Submitted:
17 April 2024
Posted:
17 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Preparing Denture Tooth Specimens
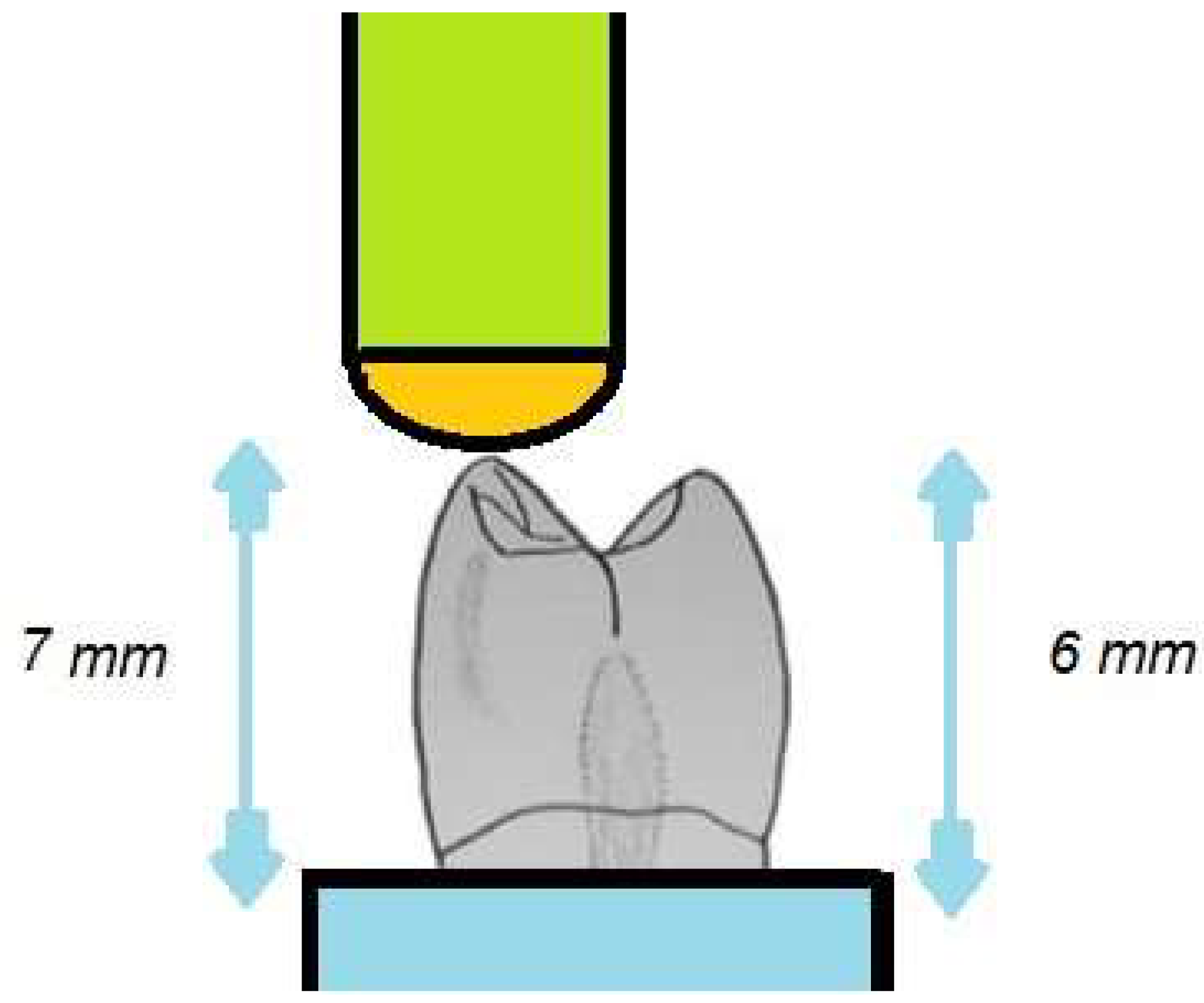
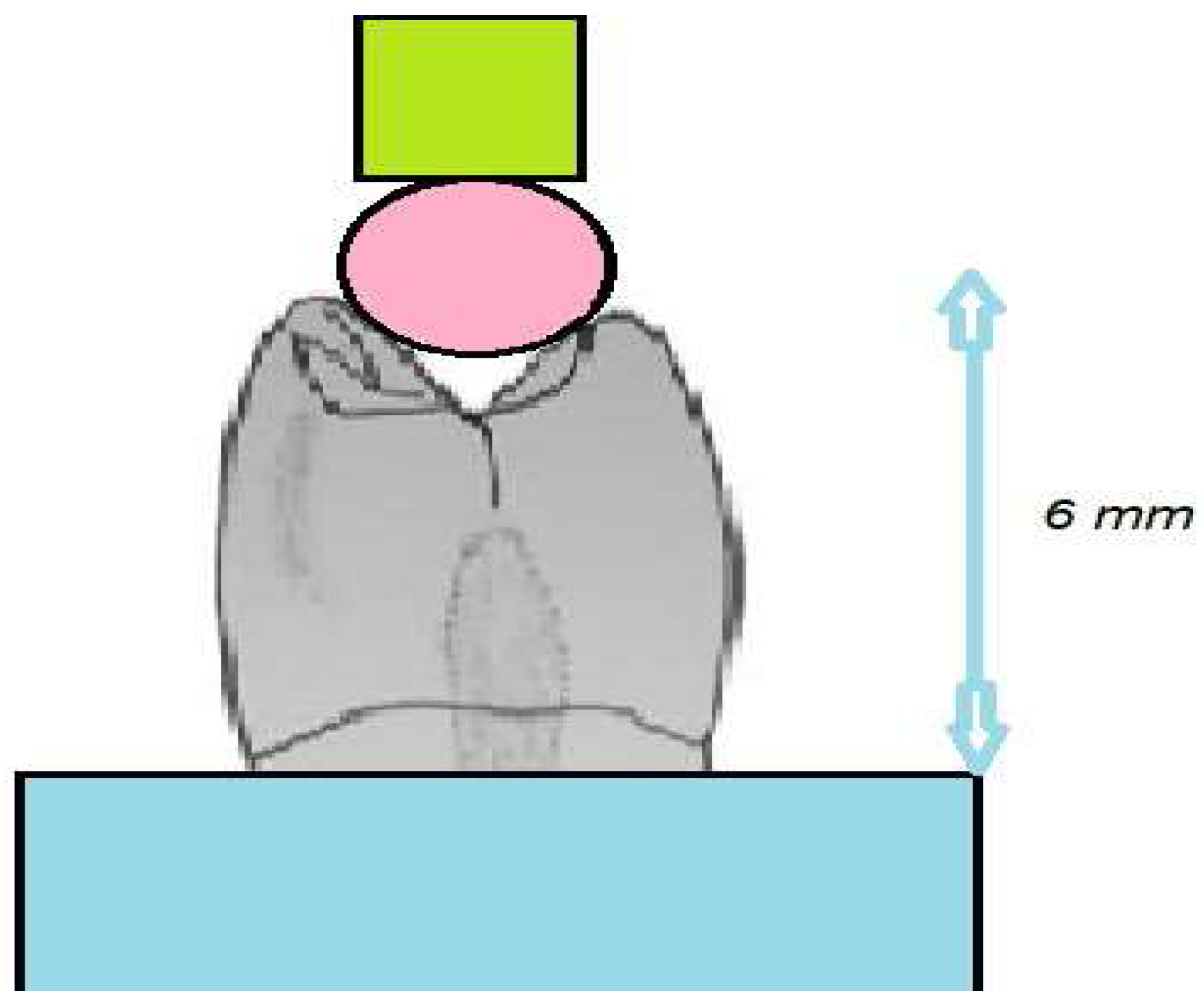
2.2. Performance of Chipping and Indirect Tensile Fracture Test
2.3. Statistical Analysis
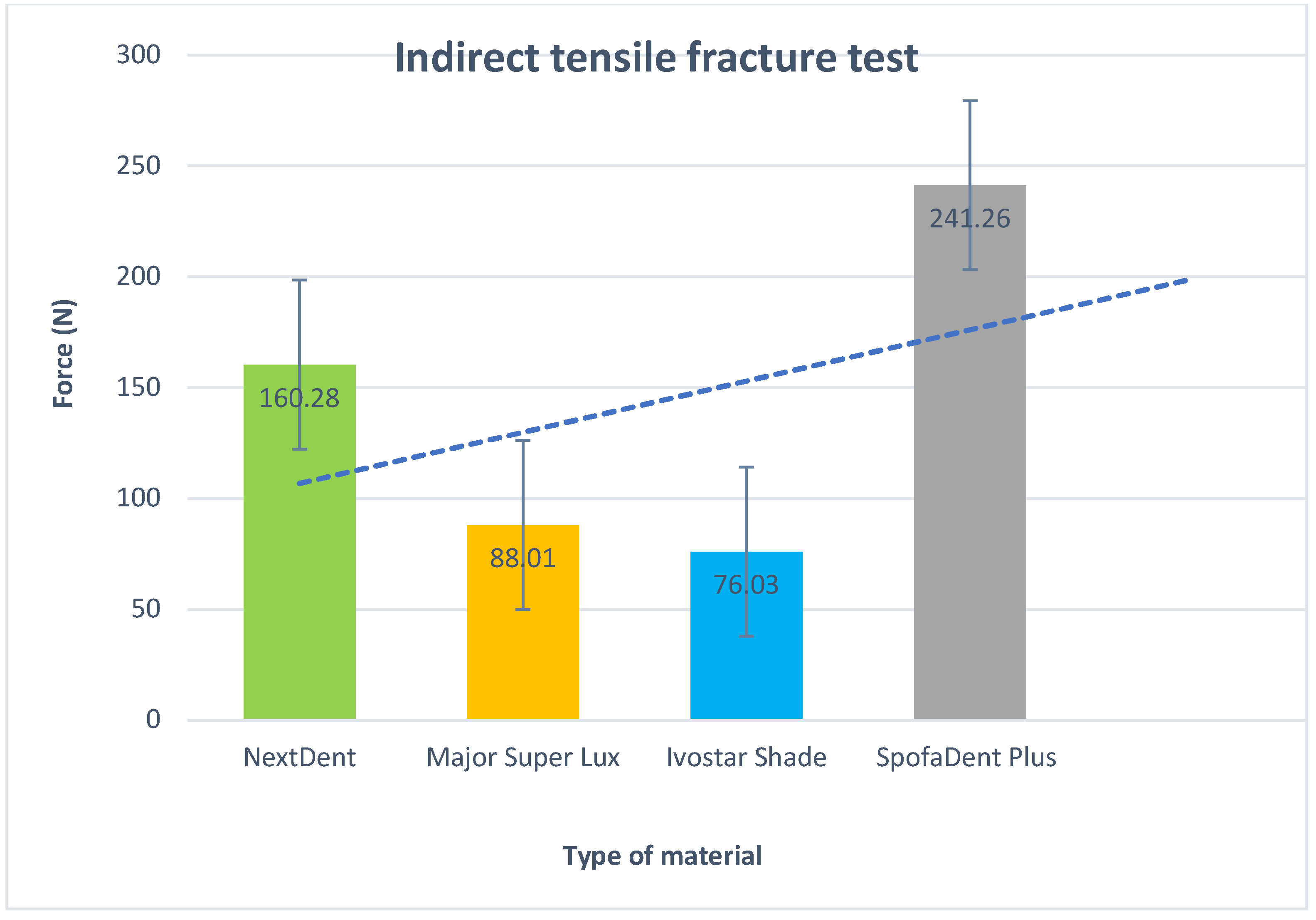
3. Results
4. Discussion
- Limited Sample Variation: Only four specific types of denture teeth were examined, potentially limiting the representation of diverse materials and manufacturing methods in dental practice. Including more types of denture teeth could offer a more comprehensive understanding of fracture resistance.
- Lack of Long-Term Durability Assessment: The study assessed fracture resistance over a short period, without considering long-term durability or the effects of repeated stress and wear. Future research should explore the performance of 3D-printed denture teeth over extended periods to assess their longevity.
- Simplified Testing Conditions: The study conducted tests under controlled laboratory conditions, which may not fully mimic the complex forces experienced by denture teeth during mastication. More realistic conditions, such as simulated chewing forces, could provide deeper insights into the performance of 3D-printed denture teeth.
- Potential Bias in Sample Selection: There is a possibility of bias in the selection of denture teeth for each group, as certain brands or types may have been chosen based on availability or researcher preference. Randomized selection or blinding methods could help mitigate bias in future studies.
- Limited Generalizability: The results might not apply universally to all categories of 3D-printed denture teeth or resin materials. Variations in factors like printing parameters, resin compositions, and post-processing methods could impact fracture resistance. Therefore, additional research encompassing a wider array of materials and manufacturing approaches is necessary for broader applicability.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Gad, M.M.; Al-Thobity, A.M.; Rahoma, A.; Abualsaud, R.; Al-Harbi, F.A.; Akhtar, S. Reinforcement of PMMA Denture Base Material with a Mixture of ZrO2 Nanoparticles and Glass Fibers. Int. J. Dent. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Gutteridge, D.L. The effect of including ultra-high-modulus polyethylene fiber on the impact strength of acrylic resin. Br. Dent. J. 1988, 164. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Takahashi, H.; Hayakawa, I. Reinforcement of denture base resin with short-rod glass fiber. Dent. Mater. J. 2007, 26, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Karacaer, O.; Polat, T.N.; Tezvergil, A.; Lassila, L.V.; Vallittu, P.K. The effect of length and concentration of glass fibers on the mechanical properties of an injection- and a compression-molded denture base polymer. J. Prosthet. Dent. 2003, 90, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Ellakwa, A.E.; Morsy, M.A.; El-Sheikh, A.M. Effect of Aluminum Oxide Addition on the Flexural Strength and Thermal Diffusivity of Heat-Polymerized Acrylic Resin. J. Prosthodont. 2008, 17, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Cevik, P.; Yildirim-Bicer, A.Z. The effect of silica and prepolymer nanoparticles on the mechanical properties of denture base acrylic resin. J. Prosthodont. 2018, 27, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Forster, A.M.; Johnson, P.M.; Eidelman, N.; Quinn, G.; Schumacher, G.; Zhang, X.; Wu, W.-L. Improving performance of dental resins by adding titanium dioxide nanoparticles. Dent. Mater. 2011, 27, 972–982. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Nathwani, N.; Taylor, L.; Sefat, F. Denture Base Composites: Effect of Surface Modified Nano- and Micro-Particulates on Mechanical Properties of Polymethyl Methacrylate. Materials 2020, 13, 307. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, M.; Vlahova, A.; Kalachev, Y.; Zlatev, S.; Kazakova, R.; Capodiferro, S. Recent Advances in 3D Printing of Polymers for Application in Prosthodontics. Polymers 2023, 15, 4525. [Google Scholar] [CrossRef]
- Wang, R.; Tao, J.; Yu, B.; Dai, L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J. Prosthet. Dent. 2014, 111, 318–326. [Google Scholar] [CrossRef]
- Bacali, C.; Badea, M.; Moldovan, M.; Sarosi, C.; Nastase, V.; Baldea, I.; Chiorean, R.S.; Constantiniuc, M. The influence of graphene in the improvement of physico-mechanical properties in PMMA Denture Base Resins. Materials 2019, 12, 2335. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Thobity, A.M.; Rahoma, A.; Abualsaud, R.; Al-Harbi, F.A.; Akhtar, S. Reinforcement of PMMA Denture Base Material with a Mixture of ZrO2 Nanoparticles and Glass Fibers. Int. J. Dent. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Thobity, A.M.; Rahoma, A.; Abualsaud, R.; Al-Harbi, F.A.; Akhtar, S. Reinforcement of PMMA Denture Base Material with a Mixture of ZrO2 Nanoparticles and Glass Fibers. Int. J. Dent. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Chuchulska, B.; Dimitrova, M.; Dochev, B. In Vitro Study of the Surface Roughness, Hardness, and Absorption of an Injection-Molded Denture Base Polymer, Manufactured under Insufficient Mold Solidification. Appl. Sci. 2024, 14, 2906. [Google Scholar] [CrossRef]
- Dimitrova, M.; Chuchulska, B.; Zlatev, S.; Kazakova, R. Colour Stability of 3D-Printed and Prefabricated Denture Teeth after Immersion in Different Colouring Agents—An In Vitro Study. Polymers 2022, 14, 3125. [Google Scholar] [CrossRef] [PubMed]
- Karacaer, O.; Polat, T.N.; Tezvergil, A.; Lassila, L.V.; Vallittu, P.K. The effect of length and concentration of glass fibers on the mechanical properties of an injection-and a compression-molded denture base polymer. J. Prosthet. Dent. 2003, 90, 385–393. [Google Scholar] [CrossRef]
- Ellakwa, A.E.; Morsy, M.A.; El-Sheikh, A.M. Effect of Aluminum Oxide Addition on the Flexural Strength and Thermal Diffusivity of Heat-Polymerized Acrylic Resin. J. Prosthodont. 2008, 17, 439–444. [Google Scholar] [CrossRef]
- Cevik, P.; Yildirim-Bicer, A.Z. The effect of silica and prepolymer nanoparticles on the mechanical properties of denture base acrylic resin. J. Prosthodont. 2018, 27, 763–770. [Google Scholar] [CrossRef]
- Chuchulska, B.; Dimitrova, M.; Vlahova, A.; Hristov, I.; Tomova, Z.; Kazakova, R. Comparative Analysis of the Mechanical Properties and Biocompatibility between CAD/CAM and Conventional Polymers Applied in Prosthetic Dentistry. Polymers 2024, 16, 877. [Google Scholar] [CrossRef]
- Nejatian, T.; Nathwani, N.; Taylor, L.; Sefat, F. Denture Base Composites: Effect of Surface Modified Nano- and Micro-Particulates on Mechanical Properties of Polymethyl Methacrylate. Materials 2020, 13, 307. [Google Scholar] [CrossRef]
- Zhang, X.-Y.; Zhang, X.-J.; Huang, Z.-L.; Zhu, B.-S.; Chen, R.-R. Hybrid effects of zirconia nanoparticles with aluminum borate whiskers on mechanical properties of denture base resin PMMA. Dent. Mater. J. 2014, 33, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Tao, J.; Yu, B.; Dai, L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J. Prosthet. Dent. 2014, 111, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Bacali, C.; Badea, M.; Moldovan, M.; Sarosi, C.; Nastase, V.; Baldea, I.; Chiorean, R.S.; Constantiniuc, M. The influence of graphene in improvement of physico-mechanical properties in PMMA Denture Base Resins. Materials 2019, 12, 2335. [Google Scholar] [CrossRef]
- Ravdeep, S.; Mann, N.; Dorin, R. Fracture toughness of conventional, milled and 3D printed denture bases. Dental Materials 2022, 38, 1443–1451. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM Complete Denture Resins: An Evaluation of Biocompatibility, Mechanical Properties, and Surface Characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef]
- Nakamura, M.; Takahashi, H.; Hayakawa, I. Reinforcement of denture base resin with short-rod glass fiber. Dent. Mater. J. 2007, 26, 733–738. [Google Scholar] [CrossRef]
- Karacaer, O.; Polat, T.N.; Tezvergil, A.; Lassila, L.V.; Vallittu, P.K. The effect of length and concentration of glass fibers on the mechanical properties of an injection-and a compression-molded denture base polymer. J. Prosthet. Dent. 2003, 90, 385–393. [Google Scholar] [CrossRef]
- Ellakwa, A.E.; Morsy, M.A.; El-Sheikh, A.M. Effect of Aluminum Oxide Addition on the Flexural Strength and Thermal Diffusivity of Heat-Polymerized Acrylic Resin. J. Prosthodont. 2008, 17, 439–444. [Google Scholar] [CrossRef]
- Cevik, P.; Yildirim-Bicer, A.Z. The effect of silica and prepolymer nanoparticles on the mechanical properties of denture base acrylic resin. J. Prosthodont. 2018, 27, 763–770. [Google Scholar] [CrossRef]
- Sun, J.; Forster, A.M.; Johnson, P.M.; Eidelman, N.; Quinn, G.; Schumacher, G.; Zhang, X.; Wu, W.-L. Improving performance of dental resins by adding titanium dioxide nanoparticles. Dent. Mater. 2011, 27, 972–982. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Nathwani, N.; Taylor, L.; Sefat, F. Denture Base Composites: Effect of Surface Modified Nano- and Micro-Particulates on Mechanical Properties of Polymethyl Methacrylate. Materials 2020, 13, 307. [Google Scholar] [CrossRef]
- Zhang, X.-Y.; Zhang, X.-J.; Huang, Z.-L.; Zhu, B.-S.; Chen, R.-R. Hybrid effects of zirconia nanoparticles with aluminum borate whiskers on mechanical properties of denture base resin PMMA. Dent. Mater. J. 2014, 33, 141–146. [Google Scholar] [CrossRef]
- Wang, R.; Tao, J.; Yu, B.; Dai, L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J. Prosthet. Dent. 2014, 111, 318–326. [Google Scholar] [CrossRef]
- Bacali, C.; Badea, M.; Moldovan, M.; Sarosi, C.; Nastase, V.; Baldea, I.; Chiorean, R.S.; Constantiniuc, M. The influence of graphene in improvement of physico-mechanical properties in PMMA Denture Base Resins. Materials 2019, 12, 2335. [Google Scholar] [CrossRef]
- Dimitrova, M.; Corsalini, M.; Kazakova, R.; Vlahova, A.; Chuchulska, B.; Barile, G.; Capodiferro, S.; Kazakov, S. Comparison between Conventional PMMA and 3D Printed Resins for Denture Bases: A Narrative Review. J. Compos. Sci. 2022, 6, 87. [Google Scholar] [CrossRef]
- Alshabib, A.; Silikas, N.; Watts, D.C. Hardness and fracture toughness of resin-composite materials with and without fibers. Dent. Mater. 2019, 35, 1194–1203. [Google Scholar] [CrossRef] [PubMed]
- Al-Harbi, F.A.; Abdel-Halim, M.S.; Gad, M.M.; Fouda, S.M.; Baba, N.Z.; AlRumaih, H.S.; Akhtar, S. Effect of nanodiamond addition on flexural strength, impact strength, and surface roughness of PMMA denture base. J. Prosthodont. 2018, 28, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Johnson, A.; van Noort, R. Reinforcement of denture base resin. Adv. Sci. Technol. 2006, 49, 124–129. [Google Scholar]
- Balos, S.; Pilic, B.; Markovic, D.; Pavlicevic, J.; Luzanin, O. Poly (methyl-methacrylate) nanocomposites with low silica addition. J. Prosthet. Dent. 2014, 111, 327–334. [Google Scholar] [CrossRef]
- Nobrega, A.S.; Andreotti, A.M.; Moreno, A.; Sinhoreti, M.A.; dos Santos, D.M.; Goiato, M.C. Influence of adding nanoparticles on the hardness, tear strength, and permanent deformation of facial silicone subjected to accelerated aging. J. Prosthet. Dent. 2016, 116, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Vojtkova, H.; Lassila, V.P. Impact strength of denture polymethyl methacrylate reinforced with continuous glass fibers or metal wire. Acta Odontol. Scand. 1995, 53, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-Y.; Zhang, X.-J.; Huang, Z.-L.; Zhu, B.-S.; Chen, R.-R. Hybrid effects of zirconia nanoparticles with aluminum borate whiskers on mechanical properties of denture base resin PMMA. Dent. Mater. J. 2014, 33, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Takahashi, H.; Hayakawa, I. Reinforcement of denture base resin with short-rod glass fiber. Dent. Mater. J. 2007, 26, 733–738. [Google Scholar] [CrossRef]
- Sun, J.; Forster, A.M.; Johnson, P.M.; Eidelman, N.; Quinn, G.; Schumacher, G.; Zhang, X.; Wu, W.-L. Improving performance of dental resins by adding titanium dioxide nanoparticles. Dent. Mater. 2011, 27, 972–982. [Google Scholar] [CrossRef]

| Product | Composition | Detail | Manufacturer |
|---|---|---|---|
| NextDent | Methacrylate-based photopolymerized resin | 3D printing | 3D Systems, Soesterberg, The Netherlands |
| Ivostar Shade | MPM–PMMA * | Mold XS | Ivoclar Vivadent, Schaan, Liechtenstein |
| Spofadent™Plus | MPM–PMMA * | Mold XS | SpofaDental, Jičín, Czechia |
| Major Super Lux | MPM–PMMA * | Mold XS | Major Prodotti Dentari SPA, Moncalieri, TO, Italy |
| (I) V2 | (J) V2 | Mean Values (I-J) |
Standard Deviation | Р | 95% - Interval of confidentiality | |
| Lower | Upper | |||||
| NextDent | Ivostar Shade | -.346413* | .022049 | <0.01 | -.28645 | -.17284 |
| Major Super Lux | -.325271* | .022074 | <0.01 | -.34831 | -.23442 | |
| SpofaDent Plus | -.478271* | .022087 | <0.01 | -.40421 | -.29212 | |
| SpofaDent Plus | NextDent | .429414* | .022089 | <0.01 | .17563 | .28646 |
| Major Super Lux | -.261857* | .022053 | .028 | -.11876 | -.00484 | |
| SpofaDent Plus | -249657* | .022011 | <0.01 | -.14758 | -.06286 | |
| Major Super Lux |
NextDent | .274571* | .022049 | <0.01 | .23852 | .34834 |
| Ivostar Shade | .141853* | .022061 | .028 | .00487 | .11887 | |
| SpofaDent Plus | -.158002* | .022061 | .045 | -.11508 | -.00094 | |
| Ivostar Shade | NextDent | .429277* | .022063 | <0.01 | .29226 | .40633 |
| Major Super Lux | .314857* | .022063 | <0.01 | .06286 | .17687 | |
| Ivostar Shade | .258300* | .022069 | .045 | .00096 | .11508 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





