2. Materials and Methods
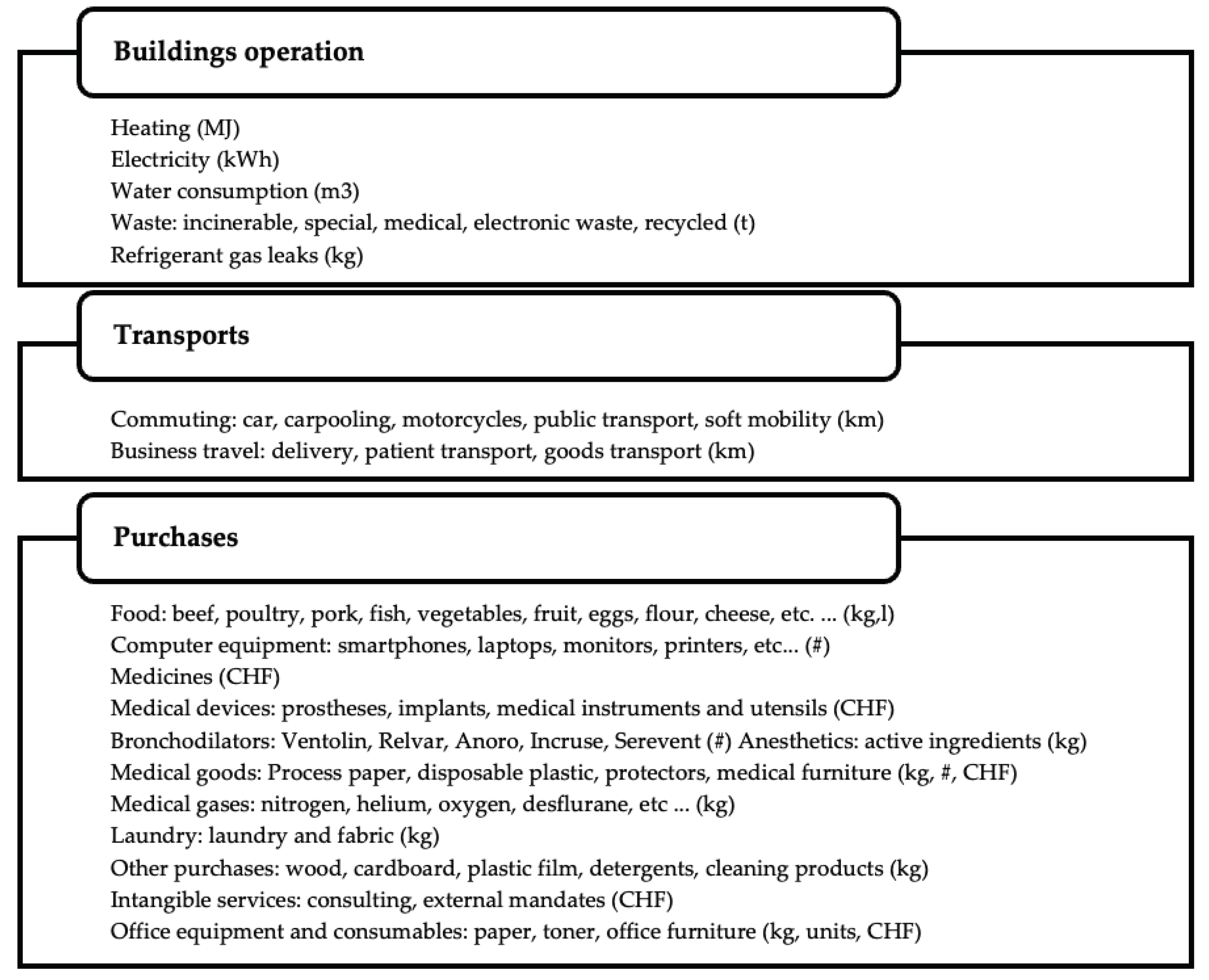
Our approach for evaluating the carbon footprint of the healthcare system of the Geneva canton relies on gathering data from key stakeholders in this system. We sought the collaboration of hospitals and clinics, both public and private, nursing homes, dispensing pharmacies, medical offices, the homecare institution, analysis laboratories and ambulance services. We interviewed each stakeholder relevant to the scope of the study to collect its data (see
Figure 1), enabling us to assess the specific carbon footprint of its activity according to the greenhouse gas protocol [
8].
Where specific data was not available, we used similar data from the same type of stakeholder. For example, to approximate the carbon footprint of anaesthetic gases from one private hospital that had not produced any data on this subject, we extrapolated it from another hospital based on hospitalisation activities. This hybrid method, combining
bottom-up and
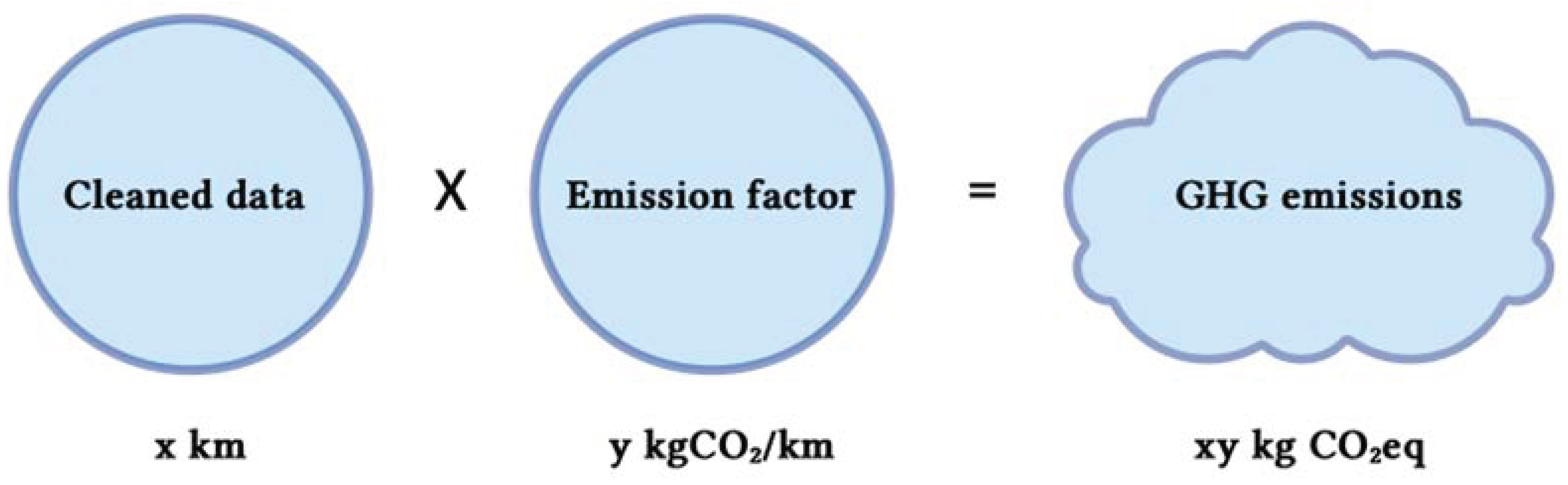
top-down data collection, enables us to obtain a complete picture for estimating the carbon footprint of Geneva's hospitals system, while remaining as close as possible to the specific characteristics of each actor. The gathered raw data was subsequently converted into equivalent tons of CO
2 (tCO
2 eq) (
Figure 2). In most instances, the data was presented in terms of item quantities, such as kilometres travelled, CHF, kWh, MJ.
To do so, we used pre-calculated emission factors (EFs) (see
Table 1), although these introduce a degree of uncertainty as they are often based on national or even global averages. However, this method is the one most commonly used, as it is often not feasible to systematically carry out a full life cycle analysis of each emission item. We used the
EcoInvent 3.9 database that we consulted using
OpenLCA 2.0 software [
9,
10] (
Table 1). This database provides global data or data specific to Switzerland, depending on the activity. We also used
Mobitool 3.0 database (which largely incorporates
EcoInvent's emission factors), the standard for environmental assessment of means of transport and mobility in Switzerland.
Unfortunately, there are very few specific EFs for each medicine. For some that had been identified as highly polluting, complete life cycle studies have been carried out and are available in the literature. This is the case for certain anesthetic gases and bronchodilators, which has enabled us to quantify their impact more specifically [
11,
12].
For the other medicines, we used a monetary EF calculated by the French Environment and Energy Management Agency based on EEIOT (
Environmentally Extended Input Output Table) economic models [
13]. Monetary EF are an indicator that measures the quantity of greenhouse gas emissions produced for each monetary unit generated by an economic activity. It helps to assess the environmental efficiency of activities by relating economic value to carbon emissions. We did not find any Swiss data in this area, so we relied on the existing French "Base Empreinte" database [
13]. We assumed that the estimates produced were sufficiently close to that of the canton of Geneva, given that this sector is highly globalised, with around 80% of active ingredients manufactured in India and China [
14].
For the fuels category, the Swiss Confederation's
KBOB tool (IPB 2009/1:2022, Version 2) provided us with specific EFs for Switzerland [
15]. Finally, electricity in Geneva is already highly decarbonised, with more than 30% of electricity generated from local renewable sources and around 70% from the Swiss mix, which also has a low carbon content compared with other countries such as Germany. The EF was calculated jointly by the Geneva entities, OCSTAT, OCEN, SIG and the Direction Durabilité et Climat (DDC).
Table 1.
Databases utilised for the carbon footprint calculation.
Table 1.
Databases utilised for the carbon footprint calculation.
| Source of emission factors |
Category of raw data |
| EcoInvent 3.9 [10] |
Food, purchases, wastewater treatment, waste |
| Mobitool 3.0 [16] |
Transports |
| BaseEmpreinte V23.1 [13] |
Monetary EF for medicines and medical activities |
| The Shift Project Excel Chiffrage 2023 v1.0 [17] |
Monetary EF for medical devices |
| KBOB / IPB 2009/1:2022, Version 2 [15] |
Fuels and combustibles |
| OCSTAT, OCEN, DDC, SIG 2022 [18] |
Specific electricity EF for Geneva |
| Andersen et al, 2012 [19] |
Anaesthetic gases (sevoflurane, desflurane, isoflurane) |
| Janson et al, 2020 [12] |
Bronchodilators |
| Parvatker et al, 2019 [11] |
Anaesthetic gases |
Finally, we have modelled emission reduction scenarios on the shared socio-economic trajectories published in 2023 by the IPCC [
20] (
Table 2). These scenarios are quantified objectives, distributed by categories, to align with the IPCC trajectories. These objectives are quantified not based on each measure, but as targets to be achieved for every main category. The first scenario does not require any specific action by the healthcare system, and we have called it "business as usual". It is aligned with the IPCC's SSP2-4.5 scenario. According to this trajectory, emissions will remain stable in 2030 and 2040, despite population growth and ageing, because the healthcare system’s carbon footprint will be mitigated by the gradual decarbonisation of the overall economy and society, from electricity to heating, infrastructure and behaviour with regard to mobility and food. The second scenario represents the impact of "modest" actions on GHG emissions. It is based on the SSP1-2.6 scenario. The third scenario is based on coordinated and "ambitious" actions by all the players in the canton and is inspired by the IPCC's SSP1-1.9 scenario.
3. Results
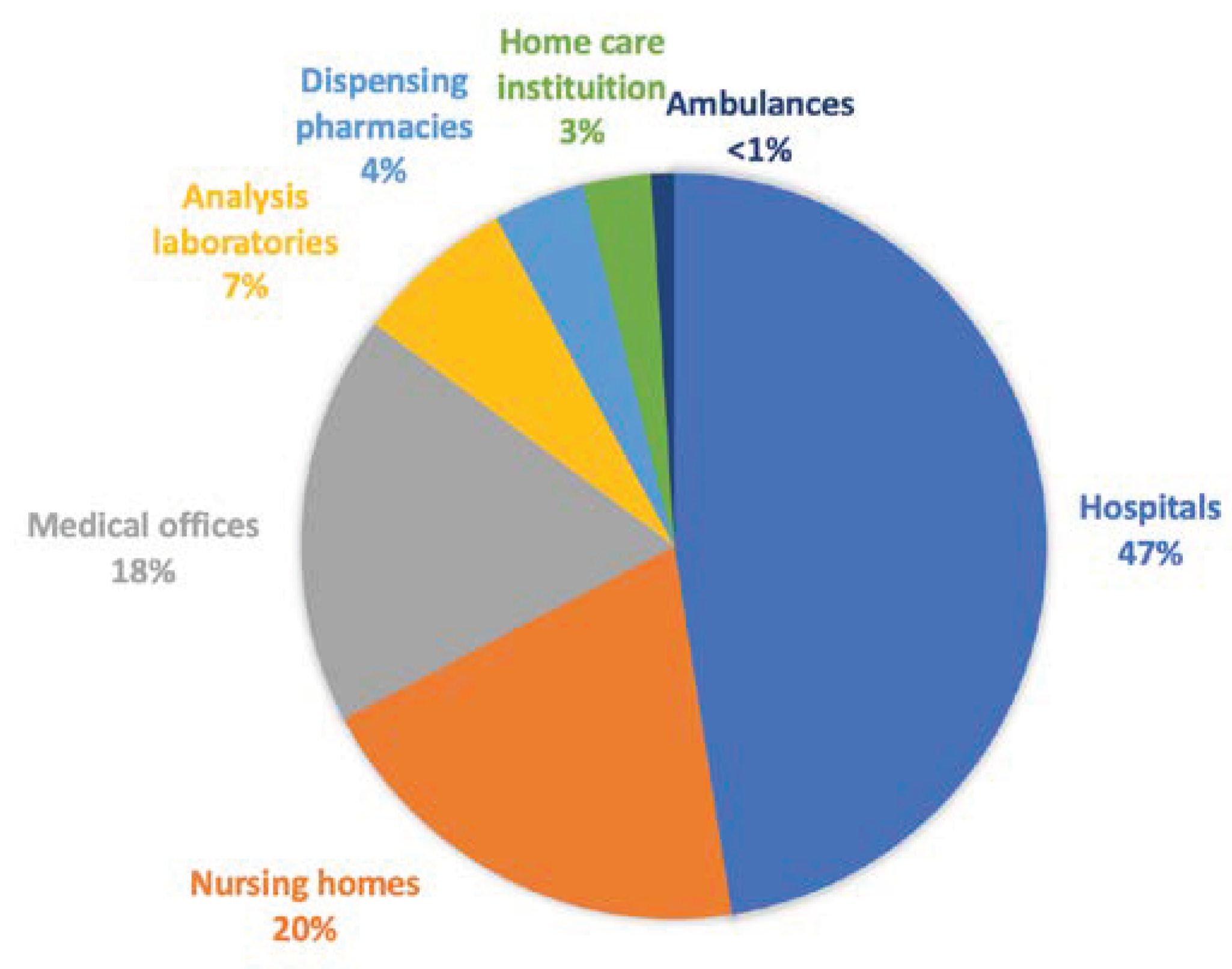
Our overall estimate of the carbon footprint of the Geneva healthcare system within the scope stated is 436,831 tonnes of CO
2 equivalent for the year 2022, which represents approximately 1.25% of Switzerland's total carbon footprint. Unfortunately, due to the absence of a carbon footprint for the Geneva canton, we couldn’t provide yet this comparison to the canton level. Our results make it possible to classify GHG emissions by sub-sector of the healthcare system. In a first analysis, by excluding provisionally medicines and medical devices, conforming to The Shift Project’s illustration of the breakdown of emissions by player, we logically obtain the hospital sub-sector in 1st position, which represents 46% of the sector's emissions (
Figure 3). Nursing homes and medical offices come next, with 20% and 18% respectively.
Finally, the analysis laboratories, dispensing pharmacies, homecare institutes and ambulance services each accounted for less than 10%. These results are in line with those obtained by The Shift Project. The Shift Project, when setting aside the establishment for disabled and the health insurances, estimates that 46% of the carbon footprint can be attributed to hospitals, 28% to medical offices and 25% to home care institution [
2]. In the canton of Geneva, if we use the same grouping as The Shift Project, i.e. by classifying laboratories, dispensing pharmacies and medical offices in a category called "ambulatory medicine", we obtain 29% of the carbon footprint, and if we group together nursing homes and the homecare institute, we obtain 23%, close to those of The Shift Project with a similar scope.
Unfortunately, the results of analysis laboratories could not be integrated directly, due to the lack of cooperation from this sub-sector. However, an estimate was made using economic data and monetary factors for medical activity, giving an estimated total carbon footprint of 12,760 tonnes of CO
2 equivalent for all the analysis laboratories in the canton of Geneva. The detailed breakdown by CO
2-emitting activity for each player in the healthcare system can be consulted in the Supplementary
Figures (S1–S7).
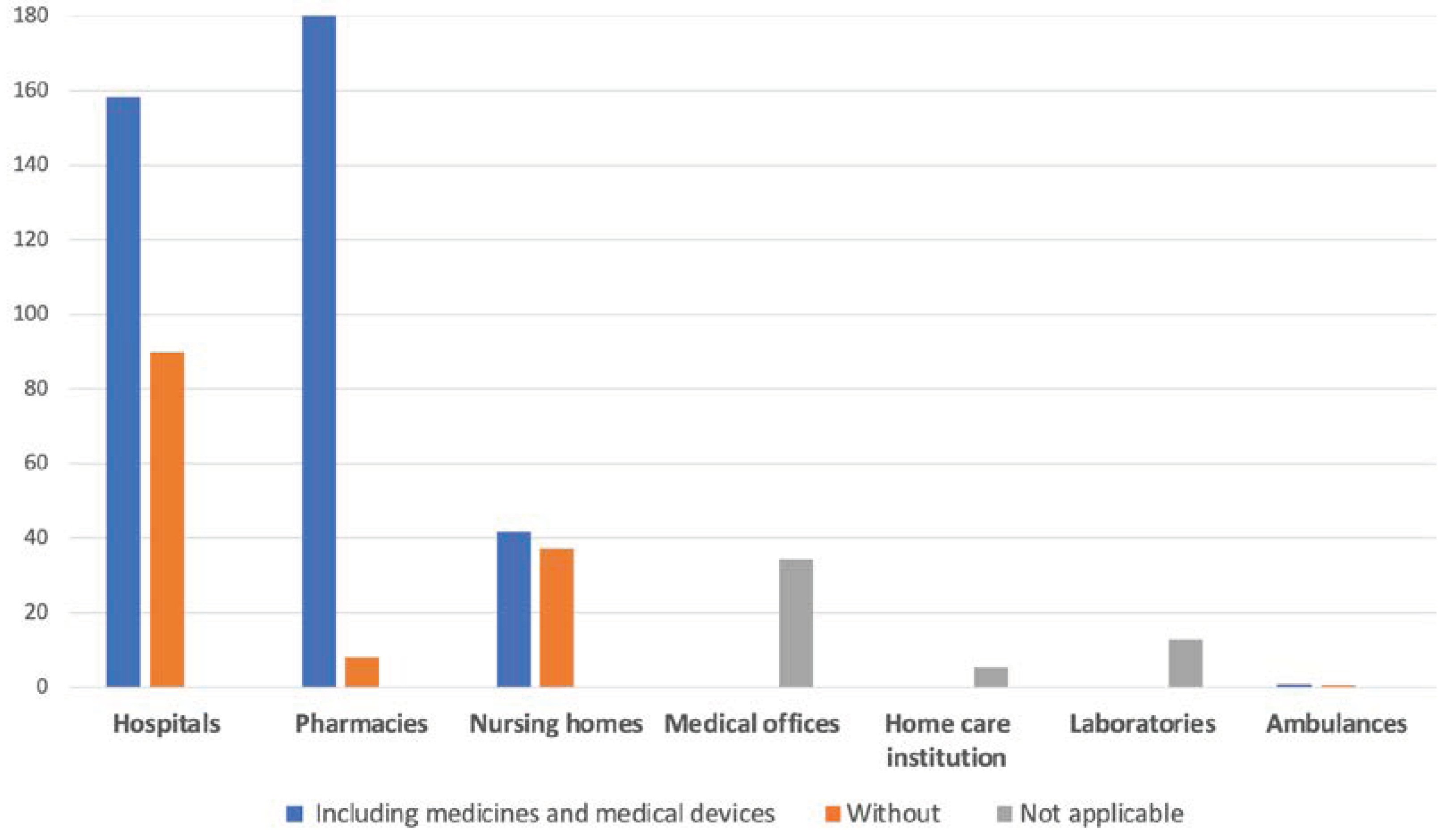
In a second analysis, taking into account medicines and medical devices, the situation is quite different. Dispensing pharmacies (ambulatory and not hospital pharmacies), whose business model is based mainly on the sale of medicines, rank first in terms of GHG emissions, ahead of hospitals (
Table 3,
Figure 4). Of course, the carbon footprint of medicines can only be attributed to dispensing pharmacies indirectly, in their purchases activity.
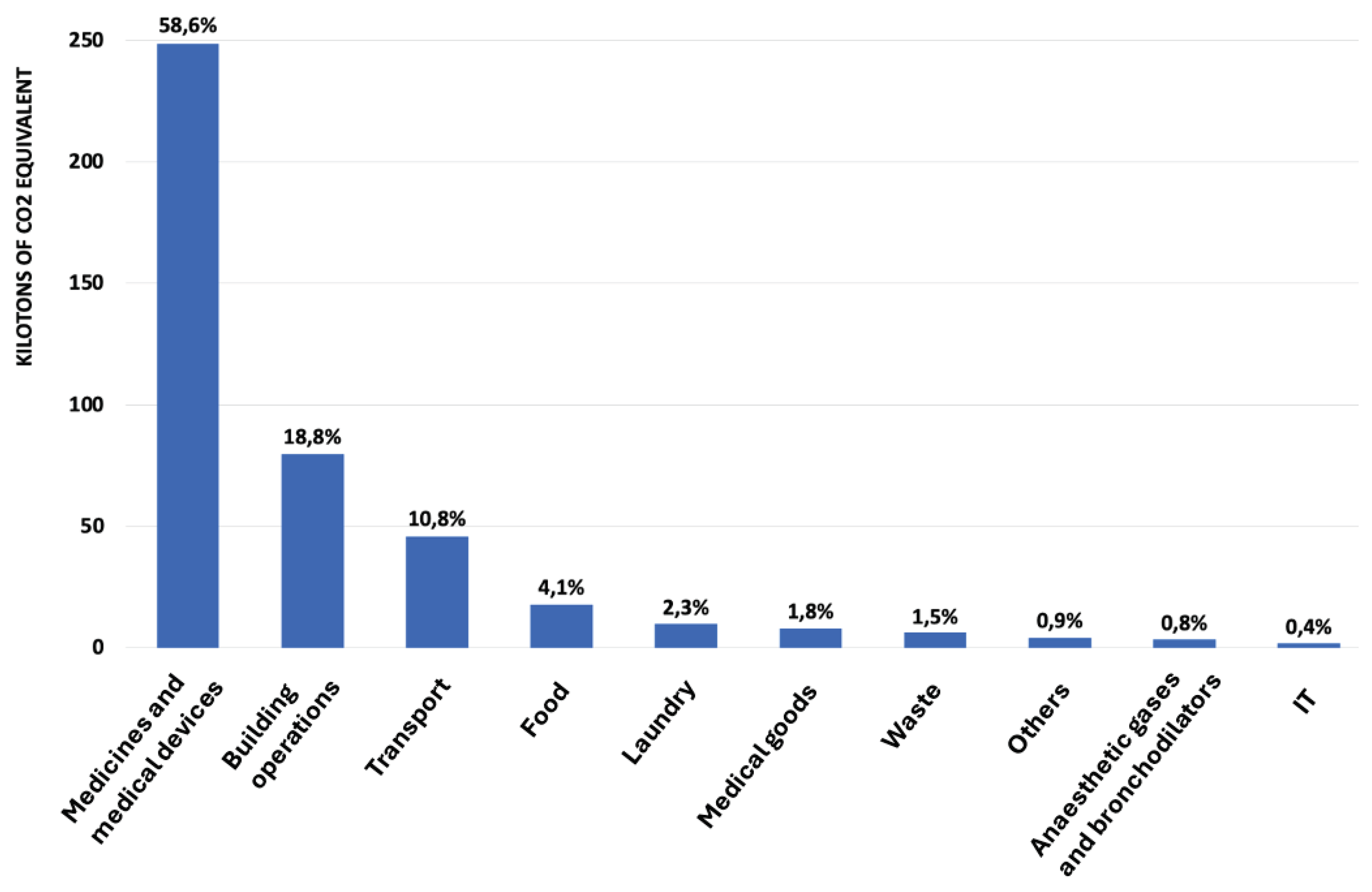
Thirdly, we detailed the distribution of greenhouse gas (GHG) emissions within the Geneva healthcare system in descending order, highlighting the predominant impact of different activities on the overall carbon footprint. At the top of the list, medicines and medical devices significantly dominate, accounting for 58.6% of the total carbon footprint. Buildings and their operation follow at 18.8%, highlighting the importance of sustainable practices in the conception and operation of medical infrastructures.
Transport accounts for 10.8% of emissions, while food, laundry and the purchase of medical equipment also contribute, with 4.1%, 2.3% and 1.8%, respectively. Waste, which includes various forms of waste generated by healthcare system activities, accounts for 1.5%. Non-medical purchases, anaesthetic gases and bronchodilators, and IT complete the list with 0.9%, 0.8%, and 0.4%, respectively (
Figure 5).
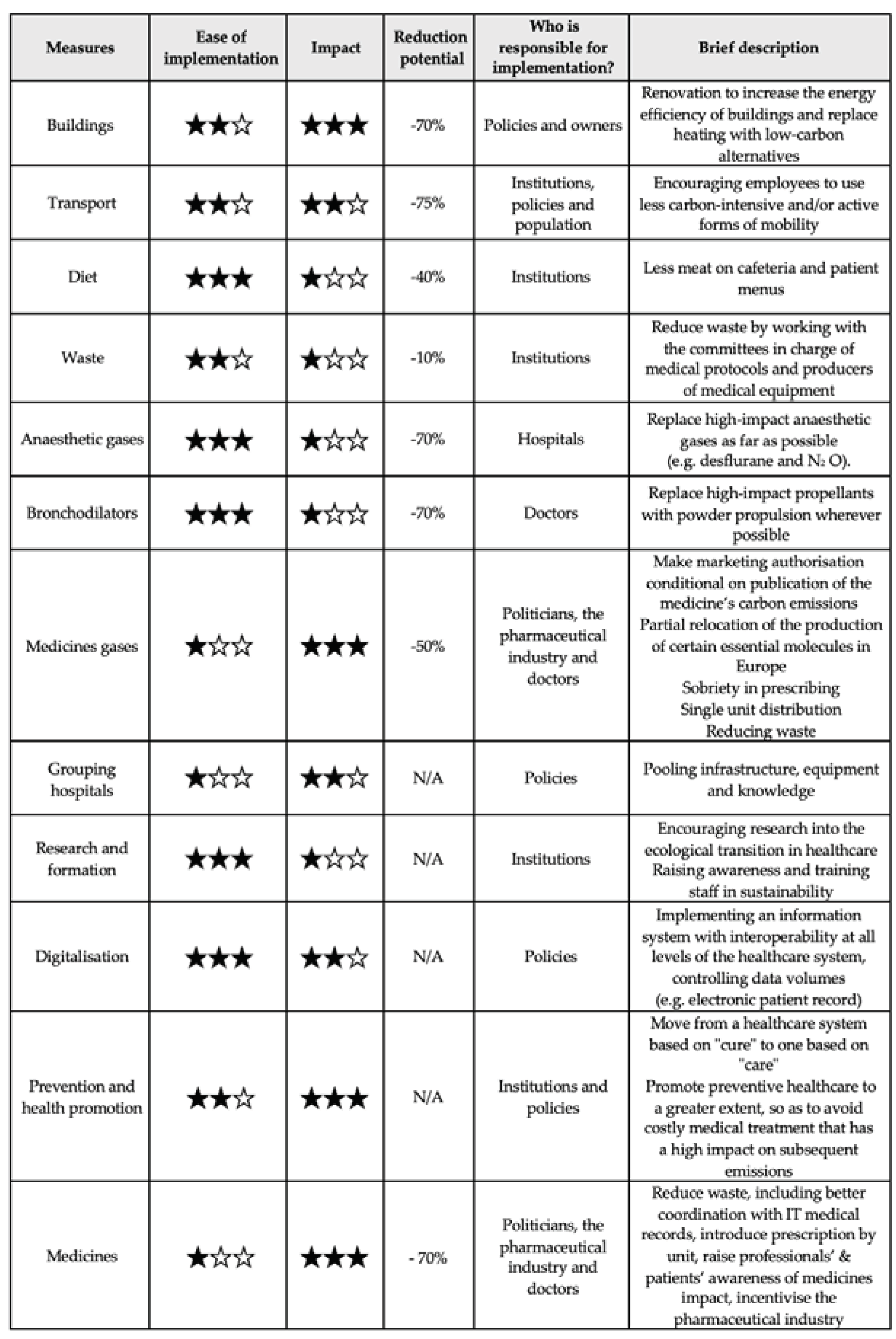
We show below a table summarising the corresponding measures that have been drawn up. The
Table 4 details the measure, the ease with which measures can be applied, their potential to reduce the carbon footprint, the responsible entitie(s) for their application and a brief description of the applicable measures.
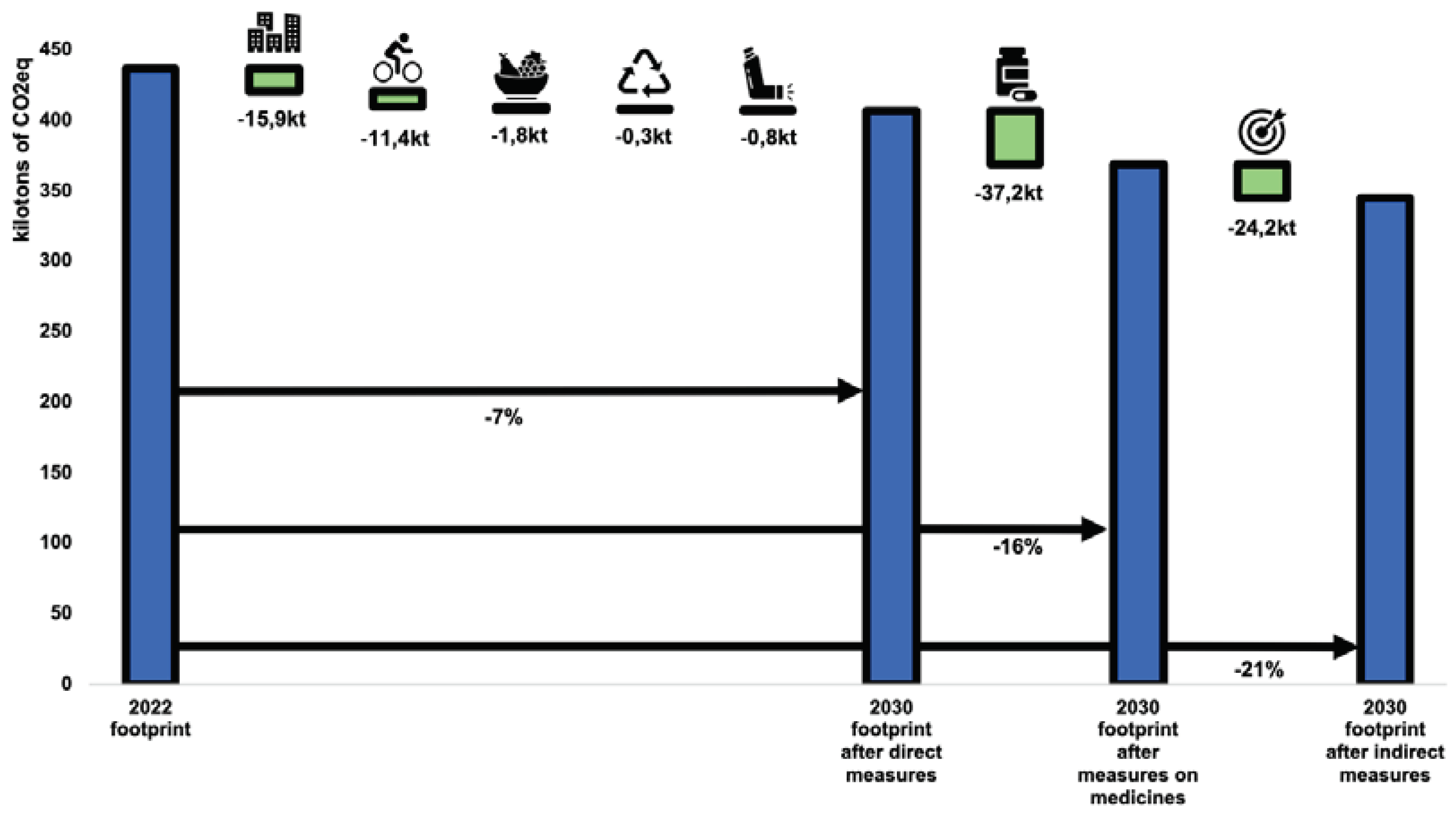
The scenario involving modest efforts by 2030 (
Figure 6) is in line with the IPCC's SSP1-2.6 scenario and aims to reduce GHG emissions from the healthcare system by 21%. Direct measures alone would help to reduce the carbon footprint by 7%, largely thanks to buildings and infrastructures. Indirect action levers and measures on medicines would enable the gap to be narrowed to the 21% target.
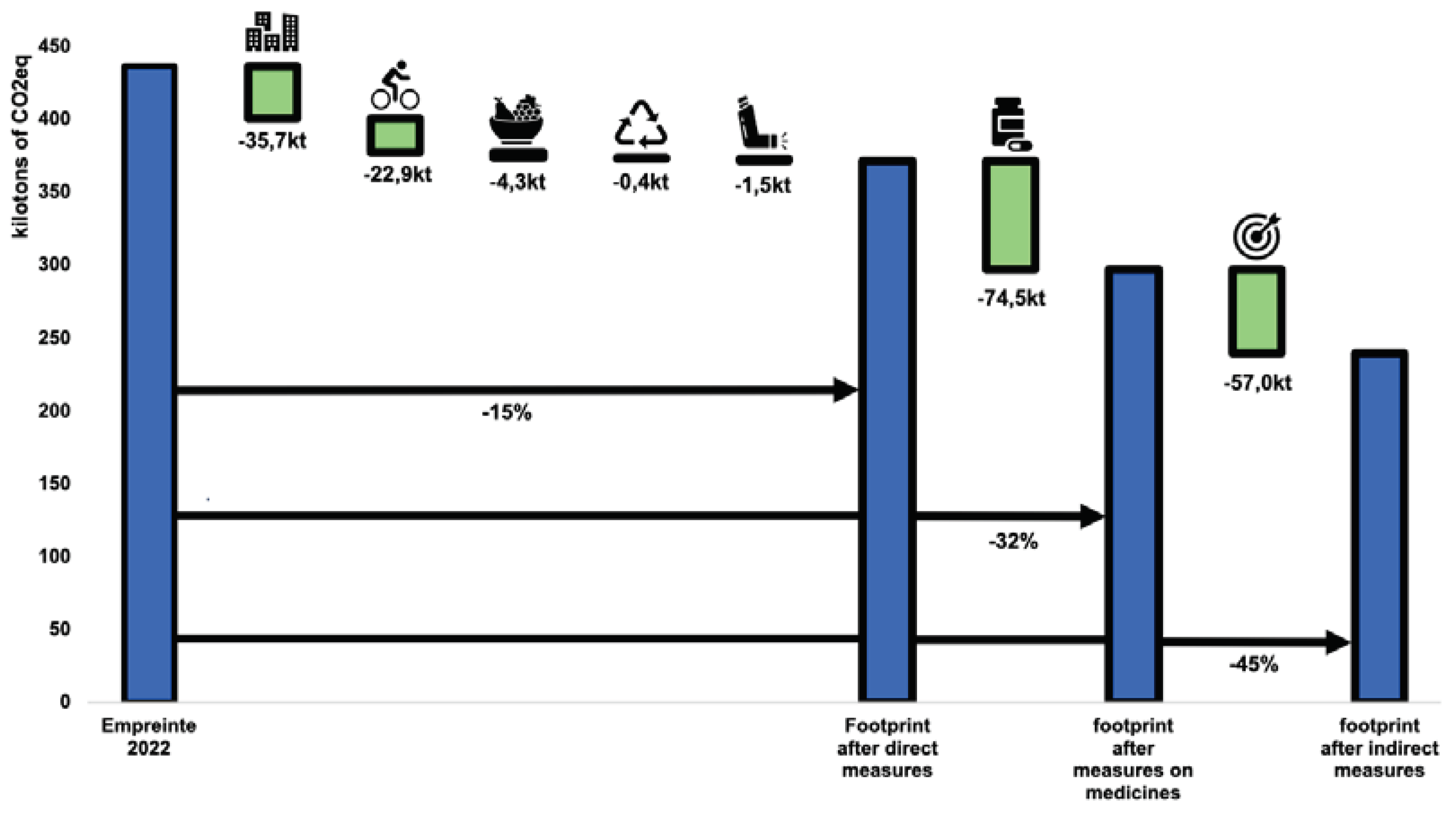
We decided to combine the scenario involving ambitious efforts for 2030 and modest efforts for 2040 because of the proximity of their targets, namely -43% for 2030 and -46% for 2040 (
Figure 7). We have therefore selected -45% as the target and drawn up this scenario with the various reductions broken down by item. Here, direct measures would contribute to a 15% reduction in the carbon footprint, while medicines and indirect measures would enable the final target of -45% to be achieved.
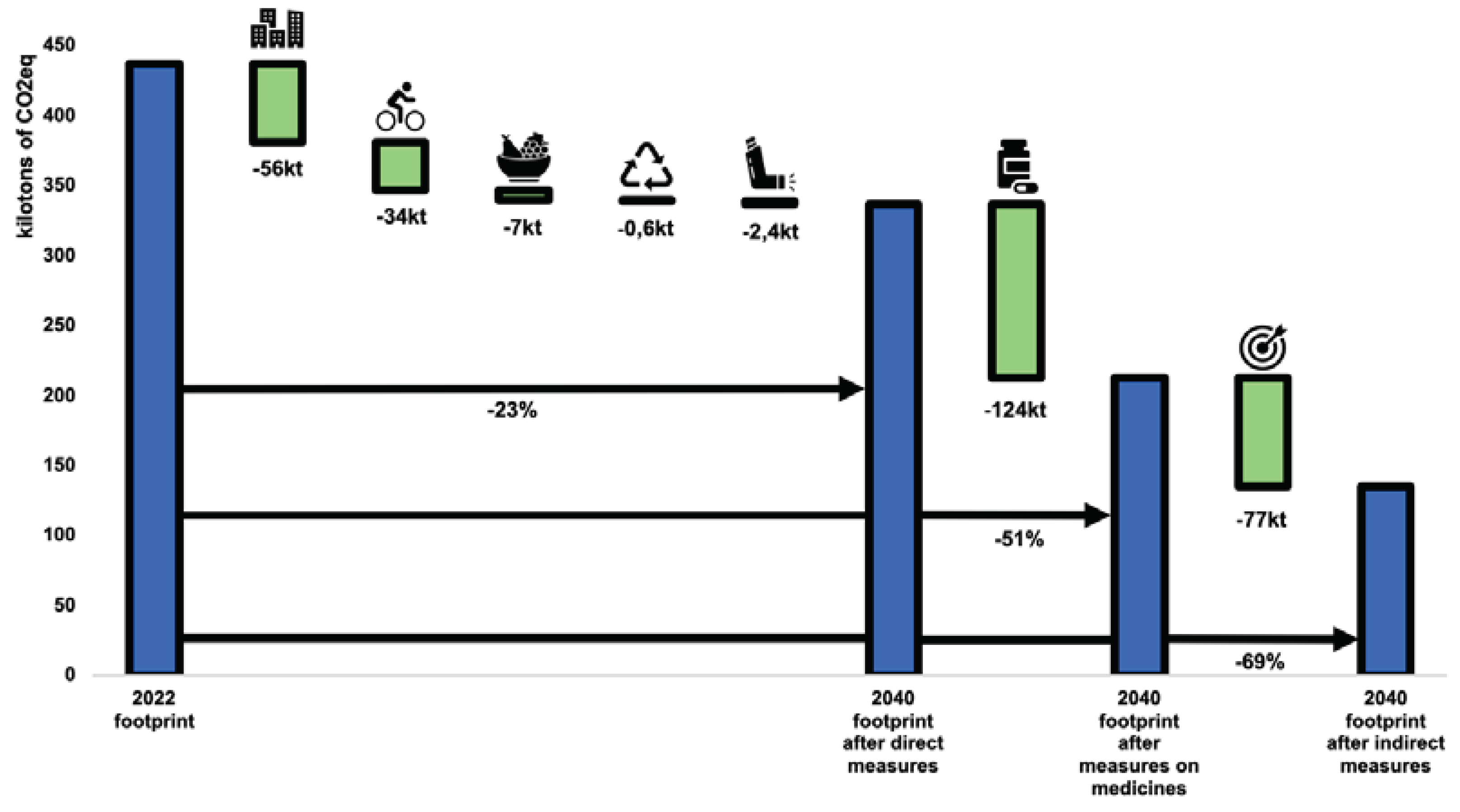
For this last scenario (
Figure 8), which is probably the most convincing because of its timeframe allowing for real long-term action plans as well as the start of the effect of certain indirect measures, we base ourselves on the SSP1-1.9 projection, with the long-term objective of achieving carbon neutrality by 2050 to limit global warming to +1.5 °C. Once again, direct measures will make it possible to reduce the carbon footprint by -23%, mainly through the heating of buildings and transport. We expect that by 2040, medicines will be produced and transported using only low-carbon energy sources, and that their waste will have been totally controlled. We also expect that our proposals for indirect measures, such as prevention and health promotion, digitisation of the healthcare system and the adoption of active modes of transport and healthy eating within planetary limits, will help to reduce the carbon footprint by 69% or more.
4. Discussion
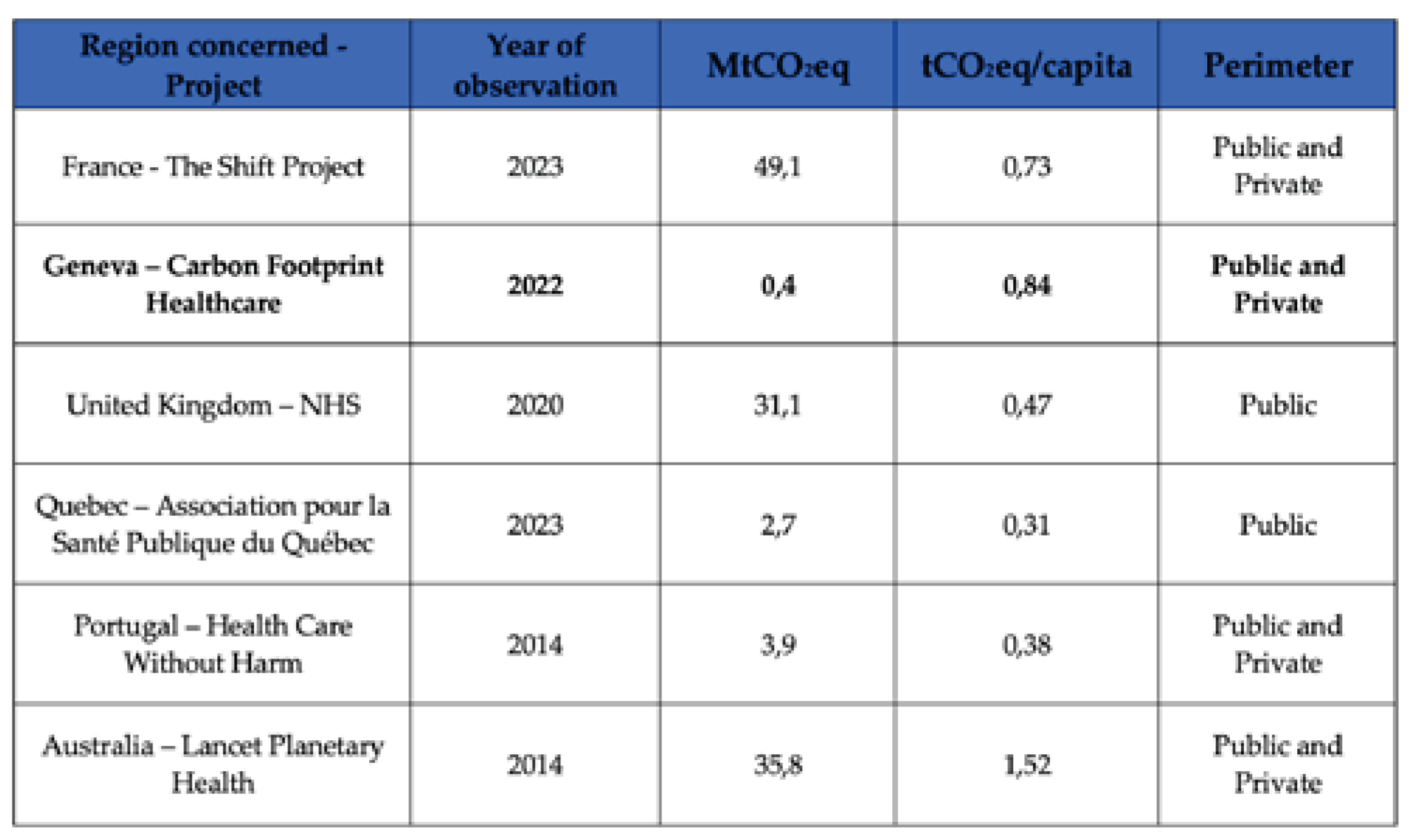
It is interesting to compare our results with the various projects carried out in other healthcare systems (
Table 5). Although Geneva's is the smallest, it is a cutting-edge healthcare system that is certainly similar to others around the world. Compared with France, whose Shift Project initiative has the methodology and scope closest to our own, we see that Geneva's carbon footprint per capita is more than 16% higher, rising from 0.73 to 0.84 tCO
2 eq. These figures should be put into perspective with the study by
Andrieu et al. published in 2023, which showed that the Swiss healthcare system had an energy footprint more than three times greater than that of France [
6]. In the UK, the per capita footprint is significantly lower than in Geneva. This result can be explained by a fully state-run healthcare system, a different scope of study and the fact that discussions on reducing their carbon footprint began in 2008. The other studies, on the Quebec, Portuguese and Australian healthcare systems, were carried out using a purely top-down approach, without collecting raw data from the healthcare institutions, a method that is very different from ours.
Keeping in minds these findings, direct and indirect measures emerge to curb the GHG emission. For each of the emission items, we unfold specific levers for action. These direct levers include areas such as optimum energy efficiency for buildings, modes of transport that favour low-GHG-emitting mobility, food, with the adoption of a diet served to staff and to nursing home residents that respects planetary limits, and waste management based on the 3R principles (Reduce, Reuse, Recycle), substitution of anaesthetic gases that are major sources of greenhouse gases, such as desflurane and nitrous oxide, replacement of bronchodilator aerosols with powder formulations wherever possible (and acceptable to the patient), and proposals for (inter-)national incentives to make medicines less carbon-intensive and promote the repatriation of part of their production.
At the same time, we have identified indirect levers that act as catalysts for other, more direct measures. Through coordination among hospitals to consolidate infrastructure and collectively manage costs, coupled with specialised training initiatives aimed at fostering awareness of sustainable healthcare practices among professionals, significant reductions in carbon emissions could be anticipated. Furthermore, offering incentives to stimulate research endeavours in this domain, alongside the streamlining of digital processes to enable personalised precision medicine, waste reduction in healthcare, and the promotion of preventive measures addressing diet, tobacco, alcohol, and physical activity, further contribute to this goal. Each of these levers would contribute to achieving the objectives set out in our scenarios, propelling the healthcare system towards the lowest possible carbon footprint, in a more sustainable and resilient way.
The suggested action levers in this study are rooted in best practices for reducing the healthcare system's carbon footprint, gleaned from thorough literature reviews and stakeholder discussions. Their applicability relies on the distinct characteristics, needs, and actions of various stakeholders. Many of the proposed measures offer co-benefits, positively impacting both public health and the environment, while simultaneously contributing to the economic sustainability of those implementing the actions. Each recommended measure aligns closely with the guidelines set forth by The Shift Project in France and the NHS Net zero initiative in the UK.
Several direct measures are proposed for buildings, including the implementation of efficient thermal renovations that meet the highest standards. Switching heating systems from fossil fuels to sources with a lower carbon footprint would substantially reduce GHG emissions linked to heat production, as would the gradual replacement of refrigeration gases with low environmental impact air conditioning systems.
For transport, the emphasis is on increasing the modal share of active modes of transport, such as cycling and walking, which are beneficial for both health and the carbon footprint. A Swedish study states that an investment of €100 million between 2018 and 2030 in Stockholm's cycling infrastructure would result in an annual saving of €12.5 million in healthcare costs through increased physical activity alone [
21]. It is also recommended to encourage the use of public transport as well as car-sharing. In addition, partial teleworking for administrative staff could be encouraged, if not already in place. Business vehicle fleets could gradually switch to electric engines. It is also recommended that executive air travel to conferences be limited, while encouraging e-learning and videoconferencing, and promoting the use of rail travel wherever it is possible. Furthermore, developing telemedicine would also help to limit non-essential patient travel. Finally, the reduction of the number of vehicles that emit greenhouse gases and fine particles (of all types) would not only help to lower the carbon footprint but would also improve people's respiratory health by reducing their exposure.
Regarding catering and food consumption in everyday life, the aim is to tend towards the
"healthy planet" dietary recommendations of the EAT-Lancet commission [
22]. This diet, which is not only beneficial for the environment, should prevent the deaths of between 10.9 and 11.6 million people a year worldwide. In concrete terms, a healthier diet means cutting red meat and added sugars by more than 50% (compared with current Western diets) and doubling the portions of vegetables, fruits, and nuts. What's more, combating food waste in the catering industry, estimated at around 20% by The Shift Project, would have a significant carbon impact.
Waste must be reduced at source. Accordingly, three major lines of action could be following the 3R rule (Reduce, Reuse, Recycle) to prevent the production of incinerable waste. A pilot study carried out on anaesthetic waste at the University Hospital Lausanne, Switzerland, showed that medical waste, whose incineration has three times the impact of household waste [
13], could be reduced by 85% after proper sorting [
23]. As far as medical devices are concerned, reuse should be encouraged rather than the use of disposable products, by supporting the production and use of reusable medical devices in conditions that ensure patient safety and maintain the quality of care.
Numerous studies have shown that anaesthetic gases have a significant impact on the environment. It is proposed to ban the use of anaesthetic gases with a high greenhouse effect, such as desflurane and nitrous oxide, and to replace them with sevoflurane or other alternatives [
19]. Desflurane and nitrous oxide have a 100-year global warming potential that is 2,540 and 273 times greater than that of CO
2, compared with 130 times for sevoflurane. Nitrous oxide is used not only in anaesthesia but also frequently in outpatient treatment. It would be possible to reduce GHG emissions from anaesthetic gases to virtually zero by replacing desflurane and nitrous oxide with alternatives [
24]. In addition, several studies recommend performing more intravenous anaesthesia rather than using gas [
25]. Finally, it is recommended that the use of bronchodilator inhalers using dry powder propulsion should be systematised, whenever possible, or with propellant gases that have a low environmental impact, emitting up to 28 times less GHG than conventional gas inhalers [
26].
In order to minimise the carbon footprint of medicines and medical devices, it is suggested that producers be encouraged to lower the unit carbon cost of each medicine by taking action on manufacturing processes and the carbon intensity of the energy used. It is also recommended to reduce the wastage of medicines and medical devices. We could hope to reduce the quantity of medicines wasted through better coordination between doctors and carers using IT tools and the implementation of electronic patient records, including access to the pharmacist. The availability of medicine prescription by unit in pharmacies would also help. Solutions should be explored to raise awareness not only among patients, but also among the medical and nursing professions, of the need to use healthcare responsibly and to promote more targeted prevention, diagnosis, and treatment practices, thereby avoiding unnecessary over-consumption of care. These country-wide incentives, coupled with concrete commitments, would create significant pressure for greener practices, while ensuring the continued availability of medicines essential to the health of the population.
Indirect levers represent cross-cutting actions that would act as catalysts, enabling future levers of action to be activated. Acting solely on the above-mentioned direct levers will probably not be enough to achieve ambitious targets for reducing GHG emissions, and measures that genuinely address healthcare processes and professions are needed. Through these various measures, it would be advisable to start thinking about the role of the healthcare system, which would aim more at keeping the population in good health and less at simply waiting for them to develop illnesses that then need to be treated. This virtuous circle presupposes greater promotion of preventive health care, so as to avoid costly medical treatment with high subsequent emissions. Recourse to emergency services and hospital treatment could be minimised as far as possible, given their very large contribution to the carbon footprint of the cantonal healthcare system. A far-reaching and gradual transformation of the healthcare system, particularly in terms of access to care, could be implemented. In Denmark, for example, patients are obliged to go through a general practitioner, who then refers them to a specialist, or for further tests, or even to hospital. This reform has enabled them to reduce the number of hospitals from 128 to 21 in forty years [
27]. These transformations, which are useful for the sustainability and resilience of our healthcare system, would need to be steered at government level, and would require support and training for healthcare professionals, greater expertise in these issues, the use of digital technology to support process efficiency, and the promotion of preventive behaviours conducive to better population health.
Acting upstream on prevention and health promotion would make it possible to improve the health of the people of Geneva and reduce their recourse to healthcare. The challenge is to better control the demand for care and travel, make less use of infrastructure, consume less medicines, use fewer medical devices, imaging and biological analyses, all in the service of more effective and efficient medicine. An analysis of healthcare expenditure reveals that Switzerland devotes less than 3% of its healthcare expenditure to prevention and health promotion, which places it below the average for OECD countries [
28]. The desire to reduce the carbon footprint of the healthcare system could prove to be an opportunity for the players involved to consider prevention as a genuine investment. The return on investment (ROI) for each franc invested in the fight against tobacco smoking is between 28 and 48 francs, and between 11 and 29 francs for the fight against alcohol [
29].
Switzerland faces considerable costs associated with addiction to tobacco, alcohol and illicit drugs, amounting to CHF 3 billion, CHF 477 million and CHF 274 million respectively for 2017 [
30]. The direct costs to the healthcare system attributable to patients suffering from these addictions are considerable, totalling almost CHF 4 billion. It should be noted that our FE estimates that every 1,000 francs spent on services and activities related to human health approximately emits 100 kg of CO
2[
13]. Based on the population of Geneva, and on the assumption that the Geneva population is no more affected by these addictions than the rest of the Swiss population, the direct costs of these addictions for the canton's healthcare system would be in the region of CHF 221 million per year. Multiplied by the emission factor used in our study, this would correspond to an emission of 22,000 tCO
2eq linked to these addictions alone. Prevention aimed at reducing these risky behaviours, both for the individual and for the planet, would make it possible to reduce the use of the healthcare system and the carbon footprint of the associated care.
Promoting active mobility, such as cycling and walking, is good for health and the environment [
21]. Reducing the number of vehicles that emit greenhouse gases and fine particles and increasing the modal share of active mobility will not only help to reduce the carbon footprint but will also improve people's health by reducing their exposure to pollution and increasing their physical activity. The promotion of moderate daily physical activity, a healthy diet (Planetary Diet [
22]), intellectual practices and socialisation limit many chronic diseases (e.g. diabetes, obesity, cardiovascular disease, cancer and Alzheimer's disease), and reducing alcohol and tobacco consumption would generate major health gains and substantial savings, while reducing the carbon footprint of the healthcare system. Our analyses underline the importance of investing in prevention, first and foremost in terms of public health, but also in terms of economic efficiency and environmental sustainability.
Our study enabled us to decipher the main sources of carbon dioxide emission in the Geneva's healthcare system. On the medical context, medicines and medical devices play a prominent role and even overshadow other emission items in hospitals. When comparing the different healthcare sub-sector, hospitals come out on top and account for almost 50% of the total carbon footprint of the healthcare system. Unsurprisingly, we find the same major emission items as in other economic branches, namely the heating of the buildings, professional and commuting transportation, and food. On the one hand, this shows the responsibility of hospitals and public health policies to reduce their impact that had already been highlighted in previous studies. On the other hand, this encourages a raise in awareness of the other, more heterogeneous, actors who are accountable for the other half of the emissions and who should share the goal of overall decrease of emissions.
Our study of the carbon footprint of the healthcare’s hospital system sought to be as representative as possible of the GHG emissions emitted by this system in the canton of Geneva and seeks to provide trends and estimates rather than precise measurements. However, it is essential to take into account several limitations that may have affected the accuracy and sometimes the reliability of some of our results.
Firstly, the lack of direct measurement of greenhouse gases (GHGs) is a constraint faced by this type of study. The collection of raw data subsequently converted into tCO
2 eq by emission factors and the use sometime of monetary units (CHF) to quantify GHG emissions, particularly for medicines, may have introduced levels of uncertainty. The monetary factor used for medicines is independent of the type of medicine, which does not necessarily reflect the reality of the emissions associated with each medicine but produces an average that we hope is representative. We have used a French EF for medicines, even though the medicine prices differ in Switzerland and can introduce uncertainties. Furthermore, monetary EFs, by their very nature, are estimated with a very high degree of uncertainty [
13]. The results of calculations using these factors should therefore be treated with caution. Emission factors based on raw data are much more accurate, with uncertainties ranging from a few percent for heating, for example, to around 60% for certain modes of transport per km [
13].
Secondly, it should be noted that neither the NHS Net zero initiative, nor The Shift Project up to 2022 have carried out final uncertainty interval calculations on their carbon footprint results. In 2023, The Shift Project arrives at an uncertainty interval of between 6.6 and 10% of their carbon footprint. Their project, at national level, uses a lot of estimates, averages, and extrapolation. We expect to achieve a similar level of uncertainty intervals by using few monetary EFs and few subjective estimates, and by collecting a lot of data in the field.
It is essential to be aware of these limitations in order to interpret the results of our analyses, but these limitations should not change the main message derived from this study, as they are very consistent with those found in the international literature on the subject.