Introduction
Skeletal class II malocclusion is one of the most common orthodontic problems, affecting about 30% of the population [
1,
2]. Class II development can occur from a variety of skeletal and dental factors, although mandibular retrognathism is considered to be the primary cause [
3,
4]. Functional appliances are often utilized to treat class II malocclusion caused by mandibular retrognathism [
5,
6,
7]. Class II elastics or removable functional appliances are typically recommended for class II malocclusion in growing populations. However, using these therapeutic methods increases serious concerns about patient compliance. Fixed functional appliances [FFAs] are an effective treatment option for Class II malocclusion in post-adolescent patients whose growth has mostly finished [
8]. A functional orthodontic treatment consists of repositioning the mandible to generate force through the contraction of the corresponding muscles; this force is subsequently transmitted to the teeth, skeletal system, and temporomandibular joint [TMJ] [
9]. Thus, it is important to assess the TMJ modifications brought on by functional orthodontic treatment [
10]. Magnetic resonance imaging [MRI] is the preferred modality for assessing the soft tissue anatomical structures within the TMJ, particularly in determining the disk's position and shape [
11].
Numerous research has been conducted on the changes in the skeletal, dental, and condyles after class II correction [
12,
13,
14,
15,
16]. Few studies compared the various available tools for class II treatment and their impact on the articular disc. This study aimed to assess and compare the positional and dimensions changes in the Temporomandibular Joint disc resulting from various class II correctors before and after correcting the class II molar relation using MRI.
Study design
A prospective parallel randomized clinical trial was conducted.
Study Setting
A total of 39 patients, 14 boys, and 25 girls, between the ages of 15 and 23 who had mandibular retrognathism and angle Class II division 1 malocclusion were chosen sequentially for treatment.
Inclusion criteria were patients with clinical manifestation of a retrognathic mandible, as determined by cephalometric study, with an ANB angle larger than 4֯, due to the retrognathic mandible [SNB angle < 78◦], Permanent dentition with angle Class II division 1 malocclusion with no missing or history of extraction. Patients without history of TMJ dislocation or pain. No history of orthodontic treatment. Complete treatment records [cephalometric and panoramic X-ray, photography, and digital study models]. Absence of transverse pre-treatment discrepancy. Non-extraction treatment strategy and Class I occlusal relationship following treatment. Cervical vertebrae maturation stages 4,5, and/or 6 in healthy pro-pubertal patients [
17]. Patients having a history of trauma or TMJ operations, severe TMDs, systemic issues such as pregnancy, former orthodontic treatment, claustrophobia, or dental appliances or restorations that could have compromised patient safety during an MRI scan were not included in the study.
Sample size calculation:
The calculation of the sample size was performed utilizing the power analysis assessment tool G*power, version 3.1.9.7 [Franz Faul Universität, Kiel, Germany]. Considering an effect size of 0.649 and a significance level of 0.05, an 80% statistical power could be generated to identify significant differences with a sample size of 39 patients divided into three groups [
18].
Groups randomization
The study participants were randomly assigned to different groups using an online randomization strategy developed by online software available on the website.
https://www.graphpad.com/quickcalcs/. The allocation ratio was determined as 1:1:1. The researchers involved in the study were unaware of the group assignment. Following the initial clinical and radiological assessment, the patients were allocated into three groups of 13 individuals each: Power scope 2[American Orthodontics], SARA-Sabagh Advanced Repositioning Appliance [Forestadent, Germany],
CS-
2000® Niti spring class II corrector [Dyna flex]. The study was authorized by the Local Research Ethics Committee of Hawler Medical University (HMU D.22). Every participant who is a part of this research has provided written informed consent that details every stage of treatment.
Starting fixed orthodontic treatment
All patients were treated with MBT 0.022̎ bracket [Dentaurum GmbH & Co. KG, discovery] collected from private orthodontic practices in Erbil city. After initial leveling and alignment, and one month after the insertion of the 0.019”x 0.025” Niti archwire, patients were sent to take an MRI of the TMJs. The duration of fixed functional appliance treatment was about 5-7 months.
MRI evaluation
Magnetic resonance imaging [MRI] scans of the right and left temporomandibular joints [TMJs] were conducted at two specific time intervals during treatment: immediately before the placement of the fixed functional device [T1], and after attaining class I molar relation [T2]. The MRIs were performed with the mandible closed [MC] and opened [MO] at the Erbil International Hospital using a 3.0 T Magnetom Trio [Siemens Medical, Germany] with a 32-channel head coil. T Turbo spin echo T2-weighted coronal images [repetition time, 5400 ms; echo time, 71 ms; flip angle: 90֯; slice thickness, 3 mm; interslice gap, 1 mm; field of view [FoV], 200; regional FoV, 64] as closed mouth, and parasagittal proton density spin-echo images [repetition time, 2850 ms; echo time, 66 ms; flip angle, 90; slice thickness, 3 mm; interslice gap, 0.3 mm; m; FoV, 150; regional FoV, 90] with the mouth closed and open were obtained. The images were measured twice by a general radiologist [10 years of experience] who was blinded to the patient’s clinical condition. The observer repeated the trial 15 days apart to measure intra-observer variability. The statistical analysis includes all measurement mean values. All the measurements were done using Radiant DICOM viewer 2023.1 software and those sections were chosen that displayed the maximum width of the condyle and disc.
Statistical Analysis
The data was organized and presented in a tabular format using Microsoft Excel. GraphPad Prism 10.2.2.397 Windows was utilized for data analysis. The explanatory and outcome factors were analyzed using descriptive statistics, specifically the mean and standard deviation for quantitative data, and frequency and percentage for qualitative variables.
To evaluate the data for normality, the Shapiro-Wilk test was employed. Using a paired t-test, the means of numerous parameters at baseline and after the intervention were compared. By utilizing one-way ANOVA, the means of the three groups were compared. A p-value of less than 0.05 was deemed statistically significant for all two-tailed analyses. The assessment of intra-examiner reliability was conducted by calculating the intraclass correlation coefficient [ICC] and 95% confidence intervals at a significance level of 5% [p ≤ 0.050]. When the degree of agreement between measures was less than 5° and 95% of the subjects' measures fell within the upper and lower limits of agreement, then the measures were considered to agree.
Results
The current study shows that group DF has a significant effect on the forward position of condyle and retrusion of the disc, increased posterior joint space, and decreased disc length in the closed-mouth technique and a decrease in the disc length and increased width of the disc in the open-mouth technique [
Table 1 and
Table 2]. In the closed mouth technique, the number of non-biconcave discs was 10 on the right side before treatment while one patient had improved the shape of the disc. While on the left side, 8 patients had no biconcave form which decreased to 7 after treatment. In the open mouth technique, the number of discs was non-biconcave was 8 on the right side before treatment while three patients have improved the shape of the disc. While on the left side, 10 patients had no biconcave form which decreased to 7 after treatment. 23 % of joints were interiorly displaced before treatment and remained in the same position after FFA treatment.
In the PS group, a significant difference was observed in the superior joint space on the closed-mouth technique [
Table 3 and
Table 4]. In the closed mouth technique, the number of non-biconcave discs was 10 on the right side before treatment while three patients improved the shape of the disc. While on the left side, 8 patients had no biconcave form which decreased to 6 after treatment. In the open mouth technique, the number of non-biconcave discs was 7 on the right side before treatment while two patients improved the shape of the disc. While on the left side, 9 patients had no biconcave form which decreased to 6 after treatment. 15 % of joints were interiorly displaced before treatment and remained in the same position after FFA treatment.
In the SARA group, retrusion of the articular disc with protrusion of condyle has shown significant differences in the closed-mouth technique [
Table 5 and
Table 6]. In the closed mouth technique, the number of non-biconcave discs was 8 on the right and left side before treatment while two patients improved the shape of the disc. In the open mouth technique, the number of discs was non-biconcave was 6 on the right side before treatment while two patients improved the shape of the disc. While on the left side 6 patients have no biconcave form which decreased to 4 after treatment. 23 % of joints were interiorly displaced before treatment and decreased to 15% after FFA treatment. When comparing between groups, there were statistically significant differences in CPI, among all groups in closed mouth technique right side, noticeably between DF and PS, and DF and SARA. Also Disc length has been significantly was changed when comparing PS with SARA and DF with SARA.
Table 5.
Comparison of effect of disc and condyle change in group SARA [Open mouth technique].
Table 5.
Comparison of effect of disc and condyle change in group SARA [Open mouth technique].
| Left side |
Right Side |
| Variables |
Mean± SEM |
Mean± SEM |
| Before |
After |
Mean Difference |
p-value |
Before |
After |
Mean Difference |
p-value |
| DL |
7.61±0.43 |
7.57±0.74 |
-0.03±0.48 |
0.94 |
7.71±0.61 |
7.46±0.78 |
-0.24±0.27 |
0.39 |
| DW |
1.22±0.1 |
1.32±0.08 |
0.09±0.13 |
0.50 |
1.26±0.12 |
1.38±0.13 |
0.12±0.07 |
0.15 |
Table 6.
Comparison of effect of disc and condyle change in group SARA (closed mouth technique).
Table 6.
Comparison of effect of disc and condyle change in group SARA (closed mouth technique).
| Right side |
left side |
| Variables |
Mean±SEM |
p-value |
|
| Before |
After |
Mean Difference |
Before |
After |
Mean Difference |
p-value |
| PJS |
1.97±0.39 |
2.11±0.23 |
0.13±0.28 |
0.65 |
1.78±0.46 |
1.84±0.11 |
0.05±0.45 |
0.90 |
| SJS |
2.14±0.24 |
2.32±0.37 |
0.18±0.13 |
0.22 |
2.08±0.26 |
2.11±0.24 |
0.02±0.14 |
0.85 |
| AJS |
2.13±0.30 |
1.85±0.28 |
-0.27±0.16 |
0.14 |
1.88±0.20 |
1.53±0.17 |
-0.35±0.23 |
0.18 |
| CPI |
4.89±4.59 |
11.26±6.20 |
6.36±2.49 |
0.04* |
-6.86±10.06 |
10.08±5.87 |
16.94±4.98 |
0.019* |
| DL |
9.58±0.47 |
9.35±0.56 |
-0.22±0.49 |
0.66 |
8.83±0.77 |
8.19±0.77 |
-0.64±0.34 |
0.11 |
| PDA |
22.08±8.83 |
14.6±9.39 |
-7.47±2.83 |
0.04* |
7.46±4.86 |
1.1±4.81 |
-6.36±1.92 |
0.021* |
| DW |
1.38±0.11 |
1.64±0.16 |
0.25±0.17 |
0.19 |
1.25±0.21 |
1.55±0.24 |
0.29±0.17 |
0.15 |
Table 7.
Intergroup comparison of Tmj changes (T2-T1) of groups in the left side of the Closed mouth technique.
Table 7.
Intergroup comparison of Tmj changes (T2-T1) of groups in the left side of the Closed mouth technique.
| Variables |
Mean difference ±SD |
p-value (One way ANOVA) |
| G1 |
G2 |
G3 |
| PJS |
0.54±0.64 |
0.14±0.41 |
0.05±1.10 |
0.36 |
| SJS |
0.08±0.80 |
0.40±1.29 |
0.02±0.34 |
0.69 |
| AJS |
-0.14±0.39 |
-0.16±0.33 |
-0.35±0.56 |
0.0804 |
| CPI |
19.8±16.77 |
1.5±18 |
16.94±12.2 |
0.06 |
| DL |
-0.66±0.42 |
-0.56±1.25 |
-0.64±0.29 |
0.96 |
| PDA |
-2.84±9.32 |
-2.94±3.1 |
-6.368±4.72 |
0.24 |
| DW |
-0.08±0.29 |
-0.08±0.45 |
-0.29±0.43 |
0.20 |
Table 8.
Intergroup comparison of Tmj changes (T2-T1) of each two groups in the left side of the Closed mouth technique.
Table 8.
Intergroup comparison of Tmj changes (T2-T1) of each two groups in the left side of the Closed mouth technique.
| Variables |
Mean difference ±SD |
p-value |
| G1 |
G2 |
G3 |
G1 vs G2 |
G1 vs G3 |
G2 vs G3 |
| PJS |
0.54±0.64 |
0.14±0.41 |
0.05±1.10 |
0.4779 |
0.41 |
0.97 |
| SJS |
0.08±0.80 |
0.40±1.29 |
0.02±0.34 |
0.7573 |
0.99 |
0.73 |
| AJS |
-0.14±0.39 |
-0.16±0.33 |
-0.35±0.56 |
0.2876 |
0.6298 |
0.0755 |
| CPI |
19.8±16.77 |
1.5±18 |
16.94±12.2 |
0.0665 |
0.94 |
0.19 |
| DL |
-0.66±0.42 |
-0.56±1.25 |
-0.64±0.29 |
0.817 |
0.97 |
0.87 |
| PDA |
-2.84±9.32 |
-2.94±3.1 |
-6.368±4.72 |
0.84 |
0.47 |
0.42 |
| DW |
-0.08±0.29 |
-0.08±0.45 |
-0.29±0.43 |
0.64 |
0.56 |
0.17 |
Table 9.
Intergroup comparison of Tmj changes (T2-T1) of all groups in the right side of the Closed mouth technique.
Table 9.
Intergroup comparison of Tmj changes (T2-T1) of all groups in the right side of the Closed mouth technique.
| Variables |
Mean± SD |
p-value |
| G1 |
G2 |
G3 |
| PJS |
0.3±0.07 |
0.021±0.05 |
0.13±0.28 |
0.31 |
| SJS |
0.03±0.17 |
0.12±0.08 |
0.18±0.13 |
0.15 |
| AJS |
-0.25±0.15 |
-0.02±0.16 |
-0.27.14 |
0.36 |
| CPI |
26.86±13.59 |
0.70±7.31 |
6.36±2.49 |
0.01* |
| DL |
-0.56±0.24 |
-0.63±0.33 |
-0.22±0.49 |
0.67 |
| PDA |
-2.78±5.02 |
-2.73±3.11 |
-7.47±2.83 |
0.32 |
| DW |
0.09±0.11 |
0.04±0.09 |
0.25±0.17 |
0.68 |
Table 10.
Intergroup comparison of Tmj changes (T2-T1) of each two groups in the right side of the Closed mouth technique.
Table 10.
Intergroup comparison of Tmj changes (T2-T1) of each two groups in the right side of the Closed mouth technique.
| Variables |
Mean± SD |
p-value |
| G1 |
G2 |
G3 |
G1 vs G2 |
G1 vs G3 |
G2 vs G3 |
| PJS |
0.3±0.07 |
0.021±0.05 |
0.13±0.28 |
0.1855 |
0.6771 |
0.7168 |
| SJS |
0.03±0.17 |
0.12±0.08 |
0.18±0.13 |
0.3836 |
0.7362 |
0.147 |
| AJS |
-0.25±0.15 |
-0.02±0.16 |
-0.27.14 |
0.4323 |
0.9948 |
0.452 |
| CPI |
26.86±13.59 |
0.70±7.31 |
6.36±2.49 |
0.015* |
0.038* |
0.0926 |
| DL |
-0.56±0.24 |
-0.63±0.33 |
-0.22±0.49 |
0.85 |
0.45 |
0.49 |
| PDA |
-2.78±5.02 |
-2.73±3.11 |
-7.47±2.83 |
0.5783 |
0.319 |
0.8329 |
| DW |
0.09±0.11 |
0.04±0.09 |
0.25±0.17 |
0.9953 |
0.696 |
0.7452 |
Table 11.
Intergroup comparison of Tmj changes [T2-T1] of all groups on left side of open mouth technique.
Table 11.
Intergroup comparison of Tmj changes [T2-T1] of all groups on left side of open mouth technique.
| Variables |
Mean± SD |
p-value |
| G1 |
G2 |
G3 |
| DL |
-1.03±0.19 |
-0.1±0.39 |
-0.03±0.48 |
0.10 |
| DW |
0.09±0.16 |
-0.02±0.19 |
-0.09±0.13 |
0.747 |
Table 12.
Intergroup comparison of Tmj changes [T2-T1] of each two groups in left side of open mouth technique.
Table 12.
Intergroup comparison of Tmj changes [T2-T1] of each two groups in left side of open mouth technique.
| Variables |
Mean± SD |
p-value |
p-value |
| G1 |
G2 |
G3 |
G1 vs G2 |
G1 vs G3 |
G2 vs G3 |
| DL |
-1.03±0.19 |
-0.1±0.39 |
-0.03±0.48 |
0.10 |
0.058 |
0.12 |
0.88 |
| DW |
0.09±0.16 |
-0.02±0.19 |
-0.09±0.13 |
0.747 |
0.861 |
0.744 |
0.960 |
Table 13.
Intergroup comparison of Tmj changes [T2-T1] of all groups on the right side of the open-mouth technique.
Table 13.
Intergroup comparison of Tmj changes [T2-T1] of all groups on the right side of the open-mouth technique.
| Variables |
Mean± SD |
p-value |
| G1 |
G2 |
G3 |
|
| DL |
-1.52±0.16 |
-0.88±0.49 |
-0.24±0.27 |
0.56 |
| DW |
-0.03±0.11 |
0.03±0.11 |
-0.12±0.07 |
0.080 |
Table 14.
Intergroup comparison of Tmj changes [T2-T1] of each two groups on the right side of the open open-mouth technique.
Table 14.
Intergroup comparison of Tmj changes [T2-T1] of each two groups on the right side of the open open-mouth technique.
| Variables |
Mean± SD |
p-value |
| G1 |
G2 |
G3 |
G1 vs G2 |
G1 vs G3 |
G2 vs G3 |
| DL |
-1.52±0.16 |
-0.88±0.49 |
-0.24±0.27 |
0.76 |
0.04* |
0.02* |
| DW |
-0.03±0.11 |
0.03±0.11 |
-0.12±0.07 |
0.065 |
0.601 |
0.489 |
Discussion
The present study was done to evaluate the dimensional and positional changes in the articular discs with different class II correctors by using Magnetic Resonance Imaging.
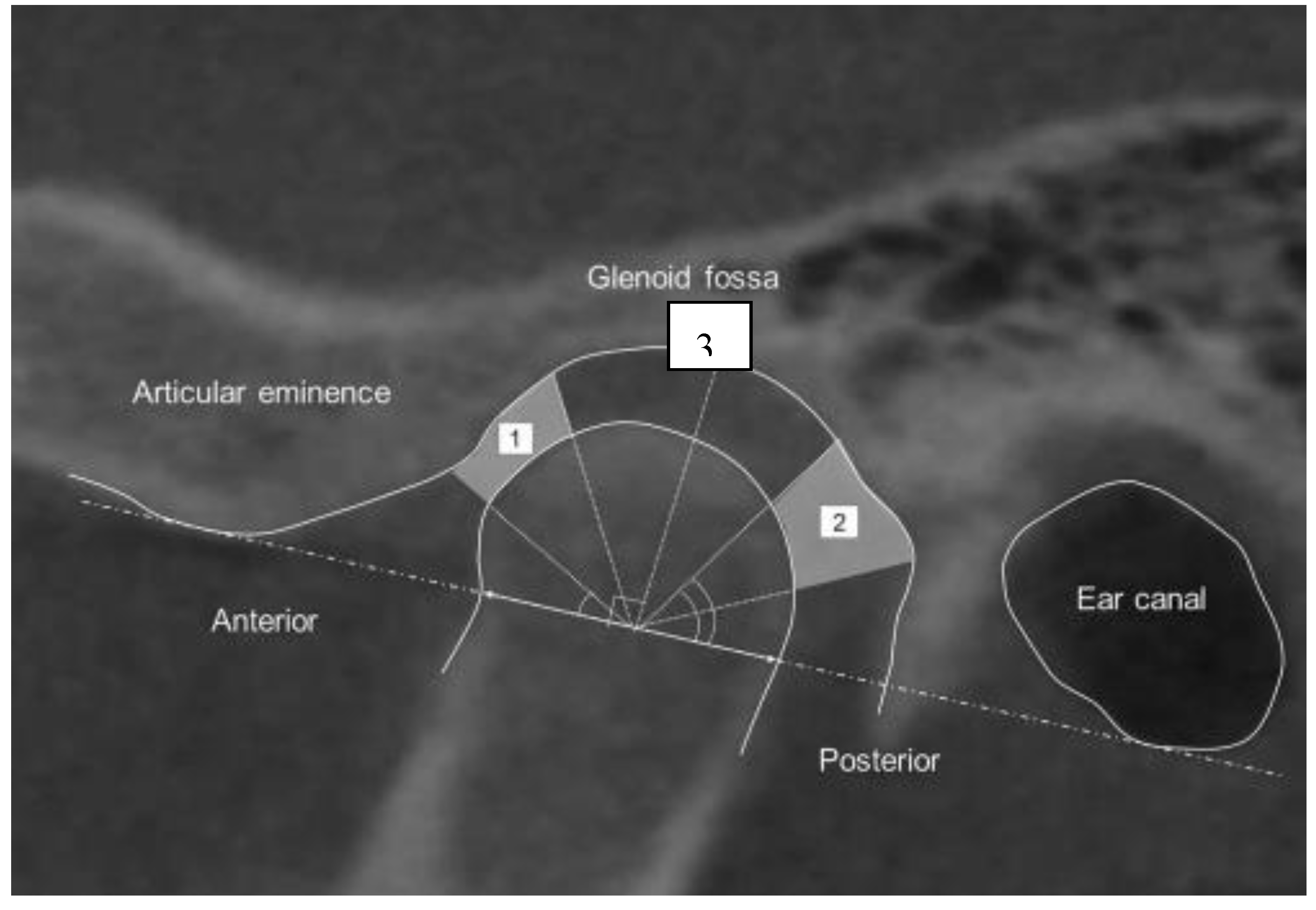
Assessment of Condylar Position [Condylar Concentricity] and Joint Spaces
According to Vargas-Pereira's proposal, the anterior joint space [AJS] is the shortest path connecting the eminence and the head of the condyle. Similarly, the posterior joint space [PJS] is defined as the smallest distance between the condylar head and the post-glenoidal fossa [
19] [
Figure 1]. After measuring the AJS and PJS, the resulting values were inputted into the following formula: JSI= [[P – A]/ [P + A]]x100, where A is the AJS, P is the PJS, and JSI is the joint space index. The physiologic limit for the condylar position ranged from –32.5% to 21.1%. The condyle's anterior position relative to the glenoid fossa is represented by a positive number, whereas a negative value suggests a posterior location of the condyle. A value of zero is referred to as concentric [
20].
In the current study, results show all groups have a protrusive effect on condyle in both the right and left sides. Among study groups, the SARA and DF appliances showed significant anterior positioning of the condyle on both sides. There was no significant difference between all groups and between each two groups. A study revealed that 75% of the patients exhibited a more anterior condyle position following treatment compared to the control group. Additionally, the condyle displayed varying degrees of forward movement about the articular fossa [
20]. In the present study, it was 78% in DF, 67% in PS, and SARA 84% found forward positioning of the condyle. The result of the current study is compatible with studies done by [
14,
19,
21,
22,
23,
24]
. According to Parvathy's study, the utilization of a functional appliance in the mandibular advancement method led to the stimulation of condylar growth in a posterior direction and remodeling of the glenoid fossa. Consequently, this process resulted in the anterior movement of the condyle to the skull [
14]. According to research, the condyle exhibited a notable increase in anterior positioning in the MRIs obtained immediately after treatment. However, after a period of one year, the condyle had reverted to its initial position. The potential cause for the return to the initial position may be attributed to the displacement of the condyle within the fossa or the successful completion of the condyle-fossa remodeling process [
25,
26].
Several investigations have reported that there are no notable alterations in the location of the condyles inside the TMJ space after therapy [
20,
25,
27,
28,
29]. They used different methods for the treatment of class II malocclusion. Nindra et al. discovered that adaptive restoration of the condyle and articular fossa occurred following functional orthodontic therapy, but their relative positions did not alter [
30].
Arici et al and Zhang et al, in their studies, have found more posterior movement of the condyle. They used different methods of analysis and removable types of functional appliances [
10,
31].
Joint spaces
Results of the current study revealed that posterior joint space has increased while anterior joint space was decreased in all study groups but only was significant in group DF. Also, SJS has been increased which indicates forward and downward movement of the condyle. The same result was found in studies done by Elfeky et al. [
23], On the other hand, Cacho et al and Kinzinger et al studying the Herbst appliance and functional mandibular advancer, respectively, found no significant changes in the joint space [
27,
32].
Disc morphology.
T2 oblique sagittal images were evaluated and classed for disc morphology using mouth close and mouth open. Based on band abnormalities, Ribeiro classified the disc as non-biconcave [abnormal morphology] or biconcave [
34]. The internal derangements of the temporomandibular joints [TMJs] are influenced by changes in the morphology of the disc, in addition to its position [
35]. The disc's morphology and interarticular pressure determine its translation with the condyle. Indeed, disc shape is crucial for maintaining the correct location throughout the function [
36]. In the present study around 85% of discs remain stable in morphology. Aidar et al in their study found that 93.75% of subjects have no alterations to disc morphology which is comparable with the current result [
37].
In 6 joints, disc morphology was improved to biconcave form with the mouth closed while in the mouth open, 8 joints were modified to biconcave. Franco et al. found that Frankel II functional regulators improved disc shape in treated subjects [
38].
Disc Length
In a study conducted by Shen et al, it was shown that the utilization of the anterior repositioning appliance resulted in an increase in disc length within the anterior disk displacement with reduction [ADDwR] group, but it led to a decrease in the anterior disk displacement without reduction [ADDwoR] group. This may be because the disc was extruded when anteriorly displaced and worsened after moving the mandible forward in the ADDWoR group. Conversely, the disk returned to its original length upon repositioning in the ADDWR group [
39].
Zhang et al conducted a study that found a significant relationship between the displacement distance and quantitative parameters such as disc length, width, and L/W. The disks demonstrated reduced lengths, increased widths, and decreased L/W as the displacement distance increased [
9].
Sagittal disc position
Silverstein et al. reported a normal range of 25.7° to −18.7°, while Vargas-Pereira reported 33° to −21° [
40,
41]. Displaced disks had the thickest posterior band previous or posterior to this point. The posterior band was used to determine the disc limit, maybe because the posterior ligament has more fat and water than the darker disc tissue and is easier to identify [
42].
In the present study, pretreatment MRIs in all three groups showed nine cases of anterior disk displacement [three DF, four PS, two SARA] whereas the remaining patients were within the normal range. In comparison between pre- and post-functional treatment, disk position showed non-significant posterior movement from its initial pretreatment position among all groups but was within the physiologic range. These findings were in accordance with the Ruf and Pancherz study [
25]. Also [Chintakanon et al, Arat
et al; Kinzinger
et al ; Wadhawan
et al] showed no statistically significant changes in disk position [
20,
26,
32,
43].
Pretreatment disc displacement determines repositioning prognosis. A partially displaced disc can be repositioned and remain stable until final inspection [
25].
On the other hand, the current result was contrary to those of Foucart et al who reported that 3 of 10 previously healthy patients who used the Herbst appliance developed disc displacement after treatment. Those authors evaluated results from removable appliances, rather than those from a fixed functional appliance as in the present study [
44]. They also used sagittal MRI and in the current study, oblique sagittal images [parasagittal] were used.
The biomechanism of the temporomandibular joints [TMJs] is influenced by several parameters, including condyle shape, articular fossa, and articular tubercle. Additionally, an abnormally large eminence may also act as a contributing factor in the development of disc displacement [
45,
46].
Aidar et al suggest that an increased overjet may be a reason leading to disk displacement [
47]. According to Patti, increasing overbite keeps the mandible and condyles in a retrieve position and may promote articular disc anterior displacement [
48]. One of limitation of the current study was small sample size, However, the results are readily apparent and hold considerable importance. It is recommended that future investigations with a larger sample size validate these findings. Lack of control group in the study can be regarded as another limitation that has not been enrolled due to ethical consideration. Future research on functional appliances should prioritize the examination of glenoid fossa and temporomandibular joint remodeling, with a particular focus on the positional alteration of the glenoid fossa. The study also emphasizes the necessity of establishing accurate techniques for assessing the magnetic resonance imaging (MRI) of the temporomandibular joint (TMJ).
Conclusion
Class II malocclusions can be effectively corrected by fixed functional appliances. The results of the study suggested that the forward condylar position within the glenoid fossa and articular disc retrusion with respect to the condylar head was statistically significant after fixed functional therapy. This study showed that arthroscopic disc repositioning significantly increases the widths of posterior and superior spaces of the joint, pushing the condyle downward and forward. The statistical significance of the position of the condyle in the glenoid fossa and the retrusion of the articular disc with respect to the condylar head was observed. The mechanism of action of functional appliances appears to include the forward migration of the C-GF complex.
References
- Sivakumar, A.; et al. A comparison of craniofacial characteristics between two different adult populations with class II malocclusion—a cross-sectional retrospective study. Biology 2021, 10, 438. [Google Scholar] [CrossRef] [PubMed]
- Booij, J.W.; et al. Treatment outcome of class II malocclusion therapy including extraction of maxillary first molars: a cephalometric comparison between normodivergent and hyperdivergent facial types. PeerJ 2022, 10, e14537. [Google Scholar] [PubMed]
- Bakhurji, E.A.; et al. Prevalence and distribution of nonsyndromic dental anomalies in children in eastern Saudi Arabia: A radiographic study. The Scientific World Journal 2021, 2021, 1–6. [Google Scholar]
- Cançado, R.H.; et al. Treatment effects of the Herbst appliance in class II malocclusion patients after the growth peak. European Journal of Dentistry 2021, 15, 39–46. [Google Scholar]
- Fouad, A.M.; Abu-Shahba, R.Y.; Barakat, E. Soft Tissue Evaluation of Mandibular Protraction Appliance IV and PowerScope in Treatment of Class II Malocclusion; A Comparative Randomized Clinical Trial. International Journal Dental and Medical Sciences Research 2023, 5, 153–161. [Google Scholar]
- Kalra, A.; Swami, V.; Bhosale, V. Treatment effects of “PowerScope” fixed functional appliance–a clinical study. Folia Medica 2021, 63, 253–263. [Google Scholar] [PubMed]
- Al Hamdany, A.K.; et al. PowerScope 2 functional appliance: A 3D finite element simulation of its action on the mandible. Journal of Oral Biology and Craniofacial Research 2023, 13, 299–305. [Google Scholar] [PubMed]
- Mathur, S.; Raghav, P. Advansync 2: A fixed functional class 2 corrector in advanced age, A case report. Heal Talk A Journal Of Clinical Dentistry. 2019, 11, 34–35. [Google Scholar]
- Zhang, Y.; et al. Clinical finite element analysis of mandibular displacement model treated with Twin-block appliance. American Journal of Orthodontics and Dentofacial Orthopedics 2023, 164, 395–405. [Google Scholar]
- Zhang, Y.; et al. Three-dimensional spatial analysis of temporomandibular joint in adolescent Class II division 1 malocclusion patients: comparison of Twin-Block and clear functional aligner. Head & Face Medicine 2024, 20, 4. [Google Scholar]
- López-Arcas, J.M.; et al. Magnetic Resonance Imaging of the Temporomandibular Joint: Key Point in the Election of Treatment. Atlas of the Oral and Maxillofacial Surgery Clinics of North America 2022, 30, 129–135. [Google Scholar]
- Dixit, S.; Sridhar, K.; Jain, U.; Prakash, A.; Ekka, S. Evaluation of Temporomandibular Joint Changes with Functional Appliance—An MRI Study. J Contemp Orthod. J Contemp Orthod 2018, 2, 7–13. [Google Scholar]
- Deshmukh, S.; et al. Evaluation of Changes in Condylar Cartilage Thickness Using MRI and Ultrasound Imaging in Patients Treated by Mandibular Advancement with Myofunctional Appliance: An In-Vivo Pilot Study. Cureus 2021, 13. [Google Scholar]
- Parvathy, R.M.; Shetty, S.; Katheesa, P. Evaluation of changes seen in TMJ after mandibular advancement in treatment of Class II malocclusions, with functional appliances, a CBCT study. Biomedicine 2021, 41, 236–242. [Google Scholar]
- Patel, B.; et al. Evaluation of Changes in Soft and Hard Tissues of TMJ among Class II Division 2 Patients after Prefunctional Orthodontics and Twin Block Functional Appliance Therapy: A Prospective MRI Study. International Journal of Clinical Pediatric Dentistry 2022, 15, 479. [Google Scholar]
- Singh1, S.; et al. MORPHOLOGICAL CONDYLAR CHANGES FOLLOWING FIXED FUNCTIONAL APPLIANCE THERAPY. Eur. Chem. Bull. 2023, 12, 2141–2149. [Google Scholar]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. [2005] ‘The cervical vertebral maturation [CVM] method for the assessment of optimal treatment timing in dentofacial orthopedics’, in Seminars in Orthodontics. Elsevier, pp. 119–129.
- Kaushik, K.; et al. Comparative Three Dimensional Evaluation of Dentoskeletal Parameters using AdvanSync & Herbst Appliance in Class II Malocclusion:“A Randomized Controlled Trial”. World 2022, 13, 229. [Google Scholar] [CrossRef]
- Chavan, S.J.; Bhad, W.A.; Doshi, U.H. Comparison of temporomandibular joint changes in Twin Block and Bionator appliance therapy: a magnetic resonance imaging study. Progress in orthodontics 2014, 15, 1–7. [Google Scholar]
- Chintakanon, K.; et al. A prospective study of Twin-block appliance therapy assessed by magnetic resonance imaging. American journal of orthodontics and dentofacial orthopedics 2000, 118, 494–504. [Google Scholar]
- Cheib, P.L.; et al. Displacement of the mandibular condyles immediately after Herbst appliance insertion-3D assessment. Turkish journal of orthodontics 2016, 29, 31. [Google Scholar]
- Benkherfallah, N.; et al. Sagittal position of the temporomandibular joint disc after treatment with an activator: an MRI study. Medical Technologies Journal 2017, 140–149. [Google Scholar]
- Elfeky, H.Y.; et al. Three-dimensional skeletal, dentoalveolar and temporomandibular joint changes produced by Twin Block functional appliance. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopadie 2018, 79. [Google Scholar]
- Jiang, Y.; et al. Three-dimensional cone beam computed tomography analysis of temporomandibular joint response to the Twin-block functional appliance. Korean Journal of Orthodontics 2020, 50, 86. [Google Scholar]
- Ruf, S.; Pancherz, H. Does bite-jumping damage the TMJ? A prospective longitudinal clinical and MRI study of Herbst patients. The Angle Orthodontist 2000, 70, 183–199. [Google Scholar]
- Wadhawan, N.; et al. Temporomandibular joint adaptations following two-phase therapy: an MRI study. Orthodontics & craniofacial research 2008, 11, 235–250. [Google Scholar]
- Cacho, A.; et al. Changes in joint space dimension after the correction of Class II division 1 malocclusion. European journal of orthodontics 2015, 37, 467–473. [Google Scholar]
- Cheib Vilefort, P.L.; et al. Condyle-glenoid fossa relationship after Herbst appliance treatment during two stages of craniofacial skeletal maturation: A retrospective study. Orthodontics & Craniofacial Research 2019, 22, 345–353. [Google Scholar]
- Guo, Y.; et al. CBCT analysis of changes in dental occlusion and temporomandibular joints before and after MEAW Orthotherapy in patients with nonlow angle of skeletal class III. BioMed Research International 2020. [Google Scholar]
- Nindra, J.; et al. Three-dimensional evaluation of condyle-glenoid fossa complex following treatment with Herbst appliance. Journal of Clinical Medicine 2021, 10, 4730. [Google Scholar]
- Arici, S.; et al. Effects of fixed functional appliance treatment on the temporomandibular joint. American journal of orthodontics and dentofacial orthopedics 2008, 133, 809–814. [Google Scholar]
- Kinzinger, G.; et al. Disc-condyle Relationships during Class II Treatment with the Functional Mandibular Advancer [FMA]. Journal of Orofacial Orthopedics= Fortschritte der Kieferorthopadie: Organ/official Journal Deutsche Gesellschaft fur Kieferorthopadie 2006, 67, 356–375. [Google Scholar]
- John, Z.A.S.; Shrivastav, S.S.; Kamble, R.; Jaiswal, E.; Dhande, R. Three-dimensional comparative evaluation of articular disc position and other temporomandibular joint morphology in Class II horizontal and vertical cases with Class I malocclusion. Angle Orthod. 2020, 90, 707–714. [Google Scholar]
- Ribeiro, R.; et al. TMJ structural evaluation by MRI in asymptomatic children and young adult volunteers. Journal of Dental Research 1995, 74, 223. [Google Scholar]
- Murakami, S.; et al. Magnetic resonance evaluation of the temporomandibular joint disc position and configuration. Dentomaxillofacial Radiology 1993, 22, 205–207. [Google Scholar]
- Okeson, J.P. [2000] ‘Anatomia funcional e a biomecaˆnica do sistema mastigato´rio’, in O. JP. [ed.] Tratamento das desordens temporomandibulares e oclusa˜o. 4th edn. Sa˜o Paulo, Brazil: Artes Me´dicas;, pp. 3–21.
- Aidar, L.A.; et al. Effects of Herbst appliance treatment on temporomandibular joint disc position and morphology: a prospective magnetic resonance imaging study. American journal of orthodontics and dentofacial orthopedics 2009, 136, 412–424. [Google Scholar]
- Franco, A.A.; et al. Fränkel appliance therapy and the temporomandibular disc: a prospective magnetic resonance imaging study. American journal of orthodontics and dentofacial orthopedics 2002, 121, 447–457. [Google Scholar]
- Shen, P.; et al. The effect evaluation of functional appliance used for class II patients with temporomandibular joint anterior disc displacement. Journal of Craniofacial Surgery 2019, 30, e15–e17. [Google Scholar]
- Silverstein, R.; et al. MRI assessment of the normal temporomandibular joint with the use of projective geometry. Oral surgery, oral medicine, oral pathology 1994, 77, 523–530. [Google Scholar]
- Pereira, M.R.V. [1997] Quantitative Auswertungen bildgebender Verfahren und Entwicklung einer neuen metrischen Analyse für Kiefergelenkstrukturen im Magnetresonanztomogramm.
- Katzberg, R.W.; et al. Magnetic resonance imaging of the temporomandibular joint meniscus. Oral surgery, oral medicine, oral pathology 1985, 59, 332–335. [Google Scholar]
- Arat, Z.M.; et al. Changes in the TMJ disc-condyle-fossa relationship following functional treatment of skeletal Class II Division 1 malocclusion: a magnetic resonance imaging study. American Journal of Orthodontics and Dentofacial Orthopedics 2001, 119, 316–19. [Google Scholar]
- Foucart, J.M.; et al. MRI study of temporomandibular joint disk behavior in chilren with hyperpropulsion appliances. L’Orthodontie Francaise 1998, 69, 79–91. [Google Scholar] [PubMed]
- Hall, M.B.; Gibbs, C.C.; Sclar, A.G. Association between the prominence of the articular eminence and displaced TMJ disks. CRANIO® 1985, 3, 237–239. [Google Scholar] [PubMed]
- Solberg, W.K.; Hansson, T.L.; Nordström, B. The temporomandibular joint in young adults at autopsy: a morphologic classification and evaluation. Journal of oral rehabilitation 1985, 12, 303–321. [Google Scholar]
- Aidar, L.A.A.; et al. Changes in temporomandibular joint disc position and form following Herbst and fixed orthodontic treatment. The Angle Orthodontist 2010, 80, 843–852. [Google Scholar] [PubMed]
- Patti [2010] : ‘Treatment of class II from prevention to surgery’, in Class II and TMJ. Int.Quintessence, pp. 409–446.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).