Submitted:
20 April 2024
Posted:
23 April 2024
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
2. Materials and Methods
| Cancer | Mean rate (cases/100,000/yr) | |
|---|---|---|
| Males | Females | |
| Bladder, urinary | 37 | 9 |
| Brain | 9 | 6 |
| Breast | 133 | |
| Colorectal | 42 | 32 |
| Corpus uteri | 28 | |
| Esophageal | 9 | 2 |
| Gastric | 7 | 3 |
| Hodgkin’s lymphoma | 3 | 3 |
| Laryngeal | 5 | 1 |
| Leukemia | 19 | 11 |
| Liver | 11 | 4 |
| Lung | 64 | 34 |
| Myeloma | 8 | 5 |
| Non-Hodgkin’s lymphoma | 24 | 16 |
| Oral cavity | 20 | 7 |
| Ovarian | 10 | |
| Pancreatic | 15 | 11 |
| prostate | 105 | |
| Renal | 24 | 12 |
3. Results
4. Discussion
4.1. Diet
4.2. Cigarette Smoking
4.3. Particulate Air Pollution
4.4. Solar UVB and Vitamin D
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Xu, J.; Murphy, S.L.; Kochanek, K.D.; Arias, E. Mortality in the United States, 2021. NCHS Data Brief 2022, 1–8. [Google Scholar]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J Clin 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Gnagnarella, P.; Muzio, V.; Caini, S.; Raimondi, S.; Martinoli, C.; Chiocca, S.; Miccolo, C.; Bossi, P.; Cortinovis, D.; Chiaradonna, F.; et al. Vitamin D Supplementation and Cancer Mortality: Narrative Review of Observational Studies and Clinical Trials. Nutrients 2021, 13, 3285. [Google Scholar] [CrossRef] [PubMed]
- Kulhanova, I.; Znaor, A.; Shield, K.D.; Arnold, M.; Vignat, J.; Charafeddine, M.; Fadhil, I.; Fouad, H.; Al-Omari, A.; Al-Zahrani, A.S.; et al. Proportion of cancers attributable to major lifestyle and environmental risk factors in the Eastern Mediterranean region. Int J Cancer 2020, 146, 646–656. [Google Scholar] [CrossRef] [PubMed]
- Garland, C.F.; Garland, F.C. Do sunlight and vitamin D reduce the likelihood of colon cancer? Int J Epidemiol 1980, 9, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer 2002, 94, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Garland, C.F. The association of solar ultraviolet B (UVB) with reducing risk of cancer: multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res 2006, 26, 2687–2699. [Google Scholar] [PubMed]
- Boscoe, F.P.; Schymura, M.J. Solar ultraviolet-B exposure and cancer incidence and mortality in the United States, 1993-2002. BMC Cancer 2006, 6, 264. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Clements, M.; Rahman, B.; Zhang, S.; Qiao, Y.; Armstrong, B.K. Relationship between cancer mortality/incidence and ambient ultraviolet B irradiance in China. Cancer Causes Control 2010, 21, 1701–1709. [Google Scholar] [CrossRef]
- Borisenkov, M.F. Latitude of residence and position in time zone are predictors of cancer incidence, cancer mortality, and life expectancy at birth. Chronobiol Int 2011, 28, 155–162. [Google Scholar] [CrossRef]
- Grant, W.B. Role of solar UVB irradiance and smoking in cancer as inferred from cancer incidence rates by occupation in Nordic countries. Dermatoendocrinol 2012, 4, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef] [PubMed]
- Herman, J.R.; Krotkov, N.; Celarier, E.; Larko, D.; Lebow, G. Distribution of UV radiation at the Earth’s surface from TOMSmeasured UV-backscattered radiances. Journal of Geophysical Research 1999, 104, 59–76. [Google Scholar] [CrossRef]
- Devesa, S.S.; Grauman, D.J.; Blot, W.J.; Pennello, G.A.; Hoover, R.N.; Fraumeni, J.F., Jr. Atlas of Cancer Mortality in the United States, 1950–1994; National Institutes of Health; National Cancer Institue, 1999. [Google Scholar]
- Group, U.S.C.S.W. U.S. Cancer Statistics Data Visualizations Tool, based on 2022 submission data (1999-2020). Available online: https://www.cdc.gov/cancer/dataviz (accessed on 15 March 2024).
- CDC. National Program of Cancer Registries. Availabe online: https://www.cdc.gov/cancer/npcr/index.htm (accessed on.
- National Cancer Institute, S., Epidemiology, and End Results (SEER) Program. Overview of the SEER Program. Available online: https://seer.cancer.gov/about/overview.html (accessed on 12 April 2024).
- Hypponen, E.; Power, C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr 2007, 85, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Kroll, M.H.; Bi, C.; Garber, C.C.; Kaufman, H.W.; Liu, D.; Caston-Balderrama, A.; Zhang, K.; Clarke, N.; Xie, M.; Reitz, R.E.; et al. Temporal relationship between vitamin D status and parathyroid hormone in the United States. PLoS One 2015, 10, e0118108. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.S.; Rybchyn, M.S.; Abboud, M.; Brennan-Speranza, T.C.; Fraser, D.R. The Role of Skeletal Muscle in Maintaining Vitamin D Status in Winter. Curr Dev Nutr 2019, 3, nzz087. [Google Scholar] [CrossRef] [PubMed]
- Rybchyn, M.S.; Abboud, M.; Puglisi, D.A.; Gordon-Thomson, C.; Brennan-Speranza, T.C.; Mason, R.S.; Fraser, D.R. Skeletal Muscle and the Maintenance of Vitamin D Status. Nutrients 2020, 12, 3270. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. Air pollution in relation to U.S. cancer mortality rates: an ecological study; likely role of carbonaceous aerosols and polycyclic aromatic hydrocarbons. Anticancer Res 2009, 29, 3537–3545. [Google Scholar]
- Moore, J.X.; Akinyemiju, T.; Wang, H.E. Pollution and regional variations of lung cancer mortality in the United States. Cancer Epidemiol 2017, 49, 118–127. [Google Scholar] [CrossRef]
- Sun, Y.; Li, Z.; Li, J.; Li, Z.; Han, J. A Healthy Dietary Pattern Reduces Lung Cancer Risk: A Systematic Review and Meta-Analysis. Nutrients 2016, 8, 134. [Google Scholar] [CrossRef]
- CDC. Diagnosed Diabetes - Non-Hispanic White (Race-Ethnicity), Adults Aged 18+ Years, Age-Adjusted Percentage, Natural Breaks, All States. Available online: https://gis.cdc.gov/grasp/diabetes/diabetesatlas-surveillance.html# (accessed on 12 April 2024).
- CDC. Behavioral Risk Factor Surveillance System. Available online: https://www.cdc.gov/brfss/index.html (accessed on 12 April 2024).
- CDC. Adult Obesity Prevalence Maps. Available online: https://www.cdc.gov/obesity/data/maps/2022/downloads/obesity-prevalence-map-by-race-ethnicity-2011-2021-508.pptx (accessed on 12 April 2024).
- USCensusBureau. State-level Urban and Rural Information for the 2020 Census and 2010 Census. Available online: https://www2.census.gov/geo/docs/reference/ua/ (accessed on 12 April 2024).
- Collaborators, U.S.B.o.D.; Mokdad, A.H.; Ballestros, K.; Echko, M.; Glenn, S.; Olsen, H.E.; Mullany, E.; Lee, A.; Khan, A.R.; Ahmadi, A.; et al. The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA 2018, 319, 1444–1472. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.; Heymach, J.V.; Wen, C.P.; Ye, Y.; Pierzynski, J.A.; Roth, J.A.; Wu, X. Different dietary patterns and reduction of lung cancer risk: A large case-control study in the U.S. Sci Rep 2016, 6, 26760. [Google Scholar] [CrossRef]
- Yu, D.; Zheng, W.; Johansson, M.; Lan, Q.; Park, Y.; White, E.; Matthews, C.E.; Sawada, N.; Gao, Y.T.; Robien, K.; et al. Overall and Central Obesity and Risk of Lung Cancer: A Pooled Analysis. J Natl Cancer Inst 2018, 110, 831–842. [Google Scholar] [CrossRef] [PubMed]
- Feller, S.; Boeing, H.; Pischon, T. Body mass index, waist circumference, and the risk of type 2 diabetes mellitus: implications for routine clinical practice. Dtsch Arztebl Int 2010, 107, 470–476. [Google Scholar] [CrossRef]
- Dhokte, S.; Czaja, K. Visceral Adipose Tissue: The Hidden Culprit for Type 2 Diabetes. Nutrients 2024, 16, 1015. [Google Scholar] [CrossRef] [PubMed]
- Davoodi, S.H.; Malek-Shahabi, T.; Malekshahi-Moghadam, A.; Shahbazi, R.; Esmaeili, S. Obesity as an important risk factor for certain types of cancer. Iran J Cancer Prev 2013, 6, 186–194. [Google Scholar] [PubMed]
- Maas, P.; Barrdahl, M.; Joshi, A.D.; Auer, P.L.; Gaudet, M.M.; Milne, R.L.; Schumacher, F.R.; Anderson, W.F.; Check, D.; Chattopadhyay, S.; et al. Breast Cancer Risk From Modifiable and Nonmodifiable Risk Factors Among White Women in the United States. JAMA Oncol 2016, 2, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Avgerinos, K.I.; Spyrou, N.; Mantzoros, C.S.; Dalamaga, M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism 2019, 92, 121–135. [Google Scholar] [CrossRef]
- Jung, U.J.; Choi, M.S. Obesity and Its Metabolic Complications: The Role of Adipokines and the Relationship between Obesity, Inflammation, Insulin Resistance, Dyslipidemia and Nonalcoholic Fatty Liver Disease. Int J Mol Sci 2014, 15, 6184–6223. [Google Scholar] [CrossRef]
- Wang, Y.; Beydoun, M.A.; Min, J.; Xue, H.; Kaminsky, L.A.; Cheskin, L.J. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol 2020, 49, 810–823. [Google Scholar] [CrossRef]
- Lee, V. Introduction to the dietary management of obesity in adults. Clin Med (Lond) 2023, 23, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Song, M.; Eliassen, A.H.; Wang, M.; Fung, T.T.; Clinton, S.K.; Rimm, E.B.; Hu, F.B.; Willett, W.C.; Tabung, F.K.; et al. Optimal dietary patterns for prevention of chronic disease. Nat Med 2023, 29, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Singh, P.N.; Sabate, J.; Fan, J.; Sveen, L.; Bennett, H.; Knutsen, S.F.; Beeson, W.L.; Jaceldo-Siegl, K.; Butler, T.L.; et al. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Intern Med 2015, 175, 767–776. [Google Scholar] [CrossRef]
- Juan, W.J.; Yamini, S.; Britten, P. Food Intake Patterns of Self-identified Vegetarians among the U.S. Population, 2007-2010. Procedia Food Science 2015, 4, 86–93. [Google Scholar] [CrossRef]
- Zhang, J.; Dhakal, I.B.; Zhao, Z.; Li, L. Trends in mortality from cancers of the breast, colon, prostate, esophagus, and stomach in East Asia: role of nutrition transition. Eur J Cancer Prev 2012, 21, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. Trends in diet and Alzheimer's disease during the nutrition transition in Japan and developing countries. J Alzheimers Dis 2014, 38, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Ballantyne, C.M. Metabolic Inflammation and Insulin Resistance in Obesity. Circ Res 2020, 126, 1549–1564. [Google Scholar] [CrossRef]
- Zatterale, F.; Longo, M.; Naderi, J.; Raciti, G.A.; Desiderio, A.; Miele, C.; Beguinot, F. Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes. Front Physiol 2019, 10, 1607. [Google Scholar] [CrossRef]
- Deng, T.; Lyon, C.J.; Bergin, S.; Caligiuri, M.A.; Hsueh, W.A. Obesity, Inflammation, and Cancer. Annu Rev Pathol 2016, 11, 421–449. [Google Scholar] [CrossRef]
- De Stefani, E.; Fierro, L.; Barrios, E.; Ronco, A. Tobacco, alcohol, diet and risk of non-Hodgkin's lymphoma: a case-control study in Uruguay. Leuk Res 1998, 22, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Aykan, N.F. Red Meat and Colorectal Cancer. Oncol Rev 2015, 9, 288. [Google Scholar] [CrossRef] [PubMed]
- Farvid, M.S.; Sidahmed, E.; Spence, N.D.; Mante Angua, K.; Rosner, B.A.; Barnett, J.B. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 2021, 36, 937–951. [Google Scholar] [CrossRef] [PubMed]
- Abu-Ghazaleh, N.; Chua, W.J.; Gopalan, V. Intestinal microbiota and its association with colon cancer and red/processed meat consumption. J Gastroenterol Hepatol 2021, 36, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Shikany, J.M.; Safford, M.M.; Newby, P.K.; Durant, R.W.; Brown, T.M.; Judd, S.E. Southern Dietary Pattern is Associated With Hazard of Acute Coronary Heart Disease in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circulation 2015, 132, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Panigrahi, G.; Goodwin, S.M.; Staffier, K.L.; Karlsen, M. Remission of Type 2 Diabetes After Treatment With a High-Fiber, Low-Fat, Plant-Predominant Diet Intervention: A Case Series. Am J Lifestyle Med 2023, 17, 839–846. [Google Scholar] [CrossRef] [PubMed]
- Ames, B.N.; Wakimoto, P. Are vitamin and mineral deficiencies a major cancer risk? Nat Rev Cancer 2002, 2, 694–704. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D. The mineral depletion of foods available to us as a nation (1940-2002)--a review of the 6th Edition of McCance and Widdowson. Nutr Health 2007, 19, 21–55. [Google Scholar] [CrossRef]
- Driscoll, C.T.; Lawrence, G.B.; Bulger, A.J.; Butler, T.J.; Cronan, C.S.; Eagar, C.; Lambert, K.F.; Likens, G.E.; Stodard, J.L.; Weathers, K.C. Acidic Deposition in the Northeastern United States: Sources and Inputs, Ecosystem Effects, and Management Strategies. BioScience 2001, 51, 180–198. [Google Scholar] [CrossRef]
- Cakmak, I.; Yazici, A.; Tutus, Y.; Ozturk, L. Glyphosate reduced seed and leaf concentrations of calcium, manganese, magnesium, and iron in non-glyphosate resistant soybean. European Journal of Agronomy 2999, 31, 114–119. [Google Scholar] [CrossRef]
- Helander, M.; Saloniemi, I.; Omacini, M.; Druille, M.; Salminen, J.P.; Saikkonen, K. Glyphosate decreases mycorrhizal colonization and affects plant-soil feedback. Sci Total Environ 2018, 642, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Bueno de Mesquita, C.P.; Solon, A.J.; Barfield, A.; al., e. Adverse impacts of Roundup on soil bacteria, soil chemistry and mycorrhizal fungi during restoration of a Colorado grassland. Applied Soil Ecology 2023, 185, 104778. [CrossRef]
- Muka, T.; Kraja, B.; Ruiter, R.; Lahousse, L.; de Keyser, C.E.; Hofman, A.; Franco, O.H.; Brusselle, G.; Stricker, B.H.; Kiefte-de Jong, J.C. Dietary mineral intake and lung cancer risk: the Rotterdam Study. Eur J Nutr 2017, 56, 1637–1646. [Google Scholar] [CrossRef] [PubMed]
- Swaminath, S.; Um, C.Y.; Prizment, A.E.; Lazovich, D.; Bostick, R.M. Combined Mineral Intakes and Risk of Colorectal Cancer in Postmenopausal Women. Cancer Epidemiol Biomarkers Prev 2019, 28, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Venturelli, S.; Leischner, C.; Helling, T.; Renner, O.; Burkard, M.; Marongiu, L. Minerals and Cancer: Overview of the Possible Diagnostic Value. Cancers (Basel) 2022, 14. [Google Scholar] [CrossRef]
- Dubey, P.; Thakur, V.; Chattopadhyay, M. Role of Minerals and Trace Elements in Diabetes and Insulin Resistance. Nutrients 2020, 12, 1864. [Google Scholar] [CrossRef] [PubMed]
- Visvanathan, K.; Mondul, A.M.; Zeleniuch-Jacquotte, A.; Wang, M.; Gail, M.H.; Yaun, S.S.; Weinstein, S.J.; McCullough, M.L.; Eliassen, A.H.; Cook, N.R.; et al. Circulating vitamin D and breast cancer risk: an international pooling project of 17 cohorts. Eur J Epidemiol 2023. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Wan, S.; Shi, J.; Xu, T.; Wang, L.; Guan, Y.; Luo, J.; Luo, Y.; Sun, M.; An, P.; et al. Antioxidant Minerals Modified the Association between Iron and Type 2 Diabetes in a Chinese Population. Nutrients 2024, 16, 335. [Google Scholar] [CrossRef]
- Nanda, M.; Sharma, R.; Mubarik, S.; Aashima, A.; Zhang, K. Type-2 Diabetes Mellitus (T2DM): Spatial-temporal Patterns of Incidence, Mortality and Attributable Risk Factors from 1990 to 2019 among 21 World Regions. Endocrine 2022, 77, 444–454. [Google Scholar] [CrossRef]
- Thun, M.J.; Henley, S.J.; Calle, E.E. Tobacco use and cancer: an epidemiologic perspective for geneticists. Oncogene 2002, 21, 7307–7325. [Google Scholar] [CrossRef]
- Giovannucci, E. An updated review of the epidemiological evidence that cigarette smoking increases risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev 2001, 10, 725–731. [Google Scholar] [PubMed]
- Dwyer-Lindgren, L.; Mokdad, A.H.; Srebotnjak, T.; Flaxman, A.D.; Hansen, G.M.; Murray, C.J. Cigarette smoking prevalence in US counties: 1996-2012. Popul Health Metr 2014, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z. Spatial analysis of MODIS aerosol optical depth, PM2.5, and chronic coronary heart disease. Int J Health Geogr 2009, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.E.; Tamura-Wicks, H.; Parks, R.M.; Burnett, R.T.; Pope, C.A., 3rd; Bechle, M.J.; Marshall, J.D.; Danaei, G.; Ezzati, M. Particulate matter air pollution and national and county life expectancy loss in the USA: A spatiotemporal analysis. PLoS Med 2019, 16, e1002856. [Google Scholar] [CrossRef] [PubMed]
- Prada, D.; Baccarelli, A.A.; Terry, M.B.; Valdez, L.; Cabrera, P.; Just, A.; Kloog, I.; Caro, H.; Garcia-Cuellar, C.; Sanchez-Perez, Y.; et al. Long-term PM(2.5) exposure before diagnosis is associated with worse outcome in breast cancer. Breast Cancer Res Treat 2021, 188, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Peller, S. Carcinogenesis as a means of reducing cancer mortality. Lancet 1936, 228, 552–556. [Google Scholar] [CrossRef]
- Engelsen, O. The relationship between ultraviolet radiation exposure and vitamin D status. Nutrients 2010, 2, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Shanbhag, S.; Nayak, A.; Narayan, R.; Nayak, U.Y. Anti-aging and Sunscreens: Paradigm Shift in Cosmetics. Adv Pharm Bull 2019, 9, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Santos, M.; Costa, P.R.; Assis, A.M.; Santos, C.A.; Santos, D.B. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev 2015, 16, 341–349. [Google Scholar] [CrossRef]
- Grant, W.B. 25-hydroxyvitamin D and breast cancer, colorectal cancer, and colorectal adenomas: case-control versus nested case-control studies. Anticancer Res 2015, 35, 1153–1160. [Google Scholar]
- McCullough, M.L.; Zoltick, E.S.; Weinstein, S.J.; Fedirko, V.; Wang, M.; Cook, N.R.; Eliassen, A.H.; Zeleniuch-Jacquotte, A.; Agnoli, C.; Albanes, D.; et al. Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts. J Natl Cancer Inst 2019, 111, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev 2014, 72, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Boucher, B.J.; Al Anouti, F.; Pilz, S. Comparing the Evidence from Observational Studies and Randomized Controlled Trials for Nonskeletal Health Effects of Vitamin D. Nutrients 2022, 14, 3811. [Google Scholar] [CrossRef] [PubMed]
- Pittas, A.G.; Dawson-Hughes, B.; Sheehan, P.; Ware, J.H.; Knowler, W.C.; Aroda, V.R.; Brodsky, I.; Ceglia, L.; Chadha, C.; Chatterjee, R.; et al. Vitamin D Supplementation and Prevention of Type 2 Diabetes. N Engl J Med 2019, 381, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Hughes, B.; Staten, M.A.; Knowler, W.C.; Nelson, J.; Vickery, E.M.; LeBlanc, E.S.; Neff, L.M.; Park, J.; Pittas, A.G.; Group, D.d.R. Intratrial Exposure to Vitamin D and New-Onset Diabetes Among Adults With Prediabetes: A Secondary Analysis From the Vitamin D and Type 2 Diabetes (D2d) Study. Diabetes Care 2020, 43, 2916–2922. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D'Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med 2019, 380, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Mondal, S.; Adhikari, N.; Banerjee, S.; Amin, S.A.; Jha, T. Matrix metalloproteinase-9 (MMP-9) and its inhibitors in cancer: A minireview. Eur J Med Chem 2020, 194, 112260. [Google Scholar] [CrossRef] [PubMed]
- Kanno, K.; Akutsu, T.; Ohdaira, H.; Suzuki, Y.; Urashima, M. Effect of Vitamin D Supplements on Relapse or Death in a p53-Immunoreactive Subgroup With Digestive Tract Cancer: Post Hoc Analysis of the AMATERASU Randomized Clinical Trial. JAMA Netw Open 2023, 6, e2328886. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. The Death D-Fying Vitamin D3 for Digestive Tract Cancers-The p53 Antibody Connection. JAMA Netw Open 2023, 6, e2328883. [Google Scholar] [CrossRef]
- Pludowski, P.; Grant, W.B.; Karras, S.N.; Zittermann, A.; Pilz, S. Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 microg) of Vitamin D for Adults in the General Population. Nutrients 2024, 16, 391. [Google Scholar] [CrossRef]
- Holloway, T.; Miller, D.; Anenberg, S.; Diao, M.; Duncan, B.; Fiore, A.M.; Henze, D.K.; Hess, J.; Kinney, P.L.; Liu, Y.; et al. Satellite Monitoring for Air Quality and Health. Annu Rev Biomed Data Sci 2021, 4, 417–447. [Google Scholar] [CrossRef] [PubMed]
| State | UVB Dose (kJ/m2) |
|---|---|
| Alabama | 6.0 |
| Alaska | |
| Arkansas | 5.7 |
| Arizona | 9.0 |
| California | 7.5 |
| Colorado | 8.2 |
| Connecticut | 4.7 |
| Delaware | 4.7 |
| District of Columbia | 4.7 |
| Florida | 8.0 |
| Georgia | 7.2 |
| Hawaii | |
| Idaho | 6.0 |
| Illinois | 4.5 |
| Iowa | 4.7 |
| Indiana | 4.7 |
| Kansas | 6.3 |
| Kentucky | 5.8 |
| Louisiana | 7.5 |
| Massachusetts | 4.6 |
| Maine | 4.1 |
| Maryland | 4.7 |
| Michigan | 4.2 |
| Minnesota | 4.1 |
| Missouri | 6.5 |
| Mississippi | 7.0 |
| Montana | 4.7 |
| North Carolina | 6.6 |
| North Dakota | 6.2 |
| Nebraska | 5.1 |
| New Hampshire | 4.1 |
| New Jersey | 5.2 |
| New Mexico | 9.5 |
| Nevada | 8.5 |
| New York | 4.7 |
| Ohio | 4.7 |
| Oklahoma | 7.5 |
| Oregon | 5.2 |
| Pennsylvania | 4.5 |
| Rhode Island | 4.7 |
| South Carolina | 7.2 |
| South Dakota | 4.5 |
| Tennessee | 6.3 |
| Texas | 7.8 |
| Utah | 8.0 |
| Virginia | 6.0 |
| Vermont | 4.2 |
| Washington | 4.5 |
| Wisconsin | 4.5 |
| West Virginia | 5.2 |
| Wyoming | 6.0 |
| Factor | DM | LCF | LCM | Obs | UVB |
|---|---|---|---|---|---|
| Alcohol | 0.40, 0.14, 0.007 | 0.03 0.00, xx | 0.24, 0.03, 0.12 | 0.25, 0.04, 0.11 | 0.35, 0.10, 0.02 |
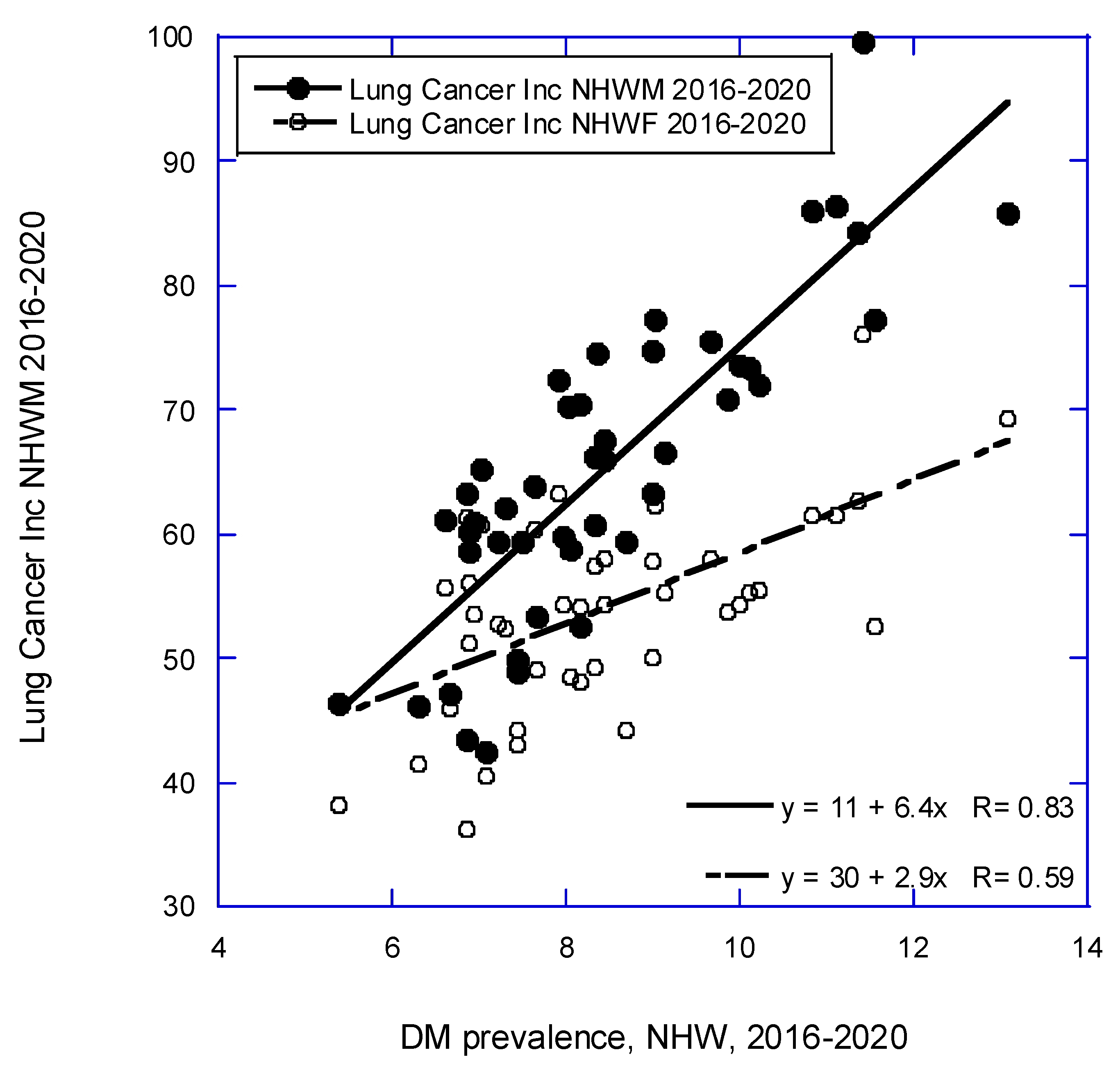
| Diabetes | 0.59, 0.33, * | 0.84, 0.69, * | 0.84, 0.69, * | 0.13, 0.00, -- | |
| Lung cancer, F | 0.88, 0.77, * | 0.54, 0.28, * | 0.14, 0.00, -- | ||
| Lung cancer, M | 0.75, 0.55, * | 0.39, 0.13, 0.008 | |||
| Obesity | 0.11, 0.00, -- |
| Cancer | Equation | r, adjusted r2, p (p) |
|---|---|---|
| All | 410 + (4.2 × Obs) − (7.3 × UVB) | 0.58, 0.30, 0.002, 0.02 |
| 350 + (4.8 × Obs) | 0.49, 0.23, <0.001 | |
| 549 − (9.5 × UVB) | 0.39, 0.13, 0.008 | |
| All less lung | 420 - (7.34 × UVB) + (0.77 * LCM) | 0.54, 0.26, 0.006, 0.01 |
| 480 - (8.3 × UVB) | 0.43, 0.16, 0.004 | |
| 370 + (0.89 × LCM) | 0.39, 0.13, 0.008 | |
| Bladder | 43 − (1.7 × UVB) + (1.5 × Alc) | 0.72, 0.50, <0.001, 0.09 |
| 48 − (1.9 × UVB) | 0.70, 0.47, <0.001 | |
| 29 + (3.1 × Alc) | 0.42, 0.16, 0.004 | |
| Brain | 8.5 − (0.14 × UVB) | 0.31, 0.08, 0.03 |
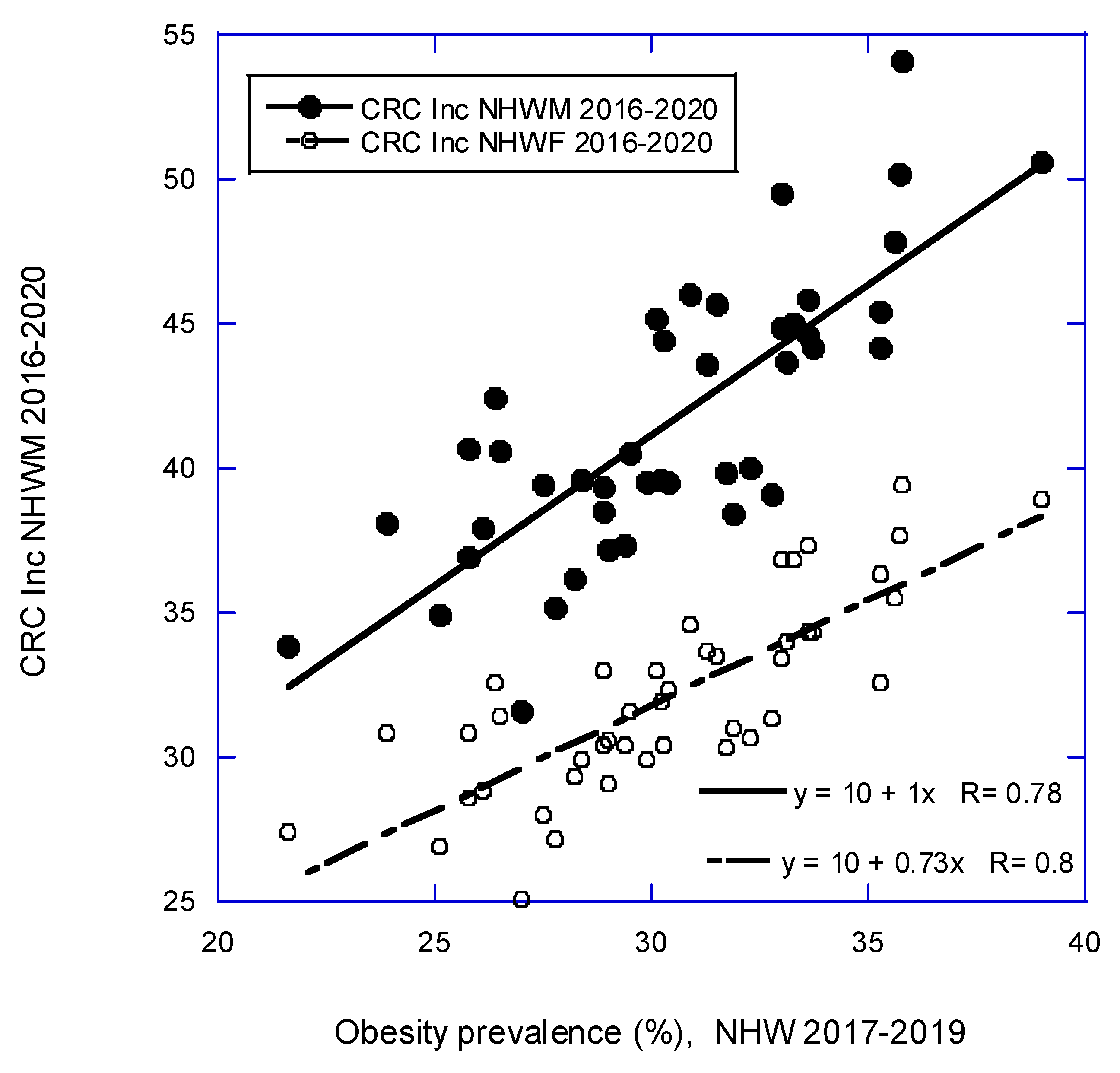
| Colorectal | 12 + (0.13 × LCM) + (0.70 × Obs) | 0.82, 0.65, <0.001 |
| 10 + (1.0 × Obs) | 0.78, 0.61, <0.001 | |
| 24 + (0.28 × LCM) | 0.73, 0.52, <0.001 | |
| Esophageal | 5.7+ (0.048 × LCM) − (0.29 × UVB) + (0.69 × Alc) | 0.77, 0.56, <0.001, 0.001, 0.006 |
| 8.5 − (0.39 × UVB) + (0.039 × LCM) | 0.71, 0.48, <0.001, <0.001 | |
| 11 − (0.44 × UVB) | 0.57, 0.31, <0.001 | |
| 7.1 + (0.69 × Alc) | 0.33, = 0.09, 0.03 | |
| Gastric | 9.0 − (0.36 × UVB) | 0.55, 0.29, <0.001 |
| Larynx | 1.3 + (0.058 × LCM) | 0.57, 0.31, <0.001 |
| Liver | 4.5 + (0.66 × DM) | 0.37, 0.12, 0.01 |
| Lung | 11 + (6.4 × DM) | 0.84, 0.69, <0.001 |
| 72 − (1.2 × UVB) | 0.14, 0.000 | |
| Non-Hodgkin’s lymphoma | 28 − (0.84 × UVB) | 0.56, 0.29, <0.001 |
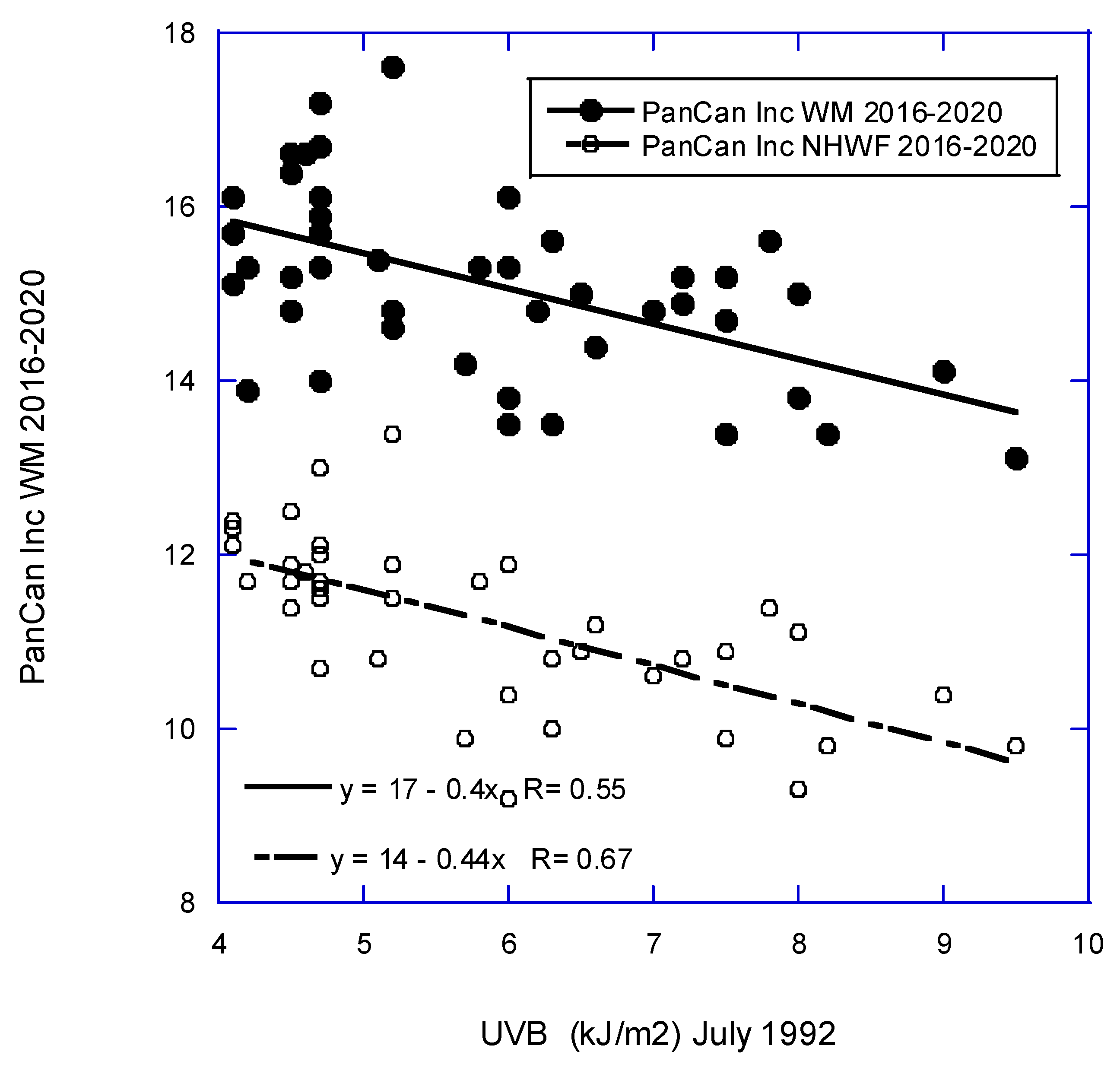
| Pancreatic | 18 − (0.40 × UVB) | 0.55, 0.29, <0.001 |
| Prostate | 130 − (3.4 × UVB) | 0.14, 0.15, 0.005 |
| Renal | 11 + (0.19 × LCM) | 0.75, 0.55, <0.001 |
| 3.6 + (0.66 × Obs) | 0.74, 0.53, <0.001 |
| Type | Equation | r, adjusted r2, p (p) |
|---|---|---|
| All | 440 − (9.8 × UVB)+ (1.7 × Obs) | 0.63, 0.37, <0.001, 0.06 |
| 430 − (7.7 × UVB) | 0.53, 0.26, <0.001 | |
| 360 + (2.5 × Obs) | 0.34, 0.09, 0.03 | |
| All less lung | 36 − (5.6 × UVB) + (0.94 × LCF) | 0.63, 0.36, 0.006, 0.009 |
| 430 − (7.7 × UVB) | 0.53, 0.26, <0.001 | |
| 310 + (1.3 × LCF) | 0.52, 0.25, <0.001 | |
| Bladder | 9.5 − (0.50 × UVB) + (1.0 × Alc) | 0.76, 0.56, <0.001, <0.001 |
| 13 − (0.64 × UVB) | 0.65, 0.41, <0.001 | |
| 5.5 + (1.5 × Alc) | 0.59, 0.33, <0.001 | |
| 5.2 + (0.074 × LCF) | 0.45, 0.18, 0.002 | |
| Breast | 160 − (2.3 × UVB) − (2.2 × DM) | 0.66, 0.41, <0.001, <0.001 |
| 180 − (2.8 × UVB) − (0.91 × Obs) | 0.65, 0.39, <0.001, <0.001 | |
| 150 − (2.4 × DM) | 0.51, 0.24, <0.001 | |
| 150 − (2.5 × UVB) | 0.47, 0.20, 0.001 | |
| 150 – (0.70 × Obs) | 0.34, 0.10, 0.02 | |
| Colorectal | 10 + (0.73 × Obs) | 0.80, 0.63, <0.001 |
| 21 + (0.21 × LCF) | 0.53, 0.27, <0.001 | |
| Corpus uteri | 38 − (1.9 × UVB) | 0.72, 0.50, <0.001 |
| Esophageal | 2.2 − (0.13 × UVB)+ (0.16 × Alc) | 0.72. 0.49, <0.001, 0.02 |
| 2.7 − (0.15 × UVB) | 0.67, 0.44, <0.001 | |
| 1.1 + (0.29 × Alc) | 0.47, 0.21, 0.001 | |
| 1.0 + (0.015 × LVF) | 0.41, 0.15, 0.006 | |
| Gastric | 4.1 − (0.14 × UVB) | 0.38, 0.12, 0.01 |
| Laryngeal | 0.19 + (0.021 × LCF) | 0.39, 0.13, 0.01 |
| Liver | 2.8 + (0.13 × DM) | 0.36, 0.11, 0.02 |
| Lung | 43 + (3.2 × DM) − (2.7 × UVB) | 0.75, 0.54, <0.001, <0.001 |
| 30 + (1.1 × Obs) − (1.8 × UVB) | 0.63, 0.36, <0.001, 0.02 | |
| 30 + (2.9 × DM) | 0.59, 0.33, <0.001 | |
| 67 − (2.2 × UVB) | 0.39, 0.13, 0.008 | |
| Non-Hodgkin’s lymphoma | 19 − (0.60 × UVB) | 0.51, 0.25, <0.001 |
| Pancreatic | 14 − (0.44 × UVB) | 0.67, 0.44, <0.001 |
| Renal | −2.0 + (0.46 × Obs) | 0.84, 0.69, <0.001 |
| 4.9 + (0.13 × LCF) | 0.55, 0.29, <0.001 |
| Cancer | UVB (2016–2020) | UVB, males [8]* |
UVB, females [8]* |
UVB (2006), males [7] |
UVB (2006), females [7] |
|---|---|---|---|---|---|
| Bladder | y | 1.13 | 1.15 | y | y |
| Brain | M only | 1.08 | 1.07 | ||
| Breast | y | 1.06 | y | y | |
| Cervical | 0.84 | n | |||
| Colon | 1.11 | 1.14 | y | y | |
| Colorectal | n | ||||
| Corpus uteri | y | 1.49 | y | ||
| Esophageal | y | 1.27 | 1.07 | y | y |
| Gastric | y | 1.42 | 1.27 | y | y |
| Hodgkin’s lymphoma | n | 1.16 | 1.19 | y | y |
| Laryngeal | n | 0.87 | 0.80 | y | y |
| Leukemia | n | 1.09 | 1.15 | n | n |
| Liver | n | 1.01 | 1.05 | n | n |
| Lung | F only | n | n | ||
| Myeloma | n | 1.19 | 1.22 | n | n |
| Non-Hodgkin’s lymphoma | y | 1.08 | 1.09 | y | y |
| Oral cavity | n | 0.77 | 0.83 | n | n |
| Ovarian | n | 1.03 | y | ||
| Pancreatic | y | 1.09 | 1.17 | y | n |
| Prostate | y | 1.20 | ? | ||
| Rectal | 1.27 | 1.14 | y | y | |
| Renal | n | 1.09 | 1.17 | y | y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





