Submitted:
11 April 2024
Posted:
15 April 2024
You are already at the latest version
Abstract
Keywords:
Introduction
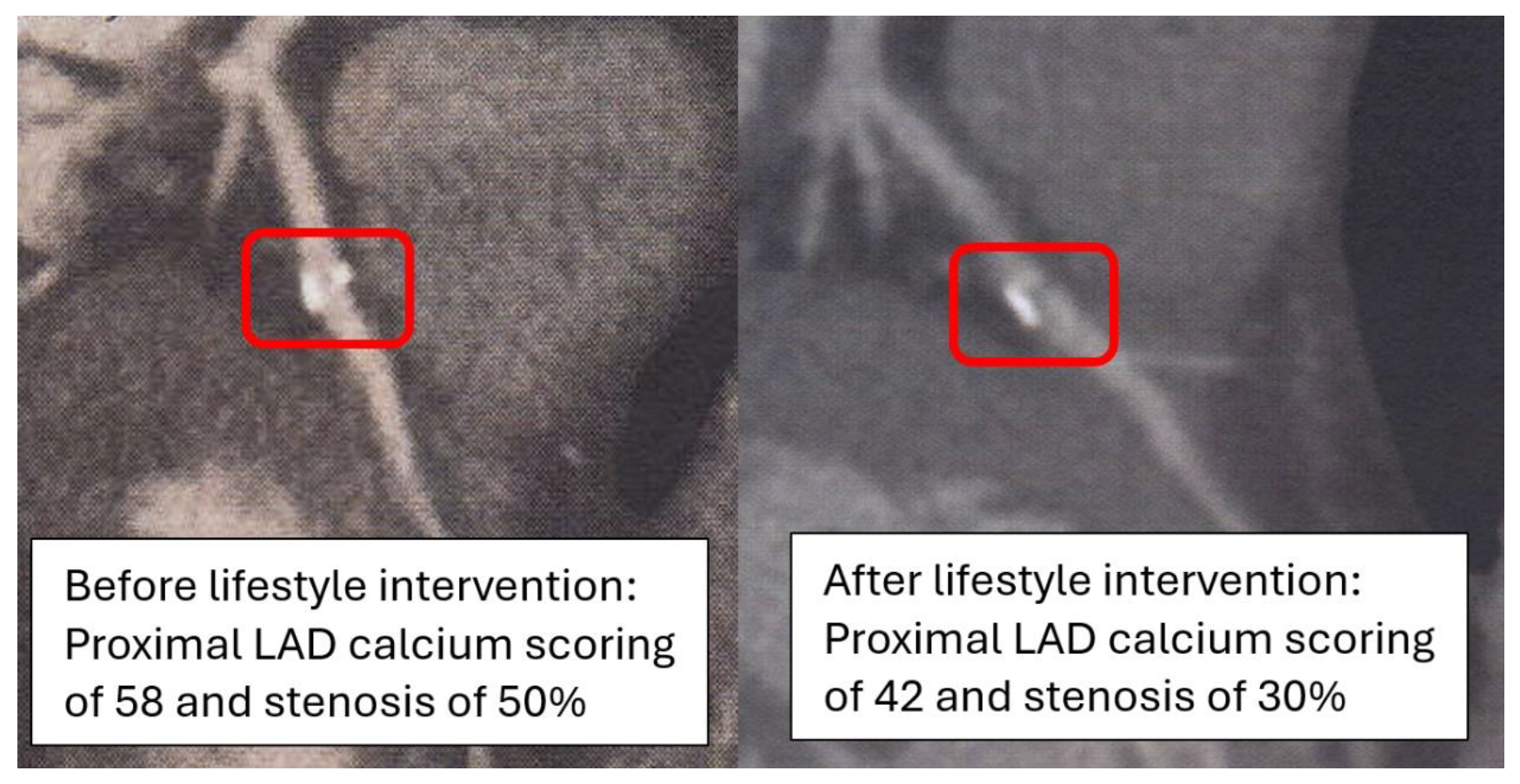
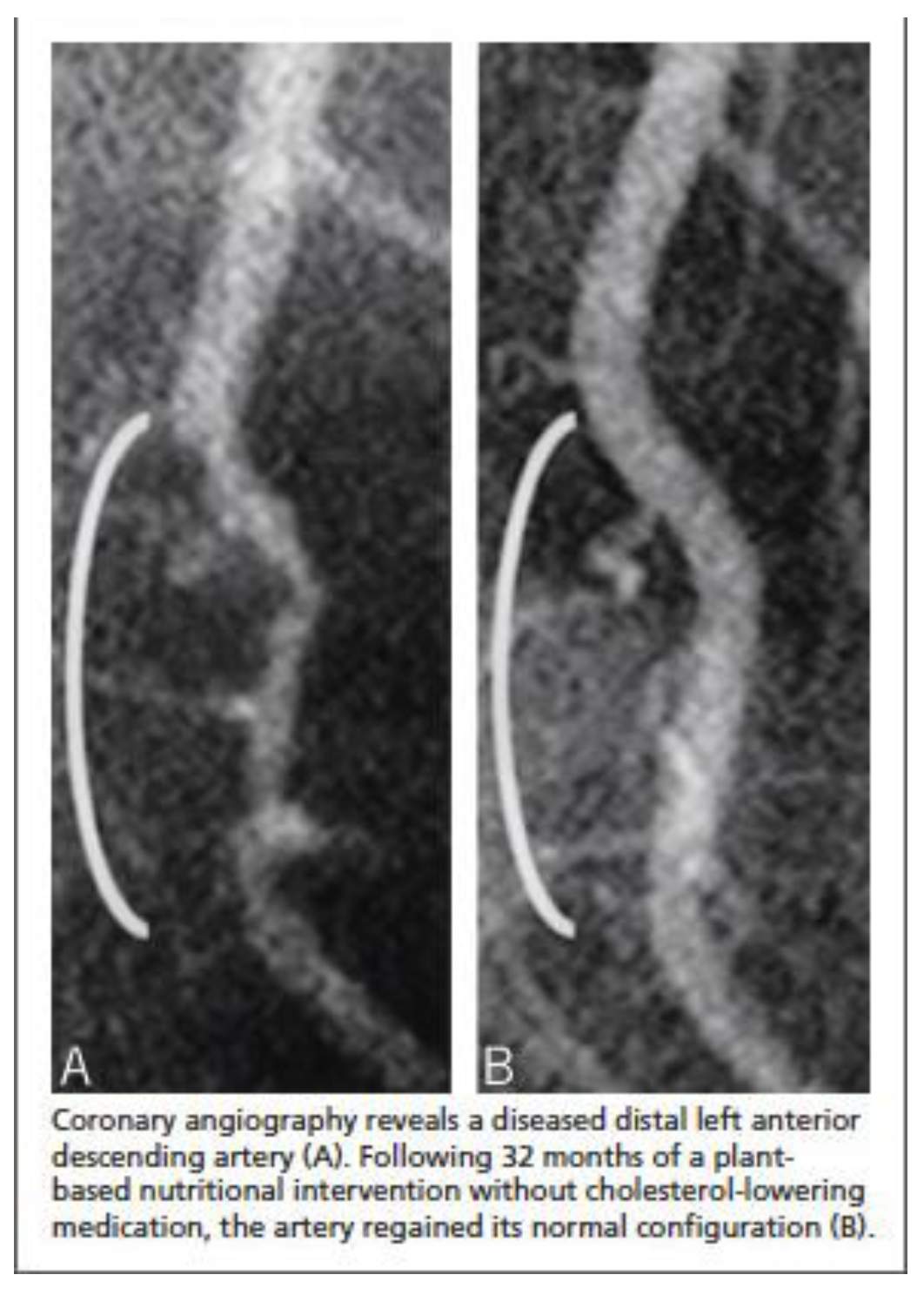
2. Case Description
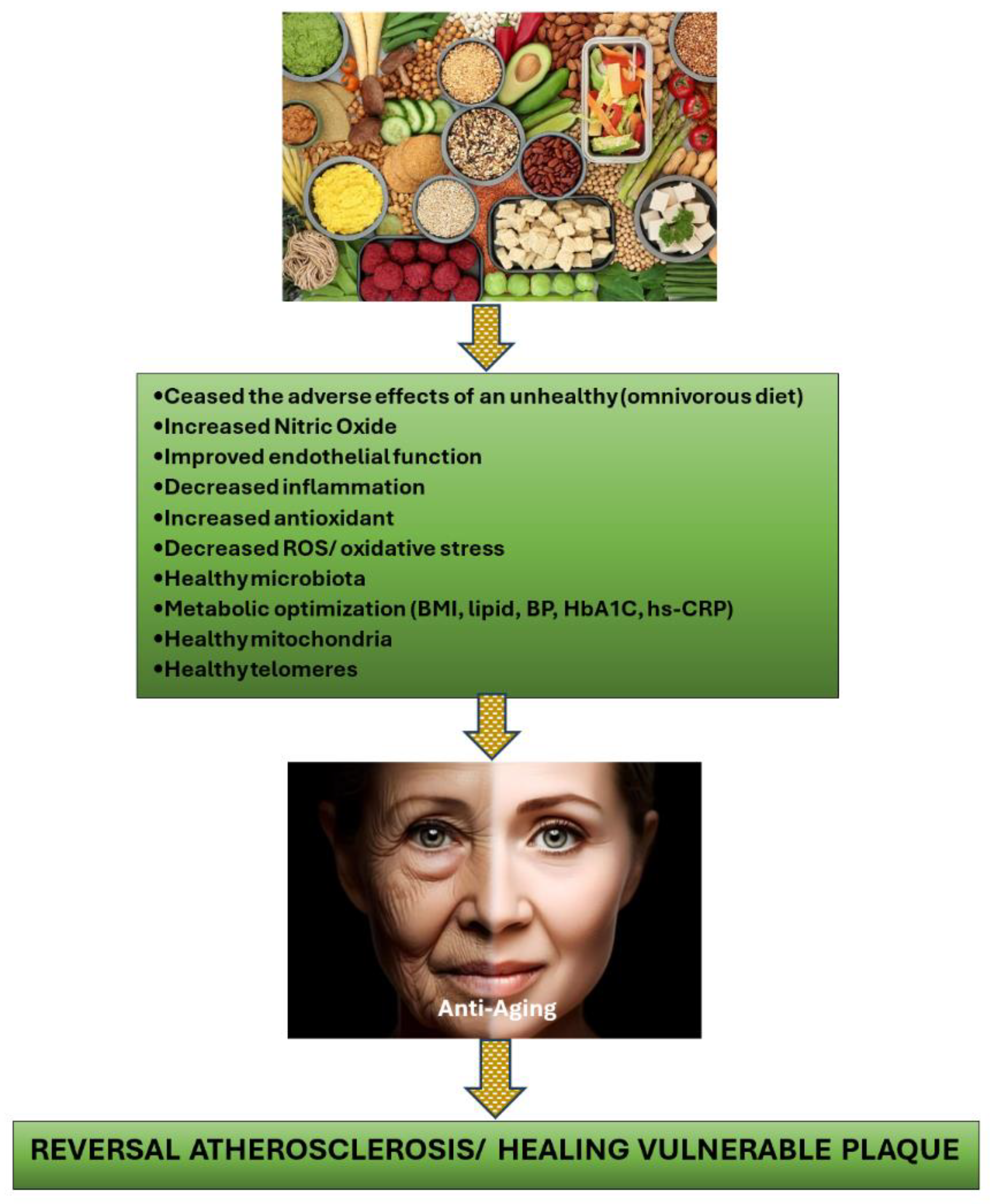
3. Discussion
4. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflict of Interest
References
- Ahmed, A.H.; Shankar, K.; Eftekhari, H.; Munir; Robertson, J.; Brewer, A.; Stupin, I.V.; Casscells, S.W. Silent myocardial ischemia: Current perspectives and future directions. 2007, 12, 189–96. [Google Scholar]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circ. 2021, 144, 916–929. [Google Scholar] [CrossRef]
- Boden, W.E.; O'Rourke, R.A.; Teo, K.K.; Hartigan, P.M.; Maron, D.J.; Kostuk, W.J.; Knudtson, M.; Dada, M.; Casperson, P.; Harris, C.L.; et al. Optimal Medical Therapy with or without PCI for Stable Coronary Disease. New Engl. J. Med. 2007, 356, 1503–1516. [Google Scholar] [CrossRef]
- Al-Lamee, R.; Thompson, D.; Dehbi, H.-M.; Sen, S.; Tang, K.; Davies, J.; Keeble, T.; Mielewczik, M.; Kaprielian, R.; Malik, I.S.; et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet 2017, 391, 31–40. [Google Scholar] [CrossRef]
- Maron, D.J.; Hochman, J.S.; Reynolds, H.R.; Bangalore, S.; O’Brien, S.M.; Boden, W.E.; Chaitman, B.R.; Senior, R.; López-Sendón, J.; Alexander, K.P.; et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N. Engl. J. Med. 2020, 382, 1395–1407. [Google Scholar] [CrossRef]
- Kurup, R.; Wijeysundera, H.C.; Bagur, R.; Ybarra, L.F. Complete Versus Incomplete Percutaneous Coronary Intervention-Mediated Revascularization in Patients With Chronic Coronary Syndromes. Cardiovasc. Revascularization Med. 2023, 47, 86–92. [Google Scholar] [CrossRef]
- Stone, G.W.; Ali, Z.A.; O’brien, S.M.; Rhodes, G.; Genereux, P.; Bangalore, S.; Mavromatis, K.; Horst, J.; Dressler, O.; Poh, K.K.; et al. Impact of Complete Revascularization in the ISCHEMIA Trial. J. Am. Coll. Cardiol. 2023, 82, 1175–1188. [Google Scholar] [CrossRef]
- Doenst, T.; Haverich, A.; Serruys, P.; Bonow, R.O.; Kappetein, P.; Falk, V.; Velazquez, E.; Diegeler, A.; Sigusch, H. PCI and CABG for Treating Stable Coronary Artery Disease. J. Am. Coll. Cardiol. 2019, 73, 964–976. [Google Scholar] [CrossRef]
- van Veelen, A.; van der Sangen, N.M.R.; Delewi, R.; Beijk, M.A.M.; Henriques, J.P.S.; Claessen, B.E.P.M. Detection of Vulnerable Coronary Plaques Using Invasive and Non-Invasive Imaging Modalities. J. Clin. Med. 2022, 11, 1361. [Google Scholar] [CrossRef]
- Tomaniak, M.; Katagiri, Y.; Modolo, R.; de Silva, R.; Khamis, R.Y.; Bourantas, C.V.; Torii, R.; Wentzel, J.J.; Gijsen, F.J.H.; van Soest, G.; et al. Vulnerable plaques and patients: state-of-the-art. Eur. Hear. J. 2020, 41, 2997–3004. [Google Scholar] [CrossRef]
- Virani, S.S.; Newby, L.K.; Arnold, S.V.; Bittner, V.; Brewer, L.C.; Demeter, S.H.; Dixon, D.L.; Fearon, W.F.; Hess, B.; Johnson, H.M.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023, 148, E9–E119, Epub 2023 Jul 20. Erratum in: Circulation. 2023 Sep 26;148(13):e148. Erratum in: Circulation. 2023 Dec 5;148(23):e186. PMID: 37471501. [Google Scholar] [CrossRef]
- Stone, G.W.; Maehara, A.; Ali, Z.A.; Held, C.; Matsumura, M.; Kjøller-Hansen, L.; Bøtker, H.E.; Maeng, M.; Engstrøm, T.; Wiseth, R.; et al. Percutaneous Coronary Intervention for Vulnerable Coronary Atherosclerotic Plaque. J. Am. Coll. Cardiol. 2020, 76, 2289–2301. [Google Scholar] [CrossRef]
- Park, S.-J.; Ahn, J.-M.; Kang, D.-Y.; Yun, S.-C.; Ahn, Y.-K.; Kim, W.-J.; Nam, C.-W.; Jeong, J.-O.; Chae, I.-H.; Shiomi, H.; et al. Preventive percutaneous coronary intervention versus optimal medical therapy alone for the treatment of vulnerable atherosclerotic coronary plaques (PREVENT): a multicentre, open-label, randomised controlled trial. . 2024. [Google Scholar] [CrossRef]
- van Veelen, A.; Küçük, I.T.; Fuentes, F.H.; Kahsay, Y.; Garcia-Garcia, H.M.; Delewi, R.; Beijk, M.A.M.; Hartog, A.W.D.; Grundeken, M.J.; Vis, M.M.; et al. First-in-Human Drug-Eluting Balloon Treatment of Vulnerable Lipid-Rich Plaques: Rationale and Design of the DEBuT-LRP Study. J. Clin. Med. 2023, 12, 5807. [Google Scholar] [CrossRef]
- Mortensen, M.B.; Dzaye, O.; Steffensen, F.H.; Bøtker, H.E.; Jensen, J.M.; Sand, N.P.R.; Kragholm, K.H.; Sørensen, H.T.; Leipsic, J.; Mæng, M.; et al. Impact of Plaque Burden Versus Stenosis on Ischemic Events in Patients With Coronary Atherosclerosis. J. Am. Coll. Cardiol. 2020, 76, 2803–2813. [Google Scholar] [CrossRef]
- Babateen, A.M.; Shannon, O.M.; Mathers, J.C.; Siervo, M. Validity and reliability of test strips for the measurement of salivary nitrite concentration with and without the use of mouthwash in healthy adults. Nitric Oxide 2019, 91, 15–22. [Google Scholar] [CrossRef]
- Puri, R.; Nissen, S.E.; Somaratne, R.; Cho, L.; Kastelein, J.J.; Ballantyne, C.M.; Koenig, W.; Anderson, T.J.; Yang, J.; Kassahun, H.; et al. Impact of PCSK9 inhibition on coronary atheroma progression: Rationale and design of Global Assessment of Plaque Regression with a PCSK9 Antibody as Measured by Intravascular Ultrasound (GLAGOV). Am. Hear. J. 2016, 176, 83–92. [Google Scholar] [CrossRef]
- Peña-Jorquera, H.; Cid-Jofré, V.; Landaeta-Díaz, L.; Petermann-Rocha, F.; Martorell, M.; Zbinden-Foncea, H.; Ferrari, G.; Jorquera-Aguilera, C.; Cristi-Montero, C. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome—A Comprehensive Review. Nutrients 2023, 15, 3244. [Google Scholar] [CrossRef]
- Salehin, S.; Rasmussen, P.; Mai, S.; Mushtaq, M.; Agarwal, M.; Hasan, S.M.; Salehin, S.; Raja, M.; Gilani, S.; Khalife, W.I. Plant Based Diet and Its Effect on Cardiovascular Disease. Int. J. Environ. Res. Public Heal. 2023, 20, 3337. [Google Scholar] [CrossRef]
- Koutentakis, M.; Surma, S.; Rogula, S.; Filipiak, K.J.; Gąsecka, A. The Effect of a Vegan Diet on the Cardiovascular System. J. Cardiovasc. Dev. Dis. 2023, 10, 94. [Google Scholar] [CrossRef]
- Tucci, M.; Marino, M.; Martini, D.; Porrini, M.; Riso, P.; Del Bo’, C. Plant-Based Foods and Vascular Function: A Systematic Review of Dietary Intervention Trials in Older Subjects and Hypothesized Mechanisms of Action. Nutrients 2022, 14, 2615. [Google Scholar] [CrossRef]
- Islam, S.U.; Ahmed, M.B.; Ahsan, H.; Lee, Y.-S. Recent Molecular Mechanisms and Beneficial Effects of Phytochemicals and Plant-Based Whole Foods in Reducing LDL-C and Preventing Cardiovascular Disease. Antioxidants 2021, 10, 784. [Google Scholar] [CrossRef]
- Mehta, P.; Tawfeeq, S.; Padte, S.; Sunasra, R.; Desai, H.; Surani, S.; Kashyap, R. Plant-based diet and its effect on coronary artery disease: A narrative review. World J. Clin. Cases 2023, 11, 4752–4762. [Google Scholar] [CrossRef]
- Bruns, A.; Greupner, T.; Nebl, J.; Hahn, A. Plant-based diets and cardiovascular risk factors: a comparison of flexitarians, vegans and omnivores in a cross-sectional study. BMC Nutr. 2024, 10, 1–13. [Google Scholar] [CrossRef]
- Di Sotto, A.; Vitalone, A.; Di Giacomo, S. Plant-Derived Nutraceuticals and Immune System Modulation: An Evidence-Based Overview. Vaccines 2020, 8, 468. [Google Scholar] [CrossRef]
- Xu, K.; Al-Ani, M.K.; Pan, X.; Chi, Q.; Dong, N.; Qiu, X. Plant-Derived Products for Treatment of Vascular Intima Hyperplasia Selectively Inhibit Vascular Smooth Muscle Cell Functions. Evidence-Based Complement. Altern. Med. 2018, 2018, 1–17. [Google Scholar] [CrossRef]
- Monsalve, B.; Concha-Meyer, A.; Palomo, I.; Fuentes, E. Mechanisms of Endothelial Protection by Natural Bioactive Compounds from Fruit and Vegetables. 2017, 89, 615–633. [CrossRef]
- Aquila, G.; Marracino, L.; Martino, V.; Calabria, D.; Campo, G.; Caliceti, C.; Rizzo, P. The Use of Nutraceuticals to Counteract Atherosclerosis: The Role of the Notch Pathway. Oxidative Med. Cell. Longev. 2019, 2019, 1–30. [Google Scholar] [CrossRef]
- Moss, J.W.E.; Ramji, D.P. Nutraceutical therapies for atherosclerosis. Nat. Rev. Cardiol. 2016, 13, 513–532. [Google Scholar] [CrossRef]
- Wei, T.; Liu, J.; Zhang, D.; Wang, X.; Li, G.; Ma, R.; Chen, G.; Lin, X.; Guo, X. The Relationship Between Nutrition and Atherosclerosis. Front. Bioeng. Biotechnol. 2021, 9. [Google Scholar] [CrossRef]
- Mitu, O.; Cirneala, I.A.; Lupsan, A.I.; Iurciuc, M.; Mitu, I.; Dimitriu, D.C.; Costache, A.D.; Petris, A.O.; Costache, I.I. The Effect of Vitamin Supplementation on Subclinical Atherosclerosis in Patients without Manifest Cardiovascular Diseases: Never-ending Hope or Underestimated Effect? Molecules 2020, 25, 1717. [Google Scholar] [CrossRef]
- Garcia, S.; Sandoval, Y.; Roukoz, H.; Adabag, S.; Canoniero, M.; Yannopoulos, D.; Brilakis, E.S. Outcomes After Complete Versus Incomplete Revascularization of Patients With Multivessel Coronary Artery Disease. J. Am. Coll. Cardiol. 2013, 62, 1421–1431. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, Y.; Brilakis, E.S.; Garcia, S. Completeness of revascularization in multivessel coronary artery disease. J. Thorac. Dis. 2016, 8, E1493–E1496. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Kang, J.; Yang, H.-M.; Yang, S.; Park, J.; Han, J.-K.; Kang, H.-J.; Koo, B.-K.; Kim, H.-S. Better Prognosis After Complete Revascularization Using Contemporary Coronary Stents in Patients With Chronic Kidney Disease. Circ. Cardiovasc. Interv. 2019, 12, e007907. [Google Scholar] [CrossRef]
- Iqbal, M.B.; Moore, P.T.; Nadra, I.J.; Robinson, S.D.; Fretz, E.; Ding, L.; Fung, A.; Aymong, E.; Chan, A.W.; Hodge, S.; et al. Complete revascularization in stable multivessel coronary artery disease: A real world analysis from the British Columbia Cardiac Registry. Catheter. Cardiovasc. Interv. 2021, 99, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Mittal, A.; Karageorgiev, D.; Romo, A.I.; Aminian, A.; Portalese, J.F.; Kharrat, E.; Gómez-Hospital, J.A.; Firman, D.; Nouche, R.T.; et al. Complete revascularization optimizes patient outcomes in multivessel coronary artery disease: Data from the e-Ultimaster registry. Catheter. Cardiovasc. Interv. 2021, 99, 961–967. [Google Scholar] [CrossRef]
- Pham, V.; Moroni, A.; Gall, E.; Benedetti, A.; Zivelonghi, C.; Picard, F. Revascularization and Medical Therapy for Chronic Coronary Syndromes: Lessons Learnt from Recent Trials, a Literature Review. J. Clin. Med. 2023, 12, 2833. [Google Scholar] [CrossRef] [PubMed]
- Giubilato, S.; Lucà, F.; Abrignani, M.G.; Gatto, L.; Rao, C.M.; Ingianni, N.; Amico, F.; Rossini, R.; Caretta, G.; Cornara, S.; et al. Management of Residual Risk in Chronic Coronary Syndromes. Clinical Pathways for a Quality-Based Secondary Prevention. J. Clin. Med. 2023, 12, 5989. [Google Scholar] [CrossRef] [PubMed]
- Ornish, D.; Scherwitz, L.W.; Billings, J.H.; Gould, K.L.; Merritt, T.A.; Sparler, S.; Armstrong, W.T.; Ports, T.A.; Kirkeeide, R.L.; Hogeboom, C.; et al. Intensive Lifestyle Changes for Reversal of Coronary Heart Disease. JAMA 1998, 280, 2001–2007. [Google Scholar] [CrossRef]
- Esselstyn CB Jr, Gendy G, Doyle J, et al. A way to reverse CAD? J Fam Pract. 2014 Jul;63(7):356-364b. PMID: 25198208.
- Mulijono, D. Mechanism of How Plant-Based Diet (PBD) Reduces the Risk of In-Stent Restenosis (ISR) and Stent Thrombosis (ST). Preprints 2024, 2024040628. [Google Scholar] [CrossRef]
- Rose, S.; Strombom, A. A Comprehensive Review of the Prevention and Treatment of Heart Disease with a Plant-Based Diet. J. Cardiol. Cardiovasc. Ther. 2018, 12, 1–12. [Google Scholar] [CrossRef]
- Bilal, M.; Ashraf, S.; Zhao, X. Dietary Component-Induced Inflammation and Its Amelioration by Prebiotics, Probiotics, and Synbiotics. Front. Nutr. 2022, 9, 931458. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, S.; Dixit, M. Role of Polyphenols and Other Phytochemicals on Molecular Signaling. Oxid. Med. Cell. Longev. 2015, 2015, 504253. [Google Scholar] [CrossRef]
- Wu, Y.-T.; Chen, L.; Tan, Z.-B.; Fan, H.-J.; Xie, L.-P.; Zhang, W.-T.; Chen, H.-M.; Li, J.; Liu, B.; Zhou, Y.-C. Luteolin Inhibits Vascular Smooth Muscle Cell Proliferation and Migration by Inhibiting TGFBR1 Signaling. Front. Pharmacol. 2018, 9, 1059. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.G.; Florida, E.; Li, H.; Parel, P.M.; Mehta, N.N.; Sorokin, A.V. Oxidized low-density lipoprotein associates with cardiovascular disease by a vicious cycle of atherosclerosis and inflammation: A systematic review and meta-analysis. Front. Cardiovasc. Med. 2023, 9, 1023651. [Google Scholar] [CrossRef] [PubMed]
- Marchio, P.; Guerra-Ojeda, S.; Vila, J.M.; Aldasoro, M.; Victor, V.M.; Mauricio, M.D. Targeting Early Atherosclerosis: A Focus on Oxidative Stress and Inflammation. Oxid. Med. Cell Longev. 2019, 2019, 8563845. [Google Scholar] [CrossRef] [PubMed]
- Ray, A.; Maharana, K.C.; Meenakshi, S.; Singh, S. Endothelial dysfunction and its relation in different disorders: Recent update. Heal. Sci. Rev. 2023, 7. [Google Scholar] [CrossRef]
- Almeida, C.; Barata, P.; Fernandes, R. The influence of gut microbiota in cardiovascular diseases—a brief review. Porto Biomed. J. 2021, 6, e106. [Google Scholar] [CrossRef] [PubMed]
- Pollicino, F.; Veronese, N.; Dominguez, L.J.; Barbagallo, M. Mediterranean diet and mitochondria: New findings. Exp. Gerontol. 2023, 176, 112165. [Google Scholar] [CrossRef]
- Cinegaglia, N.; Antoniazzi, L.; Rosa, D.; Miranda, D.; Acosta-Navarro, J.; Bortolotto, L.; Hong, V.; Sandrim, V. Shortening telomere is associated with subclinical atherosclerosis biomarker in omnivorous but not in vegetarian healthy men. Aging 2019, 11, 5070–5080. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




