1. Introduction
Asthma and Chronic Obstructive Pulmonary Disease (COPD) rank among the most significant public health challenges globally, affecting millions of individuals across diverse populations. These chronic respiratory conditions are not only leading causes of morbidity and mortality but also exert substantial economic pressures on healthcare systems and societies worldwide. In the intricate landscape of global health, the management of asthma and COPD represents a pivotal arena for intervention, aiming to mitigate their profound impact [
1,
2].
Internationally, asthma affects around 339 million people, while COPD is recognized as the third leading cause of death, affecting nearly 300 million individuals worldwide. The costs associated with managing these chronic respiratory diseases are substantial. In the United States, the total cost related to asthma exceeds
$80 billion annually, encompassing direct medical expenses and productivity losses [
3]. In Europe, the direct healthcare costs for COPD have been estimated at approximately €48.4 billion per year, primarily due to exacerbations requiring hospitalization [
4]. These figures not only highlight the magnitude of the challenge posed by these diseases but also the urgency of developing more effective management strategies to reduce their economic impact.
The burden of these diseases is particularly acute in France, where the frequency of hospital admissions due to severe asthma and COPD exacerbations highlights an urgent healthcare challenge. The annual hospital admissions for acute asthma episodes oscillate between 8,000 and 16,000, with an average hospitalization cost of approximately €3,811, underscoring the financial strain on the healthcare infrastructure [
5,
6]. COPD presents an even more formidable challenge, with exacerbations prompting an estimated 105,000 to 165,000 hospital admissions annually, each bearing an average cost of €5,342 [
7]. These figures emphasize the critical need for innovative management strategies to alleviate the healthcare system's burden and improve patient outcomes.
Despite the clear delineation of pharmacists' roles in enhancing patient care through optimized disease management, the reduction of hospital stays, and the improvement of overall quality of life [
8,
9,
10], their engagement in managing asthma and COPD patients, especially within hospital settings, remains remarkably limited. The integration of pharmacy services in the emergency department in our hospital is a step forward; however, the fast-paced nature of these environments, combined with limited pharmacist resources, necessitates a more focused and strategic approach to patient care. This study seeks to bridge this gap by meticulously identifying patient profiles most susceptible to hospitalization due to asthma and COPD complications, thereby enabling the strategic targeting of these individuals for specialized pharmaceutical interventions. Through this targeted approach, our study not only aims to unlock the potential of pharmacists in improving patient care but also endeavors to contribute significantly to the optimization of healthcare resources. By enhancing the management of chronic respiratory diseases, we aspire to foster a tangible improvement in patient outcomes, thereby reducing the recurrence of hospitalizations and the associated healthcare burden.
Moreover, this study aligns with international calls for a more integrated and patient-centered approach to managing chronic respiratory diseases, as advocated by the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [
11,
12]. By situating our research within the broader context of global health imperatives and leveraging cutting-edge data analytics, we aim to contribute valuable insights into the risk factors and patient profiles indicative of high rehospitalisation rates. In doing so, we anticipate not only advancing the field of respiratory disease management but also contributing to the formulation of policies and practices that can significantly mitigate the impact of asthma and COPD on patients and healthcare systems alike. In essence, this study represents a confluence of clinical research, pharmacological expertise, and health economics, aimed at addressing one of the most pressing healthcare challenges of our time. Through a meticulous analysis of patient data and the strategic application of pharmaceutical interventions, we seek to chart a course toward more effective, efficient, and patient-centric care for individuals suffering from asthma and COPD.
Objectives
The primary objective of this research is to comprehensively identify and evaluate the unique attributes and risk factors of individuals diagnosed with Chronic Obstructive Pulmonary Disease (COPD) or asthma, particularly those at an increased risk of rehospitalisation within six months post their initial discharge from the emergency department. This investigation aims to establish a framework for prioritizing targeted pharmaceutical interventions, optimizing patient management strategies to mitigate the likelihood of readmissions. Through a detailed analysis of patient profiles, the study endeavours to enable healthcare professionals to tailor intervention strategies more effectively, ensuring a more personalized and efficient approach to managing these chronic respiratory conditions.
2. Materials and Methods
The methodology of this study involved leveraging the Clinical Data Warehouse of the University Hospital to scrutinize rehospitalisation rates for individuals experiencing exacerbations of asthma or COPD, within a six-month timeframe following their initial discharge from the emergency department. To maintain a focused and relevant dataset, we employed stringent inclusion criteria, selecting only those adult patients who were admitted for asthma or COPD exacerbations between January and December 2019 and who had provided consent for the reuse of their data. To further refine the relevance of our study population, exclusion criteria were meticulously defined and implemented.
Patient identification was performed through the use of standardized medical coding systems, including the French Medicalization Program of Information Systems (PMSI) and the International Classification of Diseases, Tenth Revision (ICD-10). Our comprehensive analysis encompassed an array of variables, including demographic information, details of hospitalization, and clinical outcomes, with the aim of uncovering factors that significantly influence medication adherence among individuals managing asthma and COPD.
Throughout this investigation, we upheld the highest ethical standards, conducting analyses exclusively on anonymized datasets that had received approval from the appropriate ethics committee. This approach was in strict accordance with guidelines issued by the National Commission on Informatics and Liberty (CNIL), thereby ensuring the utmost confidentiality of patient data and maintaining the integrity of our research.
3. Results
Table 1 encapsulates the demographic and clinical profiles of the 140 participants in this study. The mean age of the cohort was 60.3 years, with a standard deviation of 18.8 years. A gender analysis indicated that females, who constituted slightly more than half of the participants (N=74), had a lower average age (55.0 years) compared to males (N=66), who had an average age of 66.3 years. This difference in age across genders was statistically significant (p<0.001).
In terms of specific chronic respiratory diseases, 36% of the subjects were diagnosed with asthma, and 64% with COPD (Chronic Obstructive Pulmonary Disease). Gender comparison revealed a higher prevalence of asthma among females (53%) compared to males (17%), while a larger percentage of males (83%) were affected by COPD than females (47%). These gender disparities in disease prevalence were also statistically significant (p<0.001).
The outcomes post-emergency department discharge were categorized into two groups: those who were rehospitalised and those who were not. Of the total patient group, 59% were readmitted to the hospital, whereas 41% did not require readmission. Gender-based analysis showed no significant statistical difference in hospitalization rates, with 57% of females and 62% of males being rehospitalised (p=0.52). It is notable that a modification in the management of chronic pulmonary disease post-emergency department visit was reported in 91% of the patients. Gender comparison for this metric did not reveal any significant difference, with 93% of females and 89% of males experiencing a change in their disease management (p=0.42).
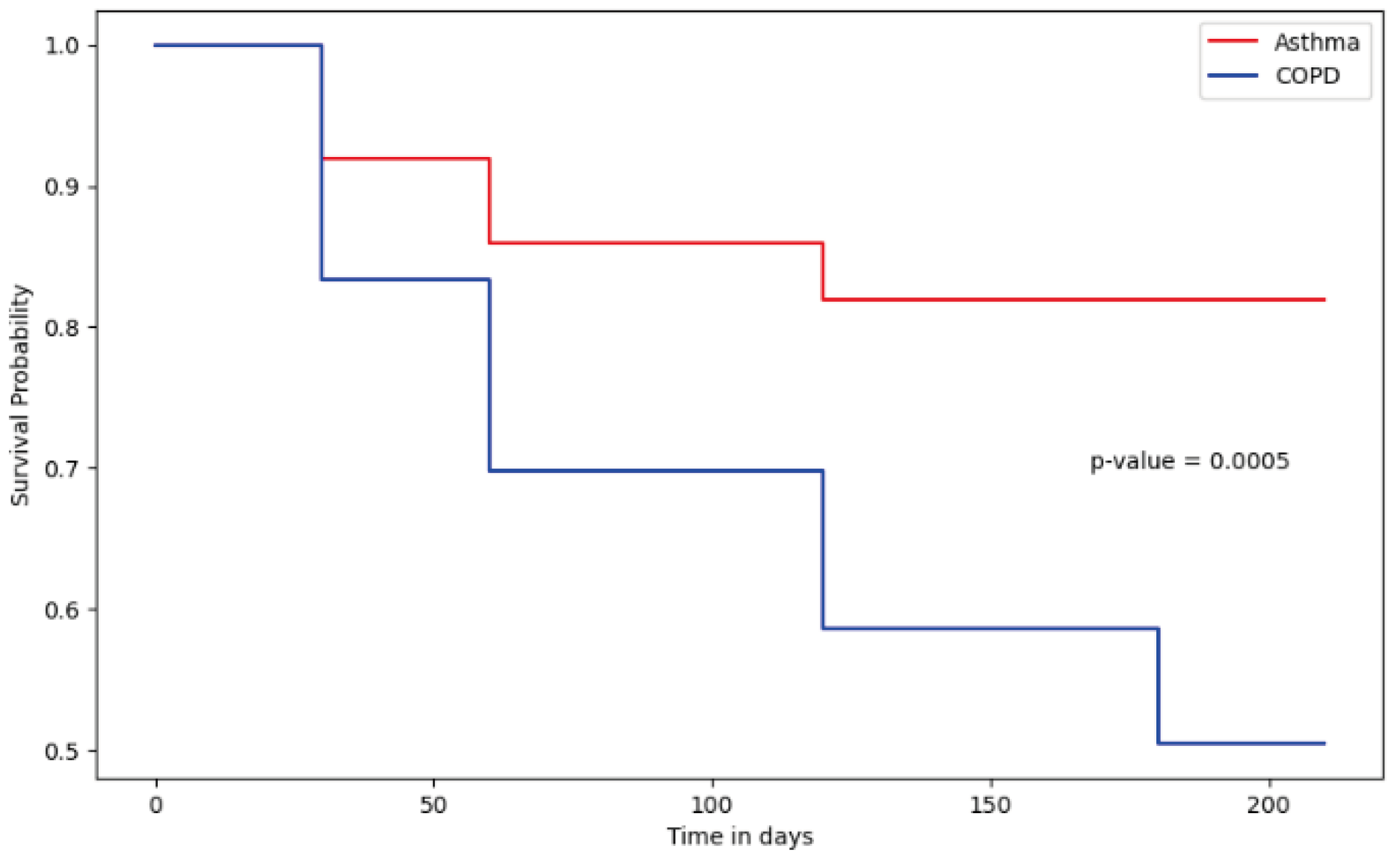
Figure 1 displays the survival analysis outcomes for asthmatic patients and those with COPD over a six-month period following their hospital discharge. The analysis uncovered a significant disparity in the probability of survival without rehospitalisation between the two patient groups, with asthmatic individuals showing a higher likelihood of survival without rehospitalisation compared to those with COPD, as evidenced by their respective survival curves. The notable difference in survival rates between the groups was statistically significant (p<0.001), highlighting the distinct impact of underlying chronic conditions on post-hospitalization trajectories. These insights suggest that care management and post-discharge follow-up strategies may need to be tailored according to the diagnosed chronic respiratory condition.
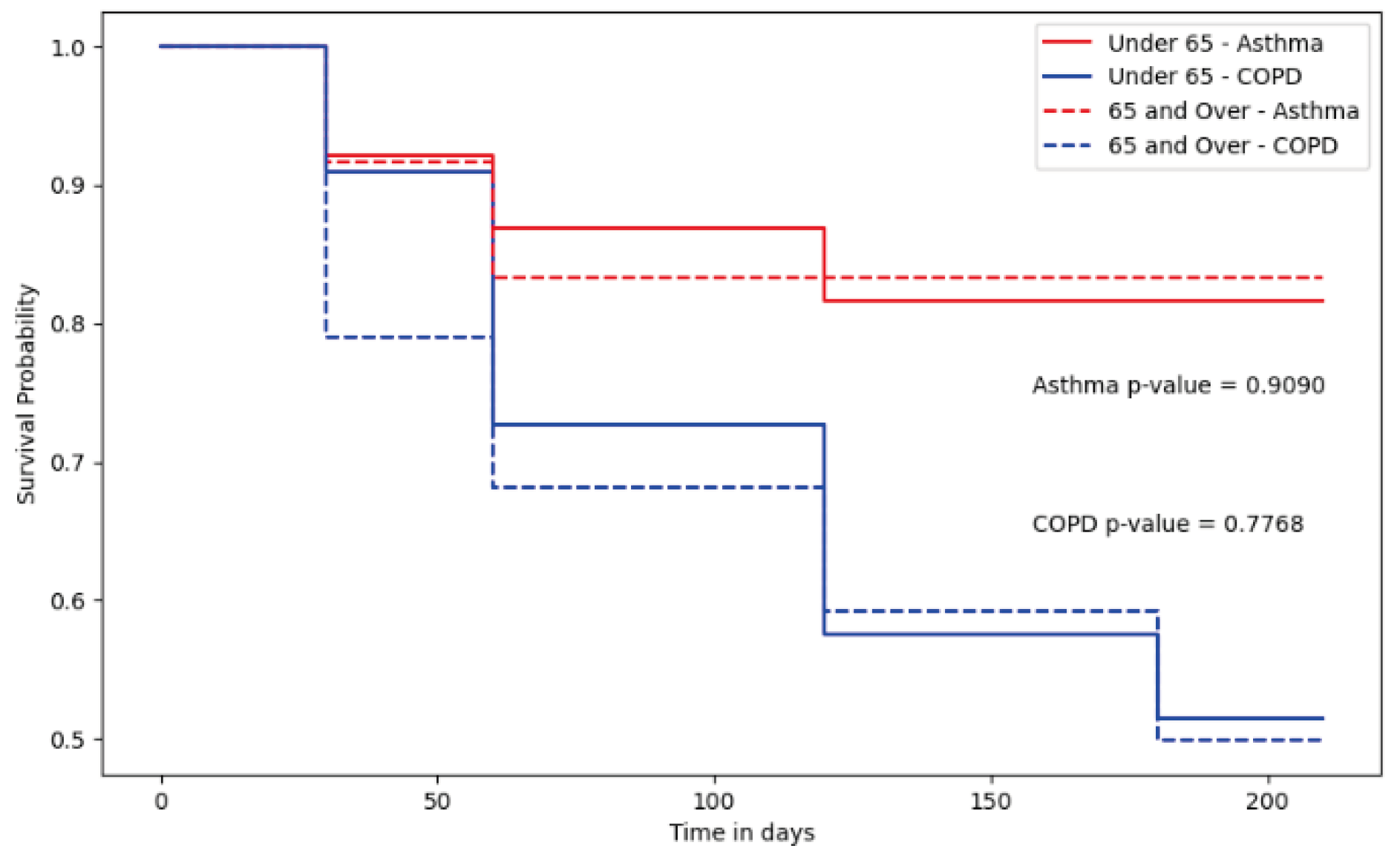
Figure 2 illustrates the survival analysis for asthmatic and COPD patients post-discharge, segmented by age group (65 years and older). This analysis did not find any significant difference based on the age of the population.
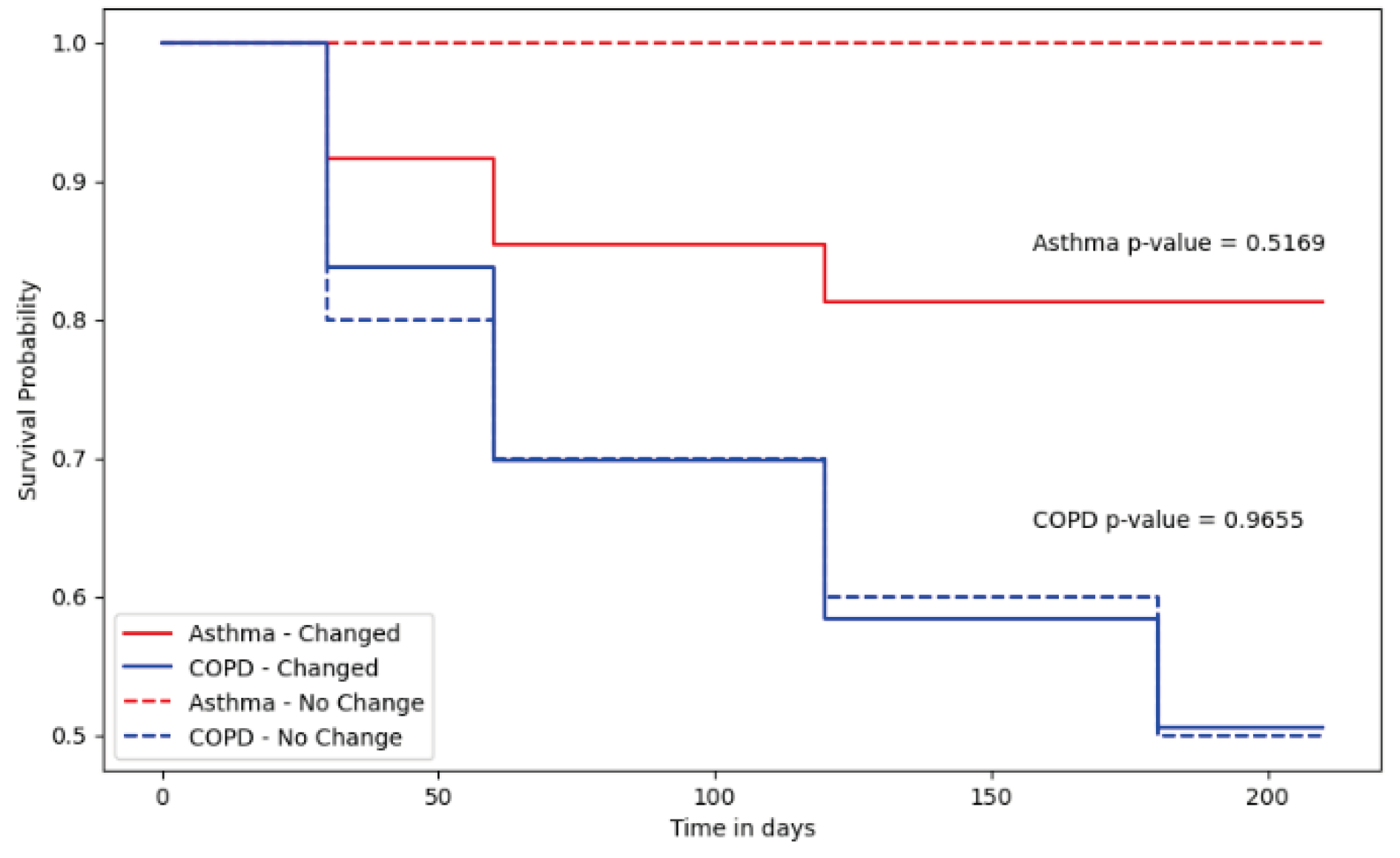
Figure 3 portrays the survival analysis outcomes for asthma and COPD patients over a six-month period post-discharge, related to therapeutic changes implemented during their stay in the emergency department. According to this variable, no significant differences were observed.
4. Discussion
The findings of this study shed light on the intricate challenges and opportunities present in the management of asthma and Chronic Obstructive Pulmonary Disease (COPD) within the healthcare system. The high frequency of treatment regimen modifications during hospital stays for 91% of patients highlights the critical role that pharmaceutical teams play in navigating the complexities of these conditions [
13]. This adaptability in treatment underscores the necessity for a dynamic approach to care, which takes into account the evolving nature of the patient's condition and the need for personalized therapeutic management.
Interestingly, the modification of treatment regimens, despite its prevalence, did not directly affect the rate of rehospitalisation within the six-month follow-up period. This finding suggests that while in-hospital treatment adjustments are crucial, they may not be sufficient on their own to prevent readmissions. This leads to the inference that factors outside the immediate scope of hospital-based care, such as patient adherence to medication and the effectiveness of post-discharge follow-up, play significant roles in the long-term management of asthma and COPD.
The substantial rate of readmission (59%) within six months post-discharge underscores a significant gap in the continuity and effectiveness of care for patients with these chronic respiratory conditions. This highlights an urgent need for strategies that extend beyond the hospital setting, focusing on patient education, adherence to treatment plans, and lifestyle adjustments. Targeted pharmaceutical interventions, particularly those that emphasize therapeutic education and empower patients with the knowledge and tools to manage their conditions effectively, emerge as pivotal in this context [
14].
Empowering patients through education on disease management, medication adherence, and lifestyle modifications not only equips them to take charge of their health but also represents a fundamental shift towards a more patient-centered approach to healthcare [
15]. Pharmacists, with their expertise in medication management and patient counselling, are uniquely positioned to lead these educational efforts [
16]. By doing so, they can significantly contribute to reducing the frequency of exacerbations and, consequently, hospital readmissions.
Furthermore, this study's insights advocate for a more integrated model of care that encompasses both the acute management of asthma and COPD in hospital settings and the ongoing support needed post-discharge. Incorporating pharmaceutical expertise throughout the patient's care journey can enhance the effectiveness of treatment plans, improve patient outcomes, and, critically, reduce the burden on healthcare systems from recurrent hospitalizations [
17].
In conclusion, the management of asthma and COPD presents a multifaceted challenge that requires a coordinated effort across different healthcare disciplines. This study underscores the importance of pharmaceutical intervention not only during hospitalization but also as a critical component of post-discharge care. By adopting a holistic and integrated approach to treatment, healthcare providers can better address the needs of patients with chronic respiratory diseases, improving their quality of life and reducing the impact of these conditions on the healthcare system.
5. Conclusions
Our research underscores that individuals diagnosed with Chronic Obstructive Pulmonary Disease (COPD) are distinctly susceptible to negative health outcomes, positioning them as the most vulnerable segment within our study's demographic. This vulnerability accentuates the imperative need for proactive management strategies tailored to this group. Nonetheless, our comprehensive analysis does not delineate a singular patient profile within the COPD cohort as necessitating prioritized attention. This revelation highlights the intricacies involved in assessing risk among COPD patients and accentuates the necessity for customized intervention strategies. These strategies should be designed to address the needs of the COPD patient population at large, rather than isolating specific subgroups for targeted approaches. This approach acknowledges the diverse manifestations of COPD and the importance of a holistic, patient-centric model of care that adapts to the multifaceted needs of all individuals affected by this condition, thereby enhancing the efficacy of treatment regimens and patient outcomes across the spectrum of COPD severity.
Author Contributions
This research benefited from the expertise and dedication of several collaborators. The conceptualization, supervision, and project mentoring were ensured by E.B. and R.L., who also provided their expertise in methodology. The information gathering and writing of the thesis were carried out by E.D., highlighting the importance of precise data collection for the success of this study. Critical manuscript review for significant intellectual contributions and the provision of specific expertise were conducted by J.R., L.M.J., and R.V., thereby ensuring the rigor and scientific quality of the research. All authors have read and approved the final version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of University Hospital of Rouen for studies involving humans. OR “The animal study protocol was approved by the Institutional.
Informed Consent Statement
Patients' non-opposition has been collected in compliance with applicable data re-use regulations (Loi Jardé and CNIL).
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to (specify the reason for the restriction).
Acknowledgments
We extend our heartfelt gratitude to Stefan Darmoni and Julien Grosjean for their invaluable support and guidance in utilizing the data warehouse. Their expertise and dedication were instrumental in the successful completion of our research. This acknowledgment reflects our appreciation for their contributions that go beyond the realms of authorship and funding, encompassing administrative and technical support that was crucial to our work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ellwood P, Asher MI, Billo NE, Bissell K, Chiang CY, Ellwood EM, et al. The Global Asthma Network rationale and methods for Phase I global surveillance: prevalence, severity, management and risk factors. Eur Respir J. 2017 Jan;49(1):1601605.
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: Systematic review and meta–analysis. J Glob Health. 5(2):020415.
- Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018 Mar;15(3):348–56.
- Wouters EFM. Economic analysis of the Confronting COPD survey: an overview of results. Respir Med. 2003 Mar;97 Suppl C:S3-14.
- Pascal L, Fuhrman C, Durif L, Nicolau J, Charpin D, Dujols P, et al. Évolution des hospitalisations pour asthme en France métropolitaine, 1998-2002. Rev Mal Respir. 2007 May;24(5):581–90.
- Chouaid C, Vergnenègre A, Vandewalle V, Liebaert F, Khelifa A. Coûts de l’asthme en France : modélisation médico-économique par un modèle de Markov. Rev Mal Respir. 2004 Jun;21(3):493–9.
- Laurendeau C, Chouaid C, Roche N, Terrioux P, Gourmelen J, Detournay B. Prise en charge et coûts de la bronchopneumopathie chronique obstructive en France en 2011. Rev Mal Respir. 2015 Sep;32(7):682–91.
- Garcia-Cardenas V, Armour C, Benrimoj SI, Martinez-Martinez F, Rotta I, Fernandez-Llimos F. Pharmacists’ interventions on clinical asthma outcomes: a systematic review. Eur Respir J. 2016 Apr;47(4):1134–43.
- Qin SB, Zhang XY, Fu Y, Nie XY, Liu J, Shi LW, et al. The impact of the clinical pharmacist-led interventions in China: A systematic review and Meta-Analysis. Int J Clin Pharm. 2020 Apr;42(2):366–77.
- Mahdavi H, Esmaily H. Impact of educational intervention by community pharmacists on asthma clinical outcomes, quality of life and medication adherence: A systematic review and meta-analysis. J Clin Pharm Ther. 2021 Oct;46(5):1254–62.
- 2022 GINA Main Report [Internet]. Global Initiative for Asthma - GINA. [cited 2024 Apr 2]. Available from: https://ginasthma.
- 2020 Gold Reports [Internet]. Global Initiative for Chronic Obstructive Lung Disease - GOLD. [cited 2024 Apr 2]. Available from: https://goldcopd.
- Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MCJM, Verhamme KMC. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J. 2015 Feb;45(2):396–407.
- Gregoriano C, Dieterle T, Breitenstein AL, Dürr S, Baum A, Maier S, et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: data from a randomized controlled trial. Respir Res. 2018;19:237.
- Khdour MR, Kidney JC, Smyth BM, McElnay JC. Clinical pharmacy-led disease and medicine management programme for patients with COPD. Br J Clin Pharmacol. 2009 Oct;68(4):588–98.
- Barnett MJ, Perry PJ, Langstaff JD, Kaboli PJ. Comparison of rates of potentially inappropriate medication use according to the Zhan criteria for VA versus private sector medicare HMOs. J Manag Care Pharm JMCP. 2006 Jun;12(5):362–70.
- Zillich AJ, Snyder ME, Frail CK, Lewis JL, Deshotels D, Dunham P, et al. A randomized, controlled pragmatic trial of telephonic medication therapy management to reduce hospitalization in home health patients. Health Serv Res. 2014 Oct;49(5):1537–54.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).