Submitted:
02 April 2024
Posted:
03 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Selection of Animals
2.3. Blood Samples
2.4. Serology
2.5. Western Blotting
2.6. PCR Detection of T. cruzi
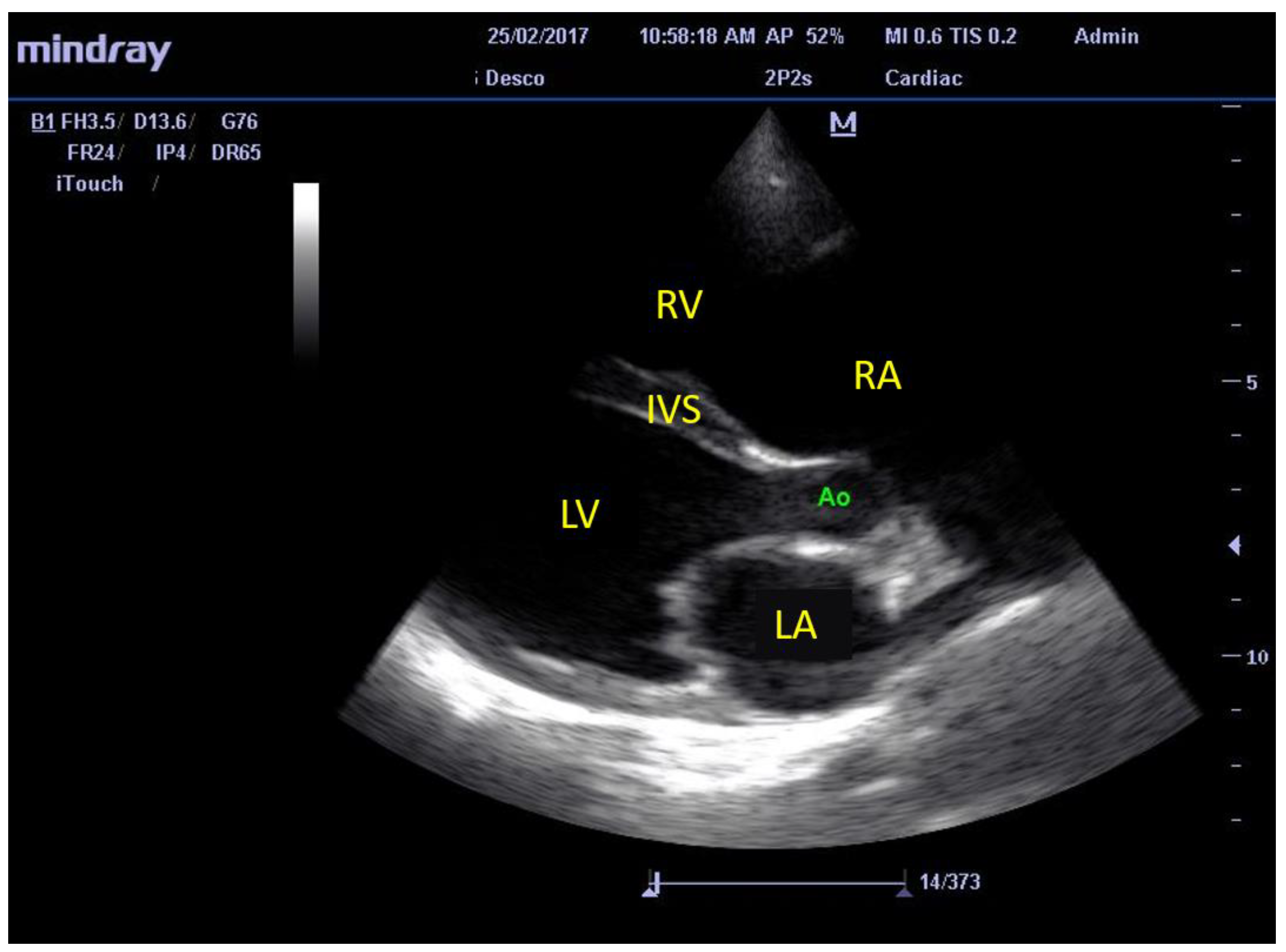
2.7. Echocardiographic Evaluation of Cardiac Structures and Function
2.8. Statistical Analysis
3. Results
3.1. Characteristics of T. cruzi Infection
3.2. Echocardiographic Findings
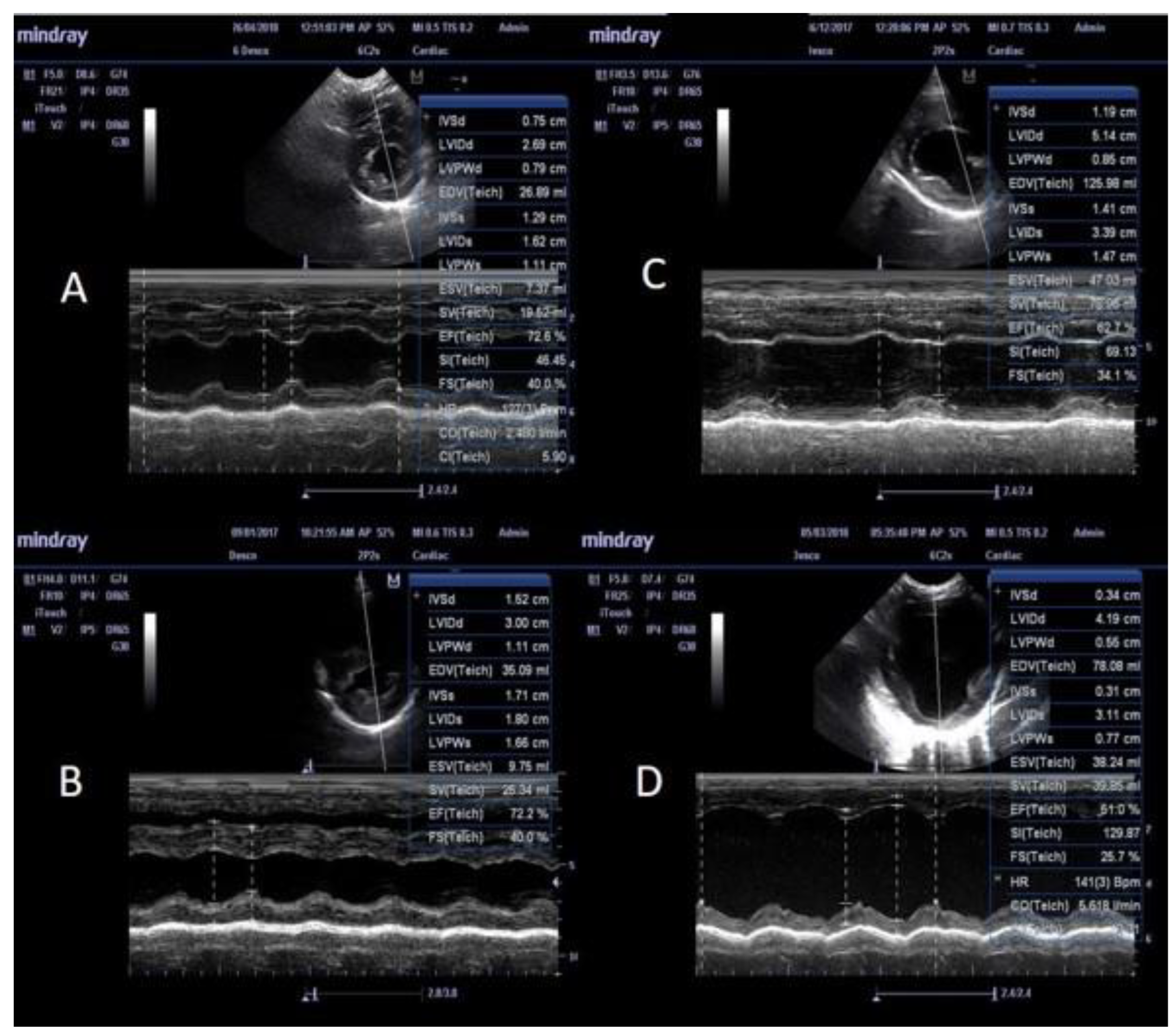
3.3. M-Mode Ultrasonographic Findings
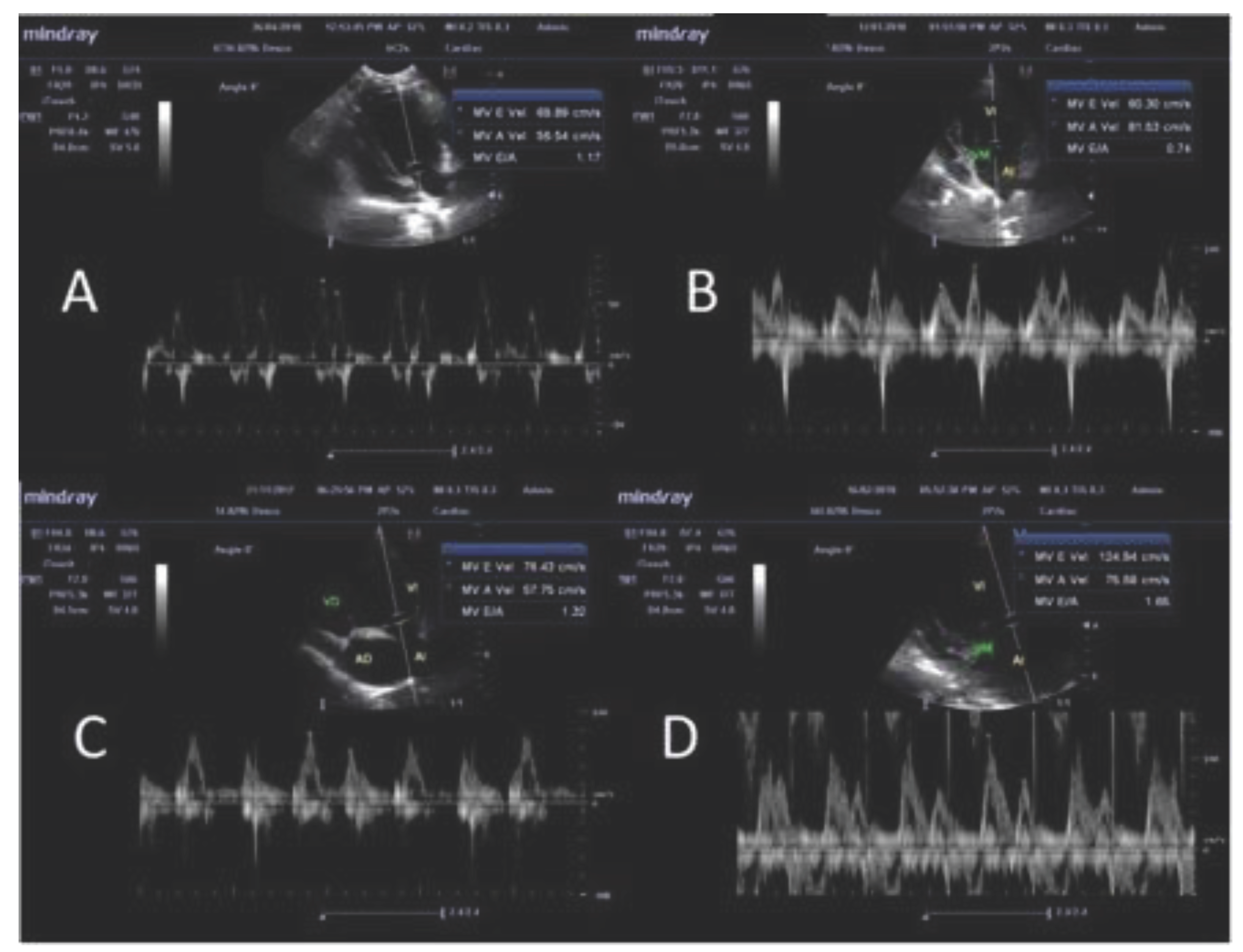
3.4. Pulse Doppler Ultrasonographic Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taylor, M.A.; Coop, R.L.; Wall, R.L. Veterinary Parasitology, 3rd ed.; Wiley-Blackwell: New Delhi, India, 2016; pp. 356–358. [Google Scholar]
- Weese, J.S.; Peregrine, A.S.; Anderson, M.E.C.; Fulford, M.B. Parasitic Diseases. In Companion Animal Zoonoses; Weese, J.S., Fulfords, M.B., Eds.; Wiley-Blackwell: Iowa, 2011; pp. 3–108. [Google Scholar]
- Jiménez-Coello, M.; Poot-Cob, M.; Ortega-Pacheco, A.; Guzma-Marin, E.; Ramos-Ligonio, A.; Sauri-Arceo, C.H.; Acosta-Viana, K.Y. American trypanosomiasis in dogs from an urban and rural area of Yucatan, Mexico. Vector Borne Zoonotic Dis. 2008, 8, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Coello, M.; Acosta-Viana, K.Y.; Guzmán-Marín, E.; Bárcenas-Irabién, A.; Ortega-Pacheco, A. American trypanosomiasis and associated risk factors in owned dogs from the major city of Yucatan, Mexico. J. Venom Anim. Toxins Incl. Trop. Dis. 2015, 21, 37. [Google Scholar] [CrossRef] [PubMed]
- Camacho, A.A. Miocardiopatía chagásica en caninos. In Afecciones Cardiovasculares en Pequeños Animales, Belerenian G.C.; Mucha, C.J., Camacho, A.A., Eds.; Inter-Médica: Buenos Aires, 2007; pp. 180–183. [Google Scholar]
- Guedes, P.M.M.; Veloso, V.M.; Alfonso, L.C.C.; Caliari, M.V.; Carneiro, C.M.; Diniz, L.F.; Marques-da-Silva, E.A.; Caldas, I.S.; do Valle Mata, M.A.; Souza, S.M.; Lana, M.; Chiari, E.; Galvao, L.M.C.; Bahia, M.T. Development of chronic cardiomyopathy in canine chagas disease correlates whith high IFN-gamma, TN-alpha, and low IL-10 production during the acute infection phase. Vet. Immunol. Immunopathol. 2009, 130, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Rassi, A. Jr.; Rassi, A.; Marin-Neto, J.A. Chagas disease. The Lancet 2010, 375, 1388–1402. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Nunes, M.C.; Dones, W.; Morillo, C.A.; Justiniano-Encina, J.; Ribeir, A.L. Chagas disease an overview of clinical and epidemiological aspects. J. Am. Coll. Cardiol. 2013, 62, 767–776. [Google Scholar]
- Barr, S.C.; Holmes, R.A.; Klei, T.R. Electrocardiographic and echocardiographic features of trypanosomiasis in dogs inoculated with North American Trypanosoma cruzi isolates. Am. J. Vet. Res. 1992, 53, 521–527. [Google Scholar] [CrossRef]
- Pascon, J.P.D.; Neto, G.B.P.; Sousa, M.G.; Sousa, M.G.; Paulino, D.; Camacho, A.A. Clinical characterization of chronic chagasic cardiomyopathy in dogs. Pesq. Vet. Bras. 2010, 30, 115–120. [Google Scholar] [CrossRef]
- Gompf, R.E. History and physical examination. In Manual of Canine and Feline Cardiology 5th ed.; Smith, F.W.K.; Tilley, L.P.; Oyama, M.; Sleeper, M.M. Eds.; Elsevier, St. Louis 2016. pp. 3–25.
- Tilley, L; Burtnick, N. ECG for the small animal practitioner. Teton New Media, Jackson Wyoming, 2009. pp. 64–84.
- Kittleson, M.D.; Kienle, R.D. Pulmonary arterial and systemic arterial hypertension. In: Small Animal Cardiovascular Medicine; Kittleson, M.D.; Kienle, R.D. Eds; Mosby, St. Louis, 1998. pp.1472-1845.
- Torres-Vargas, J.; Jimenez-Coello, M.; Guzman-Marin, E.; Acosta-Viana, K.Y.; Yadon, Z.E.; Gutierrez-Blanco, E.; Guillermo-Cordero, J.L.; Garg, N.J.; Ortega-Pacheco, A. Quantitative and histological assessment of maternal-fetal transmission of Trypanosoma cruzi in guinea pigs: An experimental model of congenital Chagas disease. PLOS Negl. Trop. Dis. 2018, 12, e0006222. [Google Scholar] [CrossRef] [PubMed]
- Boon, J.A. Veterinary Echocardiography, 2nd ed.; Wiley-Blackwell: USA, 2011; pp. 50–132. [Google Scholar]
- de Madron, E. Normal views: 2D, TM, spectral and color doppler, In: Clinical Echocardography of the Dog and Cat; de Madron, E., Chetboul, V., Bussadori, C., Eds.; Elsevier: St Luis, 2015. [Google Scholar]
- Boon, J.A. Two-dimensional and M-mode echocardiography for the small animal practitioner, 2nd ed.; Wiley-Blackwell: Iowa, 2016; pp. 75–83. [Google Scholar]
- Cornell, C.C.; Kittleson, M.D.; Della Torre, P.; Häggström, J.; Lombard, C.W.; Pedersen, H.D.; Vollmar, A.; Wey, A. Allometric scaling of M-mode cardiac measurements in normal adult dogs. J. Vet. Int. Med. 2004, 18, 311–321. [Google Scholar]
- Gallay-Lepoutre, J.; Bélanger, M.C.; Nadeau, M.E. Prospective evaluation of Doppler echocardiography, tissue Doppler imaging and biomarkers measurement for the detection of doxorubicin-induced cardiotoxicity in dogs: A pilot study. Res. Vet. Sci. 2016, 105, 153–159. [Google Scholar] [CrossRef]
- de Madron, E. Assessment of distolic function. In Clinical Echocardography of the Dog and Cat; de Madron, E., Chetboul, V., Bussadori, C., Eds.; Elsevier: St Louis, 2015; pp. 3–19. [Google Scholar]
- Chetboul, V. Dilated cardiomyopathy and other cardiomyopathies in dogs In Clinical Echocardiography of the Dog and Cat; de Madron, E., Chetboul, V., Bussadori, C., Eds.; Elsevier Masson: St Luis, 2016; pp 181–205.
- Salomone, O.A.; Juri, D.; Omelianiuk, M.O.; Sembaj, A.; Afiguerri, A.M.; Carriazo, C.; Barral, J.M.; Madoery, R. Prevalence of circulating Trypanosoma cruzi detected by polymerase chain reaction in patients with Chagas cardiomyopathy. Am. J. Cardiol. 2000, 85, 1274–1276. [Google Scholar] [CrossRef] [PubMed]
- Marin-Neto, J.A.; Cunha-Neto, E.; Maciel, B.C.; Simões, M.V. Pathogenesis of chronic Chagas heart disease. Circulation 2007, 115, 1109–1123. [Google Scholar] [CrossRef] [PubMed]
- Dumonteil, E.; Ramirez-Sierra, M.J.; Ferral, J.; Euan-Garcia, M.E.; Chavez-Nuñez, L. Usefulness of community participation for the fine temporal monitoring of house infestation by non-domiciliated triatomines. J. Parasitol. 2009, 95, 469–471. [Google Scholar] [CrossRef] [PubMed]
- Curtis-Robles, R.; Snowden, K.F.; Dominguez, B.; Dinges, L.; Rodgers, S.; Mays, G.; Hamer, S.A. Epidemiology and molecular typing of Trypanosoma cruzi in naturally-infected hound dogs and associated triatomine vectors in Texas, USA. PLOS Negl. Trop. Dis. 2017, 11, e0005298. [Google Scholar] [CrossRef]
- Meurs, K.M.; Anthony, M.A.; Slater, M.; Miller, M.W. Chronic Trypanosoma cruzi infection in dogs: 11 cases (1987-1996). J. Am. Vet. Med. Assoc. 1998, 213, 497–500. [Google Scholar] [CrossRef] [PubMed]
- Graiff, D.S. Relación entre perros seropositivos a Trypanosoma cruzi y alteraciones electrocardiográficas compatibles con miocardiopatía chagásica canina en la localidad de La Para (Córdoba-Argentina). MSc Thesis, Universidad Nacional del Litoral, Argentina. 2010.
- Vitt, J.P.; Saunders, A.B.; O'Brien, M.T.; Mansell, J.; Ajithdoss, D.K.; Hamer, S.A. Diagnostic features of acute Chagas myocarditis with sudden death in a family of boxer dogs. J. Vet. Intern. Med. 2016, 30, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Rassi, A.; de Rezende, A.J.M. American trypanosomiasis (Chagas disease). Infect. Dis. Clin. North. Am. 2012, 26, 275–291. [Google Scholar] [CrossRef]
- Steinl, D.C.; Xu, L.; Khanicheh, E.; Ellertsdottir, E.; Ochoa-Espinosa, A.; Mitterhuber, M.; Glatz, K.; Kuster, G.M.; Kaufmann, B.A. Noninvasive contrast-enhanced ultrasound molecular imaging detects myocardial inflammatory response in autoimmune myocarditis. Circ. Cardiovasc. Imaging, 2016, 9, e004720. [Google Scholar]
- Gironès, N.; Fresno, M. Etiology of Chagas disease myocarditis: autoimmunity, parasite persistence, or both? Trends. Parasitol. 2003, 19, 19–22. [Google Scholar] [CrossRef]
- Guedes, P.M.M.; Veloso, V.M.; Caliari, M.V.; Carneiro, C.M.; Souza, S.M.; de Lana, M.; Chiari, E.; Bahia, M.T.; Galvao, L.M.C. Trypanosoma cruzi high infectivity in vitro is related to cardiac lesions during long-term infection in Beagle dogs. Mem. Inst. Oswaldo Cruz, 2007, 102, 141–147. [Google Scholar] [CrossRef]
- Garzoni, L.R.; Adesse, D.; Soares, M.J.; Rossi, M.I.D.; Borojevic, R.; de Meirelles, M.D.L. Fibrosis and hypertrophy induced by Trypanosoma cruzi in a three-dimensional cardiomyocyte-culture system. J. Infect. Dis. 2008, 197, 906–915. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Neto, E.; Teixeira, P.C.; Nogueira, L.G.; Kalil. J. Autoimmunity. In Advances in Parasitology, Chagas Disease; Weiss, L.M., Tanowitz, H.B., Eds.; Elsevier Academic Press Inc.: San Diego, 2011; Volume 76, pp. 129–152.
- Jiménez-Coello, M.; Shelite, T.; Castellanos-Gonzalez, A.; Saldarriaga, O.; Rivero, R.; Ortega-Pacheco, A.; Acevedo-Arcique, C.; Amaya-Guardia, K.; Garg, N.; Melby, P.; Travi, B.L. Efficacy of recombinase polymerase amplification to diagnose Trypanosoma cruzi infection in dogs with cardiac alterations from an endemic area of Mexico. Vector Borne Zoonotic Dis. 2018, 18, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Miles, M.A.; Llewellyn, M.S.; Lewis, M.D.; Yeo, M.; Baleela, R.; Fitzpatrick, S.; Gaunt, M.W.; Mauricio, I.L. The molecular epidemiology and phylogeography of Trypanosoma cruzi and parallel research on Leishmania: looking back and to the future. Parasitology 2009, 136, 1509–1528. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, B.; Rico, T.; Sosa, S.; Oaxaca, E.; Vizcaino-Castillo, A.; Caballero, M.L.; Martínez, I. Mexican Trypanosoma cruzi Tc I strains with different degrees of virulence induce diverse humoral and cellular immune responses in a murine experimental infection model. J. Biomed. Biotechnol. 2010, 890672. [Google Scholar] [CrossRef]
- Sisson, D.D. Patophysiology of heart failure. In Textbook of Veterinary Internal Medicine, 7th ed.; Ettinger, S.J., Feldman, E.C., Eds.; Saunders; Elsevier: St Luis, 2010; pp. 1143–1158. [Google Scholar]
- Schober, K.E.; Fuentes, V.L. Effects of age, body weight, and heart rate on transmitral and pulmonary venous flow in clinically normal dogs. Am. J. Ve.t Res. 2001, 62, 1447–54. [Google Scholar] [CrossRef]
| Dilated cardiomyopathy | Group A Seronegative PCR positive |
Group B Seropositive PCR negative |
Group C Seropositive PCR positive |
Total |
| Absent | 23 | 6 | 86 | 115 |
| Present | 3 | - | 12 | 15 |
| Total | 26 | 6 | 98 | 130 |
| Parameters | Mode | A (n= 23) | Aw (n= 3) | B (n= 6) | C (n= 86) | Cw (n= 12) | Controls (n=16) |
| A: Structural features | |||||||
| IVS diastole (IVS-d)* 1 | M mode | 0.5 ± 0.07 a | 0.51 ± 0.05 | 0.4 ± 0.08 | 0.49 ± 0.08 b | 0.4 ± 0.08 a, b | 0.44 ± 0.07 |
| IVS systole (IVS-s)* 1 | M mode | 0.69 ± 0.01 | 0.66 ± 0.05 | 0.67 ± 0.17 | 0.7 ± 0.15 | 0.64 ± 0.18 | 0.64 ± 0.09 |
| LVID diastole (LVID-d)* 2 | M mode | 1.44 ± 0.24 a, | 2.02 ± 0.16 a, b | 1.57 ± 0.20 b, c | 1.35 ± 0.25 b, c, d | 2.05 ± 0.15a ,c ,d, e | 1.55 ± 0.1 b, d, e |
| LVID systole (LVID-s)* 2 | M mode | 0.83 ± 0.18 a | 1.15 ± 0.10 a, b | 0.91 ± 0.13 c | 0.76 ± 0.2 b | 1.23 ± 0.19 a, c | 0.86 ± 0.1 b |
| LVPW diastole (LVPW-d)* 2 | M mode | 0.51 ± 0.09 a | 0.39 ± 0.16 a | 0.34 ± 0.03 a, b | 0.49 ± 0.1 b, c, d | 0.4 ± 0.09 a, c, d, e | 0.47 ± 0.06 b, d, e |
| LVPW systole (LVPW-s)*2 | M mode | 0.71 ± 0.09 a | 0.62 ± 0.18 | 0.53 ± 0.11 a, b | 0.73 ± 0.12 b | 0.69 ± 0.19 b | 0.68 ± 0.08 b |
| EPSS 1 | M mode | 0.39 ± 0.21a | 0.93 ± 0.13 b | 0.5 ± 0.2 | 0.31 ± 0.21 b, c | 0.96 ± 0.09 a, c, d | 0.27 ± 0.11 b, d |
| LA/Ao 1 | B mode | 1.39 ± 0.51 a | 1.69 ± 0.51 | 1.38 ± 0.17 | 1.25 ± 0.24 b | 1.86 ± 0.43 a, b, c | 1.19 ± 0.14 c |
| SI 1 | B & M mode | 1.99 ± 0.21 a | 1.54 ± 0.1 b | 1.87 ± 0.19 | 1.97 ± 0.24 b, c | 1.53 ± 0.08 a, c | 1.75 ± 0.07 a, c |
| B: Functional features | |||||||
| Fractional shortening (FS), %** 1 | M mode | 40.35 ± 6.66 | 40.33 ± 5.69 | 38.83 ± 5.03 | 41.39 ± 11.2 | 37 ± 10.72 | 41.75 ± 5.36 |
| Ejection fraction (EF), %** 1 | M mode | 72.61 ± 7.69 | 71.2 ± 7.30 | 68.33 ± 7.51 | 72.75 ± 12.58 | 64.17 ± 14.1 | 74.09 ± 6.68 |
| Stroke volume (SV), mL** 1 | M mode | 20.85 ± 14.37 a | 33.52 ± 14.77 | 27.49 ± 26.35 | 22.17 ± 15.5 b | 51.18 ± 28.4 a, b | 24.01 ± 10.97 |
| Heart rate 1 | M mode | 102.43 ± 17.98 | 121 ± 8.54 | 95.33 ± 8.71 | 102.5 ± 31.57 | 121.25 ± 41.29 | 108.75 ± 23.95 |
| Cardiac output (CO), L/min** 1 | M mode | 2.1 ± 1.31 a | 4 ± 1.53 | 2.63 ± 2.52 | 2.22 ± 1.55 b | 6.6 ± 5.13 a, b | 2.46 ± 0.81 |
| E/A ratio 1 | PW Doppler | 1.53 ± 0.34 a | 1.24 ± 0.24 | 1.35 ± 0.26 | 1.37 ± 0.34 | 1.41 ± 0.61 | 1.1 ± 0.29 a |
| Age, years 1 | ….. | 9.83 ± 3.46 a | 7.33 ± 3.78 | 7.33 ± 3.33 | 8.52 ± 4.01 | 9.83 ± 2.25 | 5.94 ± 3.23 a |
| Weight, kg 1 | ….. | 8.41 ± 6.31 | 9.53 ± 7.33 | 13.06 ± 11.86 | 12.77 ± 10.03 | 16.03 ± 18.61 | 9.56 ± 6.84 |
| Parameters | Mode | A (n=23) | B (n=6) | C (n=85) | Reference value | |||
| Increase (%) | Decrease (%) | Increase (%) | Decrease (%) | Increase (%) | Decrease (%) | |||
| IVS at diastole (IVS-d) | M mode | 4.35 | … | … | … | 8.24 | 1.18 | 0.29 - 0.59 1 |
| IVS at systole (IVS-s) | M mode | 13.04 | … | 16.67 | … | 22.35 | 2.35 | 0.43 - 0.79 1 |
| LVID at diastole (LVID-d) | M mode | … | 21.74 | … | 16.67 | … | 38.82 | 1.27 - 1.85 1 |
| LVID at systole (LVID-s) | M mode | … | 21.74 | … | … | … | 42.35 | 0.71 - 1.26 1 |
| LVPW at diastole (LVPW-d) | M mode | 13.04 | … | … | … | 10.59 | 1.18 | 0.29 - 0.60 1 |
| LVPW at systole (LVPW-s) | M mode | … | … | … | 33.33 | 9.41 | 1.18 | 0.48 - 0.87 1 |
| Fractional shortening (FS) | M mode | 8.70 | 13.04 | … | 16.67 | 22.35 | 20.00 | 33.6 - 49.9 2 |
| Ejection fraction (EF) | M mode | 8.70 | 4.35 | … | 16.67 | 22.35 | 12.94 | 58.9 - 82.9 3 |
| E/A ratio | PW Doppler | 26.09 | 8.70 | 16.67 | … | 11.76 | 3.53 | 0.98 - 1.7 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





