Submitted:
03 April 2024
Posted:
03 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
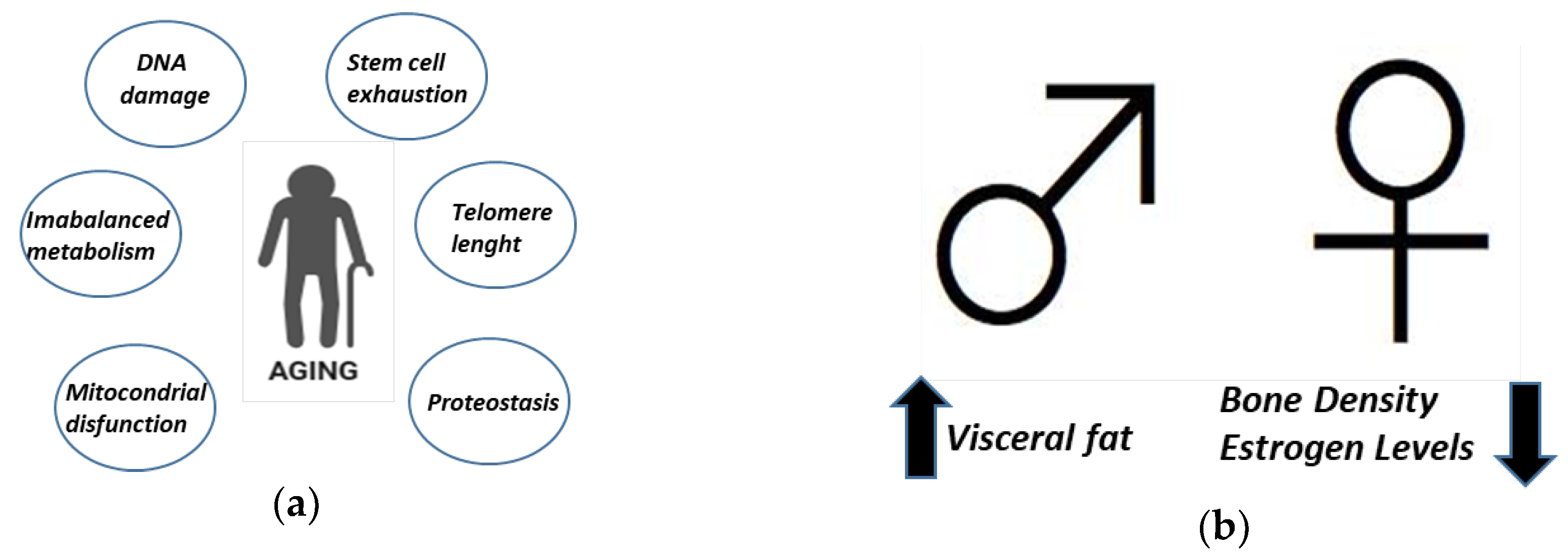
2.1. Aging
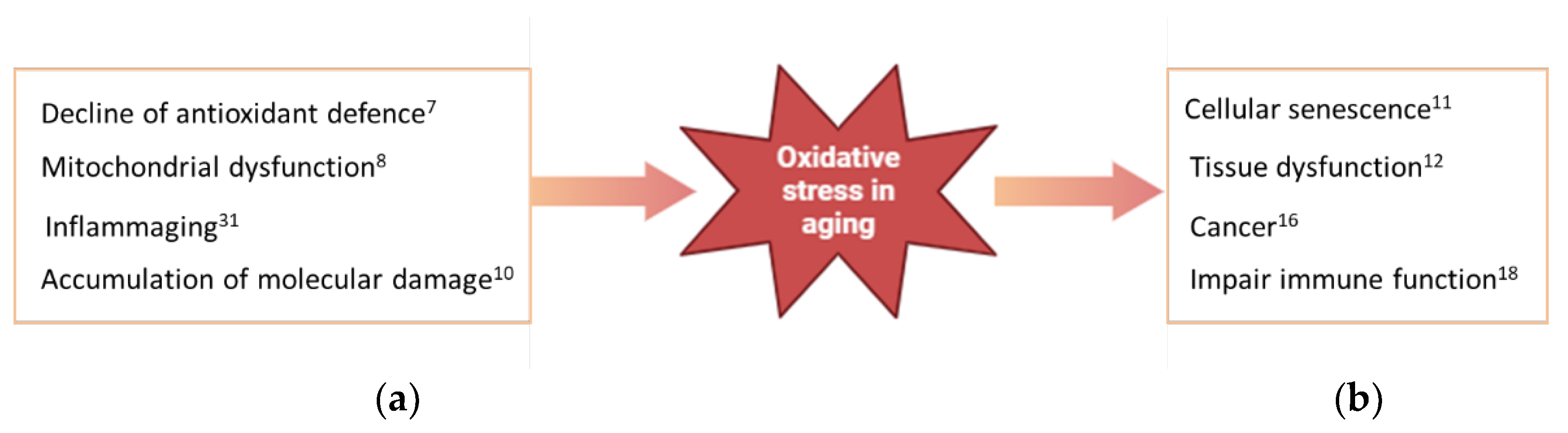
2.2. Oxidative Stress in Aging
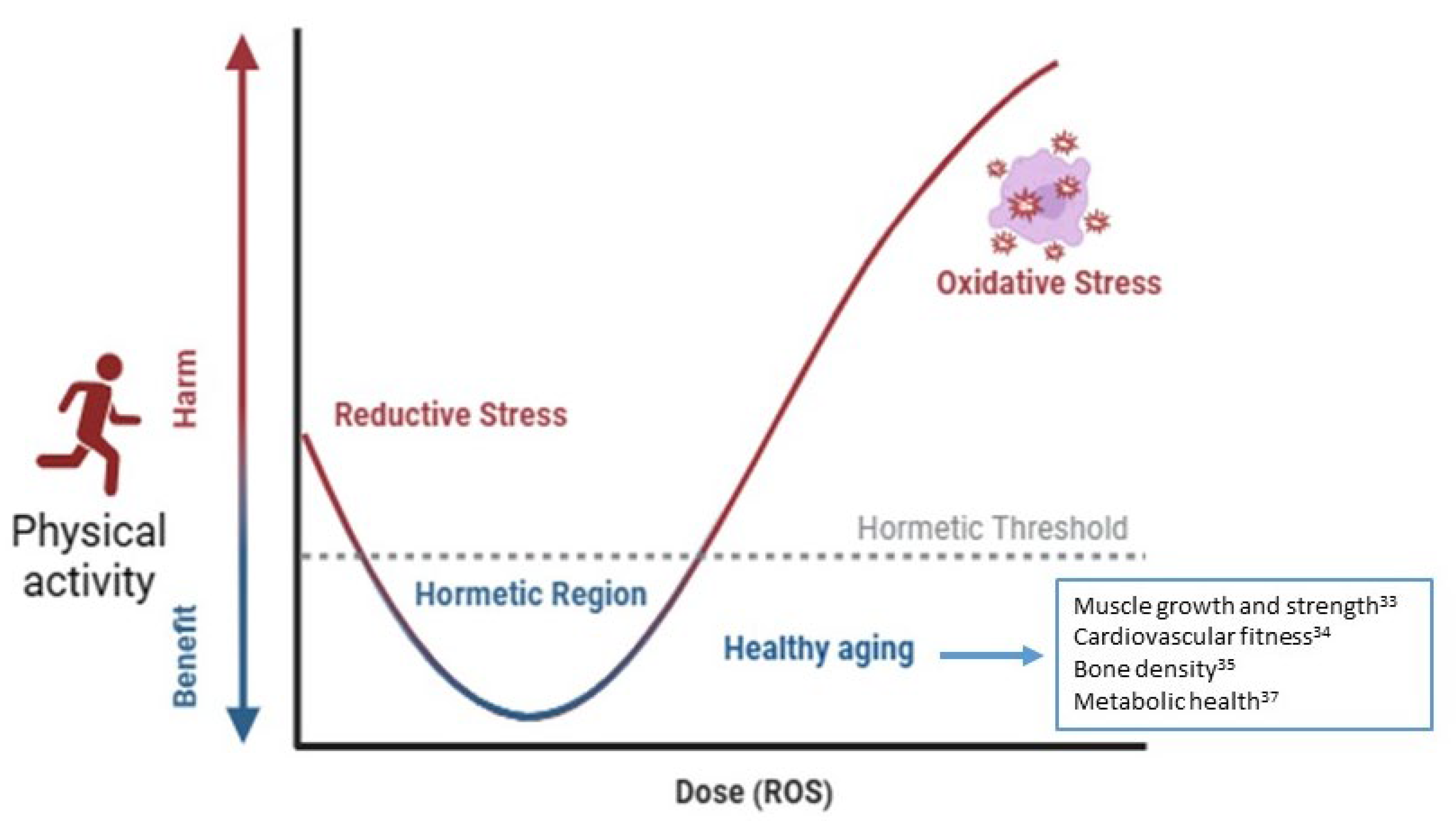
2.3. Hormesis, Aging and Physical Activity
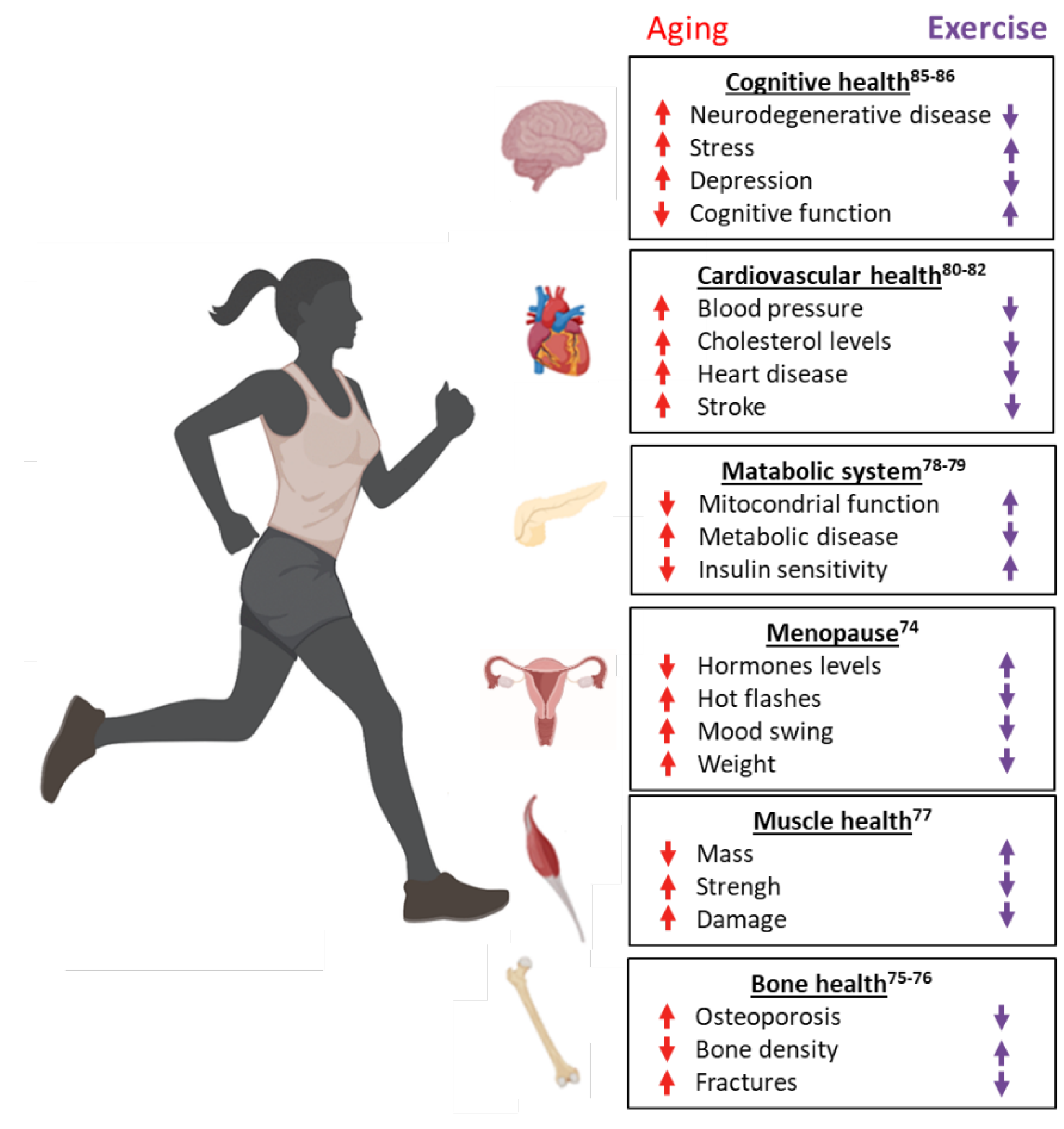
2.4. Physical Activity in Aging
2.5. Sarcopenia in Aging
2.5. Sarcopenia, Mitochondrial Dysfunction and Physical Activity
2.6. Aging and Physical Activity in Women
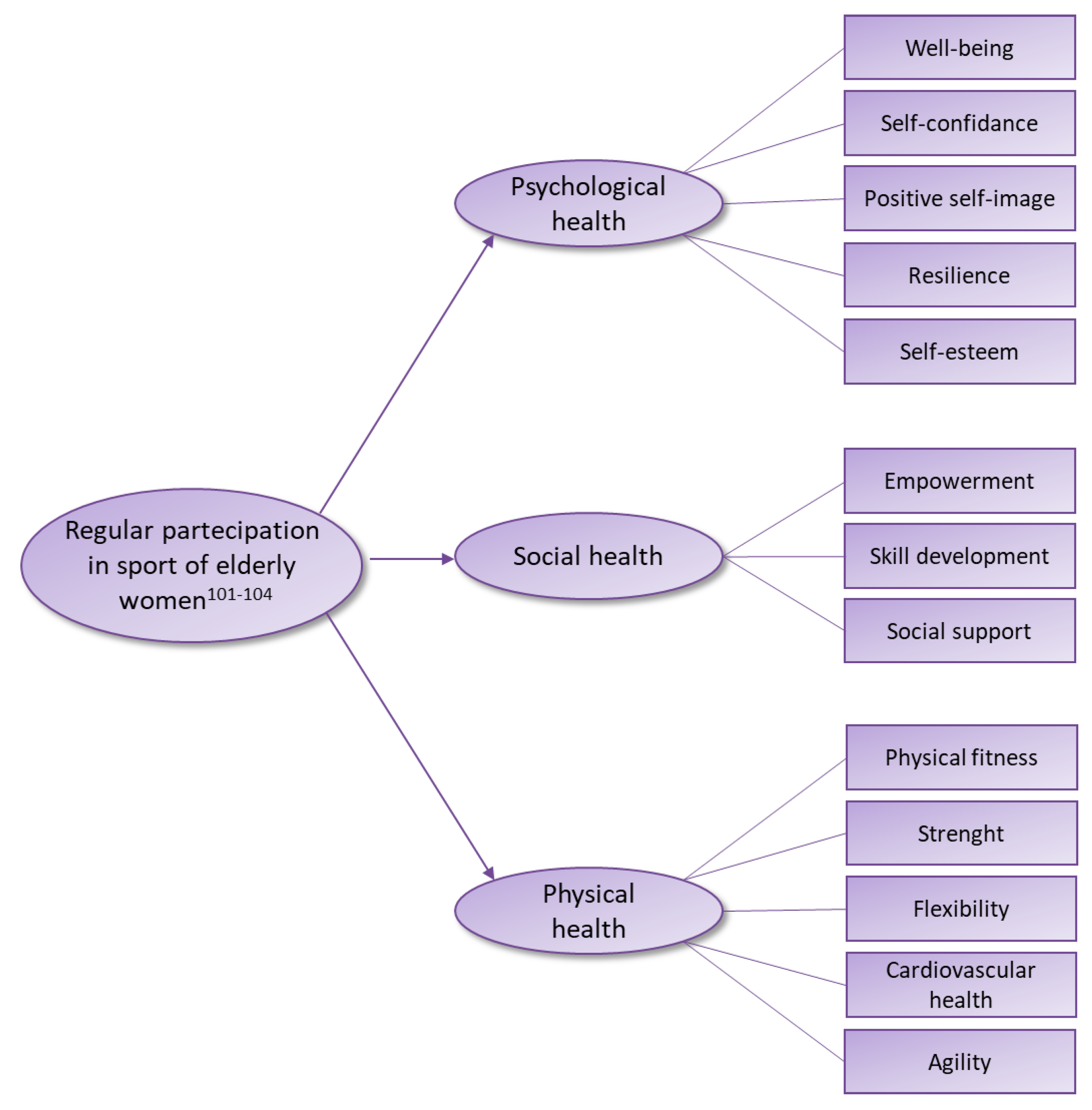
2.7. Sport and Elderly Women
5. Conclusions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Dziechciaż, M.; Filip, R. Biological psychological and social determinants of old age: bio-psycho-social aspects of human aging. Ann Agric Environ Med. 2014, 21, 835–8. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Bustamante-Sanchez, Á.; Mielgo-Ayuso, J.; Martínez-Guardado, I.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Antioxidants and Sports Performance. Nutrients. 2023, 15, 2371. [Google Scholar] [CrossRef]
- Ferrucci, L.; Gonzalez-Freire, M.; Fabbri, E.; Simonsick, E.; Tanaka, T.; Moore, Z.; Salimi, S.; Sierra, F.; de Cabo, R. Measuring biological aging in humans: A quest. Aging Cell. 2020, 19, e13080. [Google Scholar] [CrossRef] [PubMed]
- Hägg, S.; Jylhävä, J. Sex differences in biological aging with a focus on human studies. Elife. 2021, 10, e63425. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Mills, K.; le Cessie, S.; Noordam, R.; van Heemst, D. Ageing, age-related diseases and oxidative stress: What to do next? Ageing Res Rev. 2020, 57, 100982. [Google Scholar] [CrossRef]
- Viña, J.; Olaso-Gonzalez, G.; Arc-Chagnaud, C.; De la Rosa, A.; Gomez-Cabrera, M.C. Modulating Oxidant Levels to Promote Healthy Aging. Antioxid Redox Signal. 2020, 33, 570–579. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Miller, B.; Kumagai, H.; Silverstein, A.R.; Flores, M.; Yen, K. Mitochondrial-derived peptides in aging and age-related diseases. Geroscience. 2021, 43, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Vatic, M.; von Haehling, S.; Ebner, N. Inflammatory biomarkers of frailty. Exp Gerontol. 2020, 133, 110858. [Google Scholar] [CrossRef] [PubMed]
- Schaum, N.; Lehallier, B.; Hahn, O.; Pálovics, R.; Hosseinzadeh, S.; Lee, S.E.; Sit, R.; Lee, D.P.; Losada, P.M.; Zardeneta, M.E.; Fehlmann, T.; Webber, J.T.; McGeever, A.; Calcuttawala, K.; Zhang, H.; Berdnik, D.; Mathur, V.; Tan, W.; Zee, A.; Tan, M.; Tabula Muris Consortium; Pisco, A. O.; Karkanias, J.; Neff, N.F.; Keller, A.; Darmanis, S.; Quake, S.R.; Wyss-Coray, T. Ageing hallmarks exhibit organ-specific temporal signatures. Nature. 2020, 583, 596–602. [Google Scholar] [CrossRef]
- Finkel, T.; Holbrook, N.J. Oxidants, oxidative stress and the biology of ageing. Nature. 2000, 408, 239–47. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.C.; Bennett, M. Aging and atherosclerosis: mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ Res. 2012, 111, 245–59. [Google Scholar] [CrossRef] [PubMed]
- Hajam, Y.A.; Rani, R.; Ganie, S.Y.; Sheikh, T.A.; Javaid, D.; Qadri, S.S.; Pramodh, S.; Alsulimani, A.; Alkhanani, M.F.; Harakeh, S.; Hussain, A.; Haque, S.; Reshi, M.S. Oxidative Stress in Human Pathology and Aging: Molecular Mechanisms and Perspectives. Cells. 2022, 11, 552. [Google Scholar] [CrossRef] [PubMed]
- Ionescu-Tucker, A.; Cotman, C.W. Emerging roles of oxidative stress in brain aging and Alzheimer’s disease. Neurobiol Aging. 2021, 107, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Trist, B.G.; Hare, D.J.; Double, K.L. Oxidative stress in the aging substantia nigra and the etiology of Parkinson’s disease. Aging Cell. 2019, 18, e13031. [Google Scholar] [CrossRef]
- Jelic, M.D.; Mandic, A.D.; Maricic, S.M.; Srdjenovic, B.U. Oxidative stress and its role in cancer. J Cancer Res Ther. 2021, 17, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Klaunig, J.E. Oxidative Stress and Cancer. Curr Pharm Des. 2018, 24, 4771–4778. [Google Scholar] [CrossRef] [PubMed]
- Martínez de Toda, I.; Vida, C.; Sanz San Miguel, L.; De la Fuente, M. Function, Oxidative, and Inflammatory Stress Parameters in Immune Cells as Predictive Markers of Lifespan throughout Aging. Oxid Med Cell Longev. 2019, 2019, 4574276. [Google Scholar] [CrossRef] [PubMed]
- Frasca, D.; Blomberg, B.B. Adipose tissue, immune aging, and cellular senescence. Semin Immunopathol. 2020, 42, 573–587. [Google Scholar] [CrossRef] [PubMed]
- Harman, D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956, 11, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Finkel, T.; Holbrook, N.J. Oxidative stress and aging: Catalase is a longevity determinant enzyme. Nature. 2000, 408, 239. [Google Scholar] [CrossRef]
- Evans, J.L.; Goldfine, I.D.; Maddux, B.A.; Grodsky, G.M. Are oxidative stress-activated signaling pathways mediators of insulin resistance and β-cell dysfunction? Diabetes. 2003, 52, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, X.; Vikash, V.; Ye, Q.; Wu, D.; Liu, Y.; Dong, W. ROS and ROS-Mediated Cellular Signaling. Oxid. Med. Cell. Longev. 2016, 2016, 4350965. [Google Scholar] [CrossRef] [PubMed]
- Dröge, W. Free radicals in the physiological control of cell function. Physiol. Rev. 2002, 82, 47–95. [Google Scholar] [CrossRef] [PubMed]
- Kaludercic, N.; Mialet-Perez, J.; Paolocci, N.; Parini, A.; Di Lisa, F. Monoamine oxidases as sources of oxidants in the heart. J. Mol. Cell. Cardiol. 2014, 73, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Yasui, H.; Hayashi, S.; Sakurai, H. Possible involvement of singlet oxygen species as multiple oxidants in p450 catalytic reactions. Drug Metab. Pharmacokinet. 2005, 20, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Southam, C.M.; Erhlich, J. Effects of extracts of western red-cedar heartwood on certain wood-decaying fungi in culture. Phytophathology 1943, 33, 517–524. [Google Scholar]
- Rattan, S.I. Hormesis in aging. Ageing Res Rev. 2008, 7, 63–78. [Google Scholar] [CrossRef] [PubMed]
- Bayod, S.; Del Valle, J.; Lalanza, J.F.; Sanchez-Roige, S.; de Luxán-Delgado, B.; Coto-Montes, A.; Canudas, A.M.; Camins, A.; Escorihuela, R.M.; Pallàs, M. Long-term physical exercise induces changes in sirtuin 1 pathway and oxidative parameters in adult rat tissues. Exp Gerontol. 2012, 47, 925–35. [Google Scholar] [CrossRef] [PubMed]
- Martel, J.; Ojcius, D.M.; Ko, Y.F.; Ke, P.Y.; Wu, C.Y.; Peng, H.H.; Young, J.D. Hormetic Effects of Phytochemicals on Health and Longevity. Trends Endocrinol Metab. 2019, 30, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Ristow, M.; Zarse, K. How increased oxidative stress promotes longevity and metabolic health: The concept of mitochondrial hormesis (mitohormesis). Exp Gerontol. 2010, 45, 410–8. [Google Scholar] [CrossRef] [PubMed]
- Santoro, A.; Martucci, M.; Conte, M.; Capri, M.; Franceschi, C.; Salvioli, S. Inflammaging, hormesis and the rationale for anti-aging strategies. Ageing Res Rev. 2020, 64, 101142. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.L.; Kang, C.; Zhang, Y. Exercise-induced hormesis and skeletal muscle health. Free Radic Biol Med. 2016, 98, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Di Raimondo, D.; Rizzo, G.; Musiari, G.; Tuttolomondo, A.; Pinto, A. Role of Regular Physical Activity in Neuroprotection against Acute Ischemia. Int J Mol Sci. 2020, 21, 9086. [Google Scholar] [CrossRef]
- Ashe, M.C.; Santos, I.K.D.; Edward, N.Y.; Burnett, L.A.; Barnes, R.; Fleig, L.; Puyat, J.H.; Sale, J.E.M.; McKay, H.A.; Giangregorio, L.M. Physical Activity and Bone Health in Men: A Systematic Review and Meta-Analysis. J Bone Metab. 2021, 28, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.A.; Scott, D.; Seibel, M.J.; Cumming, R.G.; Naganathan, V.; Blyth, F.M.; Le Couteur, D.G.; Waite, L.M.; Handelsman, D.J.; Hirani, V. Higher-Impact Physical Activity Is Associated With Maintenance of Bone Mineral Density But Not Reduced Incident Falls or Fractures in Older Men: The Concord Health and Aging in Men Project. J Bone Miner Res. 2021, 36, 662–672. [Google Scholar] [CrossRef] [PubMed]
- Amanat, S.; Ghahri, S.; Dianatinasab, A.; Fararouei, M.; Dianatinasab, M. Exercise and Type 2 Diabetes. Adv Exp Med Biol. 2020, 1228, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Tamura, Y.; Omura, T.; Toyoshima, K.; Araki, A. Nutrition Management in Older Adults with Diabetes: A Review on the Importance of Shifting Prevention Strategies from Metabolic Syndrome to Frailty. Nutrients. 2020, 12, 3367. [Google Scholar] [CrossRef] [PubMed]
- Nuzum, H.; Stickel, A.; Corona, M.; Zeller, M.; Melrose, R.J.; Wilkins, S.S. Potential Benefits of Physical Activity in MCI and Dementia. Behav Neurol. 2020, 2020, 7807856. [Google Scholar] [CrossRef] [PubMed]
- Nuzum, H.; Stickel, A.; Corona, M.; Zeller, M.; Melrose, R.J.; Wilkins, S.S. Potential Benefits of Physical Activity in MCI and Dementia. Behav Neurol. 2020, 2020, 7807856. [Google Scholar] [CrossRef] [PubMed]
- Fiorenza, M.; Gliemann, L.; Brandt, N.; Bangsbo, J. Hormetic modulation of angiogenic factors by exercise-induced mechanical and metabolic stress in human skeletal muscle. Am J Physiol Heart Circ Physiol. 2020, 319, H824–H834. [Google Scholar] [CrossRef] [PubMed]
- Santoro, A.; Martucci, M.; Conte, M.; Capri, M.; Franceschi, C.; Salvioli, S. Inflammaging, hormesis and the rationale for anti-aging strategies. Ageing Res Rev. 2020, 64, 101142. [Google Scholar] [CrossRef] [PubMed]
- Eckstrom, E.; Neukam, S.; Kalin, L.; Wright, J. Physical Activity and Healthy Aging. Clin Geriatr Med. 2020, 36, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Nystoriak, M.A.; Bhatnagar, A. Cardiovascular Effects and Benefits of Exercise. Front Cardiovasc Med. 2018, 5, 135. [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016, 17, 567–80. [Google Scholar] [CrossRef] [PubMed]
- Wanigatunga, A.A.; Tudor-Locke, C.; Axtell, R.S.; Glynn, N.W.; King, A.C.; McDermott, M.M.; Fielding, R.A.; Lu, X.; Pahor, M.; Manini, T.M. Effects of a Long-Term Physical Activity Program on Activity Patterns in Older Adults. Med Sci Sports Exerc. 2017, 49, 2167–2175. [Google Scholar] [CrossRef] [PubMed]
- Merom, D.; Stanaway, F.; Gebel, K.; Sweeting, J.; Tiedemann, A.; Mumu, S.; Ding, D. Supporting active ageing before retirement: a systematic review and meta-analysis of workplace physical activity interventions targeting older employees. BMJ Open. 2021, 11, e045818. [Google Scholar] [CrossRef] [PubMed]
- Gamberi, T.; Gorini, G.; Fiaschi, T.; Morucci, G.; Pratesi, S.; et al. Effect of Functional Fitness on Plasma Oxidation Level in Elders: Reduction of the Plasma Oxidants and Improvement of the Antioxidant Barrier. American Journal of Sports Science 2018, 6, 55–64. [Google Scholar] [CrossRef]
- Morucci, G.; Ryskalin, L.; Pratesi, S.; Branca, J.J.V.; Modesti, A.; Modesti, P.A.; Gulisano, M.; Gesi, M. Effects of a 24-Week Exercise Program on Functional Fitness, Oxidative Stress, and Salivary Cortisol Levels in Elderly Subjects. Medicina 2022, 58, 1341. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.; El Assar, M.; Álvarez-Bustos, A.; Rodríguez-Mañas, L. Physical activity and exercise: Strategies to manage frailty. Redox Biol. 2020, 35, 101513. [Google Scholar] [CrossRef] [PubMed]
- Billot, M.; Calvani, R.; Urtamo, A.; Sánchez-Sánchez, J.L.; Ciccolari-Micaldi, C.; Chang, M.; Roller-Wirnsberger, R.; Wirnsberger, G.; Sinclair, A.; Vaquero-Pinto, N.; Jyväkorpi, S.; Öhman, H.; Strandberg, T.; Schols, J.M.G.A.; Schols, A.M.W.J.; Smeets, N.; Topinkova, E.; Michalkova, H.; Bonfigli, A.R.; Lattanzio, F.; Rodríguez-Mañas, L.; Coelho-Júnior, H.; Broccatelli, M.; D’Elia, M.E.; Biscotti, D.; Marzetti, E.; Freiberger, E. Preserving Mobility in Older Adults with Physical Frailty and Sarcopenia: Opportunities, Challenges, and Recommendations for Physical Activity Interventions. Clin Interv Aging. 2020, 15, 1675–1690. [Google Scholar] [CrossRef] [PubMed]
- Barajas-Galindo, D.E.; González Arnáiz, E.; Ferrero Vicente, P.; Ballesteros-Pomar, M.D. Effects of physical exercise in sarcopenia. A systematic review. Endocrinol Diabetes Nutr (Engl Ed). 2021, 68, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Rosenburg, I. Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr. 1989, 50, 1231–1233. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Landi, F.; Cesari, M.; Fielding, R.A.; Visser, M.; Engelke, K.; et al. Pitfalls in the measurement of muscle mass: a need for a reference standard. J Cachexia Sarcopenia Muscle. 2018, 9, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, T. Efficacy of progressive resistance training interventions in older adults in nursing homes: a systematic review. J Am Med Dir Assoc. 2012, 13, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Cannataro, R.; Carbone, L.; Petro, J.L.; Cione, E.; Vargas, S.; Angulo, H.; Forero, D.A.; Odriozola-Martínez, A.; Kreider, R.B.; Bonilla, D.A. Sarcopenia: Etiology, Nutritional Approaches, and Mirnas. Int. J. Mol. Sci. 2021, 22, 9724. [Google Scholar] [CrossRef] [PubMed]
- Martin, F.C.; Ranhoff, A.H. Frailty and Sarcopenia. 2020 Aug 21. In: Falaschi P, Marsh D, editors. Orthogeriatrics: The Management of Older Patients with Fragility Fractures [Internet]. 2nd ed. Cham (CH): Springer; [PubMed]
- Bao, W.; Sun, Y.; Zhang, T.; Zou, L.; Wu, X.; Wang, D.; Chen, Z. Exercise Programs for Muscle Mass, Muscle Strength and Physical Performance in Older Adults with Sarcopenia: A Systematic Review and Meta-Analysis. Aging Dis. 2020, 11, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Mende, E.; Moeinnia, N.; Schaller, N.; Weiß, M.; Haller, B.; Halle, M.; Siegrist, M. Progressive machine-based resistance training for prevention and treatment of sarcopenia in the oldest old: A systematic review and meta-analysis. Exp Gerontol. 2022, 163, 111767. [Google Scholar] [CrossRef] [PubMed]
- Marcos-Pardo, P.J.; González-Gálvez, N.; López-Vivancos, A.; Espeso-García, A.; Martínez-Aranda, L.M.; Gea-García, G.M.; Orquín-Castrillón, F.J.; Carbonell-Baeza, A.; Jiménez-García, J.D.; Velázquez-Díaz, D.; Cadenas-Sanchez, C.; Isidori, E.; Fossati, C.; Pigozzi, F.; Rum, L.; Norton, C.; Tierney, A.; Äbelkalns, I.; Klempere-Sipjagina, A.; Porozovs, J.; Hannola, H.; Niemisalo, N.; Hokka, L.; Jiménez-Pavón, D.; Vaquero-Cristóbal, R. Sarcopenia, Diet, Physical Activity and Obesity in European Middle-Aged and Older Adults: The LifeAge Study. Nutrients. 2020, 13, 8. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.J.; Lim, Y.H.; Yun, J.M.; Yoon, H.J.; Park, M. Sex- and age-specific effects of energy intake and physical activity on sarcopenia. Sci Rep. 2020, 10, 9822. [Google Scholar] [CrossRef] [PubMed]
- Fukunaga, T.; Mori, S.; Omura, T.; Noda, Y.; Fujita, Y.; Ohsawa, I.; Shigemoto, K. Muscle Fiber Type Specific Alterations of Mitochondrial Respiratory Function and Morphology in Aged Female Mice. Biochem. Biophys. Res. Commun. 2021, 540, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Mankhong, S.; Kim, S.; Moon, S.; Kwak, H.B.; Park, D.H.; Kang, J.H. Experimental Models of Sarcopenia: Bridging Molecular Mechanism and Therapeutic Strategy. Cells. 2020, 9, 1385. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.-H.; Singh, S.P.; Raffaele, M.; Waldman, M.; Hochhauser, E.; Ospino, J.; Arad, M.; Peterson, S.J. Adipocyte-Specific Expression of PGC1α Promotes Adipocyte Browning and Alleviates Obesity-Induced Metabolic Dysfunction in an HO-1-Dependent Fashion. Antioxidants. 2022, 11, 1147. [Google Scholar] [CrossRef] [PubMed]
- Delrieu, L.; Martin, A.; Touillaud, M.; Pérol, O.; Morelle, M.; Febvey-Combes, O.; Freyssenet, D.; Friedenreich, C.; Dufresne, A.; Bachelot, T.; et al. Sarcopenia and Serum Biomarkers of Oxidative Stress after a 6-Month Physical Activity Intervention in Women with Metastatic Breast Cancer: Results from the ABLE Feasibility Trial. Breast Cancer Res. Treat. 2021, 188, 601. [Google Scholar] [CrossRef]
- Luo, J.; Mills, K.; le Cessie, S.; Noordam, R.; van Heemst, D. Ageing, Age-Related Diseases and Oxidative Stress: What to Do Next? Ageing Res. Rev. 2020, 57, 100982. [Google Scholar] [CrossRef] [PubMed]
- Kadoguchi, T.; Shimada, K.; Miyazaki, T.; Kitamura, K.; Kunimoto, M.; Aikawa, T.; Sugita, Y.; Ouchi, S.; Shiozawa, T.; Yokoyama-Nishitani, M.; et al. Promotion of Oxidative Stress Is Associated with Mitochondrial Dysfunction and Muscle Atrophy in Aging Mice. Geriatr. Gerontol. Int. 2020, 20, 78–84. [Google Scholar] [CrossRef]
- Tang, H.; Inoki, K.; Brooks, S.V.; Okazawa, H.; Lee, M.; Wang, J.; Kim, M.; Kennedy, C.L.; Macpherson, P.C.D.; Ji, X.; et al. MTORC1 Underlies Age-related Muscle Fiber Damage and Loss by Inducing Oxidative Stress and Catabolism. Aging Cell. 2019, 18, e12943. [Google Scholar] [CrossRef] [PubMed]
- Erlich, A.T.; Tryon, L.D.; Crilly, M.J.; Memme, J.M.; Moosavi, Z.S.M.; Oliveira, A.N.; Beyfuss, K.; Hood, D.A. Function of specialized regulatory proteins and signaling pathways in exercise-induced muscle mitochondrial biogenesis. Integr. Med. Res. 2016, 5, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Ko, I.G.; Jeong, J.W.; Kim, Y.H.; Jee, Y.S.; Kim, S.E.; Kim, S.H.; Jin, J.J.; Kim, C.J.; Chung, K.J. Aerobic exercise affects myostatin expression in aged rat skeletal muscles: A possibility of antiaging effects of aerobic exercise related with pelvic floor muscle and urethral rhabdosphincter. Int. Neurourol. J. 2014, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Takeshima, N.; Rogers, M.E.; Islam, M.M.; Yamauchi, T.; Watanabe, E.; Okada, A. Effect of concurrent aerobic and resistance circuit exercise training on fitness in older adults. Eur. J. Appl. Physiol. 2004, 93, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Reginster, J.-Y.Y.; Slomian, J.; Buckinx, F.; Quabron, A.; Dardenne, N.; Bruyère, O.; Locquet, M.; Bruyère, O. Prevalence of sarcopenia: The impact of different diagnostic cut-off limits. J. Musculoskelet. Neuronal Interact. 2014, 14, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Witkowski, S.; Evard, R.; Rickson, J.J.; White, Q.; Sievert, L.L. Physical activity and exercise for hot flashes: trigger or treatment? Menopause. 2023, 30, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.W.; Bass, M.A.; Ting, L.; Brown, B. Influence of yard work and weight training on bone mineral density among older U. S. women. J Women Aging. 2002, 14, 139–48. [Google Scholar] [CrossRef] [PubMed]
- O’Bryan, S.J.; Giuliano, C.; Woessner, M.N.; Vogrin, S.; Smith, C.; Duque, G.; Levinger, I. Progressive Resistance Training for Concomitant Increases in Muscle Strength and Bone Mineral Density in Older Adults: A Systematic Review and Meta-Analysis. Sports Med. 2022, 52, 1939–1960. [Google Scholar] [CrossRef]
- Kim, S.W.; Park, H.Y.; Jung, W.S.; Lim, K. Effects of Twenty-Four Weeks of Resistance Exercise Training on Body Composition, Bone Mineral Density, Functional Fitness and Isokinetic Muscle Strength in Obese Older Women: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022, 19, 14554. [Google Scholar] [CrossRef] [PubMed]
- Maréchal, R.; Ghachem, A.; Prud’homme, D.; Rabasa-Lhoret, R.; Dionne, I.J.; Brochu, M. Physical activity energy expenditure and fat-free mass: relationship with metabolic syndrome in overweight or obese postmenopausal women. Appl Physiol Nutr Metab. 2021, 46, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Wasserfurth, P.; Nebl, J.; Schuchardt, J.P.; Müller, M.; Boßlau, T.K.; Krüger, K.; Hahn, A. Effects of Exercise Combined with a Healthy Diet or Calanus finmarchicus Oil Supplementation on Body Composition and Metabolic Markers-A Pilot Study. Nutrients. 2020, 12, 2139. [Google Scholar] [CrossRef] [PubMed]
- El Khoudary, S.R.; Aggarwal, B.; Beckie, T.M.; Hodis, H.N.; Johnson, A.E.; Langer, R.D.; Limacher, M.C.; Manson, J.E.; Stefanick, M.L.; Allison, M.A.; American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention; and Council on Cardiovascular and Stroke Nursing. Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation. 2020, 142, e506–e532. [Google Scholar] [CrossRef] [PubMed]
- Giardina, E.G. Heart disease in women. Int J Fertil Womens Med. 2000, 45, 350–7. [Google Scholar] [CrossRef] [PubMed]
- LaMonte, M.J.; Manson, J.E.; Chomistek, A.K.; Larson, J.C.; Lewis, C.E.; Bea, J.W.; Johnson, K.C.; Li, W.; Klein, L.; LaCroix, A.Z.; Stefanick, M.L.; Wactawski-Wende, J.; Eaton, C.B. Physical Activity and Incidence of Heart Failure in Postmenopausal Women. JACC Heart Fail. 2018, 6, 983–995. [Google Scholar] [CrossRef]
- Trachsel, L.D.; Boidin, M.; Henri, C.; Fortier, A.; Lalongé, J.; Juneau, M.; Nigam, A.; Gayda, M. Women and men with coronary heart disease respond similarly to different aerobic exercise training modalities: a pooled analysis of prospective randomized trials. Appl Physiol Nutr Metab. 2021, 46, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Glassberg, H.; Balady, G.J. Exercise and heart disease in women: why, how, and how much? Cardiol Rev. 1999, 7, 301–8. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, N.T.; Mielke, M.M. Sex Differences in Alzheimer’s Disease. Neurol Clin. 2023, 41, 343–358. [Google Scholar] [CrossRef] [PubMed]
- Scheyer, O.; Rahman, A.; Hristov, H.; Berkowitz, C.; Isaacson, R.S.; Diaz Brinton, R.; Mosconi, L. Female Sex and Alzheimer’s Risk: The Menopause Connection. J Prev Alzheimers Dis. 2018, 5, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Faravelli, C.; Alessandra Scarpato, M.; Castellini, G.; Lo Sauro, C. Gender differences in depression and anxiety: the role of age. Psychiatry Res. 2013, 210, 1301–3. [Google Scholar] [CrossRef] [PubMed]
- Aibar-Almazán, A.; Hita-Contreras, F.; Cruz-Díaz, D.; de la Torre-Cruz, M.; Jiménez-García, J.D.; Martínez-Amat, A. Effects of Pilates training on sleep quality, anxiety, depression and fatigue in postmenopausal women: A randomized controlled trial. Maturitas. 2019, 124, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Cunha, P.M.; Werneck, A.O.; Nunes, J.P.; Stubbs, B.; Schuch, F.B.; Kunevaliki, G.; Zou, L.; Cyrino, E.S. Resistance training reduces depressive and anxiety symptoms in older women: a pilot study. Aging Ment Health. 2022, 26, 1136–1142. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Haskell, W.L.; Taylor, C.B.; Kraemer, H.C.; DeBusk, R.F. Group- vs home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA. 1991, 266, 1535–42. [Google Scholar] [CrossRef] [PubMed]
- Eyigor, S.; Karapolat, H.; Durmaz, B. Effects of a group-based exercise program on the physical performance, muscle strength and quality of life in older women. Arch Gerontol Geriatr. 2007, 45, 259–71. [Google Scholar] [CrossRef] [PubMed]
- Gulli, G.; Cevese, A.; Cappelletto, P.; Gasparini, G.; Schena, F. Moderate aerobic training improves autonomic cardiovascular control in older women. Clin Auton Res. 2003, 13, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.M.; Dal Bello-Haas, V.P.; Farthing, J.P.; Crockett, K.L.; Haver, C.R.; Johnston, G.; Basran, J. Falls and Wrist Fracture: Relationship to Women’s Functional Status after Age 50. Can J Aging. 2016, 35, 361–71. [Google Scholar] [CrossRef] [PubMed]
- Pinkas, J.; Gujski, M.; Humeniuk, E.; Raczkiewicz, D.; Bejga, P.; Owoc, A.; Bojar, I. State of Health and Quality of Life of Women at Advanced Age. Med Sci Monit. 2016, 22, 3095–105. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, L.; Leng, X.; La Monte, M.J.; Tindle, H.A.; Cochrane, B.B.; Shumaker, S.A. Functional Independence in Late-Life: Maintaining Physical Functioning in Older Adulthood Predicts Daily Life Function after Age 80. J Gerontol A Biol Sci Med Sci. 2016, 71 (Suppl 1), S79–86. [Google Scholar] [CrossRef] [PubMed]
- Parra-Rizo, M.A.; Sanchís-Soler, G. Physical Activity and the Improvement of Autonomy, Functional Ability, Subjective Health, and Social Relationships in Women over the Age of 60. Int J Environ Res Public Health. 2021, 18, 6926. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Ahn, N.; Park, J.; Kim, K. 12-Week Exercise Training of Knee Joint and Squat Movement Improves Gait Ability in Older Women. Int J Environ Res Public Health. 2021, 18, 1515. [Google Scholar] [CrossRef] [PubMed]
- Lauche, R.; Schumann, D.; Sibbritt, D.; Adams, J.; Cramer, H. Associations between yoga practice and joint problems: a cross-sectional survey among 9151 Australian women. Rheumatol Int. 2017, 37, 1145–1148. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.C.; Oliveira, R.G.; Pires-Oliveira, D.A. Comparison between static stretching and the Pilates method on the flexibility of older women. J Bodyw Mov Ther. 2016, 20, 800–806. [Google Scholar] [CrossRef] [PubMed]
- de Resende-Neto, A.G.; do Nascimento, M.A.; de Sá, C.A.; Ribeiro, A.S.; Desantana, J.M.; da Silva-Grigoletto, M.E. Comparison between functional and traditional training exercises on joint mobility, determinants of walking and muscle strength in older women. J Sports Med Phys Fitness. 2019, 59, 1659–1668. [Google Scholar] [CrossRef] [PubMed]
- Dunsky, A.; Netz, Y. Physical activity and sport in advanced age: is it risky? a summary of data from articles published between 2000-2009. Curr Aging Sci. 2012, 5, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Kirby, J.B.; Kluge, M.A. For the Love of the Game: An Exploration of the Experiences and Psychosocial Development of Women 70 Years of Age and Older Who Play Volleyball. J Aging Phys Act. 2022, 30, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Deck, S.; Doherty, A.; Hall, C.; Schneider, A.; Patil, S.; Belfry, G. “Older, Faster, Stronger”: The Multiple Benefits of Masters Sport Participation. J Aging Phys Act. 2023, 31, 786–797. [Google Scholar] [CrossRef] [PubMed]
- Huebner, M.; Meltzer, D.; Ma, W.; Arrow, H. The Masters athlete in Olympic weightlifting: Training, lifestyle, health challenges, and gender differences. PLoS One. 2020, 15, e0243652. [Google Scholar] [CrossRef] [PubMed]
- Kolt, G.S.; Driver, R.P.; Giles, L.C. Why older Australians participate in exercise and sport. J Aging Phys Act. 2004, 12, 185–98. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





