Introduction
The Respiratory Syndrome in the Middle East A new coronavirus known as MERIS-CoV causes severe respiratory diseases in people. The primary reservoir and source of infection for humans is thought to be dromedary camels, which are thought to have contracted the virus from bats. Due to its enormous genetic variety and rapid evolution, the virus can circulate in different nations and areas as different strains and clusters. Molecular epidemiology and phylogenetic research have demonstrated that MERS-CoV has been transmitted from human to human through intimate contact, particularly in healthcare settings, and that there have been several spillover events from camels to humans. It can also be transmitted via breathing in contaminated air, coming into touch with contaminated objects, and respiratory droplets. The first case 65-year-old man who passed away from acute pneumonia and multiple organ failure [
1]. As of right now, most MERS-CoV cases have their origins in Middle Eastern nations, such as Saudi Arabia, the UAE, Qatar, Oman, Kuwait, and Iran [
1,
2,
3] MERS-CoV-related clinical disease might vary from moderate upper respiratory symptoms to multisystem failure and fulminant pneumonia. Compared to other coronaviruses, MERS-CoV poses a greater risk. The incubation period spanned two to fourteen days, and the risk of fatality was increased for those with underlying medical disorders. A new coronavirus known as Middle East Respiratory Syndrome Coronavirus (MERS-CoV) causes severe respiratory diseases in people [
4].
MERS-CoV has caused multiple outbreaks in Saudi Arabia and other parts of the Middle East since 2012. This poses a danger of transmission and fatality, especially in vulnerable populations [
3,
5].
Our goal in this review of the literature was to give a thorough overview of the MERS-CoV outbreak in Saudi Arabia, covering its epidemiological analysis, public health response, effects, and takeaways. based on the research that have been published and their contributions to the subject This study intends to reduce the risk of MERS-CoV transmission and highlight the importance and relevance of this issue, as well as provide feasible measures for averting future outbreaks. It is our goal that these results will add to the current conversation on MERS-CoV and influence Saudi Arabia's public health practices and policies.
Background
Middle East Respiratory Disease A zoonotic virus known as coronavirus (MERS-CoV) was discovered in Saudi Arabia in 2012 [
1,
6]; thought to have originated in bats and is spread to people through camels. It is genetically different from the new coronavirus that causes COVID-19 and the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) [
1,
6,
7]. Through respiratory droplets, contact with contaminated bodily fluids, or exposure to contaminated settings, MERS-CoV can transfer from one person to another [
8,
9]. The virus can infect several respiratory tract cells in humans, including as the alveoli, bronchioles, and upper and lower airways [
6]. Furthermore, the kidneys, liver, and spleen are among the other organs that MERS-CoV might infect. Fever, coughing, shortness of breath, pneumonia, and organ failure are among the signs and symptoms of MERS-CoV [
6,
10].
MERS-CoV required two to fourteen days to incubate, with an average of five days [
8]. Comparing MERS-CoV to SARS-CoV (10%) and COVID-19 (2%), the former has a death rate of about thirty-five% [
5,
8,
9,
11,
12]. Older age, male sex, underlying medical disorders, and comorbidities such diabetes, hypertension, chronic lung disease, chronic kidney disease, and immunosuppression are risk factors for catastrophic outcomes from MERS-CoV infection [
3,
4,
5,
13].
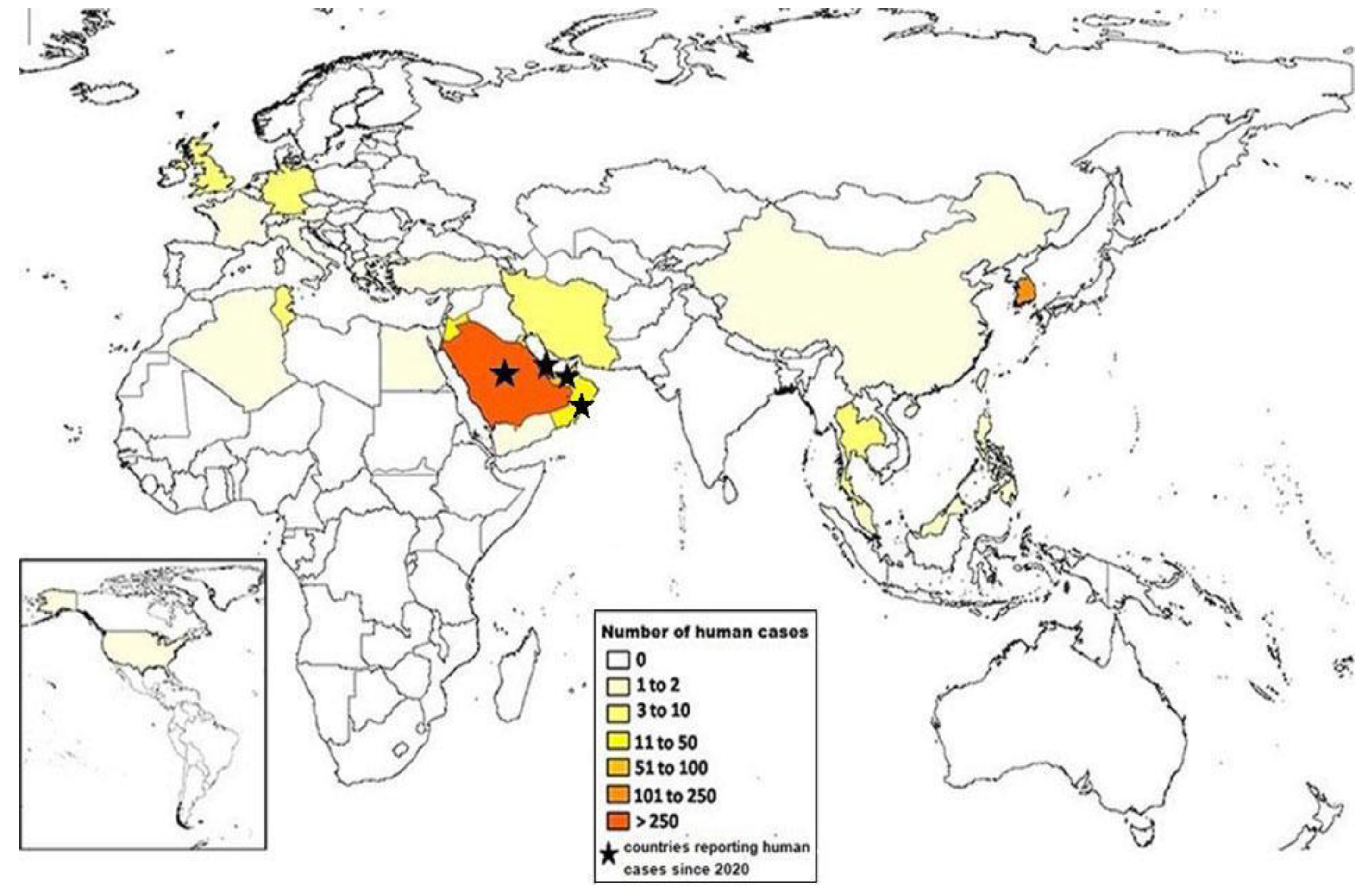
Most of the incidents had something to do with visiting or living in the Middle East, or with interacting with tourists from that area. But certain cases have also been documented in other parts of the world, including North America, Asia, Europe, and Africa (
Figure 1). Most of these infections were linked to medical personnel or tourists who had encounter camels or MERS-CoV patients in the Middle East.
Features of Outbreaks
The capital and largest city of Saudi Arabia, Riyadh, was the main target of the MERS-CoV outbreak that started in March 2023. There are about 8.5 million people living in the Riyadh region, which has an area of about 404,000 square kilometers [
3]. This outbreak's first confirmed case of MERS-CoV infection involved a 65-year-old man who met camels on a farm close to Riyadh. After being admitted to the hospital with fever, cough, and dyspnea, the patient passed away a few days later [
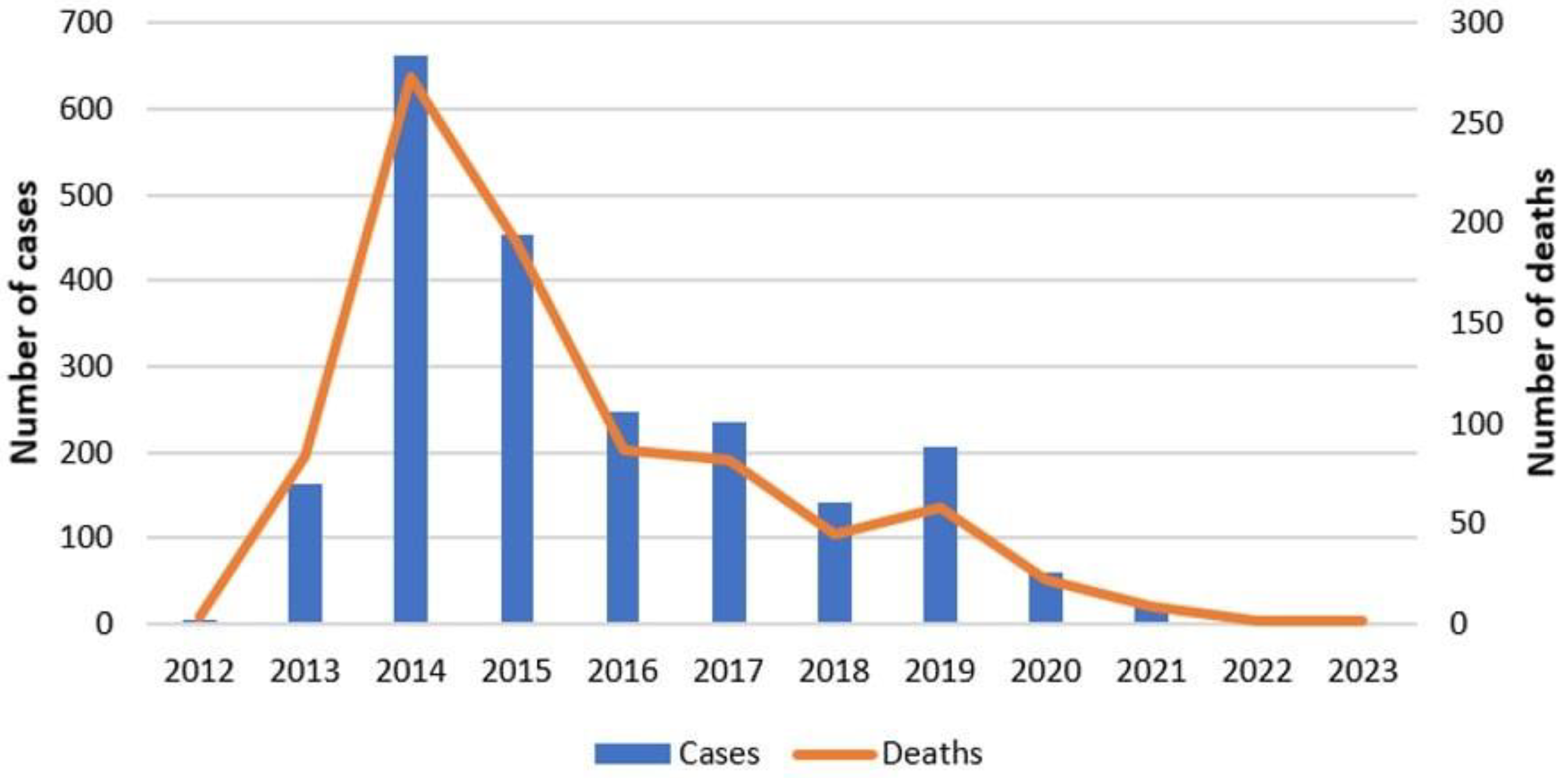
14]. The greatest number of cases (79) and deaths (28) recorded in May 2023 indicate that the outbreak peaked in April and May of that year.
Three more cases—two of which resulted in deaths—between September 13, 2022, and August 12, 2023, were recorded by the Ministry of Health. Asser, Makkah Al Mukaromah, and Riyadh were the locations of these incidents (
Figure 2).
Real-time polymerase chain reaction was used in the laboratory (RT-PCR) [
15,
16]. The three patients had symptoms like fever, coughing, and dyspnea and were not employed in the medical field. Additionally, the patients had underlying medical issues. Within 14 days of the commencement of symptoms, all three patients had drank raw camel milk, and two had previously interacted with dromedary camels. Males 42, 83, and 85 years old were the affected persons (
Table 1).
In all six WHO regions, twenty-seven countries have reported human illnesses with MERS-CoV since the virus's initial discovery in Saudi Arabia in 2012 [
1,
6,
8]. Including these latest cases, Saudi Arabia accounted for 2,196 (84%) of the 2,605 cases that were recorded. Of the 937 recorded deaths in these twenty-seven countries—including the recently reported deaths—Saudi Arabia accounted for 856 (91%) of the deaths (
Figure 3). The instances underscore the persistent existence of MERS-CoV in Saudi Arabia, as well as the ongoing danger of transmission. To stop the virus from spreading further, surveillance vigilance, early identification, and quick response times are still essential. The main goal should be to increase public knowledge of the possible dangers of coming into touch with dromedary camels and consuming raw camel milk. We can work to lessen the effects of MERS-CoV and safeguard public health both in Saudi Arabia and around the world by putting into place efficient preventive measures and encouraging public health initiatives [
17,
18,
19].
There was a seasonal trend to the outbreak; most cases happened between March and June, which is when camels calve. These results imply that camels are important in the human transmission of MERS-CoV. The outbreak also revealed a spatial trend, with most infections happening in rural areas with a high concentration of camel farming and trading. A history of direct or indirect interaction with camels or camel products, such as milk, meat, or urine, was reported by about 85% of the patients [
4,
5,
14].
Because the MERS-CoV outbreak overloaded the healthcare system, disrupted social and economic activity, and raised public concern and stigma, it had a severe impact on public health and safety [
8,
9,
10]. Additionally, because some instances of the outbreak were connected to travel or interaction with Saudi Arabian passengers, the outbreak posed a concern to nearby nations and areas.
Clinical Features and Epidemiological Studies of MERS-Co
A zoonotic virus called MERS-CoV spreads from animals to people. Research has indicated that humans can contract the disease by coming into direct or indirect contact with diseased dromedary camels, however it is still unknown how exactly the infection spreads [
2,
8,
10]. In healthcare settings, human-to-human transmission can happen and is most common among close encounters.
27 nations have reported MERS cases to the World Health Organization (WHO) in accordance with the International Health Regulations (2005) since the identification of MERS-CoV in 2012: Algeria, Austria, Bahrain, China, Egypt, France, Germany, Greece, The Islamic Republic of Iran, Italy, Jordan, Kuwait, Lebanon, Malaysia, the Netherlands, Oman, Philippines, Qatar, Republic of Korea, Kingdom of Saudi Arabia, Thailand, Tunisia, Türkiye, United Arab Emirates, United Kingdom, Philippines, and Yemen [
2,
4,
8,
9]. Middle Eastern countries report many MERS-CoV cases. The case fatality rate is 35%, however as mild instances of MERS can go unnoticed by the current surveillance systems, this figure may be overestimated rather than the genuine mortality rate.
MERS-CoV infection can cause moderate respiratory symptoms or no symptoms at all, severe acute respiratory illness, or even death [
1,
6,
20]. Shortness of breath, fever, and cough are typical signs of MERS [
1,
8]. Pneumonia is a frequent finding in MERS patients, but it is not guaranteed to occur. Additionally, reports of digestive symptoms, such as diarrhea, have been made [
4,
5,
14]. Respiratory failure brought on by severe disease may necessitate mechanical ventilation or supportive care in an intensive care unit [
3,
9,
14,
15,
21]. Severe disease is more likely to strike the elderly, those with compromised immune systems, and those suffering from long-term conditions such diabetes, hypertension, cancer, chronic lung disease, and renal disease [
5,
9]. Some unusual presentations have been documented, such as diarrhea that occurs before pneumonia develops and mild respiratory illness without fever. Patchy densities or opacities, either unilateral or bilateral, interstitial infiltrates, consolidation, or pleural effusion are possible radiographic findings. There have been reports of rapid progression to extrapulmonary consequences (acute kidney injury needing renal replacement treatment, hypotension requiring vasopressors, hepatic inflammation, and septic shock), acute respiratory failure, acute respiratory distress syndrome (ARDS), and refractory hypoxemia [
5,
8,
9]. Leukopenia, lymphopenia, thrombocytopenia, and increased lactate dehydrogenase (LDH) levels are laboratory results at the time of admission. There have been instances of coinfection with different respiratory viruses and bacteria [
2,
8].
There is currently no known vaccination or targeted therapy, however research is being done on several vaccines and medicines that are unique to MERS-CoV. Supportive care is given, considering the patient's symptoms and clinical state. Most MERS-CoV infections have been reported to the World Health Organization (WHO) by Saudi Arabia, which as of June 2020 accounted for 83.6% of all cases.
Age ≥65, underlying illnesses, and ≥5 days delay in diagnosis are among the risk factors for death from MERS-CoV infection that epidemiological investigations have discovered. However, female patients under sixty-five who have animal contact have a higher risk of dying, whereas male patients over sixty-five have a decreased risk [
2,
8,
16].
The transportation network is the main factor driving the spatial distribution of MERS-CoV, with hubs for both local and international spread being Riyadh, Saudi Arabia, and Abu Dhabi, United Arab Emirates. Due to travel and trade, the disease has been brought to other continents, where it has spread to close contact and healthcare settings [
1,
8,
10].
When compared to the preceding period from December 2021 to October 2022, when four instances were reported without any deaths, this indicates a decrease in the number of cases.
Public Health Responses
With assistance from various national and international stakeholders as well as the World Health Organization (WHO), the Ministry of Health (MOH) in Saudi Arabia has responded to the MERS-CoV outbreak in 2023. The methods to improve clinical management, risk communication, travel limitations, surveillance, infection prevention and control, and coordination were all included in the thorough responses [
18,
19,
20]. The response was successful despite certain obstacles, and it was assessed using a range of metrics that over time revealed a decrease in the number of cases and fatalities.
Improving the capability of the laboratory and surveillance systems is one of the MOH's primary initiatives. Active case detection, contact tracing, DNA analysis, environmental monitoring, animal observation, and laboratory testing were all part of this. In accordance with the International Health Regulations (IHR, 2005), the MOH notified the WHO of all verified cases and fatalities and disseminated the virus's genomic sequences to researchers worldwide. This made sure that timely and correct information was provided to direct the actions related to response and decision-making.
Increasing the effectiveness of infection prevention and control procedures was another crucial step. In communities and hospital settings, the MOH has put standard, contact, and droplet precautions into place. Healthcare professionals and other frontline responders received training, direction, and personal protective equipment (PPE) from the MOH. This shielded healthcare personnel from infection and assisted in stopping the virus's spread [
19].
Patient assistance and clinical management were given top priority. The MOH made ensuring that MERS-CoV cases were promptly diagnosed, isolated, treated, and referred. Additionally, the MOH has set up dedicated MERS-CoV treatment centers and carried out clinical investigations for treatments. This enhanced patient outcomes and the standard of care [
3].
The MOH has distributed accurate and up-to-date information about MERS-CoV and its symptoms, transmission, prevention, and control to increase public awareness and encourage risk communication. To promote health education and behavioral change, the MOH also collaborated with a variety of media sources, social media platforms, religious leaders, community leaders, and civil society organizations. This promoted public awareness and confidence in health officials [
9,
21].
To stop the virus from spreading further, screening procedures and travel restrictions were also put in place. Travelers were warned by the MOH to stay away from camels and camel products in impacted areas and to get medical help if they had signs of MERS-CoV infection. At ports of entry and departure, the MOH also checked visitors for respiratory ailments and exposure records.
The reaction has been successful despite several obstacles, including a lack of workforce and resources in remote or rural areas, obstacles to behavioral change arising from cultural and religious beliefs, political and socioeconomic instability in the area, and the introduction of new viral strains. Over time, the number of cases and deaths decreased, according to the CDR, CFR, R0, IAR, and VCR indices. This result implies that the public health approach is successful in stopping new infections.
Still, there is potential for improvement in terms of raising the vaccination rate, improving infection prevention and control protocols, and fortifying the security of global health. To overcome these obstacles and guarantee a well-coordinated and long-lasting response to upcoming outbreaks, the MOH should keep up its strong collaboration with the WHO and other relevant parties.
Effect, Takeaways, Post-Epidemic Analysis, and Readiness
The MERS-CoV outbreak is not the first or the last respiratory illness outbreak that puts the world's health at risk and puts hospital infection control procedures to the test [
17,
18,
22]. Prior SARS outbreaks in 2003 and COVID-19 outbreaks in 2019–2020 have shown that novel coronaviruses can spread quickly across nations and continents, cause serious sickness, and even result in death [
8,
9,
17]. Not only have these epidemics taught us important lessons about reducing nosocomial respiratory pathogen transmission, but they have also improved hospital infection management [
7].
Public health, healthcare systems, and society are all significantly impacted by the MERS-CoV outbreak, both in Saudi Arabia and beyond. It impacts social and economic spheres, stresses the healthcare system, and results in substantial morbidity and mortality among affected persons. But it also offers important insights for managing infectious disease epidemics in the future. (
Figure 4) Among the lessons learned are the importance of prompt case detection and reporting, efficient infection prevention and control procedures, and community-based interventions and clear, consistent risk communication to empower the public [
15,
21].
Safe and efficient vaccines and treatments against MERS-CoV must be developed and implemented to stop or manage such outbreaks and lower the risk of MERS-CoV transmission [
13,
23]. Enhancing global health security and readiness via multisectoral and multilateral cooperation and coordination is also crucial [
17]. We can better equip ourselves for future outbreaks by funding the development of MERS-CoV vaccines and treatments, as well as making sure they are accessible and affordable.
Conclusion
The MERS-CoV outbreak in Saudi Arabia poses a serious risk to public health and has put the nation's and the region's healthcare systems under strain. Despite several obstacles, hurdles, and problems, including scarce resources, slow reporting, low compliance, a lack of coordination, inadequate testing, false information, and political meddling, the Ministry of Health (MOH) and its partners' answers were praiseworthy and making advancements. On the other hand, the outbreak had a profound effect on Saudi Arabian society, public health, and healthcare institutions. This outbreak serves as a reminder of the ongoing and changing risks to international health, security, and preparedness that newly and re-emerging infectious diseases represent. Enhancing monitoring and laboratory capabilities, putting in place efficient infection prevention and control measures, creating and implementing safe and effective vaccines and treatments, empowering, and involving the public, and bolstering regional and international collaboration and coordination are therefore imperative. It is imperative to take proactive measures that prioritize early case detection and reporting, timely and transparent data sharing among stakeholders, effective risk communication, community-based interventions, and multisectoral and multilateral collaboration to prevent or mitigate these consequences.
The Saudi Arabian MERS-CoV outbreak serves as a timely reminder of the significance of anticipating and responding to new infectious disease outbreaks. We can shield our communities and ourselves from the damaging impacts of infectious diseases on people's health and well-being by cooperating to address these issues.
References
- Zhang AR, Shi WQ, Liu K, Li X Lou, Liu MJ, Zhang WH, et al. Epidemiology and evolution of Middle East respiratory syndrome coronavirus, 2012–2020. Infect Dis Poverty. 2021 Dec 1;10(1).
- Al-Jasser FS, Nouh RM, Youssef RM. Epidemiology, and predictors of survival of MERS-CoV infections in Riyadh region, 2014–2015. J Infect Public Health. 2019 Mar 1;12(2):171–7. [CrossRef]
- Nature [Internet]. Saudi Arabia worst hit by MERS; [cited 2024 Jan 23]. Available from: https://www.nature.com/articles/d42473-019-00425-9.
- Altaluoni A, Byung Chul C. Epidemiologic characteristic of human Middle East respiratory syndrome in Saudi Arabia, 2015–2017. J Infect Public Health. 2019 Jan;12(1):136–7. [CrossRef]
- Nassar, M. S., Bakhrebah, M. A., Meo, S. A., Alsuabeyl, M. S., & Zaher, W. A. (2018). Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: epidemiology, pathogenesis, and clinical characteristics. European review for medical and pharmacological sciences, 22(15), 4956–4961. [CrossRef]
- Chughtai A. Epidemiology and Characteristics of Middle East Respiratory Syndrome Coronavirus (MERS-CoV). 2022.
- Choudhary OP, Priyanka, Singh I, Rodriguez-Morales AJ. Second wave of COVID-19 in India: Dissection of the causes and lessons learnt. Vol. 43, Travel Medicine, and Infectious Disease. Elsevier Inc.; 2021.
- Ebrahim SH, Maher AD, Kanagasabai U, Alfaraj SH, Alzahrani NA, Alqahtani SA, et al. MERS-CoV Confirmation among 6,873 suspected persons and relevant Epidemiologic and Clinical Features, Saudi Arabia — 2014 to 2019. EClinicalMedicine. 2021 Nov 1; forty-one.
- Article Nadira Al-Baghli RA, Ali Al Dorazi S, Mohammed Nooh MBBS RS, Hassan Zainaldeen M, Alsahi SM, Ahmed Al Talib A, et al. Archives of Infectious Diseases & Therapy Incidence, management, and outcome of MERS CoV outbreak in a hospital, Eastern Province, Saudi Arabia [Internet]. 2020. Available from: www.opastonline.com.
- Bernard-Stoecklin S, Nikolay B, Assiri A, Bin Saeed AA, Ben Embarek PK, El Bushra H, et al. Comparative Analysis of Eleven Healthcare-Associated Outbreaks of Middle East Respiratory Syndrome Coronavirus (Mers-Cov) from 2015 to 2017. Sci Rep. 2019 Dec 1;9(1). [CrossRef]
- Priyanka, Choudhary OP, Singh I. Evolution of SARS-CoV-2: A prediction on the lineages and vaccine effectiveness. Vol. 40, Travel Medicine, and Infectious Disease. Elsevier Inc.; 2021.
- Choudhary OP, Saied ARA, Priyanka, Ali RK, Maulud SQ. Russo-Ukrainian war: An unexpected event during the COVID-19 pandemic. Vol. 48, Travel Medicine, and Infectious Disease. Elsevier Inc.; 2022.
- Priyanka, Choudhary OP, Singh I. Protective immunity against COVID-19: Unravelling the evidence for humoral vs. cellular components. Vol. 39, Travel Medicine, and Infectious Disease. Elsevier Inc.; 2021.
- Al Hajjar S, Memish ZA, McIntosh K. Middle east respiratory syndrome coronavirus (MERS-CoV): A perpetual challenge. Vol. 33, Annals of Saudi Medicine. 2013. p. 427–36. [CrossRef]
- Al-Tawfiq JA, Memish ZA. Infection control measures for the prevention of MERS coronavirus transmission in healthcare settings. Vol. 14, Expert Review of Anti-Infective Therapy. Taylor and Francis Ltd; 2016. p. 281–3.
- Al-Nafisi A, Almutairi A, Al-Mudarra S, Saudi A, Epidemiology F, Program T, et al. Infection Prevention and Control for the MERS-COV, 2019: A Teaching Case-Study Student’s Guide.
- Risk CommuniCation and Community EngagEmEnt foR Ebola ViRus disEasE PREPaREdnEss Lessons Learnt and Recommendations from Burundi, Rwanda, South Sudan, Tanzania and Uganda Risk Communication and Community Engagement for Ebola Virus Disease Preparedness and Response REPORT OF A UNICEF REVIEW MEETING.
- Hospital Infection Control Guidelines.
- Control Branch I, for Health Protection C. Guidelines on Infection Control Practice in the Clinic Settings of Department of Health Content INDEX.
- MIDDLE EAST RESPIRATORY SYNDROME CORONAVIRUS; GUIDELINES FOR HEALTHCARE PROFESSIONALS. 2018.
- Advice to Health Care Workers caring for patients with MERS-CoV infection Statement of the Health Security Committee (HSC)* based on scientific input by the European Centre for Disease Prevention and Control (ECDC) [Internet]. 2015. Available from: http://apps.who.int//iris/bitstream/10665/174652/1/WHO_MERS_IPC_15.1_eng.pdf?ua=1A.
- Anis H, Essayli D, Emir Hamitoglu A, Basha Shaik A, Nazir A, Wellington J, et al. Mental health impact of the catastrophic 2023 earthquake on Turkish youth: psychological distress amidst humanitarian crises. International Journal of Surgery: Global Health. 2023 Jul;6(4). [CrossRef]
- Priyanka, Choudhary, OP, Singh I. Making sound public health decisions for the roll-out of COVID-19 vaccines. J Travel Med. 2021 May 1;28(4). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).