary tract. In this study, we fabricated biosheets using iBTA technology in cats and implanted the biosheets into the urinary bladder in order to investigate their biocompatibility and utility as a scaffold for the reconstruction of the feline urinary tract.
2. Materials and Methods
2.1. Animals
Six healthy domestic cats (2 males and 4 females) aged 5 months with a body weight of 2-3 kg were used in this study. All cats received a prescription diet (pH Control 1, Royal Canin, Aimargues, France) to minimize the risk of urolithiasis, and were allowed free access to water. All animal experiments were approved by the Animal Care Committee of the Graduate School of Agricultural and Life Sciences at the University of Tokyo.
2.2. Mold Preparation for Graft Fabrication
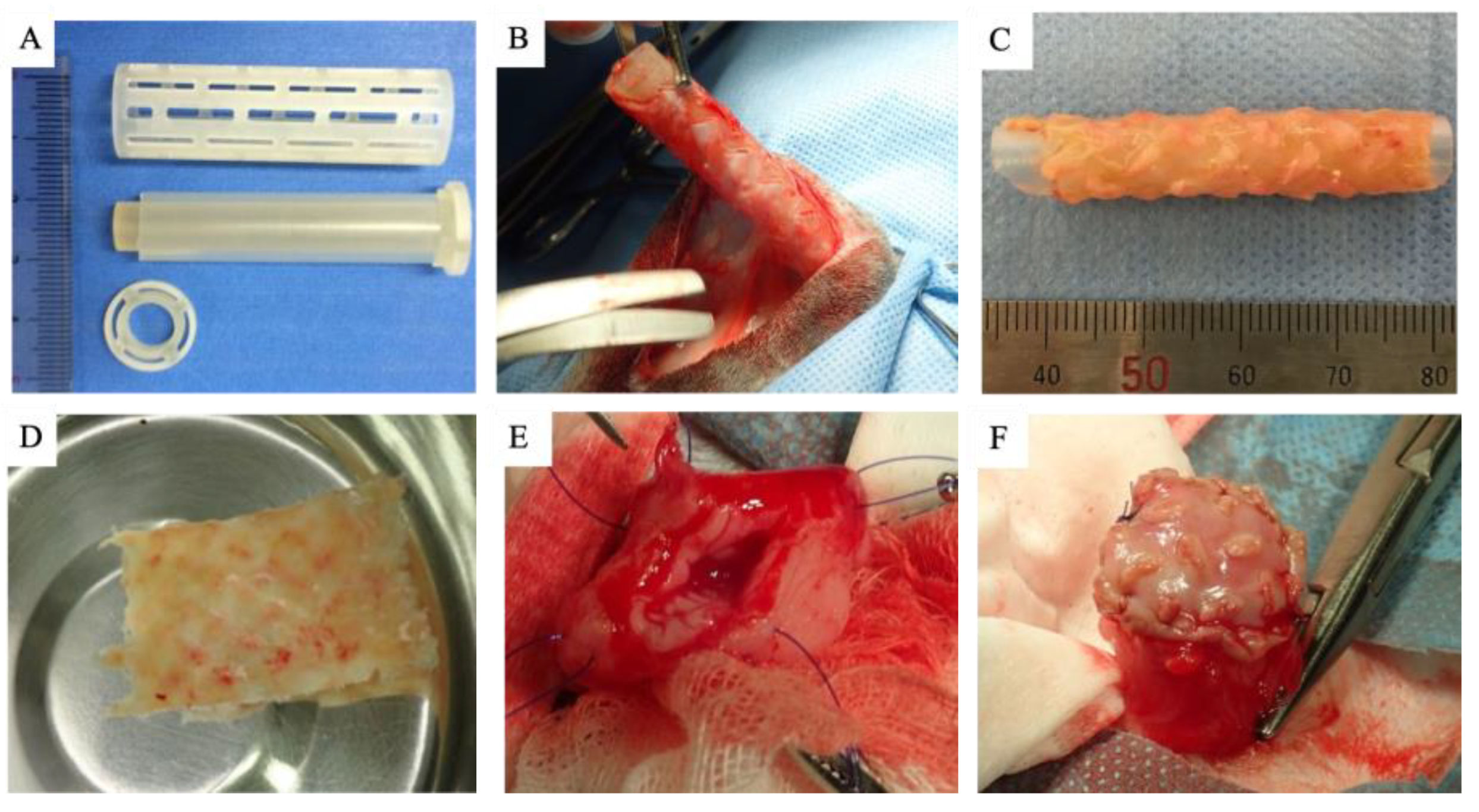
The mold was assembled from two parts, consisting of a silicone tube with a stainless-steel rod inserted inside, enclosed in a cylindrical plastic cage with varying types of linear windows (
Figure 1A). The assembly was fixed with a flat plastic cap at both ends. Each of the components were constructed using a 3-D rapid prototyping printer (Project 3510 HD, 3D Systems, Rock Hill, SC, USA). The gap between the silicone tube and outer plastic cage was set at 0.5-1 mm. The size of the mold was 5.5 cm in length and 1.0-1.5 cm in diameter.
2.3. Embedding of Mold and Graft (Biosheet) Fabrication
All surgical procedures were performed under general anesthesia. Atropine sulfate (0.01 mg/kg, IV), butorphanol (0.2 mg/kg, IV) and ampicillin (30 mg/kg, IV) were administered as preanesthetic medications. General anesthesia was induced with alfaxalone (5 mg/kg, IV) and maintained with isoflurane (2.0%). Two molds were separately embedded into the subcutaneous tissue of the right or left lumbar region in each cat. The skin incision was closed with a 4-0 nylon suture. Ampicillin (30 mg/kg, IV, BID) and robenacoxib (2 mg/kg, SC, SID) was administered postoperatively for 3 days. The molds were harvested after 2 months under general anesthesia as described above (
Figure 1B). By trimming the surrounding tissue and removing the outer plastic cage, a tubular tissue structure was obtained (
Figure 1C). After confirming there was no defect in the tissue graft, the tubular structure was cut longitudinally to obtain a sheet-shaped graft (biosheet) (
Figure 1D). The biosheet was then trimmed to a size of 1 x 2 cm and preserved in 70% ethanol. A piece of residual tissue was fixed in 10% formalin and embedded in paraffin for histopathological examination (hematoxylin-eosin (HE) and Masson’s trichrome (MT) stains).
2.4. Biosheet Implantation
Under general anesthesia, a section of the cranial ventral bladder wall (1 x 2 cm) was excised (
Figure 1E). The biosheet was washed in saline before implantation, placed into the excised site, and then sutured using a simple continuous suture pattern with a 4-0 nylon suture (
Figure 2F). After implantation, the bladder was filled with saline to test for leakage and covered with omentum. Finally, the abdominal wall and skin incision was closed with a 4-0 PDS and 4-0 nylon suture, respectively. A urinary catheter was inserted into the bladder.
2.5. Clinical Evaluation after Implantation
The animals were hospitalized for 5 days after implantation and received careful monitoring for signs of hematuria, pollakiuria, and urine leakage. Animals were also administered ampicillin (30 mg/kg, IV) once daily, and robenacoxib (2 mg/kg, SC) twice daily for 1 week. The urinary catheter was removed at 3 days after implantation. Serum biochemical analysis including blood urea nitrogen (BUN) and creatinine concentrations were closely monitored during hospitalization. Ultrasound examination of the implantation site was also performed at 1 day, 1 month and 3 months post implantation.
2.6. Histological Evaluation
Three of the six cats were humanely euthanatized after 1 and 3 months of implantation. The bladders were fixed with 10% formalin for 24 hours and tissue containing the implanted biosheets were embedded in paraffin. Sections of 4 μm thickness were then processed and stained by HE and MT. Immunohistochemistry was also performed using monoclonal antibodies against α-smooth muscle actin, Desmin, CD31 and S-100 to evaluate the migration and maturation of myofibroblasts, myocytes, vascular endothelium, and neural fibers, respectively.
3. Results
3.1. Biosheet Characterization
After 2 months of implantation in the subcutaneous tissue, the mold was encapsulated with collagenous connective tissue (
Figure 1B). A tubular tissue structure was obtained from the silicone tube after careful trimming of the surrounding connective tissue (
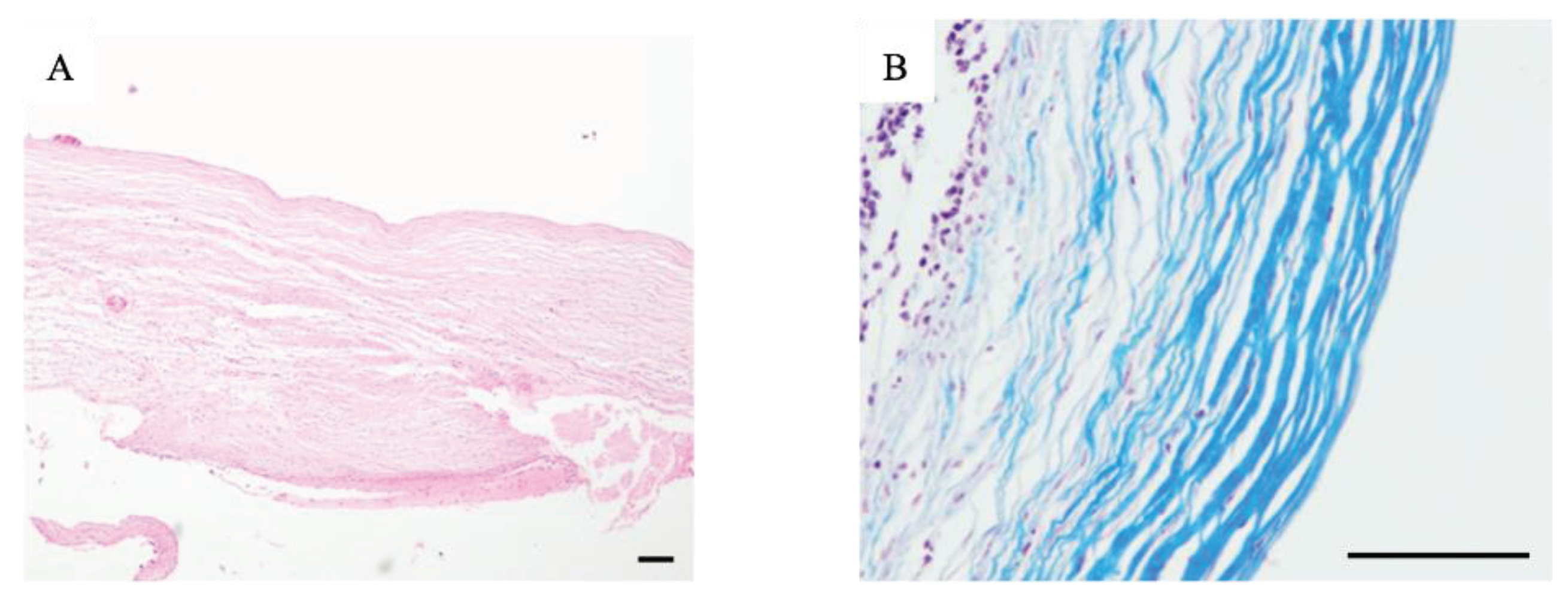
Figure 1C). However, 4 of the 12 molds resulted in incomplete tissue grafts with thin or defective walls. The remaining 8 grafts were smooth and whitish in color, with a thickness of 0.5-1 mm according to the designated mold. One cat received a biosheet harvested from another cat due to incomplete fabrication of the autologous biosheet. HE and MT staining revealed that the tissues obtained were fibrous and rich in collagen, with fibroblasts infiltrating into the connective tissue (
Figure 2B).
3.2. Biosheet Implantation and Postoperative Evaluation
The biosheets were able to tolerate surgical manipulation and could be easily sutured to the bladder wall (
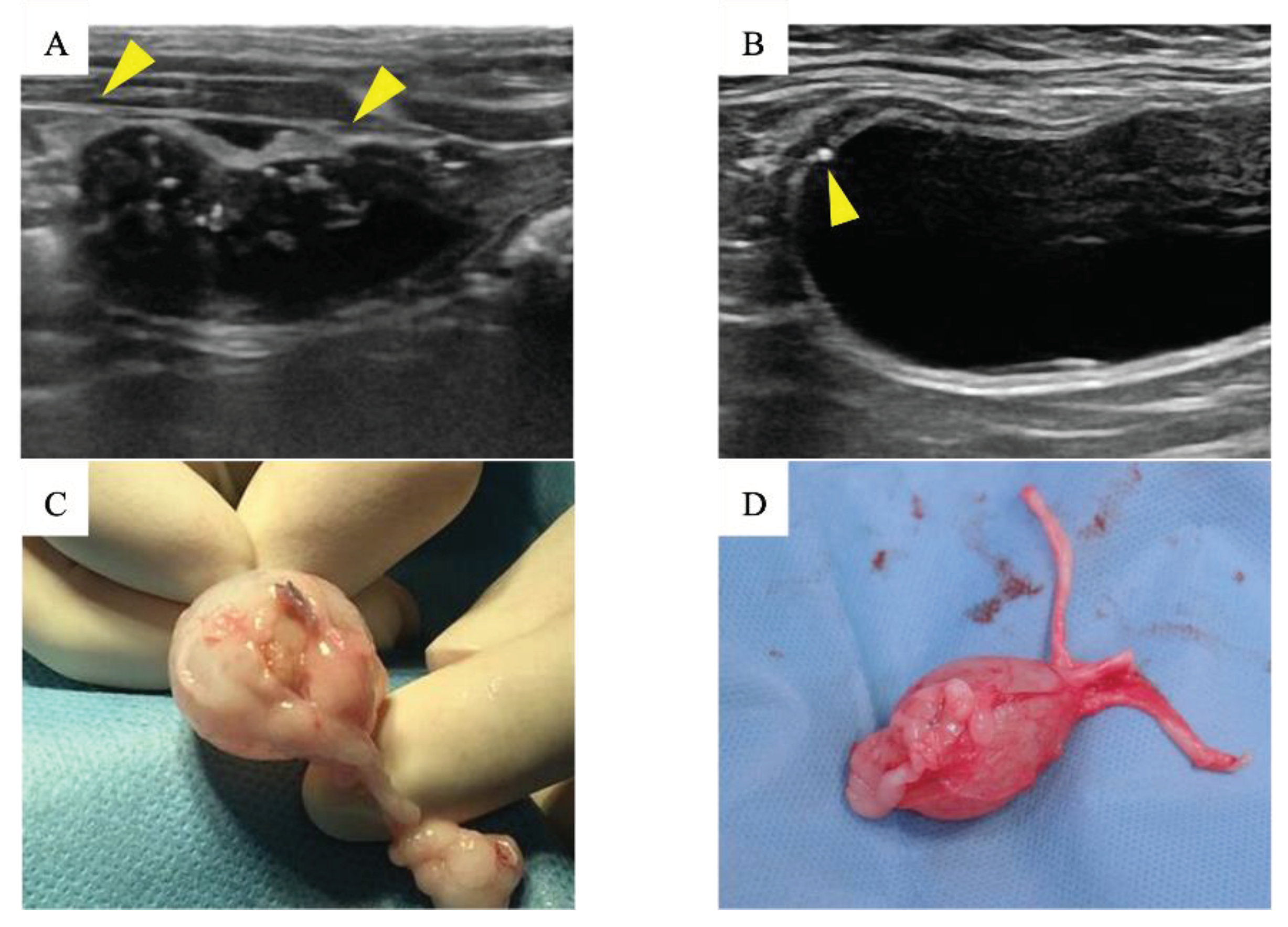
Figure 1F). No urine leakage was observed perioperatively. Hematuria was observed soon after surgery in all cats, but resolved within 3 days, after which the urinary catheter was removed. Serum biochemical analysis including BUN and creatinine did not indicate any severe abnormalities in any of the cats. Based on the ultrasound findings, urine leakage was not observed throughout the observation period. Ultrasound examination of the region containing the biosheet at 1 month post implantation showed a thickened bladder wall with an irregular margin (
Figure 3A). However, these abnormal findings disappeared after 3 months, and the implanted area appeared to be as smooth as a native bladder (
Figure 3B).
3.3. Histological Examination
There was severe adhesion of the implantation site to the omentum, and the biosheets could not be identified by gross observation (
Figure 3C, D). The implantation site was stiff and seemed to have little flexibility for 1 month after implantation. The site regained flexibility similar to that of a native bladder wall after 3 months.
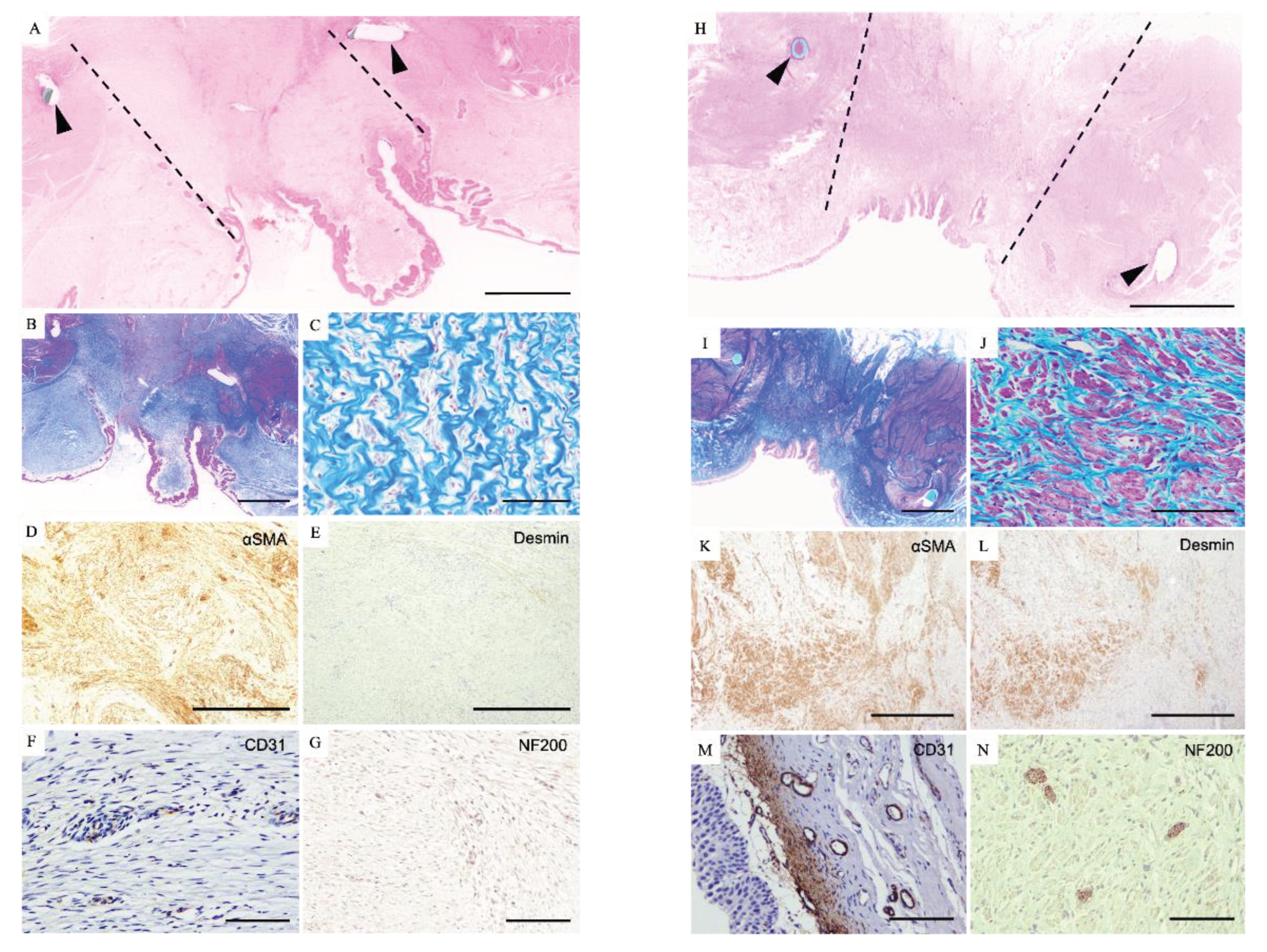
HE and MT staining revealed hyperproliferation of the urothelium by which the lumen of the bladder was almost entirely covered (
Figure 4A, B). There was observed remarkable ingrowth of fibroblastic cells into the biosheets under the urothelium layer (
Figure 4C). Immunohistochemistry revealed these fibroblastic cells were positive for αSMA, indicating that they were myofibroblasts (
Figure 4D). However, cells expressing Desmin, a marker for mature myocytes, were not detected (
Figure 4E). On the other hand, CD31 positive cells were observed in this area, indicating micro-neovascularization 1 month after implantation (
Figure 4F). No NF200 positive nerve fibers were detected (
Figure 4G).
After 3 months, the implantation site had a smooth lumen and was completely covered by urothelial cells forming a pseudostratified-like urothelium (
Figure 4H). MT staining revealed a well-organized extracellular matrix (
Figure 4I). A bundle of mature cells in the implanted region was observed and these cells were positive not only for αSMA but also for Desmin (
Figure 4J-L). These findings indicate the processes involved in the reconstruction of the submucosal layer and smooth muscle layer. Further, there was development of vasculature with CD31 expression in this region (
Figure 4M). Moreover, NF200-positive spindle-shaped cells were observed between the bundles of smooth muscle cells (
Figure 4N).
4. Discussion
The fabrication of tissue grafts such as biotubes and biosheets using iBTA technology has been reported in rats rabbits dogs, goats, and humans[
5,
9,
12,
13,
14,
15,
16]. In this study, we demonstrated that it is also possible to make such grafts in cats. However, the success rate for the formation of implantable biosheets was 67% (8/12), which was lower than the previous studies in goats [
15,
17]. Although inflammation due to infection after mold implantation is reported to be a factor in graft formation failure [
15], there were no findings indicating infection in this study. In order to form a graft of sufficient thickness, blood vessel infiltration into the mold and a sufficient supply of nutrients is necessary [
17,
18]. Therefore, it may be that graft formation failure occurred as a result of insufficient vascularization within the mold. It is also possible that the immune response to silicone in cats is weaker than in other species. It has been reported that the windows of the outer cylindrical cage of the mold help promote cell infiltration, and that the number and size of these windows are related to the efficiency of graft formation [
13]. Therefore, it may be necessary to make adjustments to the mold for cats, such as increasing the number or size of the windows. Further, in this study, the efficiency of graft formation differed between the molds embedded in the right lumbar region to those embedded in the left, suggesting that differences in the rate of graft formation may not be due to biological factors alone. In general, cats tend to rub their bodies against walls or objects as a form of marking behavior. The cats in this study also often rubbed their bodies against their cages, which may have caused mechanical stimulation to the implantation site. These behavioral characteristics of cats may have resulted in an unfavorable environment for graft formation.
Tissue grafts for implantation into the urinary tract need to have high biocompatibility as well as being elastic and flexible enough to store and transport urine [
19,
20]. The biosheet used for implantation had a thickness of 0.5-1.0 mm and was strong enough to withstand surgical manipulation. No urine leakage was observed immediately after implantation, and the biosheet successfully compensated for the defect in the bladder wall. Therefore, the biosheet was considered to have sufficient biocompatibility to be used as a graft for urinary tract reconstruction. The luminal surface of the bladder, including the implanted biosheet, was mostly covered by urothelium 1 month after implantation and was completely covered with multilayered urothelium after 3 months. Urothelium plays a role in protecting the bladder wall from urine stimulation. Therefore, early regeneration of the urothelium layer is considered essential for bladder reconstruction[
20]. Based on these results, the biosheets formed in this study were considered to function excellently as a scaffold for migration of the transitional epithelium. In addition, infiltration of myofibroblasts, which are involved in scar formation, was observed in the biosheet, and it was thought that this contributed to the promotion of epithelialization.
Three months after implantation, reconstruction of the muscle layer was confirmed, along with increased flexibility of the biosheet implantation site. Smooth muscle is essential for bladder compliance and contractility, and its regeneration is induced by adequate angiogenesis and migration of urothelium [
21]. In the areas where muscle cell clusters were observed, a new vascular network had also developed, suggesting that this contributed to the maturation and proliferation of muscle cells resulting in the recovery of contractility. Angiogenesis also promotes nerve fiber infiltration in bladder regeneration [
22]. In this study, infiltration of nerve fibers between muscle cells was also observed, suggesting that angiogenesis played an important role in the functional reconstruction of the bladder wall. Although we did not investigate the motility of the bladder smooth muscle, the appearance of nerve fibers suggested the recovery of urine excretory function. In the previous study using dogs, the biosheets successfully played a functional role as a scaffold for urothelium regeneration, but no mature muscle cells or nerve fibers appeared even after 3 months of implantation [
12]. This may be due to the larger size of the bladder defect (3 x 5 cm) compared to the present study. However, abundant vascularization was also observed, suggesting that smooth muscle and nerve regeneration could be expected with longer observation periods.
From the results of this study, it can be thought that more than 2 months is needed to form an implantable graft using iBTA technology in cats. However, urinary tract obstruction often requires immediate intervention, and preparing an autologous transplant would be difficult in clinical practice. In this study, an allogeneic biosheet was implanted in one cat and observed for 3 months, but there were no findings suggesting immune rejection, and bladder wall reconstruction was similarly observed to autologous biosheets. Therefore, even the allogenic biosheets prepared and preserved in advance using iBTA can be expected to be used for urinary tract reconstruction.
5. Conclusions
Biosheets can be induced by in body tissue architecture (iBTA) in cats and are expected to have high biocompatibility as graft materials for urinary tract reconstruction, contributing to histological and functional reconstruction.
Author Contributions
Conceptualization, N.F. and A.F.; methodology, N.F., F.S., and A.F.; investigation. N.F., F.S., M.T.; resources, N.F. and Y. N.; writing—original draft preparation, N.F. and F. S.; writing—review and editing, H.N.; supervision, R.N., A.F.; project administration, R.N., A.F.; funding acquisition, N.F. and A.F.. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a Grant-in-Aid (KAKENHI, grant numbers 17K15377) from the Japan Society for the Promotion of Science.
Institutional Review Board Statement
All animal experiments were approved by the Animal Care Committee of the Graduate School of Agricultural and Life Sciences at the University of Tokyo. Approval number: 15H-99.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Palm, C.; Westropp, J. . Cats and Calcium Oxalate. Strategies for Managing Lower and Upper Tract Stone Disease. J. Feline Med. Surg. 2011, 13, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Kyles, A.E.; Hardie, E.M.; Wooden, B.G.; Adin, C.A.; Stone, E.A.; Gregory, C.R.; Mathews, K.G.; Cowgill, L.D.; Vaden, S.; Nyland, T.G. Management and Outcome of Cats with Ureteral Calculi. J. Am. Vet. Med. Assoc. 2005, 226, 937–944. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.F.; Aronson, L.R.; Brown, D.C. Postoperative Mortality in Cats After Ureterolithotomy. Vet. Surg. 2011, 40, 438–443. [Google Scholar] [CrossRef]
- Wormser, C.; Clarke, D.L.; Aronson, L.R. Outcomes of Ureteral Surgery and Ureteral Stenting in Cats: 117 Cases (2006–2014). J. Am. Vet. Med. Assoc. 2016, 248, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Hayashida, K.; Kanda, K.; Yaku, H.; Ando, J.; Nakayama, Y. Development of an in Vivo Tissue-Engineered, Autologous Heart Valve (the Biovalve): Preparation of a Prototype Model. J. Thorac. Cardiovasc. Surg. 2007, 134, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.H.; Efendy, J.L.; Campbell, G.R. Novel Vascular Graft Grown within Recipient’s Own Peritoneal Cavity. Circ. Res. 1999, 85, 1173–1178. [Google Scholar] [CrossRef]
- Satake, R.; Komura, M.; Komura, H.; Kodaka, T.; Terawaki, K.; Ikebukuro, K.; Komuro, H.; Yonekawa, H.; Hoshi, K.; Takato, T.; et al. Patch Tracheoplasty in Body Tissue Engineering Using Collagenous Connective Tissue Membranes (Biosheets). J. Pediatr. Surg. 2016, 51, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Kanda, K.; Ishibashi-Ueda, H.; Yaku, H.; Nakayama, Y. Autologous Small-Caliber “Biotube” Vascular Grafts with Argatroban Loading: A Histomorphological Examination after Implantation to Rabbits. J. Biomed. Mater. Res. - Part B Appl. Biomater. 2010, 92, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Ishii, D.; Enmi, J. ichiro; Moriwaki, T.; Ishibashi-Ueda, H.; Kobayashi, M.; Iwana, S.; Iida, H.; Satow, T.; Takahashi, J.C.; Kurisu, K.; et al. Development of in Vivo Tissue-Engineered Microvascular Grafts with an Ultra Small Diameter of 0.6 mm (MicroBiotubes): Acute Phase Evaluation by Optical Coherence Tomography and Magnetic Resonance Angiography. J. Artif. Organs 2016, 19, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, Y.; Kaneko, Y.; Takewa, Y.; Okumura, N. Mechanical Properties of Human Autologous Tubular Connective Tissues (Human Biotubes) Obtained from Patients Undergoing Peritoneal Dialysis. J. Biomed. Mater. Res. - Part B Appl. Biomater. 2016, 104, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, Y.; Kaneko, Y.; Okumura, N.; Terazawa, T. Initial 3-Year Results of First Human Use of an in-Body Tissue-Engineered Autologous “Biotube” Vascular Graft for Hemodialysis. J. Vasc. Access 2020, 21, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Iimori, Y.; Iwai, R.; Nagatani, K.; Inoue, Y.; Funayama-Iwai, M.; Okamoto, M.; Nakata, M.; Mie, K.; Nishida, H.; Nakayama, Y.; et al. Urinary Bladder Reconstruction Using Autologous Collagenous Connective Tissue Membrane “Biosheet®” Induced by in-Body Tissue Architecture: A Pilot Study. Regen. Ther. 2020, 15, 274–280. [Google Scholar] [CrossRef]
- Furukoshi, M.; Moriwaki, T.; Nakayama, Y. Development of an in Vivo Tissue-Engineered Vascular Graft with Designed Wall Thickness (Biotube Type C) Based on a Novel Caged Mold. J. Artif. Organs 2016, 19, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Takewa, Y.; Yamanami, M.; Kishimoto, Y.; Arakawa, M.; Kanda, K.; Matsui, Y.; Oie, T.; Ishibashi-Ueda, H.; Tajikawa, T.; Ohba, K.; et al. In Vivo Evaluation of an In-Body, Tissue-Engineered, Completely Autologous Valved Conduit (Biovalve Type VI) as an Aortic Valve in a Goat Model. J. Artif. Organs 2013, 16, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, Y.; Takewa, Y.; Sumikura, H.; Yamanami, M.; Matsui, Y.; Oie, T.; Kishimoto, Y.; Arakawa, M.; Ohmuma, K.; Tajikawa, T.; et al. In-Body Tissue-Engineered Aortic Valve (Biovalve Type VII) Architecture Based on 3D Printer Molding. J. Biomed. Mater. Res. - Part B Appl. Biomater. 2015, 103, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Higashita, R.; Miyazaki, M.; Oi, M.; Ishikawa, N. First-in-Human Results of an in-Body Tissue Architecture-Induced Tissue-Engineered Vascular Graft “Biotube” for Application in Distal Bypass for Chronic Limb-Threatening Ischemia. J. Vasc. Surg. Cases, Innov. Tech. 2022, 8, 488–493. [Google Scholar] [CrossRef]
- Funayama, M.; Matsui, Y.; Tajikawa, T.; Sasagawa, T.; Saito, Y.; Sagishima, S.; Mizuno, T.; Mizuno, M.; Harada, K.; Uchida, S.; et al. Successful Implantation of Autologous Valved Conduits with Self-Expanding Stent (Stent-Biovalve) within the Pulmonary Artery in Beagle Dogs. J. Vet. Cardiol. 2015, 17, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Oie, T.; Yamanami, M.; Ishibashi-Ueda, H.; Kanda, K.; Yaku, H.; Nakayama, Y. In-Body Optical Stimulation Formed Connective Tissue Vascular Grafts, “Biotubes,” with Many Capillaries and Elastic Fibers. J. Artif. Organs 2010, 13, 235–240. [Google Scholar] [CrossRef]
- Elsawy, M.M.; de Mel, A. Biofabrication and Biomaterials for Urinary Tract Reconstruction. Res. Reports Urol. 2017, 9, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Pokrywczynska, M.; Gubanska, I.; Drewa, G.; Drewa, T. Application of Bladder Acellular Matrix in Urinary Bladder Regeneration: The State of the Art and Future Directions. Biomed Res. Int. 2015. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.K.; Madihally, S. V.; Palmer, B.; Frimberger, D.; Fung, K.M.; Kropp, B.P. Biomatrices for Bladder Reconstruction. Adv. Drug Deliv. Rev. 2015, 82, 47–63. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Chen, W.; Chen, B.; Shan, T.; Jia, W.; Hou, X.; Li, L.; Ye, G.; Dai, J. Bladder Regeneration in a Canine Model Using a Bladder Acellular Matrix Loaded with a Collagen-Binding bFGF. Biomater. Sci. 2017, 5, 2427–2436. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).