Introduction
There are three situations when the Subcrestally Placed Implant (SPI) technique is necessary. First, it satisfies the esthetic requirements with an emergent profile, particularly in molar restoration cases. Second, it addresses the challenge of narrow ridges suitable for implant placement. Using the SPI technique, a favorable phenotype can be achieved.^[
1] Third, the technique is applicable when implants are placed in the premolar or anterior region adjacent to healthy natural teeth, especially in the upper area, where there are differences in the levels of the edentulous ridge between the buccolingual and mesiodistal interproximal areas.
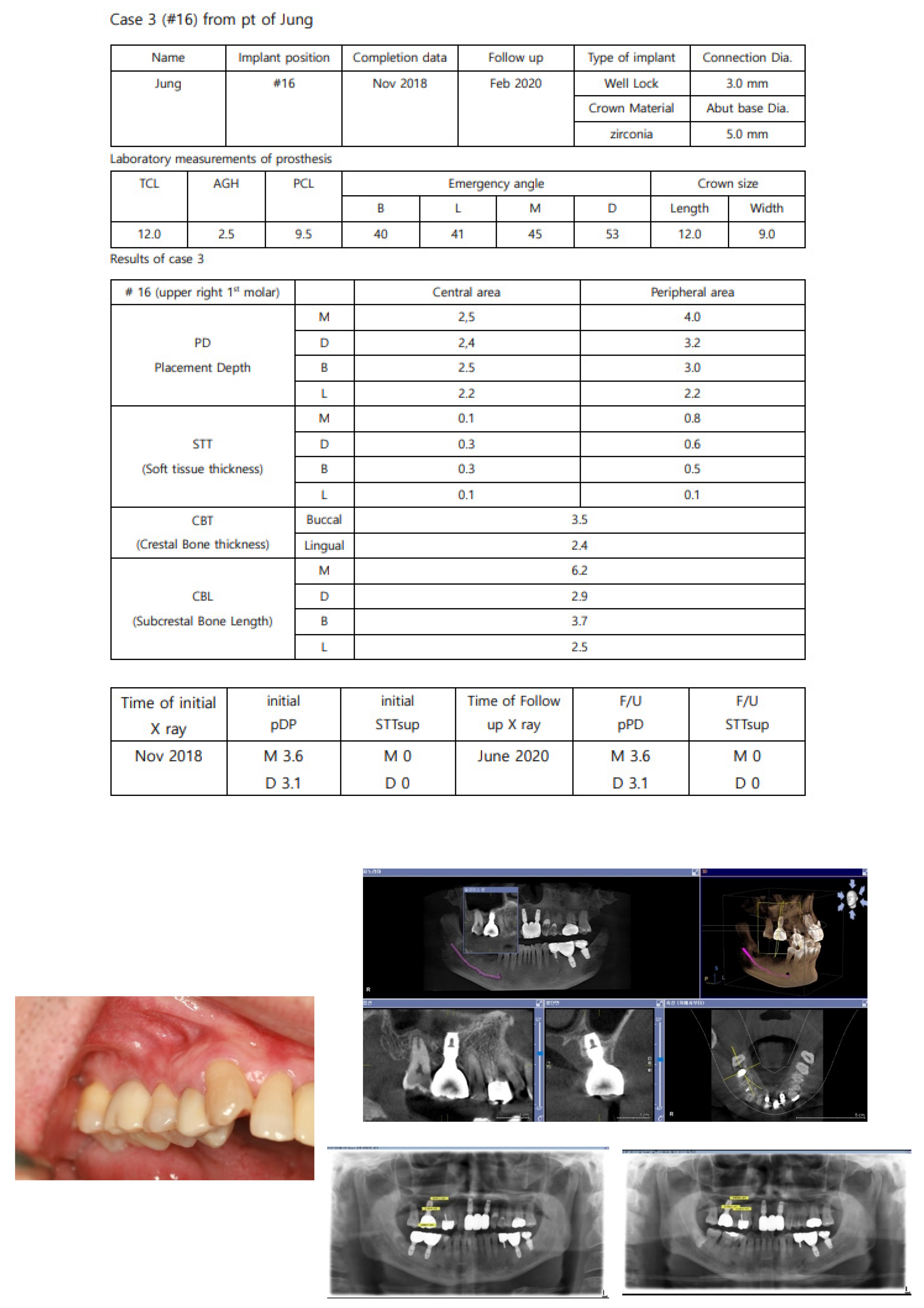
However, when implants are placed subcrestally, there have been concerns regarding the biologic width because the SPI may cause a deep pocket, which has been considered harmful to periodontal and peri-implant health. The concept of biologic width around a natural tooth was proposed in 1961.^[
2] It is defined as anatomical gingival soft tissue extending from the gingival sulcus to the alveolar crest, approximately 2 mm wide, comprising 0.97 mm of junctional epithelium and 1.07 mm of connective tissue.^[
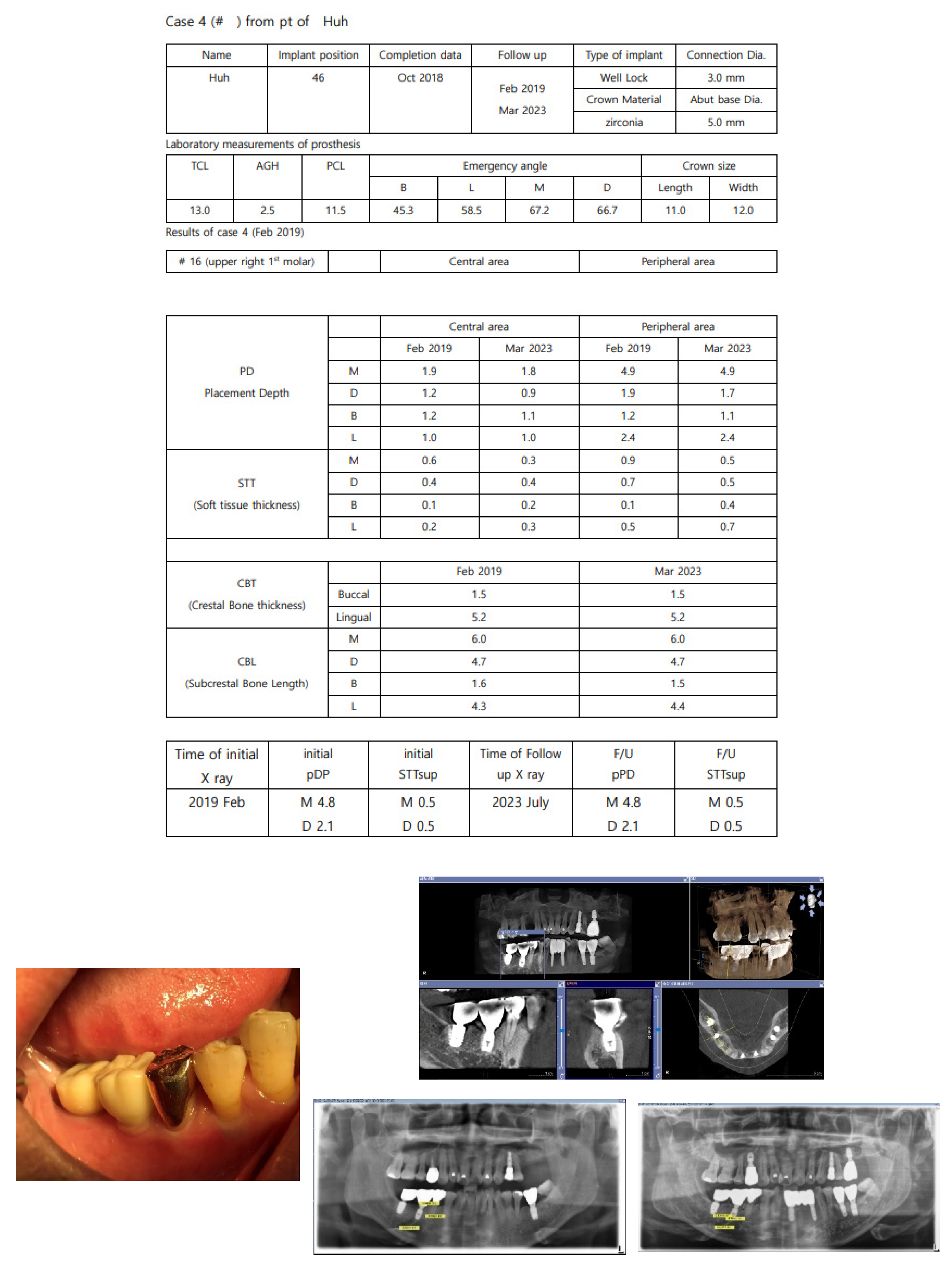
3] This structure performs mechanical and immunological functions to protect the inner structure from external stimuli. The size and disposition of the biologic width are determined by the position of implant fixtures and the design of the prostheses, which can affect the stability and appearance of the implants.^[
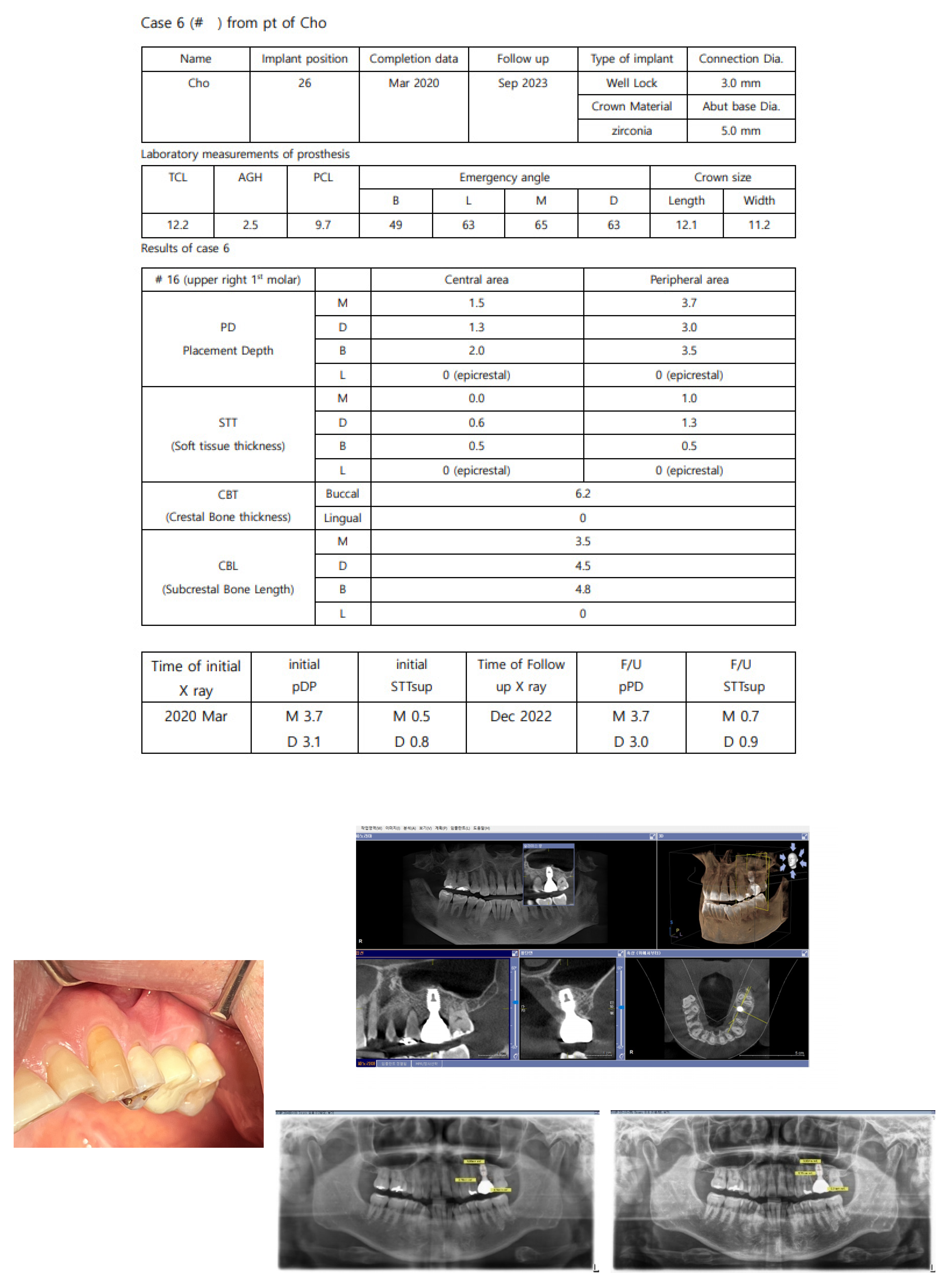
4,
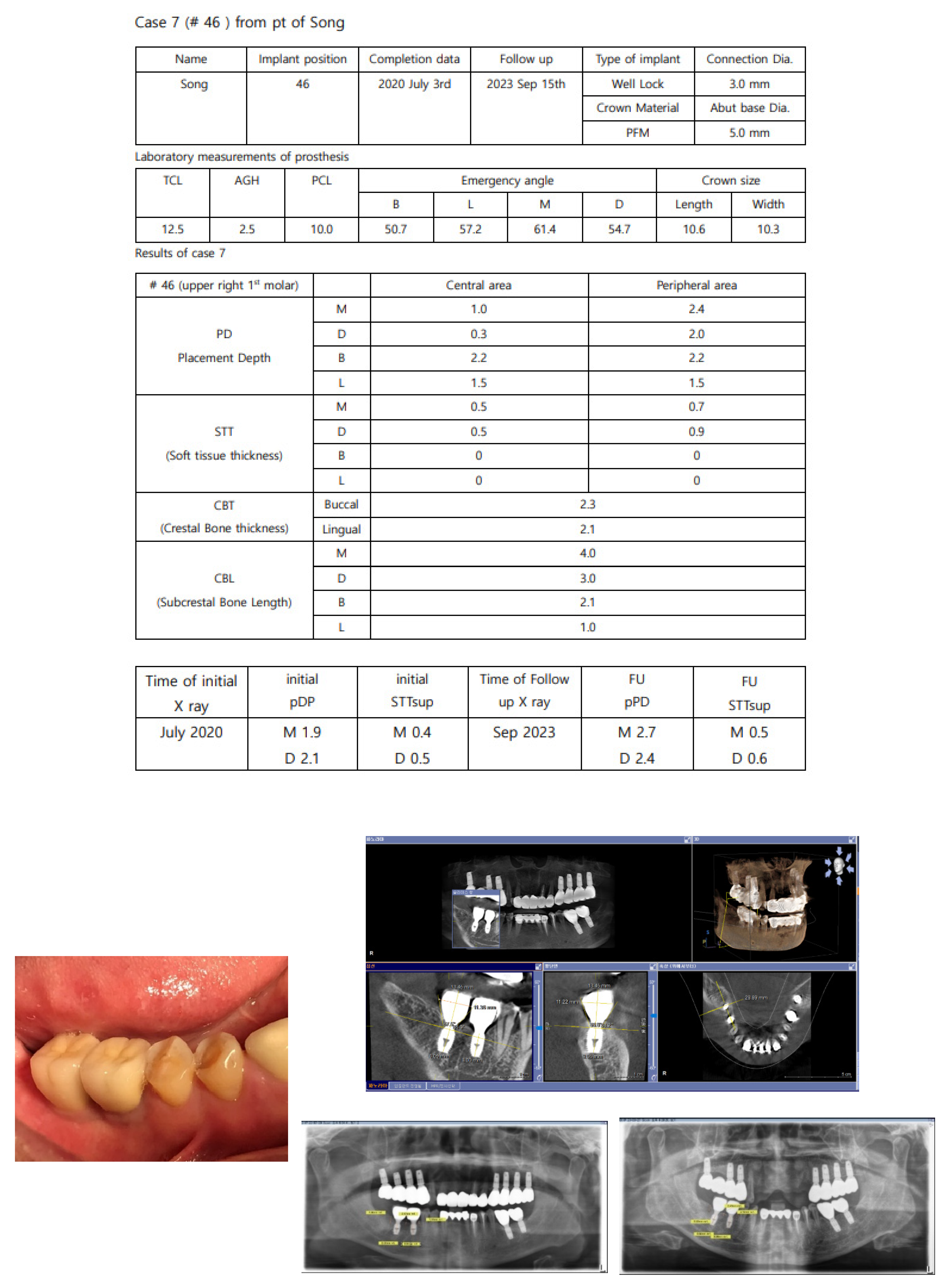
5] Although the same term "biologic width" is applied to the soft tissue around implants and shares some similarities, it differs in structure. It is typically 3-4 mm of soft tissue in the vertical dimension from the top of the peri-implant mucosa to the first bone-to-implant contact and performs similar functions as the biologic width around natural teeth.^[
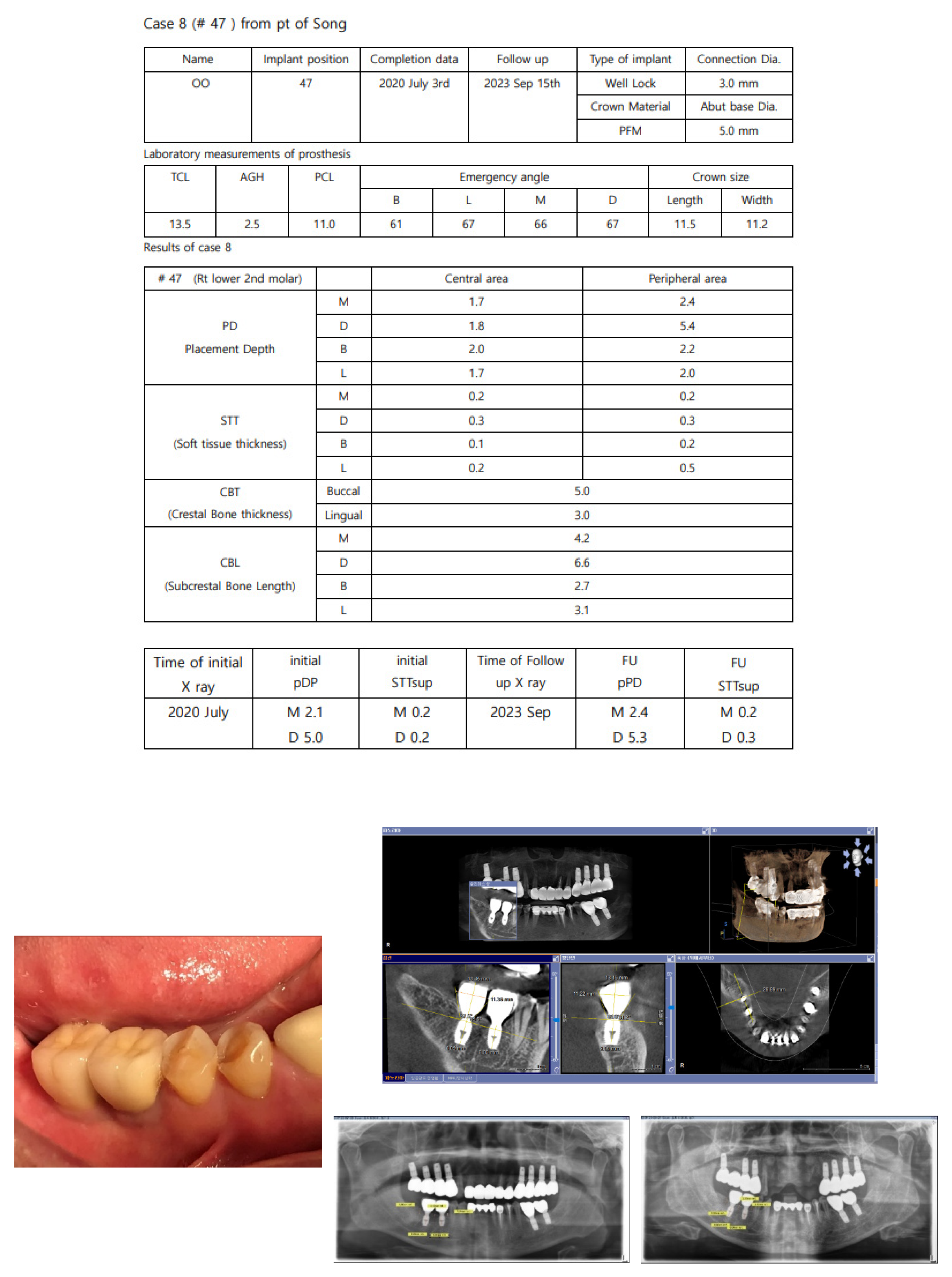
6]
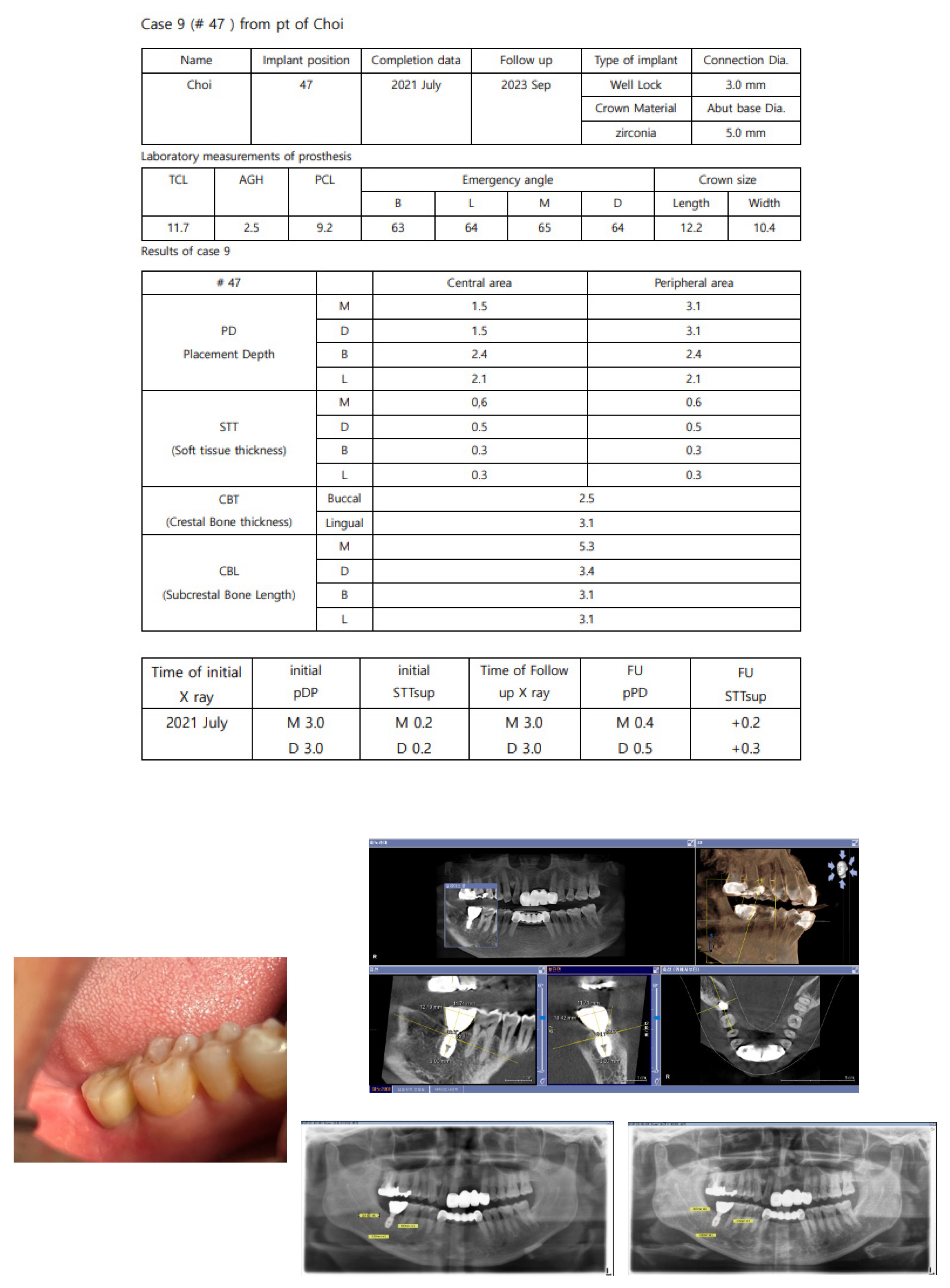
This article introduces a new approach, 3-Dimensional Soft Tissue Analysis (3DSTA), to investigate the soft tissue of SPIs, which are known to have benefits for both stability and esthetics when certain requirements are met. These include techniques to avoid excessive cement remnants, ensure hermetic abutment connections, and respect the biologic soft tissue dimensions. To fulfill these requirements, implants with internal connections and platform switching (IPS) design were used. The depth of placement, especially in molar regions, is often deeper to emulate the size and appearance of natural teeth. This result may seem counterintuitive because of the inevitable long soft tissue distance subgingivally (or submucosally), which can be mistakenly perceived as a pocket. The resultant soft tissue architecture surrounding SPIs with IPS design may confuse clinicians accustomed to the traditional concept of biologic width and the conventional idea of a pocket. This confusion arises from the reliance on 2-dimensional analyses, which have been standard for decades in studying the soft tissue around both natural teeth and dental implants. For example, the results from studies of biologic width around natural teeth and implants are typically represented as a certain length (0.97 mm and 1.07 mm for epithelial and connective attachments, respectively) in one direction. These findings are applicable to all aspects of teeth and implants, i.e., mesial, distal, buccal, and lingual. However, unlike natural teeth, implants exhibit an emerging phenomenon, and the architecture of the bone and the soft tissue around implants should be interpreted in a multidirectional way. To achieve a natural emergent profile, CAD/CAM customized healing abutments can be utilized.^[
7] With a better understanding of the underlying bone architecture and its related soft tissue structure, implant prostheses can be made healthier and more natural.
Two Goals of dental implants
Clinicians consider two primary goals when selecting an implant technique. The first goal focuses on biological stability by achieving structural integrity, while the second addresses the functional and esthetic aspects. The depth of implant placement plays a crucial role in both goals, ultimately influencing the nature of the soft tissue sealing around implants, which includes connective tissue and junctional epithelium.
The first goal is to prevent bone loss around implants. Historically, the development of implantology has seen various designs in the connection part between implant fixtures and abutments to enhance biological stability by accommodating the so-called biologic width. Initially, the external hex connection type was known for its unavoidable annual bone loss. To mitigate this, the platform switching concept was introduced. Presently, many implant products utilize the internal connection type and platform switching (IPS) designs, which are reported to foster a beneficial environment for soft tissue by providing a bacterial seal to some degree, varying by manufacturer.^[
8] Additionally, other designs like one-body type implants, tissue level implants, and Morse taper screwless implant connection designs have been introduced to improve biological stability. These designs are recognized for their biologically favorable merits, though they also have demerits linked to their unique characteristics. Linkevicius et al. demonstrated that bone loss could be prevented by establishing sufficient biological protection, which is related to soft tissue thickness, and showed that subcrestal implant placement could contribute to this environmental improvement. Vervaeke et al. suggested the positive effects of subcrestal implant placement on bone remodeling by re-establishing the biologic width.^[
9,
10]
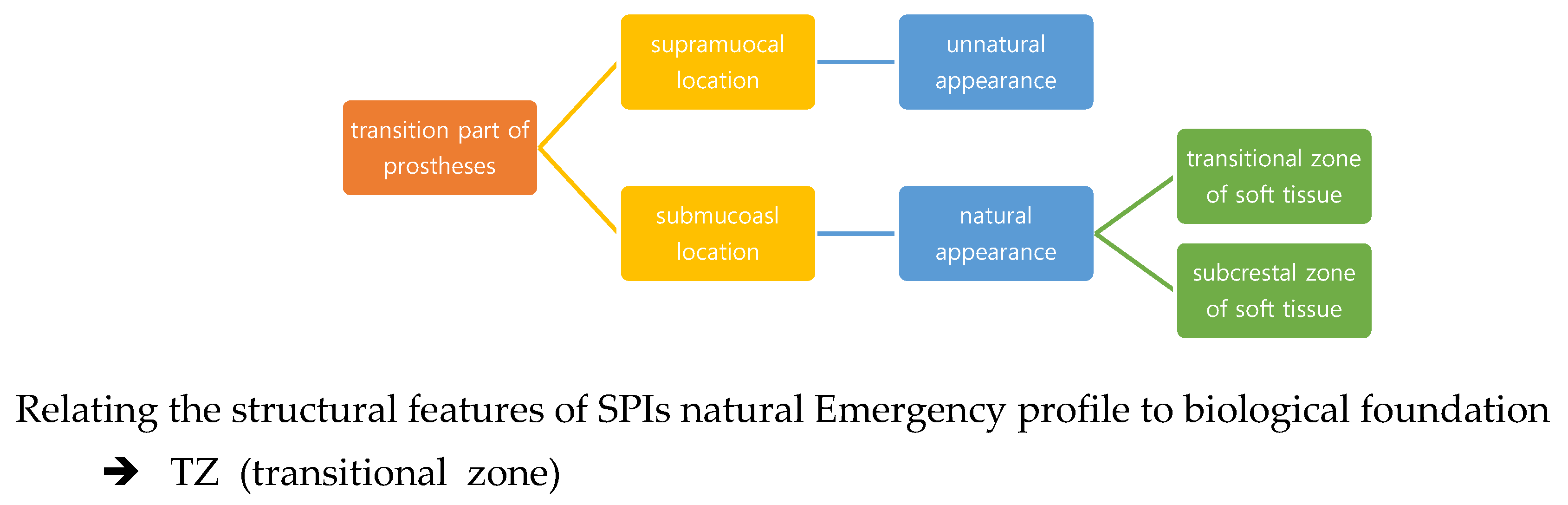
The second goal is to emulate the natural appearance and function of teeth. This goal requires the recreation of a 3-dimensional space to construct artificial structures (including implants, abutments, and prostheses) upon the biological foundation of bone and soft tissue. Dental implant restorations emerge from the submucosal components—the connection between abutments and implant fixtures typically have a narrower diameter (average 3.0 – 5.0 mm) than their upper supramucosal counterparts (average 8-12 mm). To achieve a natural appearance, this transition part should increase gradually. Both the depth of the implant fixture and the destined diameter of the final restoration influence the emerging angle, thereby defining the emergent profile. When the crown part matches the final size of natural teeth diameters from the cervical area just above the marginal gingiva with its transition part lying submucosally, the result appears natural. Conversely, if the transition part is observed at the supramucosal area or the final crown size is smaller than that of natural teeth, the result does not appear natural.^[
11] Natalia Palacios-Garzón reported that there is no significant difference in bone loss between implants placed at subcrestal and crestal levels after a systematic review and meta-analysis, suggesting that factors other than placement level might influence bone loss, and that subcrestal placement could be more favorable for a natural emergent profile if it is not directly associated with bone loss.^[
12]
Figure 1.
The Transition Part in Implant Design. The transition part refers to the distance from the connection between the fixture and abutment to the final cervical area of the crown. Aesthetically, if the transition part is visible supramucosally, it tends to appear unnatural. Conversely, when it lies submucosally, the appearance is more natural. This section includes both vertical and horizontal components, which together determine the angle of the emergent profile of the final restoration.
Figure 1.
The Transition Part in Implant Design. The transition part refers to the distance from the connection between the fixture and abutment to the final cervical area of the crown. Aesthetically, if the transition part is visible supramucosally, it tends to appear unnatural. Conversely, when it lies submucosally, the appearance is more natural. This section includes both vertical and horizontal components, which together determine the angle of the emergent profile of the final restoration.
Emerging Phenomenon and the Transitional Zone
The traditional concept of biologic width, derived from studies on natural teeth, is often applied to interpreting the soft tissue around dental implants. Anatomically, this biologic width comprises epithelium and connective tissue, and while generally consistent, it does exhibit some variability. Functionally, it serves as the primary defense line for both natural teeth and implants against foreign invasions through its mechanical sealing ability and immunological functions. This transition area, known as the 'biologic width' in natural teeth, primarily has a vertical component. Some tissue-level implants with wide diameters also display only vertical components because the diameter difference between crowns and connection parts is minimal, simplifying the application of natural teeth's biologic width concepts to dental implants. However, implants with Internal Platform Switching (IPS) design feature horizontal distance differences, which constitute the horizontal component while the prostheses pass through the transitional zone, either submucosally or supramucosally.
When planning a crown that mimics the diameter of natural teeth, several factors must be considered to determine the depth of implant placement. One crucial consideration is respecting the biologic width, which entails allocating adequate space for the soft tissue around the transmucosal area of implants. When considering only a vertical component, the guideline for implant depth follows the traditional biologic width, typically 3-4 mm. This minimum soft tissue thickness or space is the primary concern to adhere to biological principles. However, when both vertical and horizontal components are considered, the emergent angle affects the space for soft tissue, potentially creating a favorable or unfavorable environment depending on the angle. Thus, both the intended emergent angle and the horizontal component's distance difference must be considered as guidelines for determining the depth of implant fixture placement during the first surgery.
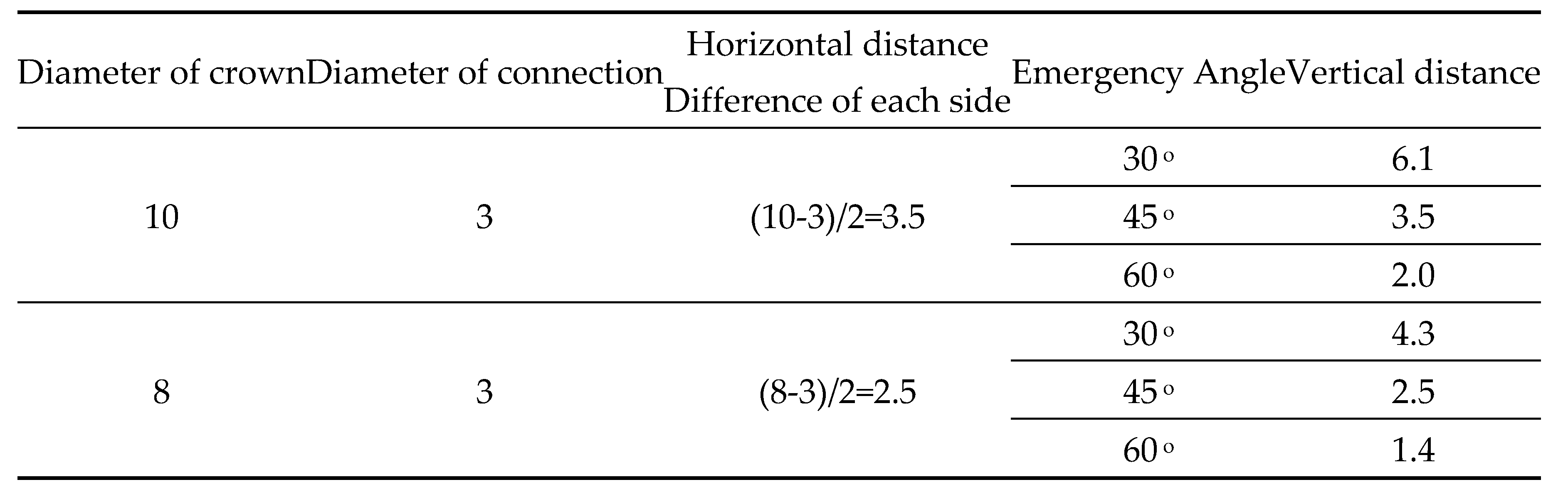
The average posterior molars have a breadth and width (or mesiodistal or buccolingual length) of about 10 mm. However, the starting points of implant crowns, which are the fixture-abutment connection joints, average 3.0 mm in diameter. The diameter of crowns should gradually increase to 10 mm from 3 mm. The calculated horizontal difference is (10−3)/2=3.5(10−3)/2=3.5 mm. This 3.5 mm horizontal increasing distance on each side from the center should increase within its accompanying vertical components if the emerging angle is 45 degrees. It was reported that when the emerging angle is less than 30 degrees, crestal bone changes were minimal due to more stable biologic width.^[
13,
14] For instance, when the horizontal difference distance is 3.5 mm and the intended emergent angle is 30 degrees, the required vertical distance is 3.5×1.7=6.13.5×1.7=6.1 mm. Alternatively, when the horizontal difference distance is 2 mm (in the premolar area) and the intended emergent angle is 30 degrees, the required vertical distance is 2×1.7=3.42×1.7=3.4 mm.
Figure 2.
Table of Vertical Distance Calculations. This table presents examples of how to calculate the required vertical distance based on different emergent angles and horizontal distances of difference for bone level implants designed with Internal Platform Switching (IPS). Each entry illustrates the necessary adjustments in vertical distance to accommodate specified emergent angles, providing a precise guide for implant placement to achieve optimal aesthetic and functional outcomes.
Figure 2.
Table of Vertical Distance Calculations. This table presents examples of how to calculate the required vertical distance based on different emergent angles and horizontal distances of difference for bone level implants designed with Internal Platform Switching (IPS). Each entry illustrates the necessary adjustments in vertical distance to accommodate specified emergent angles, providing a precise guide for implant placement to achieve optimal aesthetic and functional outcomes.
Implant Placement and Emergent Angle Determination
The depth of placement and the emergent angle should be determined based on the intended final crown size. However, when placing a tissue-level implant, the horizontal difference is typically less than 2 mm. In such cases, the part of the machined surface area transitions through the soft tissue, and the prosthesis margin is located above the biologic width. Due to the short horizontal distance, the emerging curve is not as pronounced or significant as with bone level implants.
With implants using Internal Platform Switching (IPS), a natural appearance is achieved only when the transition part is located submucosally, allowing the crown to emerge just above the gingiva with the final diameter matching that of natural teeth. This setup determines the vertical component of the submucosal transition part to ensure the final results look natural. In molar regions, the vertical distance required by the above calculations necessitates placing implant fixtures subcrestally to obtain additional vertical distance (about 2 mm) plus the conventionally accepted biologic width of 3-4 mm.
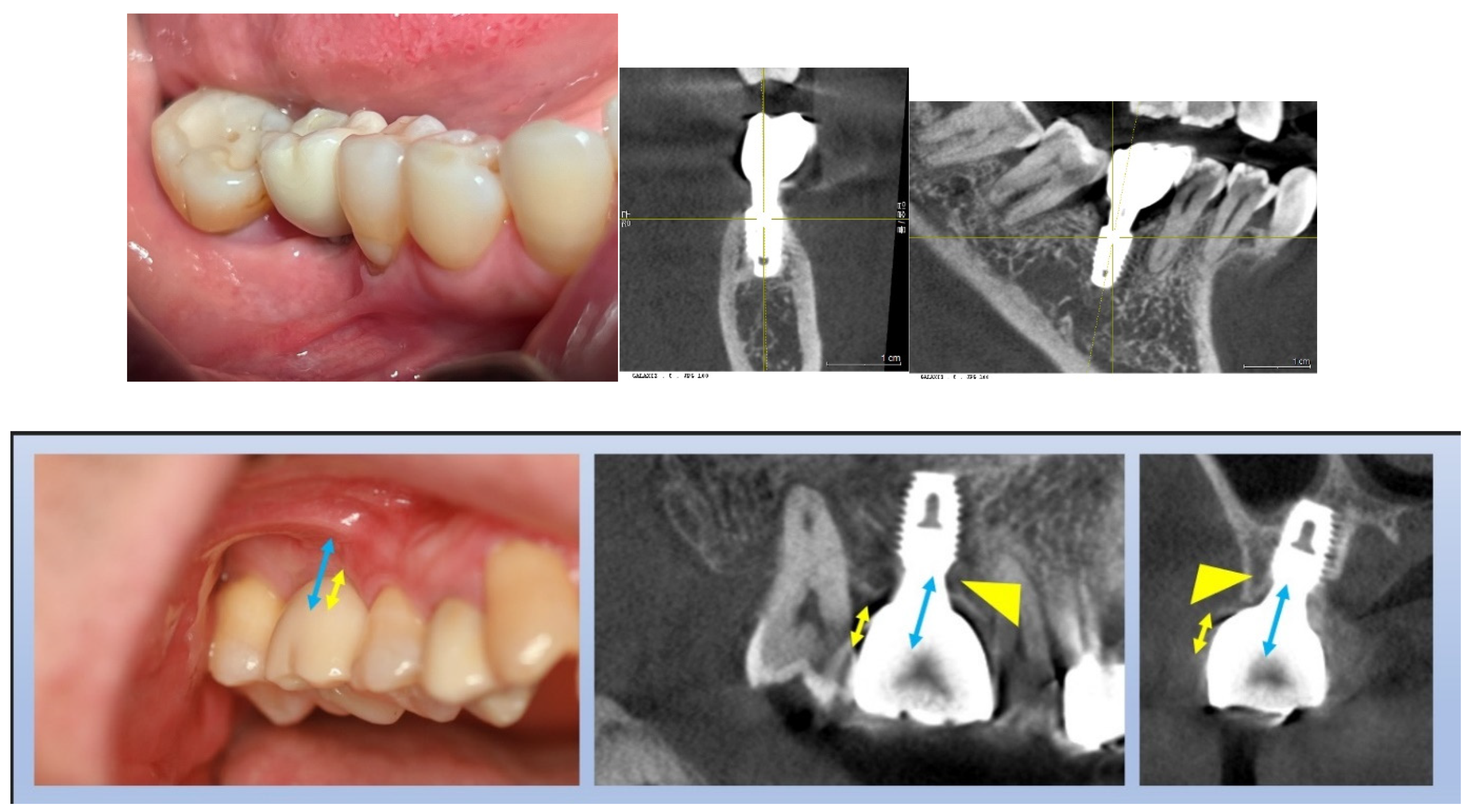
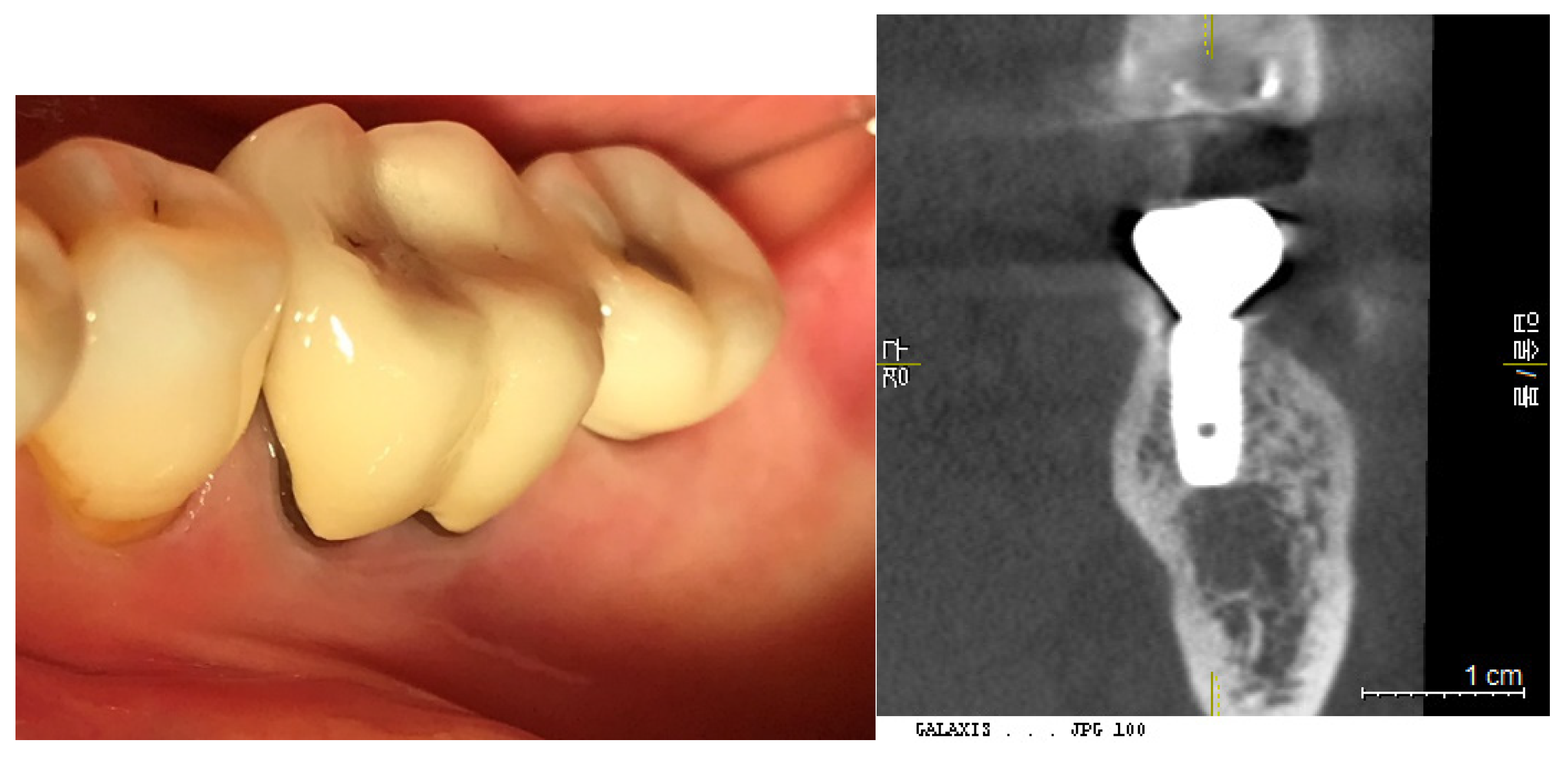
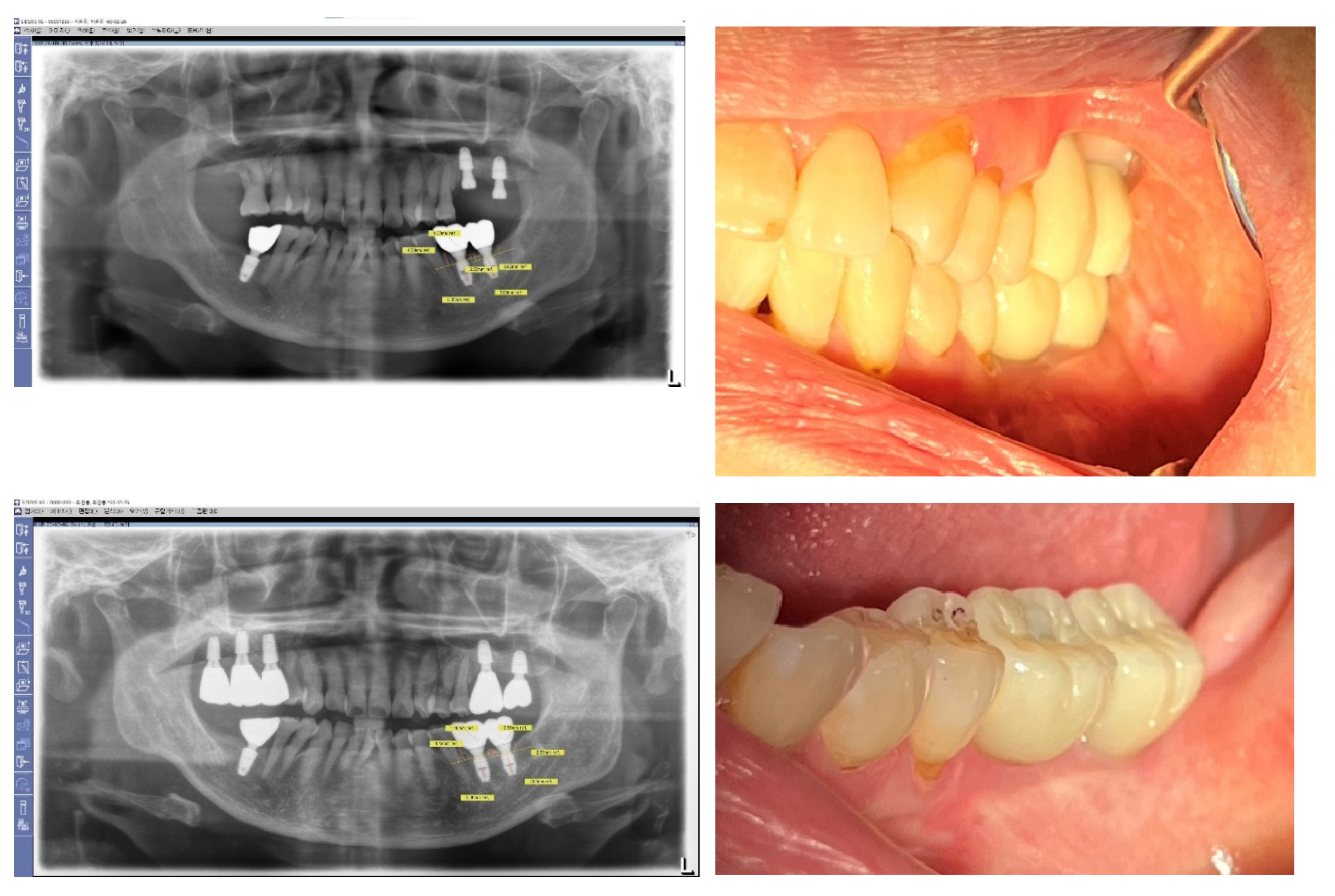
Figure 3 and Figure 4: Impact of Implant Placement Depth on Clinical Crown Shape
These figures demonstrate the effect of the depth of implant placement on the shape of the clinical crown.
Figure 3 shows an equicrestal placement of a second molar implant, where insufficient vertical space necessitates a smaller diameter or an abrupt emergent profile for the clinical crown. In contrast,
Figure 4 illustrates a subcrestal placement for a first molar implant, which provides sufficient vertical space allowing for the creation of a more natural-looking clinical crown with a gradual emerging profile.
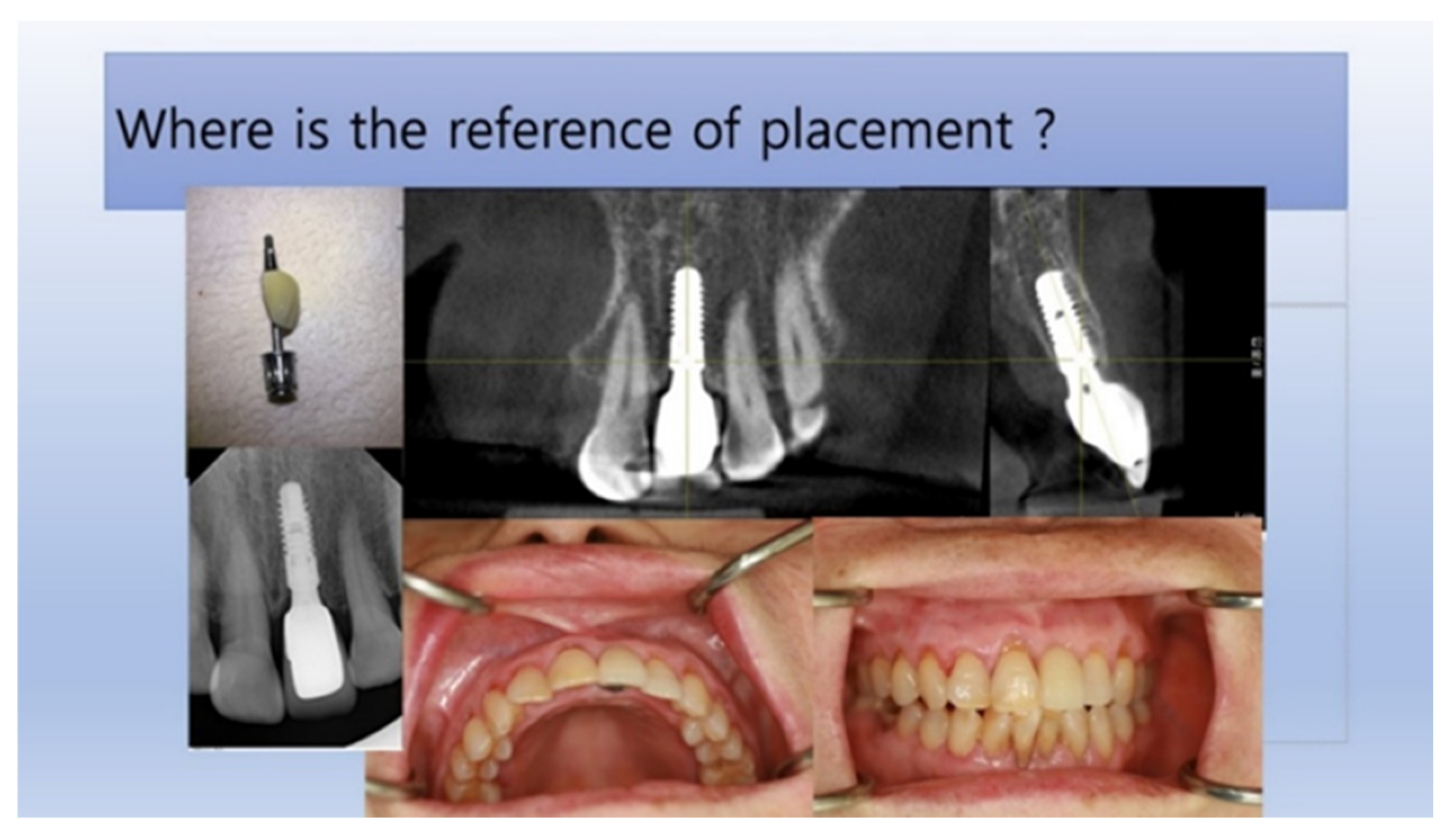
Figure 3.
Case Study of Epi-Crestal Placement of a Second Molar Implant. This figure illustrates a case where a second molar implant was placed epi-crestally, resulting in a smaller clinical crown size and an unnatural appearance due to an improper emergent profile compared to the adjacent natural molar. This outcome is attributed to the shallow depth of placement, which causes the transition part to be exposed supramucosally.
Figure 3.
Case Study of Epi-Crestal Placement of a Second Molar Implant. This figure illustrates a case where a second molar implant was placed epi-crestally, resulting in a smaller clinical crown size and an unnatural appearance due to an improper emergent profile compared to the adjacent natural molar. This outcome is attributed to the shallow depth of placement, which causes the transition part to be exposed supramucosally.
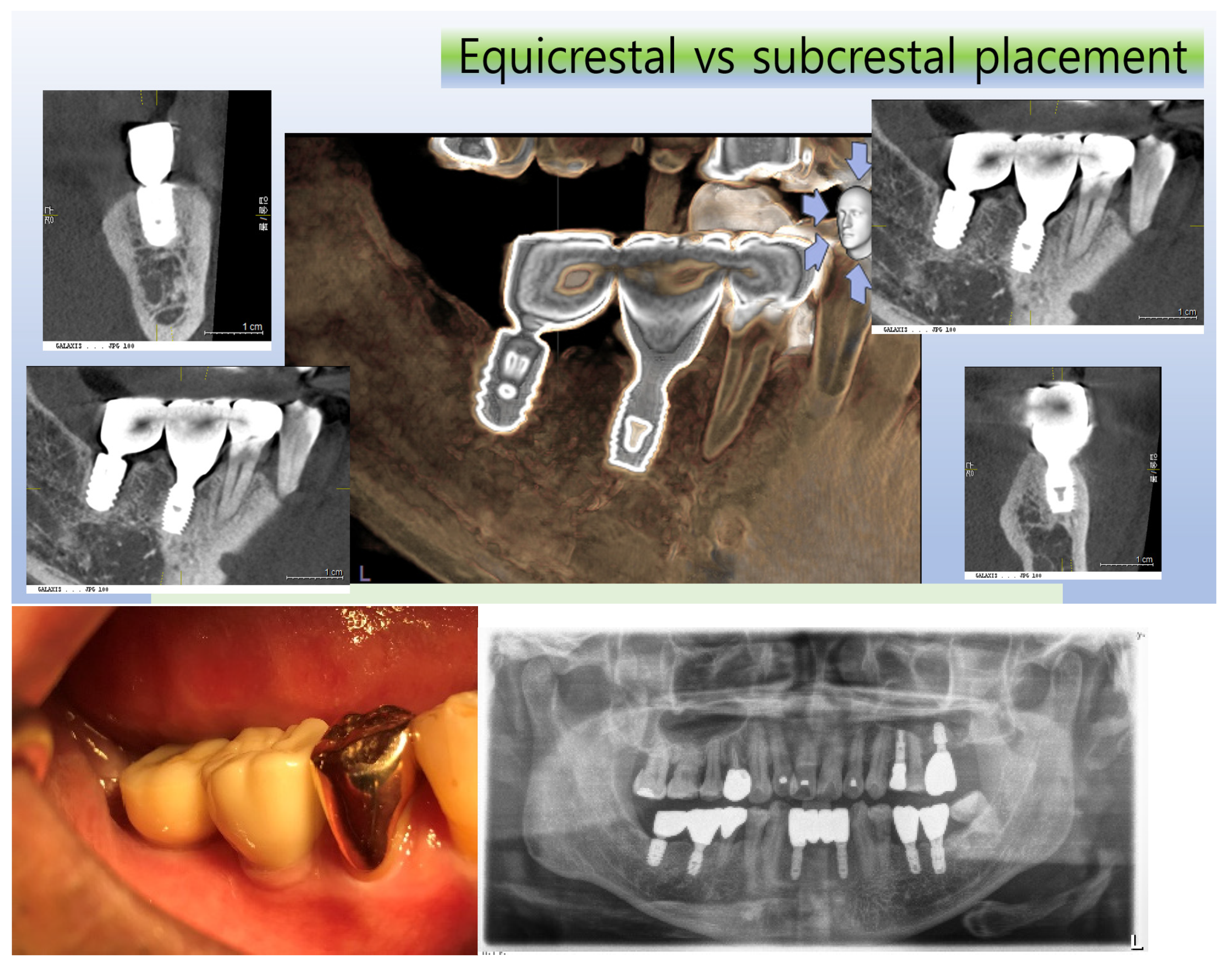
Figure 4.
Comparative Case of Equicrestal vs. Subcrestal Implant Placement. This figure demonstrates the differences between equicrestal and subcrestal implant placements. For the implant in the position of the second molar, equicrestal placement results in a molar diameter reaching a short vertical distance, leading to an abrupt emergent profile with the transition part located supramucosally. In contrast, for the implant in the position of the first molar, subcrestal placement yields a more natural appearance, as it allows for a gradual emergence with the vertical distance matching the horizontal distance needed for diameter increase, and the transition part located submucosally.
Figure 4.
Comparative Case of Equicrestal vs. Subcrestal Implant Placement. This figure demonstrates the differences between equicrestal and subcrestal implant placements. For the implant in the position of the second molar, equicrestal placement results in a molar diameter reaching a short vertical distance, leading to an abrupt emergent profile with the transition part located supramucosally. In contrast, for the implant in the position of the first molar, subcrestal placement yields a more natural appearance, as it allows for a gradual emergence with the vertical distance matching the horizontal distance needed for diameter increase, and the transition part located submucosally.
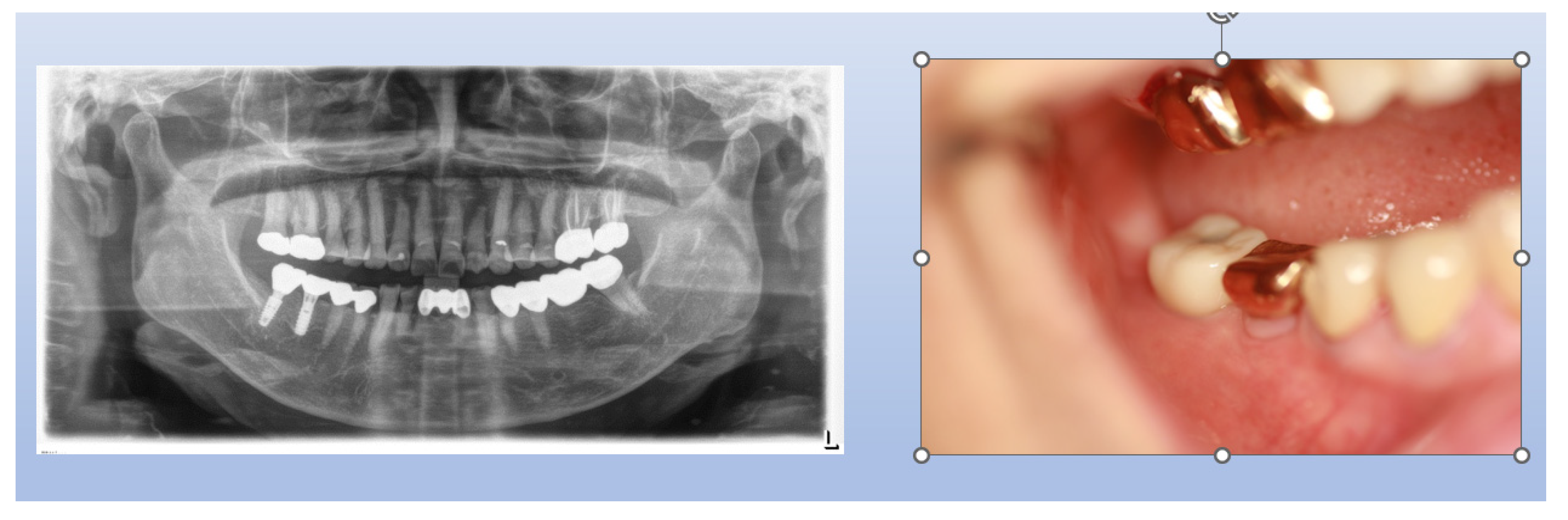
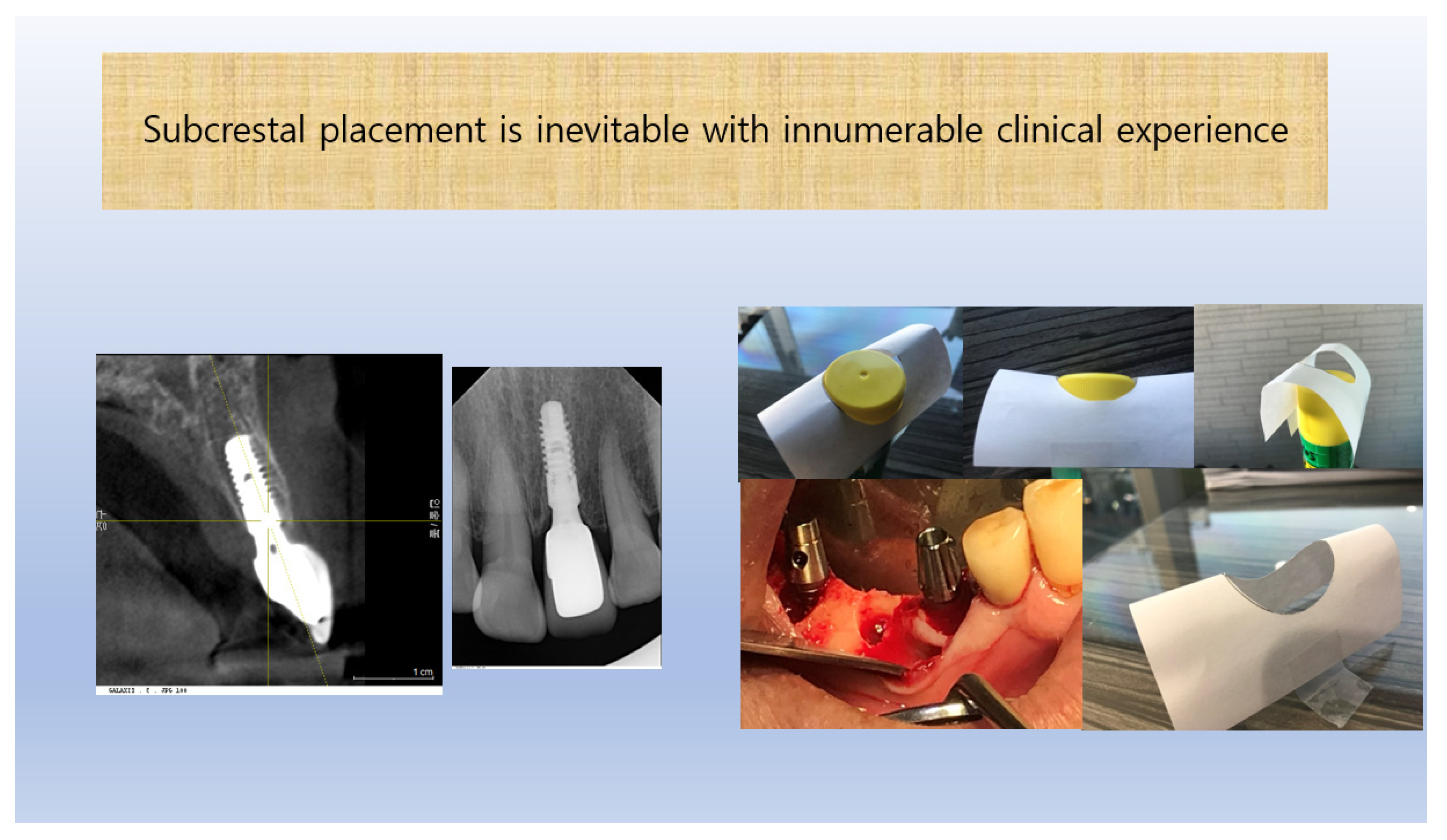
Situations When Implant Fixtures are Placed Subcrestally
Additional Reasons for Subcrestal Implant Placement
Subcrestal placement of implant fixtures is often necessary beyond aesthetic or anatomical considerations. Typically, the standard reference point for determining fixture depth is the most apical part of the crestal area—the most apical point. Outside of this area, placing the fixture subcrestally becomes inevitable unless the bone is trimmed. However, bone trimming can be detrimental, especially when the adjacent teeth share the crestal (septal) bone. Furthermore, preserving the crestal bone above a subcrestally placed fixture can enhance mucosal support by maintaining essential blood supply, which is crucial for achieving stable and aesthetically pleasing results.
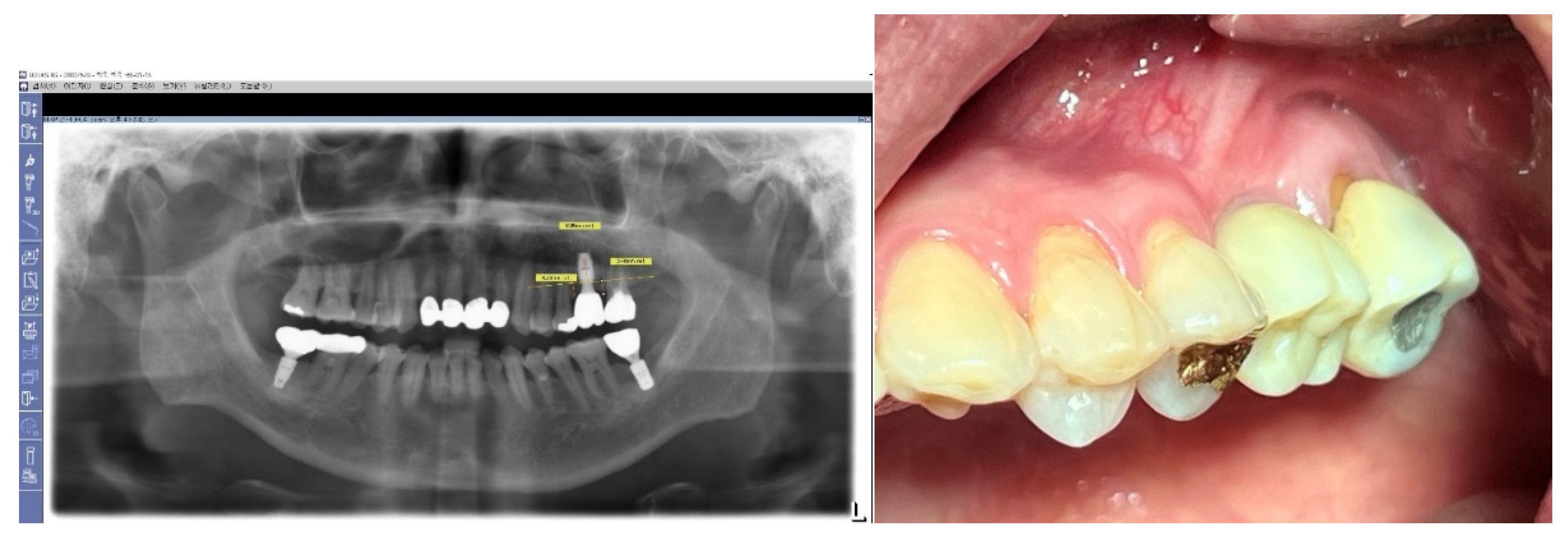
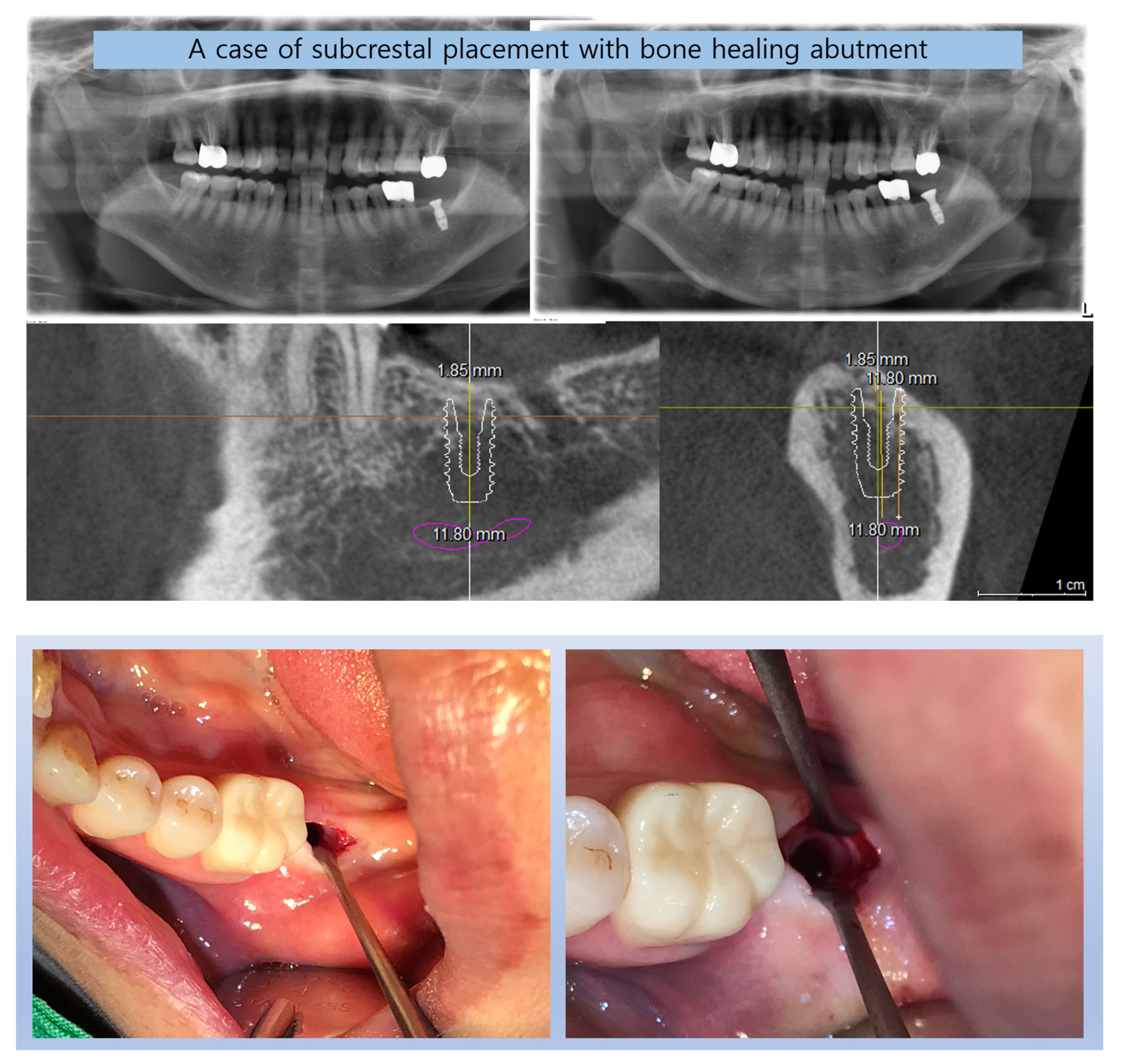
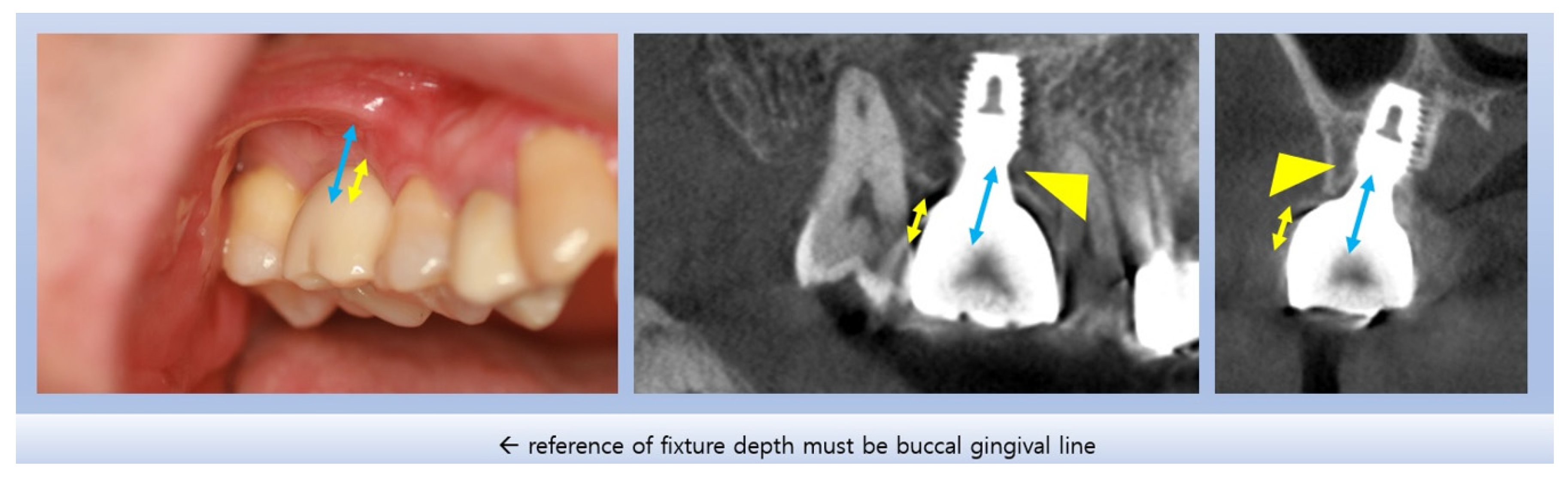
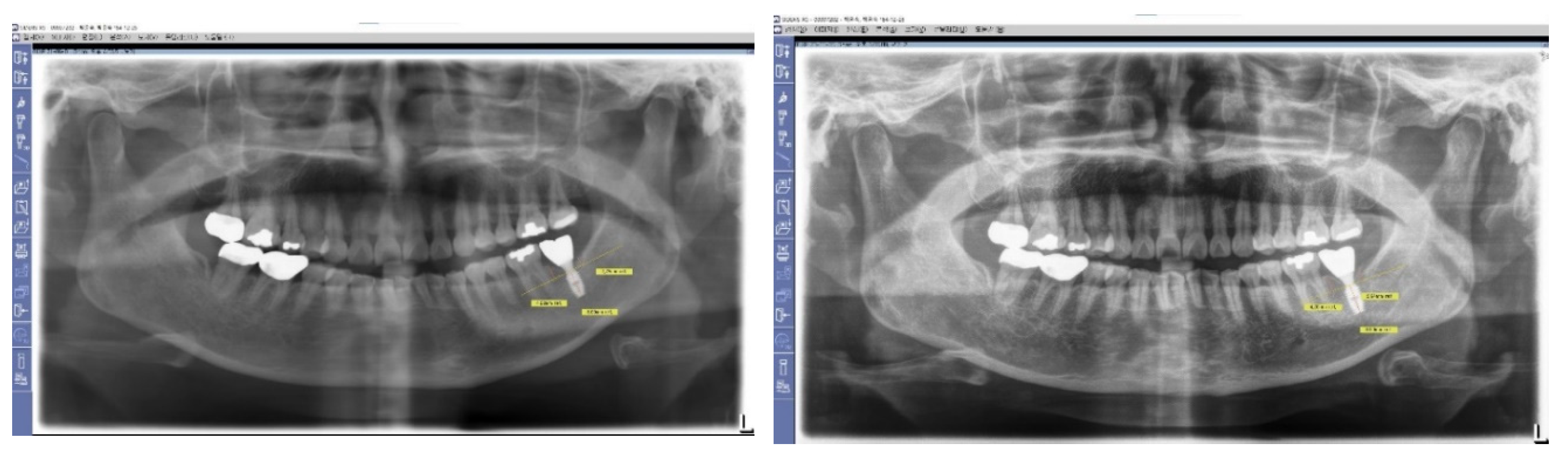
Figure 5.
This figure illustrates a case where a plain X-ray image suggests that the implant was placed subcrestally, but a CBCT (Cone Beam Computed Tomography) image reveals that the fixture was actually placed epi-crestally in the buccolingual aspect.
Figure 5.
This figure illustrates a case where a plain X-ray image suggests that the implant was placed subcrestally, but a CBCT (Cone Beam Computed Tomography) image reveals that the fixture was actually placed epi-crestally in the buccolingual aspect.
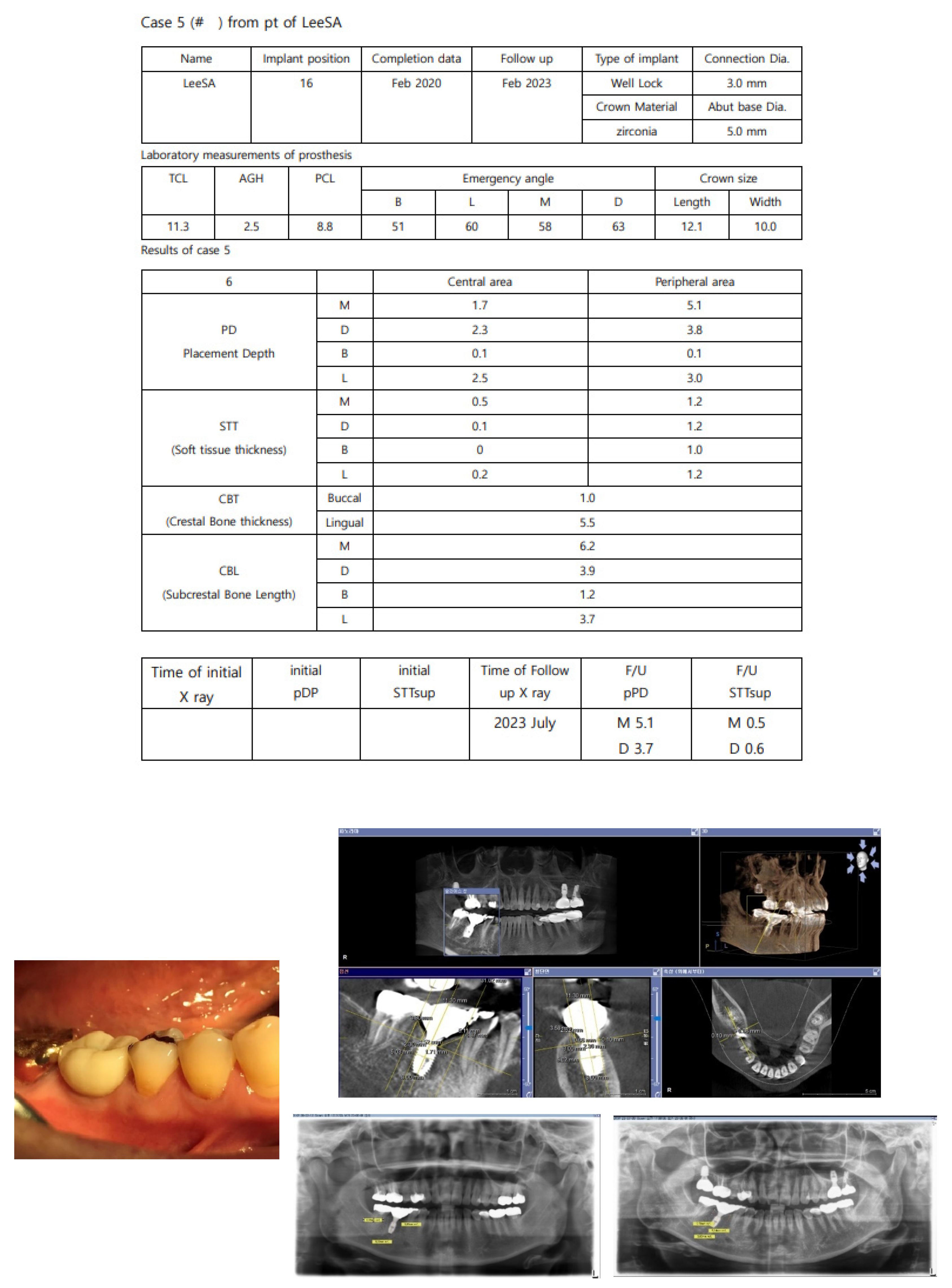
Motivation of this Report as to Seek for Biological Foundation for SPIs
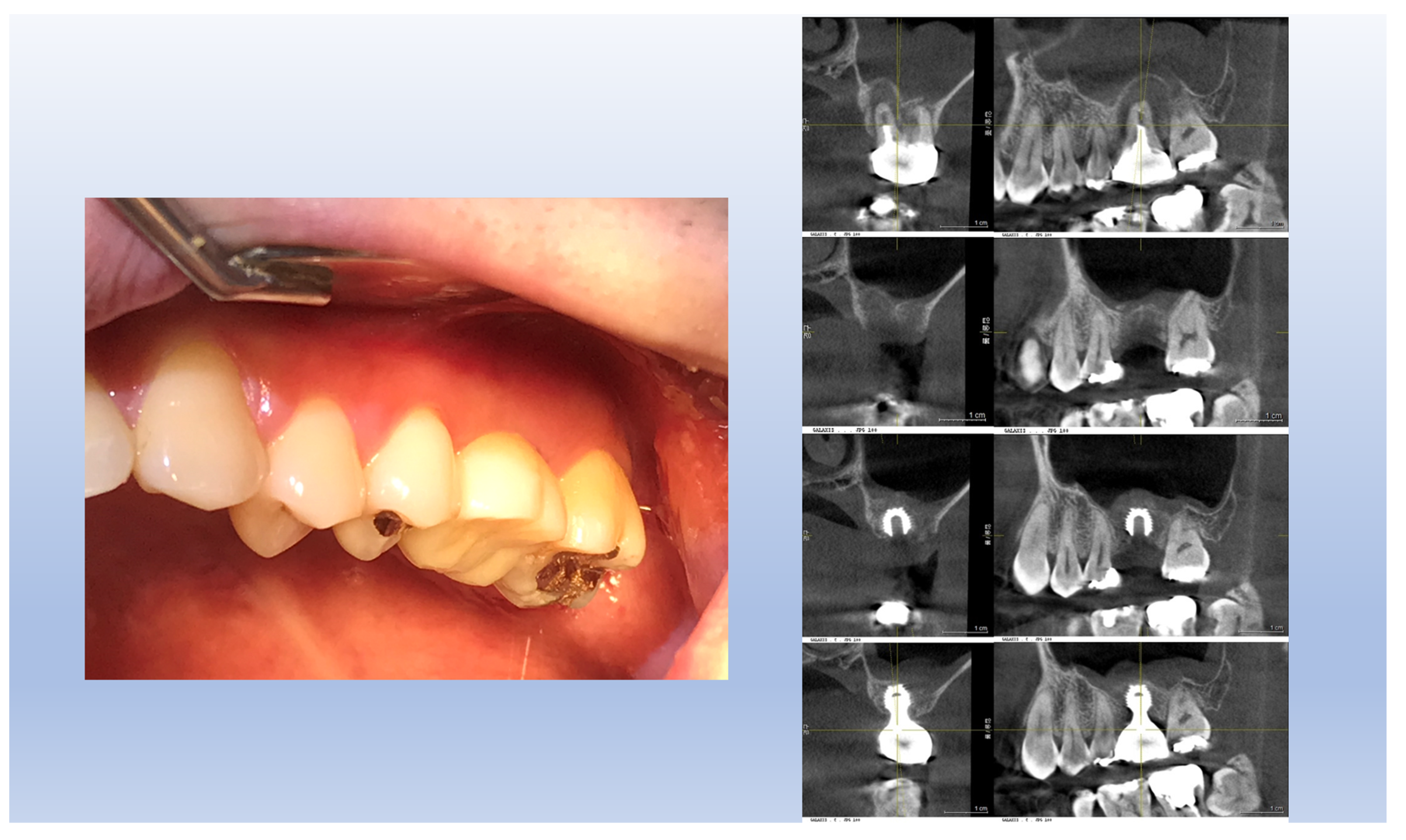
The motivation for this report is to explore the biological foundations for Subcrestally Placed Implant (SPI) techniques, particularly when fixtures are placed more subcrestally than conventional biologic width considerations might anticipate. This approach raises questions about the stability of such placements, which this report aims to address by investigating the clinical results of subcrestally placed IPS design implants.
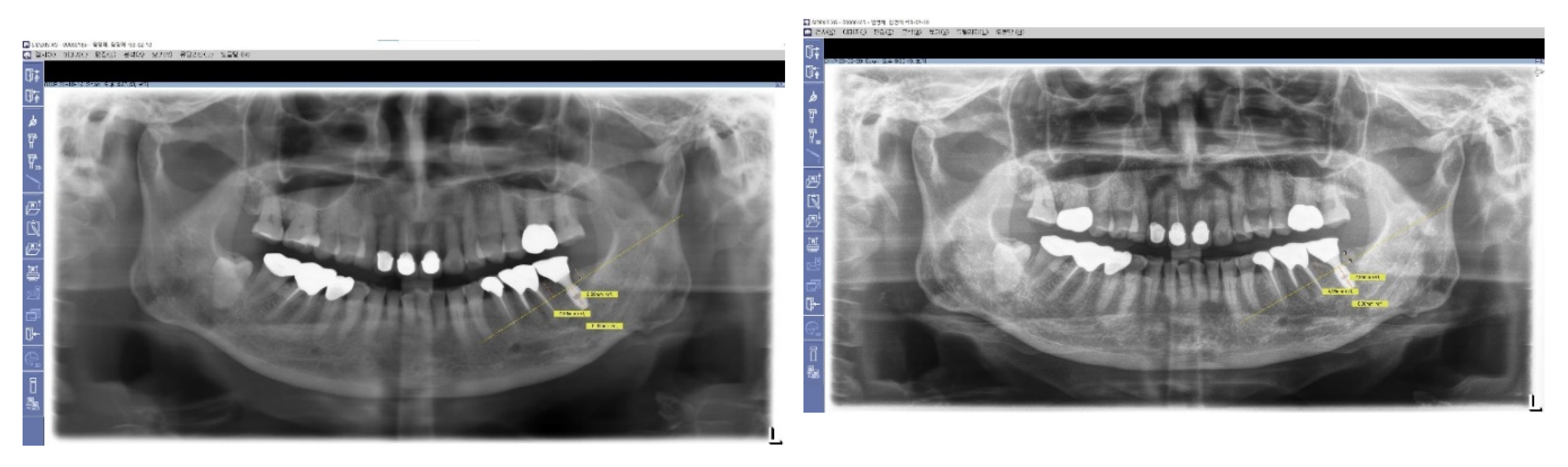
Typically, a plain X-ray (panoramic view, or standard oral) is recommended for routine follow-up examinations to assess the outcomes of implant placements. However, using plain X-rays to observe the depth of an implant fixture and to study its relationship with surrounding tissues (bone and soft tissue) is limited, as this imaging modality only provides information on the mesiodistal relationship. Occasionally, while plain X-rays may indicate that implant fixtures are placed very deep, further examination using Cone Beam Computed Tomography (CBCT) can reveal that the buccal depth of implant placement is actually epi-crestal.
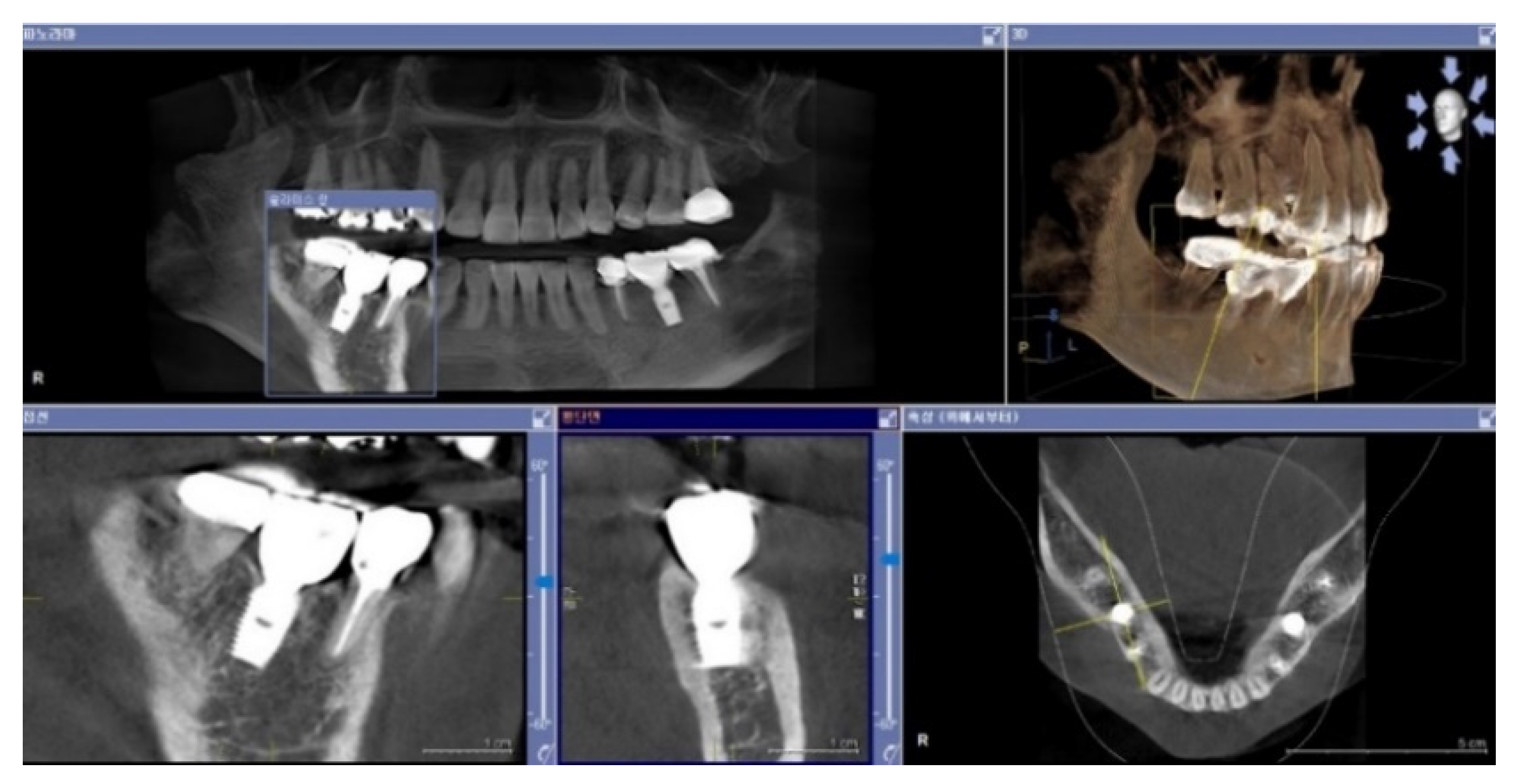
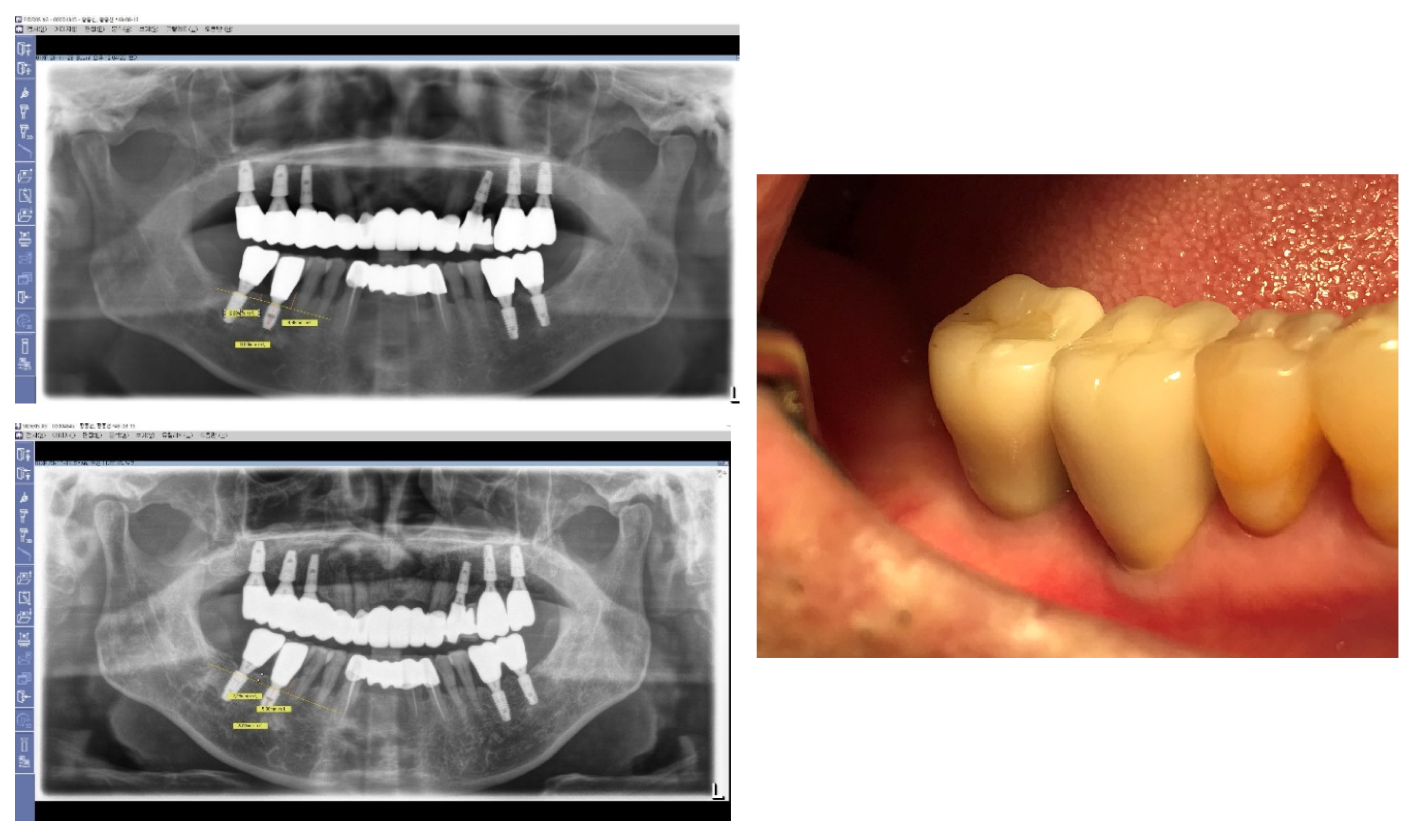
In this study, images from CBCT reviews were utilized for a 3-dimensional analysis to investigate not only the mesiodistal aspects but also the buccal and lingual sides, examining the relationship between the artificial implant complex (implant fixture, abutment, and crown) and the biological tissues (bone and soft tissue).
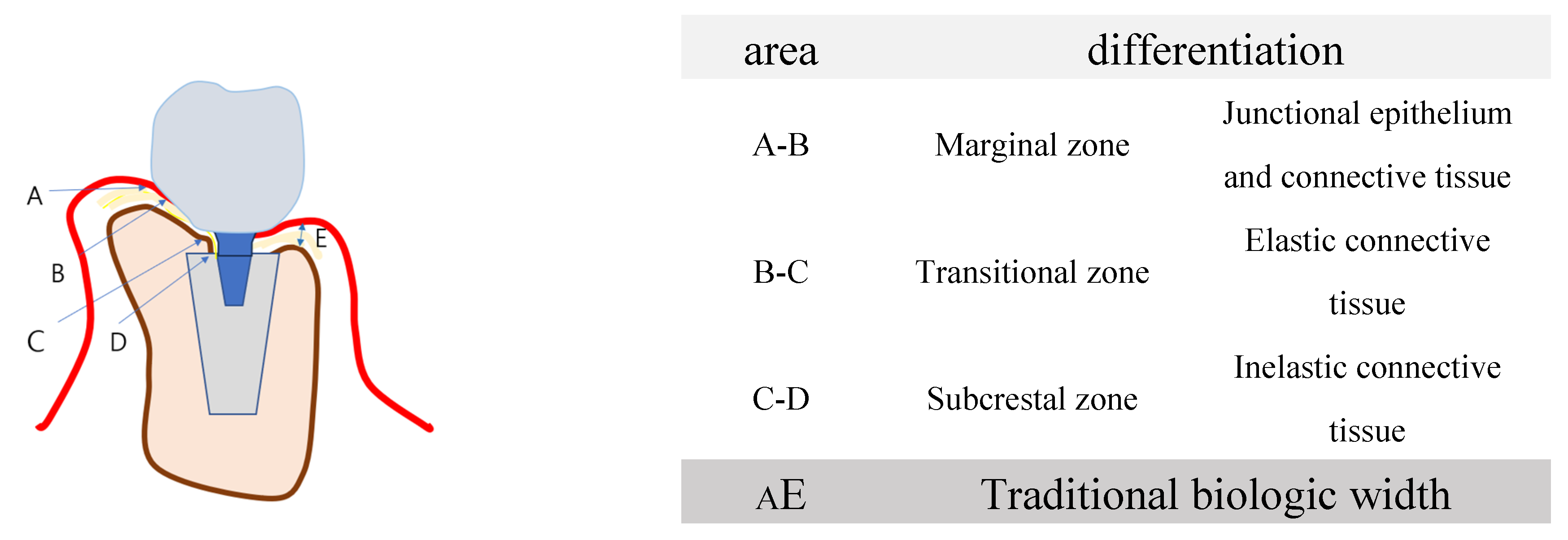
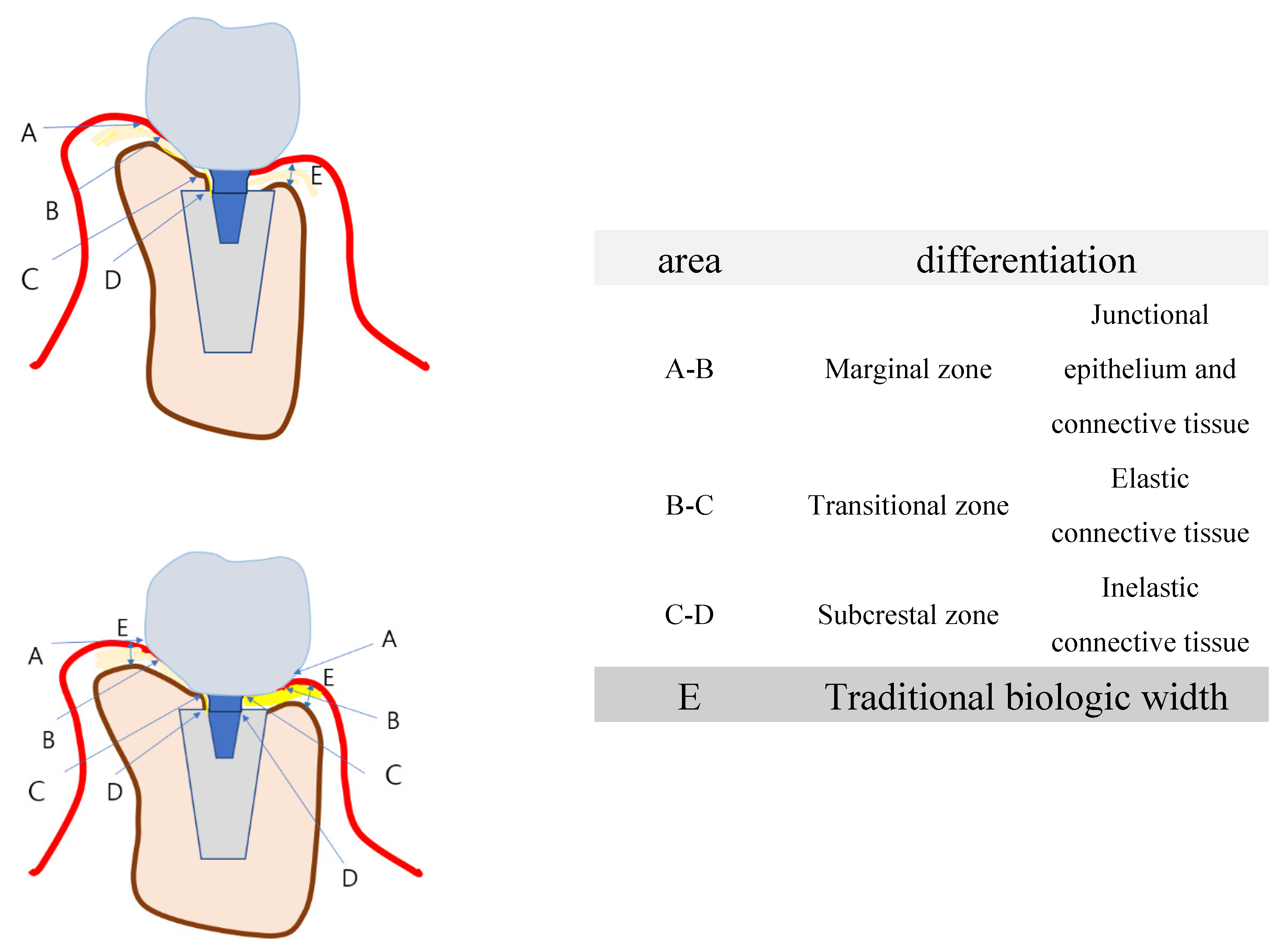
3. -Dimensional Classification of the Soft Tissue around Implants for 3DSTA
The traditional model for biologic width faces some limitations in explaining the relationship between the soft tissue and bone with subcrestally placed implants in a three-dimensional manner. For the purpose of this study, the soft tissue around implants has been categorized into three distinct zones: 1) Marginal Zone, 2) Transitional Zone, and 3) Subcrestal Zone. The dimensions of the Transitional Zone and the Subcrestal Zone were measured for their width and length using CBCT.
Ramon Gomez-Meda et al. proposed the "esthetic biologic contour" concept for implant restoration emergency profile design, in which the subgingival contour is divided into three zones: Zone E for esthetic conditioning composed of sulcus epithelium, Zone B for biologic boundary area composed of junctional epithelium, and Zone C for crestal bone stability composed of connective tissue.^[
4] However, there are notable differences between his division and the classifications in this article regarding the boundaries of each zone and the approach to managing the connective tissue area in relation to the position of implants and the design of the prostheses for SPIs.
Figure 6.
Schematic Drawing of Submucosal Soft Tissue Zones. This figure presents a schematic drawing that differentiates the submucosal soft tissue around implants into three zones: 1) Marginal Zone, 2) Transitional Zone, and 3) Subcrestal Zone.
Figure 6.
Schematic Drawing of Submucosal Soft Tissue Zones. This figure presents a schematic drawing that differentiates the submucosal soft tissue around implants into three zones: 1) Marginal Zone, 2) Transitional Zone, and 3) Subcrestal Zone.
Evaluating Soft Tissue around Implants: Limitations and Techniques
There are limited clinical methods available for examining soft tissue around implants beyond probing the depth of the sulcus. Probing, especially around curved sulci with a metal probe, is challenging, and no universally accepted standard values exist for the sulcus depth of subcrestally placed implants. Despite these challenges, Subcrestally Placed Implants (SPIs) are highly valued for achieving the ultimate aesthetic goals in implantology. Numerous clinical reports affirm the positive outcomes of SPIs from a biological perspective. However, the traditional concept of biologic width, typically viewed in a two-dimensional context, falls short in accurately depicting the phenomena occurring around SPIs. This limitation may cause the deep positions after SPIs to be viewed negatively, despite positive clinical outcomes, thus necessitating a reevaluation to address the complexities of soft tissue dynamics around implants. This is particularly relevant given the long-term clinical data indicating that subcrestally placed implants can remain stable without clinical signs and symptoms of peri-implantitis or peri-implant mucositis.
The purpose of this report is to address these shortcomings and to provide a more comprehensive explanation of the phenomena around SPIs.
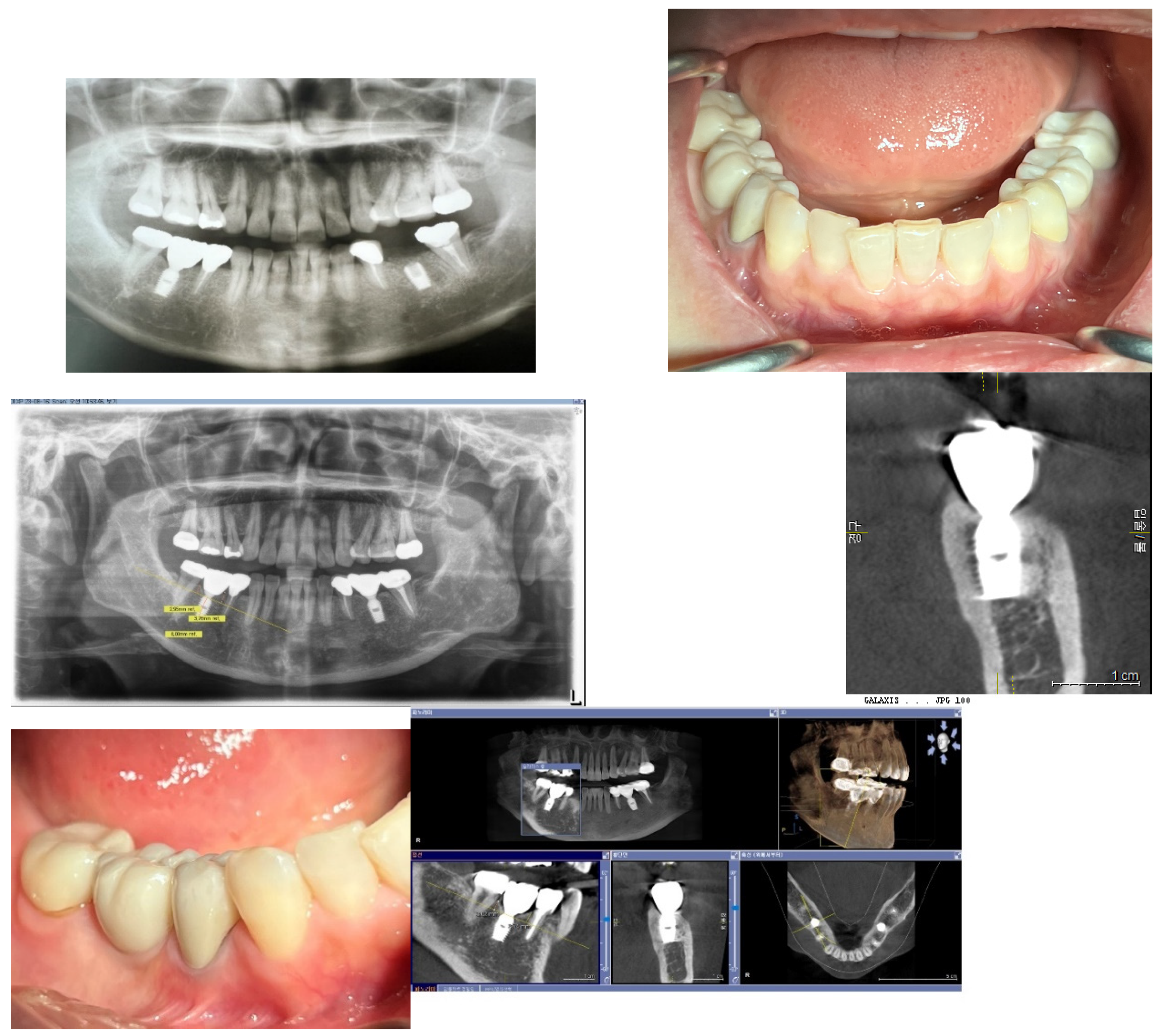
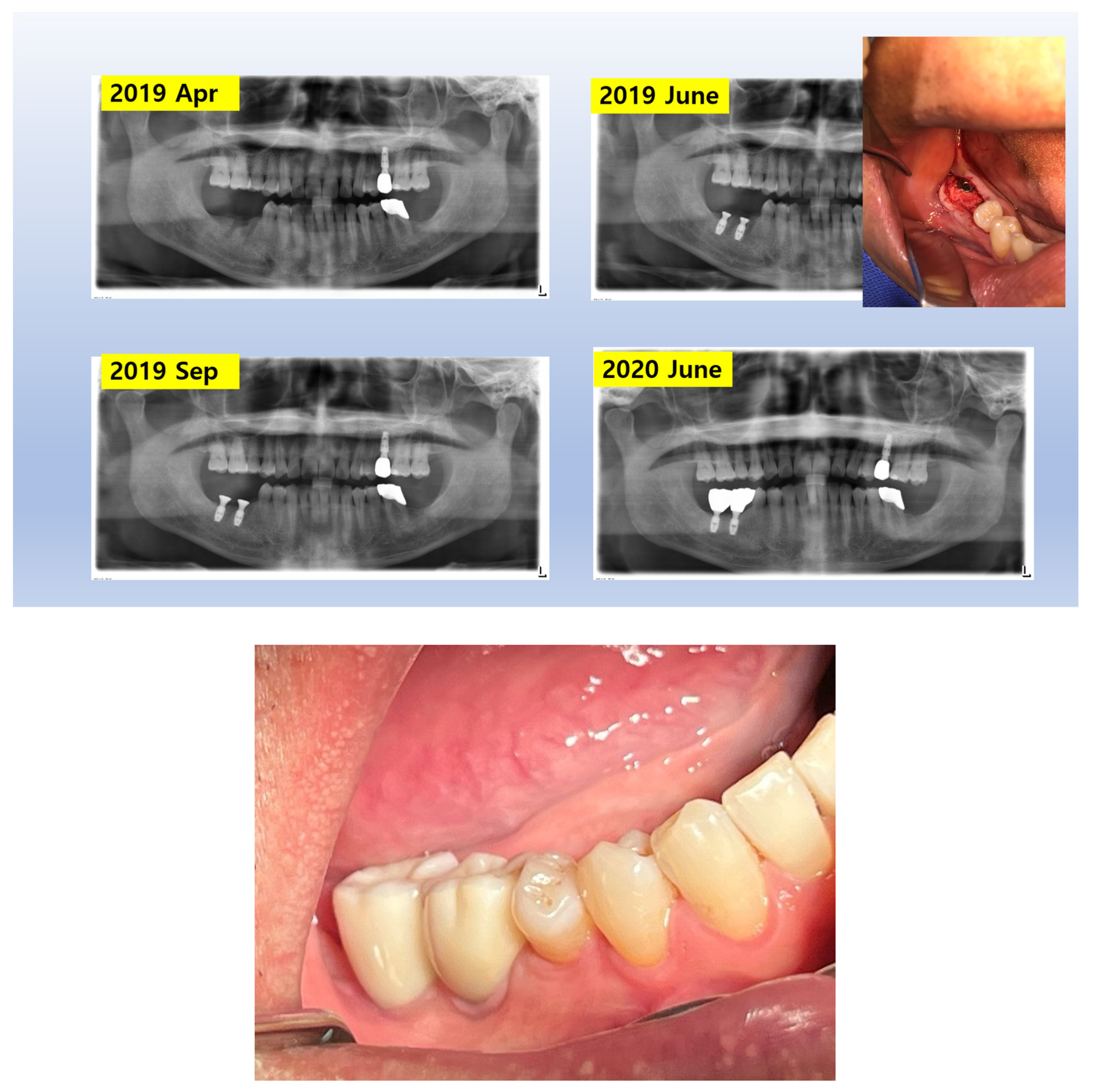
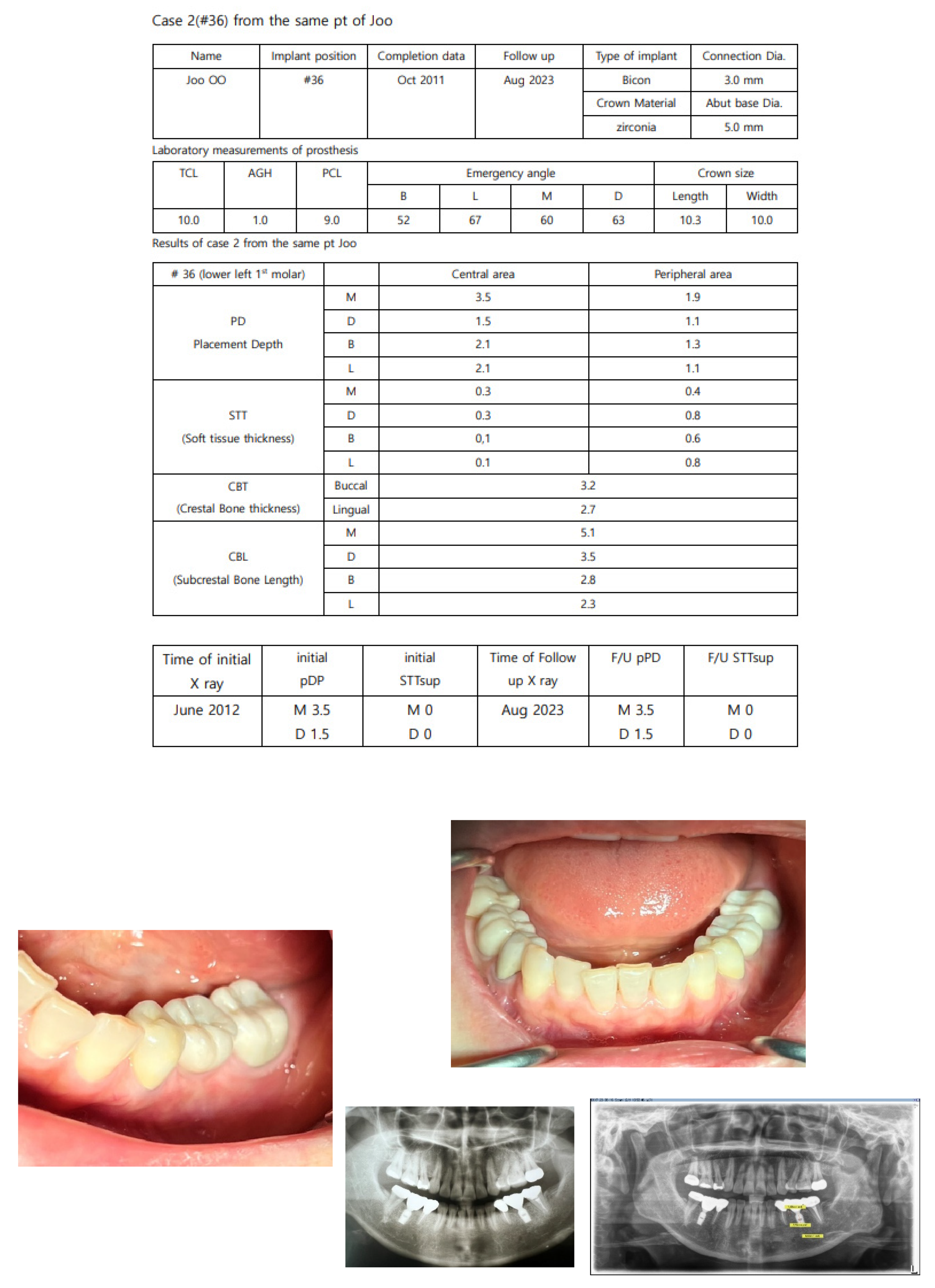
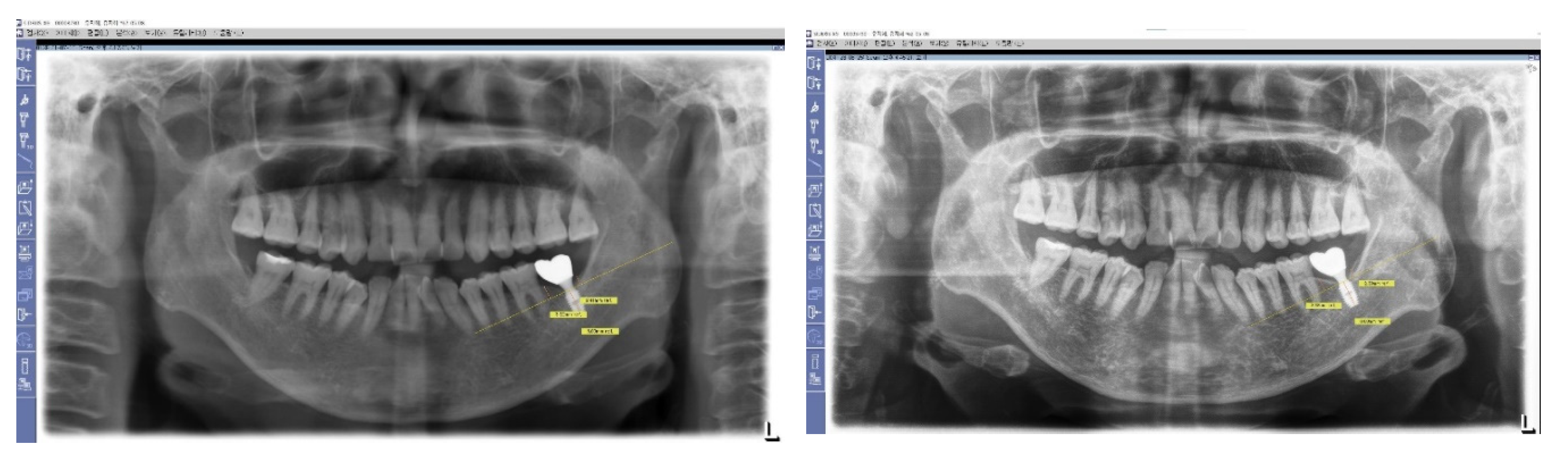
Figure 7.
Long-Term Stability of Lower First Implants. This figure displays a panoramic view X-ray taken in 2023, showing the stable results of both lower first implants that were placed in 2012. These implants, which utilize Subcrestally Placed Implants (SPI) with Internal Platform Switching (IPS) design (specifically Bicon implants), demonstrate long-term stability and successful integration.
Figure 7.
Long-Term Stability of Lower First Implants. This figure displays a panoramic view X-ray taken in 2023, showing the stable results of both lower first implants that were placed in 2012. These implants, which utilize Subcrestally Placed Implants (SPI) with Internal Platform Switching (IPS) design (specifically Bicon implants), demonstrate long-term stability and successful integration.
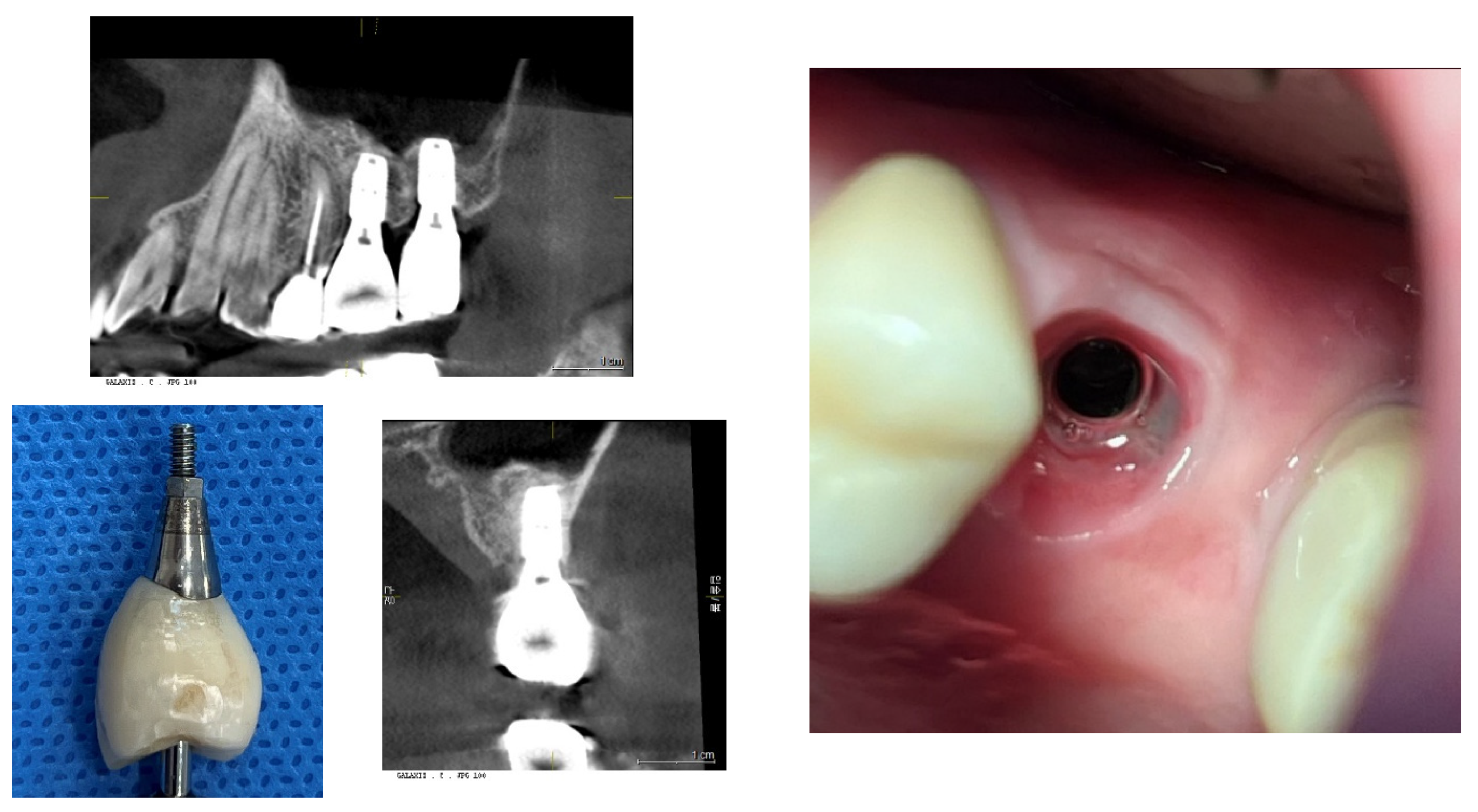
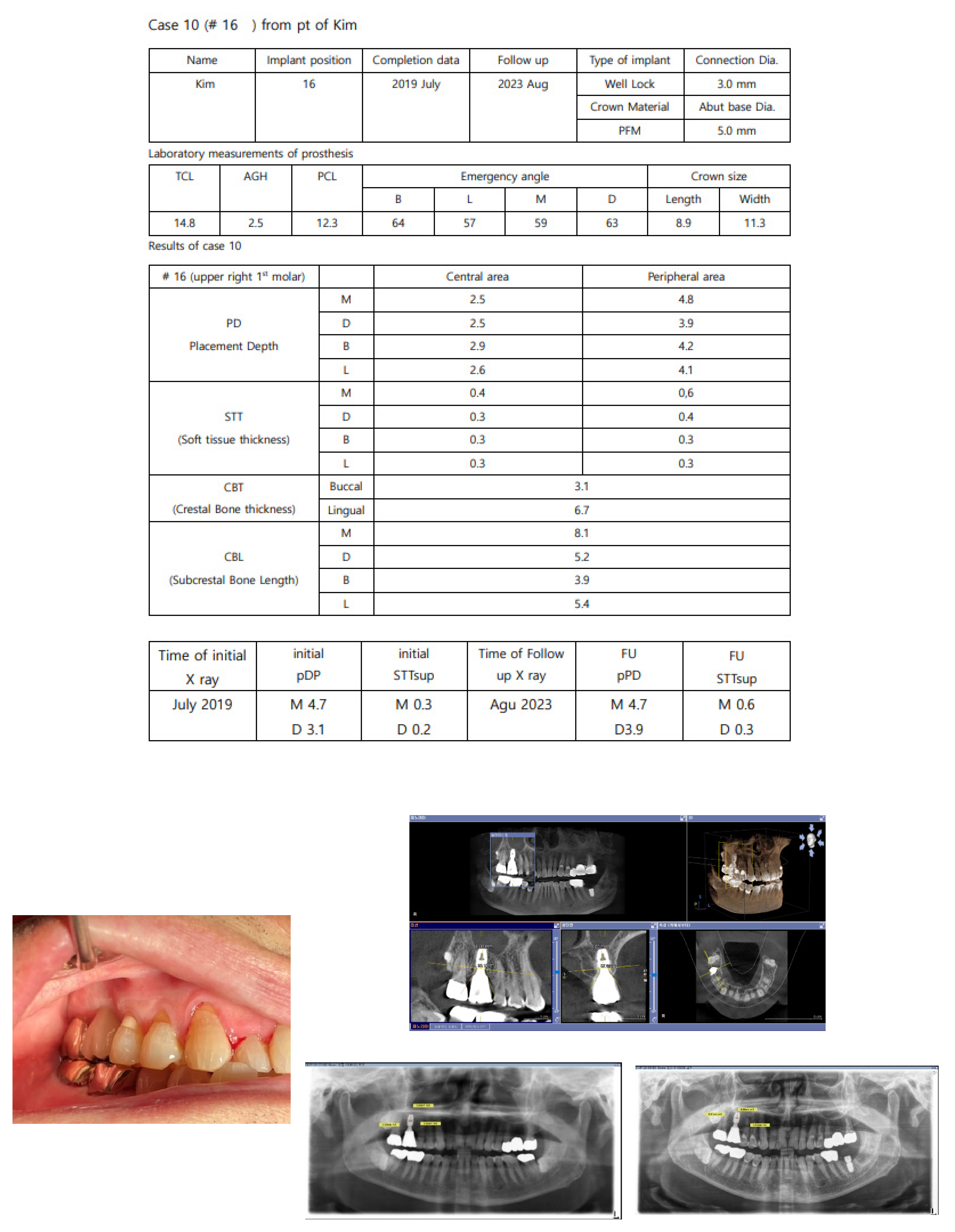
Data Collection
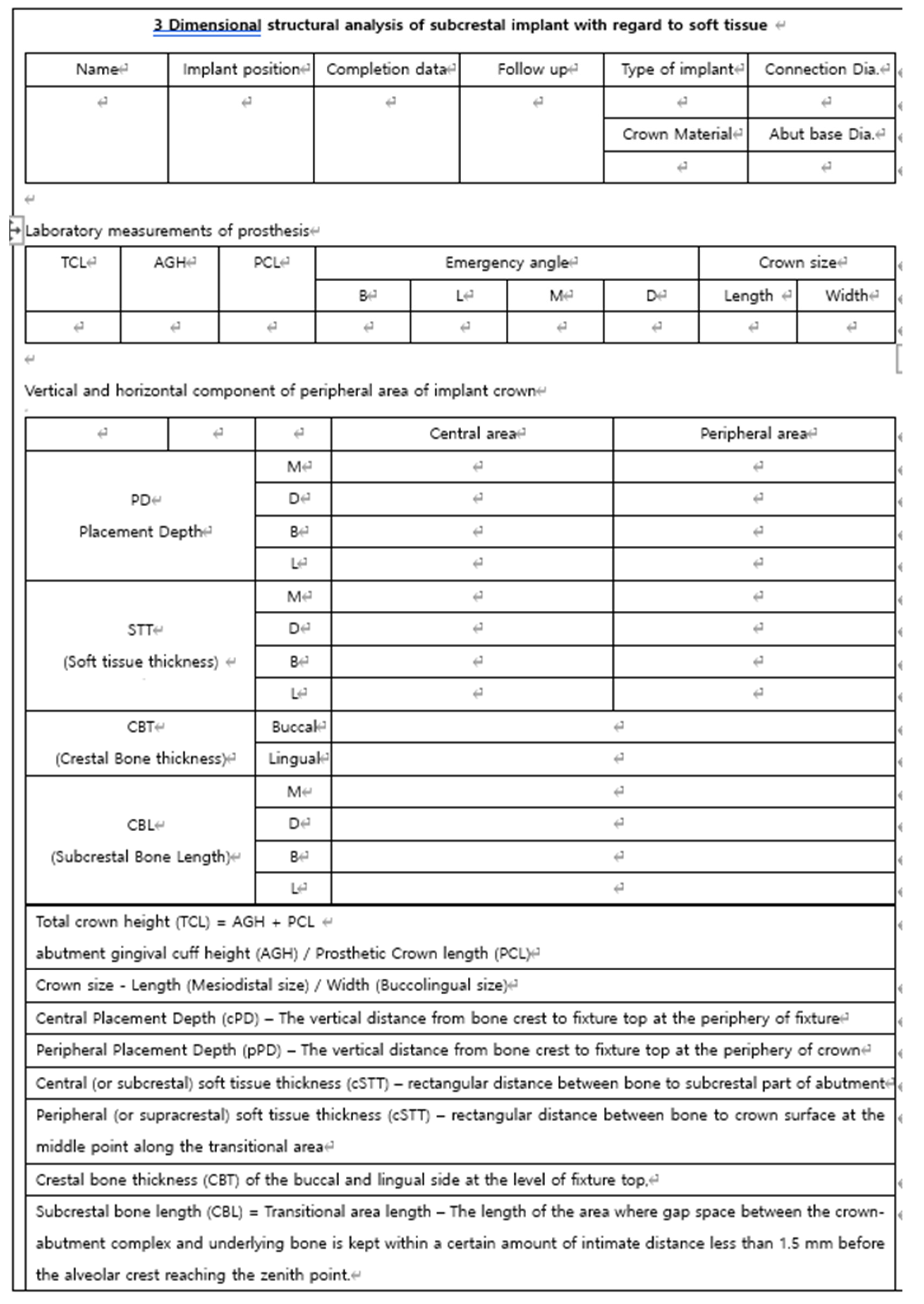
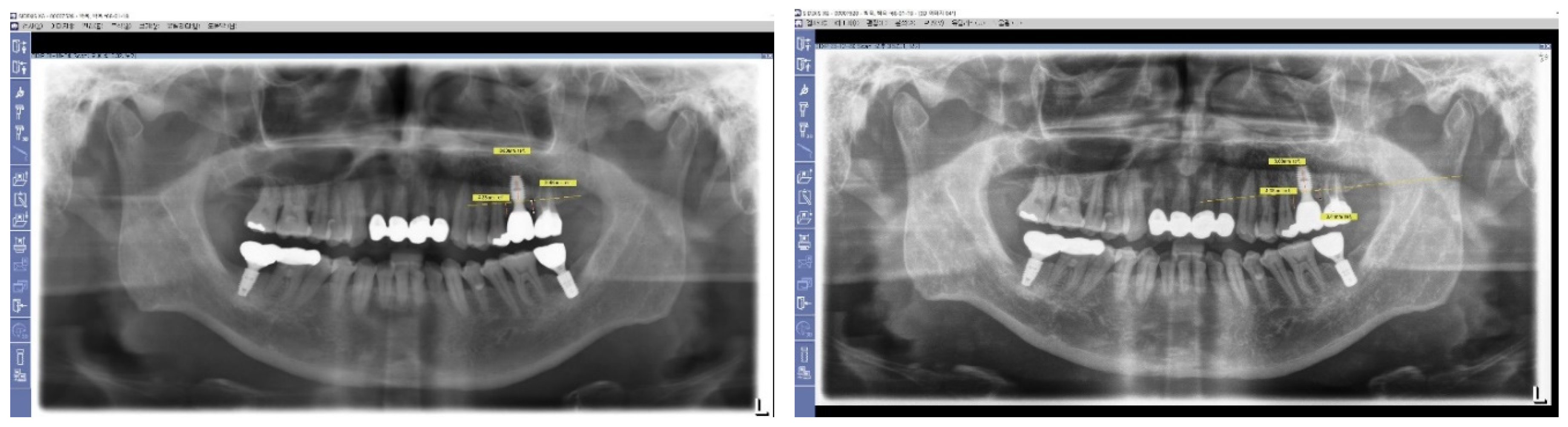
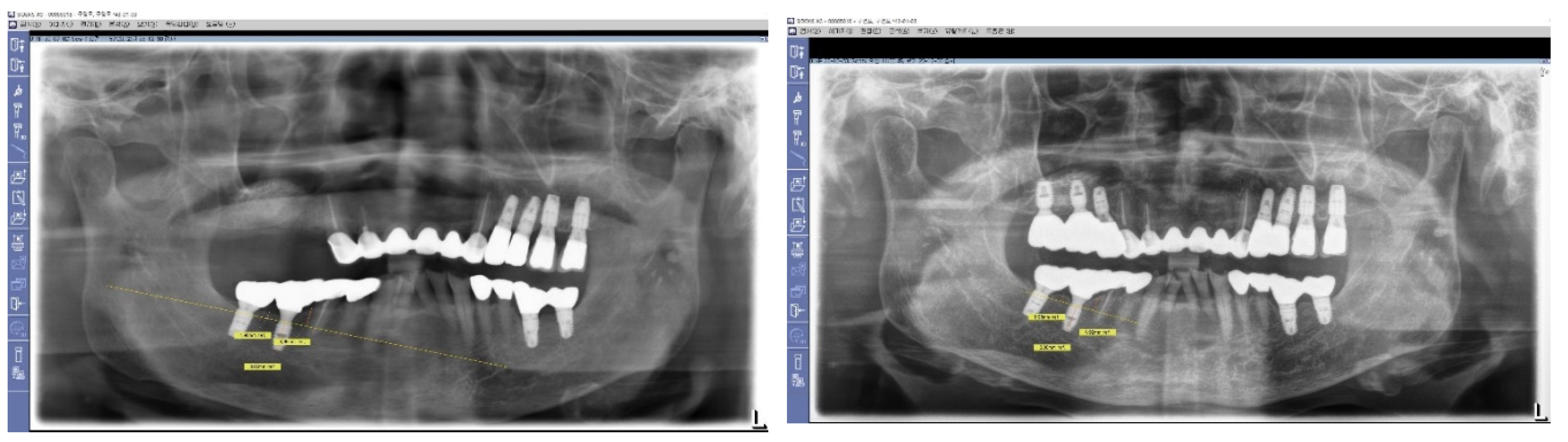
Figure 10.
Measurement Items Recorded from CBCT. This figure outlines the specific items used for recording measurements from the CBCT scans of each patient, enhancing understanding of the data collection process used for analysis.
Figure 10.
Measurement Items Recorded from CBCT. This figure outlines the specific items used for recording measurements from the CBCT scans of each patient, enhancing understanding of the data collection process used for analysis.
Procedures for Measurement
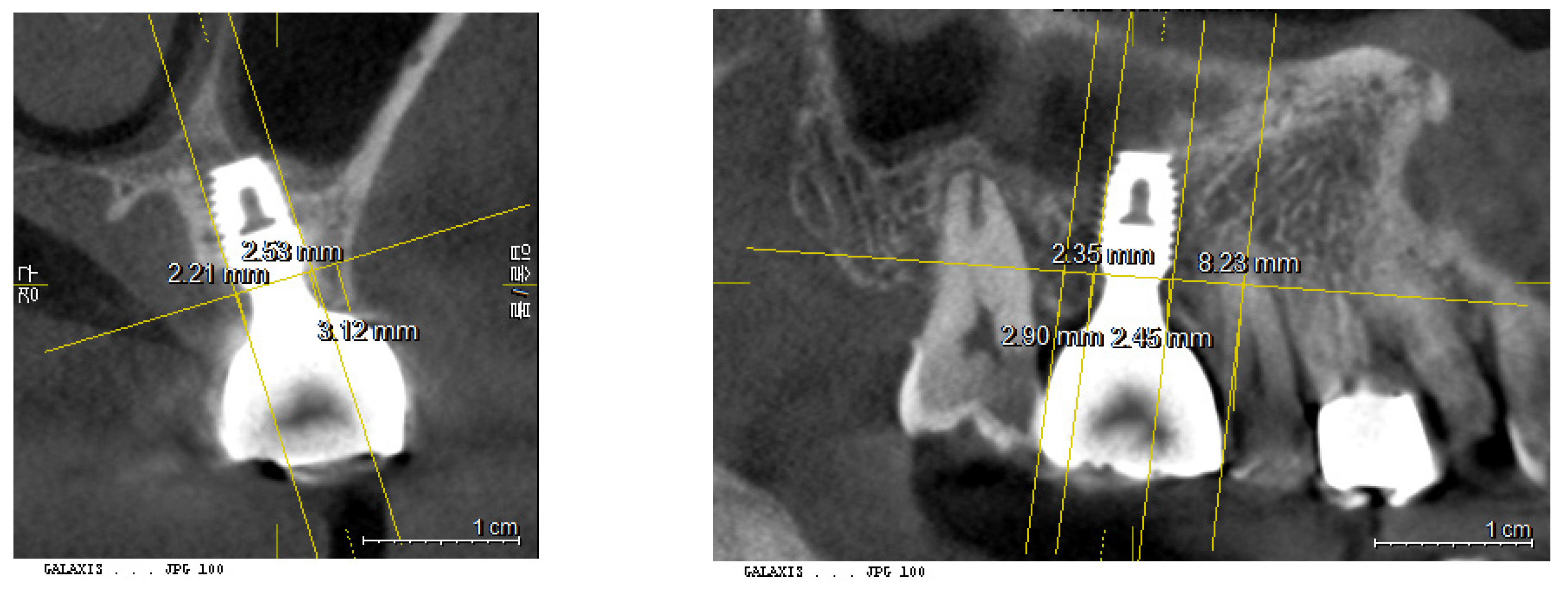
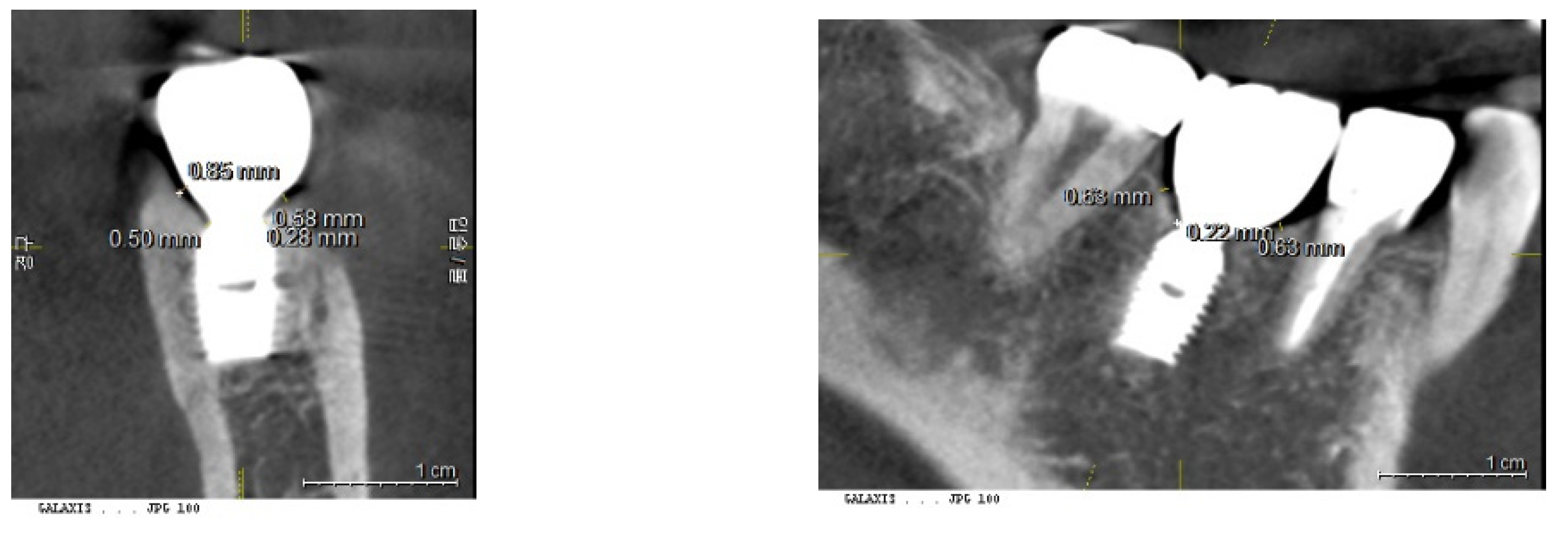
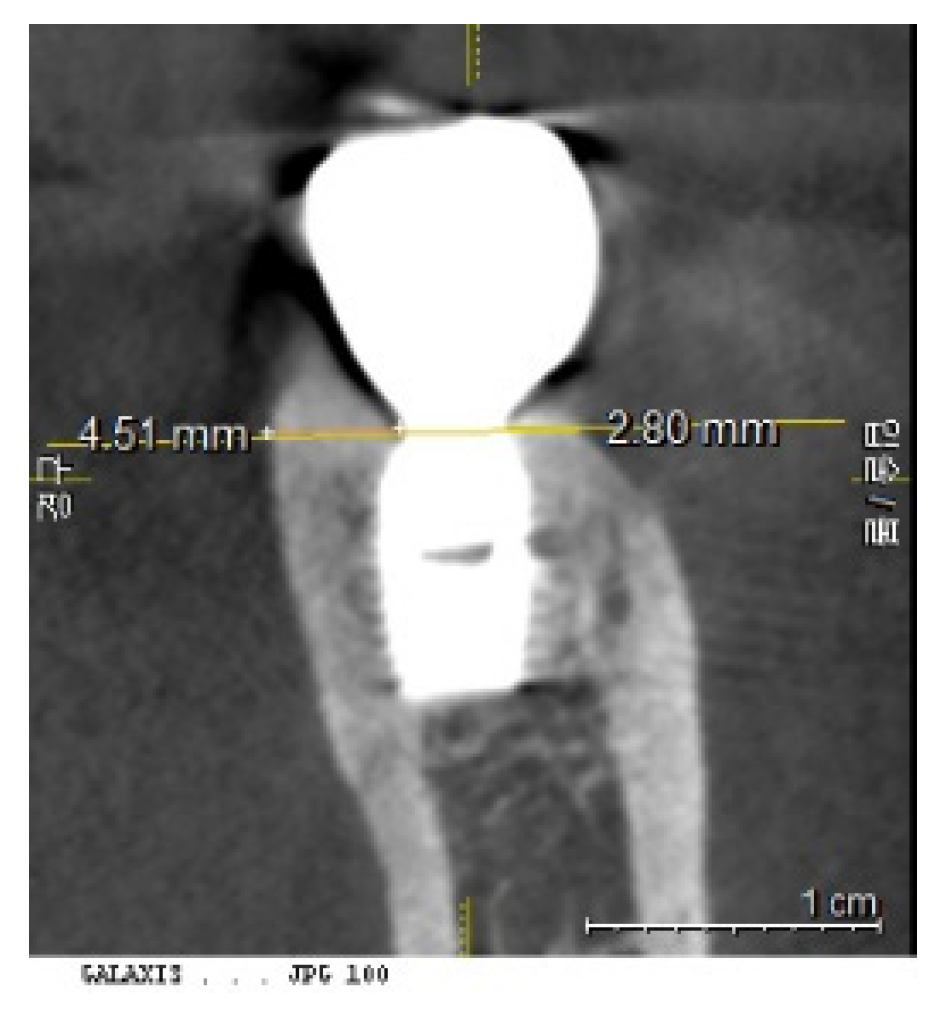
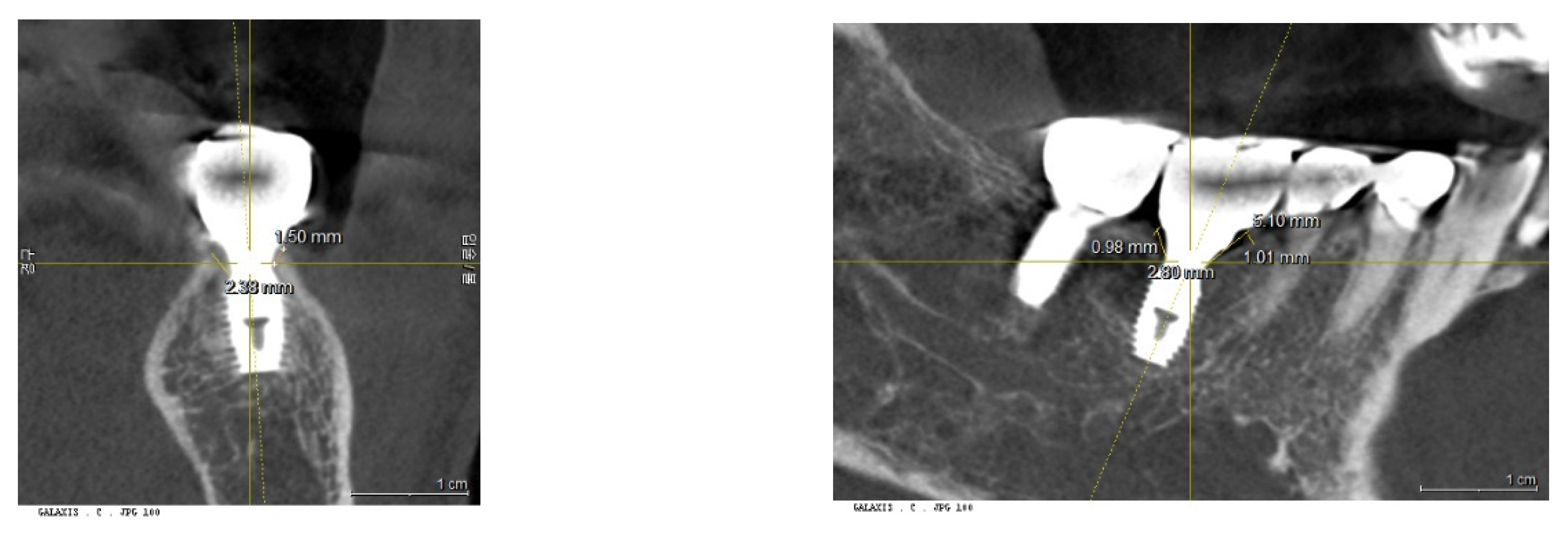
Measurements from the panoramic views and CBCT were conducted using Sirona Dental Systems (Device: XIOX Plus ORTHOPHOS_XG_3D; Programs: SIDEXIS, GALILEOS Implant Viewer; Version 1.9.5605.25519 ID7).
Calibration of CBCT: To ensure accuracy, the presentation plane of the CBCT was centered around the long axis of the fixture. This allowed for the confirmation of the fixture's size—both diameter and length—against its known original dimensions.
Figure 11.
Calibration of CBCT Images. This figure demonstrates the calibration process where images are coordinated along the long axis of the fixtures. This alignment is crucial for accurate measurement and analysis, ensuring that the fixture dimensions are accurately reflected in the CBCT images.
Figure 11.
Calibration of CBCT Images. This figure demonstrates the calibration process where images are coordinated along the long axis of the fixtures. This alignment is crucial for accurate measurement and analysis, ensuring that the fixture dimensions are accurately reflected in the CBCT images.
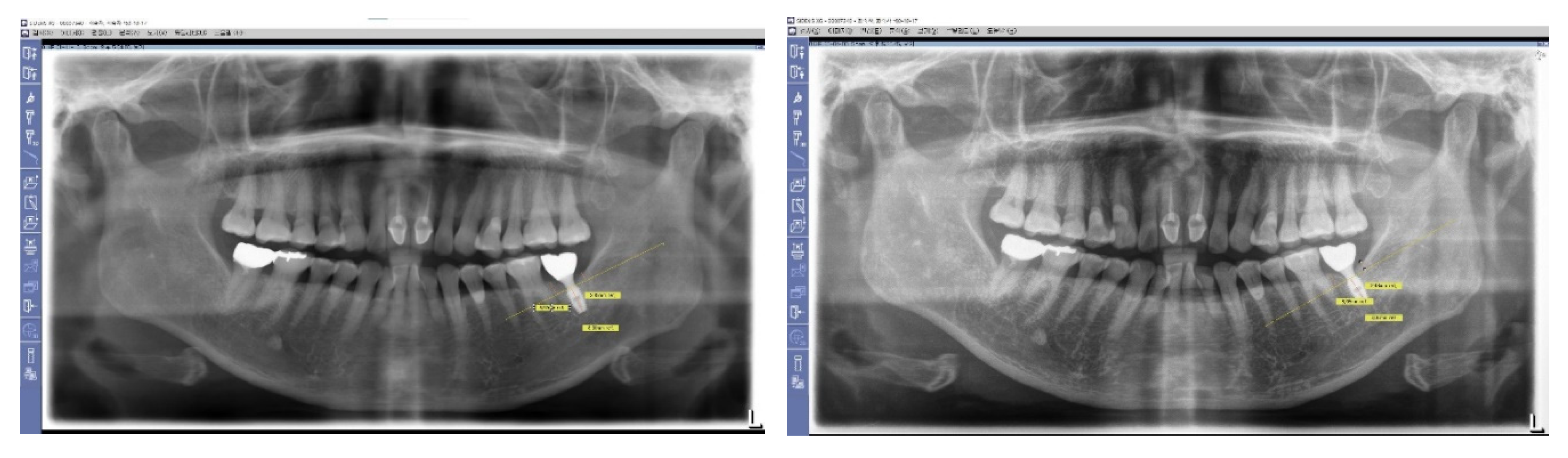
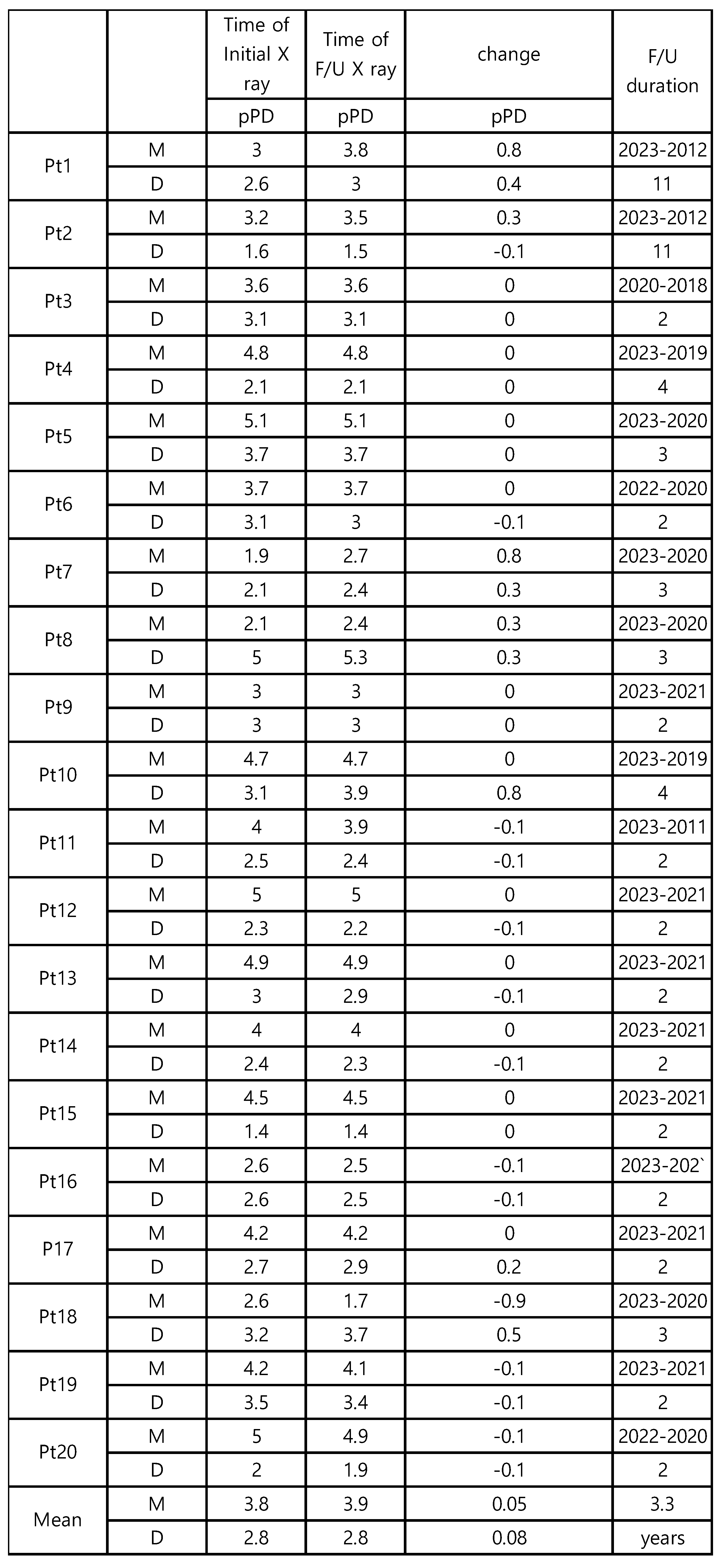
1. Measurement of Peripheral Placement Depth (pPD) from Panoramic View
The Peripheral Placement Depth (pPD) was measured using panoramic views rather than 3-dimensional soft tissue analysis (3DSTA). This involved determining the perpendicular distances from the top of the crestal bone to the top of the implant fixture at both the mesial and distal sides. Measurements were taken after a calibration process utilizing the known fixture length as a reference.
2. Measurement of Placement Depth (PD) from CBCT - 3DSTA
Placement depth was assessed using CBCT in the 3DSTA context, focusing on both the central and peripheral areas in mesiodistal and buccolingual aspects:
a) Central Placement Depth (cPD): - The depth at the central area was measured as the perpendicular distance from the top point of the crestal bone to the platform of the implant fixture at its most outer point (e.g., at the 5 mm point of a 5 mm diameter fixture).
b) Peripheral Placement Depth (pPD) - Mesiodistal and Buccolingual Aspects: - In the mesiodistal aspect, the depth was measured as the perpendicular distance from the top point of the crestal bone to the platform of the implant fixture at the most outer point of the crown. - In the buccolingual aspect, the depth was measured from the most coronal top point of the crestal bone to the platform of the implant fixture.
3. Soft Tissue Thickness (STT) from CBCT - 3DSTA
Soft Tissue Thickness was measured using CBCT, focusing on both the central and peripheral areas, and assessing the dimensions mesiodistally and buccolingually. This measurement is crucial for understanding the vertical component of the soft tissue surrounding the implants, analogous to the traditional concept of biologic width.
a) Central Soft Tissue Thickness (cSTT) or Subcrestal STT (STTsub): - Measured as the perpendicular distance from the outer part of the abutment to the adjacent crestal bone at the subcrestal area. It reflects the thickness of soft tissue directly covering the abutment's embedded part, serving as a functional demarcation between the living bone tissue and the external environment, similar to the Schneiderian membrane in the sinus.
b) Peripheral Soft Tissue Thickness (pSTT) or Supracrestal STT (STTsupra): - Measured as the perpendicular distance from the outer part of the crown to the adjacent crestal bone at the supracrestal area. The reference plane used for measuring pSTT is identical to that used when measuring the Peripheral Placement Depth (pPD), ensuring consistency in measurement criteria across different dimensions.
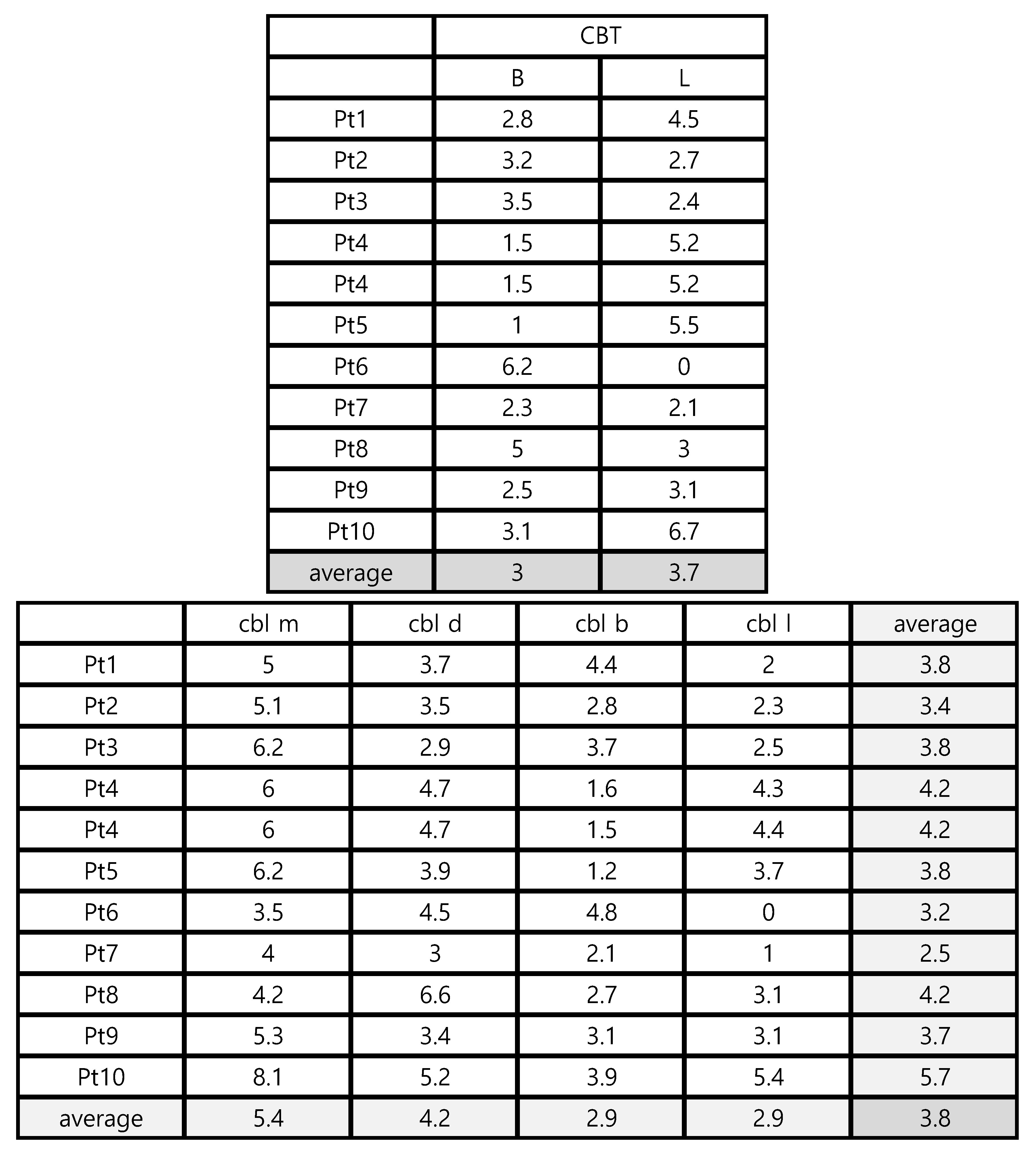
4. Crestal Bone Thickness (CBT) from CBCT - 3DSTA
Crestal Bone Thickness is measured buccolingually, focusing solely on the dimension from the most inner point of the crestal bone contacting the fixture at the level of the fixture top, to the most outer point of the surrounding crestal bone. This specific measurement provides critical information regarding the thickness and health of the bone encompassing the implant, which is vital for assessing the stability and long-term viability of the implant.
5. Crestal Bone Length (CBL) = Transitional Zone Length from CBCT - 3DSTA
Crestal Bone Length, corresponding to the Transitional Zone Length, is measured as long as the peripheral soft tissue thickness between the crown-abutment complex and the surface of the crestal bone is maintained within 1.0 mm. The measurement is taken from the most inner contacting point of crestal bone with the fixture to the most outer point of crestal bone, conducted both buccolingually and mesiodistally. It can be regarded as the horizontal component of the soft tissue surrounding the implants.
Discussion
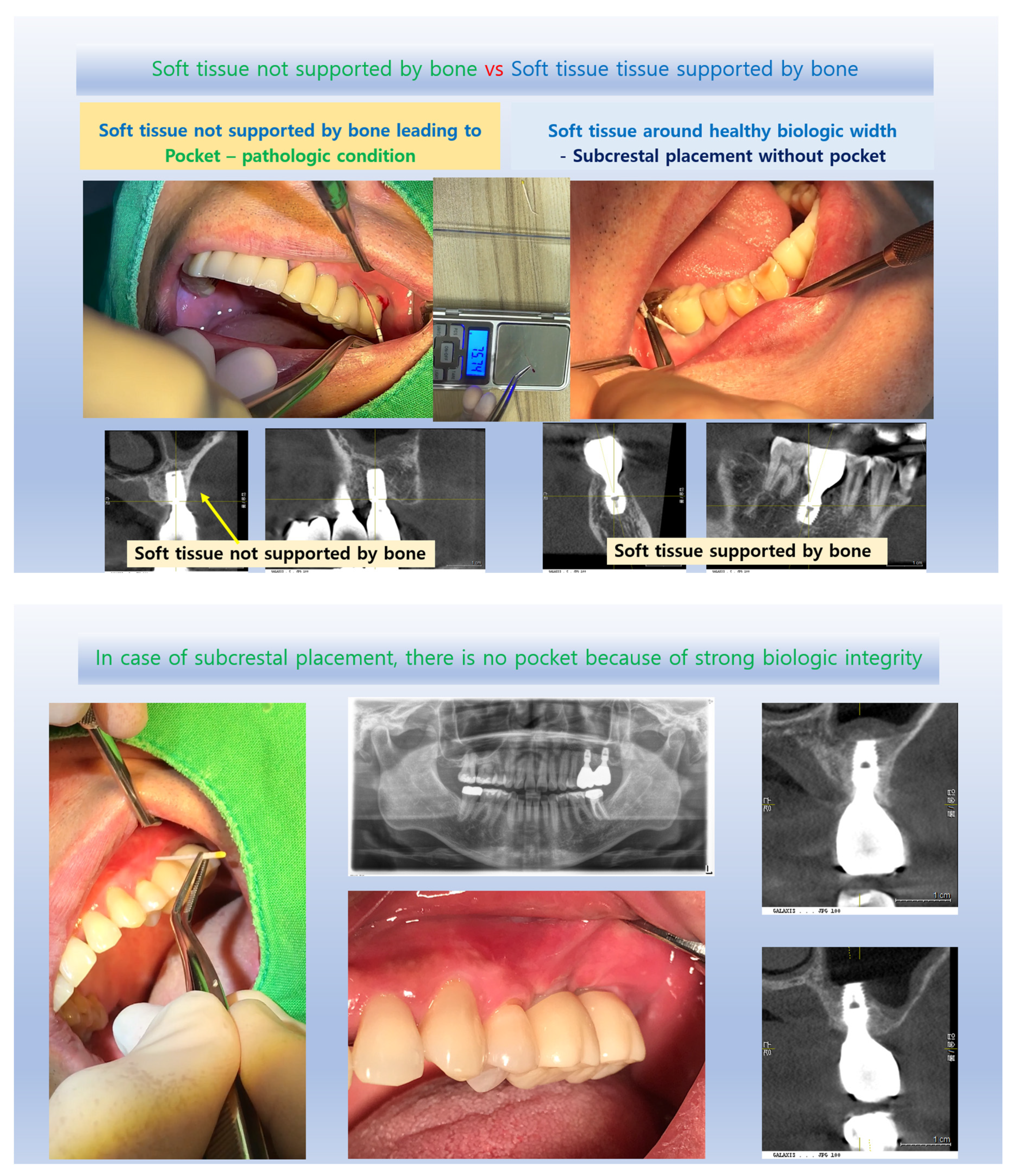
The Necessity of SPI and Its Inevitable Question of Long Soft Tissue (TZ)
Subcrestally Placed Implants (SPIs) with Internal Connection and Platform Switching (IPS) designs are recognized for their potential benefits in enhancing bone stability through the strengthening of soft tissue. However, SPIs also result in a prolonged soft tissue distance beneath the prostheses, which seems to contradict the conventional understanding of a periodontal pocket. This paradox may be partly due to the lack of three-dimensional analysis of the soft tissue beneath the prostheses of SPIs, contributing to ongoing concerns in the field.
The longevity and health of implants largely depend on the absence of peri-implantitis. Therefore, achieving minimal or no bone changes during follow-up periods remains a fundamental objective in implant dentistry. Despite concerns about the significant prevalence of peri-implant mucositis and peri-implantitis, often associated with microbial infections characterized as site-specific, biofilm-mediated host inflammatory responses^[
15,
16], the findings from my study are encouraging, showing almost no bone changes over several years. These results suggest that SPIs, when properly managed, may effectively mitigate some of the traditional risks associated with biological width.
Early Crestal Bone Loss and Biologic Width
Early crestal bone loss (EBL) has been attributed to several factors, but a significant cause is the need to accommodate biologic width^[
16]. Creating a favorable biological environment that makes implants immune to microbial infection is crucial for the ultimate success of implants in biological terms. Additionally, achieving an aesthetically pleasing appearance and appropriate function is closely tied to the design of the prosthesis^[
17].
This relationship underscores the complexity of implantology, where each aspect of implant design and placement must be carefully considered to balance aesthetic outcomes with long-term biological stability.
Having Natural Crown Shape and Size
Proper implant prosthetic design, including appropriate size, allows implant crowns to function like natural teeth by effectively transferring masticatory forces and offering an aesthetically pleasing appearance. The implant prosthesis can be divided into supramucosal and submucosal parts. The supramucosal part, which is the visible crown, plays a crucial role in aesthetics. If this part harmoniously matches the neighboring natural teeth in terms of size, color, and morphology, it can seamlessly blend in, appearing entirely natural. For the crown to be perceived as natural, its diameter must correctly match that of natural teeth from the cervical area—the starting point of the supramucosal part.
Emerging Phenomenon in Implant Design
The emerging phenomenon observed in dental implants is primarily due to the horizontal distance between the crown diameter and the abutment-fixture connection diameter at the submucosal level. This spatial difference allows the crown to transition smoothly from the narrower abutment to the broader coronal structure, mimicking the natural contour of teeth where the crown gradually flares out from the gum line.
In contrast, certain types of tissue-level implants that exhibit no significant diameter difference between the implant fixture (or abutment/fixture junction) and the crown do not demonstrate this emerging phenomenon. This design more closely resembles natural teeth, which typically show minimal diameter differences between roots and crowns, thus eliminating concerns associated with the emerging phenomenon in implants.
Figure 12.
mm of facial soft tissue thickness around the final restorations^[
18]. However, these guidelines often overlook the specific requirements for subcrestal soft tissue thickness and do not fully address challenges associated with the emerging phenomenon.
Figure 12.
mm of facial soft tissue thickness around the final restorations^[
18]. However, these guidelines often overlook the specific requirements for subcrestal soft tissue thickness and do not fully address challenges associated with the emerging phenomenon.
Ideally, the bone table of an edentulous crestal ridge should be broad enough to comfortably accommodate an implant of regular diameter (3.5 – 5.0 mm) with adequate marginal crestal bone, allowing uniform placement depth across the implant. However, such ideal conditions are rare in clinical practice^[
19]. More commonly, clinicians face narrower crests that necessitate placing implants subcrestally based on the most apical part of the crest, unless bone grafting is performed. This approach is more reflective of real-world clinical scenarios and underscores the need for careful planning and adaptation to varying anatomical landscapes.
Despite the prevalence of these conditions, there remains a lack of extensive research on the topographic relationship between the implant components (abutment and prosthesis complex) and the biological environment. Such studies are crucial for understanding the long-term biologic integrity and stability of implant structures.
Figure 13.
Unlike a natural gingival sulcus, which is a normal anatomical structure when the periodontium is healthy, a periodontal pocket indicates pathological deepening and is characterized by inflammation, bone destruction, and detachment of the junctional epithelium^[
21]. This difference is crucial in dental practice, as the mere measurement of depth can predispose clinicians to judge the periodontal state as compromised. However, this perspective may be a preconception when analyzing implants, where a longer soft tissue transitional area (sometimes misinterpreted as a pathologic pocket) is often considered undesirable despite clinical evidence showing stable results in deeply placed implants.
Figure 13.
Unlike a natural gingival sulcus, which is a normal anatomical structure when the periodontium is healthy, a periodontal pocket indicates pathological deepening and is characterized by inflammation, bone destruction, and detachment of the junctional epithelium^[
21]. This difference is crucial in dental practice, as the mere measurement of depth can predispose clinicians to judge the periodontal state as compromised. However, this perspective may be a preconception when analyzing implants, where a longer soft tissue transitional area (sometimes misinterpreted as a pathologic pocket) is often considered undesirable despite clinical evidence showing stable results in deeply placed implants.
Three-Dimensional Analysis and Subcrestal Implant Placement: The advent of Cone Beam Computed Tomography (CBCT) and its widespread use in implantology have shown that many implants are placed subcrestally, at least partially, without causing distinguishable pathological issues compared to epi-crestally placed implants^[
12]. A lack of systematic methods for analyzing the submucosal soft tissue around subcrestally placed implants in a three-dimensional way likely contributes to unfounded pessimistic views. Three-dimensional soft tissue analysis (3DSTA) is particularly vital for subcrestal placements known to help reduce bone loss incidence^[
1,
22,
23,
24,
25]. This technique also supports the creation of more natural-looking prostheses by providing sufficient space to offset the diameter difference between crowns and abutment-fixture connections, ensuring an appropriate emergence profile. Some authors have pointed out the limitations of two-dimensional analysis in studying implants and have suggested using micro-computed tomography for more detailed and accurate assessments^[
26].
The Strengthening Effect of the Transitional Zone as a Biological Barrier
The absence of crestal bone change often signifies one of the best outcomes for implants. Traditionally, changes in crestal bone surrounding implants have been extensively studied. However, few reports have analyzed these changes in three-dimensional ways. Subcrestal placement of implants has been reported to offer advantages in terms of bone changes^[
27,
28]. Despite some negative reports about subcrestal placement techniques, these variations can often be attributed to different clinical approaches. For instance, deeply placed implants with excessive distance between soft tissue and abutments may lead to bone resorption due to inadequate mechanical sealing by the soft tissue. Additionally, if excessive cement remnants are not properly removed in subcrestally placed cases, they may lead to peri-implantitis. Previous studies have also included implants with external hex connection designs or matching platform designs, which may affect the relationship between fixture depth and bone loss.
The cases discussed in this article demonstrate the benefits of subcrestal implant placement, particularly when the distance between submucosal implant components and submucosal soft tissue is maintained closely at the Transitional Zone (TZ) and when the extraoral cementation technique effectively addresses issues with excessive cement remnants. Natalia Palacios-Garzon highlights internal connection and platform switching as positive factors for subcrestal placement. Muhammad H.S. Saleh reported that a subcrestal Implant-Abutment Junction (IAJ) position results in slightly less crestal bone loss compared to both supracrestal and equicrestal positions. It can be suggested that the soft tissue around the subcrestal implants may have a strengthening effect on the biologic width^[
8,
28].
Michitsuna Katafuchi et al. noted that an emergence angle greater than 30 degrees is a significant risk indicator for peri-implantitis, and a convex profile poses additional risks for bone-level implants^[
29]. The emergence angle, designed to create a natural-looking appearance of implant restorations, is correlated with the depth of implant placement. Insufficient placement depth results in an unfavorable emergence angle, restricting space for the soft tissue environment. In this study, the average emergence angle was 32 degrees. Deeper placement contributes to achieving such a gradual angle. However, it is necessary to further elucidate how the varying environments of surrounding soft tissue can influence the determination of the emergence angle. The author postulates that the emergence angle might be favorably altered in relation to the soft tissue, depending on the topography, particularly when there is ample soft tissue with sufficient blood supply (for instance, an emergence angle of 60 to 30 degrees might be acceptable under these conditions).
The Role of Epithelial Health and Integration in Dental Implant Success
The successful healing and maintenance of epithelial and connective tissues around dental implants are critical to the overall success of the implant^[
30]. Epithelial downgrowth, a natural immune response to protect against pathogens, occurs to compensate for the disruption of tissue integrity, typically following accidents or surgical interventions. This process, known as epithelialization, is a primary response for repairing damaged tissues and is not harmful in itself.
However, unlike natural tissues, the structures around dental implants are artificially created and require integration into the body's systems to be considered healthy. This integration involves establishing a form of structural integrity that includes adequate blood supply, normal physiological function, and an immune defense mechanism. For implants, this integrity must be maintained without disruption to prevent unhealthy epithelial downgrowth, despite the inherently longer and broader soft tissue barriers around implants compared to natural teeth.
Figure 14.
This focused source means that a larger soft tissue area receiving blood from the alveolar bone results in healthier tissues, reducing susceptibility to inflammation and resistance to bone loss. This is particularly beneficial since dental implants inherently lack connective tissue attachment and have a poorer blood supply due to the absence of periodontal ligaments. The enlarged TZ in subcrestal placements can compensate for these disadvantages by strengthening the biologic width.
Figure 14.
This focused source means that a larger soft tissue area receiving blood from the alveolar bone results in healthier tissues, reducing susceptibility to inflammation and resistance to bone loss. This is particularly beneficial since dental implants inherently lack connective tissue attachment and have a poorer blood supply due to the absence of periodontal ligaments. The enlarged TZ in subcrestal placements can compensate for these disadvantages by strengthening the biologic width.
Figure 15.
Similarity in Biologic Width Between Implants and Natural Teeth. When healing abutments or similar structures are placed without horizontal widening, the soft tissue around implants parallels the biologic width of natural teeth. In such cases, the biologic width closely matches the thickness of the adjacent surface mucosa. This alignment is particularly noted with the use of external hex connection type implants.
Figure 15.
Similarity in Biologic Width Between Implants and Natural Teeth. When healing abutments or similar structures are placed without horizontal widening, the soft tissue around implants parallels the biologic width of natural teeth. In such cases, the biologic width closely matches the thickness of the adjacent surface mucosa. This alignment is particularly noted with the use of external hex connection type implants.
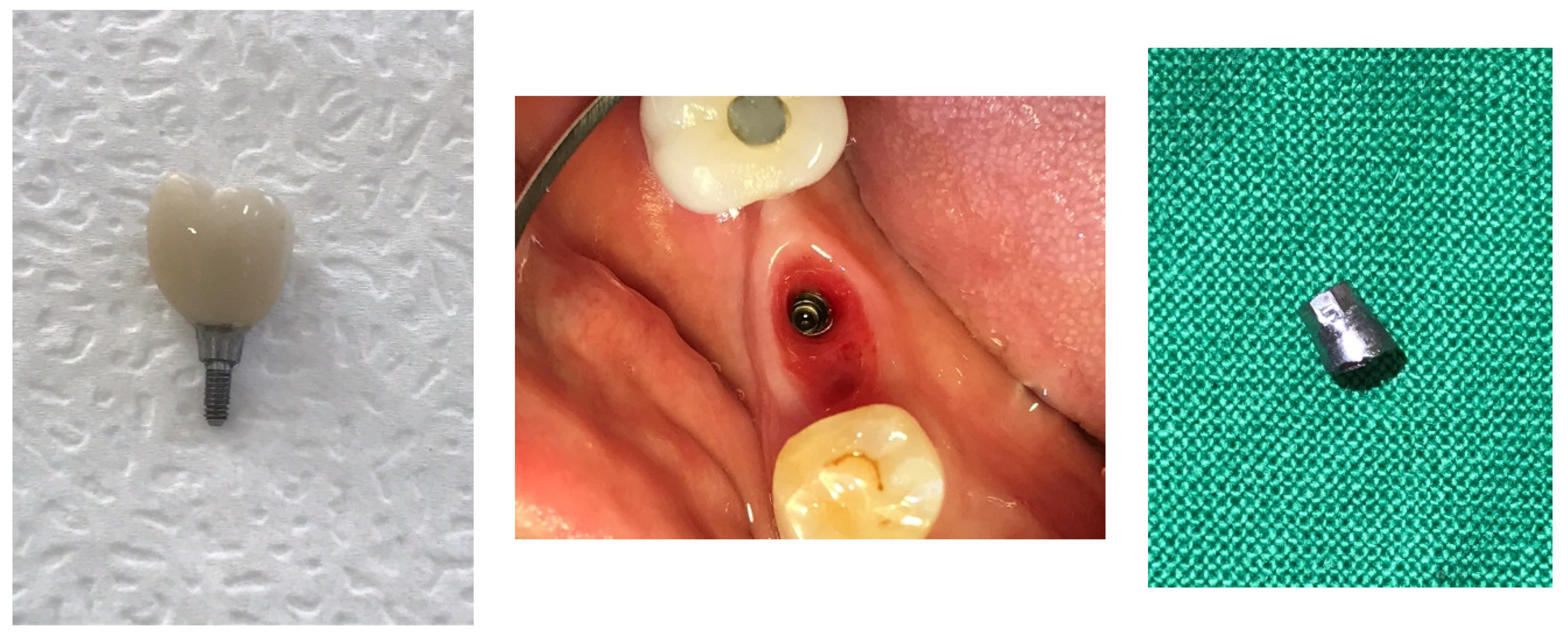
Biologic Width Observations and Shifts in Implant Design
At sites where healing abutments or prostheses lacking horizontal extensions for an emergence profile are placed on flat and broad crestal bones, dentists could observe a biologic width that closely matched that of natural teeth. This alignment was particularly noted with the use of external hex connection type implants. Today, however, such scenarios are less common with Subcrestally Placed Implants (SPIs), especially in posterior positions. This change is due to a perceived weaker biologic sealing effect than the biologic sealing effect in SPIs, attributed to a narrower soft tissue sealing area that provides less blood supply. This reduction in vascular support potentially compromises the long-term stability and integration of these implants.
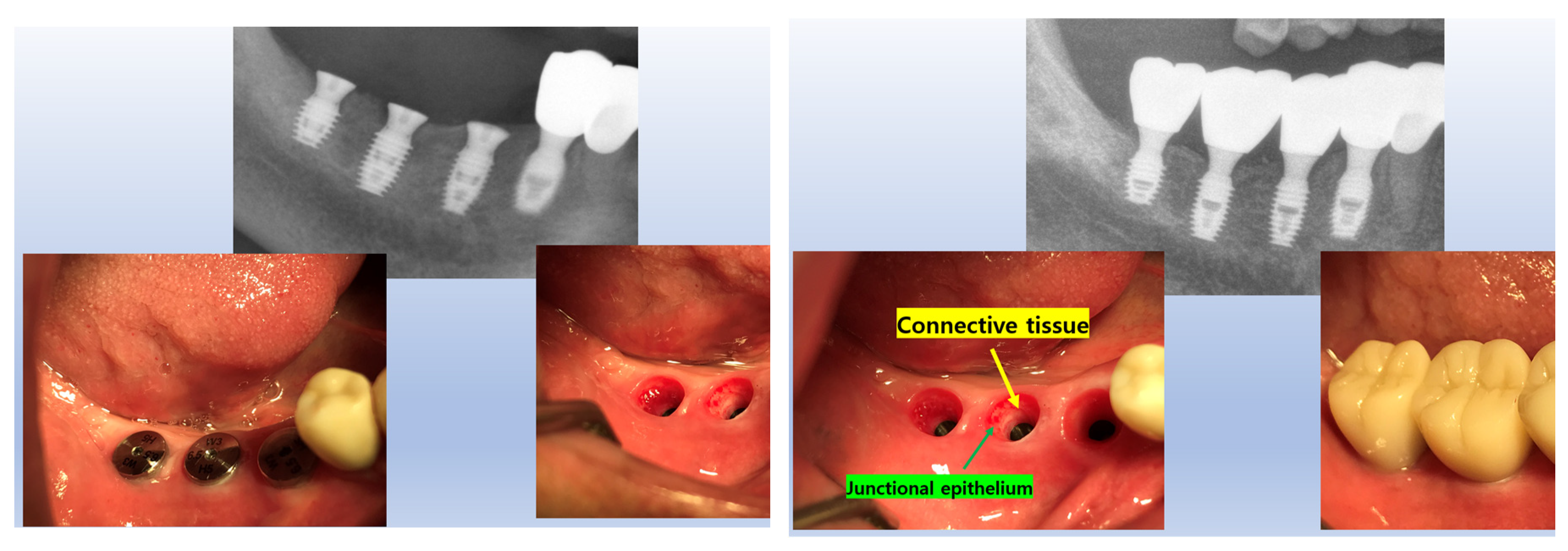
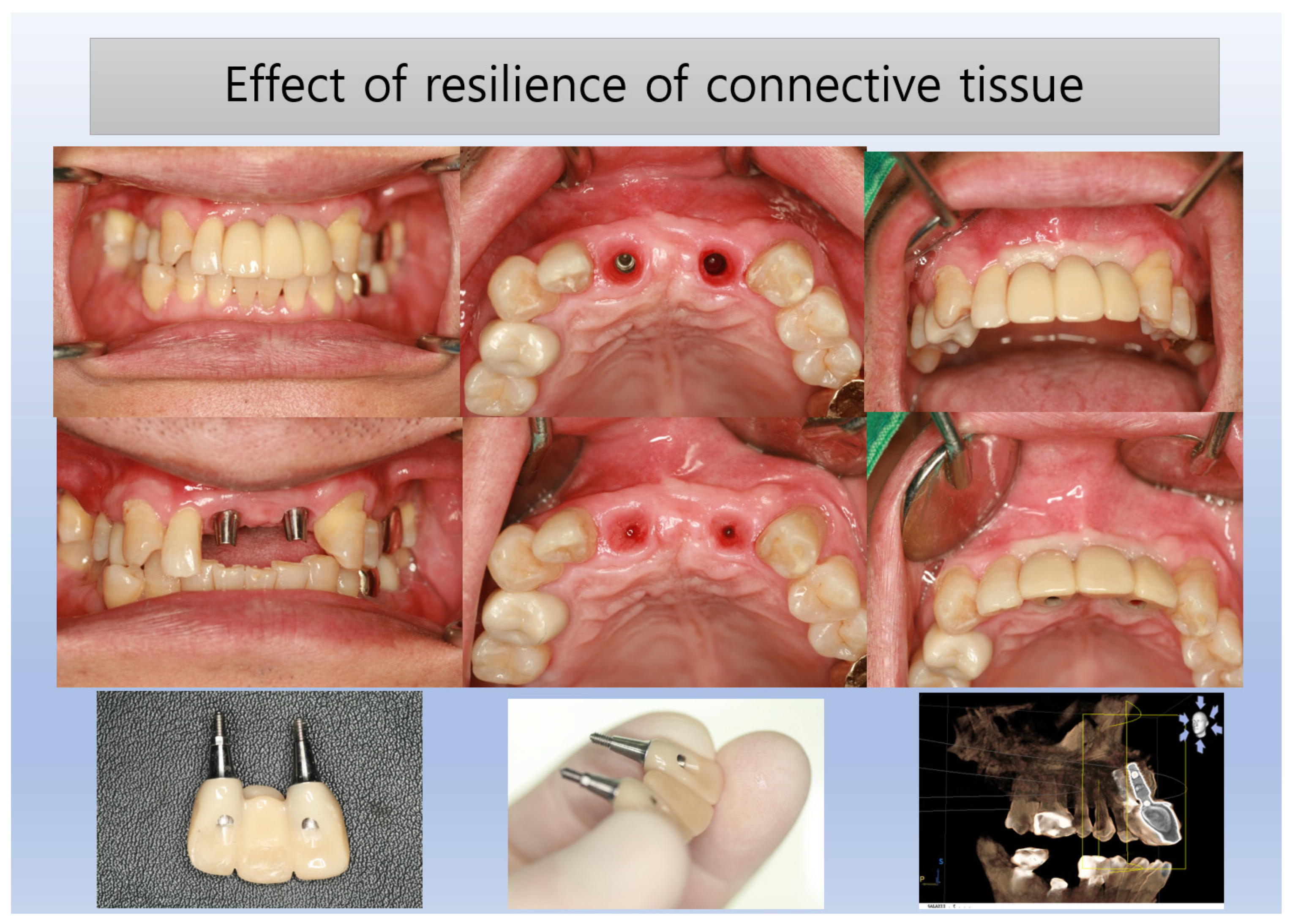
Enhanced Biologic Sealing in SPIs: A CBCT Analysis of Transmucosal Soft Tissue Dimensions
The cases examined in this study demonstrate that the area of transmucosal soft tissue, which corresponds to the junctional epithelium and connective tissue (the biologic width), around dental implants is enlarged due to deep subcrestal placement. This enlargement was quantitatively analyzed using Cone Beam Computed Tomography (CBCT). The results indicated that the average length of the Transitional Zone (TZ) was 3.8 mm, with an average thickness of 0.6 mm. These measurements suggest that the majority of the TZ is composed primarily of connective tissue. As the TZ extends toward the peripheral area and its thickness increases to more than 1.0-1.5 mm, it typically becomes covered with junctional epithelium. The predominant structure of the submucosal area is a connective tissue zone with junctional epithelium primarily present at the entrance, measuring approximately 0.5-1 mm, as detailed by Ikiru Atsuta et al.^[
30].
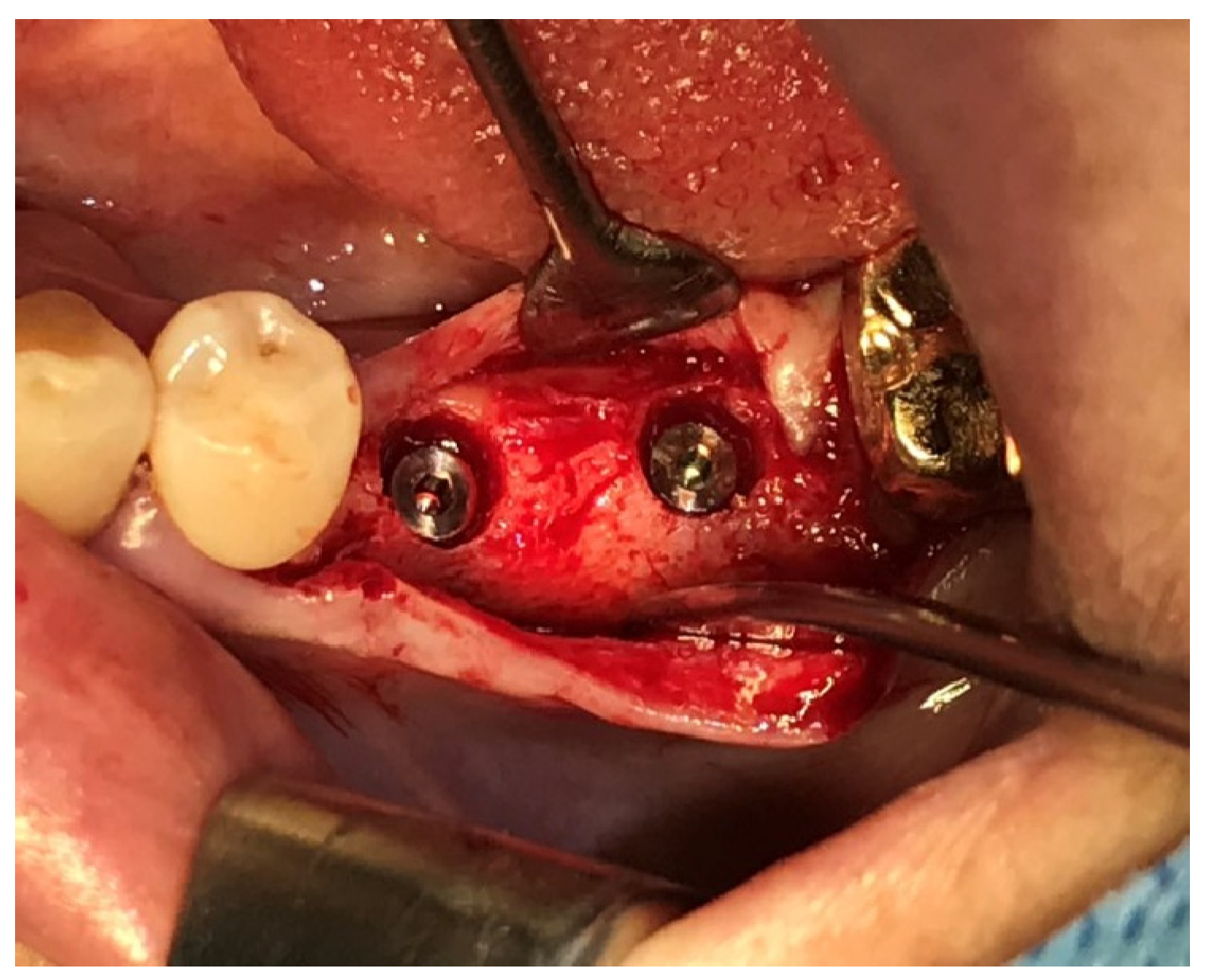
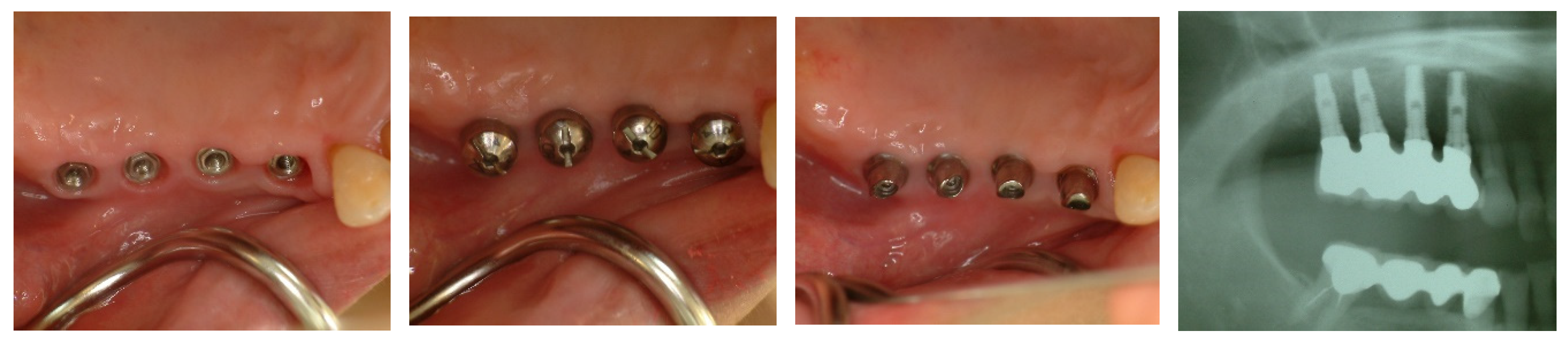
Figure 16.
Transmucosal Soft Tissue Structures in Subcrestally Placed Implants. This figure presents clinical images showcasing the transmucosal area related to the junctional epithelium and connective tissue (the biologic width) in subcrestally placed implants (SPIs), captured either after the removal or before the placement of the prosthetic parts. Compared to epi- or equi-crestal implant placements, these SPIs exhibit a larger area of transmucosal soft tissue. The right image distinctly identifies three layers: the subcrestal zone, the Transitional Zone (TZ), and the marginal zone, where the pale pink color closely matches the adjacent oral epithelium.
Figure 16.
Transmucosal Soft Tissue Structures in Subcrestally Placed Implants. This figure presents clinical images showcasing the transmucosal area related to the junctional epithelium and connective tissue (the biologic width) in subcrestally placed implants (SPIs), captured either after the removal or before the placement of the prosthetic parts. Compared to epi- or equi-crestal implant placements, these SPIs exhibit a larger area of transmucosal soft tissue. The right image distinctly identifies three layers: the subcrestal zone, the Transitional Zone (TZ), and the marginal zone, where the pale pink color closely matches the adjacent oral epithelium.
Histologic Review of Connective Tissue in Dental Implants
Histologic evaluations of connective tissue in implant cases are challenging to obtain but essential for understanding tissue interfaces. This study utilized CBCT to analyze the dimensions of the Transitional Zone (TZ) in Subcrestally Placed Implants (SPIs), finding that minimal changes in this dimension indicate stable structural integrity and absence of bone loss. It suggests that maintaining a close proximity between the submucosal components of implants and the subcrestal bone is crucial for preserving tissue health, as confirmed by extensive research on connective tissue properties.
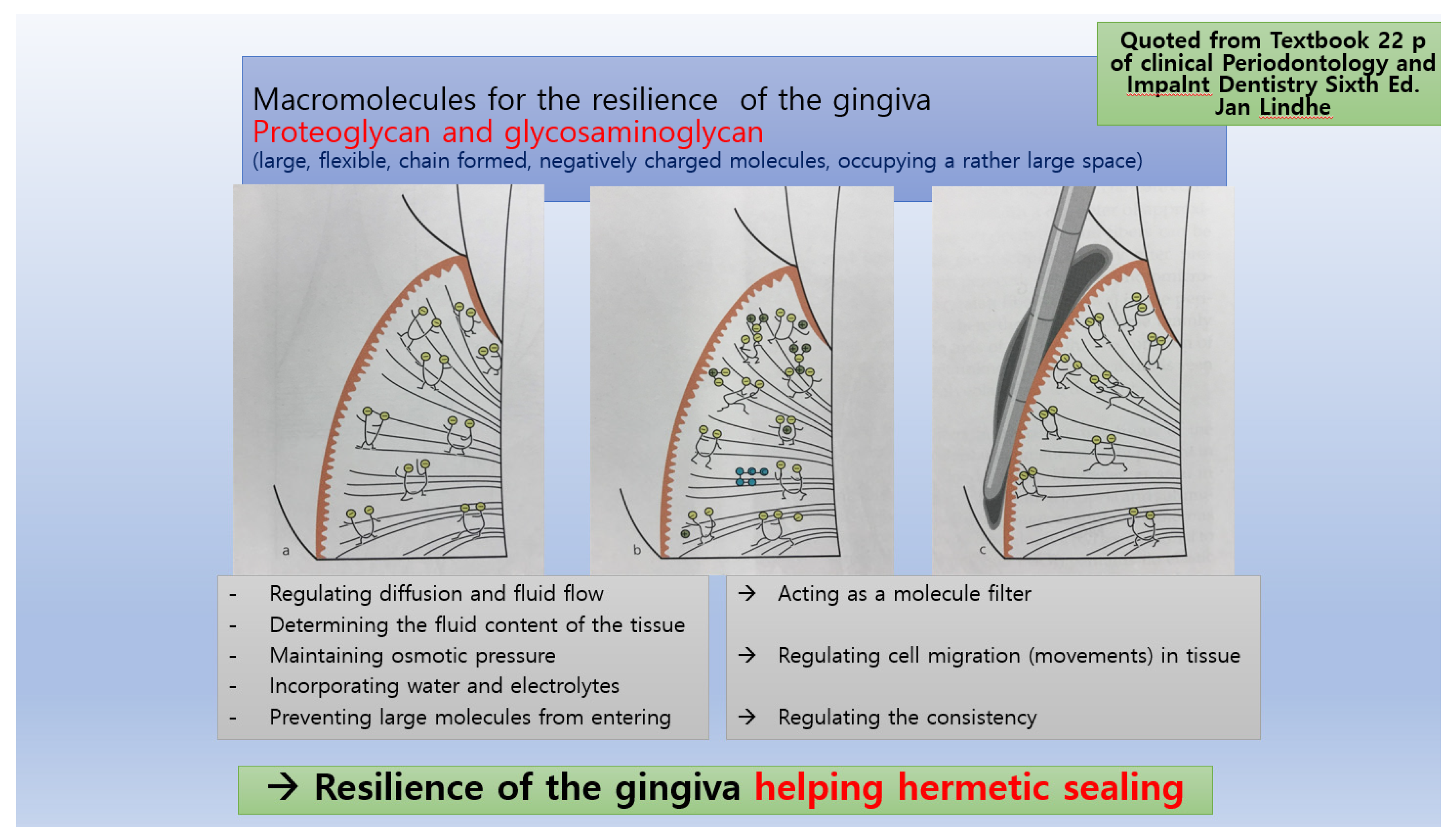
Figure 17.
Quoted from 'Clinical Periodontology and Implant Dentistry, Sixth Edition'. This image illustrates key concepts discussed in the text, providing visual support for the theoretical knowledge presented.
Figure 17.
Quoted from 'Clinical Periodontology and Implant Dentistry, Sixth Edition'. This image illustrates key concepts discussed in the text, providing visual support for the theoretical knowledge presented.
The connective tissue around dental implants plays crucial roles, contributing significantly to implant health and stability through the following functions:
Structural Support and Nutrition: It provides a robust foundation and essential blood supply for the junctional epithelium, ensuring its proper function and health.
Immune Response: Connective tissue facilitates immune reactions independently and supports the immune functions of the junctional epithelium. It also acts as a medium for the movement and transportation of cells and biochemicals, aiding systemic immune responses.
Mechanical Sealing and Resilience: The connective tissue maintains a hermetic mechanical seal around the implant through its inherent positive pressure and resilience, attributes derived from its protein-carbohydrate macromolecular structure.
Tissue Repair: It serves as a reservoir for stem cells and fibroblasts, which are crucial for ongoing repair and regeneration processes.
Bone Protection and Homeostasis: Similar to the periosteum, connective tissue protects the underlying bone and aids in maintaining bone homeostasis, ensuring the longevity and durability of the implant.
These characteristics of connective tissue around implants are essential for successful integration and long-term success, providing mechanical stability and biological compatibility.
Histologic Review of the Junctional Epithelium Around Implants
Junctional epithelial cells around dental implants, similar to those around natural teeth, exhibit a diminished capability and contain hemidesmosomes, although less effective than those in natural teeth^[
30,
31,
32]. The junctional epithelium relies on a robust foundation of connective tissue to effectively seal and protect the underlying structures. This arrangement suggests variability in connective tissue thickness along the implant, becoming thinner closer to the apex.
The junctional epithelium lies at the entrance area with about 0.5-1 mm^[
3]. It acts as a primary defense barrier against microbial invasion and plays a crucial immunologic role^[
30,
31,
33]. It features a high rate of cell turnover and consists of 15-30 cell layers, approximately 0.5 mm thick on average. Hemidesmosomes on its cell membranes face both the implant and connective tissue, facilitating adhesion while allowing immune cell mobility due to its larger intercellular spaces and fewer desmosomes compared to oral epithelium^[
32,
34,
46].
In clinical observations, it's noted that the majority of soft tissue around implants comprises connective tissue, with the epithelial layer only superficially at the coronal part. Unlike natural teeth, which integrate seamlessly with the oral mucosa, implants function as percutaneous devices with notably weaker junctional epithelium connections^[
32,
17]. This highlights the need for further investigation into the distinct roles and structural demarcations between junctional epithelium and connective tissue, especially to determine clinical implications and enhance implant integration strategies.
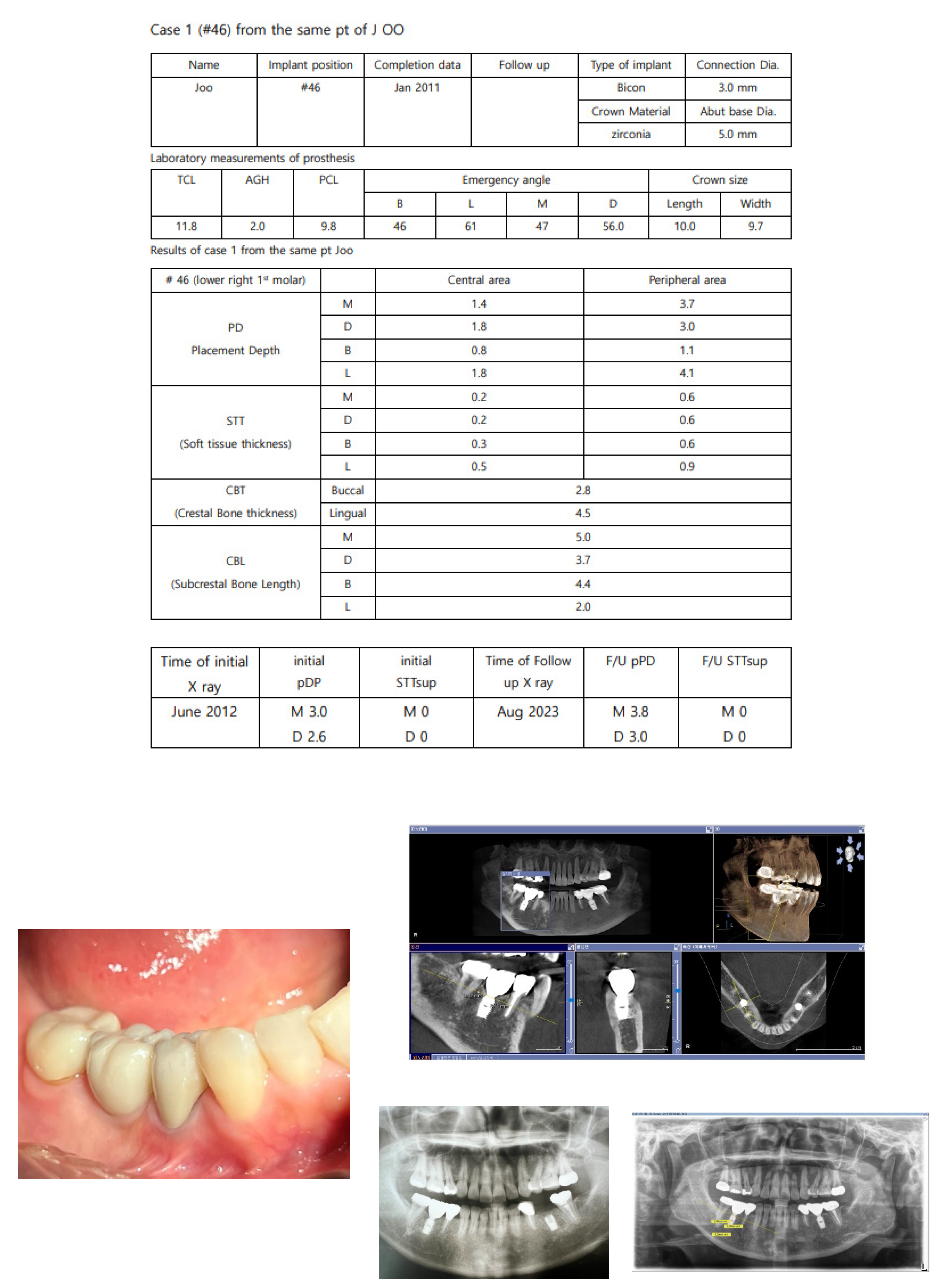
Probing Implants’ Sulcus: Evaluating Peri-Implant Soft Tissue Health
Probing the sulcus of dental implants, similar to natural teeth, involves using a periodontal probe with controlled force to measure the depth from the gingival margin to the deepest penetration of the junctional epithelium. Abrahamsson and Sodini found that a light probing force of 0.2 N reached similar depths in healthy tooth and implant sites, but in inflamed sites, the probe penetrates deeper into peri-implant tissues^[
35]. The 2017 World Workshop advises that probing of dental implants should use approximately 0.25 N, aiming for pocket depths generally under 5 mm^[
36].
Although automated periodontal probes were suggested, using metal probes on implants remains challenging due to the curvature in prosthetic designs^[
37,
38]. To assess the sealing and tightness of connective tissue, the author employed a probing technique using paper probes with a force range of 0.4-0.6 N. This method effectively demonstrated the health and resilience of peri-implant soft tissue, especially in SPIs, suggesting a substantial contribution to long-term implant stability and minimal bone change.
The roughness of implant surfaces affects bone to implant contact and initial survival rates but may increase bacterial adhesion and inflammation^[
39]. Deep implant placement can protect against oral biofilm exposure, further enhanced by a robust soft tissue barrier.
Figure 18.
Probing Peri-Implant Sulcus with Paper Points. This figure illustrates the technique of probing the sulcus depth around dental implants using paper points with a strength exceeding 0.6 N. The paper points are shown to penetrate easily into the sulcus of implants affected by peri-implantitis, with blood on the points upon withdrawal, signaling inflammation. In contrast, for healthy implants, the paper points do not penetrate the sulcus despite a longer soft tissue area, effectively demonstrating the integrity of the tissue and confirming the absence of inflammation. This visual comparison underscores the diagnostic value of paper points in assessing peri-implant health.
Figure 18.
Probing Peri-Implant Sulcus with Paper Points. This figure illustrates the technique of probing the sulcus depth around dental implants using paper points with a strength exceeding 0.6 N. The paper points are shown to penetrate easily into the sulcus of implants affected by peri-implantitis, with blood on the points upon withdrawal, signaling inflammation. In contrast, for healthy implants, the paper points do not penetrate the sulcus despite a longer soft tissue area, effectively demonstrating the integrity of the tissue and confirming the absence of inflammation. This visual comparison underscores the diagnostic value of paper points in assessing peri-implant health.
Optimizing Subcrestal Space for Stable Dental Implant Outcomes
The stable outcomes observed in this study, without the development of peri-implant pockets, are attributed to maintaining an optimal distance between subcrestal prosthetic components and subcrestal bone. This critical gap, initially set based on the rubber gingival form from the impression model, may be subject to adjustments during laboratory processing. However, these adjustments can be less precise than needed. Most clinicians strive to minimize pressure on soft tissue during prosthesis placement. Exceeding a certain gap limit (e.g., 2 mm) can induce a pocket effect, leading to potential food infiltration. This study finds that maintaining this distance at an average of 0.6 mm helps prevent such issues. Further research is essential to confirm these results and define the optimal gap distance that preserves soft tissue integrity and elasticity, along with adequate blood circulation. Additionally, the incorporation of digital dentistry, utilizing precise digital data from X-ray imaging and STL files, promises to enhance the accuracy of prosthesis fabrication, contributing to more successful implant outcomes.
Evaluating Dental Implant Results with X-ray Imaging
Clinicians typically use serial plain X-rays, often panoramic views, for postoperative assessment of bone changes in dental implants due to their efficiency and lower radiation exposure compared to CBCT. While CBCT's usage is increasing, it's primarily reserved for preoperative evaluations and treatment planning to minimize patient exposure to radiation. Routine implant check-ups can generally be conducted with plain X-rays unless a detailed three-dimensional analysis of bone structure is required due to significant clinical symptoms or signs of inflammation.
This study involved using CBCT to assess three-dimensional bone structures and submucosal soft tissue, offering a reliable measure when focused on a limited area, such as one or two teeth. For ongoing stability assessments, it is preferable to compare X-rays taken with the same machine and technique. However, due to radiation concerns, repeated CBCT scans are avoided; instead, a single postoperative CBCT within 6 months to 1 year is recommended, supplemented by annual or biannual plain X-rays. If plain X-rays indicate significant changes, a subsequent CBCT may be warranted to pinpoint issues and their development accurately.
In this study, CBCT scans taken 1-10 years post-implantation showed stable results, supported by consistent imaging techniques and additional scans performed on the same patient for unrelated surgeries, confirming no significant changes. This approach aligns with the retrospective nature of the study, which does not require consecutive CBCT comparisons.
Understanding the Peri-Implant Phenotype in Dental Implants
Modern dentistry recognizes the importance of the peri-implant phenotype, particularly when comparing soft tissue around epi-crestally and subcrestally placed implants. The stability of implants is influenced by three key phenotypic characteristics: 1. Alveolar bone thickness surrounding the implant, 2. Width and type of attached gingiva, and 3. Traditional definitions of biologic width. For optimal long-term stability, it is crucial that the buccal and lingual alveolar bone around implants maintains a minimum thickness of 2 mm; failing to meet this criterion increases the risk of bone loss^[
40].
Alveolar bone volume is essential for managing mechanical forces concentrated at the crestal area. Moreover, maintaining a substantial connective tissue zone is vital for shielding the inner bone from external elements, with blood supply to this tissue derived solely from the underlying bone. A larger foundational bone volume expands the connective tissue area, enhancing implant stability. Bone grafting is thus beneficial for sustaining stable implant results by preventing bone loss over time.
Subcrestal implant placement techniques, which increase the connective tissue area, are advantageous for creating aesthetically pleasing prostheses with a more natural emergence. Historical shifts toward platform switching in implant design have transformed vertical components of biologic width into horizontal elements, augmenting the connective tissue zone. Additionally, subcrestal placement can increase the occlusal perspective's circular soft tissue area even when the crestal ridge width is not extensive.
Frequent bone grafts and connective tissue grafts have been utilized to thicken crestal bone and strengthen soft tissue to achieve a favorable phenotype with epicrestal placement. However, subcrestal placement techniques may reduce the need for these additional procedures by allowing deeper placement within thick crestal bone, thereby enhancing soft tissue structural integrity and biologic width functionality.
Evaluating Traditional Techniques to Enhance Biologic Width
Traditionally, and even in recent practices, soft tissue grafts have been advocated to augment biologic width by thickening the connective tissue and epithelium layers. However, this method has inherent limitations—soft tissue can typically be thickened by less than double its initial size, while bone volume can be expanded much more substantially through bone grafting. This report proposes that subcrestal placement techniques are significantly more effective in enlarging the functional area of soft tissue, potentially by several times, as opposed to merely thickening it via soft tissue grafts. This approach not only more efficiently enhances biologic width but also substantially improves implant stability and aesthetics.
Surgical Techniques Using Ready-Made Abutments for Subcrestally Placed Implants
To streamline the surgical process and enhance the biologic environment, using healing abutments that match the profile of the final ready-made abutments can eliminate the need for bone modification to accommodate abutment placement. Alejandro et al. noted the significance of the distance between the implant platform and the alveolar bone crest, which can dictate the choice of gingival collar height on abutments, influencing both mucosal barrier and bone stability^[
45].
Maintaining optimal connective tissue space between the submucosal prosthetic components and the bone is crucial for leveraging the connective tissue's role effectively. While subcrestal implant placement often employs bone profiler drills to remove bony interferences and facilitate soft tissue accommodation, this approach may expose the mature bone to potential surgical trauma post-osseointegration, consuming additional time and energy. This drawback can be mitigated by employing a technique where matching healing abutments are placed during the initial surgery. Subsequently, for the final prosthesis, stock abutments with matching gingival cuff sizes are utilized to ensure seamless crown attachment, thereby reducing procedural complexity and enhancing tissue compatibility.
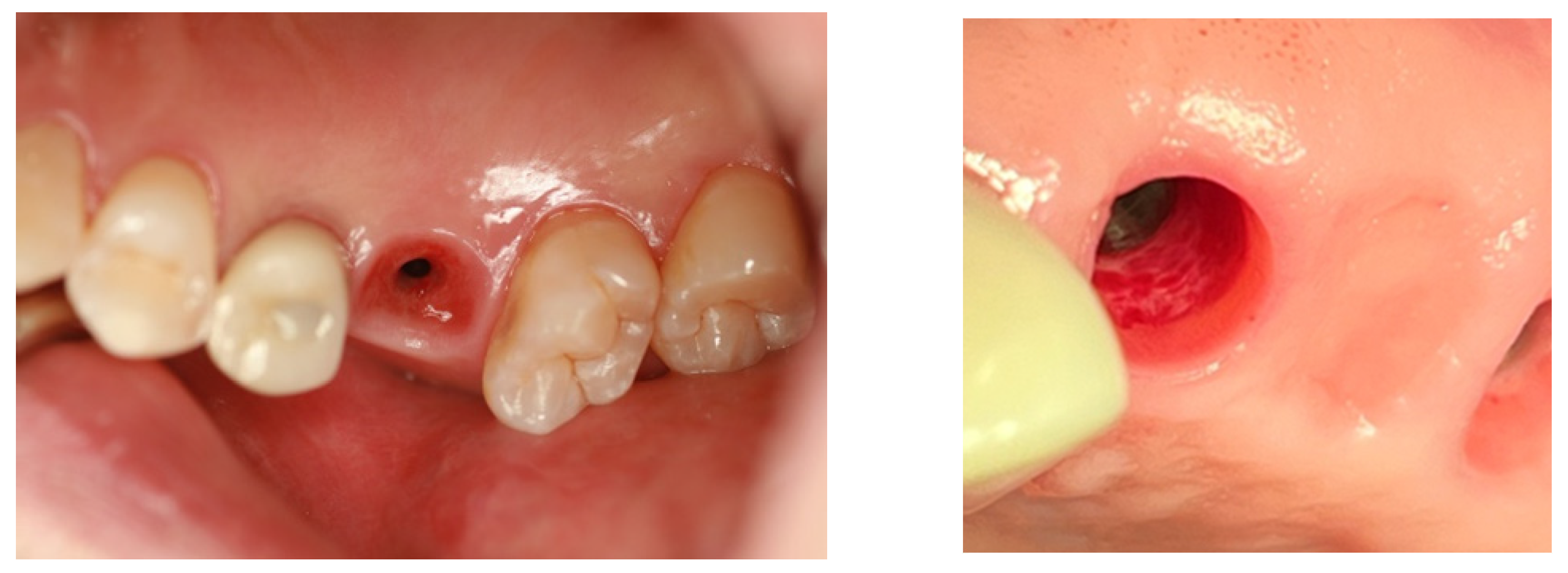
Figure 19.
Connective Tissue Layers in Subcrestally Placed Implants. This figure illustrates the two distinct layers of connective tissue observed in subcrestally placed implants. The deeper layer, adjacent to the subcrestal bone, is a very thin, periosteum-like layer with a pale white color. The superficial layer, situated above the crestal bone, is thicker and appears red. This visual distinction highlights the varied structural composition of connective tissue in different zones around dental implants.
Figure 19.
Connective Tissue Layers in Subcrestally Placed Implants. This figure illustrates the two distinct layers of connective tissue observed in subcrestally placed implants. The deeper layer, adjacent to the subcrestal bone, is a very thin, periosteum-like layer with a pale white color. The superficial layer, situated above the crestal bone, is thicker and appears red. This visual distinction highlights the varied structural composition of connective tissue in different zones around dental implants.
Figure 20.
Comparison of Transitional Zones with and without Horizontal Extensions. This figure presents a comparison of two distinct scenarios in dental implant placement concerning the transitional zone (TZ). The first scenario showcases an implant without horizontal extensions of the TZ on either side, while the second includes horizontal extensions. The traditional interpretation of biologic width, typically considered vertical, is demonstrated at the peripheral end of the crestal bone where the junctional epithelium begins. This is similarly observed at the peripheral ends of the horizontal extensions of the TZ when present.
Figure 20.
Comparison of Transitional Zones with and without Horizontal Extensions. This figure presents a comparison of two distinct scenarios in dental implant placement concerning the transitional zone (TZ). The first scenario showcases an implant without horizontal extensions of the TZ on either side, while the second includes horizontal extensions. The traditional interpretation of biologic width, typically considered vertical, is demonstrated at the peripheral end of the crestal bone where the junctional epithelium begins. This is similarly observed at the peripheral ends of the horizontal extensions of the TZ when present.
The Distribution and Angulation of the Transitional Zone
The slope of the transitional area in the connective tissue layer is typically oblique. When implant fixtures are placed at the epi-crestal level with sufficient horizontal crestal width (more than 2 mm), and the crown maintains close contact with its underlying soft tissue, it can function as a transitional zone as long as this intimate contact is maintained within a 1.0 mm range, for example. If this tight intimacy is not maintained, a gap may form where foreign material can intrude, causing the epithelial lining to extend until it reaches a healthy layer of connective tissue. If the crestal bone width is insufficient, maintaining intimate contact becomes challenging, requiring the crown at the cervical area to be thinner^[
41]. This often results in a less natural emergence profile.
Figure 21.
Visualizing Submucosal Areas during Abutment Repair. This figure shows the submucosal area exposed during the repair of a broken abutment neck after extensive use. It clearly depicts the Transitional Zone (TZ) and marginal zone, which extend obliquely or even horizontally along the mesiodistal sides. Notably, the subcrestal zone is absent on the buccolingual sides, indicating that the implant was initially placed at the epi-crestal level. This image provides a detailed view of the soft tissue layers affected by the placement level of the implant.
Figure 21.
Visualizing Submucosal Areas during Abutment Repair. This figure shows the submucosal area exposed during the repair of a broken abutment neck after extensive use. It clearly depicts the Transitional Zone (TZ) and marginal zone, which extend obliquely or even horizontally along the mesiodistal sides. Notably, the subcrestal zone is absent on the buccolingual sides, indicating that the implant was initially placed at the epi-crestal level. This image provides a detailed view of the soft tissue layers affected by the placement level of the implant.
Need for Further Research on Subcrestal Connective Tissue Width
Further research is necessary to determine the optimal width of the subcrestal connective tissue space. If this width is excessively large, it may compromise its functional integrity, allowing for the invasion of foreign materials, including bacteria, into this critical area. Establishing the appropriate dimensions is essential to maintain the protective and structural roles of this tissue in dental implantology.
Figure 22.
Natural-Looking Results Achieved by SPI Technique. This figure illustrates the effectiveness of the Subcrestally Placed Implants (SPI) technique in achieving results that closely mimic natural teeth. It demonstrates how the biologic width—comprising the transitional zone and subcrestal zone connective tissue—differs from that of natural teeth.
Figure 22.
Natural-Looking Results Achieved by SPI Technique. This figure illustrates the effectiveness of the Subcrestally Placed Implants (SPI) technique in achieving results that closely mimic natural teeth. It demonstrates how the biologic width—comprising the transitional zone and subcrestal zone connective tissue—differs from that of natural teeth.
Food Impaction and Subcrestally Placed Implants (SPIs)
Food impaction between implant-supported prostheses and adjacent teeth is more common when the embrasure space increases. Using the Subcrestally Placed Implants (SPIs) technique, which maintains intimate contact with the underlying soft tissue through an appropriate emergence profile, can significantly reduce this issue. SPIs are advantageous because they preserve a substantial amount of bone between implants and adjacent teeth, ensuring adequate soft tissue coverage above the bone. This method has been effective in minimizing food impaction, as reported by patients in this study^[
42].
Paradigm Shifts in Implant Dentistry
The evolution of implant therapy has seen significant paradigm shifts, with the focus transitioning from primarily bone-centric to an emphasis on the stability of soft tissue, recognizing their interdependence^[
43]. The optimal placement of implants is crucial as it influences the design of prosthetic components and ensures adequate space for soft tissue, impacting the overall therapeutic outcome.
Some experts argue that dental implants should ideally be placed 3 to 4 mm apical to the prospective gingival zenith on the restoration, cautioning that placing implants deeper can increase the risk of biological complications such as mucositis and peri-implantitis^[
44]. However, this viewpoint often overlooks critical variables such as variations in soft tissue thickness, implant connection designs, and techniques for managing excess cement. Moreover, traditional analyses lacking a three-dimensional perspective may not accurately depict the true implant depth, potentially misrepresenting it as excessively deep on plain X-rays.
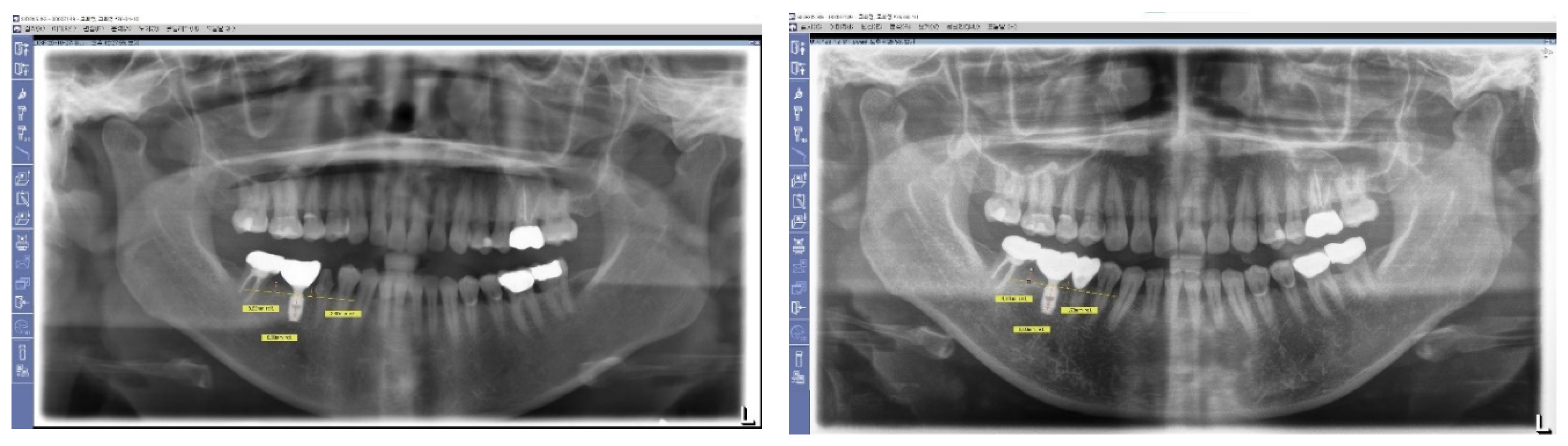
Figure 23.
Illustrating the Scalloping Effect. This figure demonstrates the scalloping effect, emphasizing the importance of using the midfacial point, rather than the interproximal point, as the reference for implant placement. It shows that to accurately create a prosthesis with a natural emergence profile, the scalloping effect distance (approximately 2 mm) must be added to the vertical distance from the fixture-abutment joint to the crestal bone level as seen in plain X-rays. This adjustment ensures that the final prosthesis aligns correctly with the natural contour of the gingiva, enhancing both aesthetic and functional outcomes.
Figure 23.
Illustrating the Scalloping Effect. This figure demonstrates the scalloping effect, emphasizing the importance of using the midfacial point, rather than the interproximal point, as the reference for implant placement. It shows that to accurately create a prosthesis with a natural emergence profile, the scalloping effect distance (approximately 2 mm) must be added to the vertical distance from the fixture-abutment joint to the crestal bone level as seen in plain X-rays. This adjustment ensures that the final prosthesis aligns correctly with the natural contour of the gingiva, enhancing both aesthetic and functional outcomes.
A three-dimensional analysis is essential, particularly due to the scalloping effect, where the interproximal gingival zenith appears more coronal than the midfacial zenith. This necessitates a more nuanced approach to implant depth evaluation to avoid biologic complications while achieving aesthetically and functionally sound results.
Gathering Soft Tissue Information for Prosthesis Fabrication
Traditionally, the primary information for fabricating dental prostheses comes from stone models, which replicate the oral mucosa using impression materials, or from oral scanning data. The design and dimensions of the prosthetic components that contact the tissue are influenced by the size and shape of the impression coping used. The choice of impression coping aids in determining the appropriate size and shape of the crown at the mucosal contact side. It's important to consider that during oral scanning, the soft tissue size may appear swollen due to the hydraulic positive pressure in the Transitional Zone (TZ) while the healing cap is removed for scanning. Conversely, the volume of the subcrestal connective tissue tends to remain relatively constant, providing a more stable basis for measurement and design.
Figure 24.
Submucosal Swelling During Prosthesis Removal. This figure illustrates the temporary swelling of the submucosal area, which reflects the resilience and hydraulic positive pressure exerted by the connective tissue. This phenomenon typically occurs when prostheses or healing abutments are removed for temporary repairs or impression procedures, highlighting the dynamic nature of the tissue's response to external manipulations.
Figure 24.
Submucosal Swelling During Prosthesis Removal. This figure illustrates the temporary swelling of the submucosal area, which reflects the resilience and hydraulic positive pressure exerted by the connective tissue. This phenomenon typically occurs when prostheses or healing abutments are removed for temporary repairs or impression procedures, highlighting the dynamic nature of the tissue's response to external manipulations.
Alejandro et al. suggested that the selection of abutment height, which influences marginal bone loss, should be guided by radiographic parameters—specifically, the distance between the implant platform and the alveolar bone crest at the time of implant placement. This approach supports the "one abutment, one-time" concept^[
45]. Chiyun Won adjusted the selection of the definitive abutment based on the biologic environment, which includes subcrestal bone, connective tissue, and junctional epithelium, as demonstrated in this study. The design of the final restoration was incorporated into the surgical planning for implant placement, allowing the SPI technique to influence both the subcrestal bone morphology and the subgingival shape of the prostheses, actively molding the soft tissue in the Transitional Zone (TZ).
The TZ is present when the crestal bone, thicker than 2 mm, supports the overlying soft tissue and maintains intimate contact with the prostheses. Conversely, when the crestal bone is thinner than 2 mm, it cannot support a TZ, and only free-standing marginal gingiva is present, corresponding to the conventional biologic width which primarily consists of a vertical component.
Figure 25.
Comparison of Marginal Zones with and without Transitional Zones in Dental Implants This image illustrates the differences in soft tissue around an implant. On the buccal side, unsupported soft tissue extending about 3 mm adheres to the conventional biologic width seen in natural teeth. In contrast, on the palatal side, the supported soft tissue includes a Transitional Zone (TZ) that maintains extended and intimate contact with overlying prostheses when healthy. Captured after a screw loosening incident ten years post-placement of an Astra Tech implant, the image shows no significant complications other than a metal tattoo in the soft tissue, resulting from friction caused by the abutment moving as the screw was unscrewed.
Figure 25.
Comparison of Marginal Zones with and without Transitional Zones in Dental Implants This image illustrates the differences in soft tissue around an implant. On the buccal side, unsupported soft tissue extending about 3 mm adheres to the conventional biologic width seen in natural teeth. In contrast, on the palatal side, the supported soft tissue includes a Transitional Zone (TZ) that maintains extended and intimate contact with overlying prostheses when healthy. Captured after a screw loosening incident ten years post-placement of an Astra Tech implant, the image shows no significant complications other than a metal tattoo in the soft tissue, resulting from friction caused by the abutment moving as the screw was unscrewed.
This article introduces the concept of the Transitional Zone (TZ) of connective tissue to elucidate the phenomena occurring around Subcrestally Placed Implants (SCIs) from functional, structural, and biological perspectives.
Conclusions
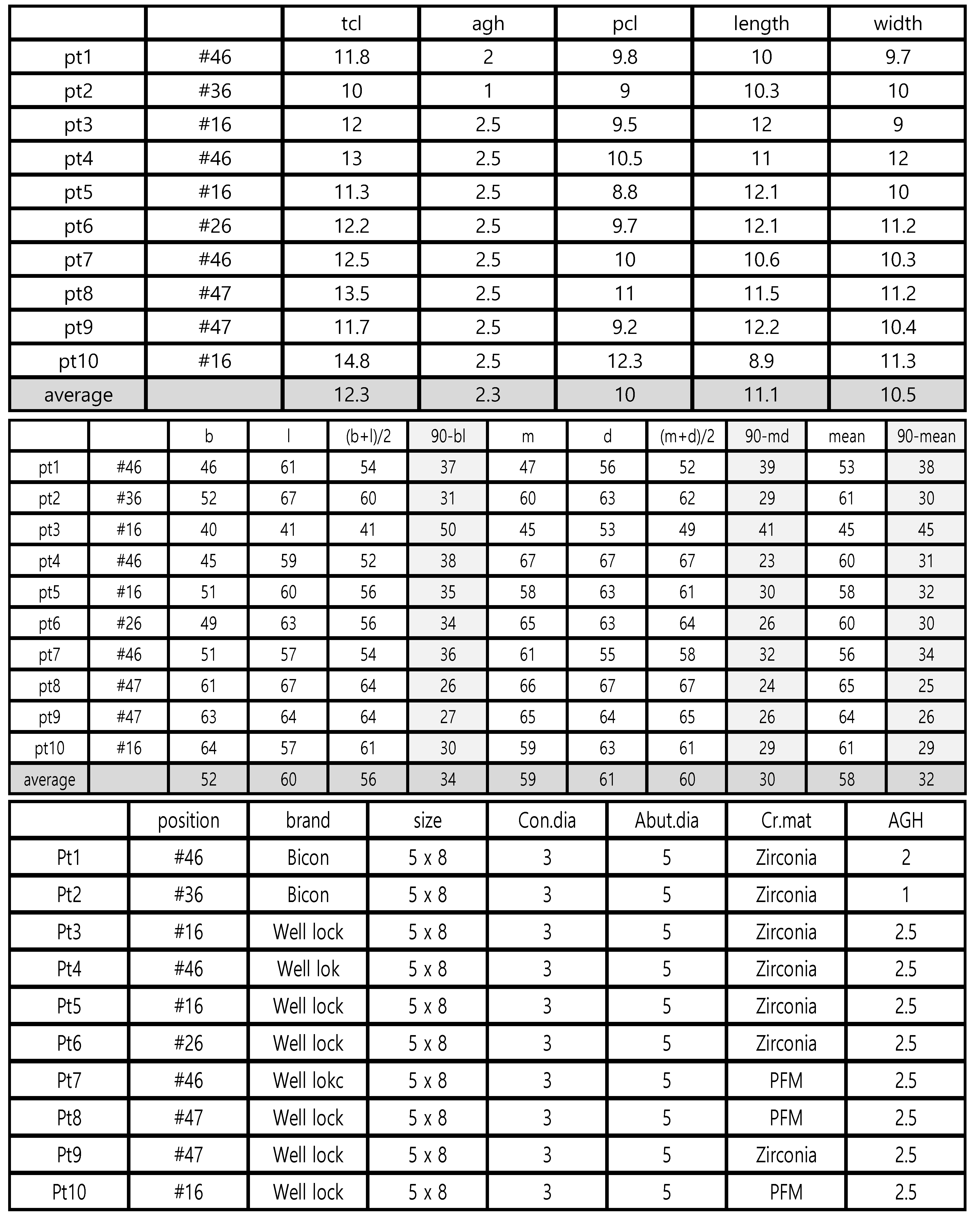
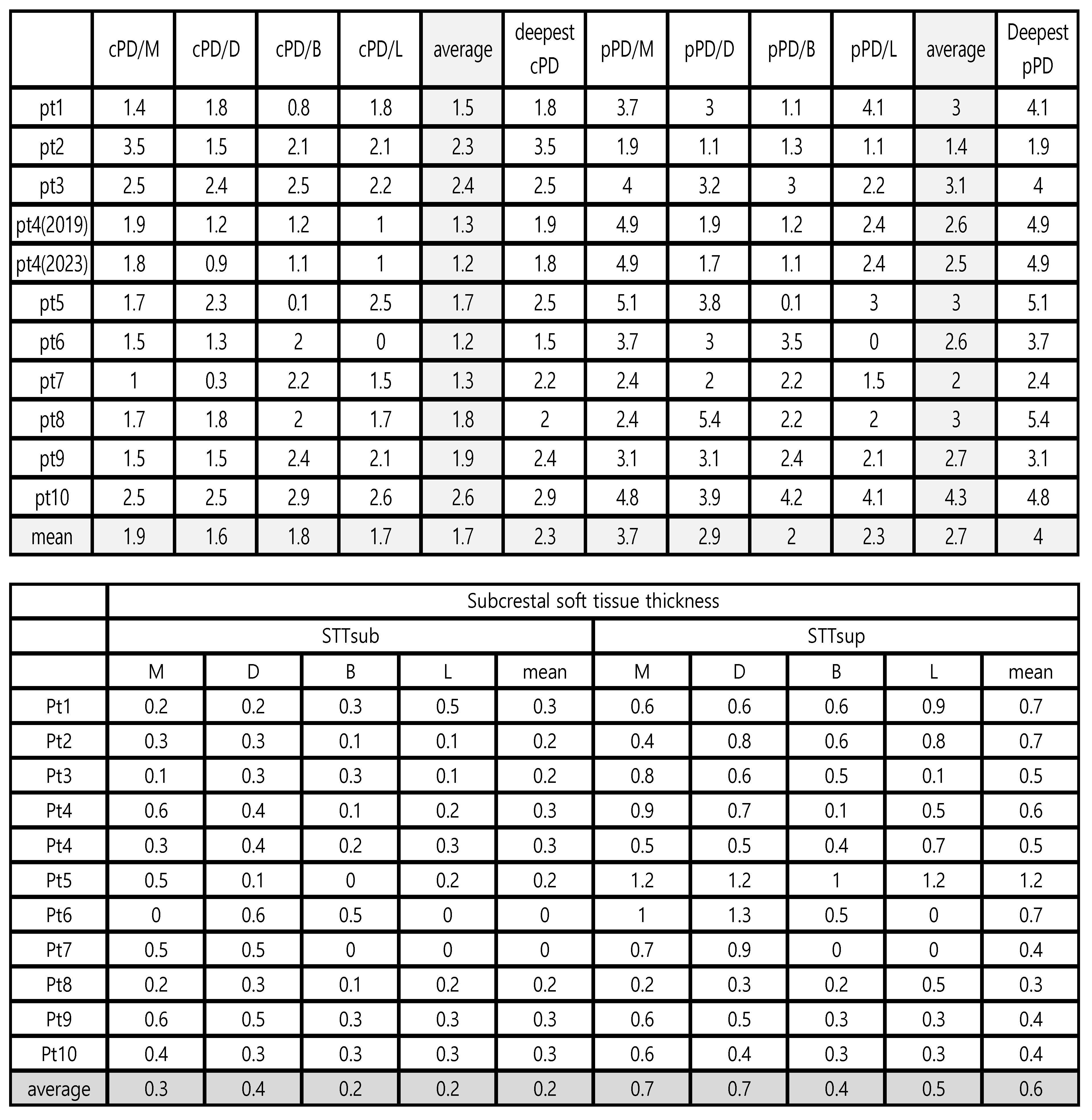
This study conducted topographical measurements of the soft tissue and crestal bone from CBCT for Subcrestally Placed Implants (SPIs) to evaluate their structural integrity and stability. Key findings include:
Panoramic analysis indicated that the crestal bone remained stable with minimal changes (mean changes of peripheral Placement Depth (pPD) were less than 0.1 mm) over an average of 3.3 years.
The average central Placement Depth (cPD) was 1.7 mm, and peripheral Placement Depth (pPD) was 2.7 mm.
The average central Soft Tissue Thickness (cSTT) was 0.2 mm, and peripheral Soft Tissue Thickness (pSTT) was 0.6 mm.
The average Crestal Mucosal Length (CML) was 3.8 mm.
The average buccal Crestal Bone Thickness (CBT) was 3.0 mm, and lingual CBT was 3.7 mm.
Due to concerns about radiation exposure, plain X-rays, specifically panoramic views, are preferred for routine monitoring of Subcrestally Placed Implants (SPIs). Correlations between panoramic X-ray results and three-dimensional CBCT measurements have validated that panoramic views are adequate for assessing implant stability, offering a safer alternative for regular checks.
For posterior implants to appear natural, it's essential to consider the depth of placement. This ensures the prosthetics emerge properly, mimicking the natural tooth appearance. Managing this emerging phenomenon correctly is crucial for aesthetic success.
Subcrestal implant placement is vital for achieving natural aesthetics in both posterior and anterior regions. Despite its benefits, there has been scarce research on how the surrounding soft tissue impacts the biologic seal.
This report encourages further systematic research into the soft tissue surrounding SPIs. Better understanding the effects of subcrestal placements could improve implant outcomes and help develop techniques that enhance the biologic seal, ultimately promoting long-term implant health