1. Introduction
Undernutrition, seen mostly in low- and middle-income countries, is a key risk factor for death in children under five years of age [
1]. Stunting is a marker of a deficient environment [
2] and is associated with delayed child development, reduced earnings in adulthood, and chronic disease. Globally, 21.9% of children under five years are stunted, and 7.3% are wasted [
3].
Before the onset of the Scaling Up Nutrition (SUN) movement, the long-term consequences of all forms of malnutrition gained the attention of researchers and practitioners globally, mainly after the publication of the Lancet series of 2008. The follow-up 2013 Lancet series extended the discussions to adolescent nutrition. The Sustainable Development Goals brought stunting to focus when targets changed from underweight to stunting. Since then, donor-funded programming has identified stunting reduction as a primary target; adequate linear growth will reduce the associated higher mortality and minimise the long-term impact on chronic conditions [
4,
5,
6,
7].
The nutritional status of children in Pakistan is alarming, with 40.2% of children under five years of age stunted, 17.7% wasted, and 28.9% underweight, with a higher prevalence of stunting in rural areas than in urban areas [
8]. In Sindh province, 45.5% of children under five are stunted[
8]. Food insecurity, poor health care, inadequate diets, lack of affordability of a balanced diet, inaccessibility to basic nutrients, gender and socio-demographic inequality, and lack of family planning are some of the core social and biological stressors contributing to the poor health of women and children in Pakistan[
9]. Despite being a predominantly agrarian country, Pakistan is 11th among 148 countries on the Food Security Risk Index (FSRI), which highlights the population's poor nutritional and health status [
10]. Diets low in animal protein sources, fruits, and vegetables and high in phytates can contribute to micronutrient deficiencies, resulting in anemia, developmental delays, and poor child growth [
11,
12].
The first 1000 days of a child's life, from conception to two years, are the most vulnerable and critical for building the foundations of optimum child growth and development [
13]. Studies aiming to reduce malnutrition in children by targeting the first 1000 days have shown improvements in birth and growth outcomes [
14]. According to a recent survey, more than half (53.7%) of Pakistani children under five years of age are anaemic, with 5.7% being severely anaemic [
8]. This indicates a deficient environment, possibly because of inadequate intake of food and nutrients or excess of illnesses. A deficient environment can delay child development and future work capacity[
2].
Common food-based interventions, including the provision of specialised nutritious food (SNF) during pregnancy, the first six months of lactation, and for infants up to two years of age, have proven to be more effective and holistic in targeting nutrient deficiencies in infants [
11,
15,
16,
17].
In low- and middle-income and food-insecure settings, complementary foods include lipid-based nutrient supplements (LNS) and fortified blended foods (FBFs). FBFs are made from readily available grains and fortified to provide sufficient energy and nutrient density to prevent undernutrition [
11]. The World Food Programme (WFP) developed a Wheat Soy Blend (WSB), a mixture of animal-sourced protein, sugar, oil, soybeans, and adjusted micronutrients[
18]. Furthermore, LNS is an energy-dense product containing micronutrients and essential fatty acids, which infants can easily consume [
19,
20]. When provided as a complementary food for infants, LNS improves nutrition-related outcomes in children[
20]. The iLiNS-DYAD study found that children randomised to take LNS had greater length, length-for-age z-scores (LAZ), weight, weight-for-age z-scores (WAZ), and a reduced prevalence of stunting at 18 months compared to the other groups [
9,
15,
21]
The primary objective of this study was to assess the effectiveness of nutritional supplementation in reducing stunting prevalence in children aged up to 59 months. The secondary objectives included reducing wasting and underweight in children up to 59 months of age.
2. Materials and Methods
Study Design
The data used in this analysis was collected from a mixed-method study[
22]. The impact evaluation design was quasi-experimental, with one program and one comparison population, and both areas matched for demographic, ethnic, and economic circumstances[
22,
23]. The impact of the intervention was measured using baseline (2014) and endline (2018) cross-sectional survey data of children 6-59 months of age.
The intervention was implemented during 2014-2017 in 29 union councils (UCs) study was conducted between August 2014 and September 2018 in the Thatta and Sujawal districts of the Sindh province. Twelve Union Councils (UCs) were selected and assigned equally to the intervention and control groups within the district. We matched the clusters based on the stunting rate in children under five years of age and population size.
Lady Health Workers (LHWs) are integral to Pakistan's maternal and child health services. Each LHW caters to approximately 100 households and 15-20 LHWs affiliated with a public sector health facility in each union council (UC). Thus, we engaged the LHWs to provide Wheat Soy Blend to pregnant and lactating women (PLW) (up to six months post-partum) and LNS-MQ to infants between six months and two years in the intervention group that would prevent stunting, wasting, and micronutrient deficiencies, while the control group received no interventions.
The Ethics Review Committee (ERC) of Aga Khan University (AKU) and the National Bioethics Committee (NBC) of Pakistan granted ethical approval for the study, including human subjects. All participants included in the study provided written informed consent before enrolment.
Study Setting and Participants
The study districts are administratively divided into nine Talukas and 55 Union Councils (UCs) with a population of approximately 1.8 million, and each UC has a minimum of one public primary healthcare facility.
The program components included the provision of a lipid-based nutrient supplement (LNS) in the form of Wawamum targeted to children six months to 23 months of age, behaviour change communication for proper complementary and feeding practices, and hand hygiene targeted to their primary caregivers (mostly mothers). This intervention occurred during the first 1000 days of an infant's life. The control group received routine health care. All children 6-59 months of age were eligible for enrollment in the study in both the intervention and control areas. The primary outcome of interest was the changes in the prevalence of stunting in children aged 6–23 months in the program compared with the control after four years of implementation. The secondary outcomes were the prevalence of wasting and underweight.
Selection of Study Areas
These districts were selected based on their high prevalence of stunting and all forms of malnutrition. In addition, there was coverage of Lady Health Workers (LHW) in the district, and there was the possibility of future scaling up. We implemented the intervention in parts of UCs with LHW coverage. The control area was a non-LHW area.
Data Collection
We collected the study data at the beginning of the intervention (2014) and towards the end (2017) and used a standard pre- and post-survey questionnaire. The data collection teams comprised four female data collectors and a male team leader. A total of six teams were hired locally for the study. Data collectors were required to have a high school education, and the team leader required graduate-level education (14th grade). All data collectors received 6-day training on all data collection techniques, anthropometric testing, and ethical issues, and one day of practical field training before the implementation of data collection. Each team leader was provided with a study manual with instructions, methodology, and sampling strategies. Questionnaires were field-tested before the study commenced, and we incorporated any changes or suggestions in the questionnaires before the initiation of data collection. The teams collected data manually from hard copies of the study questionnaires. The baseline and endline questionnaires covered sociodemographic characteristics, gestational age at enrollment, reproductive history, antenatal care, morbidity and health-seeking behaviour, past intervention exposure, and anthropometric data.
Procedures
Pregnant women were provided with Wheat Soy Blend (WSB) during pregnancy and lactation by LHWs. The WSB provided to PLW in the intervention group consisted of partially cooked wheat and soy fortified with micronutrients. PLW was supplied with 5 kg (165 g per day) of WSB every month for the duration of pregnancy and through the first six months of lactation. Supplementation was continued in the intervention group when the infant reached six months of age. Infants of these PLW were provided with LNS in the form of Wawamum from 6 to 23 months (
Table 1). Children 24-59 months received multiple micronutrient powders (MNP) (
Table 1). This intervention occurred during the first 1000 days of an infant's life. Patients in the control group received standard routine care. The reported health outcomes are the nutritional status of children 6-59 months, including stunting, wasting, and underweight.
LHWs performed a monthly follow-up during program implementation to assess adherence to the intervention. We used participant recall and observations of used and unused LNS sachets and WSB to collect data on adherence at all intervention households at each visit. Anthropometry was performed by trained survey staff using digital scales (Seca Uniscales model 874), height boards (Seca 213) and infant meters (Seca model 210). The Agha Khan University team trained the survey staff, which included standardisation exercises during the initial orientation before the baseline and end-line surveys.
A monitoring team conducted the quality assurance of the data. The team randomly visited 5% of the households to validate data collection. Team leaders supervised the data collection teams, and a field supervisor and project manager conducted further data monitoring. The field supervisor ensured data quality through ENA-SMART software by conducting weekly plausibility checks for anthropometric measurements.
Sample Size
The sample size for this study was determined to compare two cross-sectional surveys to assess the impact of intervention in achieving a 10% reduction in the prevalence of stunting over the four-year implementation period. We based our calculations on a baseline stunting prevalence of 49% in Sindh to estimate the potential impact of the interventions (with α=0.05 and power=0.80), and each group consisted of 3200 participants.
Statistical Analysis
Data were entered into the Visual FoxPro database and analysed using STATA version 17 (Stata/SE 17 Stata Corporation, College Station, TX, USA). Household characteristic data were analysed for all participants who completed the survey. The wealth quintiles were constructed using principal component factors (pcf) for data reduction and extraction of the maximum variance [
7]. This includes individual, household and community access to resources. The composite score included 33 variables: ownership of assets, land, livestock, household construction, and access to sanitation facilities.
We used DID analyses for repeated cross-sectional surveys (baseline and end line) to examine the program's impact on child outcomes by utilising the value of the propensity score [
23,
24]. Propensity score matching constructs a statistical comparison group based on a model of the probability of participating in treatment using the observed characteristics [
24].
We then matched the participants to non-participants based on the probability or propensity score. Variable selection for matching was based on theoretical relation to anthropometric outcomes and included maternal education, wealth quintiles, hand hygiene indicators, gender, household density, and food insecurity. A difference-in-differences test among matched subjects estimated the mean change in outcomes in the intervention group after subtracting the mean change in outcomes in the control group.
3. Results
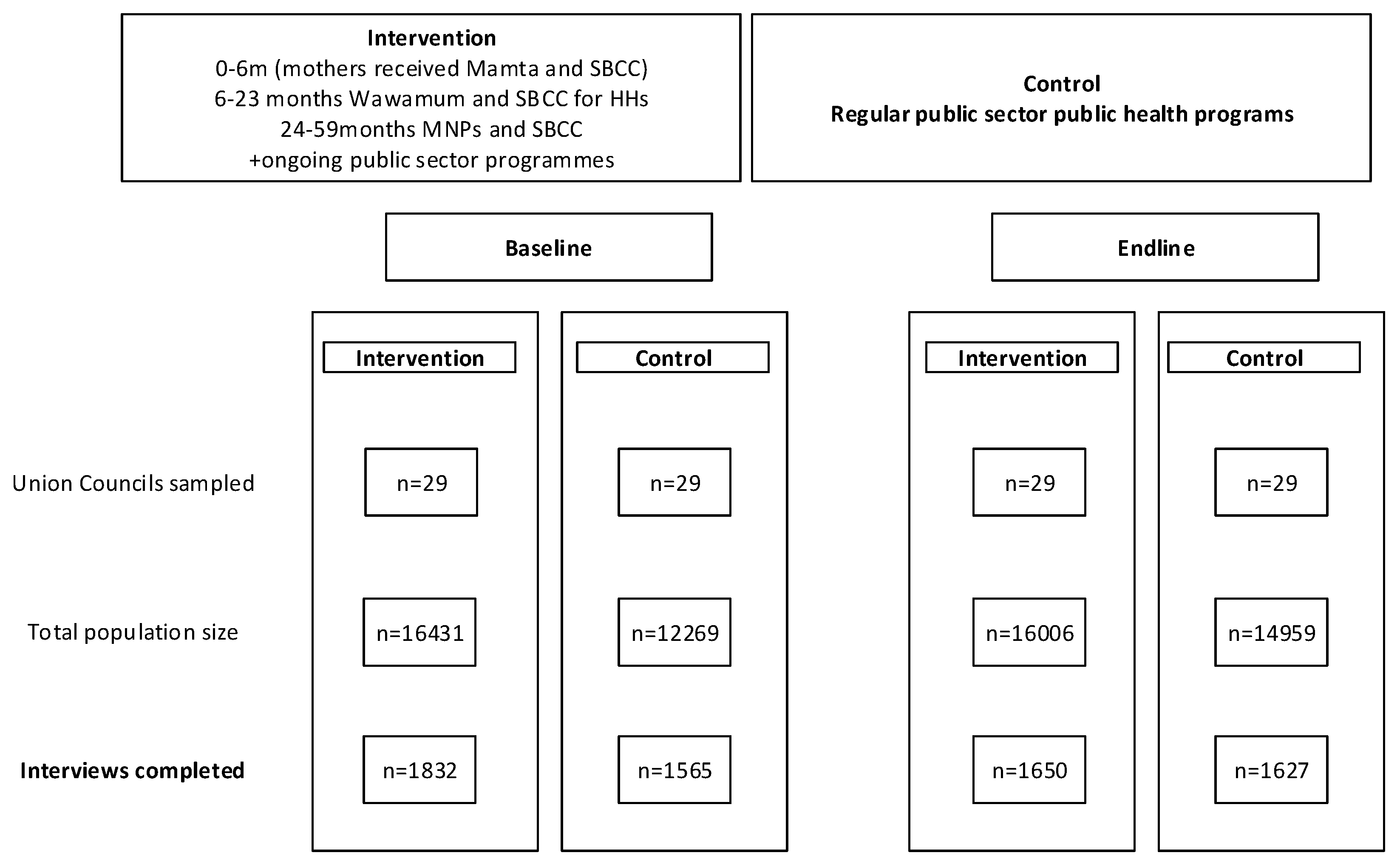
We analysed a total of 3397 children 6-59 months (1832 intervention, 1565 control) at baseline compared to 3277 children (1650 intervention, 1627 control) at the end-line survey (
Table 2).
3.1.1. Baseline characteristics
At baseline, the household density of the intervention group was 7.1 compared to 6.2 in the control group (
Table 2). Among the children 6-59 months, 51.9% of males and 48.1% of females were analysed in the intervention group compared to 51.1% of males and 48.9% of females in the control group.
3.1.2. End Line Characteristics
At the end line, household density in both the intervention and control groups was 7.3. There was no statistically significant difference in the chi-square test between the intervention and control groups (p=0.689). Among the screened children 6-59 months, 48.9% were males and 51.1% females in the intervention group, compared to 53.3% males and 46.7% females in the control group. In the intervention group, 82.9% of the mothers had no education compared to 93.2% in the control group. 4.6% and 12.5% of the mothers in the intervention group had secondary or higher education and primary or middle education, respectively.
3.1.3. Effects of the Nutritional Supplementation Program on the Prevalence of Stunting
Table 3 presents the results from the difference-in-differences analysis, illustrating the differential changes in childhood stunting and wasting rates between the intervention and control arms. Overall, the intervention had a large differential change in childhood stunting, it was not statistically significant [DID = −5.1 percentage points (pp), p=0.079]. However, for children aged 24-59 months, the study found that the intervention had a more pronounced and statistically significant effect on stunting, with a difference in stunting prevalence of -13 percentage points [p = 0.001]. The intervention showed a stronger effect on girls (DID = -5.7pp, p=0.171) than boys (DID = -3.9pp, p=0.334), although neither was significant. We also assessed the impact of the intervention across various wealth groups. We observed a substantial variation in the intervention's effect on childhood stunting among different wealth groups. The difference in stunting prevalence was most pronounced, with a decline of -21.2 percentage points [p = 0.001] in the highest wealth quintile.
3.1.4. Effects of the Nutritional Supplementation Program on the Prevalence of Wasting
As presented in
Table 3, the intervention had no significant impact on wasting [DID = −2.1 percentage points (pp), p=0.298]. The intervention showed a more substantial effect on boys, with a difference in the prevalence of wasting at -6.4 percentage points [p = 0.027]. In contrast, there was no effect for the girls' group (DID = 3.3 pp, p=0.239). We also assessed the impact of the intervention across various wealth groups. We observed a substantial variation in the intervention's effect on childhood wasting among different wealth groups. The difference in wasting prevalence was most pronounced, with a decline of -11 percentage points [p = 0.037], in the second (lowest) wealth quintile.
3.1.5. Effects of the Nutritional Supplementation Program on the Prevalence of Underweight
As presented in the
Table 3, overall, the intervention had a large statistically significant impact on underweight [DID = −8.2 pp, p=0.004]. For children aged 24-59 months, the study found that the intervention had a more pronounced and statistically significant effect on underweight, with a difference in the prevalence of underweight of -9.4 pp [p = 0.014]. We also assessed the impact of the intervention across various wealth groups. We observed a substantial variation in the intervention's effect on childhood underweight among different wealth groups. The difference in underweight prevalence was most pronounced, with a decline of -26.9 percentage points [p = 0], in the highest and second lowest (DID=-14.7, p = 0.031) wealth quintiles.
3.2. Figures, Tables and Schemes
Figure 1.
Baseline and endline study participation in intervention and control groups in Thatta and Sajawal districts 2014-18.
Figure 1.
Baseline and endline study participation in intervention and control groups in Thatta and Sajawal districts 2014-18.
Table 1.
Contents of nutritional supplements.
Table 1.
Contents of nutritional supplements.
| RATION CONTENTS |
WSB |
WAWAMUM (PER 50 G) |
MNP (PER 1 G) |
| Daily ration (g/person/day) |
167 |
50 |
On alternate day |
| Energy (kcal) |
633 |
255 |
- |
| Protein (g) |
29.1 |
5.5 |
- |
| Fat (g) |
10.2 |
13 |
- |
| Calcium (mg) |
683 |
267.5 |
- |
| Iron (mg) |
13.9 |
5 |
10 |
| Iodine (µg) |
67 |
50 |
90 |
| Vitamin A (µg RE) |
842 |
275 |
400 |
| Thiamine B1 (mg) |
0.66 |
0.5 |
- |
| Riboflavin Vitamin B2(mg) |
1.03 |
1.05 |
- |
| Niacin (mg NE) |
15.3 |
6.5 |
6 |
| Vitamin C (mg) |
168.9 |
30 |
30 |
| Pantothenic VitB5 (mg) |
3.4 |
2 |
- |
| Vitamin B6 (mg) |
1.8 |
0.9 |
0.5 |
| Vitamin B7 (µg) |
- |
30 |
- |
| Folic Acid (µg) |
100 |
- |
902 |
| Vitamin B12 (µg) |
3 |
1.35 |
0.9 |
| Vitamin D (µg) |
10.0 |
7.5 |
- |
| Vitamin E(mg) |
- |
8 |
- |
| Vitamin K (µg) |
- |
13.5 |
- |
| Ca (mg) |
- |
- |
- |
| Cu (mg) |
- |
0.7 |
- |
| Magnesium (mg) |
- |
75 |
- |
| Manganese (mg) |
- |
0.6 |
- |
| Phosphorus (mg) |
- |
225 |
- |
| Potassium (mg) |
- |
450 |
- |
| Selenium (µg) |
49.3 |
10 |
17 |
| Na (mg) |
- |
135 |
- |
| Zn (mg) |
- |
5.5 |
- |
| Vitamin D3 (μg) |
- |
- |
5 |
| Vitamin E (mg) |
15.8 |
- |
5 |
| Vitamin K1 (µg) |
- |
- |
- |
| Vitamin B1 (mg) |
- |
- |
0.5 |
| Vitamin B2 (mg) |
- |
- |
0.5 |
| Folic acid (µg) |
- |
- |
- |
| Zinc (mg) |
11.2 |
- |
4.1 |
| Copper (mg) |
0.6 |
- |
0.56 |
| Folate (µg) |
288 |
165 |
- |
| Dry skimmed milk protein |
- |
1.8 |
- |
| ω-3 fatty acids |
- |
0.15 |
- |
| ω-6 fatty acid |
- |
1.3 |
- |
Table 2.
Child and household characteristics.
Table 2.
Child and household characteristics.
| Characteristics |
Baseline |
Endline |
| Intervention |
Control |
p value |
Intervention |
Control |
p value |
| n=1832 |
% |
n=1565 |
% |
|
n=1650 |
% |
n=1627 |
% |
|
| Average household density |
7.1 |
|
6.2 |
|
0.00 |
7.3 |
|
7.3 |
|
0.356 |
| Child sex |
|
|
|
|
0.668 |
|
|
|
|
0.012 |
| Male |
950 |
51.9% |
800 |
51.1% |
|
807 |
48.9% |
867 |
53.3% |
|
| Female |
882 |
48.1% |
765 |
48.9% |
|
843 |
51.1% |
760 |
46.7% |
|
| Age |
|
|
|
|
0.011 |
|
|
|
|
0.508 |
| 6-23 months |
849 |
46.3% |
657 |
42.0% |
|
740 |
44.8% |
711 |
43.7% |
|
| 24-59 months |
983 |
53.7% |
908 |
58.0% |
|
910 |
55.2% |
916 |
56.3% |
|
| Hand washing access* |
1549 |
84.6% |
1285 |
82.1% |
0.00 |
877 |
53.2% |
760 |
46.7% |
0.00 |
| Maternal education |
|
|
|
|
0.00 |
|
|
|
|
0.00 |
| None |
1469 |
80.2% |
1536 |
98.1% |
|
1368 |
82.9% |
1517 |
93.2% |
|
| Primary or Middle |
267 |
14.6% |
27 |
1.7% |
|
206 |
12.5% |
90 |
5.5% |
|
| Secondary or higher |
96 |
5.2% |
2 |
0.1% |
|
76 |
4.6% |
20 |
1.2% |
|
| Wealth Quintiles |
|
|
|
|
0.00 |
|
|
|
|
0.00 |
| Lowest |
187 |
10.2% |
509 |
32.5% |
|
223 |
13.5% |
449 |
27.6% |
|
| Second |
266 |
14.5% |
405 |
25.9% |
|
262 |
15.9% |
397 |
24.4% |
|
| Middle |
353 |
19.3% |
326 |
20.8% |
|
321 |
19.5% |
343 |
21.1% |
|
| Fourth |
446 |
24.3% |
251 |
16.0% |
|
402 |
24.4% |
251 |
15.4% |
|
| Highest |
580 |
31.7% |
74 |
4.7% |
|
442 |
26.8% |
187 |
11.5% |
|
Table 3.
Effects of the nutritional supplementation program on the prevalence of stunting, wasting and undernutrition**, and difference-in-difference estimation.
Table 3.
Effects of the nutritional supplementation program on the prevalence of stunting, wasting and undernutrition**, and difference-in-difference estimation.
| |
Baseline |
Endline |
|
|
| Intervention |
Control |
Difference |
p-value |
Intervention |
Control |
Difference |
p-value |
Difference in
Differences |
p-value |
| Stunting (overall) |
55.7 |
55.2 |
0.4 |
0.849 |
44.6 |
49.3 |
-4.7 |
0.01 |
-5.1 |
0.079 |
by
Gender
|
|
|
|
|
|
|
|
|
|
|
| Boys |
56.4 |
58.5 |
-2.2 |
0.485 |
45.2 |
51.4 |
-6.1 |
0.018 |
-3.9 |
0.334 |
| Girls |
54.7 |
52.5 |
2.3 |
0.489 |
44 |
47.4 |
-3.5 |
0.183 |
-5.7 |
0.171 |
| by Age Group |
|
|
|
|
|
|
|
|
|
|
| 6-23 m |
51.5 |
54.9 |
-3.4 |
0.307 |
39.7 |
39.2 |
0.5 |
0.844 |
4 |
0.358 |
| 24-59 m |
58.9 |
55 |
3.9 |
0.196 |
48.5 |
57.7 |
-9.1 |
0.00 |
-13 |
0.001 |
| by Wealth Quintiles |
|
|
|
|
|
|
|
|
|
|
| Lowest |
53.6 |
50.2 |
3.5 |
0.477 |
47.3 |
48.2 |
-0.9 |
0.853 |
-4.4 |
0.533 |
| Second |
58.4 |
57.5 |
0.9 |
0.844 |
50.6 |
50.2 |
0.4 |
0.934 |
-0.5 |
0.94 |
| Middle |
59.8 |
62 |
-2.2 |
0.639 |
48 |
49.4 |
-1.5 |
0.738 |
0.7 |
0.908 |
| Fourth |
57.5 |
58.9 |
-1.3 |
0.797 |
45.8 |
51.5 |
-5.2 |
0.174 |
-3.9 |
0.547 |
| Highest |
46.5 |
36.7 |
9.8 |
0.079 |
36.2 |
47.6 |
-11.4 |
0.001 |
-21.2 |
0.001 |
| Wasting (overall) |
17.7 |
16.2 |
1.6 |
0.314 |
11.7 |
12.2 |
-0.5 |
0.679 |
-2.1 |
0.298 |
| by Gender |
|
|
|
|
|
|
|
|
|
|
| Boys |
19.6 |
14.4 |
5.5 |
0.013 |
12.8 |
13.6 |
-0.9 |
0.636 |
-6.4 |
0.027 |
| Girls |
15.5 |
18.9 |
-3.4 |
0.122 |
10.6 |
10.7 |
-0.1 |
0.958 |
3.3 |
0.239 |
| by Age Group |
|
|
|
|
|
|
|
|
|
|
| 6-23 m |
25.6 |
16.2 |
9.4 |
0.00 |
18.1 |
14 |
4.1 |
0.052 |
-5.3 |
0.114 |
| 24-59 m |
10.8 |
15.9 |
-5.1 |
0.005 |
6.4 |
10.6 |
-4.2 |
0.004 |
0.9 |
0.712 |
| by Wealth Quintiles |
|
|
|
|
|
|
|
|
|
|
| Lowest |
16.7 |
21.1 |
-4.4 |
0.206 |
11.7 |
13.5 |
-1.8 |
0.616 |
2.5 |
0.613 |
| Second |
23.8 |
18.2 |
5.5 |
0.123 |
14 |
19.5 |
-5.5 |
0.156 |
-11 |
0.037 |
| Middle |
18.6 |
23.7 |
-5 |
0.148 |
11.3 |
13.5 |
-2.2 |
0.497 |
2.8 |
0.552 |
| Fourth |
17.2 |
13.5 |
3.7 |
0.302 |
13 |
12.6 |
0.5 |
0.862 |
-3.3 |
0.466 |
| Highest |
10.9 |
4.8 |
6.1 |
0.063 |
9.3 |
9.2 |
0.2 |
0.933 |
-5.9 |
0.12 |
| Underweight (overall) |
47.8 |
42.7 |
5.1 |
0.021 |
33.6 |
36.7 |
-3.1 |
0.078 |
-8.2 |
0.004 |
| by Gender |
|
|
|
|
|
|
|
|
|
|
| Boys |
48 |
43.9 |
4.1 |
0.184 |
35.4 |
38.2 |
-2.9 |
0.258 |
-6.9 |
0.081 |
| Girls |
47.5 |
42.9 |
4.6 |
0.146 |
31.8 |
35.1 |
-3.3 |
0.188 |
-7.9 |
0.051 |
| by Age Group |
|
|
|
|
|
|
|
|
|
|
| 6-23 m |
46.5 |
36.2 |
10.4 |
0.001 |
36.5 |
29.4 |
7.2 |
0.006 |
-3.2 |
0.444 |
| 24-59 m |
48.4 |
50.6 |
-2.2 |
0.453 |
31.2 |
42.7 |
-11.6 |
0.00 |
-9.4 |
0.014 |
| by Wealth Quintiles |
|
|
|
|
|
|
|
|
|
|
| Lowest |
46.8 |
46.6 |
0.2 |
0.973 |
33.3 |
38.7 |
-5.3 |
0.285 |
-5.5 |
0.424 |
| Second |
50.9 |
48.2 |
2.7 |
0.566 |
34.9 |
47 |
-12.1 |
0.015 |
-14.7 |
0.031 |
| Middle |
53.5 |
50.3 |
3.2 |
0.493 |
39.4 |
36.9 |
2.5 |
0.575 |
-0.8 |
0.906 |
| Fourth |
45.5 |
45.2 |
0.3 |
0.961 |
36.3 |
39.6 |
-3.3 |
0.381 |
-3.6 |
0.578 |
| Highest |
41.7 |
20.2 |
21.5 |
0 |
26.2 |
31.6 |
-5.4 |
0.08 |
-26.9 |
0 |
5. Discussion
The intervention demonstrated a significant reduction in underweight among children aged 6-59 months, with a substantial impact on childhood stunting, particularly in older age groups and higher wealth quintiles. However, no significant impact was observed on wasting. Notably, while the intervention significantly reduced stunting in children aged 24-59 months, this effect was not observed in younger children aged 6-23 months; though a large differential change in stunting was observed.
Stunting and underweight, though easily measurable in surveys, may not fully capture overall health status, nutritional deficiencies, or child development. Stunting often reflects deficient environments influenced by nutrient and food limitations [
2]. Nutritional supplementation may have played a significant role in improving the deficient environment, leading to reduced stunting and underweight.
An RCT conducted on a subset of our study population showed promising evidence [
9,
22] that LNS during the first 1000 days of life improved linear growth and reduced stunting in children at 24 months of age[
25]. When the intervention is implemented in the controlled circumstances of a randomised controlled trial, it impacts child growth. However, the impact is less clear when the intervention is delivered in a public sector program. We observed that the RCT focused on 6-23 months old children whereas the quasi-experimental study included children up to 59 months in the intervention. The reasons for this difference in outcome between the RCT and our study could be many including uninterrupted supply chain of LNS, more engagement and prioritization by lady health workers, more compliance and non-sharing of LNS with other siblings, and effective behavioral change communication (BCC). In the quasi experimental study, the challenge becomes more when BCC is merely replaced by education or awareness sessions that do not focus on small doable actions which are enablers of a behaviour change[
26,
27]. The lack of an impact in the younger age group might be shorter exposure to nutrient supplements compared to older children. In our study, these older children between 24 and 59 months would have completed their LNS up to 23 months of age and continued with MNP, but the younger age group was still receiving the supplements. It is difficult to ascertain strict adherence to the daily consumption of LNS. There are also chances for an interrupted supply chain for LNS in the far-flung areas of Thatta and Sajawal, which could be a reason for observing the impact in the highest wealth quintiles and older age groups as they had more access to other foods and more nutrients, and the supplement just helped them to bridge the minimum requirement. Supply chain delays can easily be considered as reasons for the unmet needs of children from less wealthy households and younger age groups. It can also be argued that since the impact of LNS supplementation in an RCT [
9] performed on a subset of these children was only observed at 24 months, this could be considered as a minimum supplementation period for observing any significant impact. It also questions the effectiveness of maternal supplementation alone if the impact is only visible after the child has completed supplementation up to 24 months of age. In addition, the highest wealth quintile and older age groups (longer supplementation) clearly show a significant DID in stunting levels, illustrating the impact of nutritional supplementation in improving one element of the deficient environment, but this may not have been the case for children from lower wealth quintiles and younger age groups, and thus a non-significant DID result. Another finding is that the improvement was greater in boys than in girls. A lower impact on girls can be attributed to gender preference, which is well-documented in the local context [
28,
29].
Studies also suggest that combining BCC with supplementary foods in deficient or food insecure environments improves dietary diversity [
24]. Our interventions addressed the nutrient gap through supplementation underpinned by behaviour change communication and was delivered through a public sector mechanism. This showed that such an intervention is possible and sustainable if the local supply chain is established. However, it is possible that the complimentary feeding at homes is substantially inadequate and the supplementation through nutrition programs may not be sufficient to bridge the nutrient gap [
24]. We have also observed the change in stunting reduction is significant in high wealth quintiles, which could be because of lesser nutrient gap; that was bridged by the supplementation and underpinned by BCC. The significant impact on underweight and differential change in stunting support that scale up will benefit the community. The impact may feel small on percentages but given the population size in Pakistan, the numbers are huge and thus will have an intergenerational impact in the lives of many in improving their deficient environment. This will not only reduce the burden on health system, but it will also reduce the deficient environments which stunting is an outcome and leads to benefits beyond health sector. Given that it was the first such effort in Pakistan, it is critical that scale-up is considered with designer thinking and locally acclimatized to each of the focus districts.
Our trial presented challenges similar to many other trials where short- to medium-term assessments of stunting prevention programs (interventions) have not significantly reduced stunting [
24]. These programs may have achieved other outcomes, but their limited impact on stunting may undermine their credibility in front of policymakers[
24]. Evidence suggests that the reduction in stunting prevalence also depends on underlying factors such as the social and political situation, economic factors, and sanitation conditions [
30].
Our study population had levels and patterns of child undernutrition comparable to many other low- and middle-income countries. Studies have found that the prevalence of stunting and underweight gradually increases with age from birth until 24 to 36 months [
31] [
31]We found similar patterns in our data where stunting and underweight were higher with increasing child age, especially in children older than two years [
6,
32]. Our findings are similar to those of studies conducted in other Asian countries [
32,
33]. Also, a study from Nigeria suggested that appropriate supplementation in the first 1000 days of life can avert stunting [
34]. Studies also observed that stunting levels reduce as household wealth increases, a finding we observed in our study [
6].
This study has a large sample, with matching controls within the district, and documents good participation. This study uses DID analysis and propensity score matching approach to estimate impact. It also allows evaluating an LNS-based product approach implemented through Lady Health Workers (LHW). It evaluates programs in the public sector where differences existed between the program and comparison districts at baseline and the end line. We used a cross-sectional survey design with intervention and control areas at baseline and end-line surveys to assess the absolute effect of the intervention program. However, the stunting prevention program has some limitations. First, we did not have data on exposure to LNS and MNP for children aged 6-59 months. As cross-sectional surveys cannot establish causality, we could not link the reduction in stunting prevalence to the consumption of LNS and MNP. Second, the impact on children 6-23 months can be due to the exposure of their mothers to supplements during pregnancy and lactation, as well as the children's own exposure to LNS. Hence, exposure to both supplements may have contributed to the reduction in stunting, wasting, and underweight among older children 24-59 months at the end line. In addition, occasional and continued exposure to other donor-funded projects in the study areas is possible.
It is important to consider that the real goal of nutritional programs is not only to change the statistical indicators but also to reduce the long-term consequences and child mortality linked to poor linear growth. This change will require social and political commitments leading to multi-sectoral interventions that will improve deficient environments, including targeting the affordability of families to access essential nutrients. Standalone interventions will not bring drastic changes across the population. This study clearly shows the need to look at indicators beyond stunting, wasting and underweight to assess program performance. These could include but are not limited to anemia in children and pregnant mothers, change in the infant and young child feeding practices thus improving dietary diversity and minimum acceptable diet. For policy perspective the gains documented in this study shows that food supplementation underpinned by effective BCC is critical for improving the deficient environment. However, we need to do more research to identify the real nutrient gap. This will help improve the deficient environments and make a difference in the lives of those constrained by the limited access and availability of nutritious food. The researcher and policymakers may also consider options for better connectivity with the program participants by deploying technological solutions (like mobile apps) to engage and improve the BCC.
5. Conclusions
In conclusion, nutritional supplementation and behavior change communication during the first 1000 days reduced stunting and underweight among children aged 24-59 months. This evidence further establishes that nutrient uptake for a short duration cannot effectively reduce stunting and underweight. It has to be a continued supplementation for 1000 days and beyond, underpinned by social, economic, and political support. Thus, the public sector can deliver continued supplementation in the first 1000 days and beyond in children 6-59 months of age. It can be an effective and scalable intervention for improving their nutritional status.
Author Contributions
K.A., T.H., M.JD. and S.B.S. designed the study; K.A. performed the analysis and drafted the manuscript; T.H., M.JD. and S.B.S. provided data analysis advice; M.S. and I.M. assisted in analysis.: M.U. and G.N. supervise the study implementation and data collection; T.H., J.I., S.A., M.JD. and S.B.S. revised the final manuscript. All authors read and approved the manuscript.
Funding
This secondary analysis/research received no external funding.
Informed Consent Statement
“Informed consent was obtained from all subjects involved in the study.
Restrictions apply to the availability of these data. Data is available on request with the permission of corresponding author of Aga Khan University, Pakistan.
Acknowledgments
We acknowledge the support of Aga Khan University field staff for data collection, entry and cleaning. We also acknowledge the support of the Government of Pakistan in supporting this work.
Conflicts of Interest
“The authors declare no conflict of interest.”.
References
- Organization, W.H., Global health risks: mortality and burden of disease attributable to selected major risk factors. 2009.
- Leroy, J.L. and E.A. Frongillo, Perspective: What Does Stunting Really Mean? A Critical Review of the Evidence. Adv Nutr, 2019. 10(2): p. 196-204. [CrossRef]
- Pakistan, U.a.G.o., National Nutrition Survey 2018: Key Findings Report. 2019.
- Pelletier, D.L., et al., The effects of malnutrition on child mortality in developing countries. Bull World Health Organ, 1995. 73(4): p. 443-8.
- Abu-Saad, K. and D. Fraser, Maternal nutrition and birth outcomes. Epidemiol Rev, 2010. 32: p. 5-25.
- Adhikari, R.P., et al., Determinants of stunting among children aged 0-59 months in Nepal: findings from Nepal Demographic and health Survey, 2006, 2011, and 2016. BMC Nutr, 2019. 5: p. 37.
- Ahmed, S., et al., Socio-economic Inequity of Malnutrition among Under-Five Children and Women at Reproductive Age in Bangladesh. World Journal of Nutrition and Health, 2013. 1(1): p. 13-17.
- UNICEF, G.o.P.a., National Nutrition Survey 2018, Key Findings Report. 2019.
- Soofi, S.B., et al., Effectiveness of nutritional supplementation during the first 1000-days of life to reduce child undernutrition: A cluster randomized controlled trial in Pakistan. Lancet Reg Health Southeast Asia, 2022. 4: p. 100035. [CrossRef]
- Khan, M. and A. Shah, Food Insecurity in Pakistan: Causes and Policy Response. Journal of Agricultural and Environmental Ethics, 2011. 24: p. 493-509.
- Dewey, K.G., Reducing stunting by improving maternal, infant and young child nutrition in regions such as South Asia: evidence, challenges and opportunities. Matern Child Nutr, 2016. 12 Suppl 1(Suppl 1): p. 27-38. [CrossRef]
- Dewey, K.G. and S. Adu-Afarwuah, Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr, 2008. 4 Suppl 1(Suppl 1): p. 24-85. [CrossRef]
- Black, R.E., et al., Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet, 2013. 382(9890): p. 427-451. [CrossRef]
- Thurstans, S., et al., The relationship between wasting and stunting in young children: A systematic review. Matern Child Nutr, 2022. 18(1): p. e13246. [CrossRef]
- Adu-Afarwuah, S., et al., Small-quantity, lipid-based nutrient supplements provided to women during pregnancy and 6 mo postpartum and to their infants from 6 mo of age increase the mean attained length of 18-mo-old children in semi-urban Ghana: a randomized controlled trial. Am J Clin Nutr, 2016. 104(3): p. 797-808. [CrossRef]
- Adu-Afarwuah, S., A. Lartey, and K.G. Dewey, Meeting nutritional needs in the first 1000 days: a place for small-quantity lipid-based nutrient supplements. Ann N Y Acad Sci, 2017. 1392(1): p. 18-29. [CrossRef]
- Ceesay, S.M., et al., Effects on birth weight and perinatal mortality of maternal dietary supplements in rural Gambia: 5 year randomised controlled trial. Bmj, 1997. 315(7111): p. 786-90. [CrossRef]
- Mridha, M.K., et al., Lipid-based nutrient supplements for pregnant women reduce newborn stunting in a cluster-randomized controlled effectiveness trial in Bangladesh. Am J Clin Nutr, 2016. 103(1): p. 236-49. [CrossRef]
- Lesorogol, C., et al., Preventative lipid-based nutrient supplements (LNS) and young child feeding practices: findings from qualitative research in Haiti. Matern Child Nutr, 2015. 11 Suppl 4(Suppl 4): p. 62-76. [CrossRef]
- Lazzerini, M., L. Rubert, and P. Pani, Specially formulated foods for treating children with moderate acute malnutrition in low- and middle-income countries. Cochrane Database Syst Rev, 2013(6): p. Cd009584. [CrossRef]
- Siega-Riz, A.M., et al., Effect of supplementation with a lipid-based nutrient supplement on the micronutrient status of children aged 6-18 months living in the rural region of Intibucá, Honduras. Paediatr Perinat Epidemiol, 2014. 28(3): p. 245-54.
- Kureishy, S., et al., A mixed methods study to assess the effectiveness of food-based interventions to prevent stunting among children under-five years in Districts Thatta and Sujawal, Sindh Province, Pakistan: study protocol. BMC Public Health, 2017. 17(1): p. 24. [CrossRef]
- Wing, C., K. Simon, and R.A. Bello-Gomez, Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu Rev Public Health, 2018. 39: p. 453-469. [CrossRef]
- Christian, P., et al., Impact Evaluation of a Comprehensive Nutrition Program for Reducing Stunting in Children Aged 6-23 Months in Rural Malawi. J Nutr, 2020. 150(11): p. 3024-3032. [CrossRef]
- Das, J.K., et al., Preventive lipid-based nutrient supplements given with complementary foods to infants and young children 6 to 23 months of age for health, nutrition, and developmental outcomes. Cochrane Database Syst Rev, 2019. 5(5): p. Cd012611.
- Fabrizio, C.S., M. van Liere, and G. Pelto, Identifying determinants of effective complementary feeding behaviour change interventions in developing countries. Maternal & Child Nutrition, 2014. 10(4): p. 575-592. [CrossRef]
- Koenker, H., et al., Strategic roles for behaviour change communication in a changing malaria landscape. Malaria Journal, 2014. 13(1): p. 1. [CrossRef]
- Basu, A.M., How pervasive are sex differentials in childhood nutritional levels in south Asia? Soc Biol, 1993. 40(1-2): p. 25-37.
- Nuruddin, R. and W.C. Hadden, Are pre-school girls more likely to be under-nourished in rural Thatta, Pakistan?-a cross-sectional study. Int J Equity Health, 2015. 14: p. 151. [CrossRef]
- Roba, A.A., et al., Prevalence and determinants of concurrent wasting and stunting and other indicators of malnutrition among children 6-59 months old in Kersa, Ethiopia. Matern Child Nutr, 2021. 17(3): p. e13172. [CrossRef]
- Victora, C.G., et al., Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. The Lancet, 2021. 397(10282): p. 1388-1399. [CrossRef]
- Correa, P.R., Factors associated with stunting among children 0 to 59 months of age in Angola: A cross-sectional study using the 2015-2016 Demographic and Health Survey. PLOS Glob Public Health, 2022. 2(12): p. e0000983. [CrossRef]
- Pasricha, S.R., et al., Benefits and Risks of Iron Interventions in Infants in Rural Bangladesh. N Engl J Med, 2021. 385(11): p. 982-995. [CrossRef]
- Ezeh, O.K., et al., Trends of Stunting Prevalence and Its Associated Factors among Nigerian Children Aged 0-59 Months Residing in the Northern Nigeria, 2008-2018. Nutrients, 2021. 13(12). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).