1. Introduction
Papillary thyroid carcinoma (PTC) possesses a significant health challenge, particularly among women who exhibit an increased incidence rate when compared to men [
1]. Although mortality rates are low relative to other types of cancer, PTC is particularly susceptible to recurrence [
2,
3]. Furthermore, Hispanic women in the United States have a disproportionately higher likelihood of experiencing recurrent PTC compared to their non-Hispanic counterparts [
4]. However, despite this increased susceptibility to advanced disease, Hispanics paradoxically exhibit lower mortality rates [
5].
Coagulation factor X (FX), encoded by the gene F10, is traditionally recognized for its role in the coagulation cascade yet has garnered attention in recent cancer research due to its involvement in tumor progression [
6]. Recent research has demonstrated interest in F10 expression in PTC [
7] The findings from prior investigations, which demonstrate the detection of FX mRNA within cancerous tissue, suggest the potential for malignant cells to produce this coagulation factor [
8]. Mechanistically, FX may promote tumor angiogenesis by activating proangiogenic factors such as vascular endothelial growth factor and promoting endothelial cell migration and tube formation [
9,
10]. Notably, FX has demonstrated evidence of inhibiting cancer cell migration as well, suggesting a multifaceted involvement in cancer progression [
11].
We hypothesize that ethnic disparities in PTC incidence and prognosis may be attributed to differential expression of FX, which will be manifested in F10 gene expression. In this study we demonstrated that lower gene expression levels in F10 correlate to the increased risk of advanced disease and lower disease-free rates observed among Hispanic women with PTC compared to non-Hispanic women.
2. Materials and Methods
Clinical data and expression values for F10 in White female patients, both Hispanic and non-Hispanic, (Thyroid Carcinoma The Cancer Genome Atlas Program (TCGA) Provisional for Cancer Genomes, mRNA expression (RNA Seq V2 RSEM)) were obtained from the cBioPortal for cancer genomics (
http://www.cbioportal.org) [
12,
13], which contains annotated TCGA data. Papillary thyroid cancer (TCGA, Firehose Legacy) mRNA expression dataset, containing 192 samples, were directly downloaded from the cBioPortal on February 29, 2024.
RNA sequencing values were log2-transformed to model proportional changes. Unpaired t-tests were employed to assess the significance of differences in gene expression between groups with recurrent PTC and disease-free status. A p-value threshold of <0.05 was considered statistically significant. Unpaired t-tests were employed to evaluate significance for both gene expression and disease-free status.
To assess the impact of gene expression levels on recurrence rates, log-rank (Mantel-Cox) tests were performed. Genes were categorized into high-expression and low-expression groups using both the median as a cutoff as well as ± 1.5 z-scores. Additionally, the Gehan-Breslow-Wilcoxon test was utilized to assess differences in survival curves between these groups. Hazard ratios (HR) were calculated to quantify the risk of recurrence associated with high and low gene expression levels. The Mantel-Haenszel method and log-rank test were utilized to compute HR, with confidence intervals (CI) of 95%. All statistical analyses were conducted using GraphPad Prism 9.1.0 software.
3. Results
3.1. Analysis of Gene Expression Differences in Disease-Free and Recurrent Papillary Thyroid Carcinoma
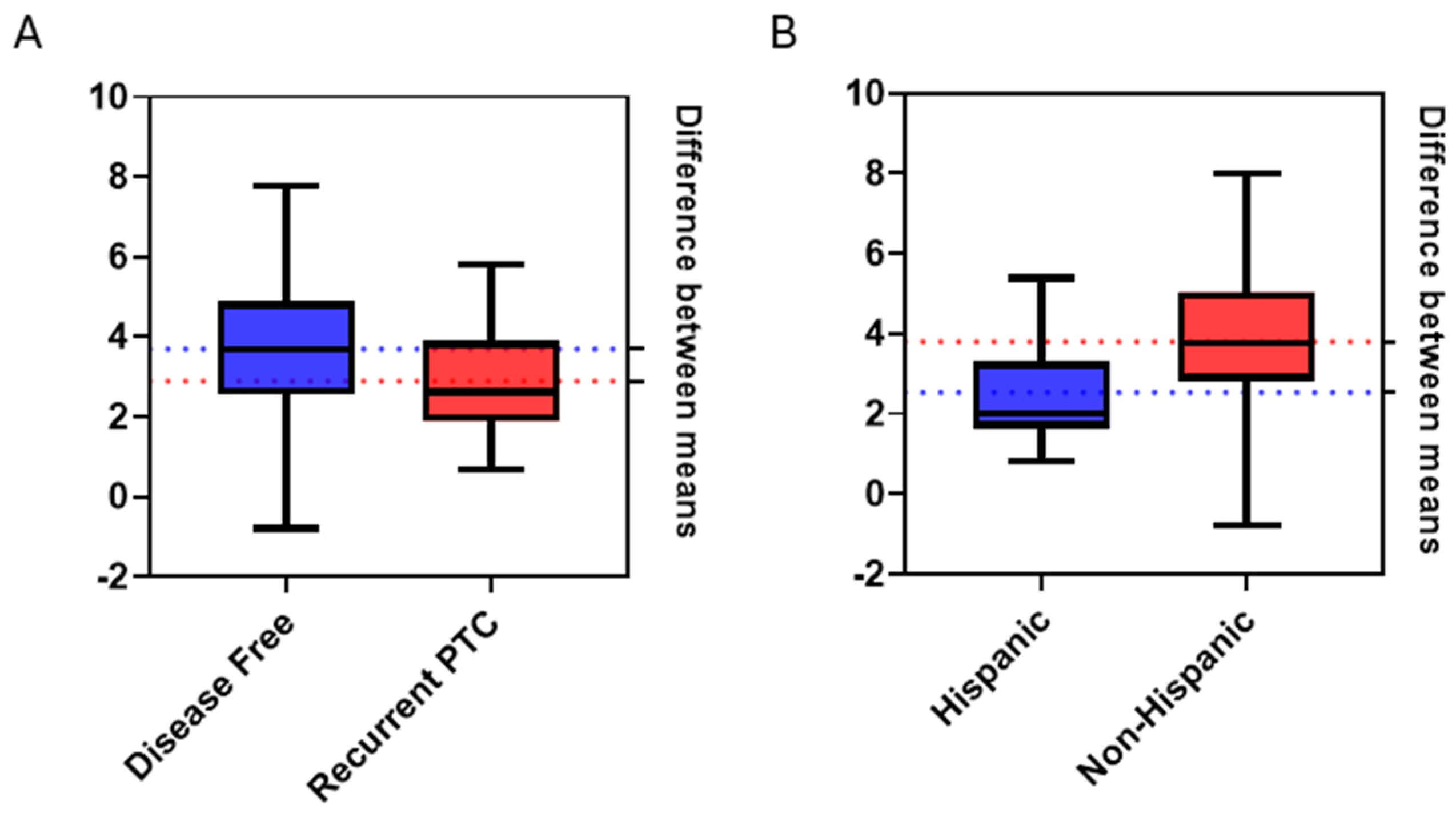
Analysis of F10 mRNA expression data without regarding any specific timeframe, by means of unpaired t-test, revealed statistically significant differences in gene expression values between groups of patients remaining disease-free and those experiencing recurrence. (
Figure 1A). In the disease-free group comprising 162 patients and the recurrent PTC group consisting of 22 patients, differences in disease status yielded a t-value of 2.18 (p=0.03). Specifically, disease-free patients showed a 2.06-fold increase in F10 mRNA expression compared to patients who experienced recurrence.
Employing a point-biserial correlation test also yielded significant results (p = 0.001) between F10 expression levels and disease-free status within a 5-year period. A correlation coefficient of -0.248 was found, indicating a moderate negative correlation between F10 gene expression and the incidence of recurrence. This observation aligns with our previous findings indicating that decreased F10 expression is linked to an elevated risk of disease recurrence in PTC patients.
3.2. Ethnic Disparities in Gene Expression Profiles
Further analysis, by means of unpaired t-test, was performed on the log2-transformed F10 gene expression data divided into two ethnic groups: 25 Hispanic and 166 non-Hispanic patients (
Figure 1B). A statistically significant difference in F10 expression was observed between Hispanics and non-Hispanics (p = 0.0003), with a t-value of 3.69. This difference corresponded to a 1.74-fold increase in F10 expression in non-Hispanic patients compared to Hispanic patients.
A point-biserial correlation test showed a negative correlation between the F10 gene expression and Hispanic patients, with a correlation coefficient of -0.169 (p = 0.019). This finding further supported ethnic disparities demonstrated in F10 gene expression from the unpaired t-test.
3.3. Comparison of Overall Survival Curves
Survival analysis was performed to assess the impact of F10 expression on patient outcomes in recurrent PTC. Both the log-rank test and Gehan-Breslow-Wilcoxon test were conducted to compare the overall survival (OS) curves between 192 patients. Based on the analysis of overall survival, both the log-rank test and the Gehan-Breslow-Wilcoxon test yielded non-significant results. The log-rank test produced a chi-square value of 0.02086 with a p-value of 0.8852, while the Gehan-Breslow-Wilcoxon test resulted in a chi-square value of 0.001909 with a p-value of 0.9652. These values confirmed no significant differences in OS curves between Hispanic and non-Hispanic patients.
3.4. Comparison of Recurrence-Free Survival Curves
To assess recurrence probability, patients were divided into high and low expression groups using mRNA expression z-scores above and below the median respectively (
Figure 2). Based on the recurrence-free survival (RFS) analysis results, there was a notable difference observed in the RFS curves between patients with low and high F10 expression levels. The log-rank test yielded a chi-square value of 3.301 with a corresponding p-value of 0.0692. However, the Gehan-Breslow-Wilcoxon test showed a χ² value of 4.477 and a p-value of 0.0344, indicating a significant difference in RFS curves between the two expression groups. Furthermore, the HR analysis showed a ratio of 2.179, indicating a higher risk of recurrence in patients with low F10 expression compared to those with high expression. Conversely, the reciprocal of this ratio was 0.4590, suggesting a reduced risk of recurrence in patients with high F10 expression. Additionally, the HR calculated using the log-rank method revealed similar findings, with a ratio of 2.321 indicating a lower risk in patients with high F10 expression and a reciprocal of 0.4308 indicating a higher risk in patients with low F10 expression.
High and low expression groups were further dichotomized using z-scores of ± 1.5 relative to all samples. While analyzing 5-year recurrence rates, the log-rank test revealed a statistically significant difference in recurrence between patients with low and high F10 expression (χ² = 5.003, p = 0.0253). Similarly, the Gehan-Breslow-Wilcoxon test confirmed this finding, demonstrating a significant divergence in survival curves (χ² = 4.918, p = 0.0266). In comparison to high and low expression groups defined by the median, ± 1.5 z-score groups yielded more significant results further highlighting the role F10 may play in recurrent PTC.
HR were calculated to quantify the risk of recurrent papillary thyroid cancer associated with high F10 expression compared to low expression. The Mantel-Haenszel method yielded a HR of 14.43 (95% CI: 1.391 to 149.6), indicating a substantially elevated risk of recurrence in patients with low F10 gene expression. Conversely, the reciprocal of the hazard ratio was 0.06932 (95% CI: 0.006685 to 0.7188), signifying a markedly reduced risk of recurrence in patients with low F10 gene expression.
4. Discussion
The disparities in the incidence, progression, and prognosis of cancer among different ethnic groups, particularly Hispanic and non-Hispanic populations, have long been recognized but poorly understood [
14,
15]. Our investigation of the distinct expression patterns suggests a decreased level of F10 expression in PTC cases increases susceptibility to recurrence. Furthermore, a similar decrease in F10 expression seems evident among Hispanic patients diagnosed with PTC in comparison to their non-Hispanic counterparts. Considering the higher reported rates of recurrence in Hispanic women, this investigation highlights these disparities in PTC and supports the importance of considering ethnic diversity in cancer research and clinical practice [
4].
Importantly, our study unveils a potential link between F10 expression levels and disease recurrence in PTC, with lower F10 expression associated with an increased risk of recurrence. This finding suggests prognostic value of F10 and the potential utility of F10 as a biomarker for risk stratification and treatment decision-making in PTC patients. Moreover, the observed ethnic disparities in F10 expression levels underscore the importance of accounting for genetic and environmental factors that may contribute to differential cancer susceptibility and outcomes among diverse populations.
The observed decrease in F10 expression levels among Hispanic patients compared to non-Hispanic counterparts prompts critical reflections on the multifaceted roles of FX in cancer biology. Our findings align with studies done on colon, lung and breast cancer cells that suggest FX may have a protective role against cancer progression [
11]. It is plausible that this could be explained by the role FX plays in inflammation and the activation of protease-activated receptors (PAR) [
16,
17]. PAR activation has been associated with a reduction in autophagy and could therefore contribute to increased rates of recurrence in cancer; particularly, this is the case when considering that reduced autophagy is a risk factor for tumor recurrence [
18,
19,
20].
Our study is not without limitations, however. One notable limitation is the assumption that gene expression levels directly translate into protein expression and functional outcomes. Although we observed statistically significant differences in F10 mRNA expression between patients with recurrent PTC and those remaining disease-free, we did not directly measure protein expression levels or functional activity of FX in tumor progression. This discrepancy between gene expression and protein expression/function could be influenced by post-transcriptional and post-translational regulatory mechanisms, such as alternative splicing, mRNA stability, translation efficiency, and protein degradation rates. More research is needed to fully understand the mechanisms and associations and further investigations are needed to delineate the functional significance of F10 dysregulation in PTC progression and its potential as a therapeutic target.
In conclusion, our study provides compelling evidence of ethnic disparities in F10 expression patterns in PTC and highlights the prognostic significance of F10 in disease recurrence. The study revealed a relationship between low expression of F10 and higher rates of recurrence observed in the Hispanic patient cohort compared to non-Hispanics. Our findings suggest there exists significance of F10 as a molecular determinant contributing to ethnic variations in PTC outcomes.
Author Contributions
Conceptualization, T.P.; methodology, T.P.; validation, L.K.; formal analysis, T.P.; investigation, T.P.; data curation, T.P.; writing—original draft preparation, T.P.; writing—review and editing, L.K.; visualization, T.P.; supervision, L.K.; project administration, T.P.; funding acquisition, L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by PRSTRT2022 and NIH Grant 1R15CA287203.
Institutional Review Board Statement
This study did not require ethical approval.
Data Availability Statement
The data generated in this study are available within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Siegel, R. L.; Miller, K. D.; Fuchs, H. E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J Clin 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Pizzato, M.; Li, M.; Vignat, J.; Laversanne, M.; Singh, D.; La Vecchia, C.; Vaccarella, S. The Epidemiological Landscape of Thyroid Cancer Worldwide: GLOBOCAN Estimates for Incidence and Mortality Rates in 2020. Lancet Diabetes Endocrinol 2022, 10, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Grant, C. S. Recurrence of Papillary Thyroid Cancer after Optimized Surgery. Gland Surg 2015, 4, 52–62. [Google Scholar] [PubMed]
- Papaleontiou, M.; Evron, J. M.; Esfandiari, N. H.; Reyes-Gastelum, D.; Ward, K. C.; Hamilton, A. S.; Worden, F.; Haymart, M. R. Patient Report of Recurrent and Persistent Thyroid Cancer. Thyroid 2020, 30, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Bonner, A.; Herring, B.; Wang, R.; Gillis, A.; Zmijewski, P.; Lindeman, B.; Fazendin, J.; Chen, H. The Association of Socioeconomic Factors and Well-Differentiated Thyroid Cancer. J Surg Res 2023, 283, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Arce, M.; Pinto, M. P.; Galleguillos, M.; Muñoz, C.; Lange, S.; Ramirez, C.; Erices, R.; Gonzalez, P.; Velasquez, E.; Tempio, F.; Lopez, M. N.; Salazar-Onfray, F.; Cautivo, K.; Kalergis, A. M.; Cruz, S.; Lladser, Á.; Lobos-González, L.; Valenzuela, G.; Olivares, N.; Sáez, C.; Koning, T.; Sánchez, F. A.; Fuenzalida, P.; Godoy, A.; Contreras Orellana, P.; Leyton, L.; Lugano, R.; Dimberg, A.; Quest, A. F. G.; Owen, G. I. Coagulation Factor Xa Promotes Solid Tumor Growth, Experimental Metastasis and Endothelial Cell Activation. Cancers (Basel) 2019, 11, 1103. [Google Scholar] [CrossRef]
- Zhong, L.-K.; Gan, X.-X.; Deng, X.-Y.; Shen, F.; Feng, J.-H.; Cai, W.-S.; Liu, Q.-Y.; Miao, J.-H.; Zheng, B.-X.; Xu, B. Potential Five-mRNA Signature Model for the Prediction of Prognosis in Patients with Papillary Thyroid Carcinoma. Oncol Lett 2020, 20, 2302–2310. [Google Scholar] [CrossRef] [PubMed]
- Sierko, E.; Wojtukiewicz, M. Z.; Zimnoch, L.; Tokajuk, P.; Ostrowska-Cichocka, K.; Kisiel, W. Co-Localization of Protein Z, Protein Z-Dependent Protease Inhibitor and Coagulation Factor X in Human Colon Cancer Tissue: Implications for Coagulation Regulation on Tumor Cells. Thromb Res 2012, 129, e112–118. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A. A.; Shaker, B. T.; Bajou, K. The Plasminogen–Activator Plasmin System in Physiological and Pathophysiological Angiogenesis. Int J Mol Sci 2021, 23, 337. [Google Scholar] [CrossRef]
- Bluff, J. E.; Brown, N. J.; Reed, M. W. R.; Staton, C. A. Tissue Factor, Angiogenesis and Tumour Progression. Breast Cancer Res 2008, 10, 204. [Google Scholar] [CrossRef] [PubMed]
- Borensztajn, K.; Bijlsma, M. F.; Reitsma, P. H.; Peppelenbosch, M. P.; Spek, C. A. Coagulation Factor Xa Inhibits Cancer Cell Migration via Protease-Activated Receptor-1 Activation. Thromb Res 2009, 124, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B. E.; Sumer, S. O.; Aksoy, B. A.; Jacobsen, A.; Byrne, C. J.; Heuer, M. L.; Larsson, E.; Antipin, Y.; Reva, B.; Goldberg, A. P.; Sander, C.; Schultz, N. The cBio Cancer Genomics Portal: An Open Platform for Exploring Multidimensional Cancer Genomics Data. Cancer Discov 2012, 2, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Aksoy, B. A.; Dogrusoz, U.; Dresdner, G.; Gross, B.; Sumer, S. O.; Sun, Y.; Jacobsen, A.; Sinha, R.; Larsson, E.; Cerami, E.; Sander, C.; Schultz, N. Integrative Analysis of Complex Cancer Genomics and Clinical Profiles Using the cBioPortal. Sci Signal 2013, 6, p11. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Gomez, S. J.; Sanabria-Salas, M. C.; Fejerman, L. Breast Cancer Health Disparities in Hispanics/Latinas. Curr Breast Cancer Rep 2020, 12, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Miller, K. D.; Ortiz, A. P.; Pinheiro, P. S.; Bandi, P.; Minihan, A.; Fuchs, H. E.; Martinez Tyson, D.; Tortolero-Luna, G.; Fedewa, S. A.; Jemal, A. M.; Siegel, R. L. Cancer Statistics for the US Hispanic/Latino Population, 2021. CA Cancer J Clin 2021, 71, 466–487. [Google Scholar] [CrossRef] [PubMed]
- Rothmeier, A. S.; Ruf, W. Protease-Activated Receptor 2 Signaling in Inflammation. Semin Immunopathol 2012, 34, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Krupiczojc, M. A.; Scotton, C. J.; Chambers, R. C. Coagulation Signalling Following Tissue Injury: Focus on the Role of Factor Xa. Int J Biochem Cell Biol 2008, 40, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Zhang, T.; Xiao, X.; Shi, Y.; Duan, H.; Ren, Y. Protease-Activated Receptor-2 Promotes Kidney Tubular Epithelial Inflammation by Inhibiting Autophagy via the PI3K/Akt/mTOR Signalling Pathway. Biochem J 2017, 474, 2733–2747. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-D.; Wang, C.-C.; Tsai, M.-C.; Wu, C.-H.; Yang, H.-J.; Chen, L.-Y.; Nakano, T.; Goto, S.; Huang, K.-T.; Hu, T.-H.; Chen, C.-L.; Lin, C.-C. Interconnections between Autophagy and the Coagulation Cascade in Hepatocellular Carcinoma. Cell Death Dis 2014, 5, e1244. [Google Scholar] [CrossRef] [PubMed]
- Aqbi, H. F.; Tyutyunyk-Massey, L.; Keim, R. C.; Butler, S. E.; Thekkudan, T.; Joshi, S.; Smith, T. M.; Bandyopadhyay, D.; Idowu, M. O.; Bear, H. D.; Payne, K. K.; Gewirtz, D. A.; Manjili, M. H. Autophagy-Deficient Breast Cancer Shows Early Tumor Recurrence and Escape from Dormancy. Oncotarget 2018, 9, 22113–22122. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).