1. Introduction
Stress is a pervasive condition that affects an individual's physical, mental, and emotional well-being. It has an impact on sleep patterns, dietary habits, self-perception, and cognitive functions. Individuals experiencing comorbid stress and mental disorder face difficulties in achieving prompt recovery. Without treatment, the symptoms can endure for extended periods of time, ranging from weeks to months or even years. Many people face challenging barriers in life that may clash or intersect, leading to stress that can have negative effects on their well-being. Workplace, interpersonal, and domestic factors can all contribute to the onset of stress.
Stress can manifest both physically and cognitively, resulting in alterations in multiple physiological reactions and potentially leading to pathological conditions. These can have a detrimental impact on an individual's ability to focus and be productive, particularly by disrupting task execution. Over time, stress can exacerbate cognitive deficiencies and contribute to several issues including Diabetes, high Blood Pressure (BP), increased vulnerability to substance addiction, weakened immune system, and depression [
1,
2].
Effective stress management is crucial for sustaining optimal health. Currently, self-assessment questionnaires like the Perceived Stress Scale (PSS) [
3] are commonly used to measure stress levels. However, this method is not very practical. Technology can play a vital role in the evaluation of stress. Various suggestions have emerged, mostly utilizing smart bands, smartphones, and wearables, to acquire physiological measurements that are associated with stress detection, such as Heart Rate (HR), Heart Rate Variability (HRV), and Galvanic Skin Response (GSR), among others. No comprehensive solution for acquiring several parameters has been suggested yet due to various challenges such as limited battery life, interference from noise, device compatibility issues, system portability, user acceptance, and accuracy concerns.
This study presents advancements to the previous research conducted by the same authors [
4]. The previous work involved the development of a multichannel sensory system that focused on acquiring and processing Photoplethysmography (PPG) signals. In this study, the authors expanded the system by incorporating the acquisition of GSR and body temperature, two parameters closely associated with stress. This system also incorporated the utilization of sophisticated algorithms for the estimation of physiological parameters and the application of machine learning for the classification of stress levels. The advancements pertain to the incorporation of two more channels for monitoring BP and blood glucose levels, hence enhancing the system's ability to cater to the requirements of individuals with diabetes and hypertension. Proposed enhancements are suggested for both the intelligent stress assessment system and the developed mobile application, which would greatly assist patients in their daily life.
The structure of this article is as follows. The history of health monitoring and stress assessment is discussed in Section II, as well as the connections and effects between stress, blood pressure, and glucose levels. The methodology employed is described in Section III, including the materials and tasks that were performed. The findings acquired through the executed experimental procedures are elaborated upon in Section IV. The conclusions and future work are presented in Section V.
2. Related Work
Stress is a state of tension or pressure that arises from daily experiences or situations. It has a direct impact on the management of chronic diseases like hypertension or diabetes, which are closely linked. Moreover, stress can be a significant burden on individuals' lives. Therefore, it is crucial to effectively manage stress levels.
2.1. Impact of Stress on Diabetes
The main endocrine reactions to stress are glucocorticoids and catecholamines. Although these compounds do not have any negative effects in the short term, they might gradually alter the balance of glucose in the body by hindering the muscles and tissues from absorbing and using glucose. Extended elevation of blood sugar levels caused by this disruption in glucose regulation can lead to insulin resistance and the development of type II diabetes [
1]. In addition, it can lead to a gradual decrease in muscle mass and the accumulation of visceral fat [
5].
Metabolic abnormalities are recognized as products of chronic stress and obesity. Insulin resistance outcome of this metabolic anomaly. Survival under stress is facilitated by physiological responses that have been maintained through evolution, such as hyperglycemia and insulin resistance [
6]. White and red blood cells, the reticuloendothelial system, the central and peripheral nervous systems, and bone marrow are the largest consumers of glucose without requiring insulin [
7]. The immune system and brain are also fueled by stress hyperglycemia in response to injury, infection, and stress [
8,
9]. Acute hyperglycemia during stress may be advantageous to the body and an integral part of its evolutionary process, as discussed previously. However, chronic stress induces insulin resistance because of various factors, including chronic hyperglycemia. Thus, persistent stress causes type II diabetes.
Type II diabetes is defined by the presence of an excessive amount of glucose in the bloodstream, which cannot be effectively used by the body due to a condition called insulin resistance. It can lead to significant challenges, disturbance of daily living, and persistent health problems. Possible effects include neuropathy, nephropathy, cataracts, glaucoma, increased susceptibility to severe fungal infections, delayed wound healing, auditory impairment, and other similar issues. Patients should be motivated to participate in daily activities and adhere to regular follow-up consultations, as prevention is always better, especially considering that the illness is predominantly associated with obesity and can be reversed with dietary changes, physical exercise, and medications [
10].
2.2. Stress and Blood Pressure
Concerning the relationship between stress and BP, it is important to understand that the human body produces an abundance of hormones because of stress. These hormones transiently elevate blood pressure, resulting in increased HR and constriction of blood vessels. Fluctuations in the size of blood vessels might increase the likelihood of experiencing health issues, such as hypertension (which is characterized by high blood pressure caused by narrowed blood vessels) and hypotension (which is associated with low blood pressure due to widened blood vessels) [
11]. Clinical trials have examined the impact of cognitive behavioural approaches on blood pressure [
12].
2.3. Correlation between Diabetes and Blood Pressure
Diabetes is a long-term condition caused by insufficient insulin, which can be due to a lack of insulin production or insensitivity to insulin [
13]. It is linked to various complications primarily caused by consistently high blood glucose levels, which can result in the development of microvascular diseases (damage to small blood vessels) and macrovascular diseases (damage to arteries). Diabetic complications, such as neuropathy (nerve damage), retinopathy (eye disease), and nephropathy (kidney disease), occur due to the vascular damage that affects organs and tissues [
14].
Previous studies have confirmed a connection between hypertension and diabetes [
15]. This connection is not only since individuals with diabetes are more likely to develop hypertension compared to those without diabetes [
16], but it also increases the likelihood of these two illnesses occurring together. Therefore, the simultaneous presence of these two circumstances may result in the emergence of novel public health concerns, such as an elevated vulnerability to stroke [
17], a notable rise in disruptions to the body's natural sleep-wake cycle, and harm to specific organs [
18]. Furthermore, in patients with both diabetes and hypertension, insulin resistance is a separate risk factor for ischemic cerebral infarction, particularly lacunar infarction [
19].
2.4. Stress Management
Managing stress requires maintaining an active, wholesome, and enjoyable lifestyle. Lifestyle modifications, exercise, meditation, yoga, relaxation, and the modification of behavior and attitude are all components of stress treatment programs. Changes in perspective are vital for stress management. This necessitates an optimistic mindset and a positive perspective. Rather than a ritual, stress management is a holistic process that balances physical, psychological, emotional, and spiritual health. It enhances concentration, serenity, productivity, and perseverance.
Continuous monitoring of stress levels is essential for effective stress management. Stress is assessed using non-invasive physiological assessment methods, including Electrocardiography (ECG), HR, GSR and BP, as well as respiratory activity [
20,
21,
22].
Additionally, stress monitoring using face recognition technology has been documented [
23], [
24]. This approach leverages the functionalities of mobile devices, including tablets and smartphones [
25], [
26]. An illustration of this concept is facing recognition, which attempts to determine an individual's affective state through the comparison of a captured facial expression and a database comprising instances of facial expressions that correspond to a predetermined meaning.
3. Materials and Methods
This section provides an overview of the healthcare monitoring system that has been proposed, along with the experimental procedure used to validate the system and the fuzzy logic model that has been developed for stress assessment. Considerations were also given to the classification of blood glucose levels.
3.1. Proposed Healthcare System
The physiological parameters gathered by the proposed system can be used to evaluate the stress level and overall health of the user. The system architecture is illustrated in the following
Figure 1. To provide greater specificity, the architecture of the system comprises the subsequent layers:
Sensing System: wearable device developed for the acquisition of physiological parameters and the establishment of a communication channel with the mobile application, allowing users to be authenticated and data to be stored locally or remotely, depending on the availability of the network.
Mobile Application: a user interface is provided to access the data stored in the database. This interface allows entry of data such as glucose and blood pressure levels. It also includes a feature to classify stress levels, user authentication, and clinical advice based on the analysis of physiological indicators.
Database: tasked with the remote storage of user-specific data and information. The Google NoSQL database "Firebase" was selected for the proposed system because of its benefits in developing mobile and web applications, including its interoperability with IOS, Android, Web, Unity, and C++.
Glucose Monitor: Element NEO is a straightforward glucose monitor designed to assist users in managing diabetes by incorporating functions that reduce the likelihood of complications associated with this condition. With its backlit display, ergonomic design, and illumination at the test strip insertion point, this device is suitable for all types of users. This device has been certified by Common Era (CE) [
27].
Blood Pressure Monitor: measures BP and pulse rate and allow users to check the results directly on the screen, which changes color depending on the level of blood pressure (red, yellow, and green). This device has been certified by the U.S. Food and Drug Administration (FDA) and CE [
28].
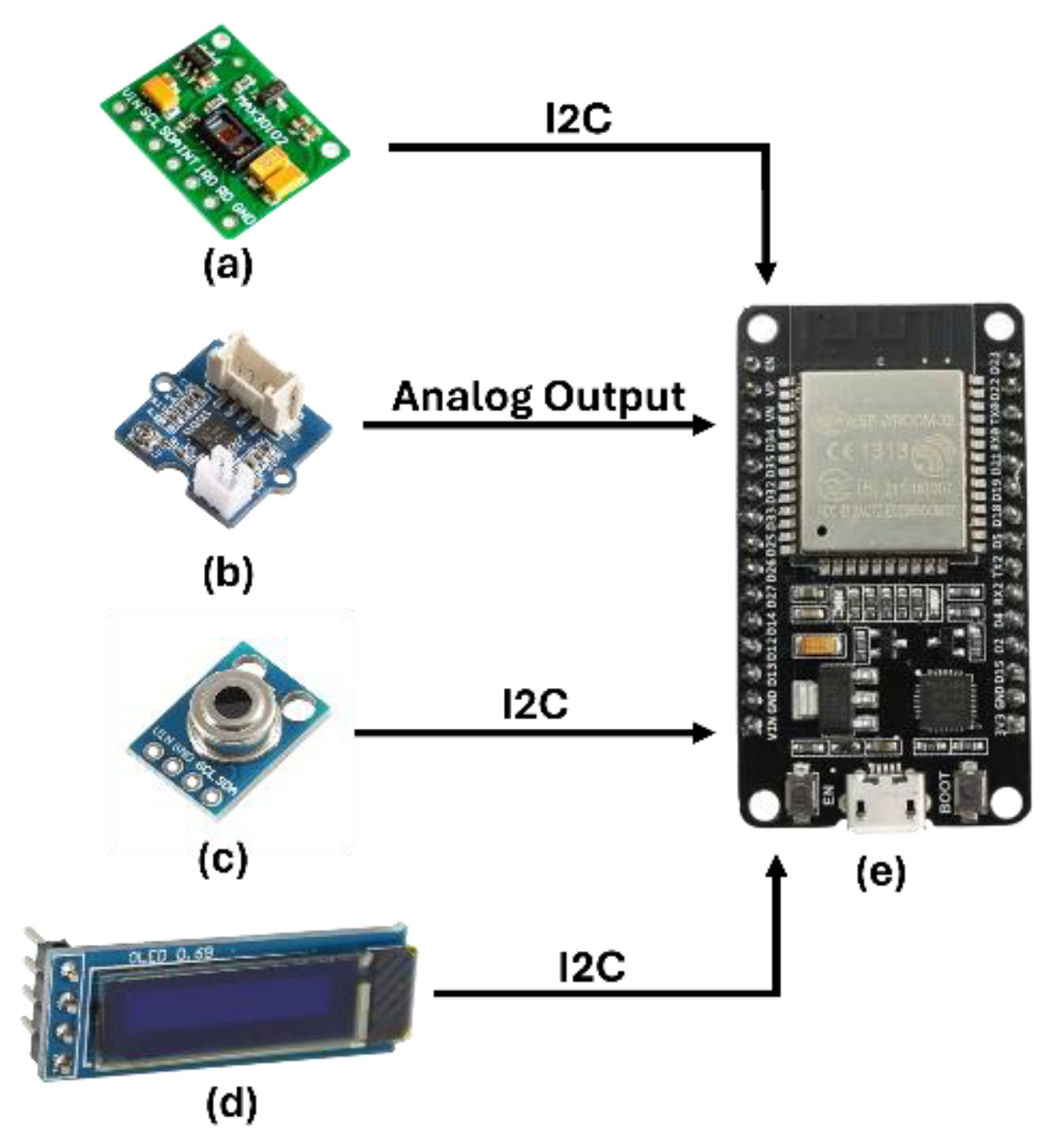
3.1.1. Sensing System
The proposed sensing system builds upon the prior research [
4] and utilizes PPG signal processing to estimate HR, Pulse Rate Variability (PRV), Blood Oxygen Saturation (SpO2), and Respiratory Rate (RR). This system also has channels for gathering physiological indicators that are essential to monitoring health status and classifying stress levels, such as GSR and Body Temperature (BT). The architecture of the sensing system is depicted in
Figure 2. The system's sampling rate is 300 samples per second, enabling it to accurately reproduce the PPG signal. To determine the values of HR, PRV, RR, and SpO2, it is crucial to identify the highest points in the signals. Therefore, the system collects two measurements of each physiological parameter every second.
The sensing system consists of an ESP32 Microcontroller with a Dual-Core 32-bit CPU, a maximum Clock speed of 240 MHz, a ROM memory capacity of 448 Kbytes, a RAM capacity of 520 Kbytes, and a Flash memory capacity of 4 MB. Utilizing Digital Signal Processing (DSP), the PPG signal was analyzed to determine the highest, lowest, and average values. Additionally, the HR, PRV, RR, and SpO2 were estimated. The data is thereafter transmitted via Bluetooth 5.1 to the mobile application for data storage purpose.
The system incorporates a MAX30102 PPG sensor that enables the capture of the infrared component of the PPG signal, which is essential for estimating HR, PRV, and RR. Additionally, it captures the red-light component of the PPG signal, which is important for estimating SpO2. Additionally, a GSR sensor was incorporated to measure changes in sweat gland activity caused by stress. The GY906 sensor accurately monitors infrared body temperature within a temperature range of -70 ºC to +380 ºC, with a precision of 0.5 ºC, regardless of whether there is physical contact or not. The system is equipped with a real-time data display screen and Li-Po batteries that offer up to 4 hours of uninterrupted monitoring autonomy each. The system components establish communication with the ESP32 through the Inter-Integrated Circuit (I2C) protocol.
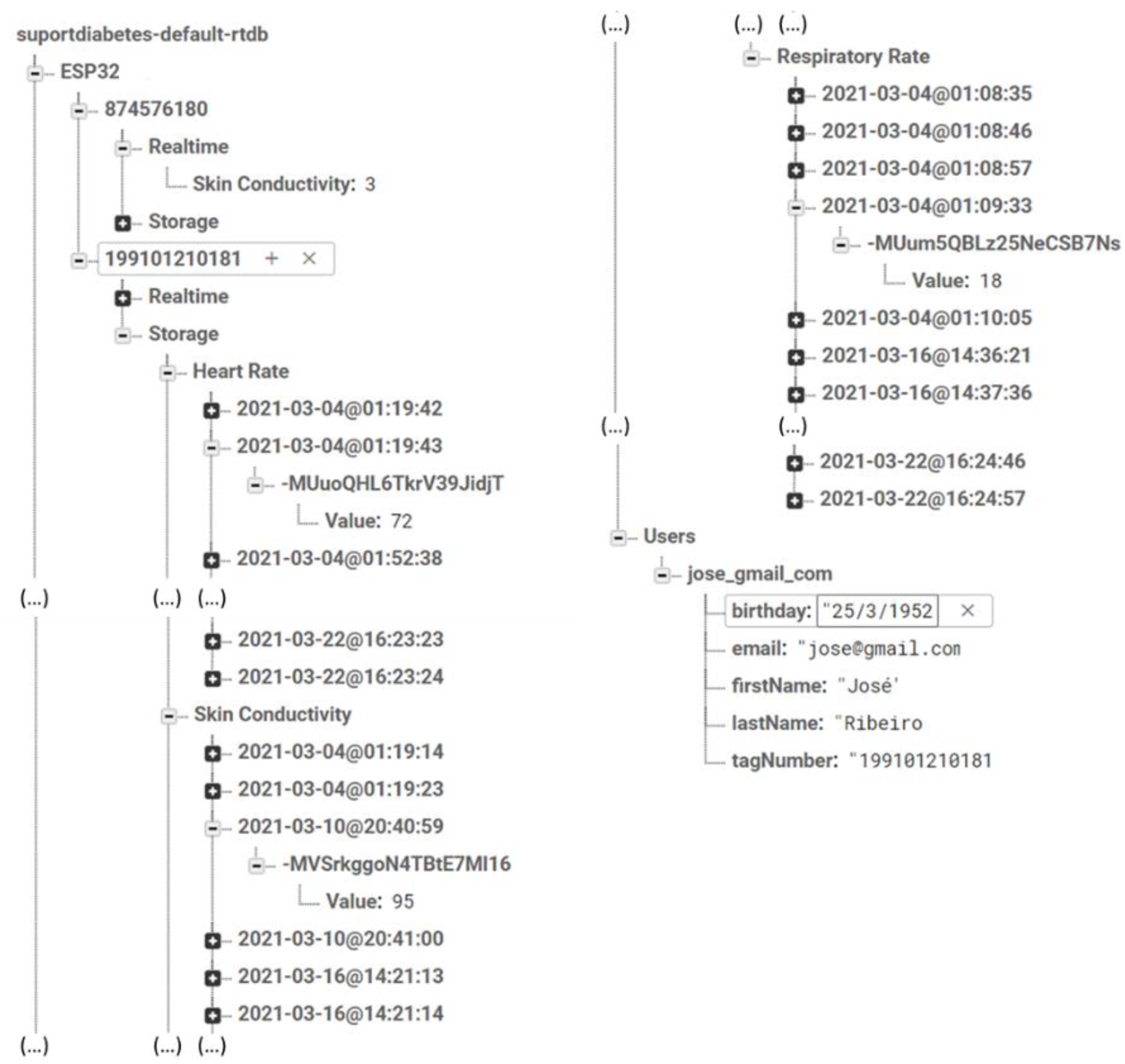
3.1.2. Database
As technology advances, intelligent systems are more dependent on efficient and automated data processing methods, such as Machine Learning (ML) approaches, Neural Networks, Deep Learning, Data Mining, and others. For these technologies to carry out their functions effectively and precisely, they require substantial quantities of data kept within databases. Therefore, selecting the most appropriate database for a system is of utmost importance. Some databases are specifically designed for processing and implementing algorithms, while others are more advantageous for quick access and customised organisation based on data type [
29].
The Google "Firebase" platform was selected for implementing this system because to its dynamic database capabilities, which offer significant benefits for mobile and web application development. It is compatible with IOS, Android, Web, Unity, and C++. This platform offers both real-time access and a high level of interaction with cloud storage, use of ML techniques, rapid and secure authentication methods, and other features [
30].
Figure 3 demonstrates how Firebase is configured to store data. Each user is assigned a unique identification (ID), and the data transmitted from the detection system and both monitors (glucose and blood pressure) is accompanied by a timestamp. Firebase organises the data within the nodes associated with each ID according to real-time data and data stored previously.
3.1.3. Mobile Application
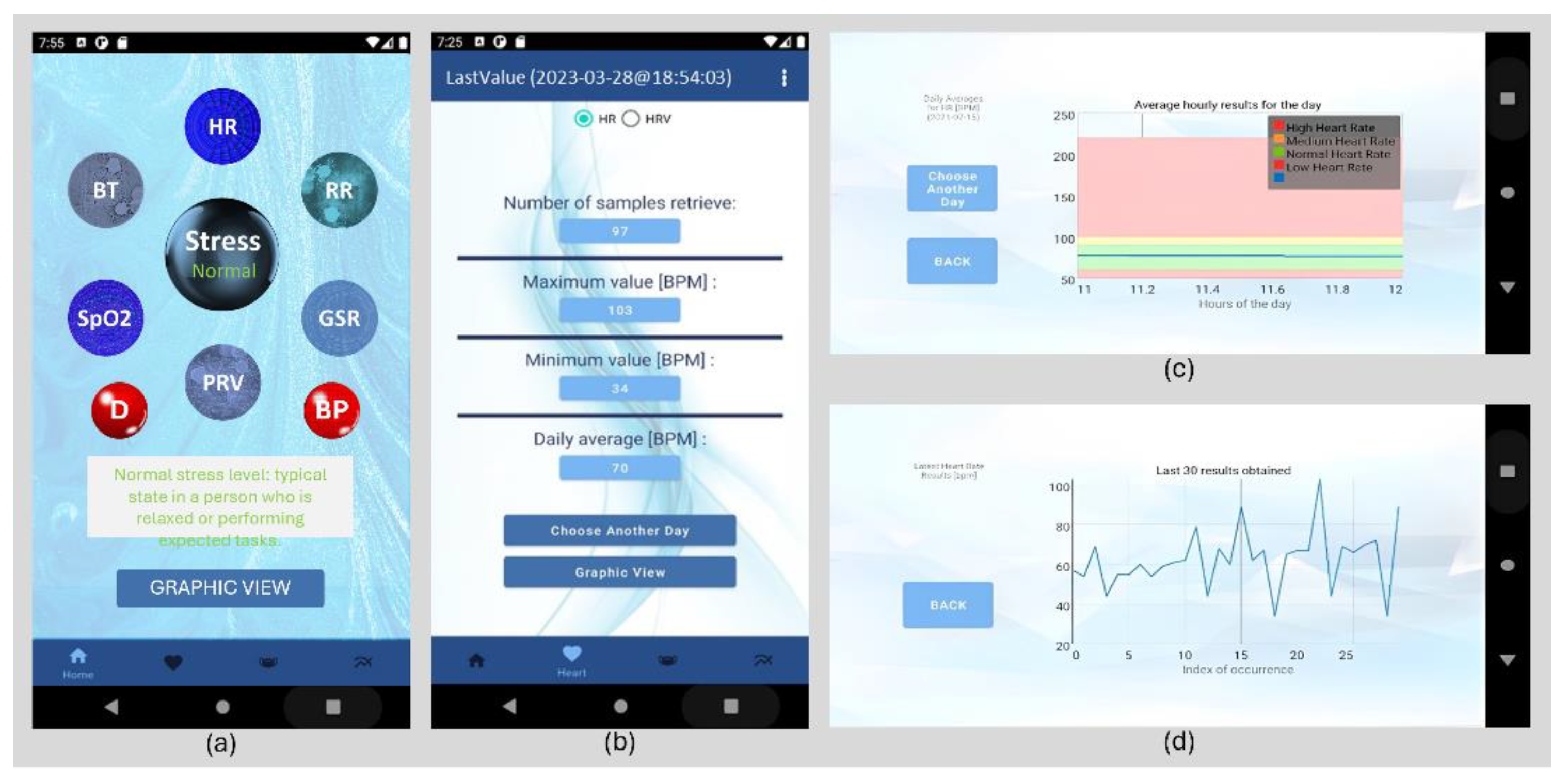
The user interface is built upon an Android mobile application, as depicted in
Figure 4. The mobile application enables user’s authentication, continuously monitor their physiological parameters, input glucose and blood pressure readings, and classify stress into three categories using the fuzzy logic model outlined in the following Subsection “3.2. Stress Assessment”.
As shown in
Figure 4 (a), the application comments on this classification and physiological parameter values. Interactive blue and red spheres provide physiological parameter information. In
Figure 4 (d), each physiological parameter's real-time progression is graphically illustrated. In
Figure 4 (b), users can access to their daily and monthly physiological parameter averages. As shown in
Figure 4 (c), these averages can be displayed on graphs with colors according to physiological parameter classifications.
3.2. Stress Assessment
The proposed algorithm for stress assessment relies on collecting stress-related physiological parameters, including HR, PRV, RR, SpO2, GSR, and BT, as described in [
4]. Additionally, BP has been incorporated into the model. The stress levels were classified using Fuzzy Logic, where we defined the reference values for each physiological parameter (HR [
31], PRV [
32], RR [
33], SpO2 [
34], GSR [
35], BT [
36], and BP [
37]). The classification and type of Membership Function were determined based on
Table 1.
The Membership Functions used in the proposed model are categorized as Trapezoidal Function Type R for "Low", Trapezoidal Function Type L for "High", and Triangular Function for "Normal", as documented in [
4] based on the physiological parameter's configuration and classification presented in
Table 1.
To implement the Fuzzy Logic model designed for stress level classification, three rules were established in accordance with the examined correlation between physiological parameters and stress [
20]. The rules are outlined in
Table 2. Following this, the stress is quantified using Equation 1.
3.3. Blood Glucose Levels
Blood glucose levels are measured in milligrams per deciliter (mg/dL) and are a crucial category for carbohydrates in biology, as they play a vital function as a metabolic energy source for cells. Prolonged elevation of glucose levels typically indicates the presence of Diabetes. Diabetes is a medical condition characterized by insufficient production of insulin by the body (type 1 diabetes) or inadequate response of the body's cells to insulin (type 2 diabetes).
To diagnose diabetes, individuals usually undergo blood glucose and hemoglobin tests. However, the results of these tests may vary depending on whether the patient has fasted or eaten food during the day. Therefore, the fluctuations in blood glucose levels [
38] are outlined in
Table 3.
3.4. Experimental Procedure
Data from 128 volunteers was considered in this study. The volunteers' specific biometric information is shown below in
Table 4. All participants gave their verbal consent. The data was cleaned and processed to ensure its accuracy and integrity and is licensed under CC BY 4.0.
The primary aim of this study is to examine the impact of stress on individuals with chronic conditions, particularly those diagnosed with diabetes. Considering the correlation between diabetes and hypertension, the system that was previously created and verified in [
4] has been modified to include two more channels. One channel is dedicated to monitoring blood glucose levels, while the other is focused on tracking blood pressure. Furthermore, the stress level assessment model used in [
4] was modified to incorporate a three-level scale and membership functions more suited to the characteristics of the data.
The experimental protocol established the simultaneous acquisition of stress, BP, and glucose data, which enabled the correlation between these three indicators. All data collection was conducted during a fasting state, taking into consideration that this is the optimal time of day for individuals with diabetes to obtain their glucose levels unaffected by the impact of food intake.
4. Results and Discussion
This section provides an analysis of the findings pertaining to the correlation between blood glucose levels and stress levels, as well as blood glucose levels and BP values. Furthermore, a comparison is conducted on the reduction of the stress assessment model's scale from five, as it was originally proposed in prior research [
4], to three.
4.1. Stress Level Classification Model Update
In a previous study, a stress assessment model comprising five levels was utilized [
4]. Nevertheless, it is important to mention that the extreme levels only consisted of residual data, which did not have any noticeable effect on the system's performance but did result in a small divergence in the accuracy of the model. Therefore, this study aimed to update these levels and thereby reduce them from five to three.
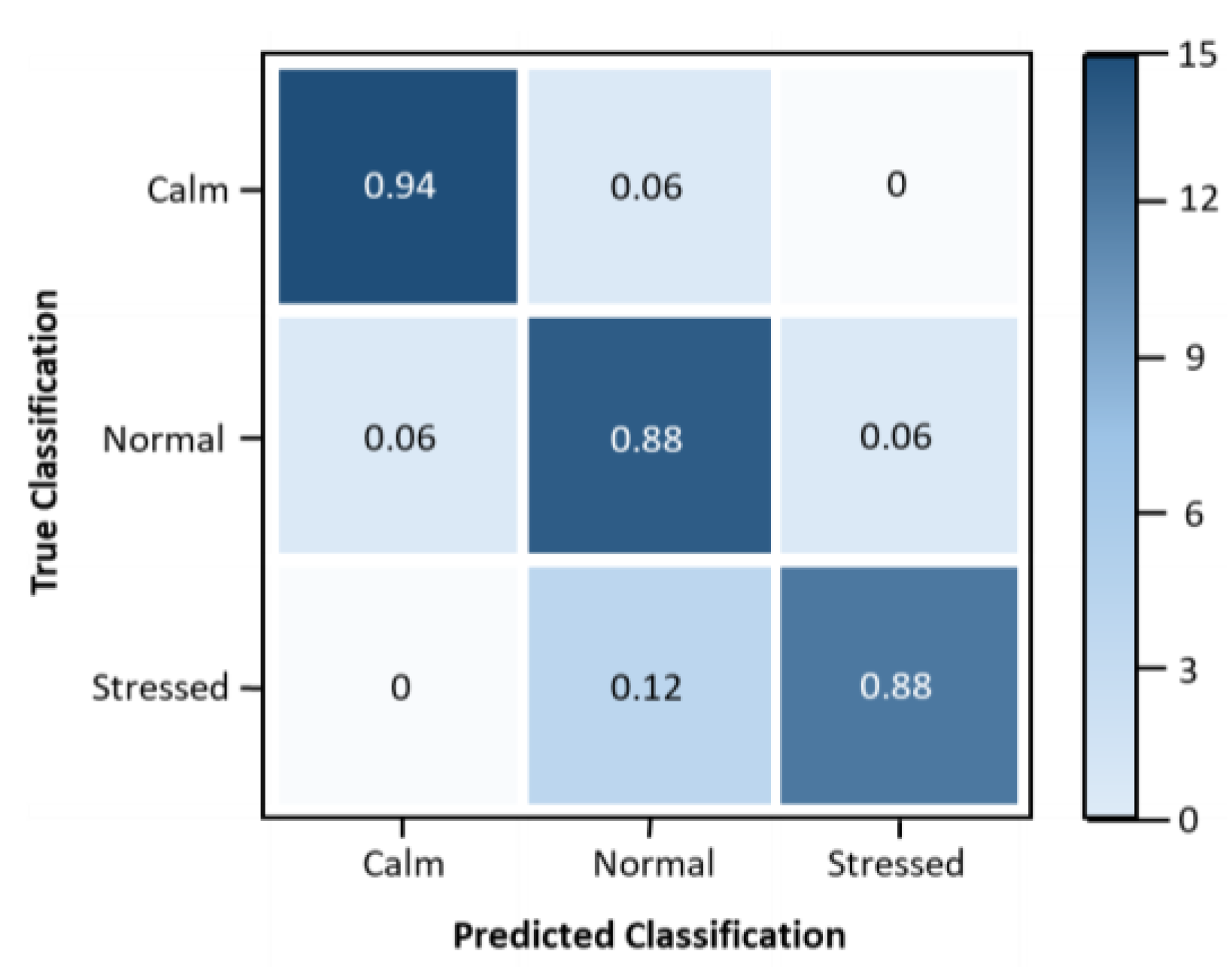
The performance of the model was evaluated using a multi-class confusion matrix, which is depicted in
Figure 5. Furthermore, several metrics were used to analyze the performance of the proposed stress assessment model, as outlined in
Table 5.
Figure 4.
Confusion Matrix with Multiple Classes for the Stress Classification Model.
Figure 4.
Confusion Matrix with Multiple Classes for the Stress Classification Model.
Table 5 demonstrates that the proposed fuzzy logic methodology update yields satisfactory outcomes in terms of precision, accuracy, sensitivity, and specificity. To enhance the suggested model, it is necessary to carry out supplementary stress induction studies or explore alternative methods of inducing stress, such as noise or light.
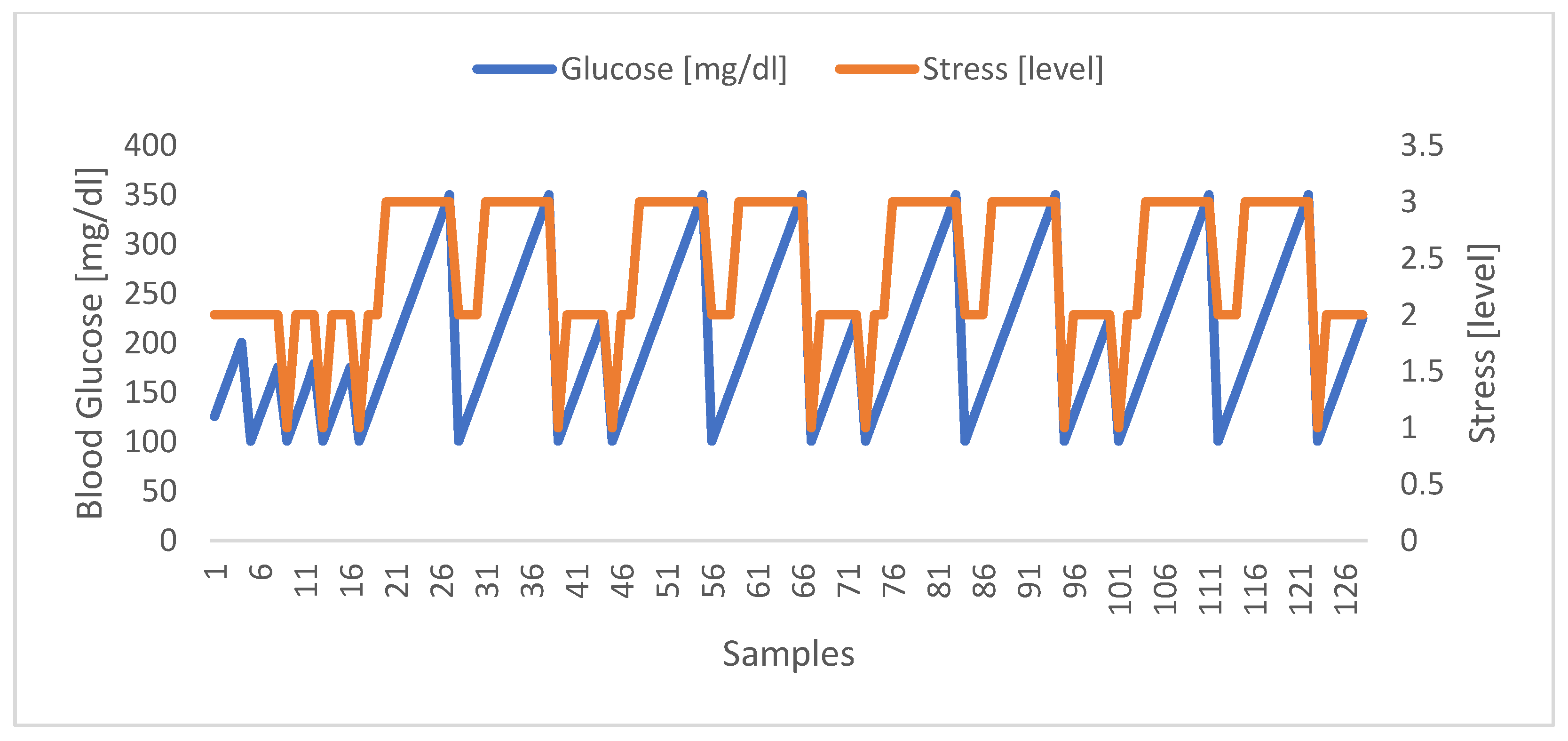
4.2. Correlation between Stress and Glucose Levels
Regarding the correlation of stress with blood glucose levels, the results obtained were promising, allowing to identify a clear relationship between the two parameters. In
Figure 5 below, it is possible to observe the evolution of the stress levels (classified from 1 to 3 as stipulated in the proposed model) and the blood glucose levels, being clear that when one increases, the other follow, and vice versa.
Figure 5.
Correlation between Stress and Glucose Levels. Highlighted in blue are the blood glucose values of the volunteers. In turn, highlighted in orange are the stress levels obtained in the same moments.
Figure 5.
Correlation between Stress and Glucose Levels. Highlighted in blue are the blood glucose values of the volunteers. In turn, highlighted in orange are the stress levels obtained in the same moments.
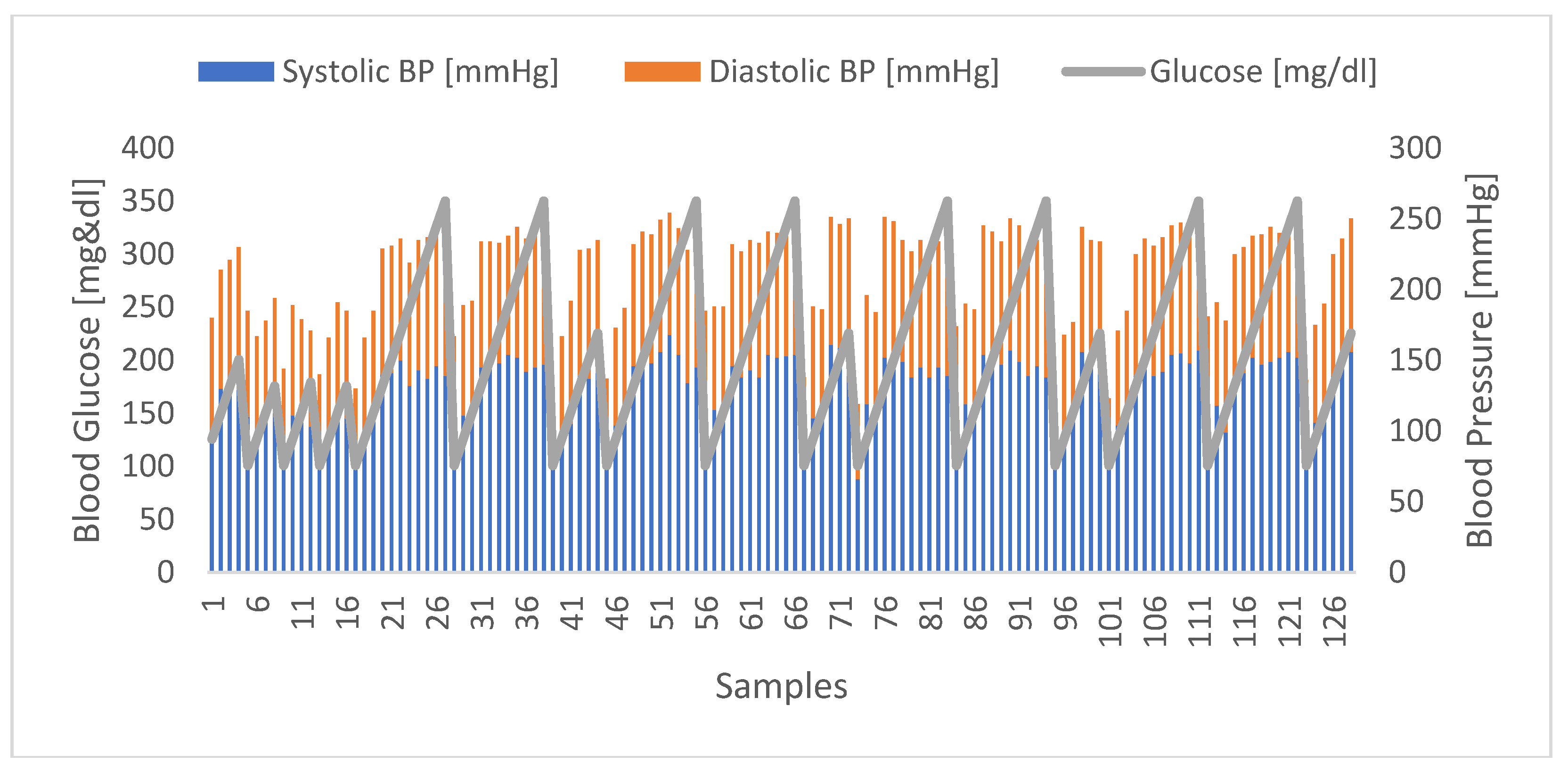
4.3. Correlation between Glucose Levels and Blood Pressure
The correlation between blood glucose levels and blood pressure was also found to be promising, as the results enabled the identification of a distinct relationship between the two parameters, considering both systolic and diastolic blood pressure components. In
Figure 6 below, it is possible to observe the evolution of glucose levels and blood pressure, to the extent that when one increases, the same is visible in the other parameter, and vice versa.
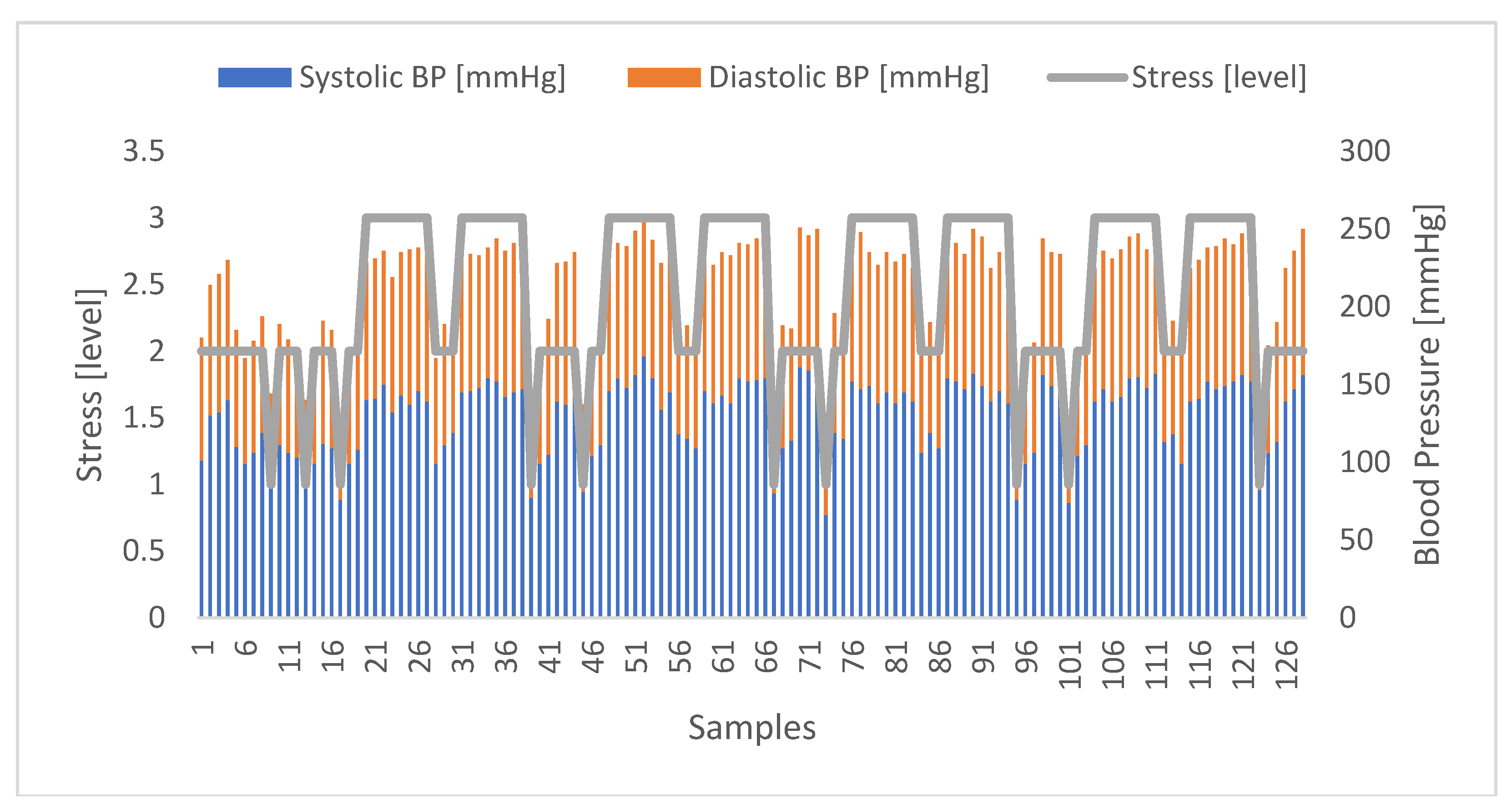
4.4. Correlation between Stress and Blood Pressure
In relation to the correlation of stress with blood pressure, the results obtained were promising, allowing to identify a clear relationship between the two parameters. In
Figure 7 below, it is possible to observe the evolution of the stress levels (classified from 1 to 3 as stipulated in the proposed model) and the blood pressure represented here through its two components, i.e. systolic blood pressure and diastolic arterial pressure.
5. Conclusions
The multichannel sensing system that has been implemented offers an important level of mobility and interactivity, enabling the real-time visualisation of health status parameters, such as stress levels. In pursuit of this objective, a mobile application was effectively designed and verified. Given that many patients with diabetes believe that controlling their well-being entails merely altering their daily routines, the way this work integrates a mobile application's user-friendly interface and an efficient system with a significant number of crucial components and mechanisms for acquiring physiological parameters is an asset in assisting these patients to gain a better understanding how their daily activities impact their health.
Significant conclusions were drawn from the experimental validation conducted to investigate the correlation between stress, diabetes, and blood pressure. These conclusions establish the relationship between these parameters and emphasise once more the importance of diabetics incorporating the management of nervous system responses into their daily routines. Despite adhering to a healthy lifestyle and carefully monitoring their blood glucose levels, diabetics should increase the concerns regarding the impact of stress.
Regarding future work, one of the next steps is to enhance the system's robustness by perhaps incorporating new mechanisms and implementing changes. One of the goals is to replace the fuzzy logic technique with more powerful machine learning techniques. Furthermore, given that the purpose of this project is to assist individuals with diabetes in their everyday activities, it would be advantageous to prioritise the development of an intelligent and mobile interface that allows for seamless user interaction. In the future, it would be beneficial to incorporate features for measuring glucose levels and blood pressure directly into the system, rather than relying on external devices currently available in the market.
Author Contributions
Conceptualization, G.R. and O.P.; methodology, G.R, J.M., O.P. and J.D.P.; hardware G.R.; software, G.R.; validation, G.R., J.M. and O.P.; formal analysis, G.R., O.P. and J.D.P.; investigation, G.R. and O.P.; resources, G.R. and O.P.; data curation, G.R.; writing—original draft preparation, G.R.; writing—review and editing, G.R., O.P. and J.D.P.; visualization, O.P. and J.D.P.; supervision, O.P.; funding acquisition, G.R. and O.P.
Funding
This work was funded by the Instituto de Telecomunicações and by FCT/MCTES through national funds and, when applicable, from EU funds co-financed under the UIDB/50008/2020 project. In addition, this work was also funded by ISCTE-Instituto Universitário de Lisboa, in the form of a merit scholarship awarded to G.R.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- T. Kuo, A. McQueen, T. C. Chen, and J. C. Wang, “Regulation of glucose homeostasis by glucocorticoids,” Adv Exp Med Biol, vol. 872, pp. 99–126, 2015. [CrossRef]
- Joshi, R. Kiran, H. K. Singla, and A. N. Sah, “Stress management through regulation of blood pressure among college students,” Work, vol. 54, no. 3, pp. 745–752, 2016. [CrossRef]
- R. Kavya, N. Nayana, K. B. Karangale, H. Madhura, and S. J. Sheela, “Photoplethysmography - A modern approach and applications,” 2020 Int. Conf. Emerg. Technol. INCET 2020, pp. 10–13, 2020. [CrossRef]
- G. Ribeiro, O. Postolache, and F. Ferrero, “A New Intelligent Approach for Automatic Stress Level Assessment Based on Multiple Physiological Parameters Monitoring,” IEEE Trans Instrum Meas, vol. 73, pp. 1–14, 2024. [CrossRef]
- K. Sharma, S. Akre, S. Chakole, and M. B. Wanjari, “Stress-Induced Diabetes: A Review,” Cureus, Sep. 2022. [CrossRef]
- Rozanski, J. A. Blumenthal, and J. Kaplan, “Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy,” Circulation, vol. 99, no. 16, pp. 2192–2217, Apr. 1999. [CrossRef]
- M. R. Soeters and P. B. Soeters, “The evolutionary benefit of insulin resistance,” Clinical Nutrition, vol. 31, no. 6, pp. 1002–1007, Dec. 2012. [CrossRef]
- P. Eter, R. S. Hepherd, B. Arbara, and B. K. Ahn, “G LUCOSE T RANSPORTERS AND I NSULIN A CTION Implications for Insulin Resistance and Diabetes Mellitus,” 1999.
- M. Oddo et al., “Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: A microdialysis study,” Crit Care Med, vol. 36, no. 12, pp. 3233–3238, 2008. [CrossRef]
- T. Duning et al., “Hypoglycemia aggravates critical illness-induced neurocognitive dysfunction,” Diabetes Care, vol. 33, no. 3, pp. 639–644. [CrossRef]
- Randall, M. Esler, B. Culp, S. Julius, and A. Zweifler, “Determinants of baroreflex sensitivity in man,” The Journal of Laboratory and Clinical Medicine, vol. 91, no. 3, pp. 514–519, Mar. 1978, Accessed: Apr. 05, 2024. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/627752/.
- V. Malhotra, “A study on the effect of individual asanas on blood pressure,” 2005. [Online]. Available: https://www.researchgate.net/publication/328214060.
- D. M. Patel, M. Bose, and M. E. Cooper, “Glucose and blood pressure-dependent pathways–the progression of diabetic kidney disease,” International Journal of Molecular Sciences, vol. 21, no. 6. MDPI AG, Mar. 02, 2020. [CrossRef]
- J. M. Forbes and M. E. Cooper, “Mechanisms of Diabetic Complications,” Physiol Rev, vol. 93, pp. 137–188, 2013. [CrossRef]
- H. Zhao, F. Zeng, X. Wang, and L. Wang, “Prevalence, risk factors, and prognostic significance of masked hypertension in diabetic patients,” Medicine (United States), vol. 96, no. 43, Oct. 2017. [CrossRef]
- Y. Lv et al., “Association of Blood Pressure with Fasting Blood Glucose Levels in Northeast China: A Cross-Sectional Study,” Sci Rep, vol. 8, no. 1, Dec. 2018. [CrossRef]
- M. Ohishi, “Hypertension with diabetes mellitus: Physiology and pathology review-article,” Hypertension Research, vol. 41, no. 6. Nature Publishing Group, pp. 389–393, Jun. 01, 2018. [CrossRef]
- H. Osawa et al., “Diabetes and hypertension markedly increased the risk of ischemic stroke associated with high serum resistin concentration in a general Japanese population: The Hisayama Study,” Cardiovasc Diabetol, vol. 8, Nov. 2009. [CrossRef]
- J. E. Lee et al., “Insulin Resistance Is a Risk Factor for Silent Lacunar Infarction,” Stroke, vol. 47, no. 12, pp. 2938–2944, Dec. 2016. [CrossRef]
- G. Ribeiro and O. Postolache, “Sensors and Mobile Interfaces for Stress level Monitoring in People with Diabetes,” in 12th International Symposium on Advanced Topics in Electrical Engineering, ATEE 2021, Institute of Electrical and Electronics Engineers Inc., Mar. 2021. [CrossRef]
- G. Ribeiro and O. Postolache, “XXX-X-XXXX-XXXX-X/XX/$XX.00 ©20XX IEEE New Approach for Stress Assessment based on Healthcare Ecosystems.
- G. Ribeiro and O. Postolache, “New Approaches to Monitoring Respiratory Activity as Part of an Intelligent Model for Stress Assessment,” in Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), Springer Science and Business Media Deutschland GmbH, 2023, pp. 726–740. [CrossRef]
- S. Tivatansakul and M. Ohkura, “Improvement of emotional healthcare system with stress detection from ECG signal,” in Proc. 37th Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. (EMBC), Aug. 2015, pp. 6792–6795. [CrossRef]
- G. Giannakakis et al., “Stress and anxiety detection using facial cues from videos,” Biomed. Signal Process. Control, vol. 31, pp. 89–101, Jan. 2017. [CrossRef]
- Y. S. Can, N. Chalabianloo, D. Ekiz, J. Fernandez-Alvarez, G. Riva, and C. Ersoy, “Personal stress-level clustering and decision-level smoothing to enhance the performance of ambulatory stress detection with smartwatches,” IEEE Access, vol. 8, pp. 38146–38163, 2020. [CrossRef]
- M. Ciman and K. Wac, “Individuals’ stress assessment using humansmartphone interaction analysis,” IEEE Trans. Affect. Comput., vol. 9, no. 1, pp. 51–65, Jan. 2018. [CrossRef]
- Element diabetes, “Element NEO”, www.elementdiabetes.com. https://www.elementdiabetes.com/language/en-US/Os-nossos-Produtos/Gluc%C3%B3metros/Element-NEO (accessed Apr. 3, 2024).
- iHealth, “iHealth Track”, ihealthlabs.eu/en. https://ihealthlabs.eu/en/blood-pressure-monitors/33-ihealth-track-6930251800835.html (accessed Apr. 3, 2024).
- Firebase, “App Development Solutions “, firebase.google.com. ‘Use Cases’. https://firebase.google.com/solutions (accessed Apr. 3, 2024).
- Firebase, “Privacy and Security in Firebase”, firebase.google.com. https://firebase.google.com/support/privacy (accessed Apr. 3, 2024).
- Healthy Lifestyle Fitness, “What's a normal resting heart rate?”, www.mayoclinic.org. https://www.mayoclinic.org/healthy-lifestyle/fitness/expertanswers/heart-rate/faq-20057979 (accessed Apr. 3, 2024).
- EHRV, “Normative HRV Scores by Age and Gender [Heart Rate Variability Chart]”, elitehrv.com. https://elitehrv.com/normal-heart-rate-variability-age-gender (accessed Apr. 3, 2024).
- Healthline, “What Is a Normal Respiratory Rate for Adults and Children?”, www.healthline.com. https://www.healthline.com/health/normal-respiratory-rate (accessed Apr. 3, 2024).
- OnHealth, “Safe, Normal, Low Blood Oxygen Levels: Pulse Oximeter Chart”, www.onhealth.com. https://www.onhealth.com/content/1/normal_low_blood_oxygen_puls e_oximeter_levels (accessed Apr. 3, 2024).
- M. V. Villarejo, B. G. Zapirain, and A. M. Zorrilla, “A stress sensor based on galvanic skin response (GSR) controlled by ZigBee,” Sensors (Switzerland), vol. 12, no. 5, pp. 6075–6101, 2012. [CrossRef]
- J. Kuht and A. D. Farmery, “Body temperature and its regulation,” Anaesthesia and Intensive Care Medicine, vol. 19, no. 9. Elsevier Ltd, pp. 507–512, Sep. 01, 2018. [CrossRef]
- heart.org, “Understanding Blood Pressure Readings”, www.heart.org/en. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings (accessed Apr. 3, 2024).
- CMI Health, “What Your Blood Glucose Test Mean”, www.cmihealth.com. https://www.cmihealth.com/blogs/news/what-your-blood-glucose-test-results-mean-cmi-health-blog (accessed Apr. 3, 2024).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).