1. Introduction
Numerous major sporting events taking place in the summer season (World Track and Field Championships, Summer Olympic, and FIFA World Cup), when players have to compete in an environment where the average temperature frequently exceeds 30°C [
1]. Exercising in hot and humid environmental conditions can pose additional challenges to physiological function, which can impair aerobic exercise capacity [
2]. Heat stress can limit exercise performance as much as 6-16% in a variety of sports, through many mechanisms including elevated core temperature, rating of perceived exertion, heart rate, and sweat rate [
3,
4]. In addition, dehydration of greater than 3% of body mass further accelerates the rise in body temperature and increases the risk of exertional heat illness (heat cramps, heat exhaustion or heat stroke) [
5,
6]. To avoid the excessive loss of body fluids and prevent hindered exercise performance, players require an effective hydration plan pre-, mid-, and post-exercise [
7,
8].
According to the American College of Sport Medicine (ACSM) hydration guidelines, ~5-7ml/kg fluids need to be consumed at least 4hr prior to exercise and 1.5L of sodium-containing fluids for each kilogram of body mass loss after exercise [
9]. Maintaining water and electrolyte balance during exercise is more critical in alleviating heat stress [
10]. Typically, players drinking ad-libitum does not lead to adequate hydration, particularly during high-intensity exercise. An effective hydration solution that contains sodium can increase fluid retention and compensate for an individual’s fluid loss and sweat sodium loss preventing hyponatremia [
11]. Athletic trainers frequently monitor players’ fluid balance and electrolyte losses in daily practice and game, in terms of providing appropriate hydration strategy. However, sweat rates and electrolyte losses can be impacted by the environmental conditions and exercise intensity resulting in a large inter-individual variability. Previous research has showed that sweat sodium losses (soccer, basketball, rugby, etc.) can range from 11.2-86.5 mmol/L [
12], with lower sweat rates observed during exercise in cool environments (5±1°C; range: 0.71-1.77 L/h) compared to hot environments (37±3°C; range: 1.12-2.09 L/h) [
13]. Thus, to prescribe any specific electrolyte-solution given the wide variation of fluid and sodium needs for a large population is difficult. To overcome this issue, a personalized approach to hydration, including quantity and electrolyte content, during exercise may better meet each player’s particular needs [
14,
15]. To our knowledge, no studies have investigated how a personalized hydration strategy affects fluid balance and exercise performance across various environmental conditions, considering drinking behavior and thirst perception will be altered by environmental conditions. Therefore, the purpose of the present study was to investigate the effects of a tailored hydration strategy under normothermic and hyperthermic environments on body fluid balance and high-intensity intermittent exercise performance. Researchers hypothesized that personalized hydration strategy would have positive effects on fluid balance and exercise performance.
2. Materials and Methods
2.1. Experimental Design
The present study was a single blinded, randomized cross-over design where each participant completed two, 5-day trial arms in a climate-controlled chamber. The first arm was set as a normothermic environment (NOR: ~23°C, 30% relative humidity) and the second arm was a hyperthermic environment (HYP: ~35°C, 30% relative humidity). The experiment was conducted in the spring (April) with the ambient temperature approximately 22-25°C. Considering ambient temperature might influence sweat composition, the environmental conditions of the heat climate-controlled chamber were close to ambient temperature. Participants first completed a maximal oxygen uptake test (VO
2max; CosMed, K5) using the Bruce treadmill test protocol [
16]. The result of VO
2max was used to prescribe exercise intensity for all exercise trials. Each arm of 5-day trial began with 3 consecutive days of familiarization exercise. Following the 3 days of familiarization, participants randomly completed a main exercise trial under a control or personalized hydration condition. Participants then crossed over to the second arm with a washout period of 7 days (
Figure 1). Whole-body sweat rate and sweat electrolyte concentrations were collected during the familiarization exercise phase to prescribe a personalized hydration strategy (PHS). An ad-libitum hydration strategy was used as the control group (CON), where the sodium content in the beverage was prescribed as a commercially available electrolyte solution. The four resulting trials were as follows: a normothermic environment with personalized hydration strategy (NOR+PHS), a normothermic environment with ad-libitum hydration strategy (NOR+CON), a hyperthermic environment with personalized hydration strategy (HYP+PHS), and a hyperthermic environment with ad-libitum hydration strategy (HYP+CON).
2.2. Participants
Twelve active, non-acclimatized participants participated in this study, (age: 19.6±0.7yr; height: 176.6±5.4cm; weight: 69.5±8.5kg; maximal oxygen uptake: 53.9±4.4ml/kg/min). Participants completed a medical history form and a physical activity questionnaire (PAR-Q) before beginning any data collection. All participants were free of any chronic diseases, non-smokers, and sports injuries that would limit their ability to exercise. No alcohol was consumed or strenuous exercise performed within 24hr of any exercise trial.
2.3. Familiarization Exercise Phase
During the 3 days of familiarization exercise under both environmental conditions, participants were told to maintain their typical diet. Participants were required to consume 500ml fluids 2hr before arriving to ensure an euhydration status. Urine specific gravity (USG) was assessed before exercise with a threshold of <1.020. If USG was greater than 1.020, the trial was rescheduled to the next day. Body mass measures (TANITA HD-395) were taken pre- and post-exercise after participants voided the bladder. Percent of body mass loss (%BML) was calculated represented as hypohydration status. Familiarization exercise consisted of running on a treadmill at 50% VO2max for 45min in the assigned environmental condition. During exercise, participants were provided plain water drinking ad-libitum.
The whole-body sweat rate and electrolyte concentrations were averaged across 3 days of familiarization exercise for each environmental condition. Whole-body sweat rate was assessed by the differences of body mass pre- and post-exercise corrected by total fluid intake and urine volume. Sweat was collected using absorbent patch technique attached to a participant’s lower back [
17]. A 70% alcohol spray and dry towel were used to clean the skin surface before adhering the sweat patch to the skin. After exercise, the sweat patch was removed and centrifuged sweat used to analyze electrolyte concentrations (Na
+, K
+, Cl
-; AUDICOM AC9900). According to the Baker et al., local sweat sodium concentration was corrected to represent the whole-body loss [
18].
2.4. Hydration Strategies
To determine the volume of fluid replacement for the PHS during the main exercise trials, the total amount of fluids consumed was equal to sweat volume loss from familiarization exercise. The PHS was made by the lemon-lime Gatorade® Zero electrolyte powder, which contains 230mg [Na+] and 70mg [K+] for every 3g pack without protein and sugar. As Na+ is the main electrolyte in the sweat, Na+ concentration in the PHS was prescribed to equal to a participant’s whole-body Na+ concentration. In CON, no specific volume of hydration was required and participants were allowed to drink ad-libitum. The sodium content of the CON solution was equal to a commercially available electrolyte beverage (~30mmol/L).
2.5. Exercise Trials
During the exercise trial visit, participants were required to consume 500ml fluids 2hr before exercise. Participants were told to keep a similar diet and wear the same clothes across exercise trials. Upon arriving to the lab, participants were asked to empty their bladder and give a urine sample for analyzing USG. If USG was greater than 1.020, the exercise trial was rescheduled. Body mass was measured and the sweat patch adhered using the same procedures conducted during the familiarization phase. The exercise trial consisted of two phases with a 5min break between. The first phase was a 45min run on the treadmill at 50%VO
2max where the hydration strategy was incorporated, and the second phase was a high-intensity intermittent exercise (HIIT) until voluntary fatigue without any fluid provided (
Figure 1). In the first phase, participants in the PHS group consumed the amount of total fluid with equally distributed every 10min, whereas participants in the CON group drank ad-libitum. The HIIT protocol was accomplished by running on the treadmill at 80%VO
2max, 5% grade for 60s followed by a fast walk at 40%VO
2max, 5% grade for 30s until volitional fatigue. The time to exhaustion and bouts completion of HIIT was used to represent the exercise performance across the trials.
2.6. Outcome Measures
Heart rate (HR) was measured during all exercise trials (Polar Team-2). Auditory canal temperature (Tc; Braun IRT 6030) was assessed to represent body core temperature. Physiological strain index (PSI) was assessed using a formula: PSI=[5×(Tcore1-Tcore0)×(39.5-Tcore0)-1]+ [5×(HR1-HR0)×(180-HR0)-1], where Tcore0 and HR0 indicated baseline values, and Tcore1 and HR1 indicated the values measured time points during exercise. In addition, participants were asked rating perceived exertion (RPE, Borg 6-20) and the perception of thirst. The assessment of thirst perception was used a Likert-scale item ranging from 0 (no thirst) to 10 (severe thirst). HR, Tc, RPE, and thirst perception were assessed every 5min in the first phase and after each intermittent bout in the second phase.
2.7. Statistical Analysis
Statistical analysis was performed using JMPro 16 (SAS Inc.) and data were expressed as mean ± standard deviation (M±SD). A one-way repeated measure analysis of variance (ANOVA) was used to compare the parameters of fluid balance across trials (NOR+PHS, NOR+CON, HYP+PHS, and HYP+CON). Student-t post-hoc was used for pairwise comparisons between trials. Two-way repeated-measures ANOVA were used to analyze the main outcomes at any specific time point and each bout across trials (trials*time) within 11 bouts of HIIT because no participant completed more than 11 bouts in HYP+CON. The main outcomes included the parameters of fluid balance (%BML, fluid intake, WBSR, LSR, sweat Na+, urine Na+, and post USG), physiological responses (HR, Tc, RPE, thirst, and PSI), and exercise performance (time to exhaustion and the number of bouts completion). Statistical significance was accepted at p<0.05.
3. Results
3.1. Fluid Balance
Table 1 shows the effects of different hydration strategies under normothermic and hyperthermic environment after exercise trials (phase 1 and 2 averaged) on the parameters of fluid balance. Two participants had a pre-exercise USG greater than 1.020 during main exercise trial and were rescheduled to the next day. The %BML was significantly lower in NOR+PHS compared to NOR+CON and HYP+CON (all
p<0.001). HYP+PHS also had a significantly lower %BML compared to NOR+CON (
p=0.002) and HYP+CON (
p<0.001). Fluid intake was significantly greater in NOR+PHS (734.2±144.9g) compared to NOR+CON (272.3±143.0g;
p<0.001) and HYP+CON (369.8±221.7g;
p<0.001). HYP+PHS (831.7±166.4g) had a significantly greater fluid intake compared to NOR+CON (272.3±143.0g;
p<0.001) and HYP+CON (369.8±221.7g;
p<0.001). Participants in PHS (NOR+PHS: 0.92±0.27g; HYP+PHS: 1.18±0.29g) had a significantly greater Na
+ intake compared to CON (NOR+CON: 0.19±0.10g; HYP+CON: 0.26±0.15g, all
p<0.001). In addition, HYP+CON had the lowest sweat Na
+ (56.2±9.0mmol/L) compared to other trials (
p<0.001). HYP+PHS (62.7±9.6mmol/L) had a significantly lower sweat Na
+ compared to NOR+PHS (67.8±14.3mmol/L) and NOR+CON (71.3±16.3mmol/L, all
p<0.001). The changes in urine Na
+ and urine K
+ concentration from pre- to post-exercise was not significant differences across the trials (all
p>0.05). WBSR and LSR were not different between any trials (all
p>0.05).
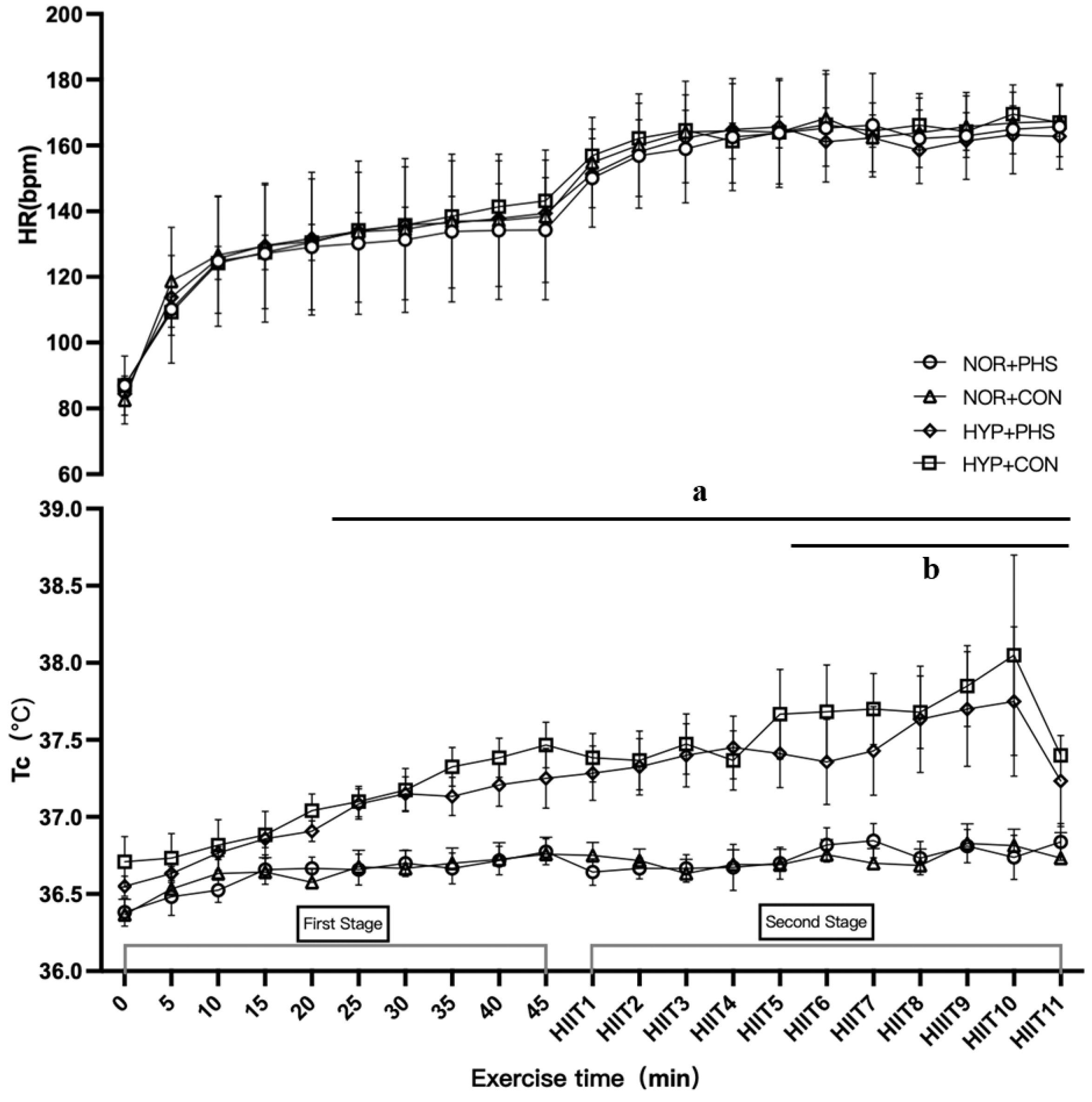
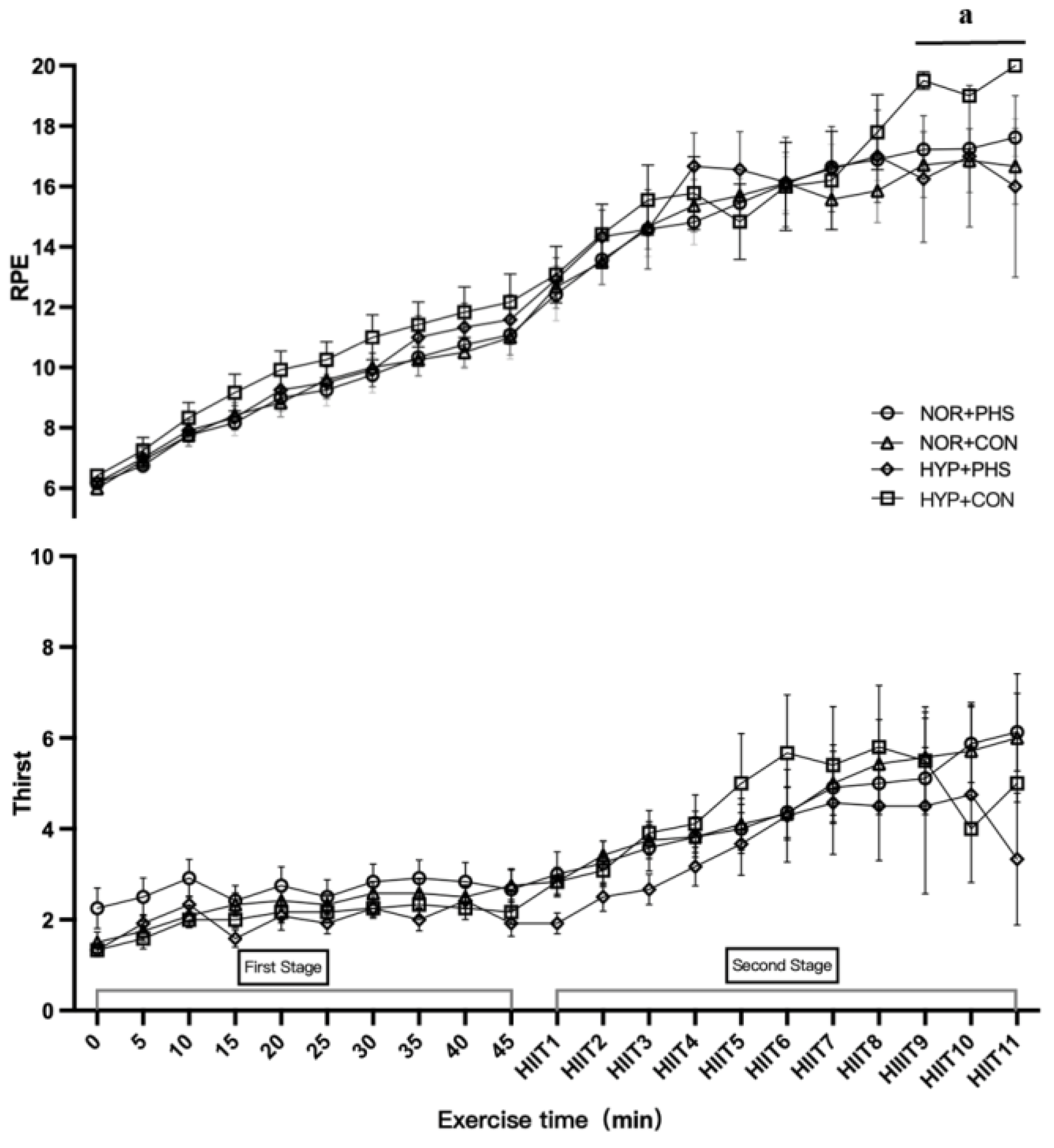
3.2. Physiological Responses
Table 2 shows the effects of different hydration strategies under normothermic and hyperthermic environments on physiological responses by exercise phase. In phase 1 when participants ran at constant workload with fluid accessibility, heart rate was not significantly differences across trials (
p=0.50). Participants in HYP trials had a significantly higher Tc compared to NOR condition (all
p<0.001), and HYP+CON participants had higher Tc (37.1±0.5℃) compared to HYP+PHS (37.0±0.4℃,
p=0.03). In addition, HYP+CON participants had a significantly greater RPE (10±3) compared to NOR+PHS (9±2,
p=0.001), NOR+CON (9±2,
p=0.001), and HYP+PHS (9±3,
p=0.03). Participants had a lower perception of thirst in HYP trials compared to NOR trials, regardless of hydration strategy (all
p<0.01), and NOR+CON participants had lower perception of thirst compared to NOR+PHS (
p<0.001).
In phase 2 of HIIT exercise, NOR+CON participants had a greater HR (167±13bpm) compared to NOR+PHS (163±14bpm,
p=0.006). Higher Tc was found in the HYP trials compared to NOR trials, regardless the hydration strategy (all
p<0.001). However, the two-way ANOVA analysis showed that averaged Tc from bouts 5-11 of HIIT in HYP+CON (37.7±0.6℃) was significant higher compared to HYP+PHS (37.5±0.7℃,
p=0.02;
Figure 2). In addition, RPE was not significant different among trials, but the averaged RPE of HIIT bout 9-11 was significantly greater in HYP+CON (19±1) compared to HYP+PHS (17±3,
p=0.005), NOR+CON (17±3,
p<0.001), and NOR+PHS (17±2,
p<0.001;
Figure 3). Participants in HYP+PHS had a significantly lower perception of thirst (3.6±2.4) in comparison to NOR+PHS (4.5±2.4,
p<0.001), NOR+CON (4.7±2.4,
p<0.001), and HYP+CON (4.2±2.2,
p=0.004), and HYP+CON participants had a lower perception of thirst compared to NOR+CON (
p=0.04). A greater PSI was found in HYP+PHS (6.6±1.8) compared to NOR+CON (5.6±0.8,
p=0.03).
3.3. Exercise Performance
Both HYP trials had a significantly shorter HIIT exercise length and less completed bouts compared to NOR trials (HYP+PHS vs. NOR+CON,
p=0.03; HYP+PHS vs. NOR+PHS,
p=0.002; and HYP+CON vs. NOR+CON,
p<0.001; HYP+CON vs. NOR+PHS,
p<0.001). In addition, within the HYP condition, HYP+PHS showed a longer exercise length and completion bout compared to HYP+CON (
p=0.04). There was no significant difference in HIIT exercise duration between NOR+CON and NOR+PHS (
p=0.26;
Figure 4).
4. Discussion
The main purpose of the present study was to investigate the effects of a personalized hydration strategy under normothermic and hyperthermic environmental conditions on body fluid balance and HIIT exercise performance. The main finding was that participants using a PHS led to significantly greater fluid and sodium intake under both normothermic and hyperthermic environmental conditions, resulting in a blunted hypohydration status. When participants drank ad-libitum (control) during the hyperthermic environment, they experienced greater thermoregulatory strain as measured by canal temperature and RPE during exercise. Importantly, PHS under hyperthermic environment prolonged HIIT exercise performance compared to the CON, suggesting a targeted approach to hydration can protect performance.
4.1. Fluid Balance
Hydration guidelines recommend players should drink sufficient amounts of sodium-containing fluid to prevent hypohydration and hyponatremia during exercise in the heat. Previous research has reported that drinking ad-libitum typically does not lead to a successful hydration [
19]. The PHS simply derived from exercise losses allowed participants to appropriately hydrate (volume and electrolyte content) without relying on mechanisms like thirst or broad guidelines. Participants also avoided over-hydrating, another problematic issue among players [
6]. Emerson et al. prescribed a PHS solution corresponding to ice-hockey players’ sweat volume. Players were required to ingest the PHS solution within an hour of practice, finally resulted in a -0.95%BML, whereas drink ad-libitum resulted in -1.14%BML [
20]. Melo-Marins et al. applied a PHS solution offset 80% of sweat loss during a time to exhaustion cycling at 70% of the maximal workload, resulted in a -0.2%BML compared to ad-libitum CON with a (-1.0%BML) [
21]. In addition, Bardis et al. prescribed PHS to offset total sweat loss in a 30-km cycling resulted in a -0.5% BML compared to ad-libitum a -1.8%BML [
22]. Lopez et al. designed a PHS according to a runner’s 4-km sweat loss multiply by 5 as target rehydration volume during a 20-km race, which also resulted in a -1.4%BML compared to -2.6%BML by ad-libitum drinking [
23]. Thus, the protection from hypohydration with a PHS in the previous research was consistent with our results. The protocol of PHS in the present study successfully reinforced fluid intake (~700-800ml) to offset participants’ sweat loss, which resulted in a blunted hypohydration status compared to the ad-libitum trials, regardless of environmental conditions. Participants drinking ad-libitum replaced nearly 41% of sweat loss, yet still exhibited mild hypohydration status (~-1% BML) under both environmental conditions. Conversely, Lopez et al. found a >2% hypohydration status when drinking ad-libitum compared to their PHS, which could be due to the exercise length and intensity being greater than the present study. Our exercise length was similar to the previous research conducted (Emerson et al. and Bardis et al.) around ~60min at moderate-vigorous intensity reflecting similar fluid balance parameters. In contrast to Lopez et al., participants completed a 20-km race by nearly 1.7hr at moderate-vigorous exercise intensity. Together, PHS could show a superior effect on hydration status compared to ad-libitum drinking during a long bout of high-intensity exercise [
18].
Uniquely, the present study prescribed the sodium content in the PHS to compensate for a participant’s sweat sodium loss. Sodium content in a commercially available beverage is typically ~250-270mg in a 500-600ml bottle. In the present study, participants required an average of 920mg and 1180mg sodium during exercise in the normothermic and hyperthermic conditions, respectively. Participants have to drink 3-4 bottles of commercially available solutions so that to match their sodium needs, which seems untenable to drink that amount of fluid during a short time frame. Two previous studies prescribed a sodium content in the PHS [
20,
24]. Ayotte et al. suggested PHS can provide sodium supplementation in a beverage, especially for those players who engage in prolonged and high intensity exercise to maintain serum sodium concentration [
24]. The sodium content in the PHS of Emerson et al. induced a lowering urine sodium concentration and an increasing in potassium from pre- to post-exercise [
20]. The present study found the similar results that urine sodium was increased and urine potassium was decreased from pre- to post-exercise across all trials, suggesting participants were in a state of sodium conservation to retain water in the kidney. In addition, sweat sodium concentration exhibited significant differences between PHS and CON under two environmental conditions. Typically, an individual’s sodium loss is impacted by many factors, such as energy expenditure, heat acclimation, dietary sodium intake, environmental conditions, or the combination of those [
25]. Sweat sodium concentration is associated with energy expenditure via increased metabolic heat production and sweat rate, consequently the rate of sodium excretion in precursor sweat increases proportionally greater than the rate of sodium reabsorption [
26]. Participants in the normothermic environment had longer exercise duration compared to hyperthermic environment, which possibly result in a greater sweat sodium concentration. On the other hand, when an individual is chronically exposed to a hot environment, an acclimatized state occurs, inducing sweat glands to be more sensitive to aldosterone by lowering sweat sodium concentration. These results corroborates with Bates et al., who also found an individual’s sweat sodium concentration was lower in summer compared to winter [
27]. Furthermore, dietary sodium intake affects sweat sodium concentration, which higher sodium intake could also result in a 10-11% greater in sweat sodium compared to low sodium diet [
28]. PHS participants consumed greater sodium during exercise, possibly improves extracellular fluid retention during/after exercise eliciting a large sweat sodium loss [
29]. Therefore, the present study cannot conclude any specific influence factor for the differences in sweat sodium concentration between trials. Future study can focus on the importance of PHS solution on the sodium loss and water retention of the body.
4.2. Exercise Performance
While PHS provides an advantage to optimize a participant’s hydration status and also offset the sodium loss, research studies are consistently looking for a PHS method to improve exercise performance. The present study found exercise duration was longer in NOR compared to HYP, regardless of hydration strategy, possibly due to environmental stress. Under normothermic environmental condition, even though participants in personalized hydration trial had a lower heart rate than ad-libitum trial, it did not cause any differences in Tc and RPE in the second phase of interval exercise. Consequently, PHS did not show a benefit of exercise performance outcomes. This is similar to Emerson et al., who reported PHS did not have advantage in exercise performance in ice-hockey field with a lesser environmental stress [
20]. Notably, PHS prolonged HIIT exercise duration by nearly 40% compared to CON under hyperthermic environmental condition. Ayotte et al. and Bradis et al. also suggested a personalized hydration strategy can improve exercise performance in the heat by lowering thermoregulatory strain and improving anaerobic power and heart rate recovery [
22,
24]. According to the “cardiovascular drift” phenomenon, the combination of hyperthermia and dehydration accelerates the reduction in muscle blood perfusion and exercise performance. Under hyperthermic environmental condition, when participants were allowed to have fluid replacement in the first exercise phase, PHS attenuates participant’s Tc and RPE. As progressed to the second phase of HIIT exercise even without any fluid intake, PHS participants still could complete more HIIT bouts, finally approaching to the similar RPE and Tc. In addition, participants drinking ad-libitum exhibited a 0.2℃ higher in Tc averaged from bout 5-11 and they also felt exercise was harder at bout 9, 10, and 11 compared to PHS, and no participant can exercise more 11 bouts in the CON trial. This may suggest that PHS can delay the rise in body temperature and RPE to the peak during exercise in the heat. By contrast, Lopez et al. and Melo-Marins et al. found PHS can attenuate rise in heart rate and skin temperature, but exercise performance remains unchanged. The possible explanation is that Lopez et al. used 4-km fluid loss to estimate a 20-km race fluid replacement, which may not accurately prescribe a PHS. In addition, in the study of Melo-Marins et al., participants were exhausted quickly after exercising for 37-38 minutes. The hypohydration status may have a small impact on exercise performance, which cannot show the benefits of PHS. On the other hand, PHS might blunt the markers of dehydration after a bout of continuous exercise, resulting in better intermittent exercise performance. Notably, under hyperthermic environmental condition, our PHS participants had lower thirst perception in phase 2 while no fluid ingested. Hypohydration status typically induced a rise in thirst perception, which is associated with an exercise performance reduction [
30,
31]. Thus, the present PHS optimizes an individual’s fluid balance and lowers the thirst perception ameliorating thermoregulatory strain to aid exercise performance in the heat. This result is so important to those sport events that are significantly affected by hypohydration status (outdoor events, heavy sweaters, etc.).
4.3. Strengths and Limitations
A strength of the present study was the experimental design with tightly controlled exercise sessions and dietary-supervised. The 3-day familiarization exercise phase assured the sweat sodium concentration represented a person’s typical status. In addition, the present study used the regional sweat collecting technique, which is one of the most feasible and popular methods for athletic trainers to assess sweat composition. Considering regional sweat sodium is typically greater than the whole-body sweat sodium concentration, this study corrected the regional sweat sodium concentration to a whole-body sweat sodium according to the previous research [
18]. Uniquely this cross-over design replicated both a normothermic and hyperthermic environmental conditions to compare outcomes. One of the limitations was that we did not measure body weight and analyze electrolyte concentration after phase 1, so that we cannot separate the markers of hydration just like the physiological responses in the
Table 2. Another limitation was that a true control (only water consumed) was not included. However, well-documented research shows a benefit in exercise performance when drinking sodium-containing beverage compared to plain water. So, our study wants to detect the differences on the outcomes between PHS and commercially available sports drink.
4.4. Practical Applications
We designed this personalized hydration strategy according to participants’ whole-body sweat rate and sweat sodium concentration that successfully offset their fluid and sodium loss. Typically, exercise physicians are required to monitor players’ sweat rate and electrolyte losses in daily practice, especially for outdoor team sports. We used absorbent technique to assess local sweat electrolyte concentrations, which considers one of the most feasible methods to assess a group of players on the field. Then, exercise physicians can easily prescribe personalized hydration solution to any athlete. In the normothermic environmental condition, the present results recommend commercially available electrolyte-solution is sufficient to maintain fluid balance and exercise performance. However, when players compete in the hyperthermic environmental condition or in high intensity situations, personalized hydration solutions should be prepared to players according to their daily fluid balance assessment.
5. Conclusions
A personalized hydration strategy based on an individual’s fluid and sodium loss successfully optimized hydration status, regardless of a hyper- or normothermic environmental condition. In hot environments, a personalized hydration strategy may be more important to improve high-intensity intermittent exercise performance by reducing thirst perception and thermoregulatory strain. In cool environments, drinking commercially available electrolyte beverages ad-libitum is sufficient to maintain exercise performance. Future research should continue investigating personalized hydration strategy method, considering the least amount of drinking volume to offset sodium loss maintaining an euhydration status.
Author Contributions
H.W. contributed to the conception and the design of this research. H.L., G.Z., and P.M. contributed to data collection. H.W. and K.E. contributed to data interpretation. H.L. wrote the original manuscript. H.W. and K.E. critically revised and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The study was founded by the University Doctoral Research Starting Funds (#YS304320150), Zhejiang Province Master Student Research Funds (#KYZ04Y22296), and Sports Science Innovation Project of General Administration of Sport of China (#23KJCX050).
Institution Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Zhejiang Normal University Ethics Committee (#No. ZSRT2022117).
Informed Consent Statement
Participants signed the inform consent prior to any assessment.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors are grateful to those who contributed to conduct this research, and especially thanks to the team coach Fei Peng.
Conflicts of Interest
All authors declare no conflict of interest.
References
- Gerrett, N.; Kingma, B.R.M.; Sluijter, R.; Daanen, H.A.M. Ambient Conditions Prior to Tokyo 2020 Olympic and Paralympic Games: Considerations for Acclimation or Acclimatization Strategies. Front Physiol 2019, 10, 414. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Clarkson, P.M.; Roberts, W.O. American College of Sports Medicine roundtable on hydration and physical activity: consensus statements. Curr Sports Med Rep 2005, 4, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Racinais, S.; Mohr, M.; Buchheit, M.; Voss, S.C.; Gaoua, N.; Grantham, J.; Nybo, L. Individual responses to short-term heat acclimatisation as predictors of football performance in a hot, dry environment. Br J Sports Med 2012, 46, 810–815. [Google Scholar] [CrossRef]
- Tatterson, A.J.; Hahn, A.G.; Martin, D.T.; Febbraio, M.A. Effects of heat stress on physiological responses and exercise performance in elite cyclists. J Sci Med Sport 2000, 3, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Convertino, V.A.; Armstrong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C., Jr.; Sherman, W.M. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 1996, 28, i–vii. [Google Scholar] [CrossRef] [PubMed]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.E.; Casa, D.J.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O. National Athletic Trainers’ Association Position Statement: Fluid Replacement for the Physically Active. J Athl Train 2017, 52, 877–895. [Google Scholar] [CrossRef]
- Casa, D.J.; Armstrong, L.E.; Hillman, S.K.; Montain, S.J.; Reiff, R.V.; Rich, B.S.; Roberts, W.O.; Stone, J.A. National athletic trainers’ association position statement: fluid replacement for athletes. J Athl Train 2000, 35, 212–224. [Google Scholar]
- Savoie, F.A.; Kenefick, R.W.; Ely, B.R.; Cheuvront, S.N.; Goulet, E.D. Effect of Hypohydration on Muscle Endurance, Strength, Anaerobic Power and Capacity and Vertical Jumping Ability: A Meta-Analysis. Sports Med 2015, 45, 1207–1227. [Google Scholar] [CrossRef]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 2007, 39, 377–390. [Google Scholar]
- Pence, J.; Bloomer, R.J. Impact of Nuun Electrolyte Tablets on Fluid Balance in Active Men and Women. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Wijering, L.A.J.; Cotter, J.D.; Rehrer, N.J. A randomized, cross-over trial assessing effects of beverage sodium concentration on plasma sodium concentration and plasma volume during prolonged exercise in the heat. Eur J Appl Physiol 2023, 123, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Ranchordas, M.K.; Tiller, N.B.; Ramchandani, G.; Jutley, R.; Blow, A.; Tye, J.; Drury, B. Normative data on regional sweat-sodium concentrations of professional male team-sport athletes. J Int Soc Sports Nutr 2017, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Shirreffs, S.M.; Aragon-Vargas, L.F.; Chamorro, M.; Maughan, R.J.; Serratosa, L.; Zachwieja, J.J. The sweating response of elite professional soccer players to training in the heat. Int J Sports Med 2005, 26, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Belval, L.N.; Hosokawa, Y.; Casa, D.J.; Adams, W.M.; Armstrong, L.E.; Baker, L.B.; Burke, L.; Cheuvront, S.; Chiampas, G.; González-Alonso, J. , et al. Practical Hydration Solutions for Sports. Nutrients 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Wingo, J.E. Exercise intensity prescription during heat stress: A brief review. Scand J Med Sci Sports 2015, 25 Suppl 1, 90–95. [Google Scholar] [CrossRef]
- Perez-Suarez, I.; Martin-Rincon, M.; Gonzalez-Henriquez, J.J.; Fezzardi, C.; Perez-Regalado, S.; Galvan-Alvarez, V.; Juan-Habib, J.W.; Morales-Alamo, D.; Calbet, J.A.L. Accuracy and Precision of the COSMED K5 Portable Analyser. Front Physiol 2018, 9, 1764. [Google Scholar] [CrossRef] [PubMed]
- Morris, N.B.; Cramer, M.N.; Hodder, S.G.; Havenith, G.; Jay, O. A comparison between the technical absorbent and ventilated capsule methods for measuring local sweat rate. J Appl Physiol (1985) 2013, 114, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; De Chavez, P.J.D.; Ungaro, C.T.; Sopena, B.C.; Nuccio, R.P.; Reimel, A.J.; Barnes, K.A. Exercise intensity effects on total sweat electrolyte losses and regional vs. whole-body sweat [Na(+)], [Cl(-)], and [K(+)]. Eur J Appl Physiol 2019, 119, 361–375. [Google Scholar] [CrossRef] [PubMed]
- Passe, D.; Horn, M.; Stofan, J.; Horswill, C.; Murray, R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int J Sport Nutr Exerc Metab 2007, 17, 284–295. [Google Scholar] [CrossRef]
- Emerson, D.M.; Torres-McGehee, T.M.; Emerson, C.C.; LaSalle, T.L. Individual fluid plans versus ad libitum on hydration status in minor professional ice hockey players. J Int Soc Sports Nutr 2017, 14, 25. [Google Scholar] [CrossRef]
- de Melo-Marins, D.; Souza-Silva, A.A.; da Silva-Santos, G.L.L.; Freire-Junior, F.A.; Lee, J.K.W.; Laitano, O. Personalized Hydration Strategy Attenuates the Rise in Heart Rate and in Skin Temperature Without Altering Cycling Capacity in the Heat. Front Nutr 2018, 5, 22. [Google Scholar] [CrossRef]
- Bardis, C.N.; Kavouras, S.A.; Adams, J.D.; Geladas, N.D.; Panagiotakos, D.B.; Sidossis, L.S. Prescribed Drinking Leads to Better Cycling Performance than Ad Libitum Drinking. Med Sci Sports Exerc 2017, 49, 1244–1251. [Google Scholar] [CrossRef]
- Lopez, R.M.; Casa, D.J.; Jensen, K.A.; Stearns, R.L.; DeMartini, J.K.; Pagnotta, K.D.; Roti, M.W.; Armstrong, L.E.; Maresh, C.M. Comparison of Two Fluid Replacement Protocols During a 20-km Trail Running Race in the Heat. J Strength Cond Res 2016, 30, 2609–2616. [Google Scholar] [CrossRef] [PubMed]
- Ayotte, D., Jr.; Corcoran, M.P. Individualized hydration plans improve performance outcomes for collegiate athletes engaging in in-season training. J Int Soc Sports Nutr 2018, 15, 27. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; De Chavez, P.J.D.; Nuccio, R.P.; Brown, S.D.; King, M.A.; Sopena, B.C.; Barnes, K.A. Explaining variation in sweat sodium concentration: effect of individual characteristics and exercise, environmental, and dietary factors. J Appl Physiol (1985) 2022, 133, 1250–1259. [Google Scholar] [CrossRef] [PubMed]
- Buono, M.J.; Claros, R.; Deboer, T.; Wong, J. Na+ secretion rate increases proportionally more than the Na+ reabsorption rate with increases in sweat rate. J Appl Physiol (1985) 2008, 105, 1044–1048. [Google Scholar] [CrossRef]
- Bates, G.P.; Miller, V.S. Sweat rate and sodium loss during work in the heat. J Occup Med Toxicol 2008, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- McCubbin, A.J.; Lopez, M.B.; Cox, G.R.; Caldwell Odgers, J.N.; Costa, R.J.S. Impact of 3-day high and low dietary sodium intake on sodium status in response to exertional-heat stress: a double-blind randomized control trial. Eur J Appl Physiol 2019, 119, 2105–2118. [Google Scholar] [CrossRef]
- Hamouti, N.; Fernandez-Elias, V.E.; Ortega, J.F.; Mora-Rodriguez, R. Ingestion of sodium plus water improves cardiovascular function and performance during dehydrating cycling in the heat. Scand J Med Sci Sports 2014, 24, 507–518. [Google Scholar] [CrossRef]
- Cheung, S.S.; McGarr, G.W.; Mallette, M.M.; Wallace, P.J.; Watson, C.L.; Kim, I.M.; Greenway, M.J. Separate and combined effects of dehydration and thirst sensation on exercise performance in the heat. Scand J Med Sci Sports 2015, 25 (Suppl. 1), 104–111. [Google Scholar] [CrossRef]
- Berkulo, M.A.; Bol, S.; Levels, K.; Lamberts, R.P.; Daanen, H.A.; Noakes, T.D. Ad-libitum drinking and performance during a 40-km cycling time trial in the heat. Eur J Sport Sci 2016, 16, 213–220. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).