Introduction
Traumatic anterior shoulder instability is one of the most common conditions in orthopaedic sports medicine, and arthroscopic repair is often the modality of choice for diagnosis and treatment. Recurrent instability is a major cause of revision presenting challenges due to distorted anatomy and difficulty in identifying anatomic lesions. The optimal management approach for individuals who have experienced failure of their initial arthroscopic procedure remains a subject of controversy [
1].
The options for surgical intervention for recurrent anterior shoulder instability most commonly include arthroscopic reversion Bankart repair (ARBR), open Latarjet bone-block procedure, and arthroscopic Bankart repair with remplissage [
2]. An international consensus study, known as the Delphi studies, identified different indications for these procedures [
3]. In their study, they underscored the importance of two pivotal bone lesions in the decision-making process for instability. Specifically, the extent of glenoid bone loss and the presence of a Hill-Sachs lesion on the humerus significantly influence the decision-making process.
Bankart repair is indicated for primary or recurrent instability with high risk for failure of non-operative management. Specific imaging findings that suggest a successful Bankart repair are minimal glenoid bone loss, on-track Hill-Sachs lesion, and magnetic resonance imaging (MRI) confirmation of labrum tear/Bankart lesion [
2,
3]. Remplissage is indicated for a large Hill-Sachs lesion either off-track or engaging at the time of arthroscopy [
4]. Recently the use of the glenoid track model for guiding surgical management has been questioned by Rashid et al. [
5].
Bone block procedures have traditionally been reserved for more severe instability with significant bone loss. The Latarjet procedure is indicated for recurrent instability, failed prior surgery, contact athlete, critical glenoid bone loss, and bipolar bone loss resulting in an off-track lesion [
6]. Finally, free flap glenoid bone grafting such as the Eden–Hybinette procedure is indicated for critical bone loss and failed prior Latarjet procedure [
7]. The cutoff for critical glenoid bone loss has yet to be defined and ranges from 15-30% of glenoid circumference, and defining a precise value will help shoulder surgeons guide triage to coracoid transfer or bone grafting in severe cases.
Bankart versus Latarjet repair is a key discussion area despite fundamental differences in technique. Bankart repair is arthroscopic, anchors avulsed labrum back into anatomic position, and addresses soft tissue stability. The Latarjet procedure is usually open, uses a coracoid graft, and relies on a combination of increased glenoid surface area and conjoint tendon sling effect to restore stability. The aims of this review are to 1) compare the instability recurrence rates for ARBR to other types of anterior stabilization, 2) determine if the effect of bipolar bone loss on recurrent instability, and 3) provide a framework for managing recurrent anterior shoulder instability. The primary research question of this systematic review is to evaluate the effectiveness of various revision techniques after failed Bankart repair. Additionally, we aim to provide valuable insights into the impact critical bone lesions have on recurrence rates.
Methods
The study design inclusion criteria comprised randomized controlled trials (RCTs) and non-randomized studies (cohort studies, case-control studies) with comparative designs. All studies included a cohort that had failed a primary Bankart repair. Revision surgical techniques included repeat arthroscopic and open Bankart repair, arthroscopic Hill-Sachs remplissage, and arthroscopic and open coracoid transfer procedures (Bristow and Latarjet procedures). Comparative surgical techniques were considered as the comparators. The primary outcome of interest was recurrent shoulder instability. Functional outcome measures (e.g., range of motion, strength, performance), patient-reported outcomes, adverse events, revision operations, and return-to-sport were analyzed when available. Only studies published in English were included.
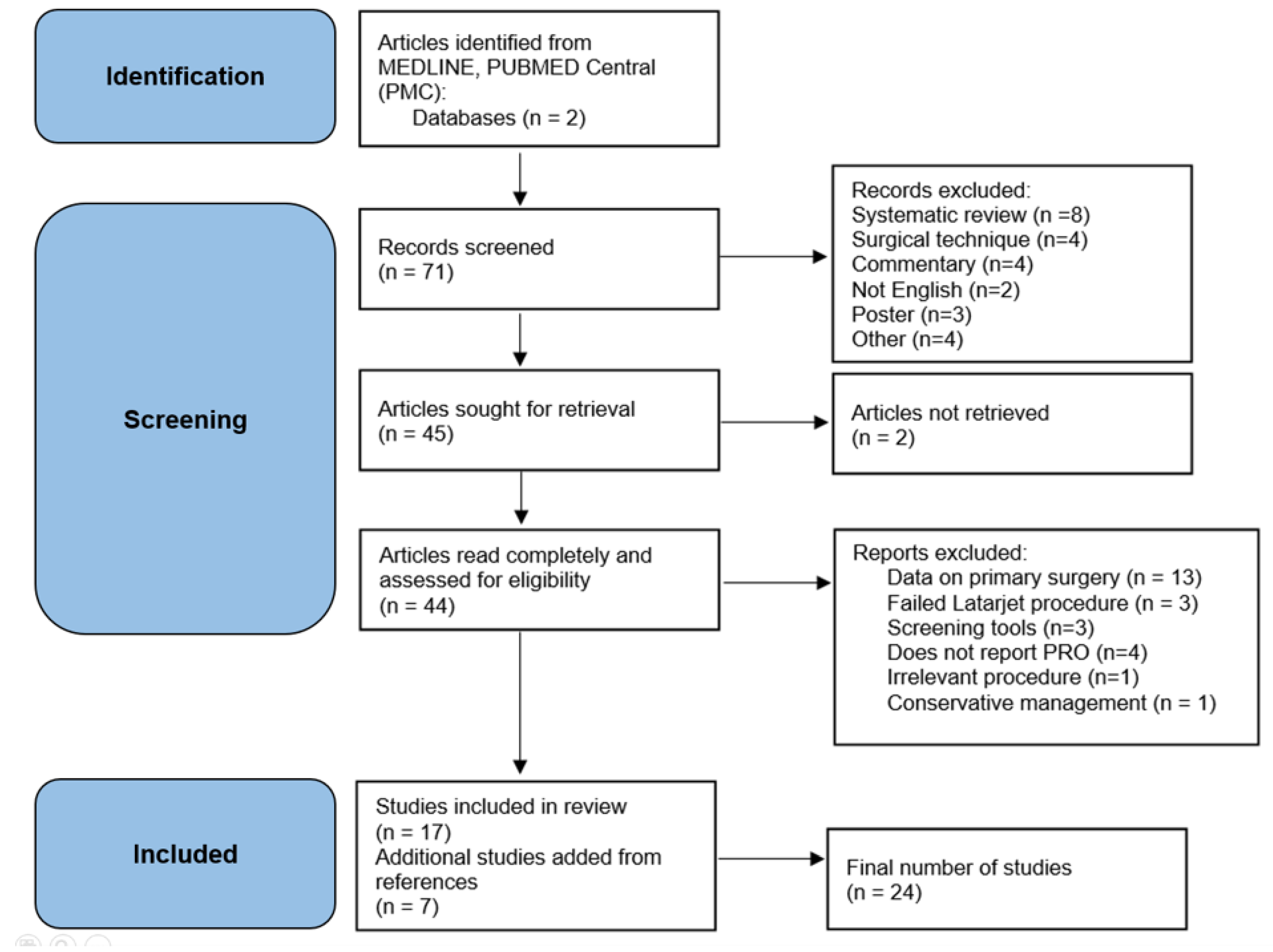
To select all relevant studies, a thorough literature review utilizing Google Scholar and PubMed search engines according to PRISMA guidelines, along with a careful examination of reference lists (see
Figure 1). A comprehensive search strategy incorporating appropriate medical subject headings (MeSH) terms and keywords pertaining to "Bankart OR Latarjet," “shoulder arthroscopy,” and "failure OR revision" was devised and tailored to each database to ensure exhaustive coverage. The study selection process engaged two independent reviewers who evaluated titles and abstracts of retrieved records for eligibility based on predefined criteria. Full-text articles of potentially suitable studies were acquired and individually assessed for definitive inclusion. Any disparities between reviewers were resolved through discourse or consultation with a third reviewer. For data extraction, devised and piloted data extraction excel tables were employed, with two independent reviewers extracting pertinent details from included studies encompassing study and participant characteristics, intervention specifics, outcomes, and adverse events. Discordances among reviewers were resolved through discussion or consultation with a third reviewer.
The risk of bias assessment for each included study was carried out by two independent reviewers, employing appropriate tools like the Cochrane Risk of Bias tool for randomized controlled trials. Data analysis and synthesis encompassed the compilation of extracted data into a master table, encompassing primary and secondary outcomes. Exploration of potential sources of heterogeneity was achieved through subgroup analyses and sensitivity analyses, which factored in considerations like surgical techniques, population characteristics (e.g., athlete type, competition level, age groups, mechanism of injury), and surgical outcomes. The systematic review protocol was registered in the PROSPERO database (ID: 536764) to enhance transparency and avoid duplication.
Results
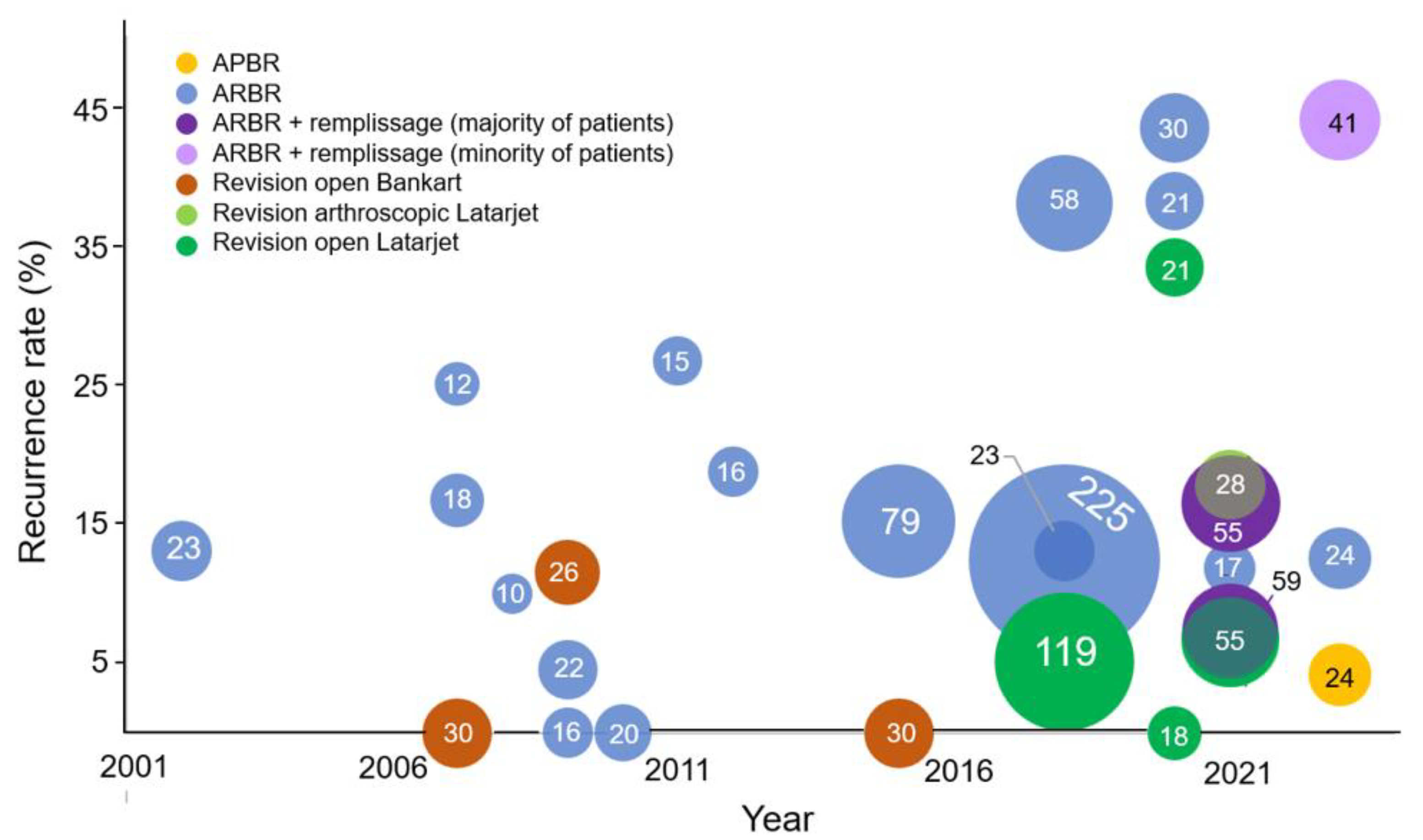
Collectively, the studies analyzed in this review encompass a substantial patient population, with a total of 1,032 patients across the included studies. Among these patients, 781 underwent arthroscopic procedures, while 251 patients underwent open surgeries. The most common procedure was the revision arthroscopic Bankart with 685 patients. There has been an increase in the use of remplissage concurrently with the Bankart repair recently since 2020 (see
Figure 2). There were 217 open Latarjet procedures.
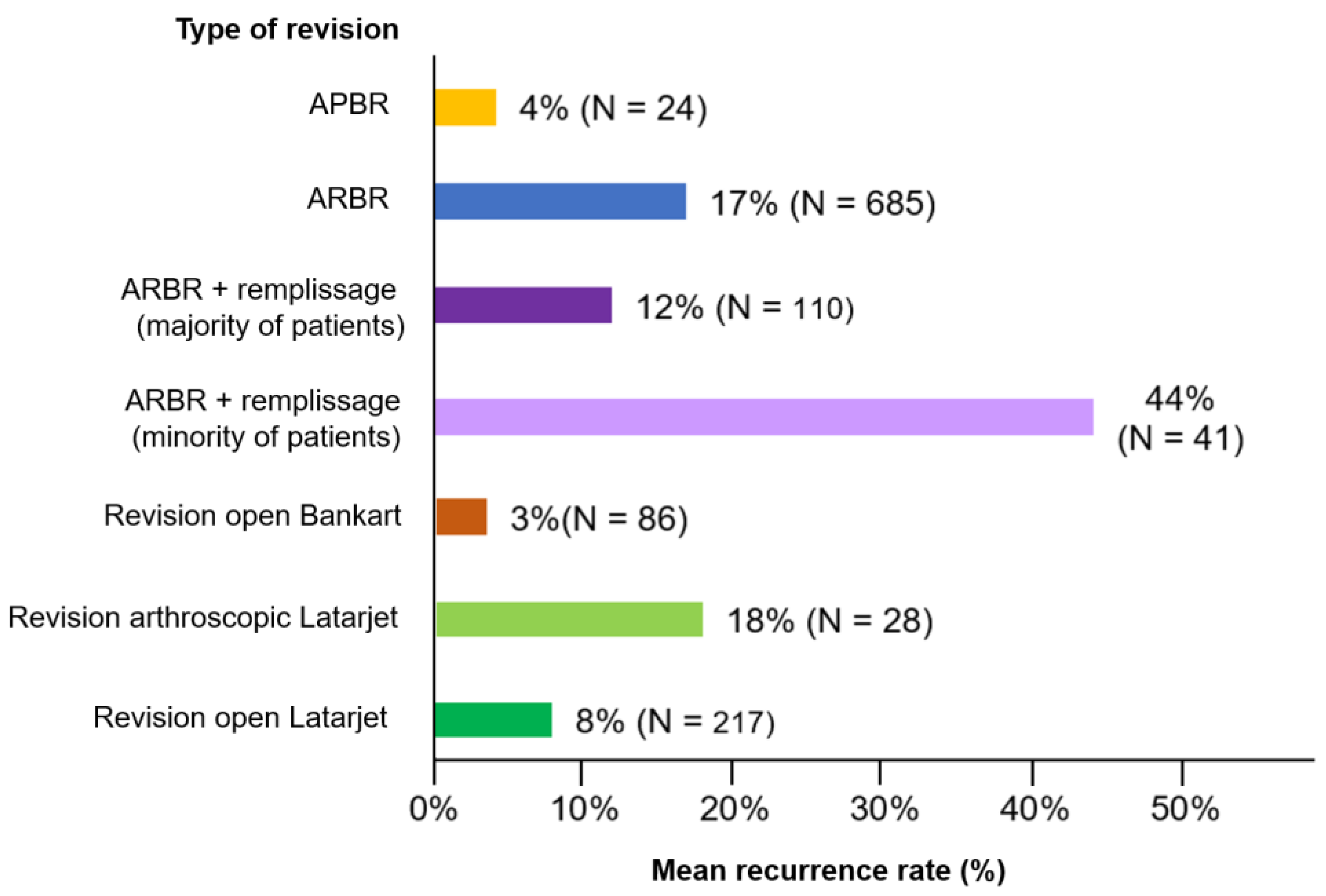
Chi-squared testing showed a significantly higher recurrence rate (17% vs. 8%; p<.001) for the revision arthroscopic Bankart repair compared to the open Latarjet procedure (see
Figure 3). However, when remplissage was used to augment the Bankart repair (exclusively in studies which included patients with off-track Hill-Sachs lesions), there was no significant difference in the recurrence rate compared to Latarjet (12% vs. 8%; p =0.24).
The preoperative findings, recurrence rates, and conclusions for each study are reported in
Table 1. There were many different findings reported across the papers, but the most common lesions identified preoperatively or intraoperatively were Hill-Sachs lesions and Bankart lesions with reported glenoid bone loss. All the studies that reported Bankart bone lesions had average glenoid bone loss less than 20%.
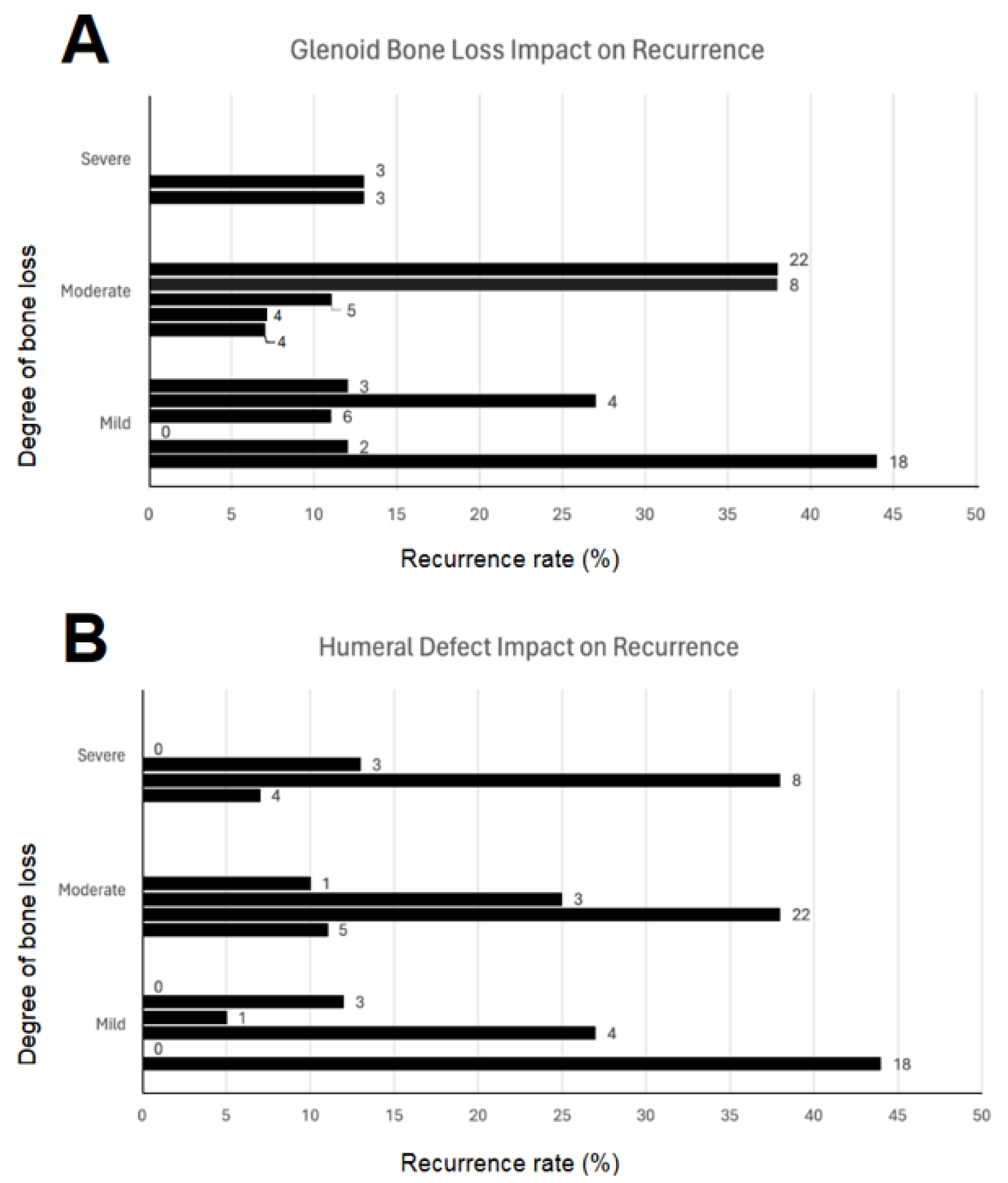
We further analyzed the glenoid and humeral lesions that were reported. As there was no universally adopted cutoffs or classification for bone loss, we found categorizing the glenoid and humeral lesions into mild, moderate, and severe across the entire study to be the best approach (see
Figure 4). The most common cutoff for critical glenoid bone loss was 20% (eight studies) with a mean cutoff of 23 ± 4.2%. After categorization, we performed a one-way ANOVA test to analyze the effects of bone loss on recurrence rates. Neither the presence of a Hill-Sachs lesion (p=0.80) nor glenoid bone loss (p=.85) had a statistically significant impact on the recurrence rate, with the caveat that supracritical glenoid bone loss was exclusively treated with coracoid transfer procedures.
Regarding recurrence rates, it is important to note that persistent instability is one of the major risks associated with surgery. Among the included studies, only 1 study did not report on the rate of recurrence [
8]. In this systematic review, the rate of recurrence ranged from 4.5% to 44%. The study by Boileau et al. reported the lowest recurrence rate of 4.5% (1/22) [
9]. On the other hand, Elamo et al., Su et al., and Slaven et al. al reported recurrence rates above 40% [
10,
11,
12]. These findings highlight the significant variability in recurrence rates observed across different patient populations and surgical techniques.
There is considerable variability in recurrence rates over time (see
Figure 2). In the last 5 years, there have been 4 studies on arthroscopic Bankart revisions that reported recurrence rates above 20%. When analyzing the conclusions, the majority of studies concluded that arthroscopic Bankart revision surgery is satisfactory and an appropriate treatment option for patients with recurrent shoulder instability. However, there were 2 studies by Slaven et al. and Elamo et al. that concluded revision Bankart procedures are not a viable option for recurrent instability due to the high recurrence rates [
10,
11]. In another study by O’Neill, they concluded that both a Bankart procedure and Latarjet procedure have poor outcomes [
13].
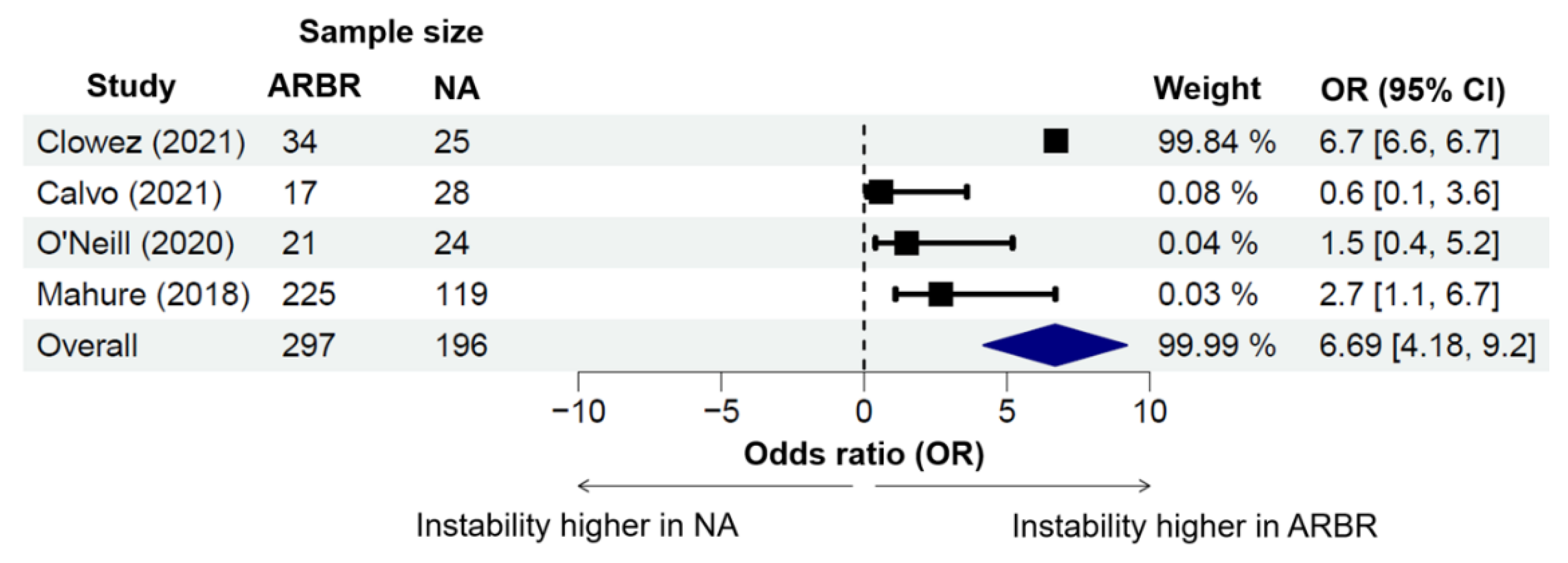
Five studies investigated recurrent instability between ARBR and non-anatomic stabilization techniques, with the majority examining the open Latarjet technique (see
Figure 5). Two studies had an open Latarjet recurrence rate of 0%, Clowez et al. (2021) and Elamo et al. (2020), leading to addition of a 0.5 zero-cell correction factor by the Mantel–Haenszel odds ratio method [
14]. The corrected odds ratio of Elamo et al. (2020) was approximately thirty, and given that the other studies’ odds ratios ranged from zero to seven, we excluded this value as an outlier [
10]. The pooled odds ratio for higher instability recurrence in ARBR was 6.69 (95% CI: 4.18-9.2).
Functional outcomes also offer important insights into the benefits of revision surgery for patients. The values consistently demonstrated improvements in the reported outcome measures following surgery. These findings suggest that arthroscopic Bankart repair can lead to positive functional outcomes, including improved shoulder stability and range of motion. Specifically, 13 studies reported on the patients returning to their sports. The rate of return to sport ranged from 50% to 91%. Four studies reported a return to sport rate exceeding 80%, indicating a favorable outcome [
15,
16,
17,
18]. Another approach to evaluating the impact on athletes is by assessing their strength, endurance, and range of motion. Bartl et al. conducted a study in which they observed significant improvements (p-value < .0001) in each of these categories following the revision compared to pre-revision measurements [
15].
Discussion
Addressing failed primary stabilization requires a thorough investigation to identify potential contributing factors. The population requiring revision surgery often presents with complicated anatomy resulting from previous repair attempts. These prior procedures can alter the normal anatomical structures, making subsequent surgeries more challenging. Scar tissue, compromised soft tissues, altered ligamentous integrity, and potential bone loss are common complexities that surgeons may encounter. The presence of these factors increases the difficulty of achieving optimal stability and functional outcomes during revision surgery.
In a cohort study conducted by Lee et al., comparing revision arthroscopic Bankart repair to the initial primary arthroscopic Bankart repair, the findings indicate that the only notable distinction in functional outcome scores was related to sports activity level. These results suggest that revision arthroscopic Bankart repair can yield highly favorable clinical outcomes [
19].
The literature consistently underscores the pivotal role of patient selection criteria in addressing shoulder instability, as evidenced by the international Delphi study [
2]. This aspect remains integral in our systematic review, where managing failed primary stabilization hinges on tackling underlying causes. Alongside patient selection, each surgical technique presents its own pros and cons. Our review found that both Bankart and Latarjet techniques significantly enhanced patient outcomes pre- and post-operatively. Our analysis aligns with Lho et al.'s findings that Latarjet have shown promising results compared to Bankart in terms of reduced instability and improved Rowe scores [
6]. Our systematic review found the Latarjet is a superior for recurrent instability following a Bankart repair. However, there was not a significant difference when a remplissage was incorporated. It's vital to acknowledge trade-offs, such as Latarjet's lower recurrence rates versus restricted motion and increased complications. Additionally, Lho et al.'s study lacks guidance on managing failed Latarjet procedures, highlighting a research gap [
6].
In addition, the management for recurrence is considerably different for a failed Bankart versus failed Latarjet technique. When a bone block fails, there are less available options for revision. Unlike a failed Bankart, there is not an option to perform the same procedure following a failure of a bone block. The systematic review by Baur et al. explored all the revision options and found variations of the Eden–Hybinette procedure are most commonly utilized in this unique situation. In their review, they ultimately found promising trends in a population with limited therapeutic options.
In our systematic review, we focused on critical bone lesions, finding no clear correlation between glenoid bone loss or Hill-Sachs lesions and recurrence rates. This lack of association may be influenced by reporting variations, especially when considering Hill-Sachs lesions. The papers were not consistent in reporting or defining the lesions of the humerus. Additionally, some papers did not detail encountered bone lesions at all.
Another aspect that could influence the validity of the bone lesion analysis, is the high variation in recurrence rates with significant outliers. Notably, three studies reported exceptionally high rates. These studies often had broad patient selection criteria. The Elamo study, for instance, compared revision arthroscopic Bankart repair with an open Latarjet repair. It's essential to note, however, that the follow-up period for the Bankart repair arm was significantly longer at 7.8 years compared to the Latarjet repair arm's 3.5 years. Furthermore, the Bankart repair group exhibited a higher participation rate in contact sports (26%) compared to the Latarjet group (15%). These discrepancies in follow-up duration and sports activity participation could have introduced bias into their conclusions, emphasizing the importance of interpreting their results cautiously.
Additionally, our systematic review encountered the study by Slaven et al., which strongly advised against revision arthroscopic stabilization. However, this study exhibited notable methodological flaws. The patient population was predominantly composed of young individuals, a recognized risk factor for failure. Furthermore, unlike other studies in this systematic review, the Slaven et al. study used remplissage sparingly, and interestingly, none of the patients who received remplissage (2 patients) experienced recurrence. These discrepancies emphasize the importance of considering the nuances in study design and patient characteristics when interpreting and applying study findings to clinical practice.
Despite the absence of a significant link, we advocate for further research specifically exploring the impact of bone lesions on stabilization failure. The high variability in inclusion and exclusion criteria among studies, along with diverse techniques used for arthroscopic soft tissue repair, necessitates additional research. Current studies should be carefully analyzed for treated pathology and specific procedures, as high recurrence rates may result from improper exclusion criteria or the omission of correct concomitant procedures. Specifically, future studies should compare arthroscopic Latarjet with arthroscopic Bankart and remplissage. Adherence to international Delphi study indications and clear description of inclusion/exclusion criteria for patients are crucial. Our study supports Hong et al's conclusion, emphasizing the need for clearer patient selection criteria to address high recurrence rates [
1].
In addition to bone lesions, our review uncovered studies emphasizing different factors contributing to failure. The study conducted by Park et al. focuses on the quality of the anterior capsulolabral complex. Their findings reveal that patients undergoing revision surgery with anterior capsular tears exhibit considerably higher failure rates compared to those with labral retears unaccompanied by capsular tears
26. Another study by Su et al. demonstrates a significant correlation between failure and the presence of off-track lesions, patients aged younger than 22, and ligamentous laxity [
12]. Additionally, an earlier investigation by Shin et al. identifies unidirectional and especially multidirectional hyperlaxity as a significant factor in recurrent instability. This study also highlights the influence of the number of prior surgeries on the recurrence rate [
20].
Although the specific procedures were extracted and listed for this systematic review, there is still variability in the concomitant procedures. Study heterogeneity was the main confounding factor, and differences existed in definitions of instability (apprehension, subluxation, or dislocation), cutoffs for critical glenoid bone loss, how studies report Hill-Sachs lesions (on-track vs. off-track, percent involvement of articular surface), and index surgeries (arthroscopic vs. open stabilization). The lack of a true control group in many studies limited the ability to calculate a pooled odds ratio for ARBR and recurrent instability.
Conclusions
Navigating the complexities of anatomical challenges stemming from previous repair attempts presents a formidable task in achieving optimal stability and functionality during revision surgery. Recurrence rates spanning 4.5% to 44% were observed in this systematic review, with caution warranted for studies exhibiting higher rates due to potential methodological shortcomings. The open Latarjet procedure had a significantly lower rate of recurrence compared to a revision arthroscopic Bankart. There was no difference when a remplissage was also completed. This systematic review also found no association between critical bone lesions such as glenoid bone loss or Hill-Sachs lesion and failure.
Future Directions
Further guidance in selecting the most effective technique for arthroscopic revision stabilization could be provided through additional cohort studies. Additionally, the absence of randomized controlled trials for revision shoulder arthroscopy is a significant limitation, and conducting such trials would be invaluable in this context. We recommend further research on the impact of bone lesions on stabilization failure, given the current lack of a significant link. Future studies should also specifically compare arthroscopic Latarjet with arthroscopic Bankart and remplissage with a hope of finding more clear patient selection criteria.
| STUDY |
PREOPERATIVE FINDINGS |
GLENOID DEFECT |
HUMERAL DEFECT |
PROCEDURE |
RECURRENCE RATE |
CONCLUSIONS |
|
LEE ET AL. [19] |
Primary Bankart- Glenoid defect 14.9%
Revision Bankart- Glenoid defect 15.6% |
Primary Bankart: Moderate
Revision Bankart: Severe |
NR |
Primary and Revision arthroscopic Bankart
Primary used remplissage 3/24
Revision used remplissage 8/24 |
Primary arthroscopic Bankart- 4.2% (1/24)
Revision arthroscopic Bankart- 12.5% (3/24) |
Clinical outcomes did not differ significantly between the primary repair group and revision group |
|
SLAVEN ET AL. [11] |
Successful revision- Glenoid bone loss 6.2% // Hill-sachs 19/23 // Off-track lesion 3/23
Failed revision- Glenoid bone loss 5.7% // Hill-sachs 15/18 // Off-track lesion 2/23 |
Successful revision: Mild
Failed revision: Mild |
Successful revision:
Mild
Failed revision: Mild |
Revsion arthroscopic Bankart
(2/41 remplissage) |
44% (18/41) |
There are very high rates of failure for revision arthroscopic procedures following a failed Bankart. These failures should not be attributed to the bone loss |
|
CLOWEZ ET AL. [17] |
Glenoid bone loss 18.5 %. // Hill-Sachs 51/59 |
Moderate |
Severe# |
Open and arthroscopic Latarjet |
7% (4/59) |
The Latarjet procedure is an efficient technique to restore shoulder stability following a failed Bankart with glenoid bone loss. |
|
CALVO ET AL. [21] |
Arthroscopic Bankart:
Glenoid bone defect (<15%) 7/17
Hill-Sachs 14/17
Arthroscopic Latarjet
Hill-Sachs 27/28
Glenoid bone defect (<15%) 15/28 |
Bankart: Mild
Latarjet: Mild |
NR |
Arthroscopic Latarjet |
Arthroscopic Bankart- 11.8% (2/17)
Arthroscopic Latarjet- 17.9% (5/28) |
Arthroscopic Latarjet did not lead to superior results compared to revision Bankart repair. |
|
SINHA ET AL. [18] |
Glenoid bone loss 17.6% |
Moderate |
NR |
Revision arthroscopic Bankart with remplissage |
7.2% (4/55) |
Revision Bankart repair with remplissage is a feasible option for recurrent shoulder instability |
|
PARK ET AL. [22] |
Capsular tear group- Glenoid bone defect 8.1%
Off track lesion 0/10
Labral tear- Glenoid bone defect 11.0% // Off-track lesion 8/45 |
Capsular tear: Mild
Labral tear: Moderate |
Capsular: Mild
Labral: Moderate |
Revision arthroscopic Bankart with remplissage |
Definite anterior capsular tears - 40% (4/10)
Labral retears- 11.1 % (5/45) |
Anterior capsular tear should be considered a factor for recurrence. |
|
ELAMO ET AL. [10] |
NR |
NR |
NR |
Revision arthroscopic Bankart
Open Latarjet |
Revision arthroscopic- 43% (13/30)
Open Latarjet- 0/18 |
Patient reported outcomes are poor after revision Bankart compared with revision Latarjet. |
|
O'NEILL ET AL. [13] |
Revision arthroscopy- Glenoid bone loss 16.58% // Off-track 7/21
Latarjet- Glenoid bone loss 20.42% // Off-track 15/24 |
Bankart: Moderate
Latarjet: Severe |
Bankart: Severe
Latarjet: Severe |
Revision arthroscopic Bankart
Open Latarjet |
Revision Bankart - 38.1% (8/21)
Latarjet 33.3% (7/21) |
Postoperative instability symptoms are common with both procedures. |
|
SU ET AL. [12] |
Glenoid bone defect 13.9% // Hill sachs lesion 30/65 // Off-track lesion 14/65 |
Moderate |
Moderate |
Revision arthroscopic Bankart |
38% (22/58) |
Arthroscopic revision stabilization is associated with a high rate of recurrent instability. |
|
MAHURE ET AL. [23] |
NR |
NR |
NR |
Revision arthroscopic Bankart
Open Latarjet |
Arthroscopic bankart -12.4% (28/225)
Open stabilization 5.1% (6/119) |
Revision arthroscopic Bankart repair had significantly higher rates of persistent instability than open revision procedures |
|
BUCKUP ET AL. [8] |
NR |
NR |
NR |
Revision arthroscopic Bankart |
7.6% (3/23) |
Athroscopic revision Bankart repair allows nonprofessional athletes to return to their sport. |
|
SHIN ET AL. [20] |
NR |
NR |
NR |
Revision arthroscopic Bankart |
15.2% (12/79) |
Revision arthroscopic anterior stabilization has satisfactory outcomes. |
|
NEVIASER ET AL. [24] |
No significant glenoid bone loss // Hill-Sachs lesion 30/30
Not deemed clinically significant |
Mild |
Mild |
Revision open Bankart |
0/30 |
The open Bankart repair offers a reliable, consistently successful option for revision |
|
ARCE ET AL. [25] |
NR |
NR |
NR |
Revision arthroscopic Bankart |
18.8% (3/16) |
Revision arthroscopic Bankart repair was associated with a low recurrence rate and restoration of acceptable function. |
|
BARTL ET AL. [15] |
Glenoid bone defect <10% -15/56
Glenoid bone defect 11-20% - 7/56 |
Mild |
NR |
Revision arthroscopic Bankart |
11% 6/56 |
Arthroscopic Bankart repair achieves results comparable with open revision repairs with a low recurrent instability rate. |
|
RYU ET AL. [26] |
Poorly tensioned capsule 9/15 // Hill sachs 14/15 // Glenoid bone loss >10% -5/15 |
Mild |
Mild |
Revision arthroscopic Bankart |
27% (4/15) |
Arthroscopic revision Bankart repair can be an effective alternative. |
|
BOILEAU ET AL. [9] |
Hill Sachs 14/22 (mild to moderate size) |
NR |
Mild |
Revision arthroscopic Bankart with capsular plication |
4.5% (1/22) |
Arthroscopic revision of failed open anterior shoulder stabilization provides satisfactory results. |
|
CHO ET AL. [16] |
Glenoid bone defect 10% 5/26
Glenoid bone defect 11-20 2/26
Engaging Hill-Sachs defect 4/26 |
Mild |
Mild |
Revision open Bankart |
11.5% (3/26) |
Open revision Bankart can provide a satisfactory outcome for failed arthroscopic Bankart repairs. |
|
NERI ET AL. [27] |
Hill Sachs 9/12 |
NR |
Moderate$
|
Revision arthroscopic Bankart |
25% (3/12) |
Arthroscopic revision Bankart repais can be used to achieve stable, pain-free, functional shoulders |
|
SISTO. [28] |
Hill Sachs (engaging) -0/30 |
NR |
Mild |
Revision open Bankart |
0/30 |
Patients with failed arthroscopic Bankart repairs can be treated with revision open Bankart repair. |
|
KIM ET AL. [29] |
Hill Sachs lesion grade III- 20/23
Glenoid defect 10% 7/23
Glenoid defect 11-20% 4/23
Glenoid defect >20% 3/23 |
Severe |
Severe |
Revision arthroscopic Bankart |
13% (3/23) |
Arthroscopic revision Bankart surgery can provide satisfactory outcome, with low recurrence rate. |
|
KREUGER ET AL. [30] |
Hill-Sachs grade 1 3/20
Hill-Sachs grade II 9/20
Hill-Sachs grade III 8/20 |
NR |
Severe |
Revision arthroscopic Bankart |
0/20 |
Arthroscopic revision stabilization is associated with a lower subjective outcome compared to initial stabilization. |
|
BARNES ET AL. [31] |
N/A |
NR |
NR |
Revision arthroscopic Bankart |
0/16 |
Arthroscopic revision anterior shoulder reconstruction is a viable alternative for patients who failed initial reconstruction |
|
FRANCESHI ET AL. [32] |
Hill-Sachs grade I (1/10)
Hill-Sachs grade II 2/10
Hill-Sachs grade III (3/10) |
|
Moderate |
Revision arthroscopic Bankart |
10% (1/10) |
Arthroscopic Bankart revision surgery is a reliable procedure. |
|
CREIGHTON ET AL. [33] |
N/A |
NR |
NR |
Revision arthroscopic Bankart |
17% (3/18) |
Arthroscopic revision instability repair results in satisfactory outcomes. |
Author Contributions
A.B. was responsible for study concept and methods design. data analysis, initial manuscript draft writing, manuscript editing, and figure and table creation. J.R. was responsible for data analysis, manuscript editing, and figure creation. W.B. was responsible for study concept and methods design and manuscript editing.
Conflicts of Interest
None of the authors have any relevant disclosures to report.
References
- Hong, I.S.; Sonnenfeld, J.J.; Sicat, C.S.; Hong, R.S.; Trofa, D.P.; Schiffern, S.C.; Hamid, N.; Fleischli, J.E.; Saltzman, B.M. Outcomes After Arthroscopic Revision Bankart Repair: An Updated Systematic Review of Recent Literature. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2023, 39, 438–451. [Google Scholar] [CrossRef] [PubMed]
- Hurley, E.T.; Matache, B.A.; Wong, I.; Itoi, E.; Strauss, E.J.; Delaney, R.A.; Neyton, L.; Athwal, G.S.; Pauzenberger, L.; Mullett, H.; et al. Anterior Shoulder Instability Part I—Diagnosis, Nonoperative Management, and Bankart Repair—An International Consensus Statement. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2022, 38, 214–223.e7. [Google Scholar] [CrossRef]
- Hurley, E.T.; Matache, B.A.; Wong, I.; Itoi, E.; Strauss, E.J.; Delaney, R.A.; Neyton, L.; Athwal, G.S.; Pauzenberger, L.; Mullett, H.; et al. Anterior Shoulder Instability Part II—Latarjet, Remplissage, and Glenoid Bone-Grafting—An International Consensus Statement. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2022, 38, 224–233.e6. [Google Scholar] [CrossRef] [PubMed]
- Fares, M.Y.; Daher, M.; Boufadel, P.; Haikal, E.R.; Koa, J.; Singh, J.; Abboud, J.A. Arthroscopic Remplissage: History, Indications, and Clinical Outcomes. Clin Shoulder Elb 2023. [CrossRef] [PubMed]
- Rashid, M.S.; Tsuchiya, S.; More, K.D.; LeBlanc, J.; Bois, A.J.; Kwong, C.A.; Lo, I.K.Y. Validating the Glenoid Track Concept Using Dynamic Arthroscopic Assessment. Orthopaedic Journal of Sports Medicine 2024, 12, 23259671241226943. [Google Scholar] [CrossRef] [PubMed]
- Lho, T.; Lee, J.; Oh, K.-S.; Chung, S.W. Latarjet Procedure for Failed Bankart Repair Provides Better Stability and Return to Sports, but Worse Postoperative Pain and External Rotation Limitations with More Complications, Compared to Revision Bankart Repair: A Systematic Review and Meta-Analysis. Knee Surg Sports Traumatol Arthrosc 2023, 31, 3541–3558. [Google Scholar] [CrossRef] [PubMed]
- Baur, A.; Satalich, J.; O’Connell, R.; Vap, A. Surgical Management of Recurrent Instability Following Latarjet Procedure – A Systematic Review of Salvage Procedures. Shoulder & Elbow 2024, 16, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Buckup, J.; Welsch, F.; Gramlich, Y.; Hoffmann, R.; Roessler, P.P.; Schüttler, K.F.; Stein, T. Back to Sports After Arthroscopic Revision Bankart Repair. Orthopaedic Journal of Sports Medicine 2018, 6, 232596711875545. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Richou, J.; Lisai, A.; Chuinard, C.; Bicknell, R.T. The Role of Arthroscopy in Revision of Failed Open Anterior Stabilization of the Shoulder. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2009, 25, 1075–1084. [Google Scholar] [CrossRef] [PubMed]
- Elamo, S.; Selänne, L.; Lehtimäki, K.; Kukkonen, J.; Hurme, S.; Kauko, T.; Äärimaa, V. Bankart versus Latarjet Operation as a Revision Procedure after a Failed Arthroscopic Bankart Repair. JSES International 2020, 4, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Slaven, S.E.; Donohue, M.A.; Tardif, R.A.; Foley, K.A.; LeClere, L.E.; Cameron, K.L.; Giuliani, J.R.; Posner, M.A.; Dickens, J.F. Revision Arthroscopic Bankart Repair Results in High Failure Rates and a Low Return to Duty Rate Without Recurrent Instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2023, 39, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Su, F.; Kowalczuk, M.; Ikpe, S.; Lee, H.; Sabzevari, S.; Lin, A. Risk Factors for Failure of Arthroscopic Revision Anterior Shoulder Stabilization. The Journal of Bone and Joint Surgery 2018, 100, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, D.C.; Christensen, G.; Kawakami, J.; Burks, R.T.; Greis, P.E.; Tashjian, R.Z.; Chalmers, P.N. Revision Anterior Glenohumeral Instability: Is Arthroscopic Treatment an Option? JSES International 2020, 4, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Bradburn, M.J.; Deeks, J.J.; Berlin, J.A.; Russell Localio, A. Much Ado about Nothing: A Comparison of the Performance of Meta-analytical Methods with Rare Events. Statistics in Medicine 2007, 26, 53–77. [Google Scholar] [CrossRef] [PubMed]
- Bartl, C.; Schumann, K.; Paul, J.; Vogt, S.; Imhoff, A.B. Arthroscopic Capsulolabral Revision Repair for Recurrent Anterior Shoulder Instability. Am J Sports Med 2011, 39, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Cho, N.S.; Yi, J.W.; Lee, B.G.; Rhee, Y.G. Revision Open Bankart Surgery After Arthroscopic Repair for Traumatic Anterior Shoulder Instability. Am J Sports Med 2009, 37, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Clowez, G.; Gendre, P.; Boileau, P. The Bristow-Latarjet Procedure for Revision of Failed Arthroscopic Bankart: A Retrospective Case Series of 59 Consecutive Patients. Journal of Shoulder and Elbow Surgery 2021, 30, e724–e731. [Google Scholar] [CrossRef] [PubMed]
- Sinha, S.; Mehta, N.; Goyal, R.; Goyal, A.; Joshi, D.; Arya, R.K. Is Revision Bankart Repair with Remplissage a Viable Option for Failed Bankart Repair in Non-Contact Sports Person Aiming to Return to Sports? IJOO 2021, 55, 359–365. [Google Scholar] [CrossRef]
- Lee, H.-M.; Lim, J.-R.; Lee, W.-W.; Kim, S.-J.; Yoon, T.-H.; Chun, Y.-M. Comparison of Arthroscopic Primary and Revision Bankart Repair for Capsulolabral Restoration: A Matched-Pair Analysis. Arch Orthop Trauma Surg 2022, 143, 3183–3190. [Google Scholar] [CrossRef]
- Shin, J.J.; Mascarenhas, R.; Patel, A.V.; Yanke, A.B.; Nicholson, G.P.; Cole, B.J.; Romeo, A.A.; Verma, N.N. Clinical Outcomes Following Revision Anterior Shoulder Arthroscopic Capsulolabral Stabilization. Arch Orthop Trauma Surg 2015, 135, 1553–1559. [Google Scholar] [CrossRef] [PubMed]
- Calvo, E.; Luengo, G.; Morcillo, D.; Foruria, A.M.; Valencia, M. Revision Arthroscopic Bankart Repair Versus Arthroscopic Latarjet for Failed Primary Arthroscopic Stabilization With Subcritical Bone Loss. Orthopaedic Journal of Sports Medicine 2021, 9, 232596712110018. [Google Scholar] [CrossRef]
- Park, I.; Lee, J.-H.; Park, J.-Y.; Shin, S.-J. Failure Rates After Revision Arthroscopic Stabilization for Recurrent Anterior Shoulder Instability Based on Anterior Capsulolabral Complex Conditions. Orthopaedic Journal of Sports Medicine 2021, 9, 232596712199589. [Google Scholar] [CrossRef]
- Mahure, S.A.; Mollon, B.; Capogna, B.M.; Zuckerman, J.D.; Kwon, Y.W.; Rokito, A.S. Risk Factors for Recurrent Instability or Revision Surgery Following Arthroscopic Bankart Repair. The Bone & Joint Journal 2018, 100-B, 324–330. [Google Scholar] [CrossRef]
- Neviaser, A.S.; Benke, M.T.; Neviaser, R.J. Open Bankart Repair for Revision of Failed Prior Stabilization: Outcome Analysis at a Mean of More than 10 Years. Journal of Shoulder and Elbow Surgery 2015, 24, 897–901. [Google Scholar] [CrossRef]
- Arce, G.; Arcuri, F.; Ferro, D.; Pereira, E. Is Selective Arthroscopic Revision Beneficial for Treating Recurrent Anterior Shoulder Instability? Clinical Orthopaedics & Related Research 2012, 470, 965–971. [Google Scholar] [CrossRef]
- Ryu, R.K.N.; Ryu, J.H. Arthroscopic Revision Bankart Repair: A Preliminary Evaluation. Orthopedics 2011, 34, 01477447–20101123-11. [Google Scholar] [CrossRef]
- Neri, B.R.; Tuckman, D.V.; Bravman, J.T.; Yim, D.; Sahajpal, D.T.; Rokito, A.S. Arthroscopic Revision of Bankart Repair. Journal of Shoulder and Elbow Surgery 2007, 16, 419–424. [Google Scholar] [CrossRef]
- Sisto, D.J. Revision of Failed Arthroscopic Bankart Repairs. Am J Sports Med 2007, 35, 537–541. [Google Scholar] [CrossRef]
- Kim, S.-H.; Ha, K.-I.; Kim, Y.-M. Arthroscopic Revision Bankart Repair. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2002, 18, 469–482. [Google Scholar] [CrossRef]
- Krueger, D.; Kraus, N.; Pauly, S.; Chen, J.; Scheibel, M. Subjective and Objective Outcome After Revision Arthroscopic Stabilization for Recurrent Anterior Instability Versus Initial Shoulder Stabilization. Am J Sports Med 2011, 39, 71–77. [Google Scholar] [CrossRef]
- Barnes, C.J.; Getelman, M.H.; Snyder, S.J. Results of Arthroscopic Revision Anterior Shoulder Reconstruction. Am J Sports Med 2009, 37, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, F.; Longo, U.G.; Ruzzini, L.; Rizzello, G.; Maffulli, N.; Denaro, V. Arthroscopic Salvage of Failed Arthroscopic Bankart Repair: A Prospective Study with a Minimum Follow-up of 4 Years. Am J Sports Med 2008, 36, 1330–1336. [Google Scholar] [CrossRef] [PubMed]
- Creighton, R.A.; Romeo, A.A.; Brown, F.M.; Hayden, J.K.; Verma, N.N. Revision Arthroscopic Shoulder Instability Repair. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2007, 23, 703–709. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).