Preprint
Article
Low Plasma Lipids are Associated with Relapsing and Lethal Visceral Leishmaniasis in HIV-Infected Patients
Altmetrics
Downloads
92
Views
88
Comments
0
A peer-reviewed article of this preprint also exists.
supplementary.docx (102.88KB )
Submitted:
29 April 2024
Posted:
30 April 2024
You are already at the latest version
Alerts
Abstract
Visceral leishmaniasis (VL) results from infection by the protozoa Leishmania infantum and L. donovani. HIV-coinfected patients may have a relapsing course of VL, even after secondary prophylaxis with amphotericin B. This study investigated whether host factors would explain the relapses. First, susceptibility to amphotericin B of L. infantum isolates was evaluated in vitro. Then, clinical data and the lipid profile of patients with relapsing and non-relapsing VL were assessed. Susceptibility to amphotericin B was similar between the isolates. CD4+ lymphocytes were reduced in both patients in the first episode and with relapsing VL. Still, the strongest blood cell associated with relapses was low total lymphocyte counts. Total plasma cholesterol, high-density lipoprotein, low-density lipoprotein, and, uniquely, triglycerides of the six individuals in the first episode and 23 with relapsing VL were lower in relapsing patients than those in the first episode. Deceased patients had extremely low, low-density lipoprotein. After CD4+ decrease, lymphocyte CD8+ reduction seem to be the final stage of the immunological failure. The lower lipid concentrations appear to be secondary to the depletion of fat stores by inflammation-induced cachexia provoked by the co-occurrence of both diseases, which can finally lead to death.
Keywords:
Subject: Medicine and Pharmacology - Internal Medicine
1. Introduction
Visceral leishmaniasis (VL), or kala-azar, is a vector-borne disease caused by the intracellular parasites Leishmania infantum and L. donovani, transmitted by sandflies. VL is characterized by prolonged fever, pallor, wasting, hepatosplenomegaly, and pancytopenia [1]. A protracted systemic inflammation mediated by cytokines is triggered [2] and fueled by the liver acute-phase response (APR) generated by the action of IL-6 [3]. The disease kills around 10% of the patients [4]. Among those cured, some have relapses and require further treatments [5].
VL became a significant opportunistic disease of AIDS, where coinfected patients maintain low CD4+ counts. According to international guidelines, these patients are treated with a longer course of liposomal amphotericin B followed by secondary prophylaxis every two to three weeks. The response is poorer than in HIV-uninfected patients, even in cases where adherence to the antiretroviral therapy (HAART) and with undetected viral load [6]. However, only a few clinical trials have been conducted on the efficacy of drug therapy for the treatment of this immunosuppressed population [7]. VL relapse is a new episode of VL that occurs after the initial treatment, frequent in patients with AIDS. Individuals with VL and AIDS represent a challenge in clinical management because they are chronically symptomatic and have higher rates of drug toxicity, relapses, and mortality [8].
Although unusual, multiple relapses can be due to parasite resistance to amphotericin B [9]. Low drug exposure caused by inadequate dosing can explain treatment or secondary prophylaxis failure [10] . However, host factors may be responsible for therapeutic failures, such as low CD4+ cell counts before treatment, without displaying drug resistance. Lipid metabolism is another possible reason since amphotericin B is associated with lipoproteins. Additionally, total cholesterol (TC) and lipoproteins levels are significantly altered in patients with VL and AIDS, and cholesterol-rich diets modify drug concentration, toxicity, and tissue distribution of amphotericin B [11].
Therefore, as an attempt to understand the factors linked to relapses and disease severity of patients with VL co-infected with HIV, this study verifies the sensitivity to amphotericin B of L. infantum isolated from HIV-infected patients with and without relapses to rule out the possibility of drug resistance to L. infantum and then investigates the association of the plasma lipid profile and other host factors with relapses.
2. Methods
Two groups of VL patients with AIDS were retrospectively studied. One group consisted of five patients, for testing amphotericin B sensitivity. Frozen stored isolates of L. infantum from four patients in their second VL episode and one from the patients in the first VL episode were tested drug sensitivity. The other group was composed by 29 patients, divided in two sub-groups. Twenty-three had relapsing VL and six were in the first episode of the disease; their medical records and lipid profile were analyzed. All were hospitalized at a reference hospital in two subgroups. Teresina, Brazil, where they were treated for VL with liposomal amphotericin B at a dose of 3mg/kg daily for two weeks. Besides treatment, patients received secondary prophylaxis for VL with liposomal amphotericin B at a dose of 3mg/kg biweekly and HAART. The patient information available spans from May 2014 to August 2020. All patients with reagent serology for HIV, with clinical signs of VL, and with a diagnosis of VL confirmed by parasitological methods were included.
L. infantum isolates were thawed and transferred to NNN medium (Novy, MacNeal, Nicolle) with Schneider's medium supplemented with heat-inactivated sterile fetal bovine serum (Gibco®), penicillin, and human urine. The samples were transferred and kept in a BOD incubator at 26 °C. For the in vitro assay with amphotericin B, M199 medium (Sigma-Aldrich, St. Louis, MO, USA) at 25 °C, supplemented with 10% heat-inactivated fetal calf serum (FCS) and 0.25% hemin was used. Amphotericin B and MTT (3-(4,5-dimethyl thiazol-2-yl) - 2,5 diphenyl tetrazolium bromide) were acquired from Sigma-Aldrich (St. Louis, MO, USA). The MTT test was performed according to Zauli-Nascimento et al. [12]. All experiments included a reference strain of L. infantum (MHOM/BR/2005/NLC) as a control. The lipid levels were compared to the cumulative number of liposomal amphotericin B doses used. For this analysis, each 50 mg vial of the drug was the unit of analysis.
Lipid fractions were analyzed from plasma samples stored at -20 °C. They were processed with the Incca Bit Analisa equipment (Belo Horizonte, Brazil). The Analisa reagent kit (Belo Horizonte, Brazil) for TC, triglycerides (TG), and direct (high-density lipoprotein (HDL) was used. Low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL) values were obtained from Fridewald's formula (VLDL=TG/5; LDL= TC-HDL-VLDL).
For data analysis of the in vitro assay, the EC50 values were expressed as mean and standard error (SEM), produced by GraphPad Prism 7.04 software. For human data analysis, the usual procedures of descriptive statistics were used. The Shapiro-Wilk test was used to check whether the data followed a normal distribution. For continuous and category variables, the Student's t-test and Fisher's exact test were performed. Pearson's and Spearman's correlation tests were used according to the data distribution. Data were tabulated and analyzed with the software Stata™, College Station, TX.
3. Results
Among the five patients from whom parasites were available to analyze the sensitivity to amphotericin B, three were males and two females, aged 38 to 55. Four isolates were taken from patients during a relapsing episode of VL, and one was isolated from a patient during the initial symptomatic phase. All had AIDS. The four patients with relapsing VL were on secondary amphotericin B prophylaxis, each one with two previous relapses.
The amphotericin B EC50 for promastigotes of the five isolates obtained is shown in Table 1. All were below the EC50 of the reference isolate MHOM/BR/2005/NLC (0.051µM). The minimum value was 0.024 µM, and the maximum was 0.042 µM. No significant differences were observed between the mean EC50 of the isolates.
Next, lipid profile of the six patients in the first episode of VL and the 23 under ongoing secondary prophylaxis was evaluated. Their general characteristics are showed in Table 2. Most were men over 40 years old. Treatment for VL was performed with liposomal amphotericin B. However, two had been previously treated with amphotericin B deoxycholate. The most frequent clinical manifestations were weight loss, pallor, fever, and hepatosplenomegaly. Clinical manifestations of relapsing and non-relapsing episodes observed at admission were similar, except for the fever, which was less common in relapsing episodes (p-value = 0.046). Complete adherence HAART was observed in 21/29 (75.9%), all with relapses. All patients who died had relapses (13.8%, p-value = 0.55). Death occurred from nine to 69 months after the samples were collected.
Table 3 shows the laboratory data of those six patients at the first episode of VL and of those 23 with a relapsing progression. Among the total 29 participants, 23 (95.8%) had low hemoglobin. The leukocyte count was low in 20 participants (74.1%), and, like neutrophils, they were lower among those with relapses (p-value = 0.025 and 0.076, respectively). Relapsing patients had much lower lymphocytes (660/mm3 vs. 1,664/ mm3, p-value = 0.005). Thrombocytopenia was seen in 12 individuals (44.5%). There was marked hypoalbuminemia and hyperglobulinemia. CD4+ cell count was low in all patients and was not statistically distinct between relapses and the first episode (142 cells/mm3 vs. 152 cells/mm3), varying from 5 cells/mm3 to 406 cells/mm3. Only three patients had a CD4+ count above 200 cells/mm3; one was in the first episode, and two had a relapsing course. Mean CD8+ cells were lower in relapsing patients (606 cells/mm3) than in those at the first-time VL episode (955 cells/mm3), but the difference was not statistically significant (p-value = 0.222). Total lymphocytes were highly correlated with CD8+ (r = 0.69, p-value = 0.003) but not with CD4+ cells. All patients in the first episode had detectable viral load.
Supplemental table shows the low concentrations of all types of lipids evaluated. The two groups of participants had mean TC much lower than the suggested threshold of 190 mg/dL, and all showed TG values below the recommended level. LDL was also much inferior to the 130 mg/dL cut-off in all patients. Twenty (68.9%) participants had HDL values below the 40 mg/dL threshold. There was no correlation between lipid levels and the cumulative number of liposomal amphotericin B doses used.
The lipid profile of the individuals with AIDS who had VL with a relapsing course and those in their first episode are shown in Figure 1. Total cholesterol was 93.2 mg/dL at the first episode and 60.2 mg/dL during a relapse (p-value = 0.005). The other lipids were also lower during relapses: HDL (44.7 vs. 30.5), LDL (28.1 vs. 14.8), VLDL (20.4 vs. 14.9), and TG (102.0 vs 73.2), all with p-value < 0.05.
The lipid profile according to mortality is shown in Table 4. Impressively, the individuals who died had much lower LDL values than the survivors (3.6 mg/dL vs. 20.4 mg/dL, p = 0.038). They were two women and two men, in the range of 41 to 59 years of age; two underwent splenectomy as a salvage approach. The two not splenectomized died of Pneumocystis jirovecii pneumonia, and the two splenectomized died apparently of sepsis and portal thrombosis. The two with available HIV load measurements had 2.8 x 105 viral RNA copies/mL and the other 4.4 x 103 copies/mL. Their LDL were 0.4 mg/dL, 1.4 mg/dL, 2.0 mg/dL and 10.4 mg/dL. No statistically significant associations with death were observed regarding TC, TG, and any other blood test.
4. Discussion
Amphotericin B is an essential drug for treating VL due to the development of drug resistance to other medications. However, in vitro resistance to amphotericin B is unusual [13]. Yet, the rescue of amphotericin B treatment with pentavalent antimonial has been previously described [14]. Here, the in vitro assay did not detect in vitro resistance, confirming previous findings [15]. The susceptibility assay was performed against promastigotes of the different isolates since it has been shown that there is a strong correlation of drug susceptibility between promastigotes and amastigotes of a given strain of Leishmania [16]. Moreover, the EC50 of isolates of L. infantum obtained prior to and after treatment with amphotericin B showed that the EC50 values were similar [17]. Therefore, the present findings indicated that treatment failure observed in the patients with relapsing VL and AIDS seems not to be due to drug parasite resistance.
The study population, comprising adult individuals with VL and AIDS, reflects the overall characteristics of preceding studies [18] but the observed mortality was higher than the mortality described for the non-HIV-infected patients [19]. The most frequent clinical manifestations were similar to those of patients without HIV. However, fever was absent in nearly half of those with a relapsing course but present in all at the first episode of VL. Therefore, the fever mediators IL-1b, TNF-a, and IL-6 seem not to play the same intense role in the pathogenesis of the relapsing course as in the first episode. Accordingly, it has been shown that Il-6-driven C-reactive protein, a marker of the APR, is very high during the first episode of VL [20]. Hypoalbuminemia and hyperglobulinemia, also markers of APR, were impressively, respectively, low and high in a patient in the first episode but not so much in patients with a relapsing evolution.
Lower mean lymphocyte CD4+ count is the primary marker of VL relapse among AIDS patients [6]. However, in this study, the distinction of relapsing patients from patients in the first episode was not, though the CD4+ cells fall, but the CD8+ reduction, since CD4+ cells were already low in both groups [20,21]. Indeed, CD8+ cells fall have been noticed even in VL non-coinfected patients with HIV [22]. Accordingly, as at the first episode of VL, CD4+ count was already low, the data suggests that CD4+ depletion antecedes CD8+ loss, denoting a two-step process in which CD4+ reduction is initially dependent on HIV infection, allowing L. infantum proliferation and worsening inflammation, and finally leading to CD8+ loss and reduced function, increasing immunosuppression, and easing future relapses. The mechanisms for total lymphocyte depletion in coinfected patients seem to involve continued systemic inflammation, thymic involution, reduced thymic output, chronic immune activation, increased lymphocyte apoptosis, T-cell exhaustion and other subtle mechanisms [20,23]. In any way, recombinant IL-7, a growth factor for the progenitor lymphoid cells, might be tried to rescue relapsing VL patients with AIDS as it has been tried for patients with sepsis [24].
Since liposomal amphotericin B is the formulation of choice for the treatment and secondary prophylaxis of VL in patients with AIDS and interacts with serum lipoproteins in vitro and in the rabbit model, influencing the drug tissue concentration [11], the hypothesis that human lipids might be involved with liposomal amphotericin B activity against Leishmania was investigated. All measured lipids were low in patients with AIDS and VL, regardless of whether they relapsed [25]. This profile is distinct from those of patients with VL or AIDS, taken separately. In VL only, TC, HDL, and LDL, are low. At the same time, VLDL and TG are higher than the controls or the recommended cut-offs [26]. The same profile is seen in patients with HIV infection and with AIDS, not under HAART [27]. After the arrival of HAART, this profile changed, according to the effects of the antiretroviral drugs [28]. Therefore, TG and, at a certain point, VLDL highlight a distinct lipid metabolism of patients with VL and AIDS together, in contrast to those with only one of the two conditions. The association between TC, LDL, HDL, VLDL, and TG with relapsing evolution suggests that the lipid profile should be investigated as a biomarker of VL relapse in cohort studies.
Two other critical points are common to VL and AIDS: inflammation and cachexia. Indeed, patients with VL have elevated markers of APR [3] , as well as patients with HIV or AIDS [29]. VL leads to cachexia [30] as well as AIDS [31] and, especially, both diseases simultaneously [20]. Patients with APR, like in sepsis and trauma, also have low TC, HDL, and LDL, usually with high TG [32,33]. Protein-energy malnutrition shows a trend for low TG and other lipids as it is observed in VL patients with AIDS: low TC, HDL, LDL, and also low TG [34,35,36]. This picture suggests that a possible mechanism for the lipid profile seen in VL and AIDS, with all measured lipids at a lower concentration, including TG, is VL- and AIDS-driven prolonged inflammation leading to cachexia, promoting lipolysis and mobilization of TG and cholesterol esters from plasma and adipose tissues to hepatocytes. This profile also suggests a two-step process, which initially conducts to progressive depletion of fat stores and lately reduces lipid recycling and availability for liver metabolism and synthesis of TC, TG, VLDL, and LDL [37] in a process that could be coined as fat metabolism exhaustion. Further investigations are required to confirm the finding of fat exhaustion in other protracted diseases with cachexia and inflammation.
An unexpected and intriguing discovery is the association of extremely low LDL with four late deaths of patients with relapsing VL and AIDS. This finding contradicts a recent review concluding that very low levels of LDL are not risky for the general population [38], although other authors found an increased risk of ischemic hemorrhagic stroke and death [39]. Moreover, a meta-analysis showed that mortality by sepsis was associated with lower TC, HDL, and LDL, albeit not with TG levels [40]. Hence, it is of interest the idea that fat exhaustion led to severe unavailability of lipids to synthesize vital lipid compounds for vitamin transport, cell membranes, the central nervous system, and steroid hormones [32]. However, the causal association of low LDL with death persists disputed, and the precise mechanisms of how low LDL would be related to death remain elusive.
The data showed that the lipid profile did not influence the action of amphotericin B on the relapsing course of VL in AIDS patients. First, the only causal relationship investigated through time, e.g., the amount of liposomal amphotericin accumulated, was not associated with any component of the lipid profile. Secondly, an experimental study with rabbits using liposomal amphotericin B [11] suggested that the higher the ingestion of cholesterol and the more TC and LDL were, the least toxic liposomal amphotericin B was, and the minor concentration of amphotericin B in the spleen was reached. Hence, as we found very low values of all lipids investigated, the hypothesis of high lipids reducing the effectiveness of amphotericin B can be ruled out. Unfortunately, amphotericin B concentration was not evaluated here. Therefore, it may be concluded that low CD4+ and, lately, CD8+ cells and low lipids were the main host factors for relapses of VL in patients with HIV.
The main study limitations are the small sample size, the retrospective and cross-sectional design. Therefore, type 2 errors may have hidden associations, as for CD8+, with the course of relapsing VL. Since the cases of the first VL episode may have been a mix with future relapsing cases, other associations may have been missed. Finally, the cross-sectional approach hindered the detection of cause-effect relationships, limited to reasonings based on the data and literature.
In the end, however, the study reveals that resistance to amphotericin B or lipid interference on its activity are not the reasons for relapsing VL in patients with AIDS. Lymphopenia due to low CD4+ added by subsequent fall of CD8+ may be the late immunological factor involved with relapses. The lipid profile of low TC, HDL, LDL, and TG may also be markers of relapses, and lipid exhaustion with extremely low LDL may indicate a higher probability of death. Studies on using cholesterol-rich diets for those with very low LD, the control of Leishmania and inflammation, recombinant IL-7, and immune checkpoint inhibitors for relapsing VL should be conducted. Finally, the association of a two-step chronic inflammation caused by the two diseases leading first to CD4+ depletion followed by CD8+ fall with progressive depletion of lipids, leading to late fat exhaustion may be intimately linked, and deserves further investigation in AIDS and its coinfections, especially those with a relapsing course such as VL.
Authors’ contribution
Conceptualization, R.V.S.S. and C.H.N.C.; Methodology, S.R.B.U., J.K.U.Y.Y., C.S.V., E.S., M.M.L.F., V.S.C.; Formal Analysis, R.V.S.S., S.R.B.U., and C.H.N.C.; Investigation, R.V.S.S, S.R.B.U., C.H.N.C; Resources, S.R.B.U., C.H.N.C.; Data Curation, R.V.S.S and C.H.N.C.; Writing – Original Draft Preparation, R.V.S.S. S.R.B.U., and C.H.N.C.; Writing – Review & Editing, R.V.S.S., D.L.C., and C.H.N.C.; Visualization, R.V.S.S. and C.H.N.C.; Supervision, S.R.B.U., C.H.N.C.; Project Administration, C.H.N.C.; Funding Acquisition, C.H.N.C.
Institutional Review Board Statement
This study was approved by the Research Ethics Committee of the Federal University of Piauí (Number 3.276.499).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Financial support
Coordination for the Improvement of Higher Education Personnel (CAPES) for the Masters scholarship for RVSS, National Council for Scientific and Technological Development (CNPq) Process Number 302571/2015-9 for CHNC, and the Institute of Tropical Diseases “Natan Portella” for the analysis of the lipid profile.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledgments
The authors are grateful to the Institute of Tropical Diseases “Natan Portella”, which provided all support for data collection.
References
- Burza S, Croft SL, Boelaert M. Leishmaniasis. Lancet 2018; 392: 951–970.
- Costa DL, Rocha RL, Carvalho RMA; et al. Serum cytokines associated with severity and complications of kala-azar. Pathog Glob Health 2013; 107: 78–87. [CrossRef]
- Wasunna KMM, Raynes JGG, Were JBOB; et al. Acute phase protein concentrations predict parasite clearance rate during therapy for visceral leishmaniasis. Trans R Soc Trop Med Hyg 1995; 89: 678–681. [CrossRef]
- Alvar J, Vélez ID, Bern C; et al. Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS ONE 2012; 7: e35671. [CrossRef]
- Reinaldo LGC, Araújo-Júnior RJC, Diniz TM; et al. Splenectomy in Patients with Visceral Leishmaniasis Resistant to Conventional Therapy and Secondary Prophylaxis: A Retrospective Cohort. Am J Trop Med Hyg; in press. Epub ahead of print 20 June 2022. [CrossRef]
- Cota GF, de Sousa MR, Rabello A. Predictors of Visceral Leishmaniasis Relapse in HIV-Infected Patients: A Systematic Review. PLoS Negl Trop Dis 2011; 5: e1153. [CrossRef]
- World Health Organization & Cochrane Response. WHO guideline for the treatment of visceral leishmaniasis in HIV coinfected patients in East Africa and South-East Asia: Web annex A: A systematic review on the treatment of visceral leishmaniasis in HIV-Leishmania coinfected persons in East Africa and So. https://apps.who.int/iris/handle/10665/354546. Licença: CC BY-NC-SA 3.0 IGO. (2022).
- Doitsh G, Greene WC. Dissecting How CD4 T Cells Are Lost During HIV Infection. Cell Host Microbe 2016; 19: 280–291. [CrossRef]
- Srivastava P, Prajapati VK, Rai M; et al. Unusual Case of Resistance to Amphotericin B in Visceral Leishmaniasis in a Region in India Where Leishmaniasis Is Not Endemic. J Clin Microbiol 2011; 49: 3088–3091. [CrossRef]
- Kip AE, Blesson S, Alves F; et al. Low antileishmanial drug exposure in HIV-positive visceral leishmaniasis patients on antiretrovirals: An Ethiopian cohort study. J Antimicrob Chemother 2021; 76: 1258–1268. [CrossRef]
- Wasan KM, Kennedy AL, Cassidy SM; et al. Pharmacokinetics, Distribution in Serum Lipoproteins and Tissues, and Renal Toxicities of Amphotericin B and Amphotericin B Lipid Complex in a Hypercholesterolemic Rabbit Model: Single-Dose Studies. Antimicrob Agents Chemother 1998; 42: 3146–3152. [CrossRef]
- Zauli-Nascimento RC, Miguel DC, Yokoyama-Yasunaka JKU; et al. In vitro sensitivity of Leishmania ( Viannia ) braziliensis and Leishmania ( Leishmania ) amazonensis Brazilian isolates to meglumine antimoniate and amphotericin B. Trop Med Int Heal. Epub ahead of print October 2009. [CrossRef]
- Rastrojo A, García-Hernández R, Vargas P; et al. Genomic and transcriptomic alterations in Leishmania donovani lines experimentally resistant to antileishmanial drugs. Int J Parasitol Drugs Drug Resist 2018; 8: 246–264. [CrossRef]
- Morizot G, Jouffroy R, Faye A; et al. Antimony to Cure Visceral Leishmaniasis Unresponsive to Liposomal Amphotericin B. PLoS Negl Trop Dis 2016; 10: e0004304. [CrossRef]
- Ponte-Sucre A, Gamarro F, Dujardin J-C; et al. Drug resistance and treatment failure in leishmaniasis: A 21st century challenge. PLoS Negl Trop Dis 2017; 11: e0006052. [CrossRef]
- Lachaud L, Bourgeois N, Plourde M; et al. Parasite Susceptibility to Amphotericin B in Failures of Treatment for Visceral Leishmaniasis in Patients Coinfected with HIV Type 1 and Leishmania infantum. Clin Infect Dis 2009; 48: e16–e22. [CrossRef]
- Durand R, Paul M, Pratlong F; et al. Leishmania infantum : Lack of Parasite Resistance to Amphotericin B in a Clinically Resistant Visceral Leishmaniasis. Antimicrob Agents Chemother 1998; 42: 2141–2143. [CrossRef]
- Cota GF, de Sousa MR, de Assis TSM; et al. Exploring prognosis in chronic relapsing visceral leishmaniasis among HIV-infected patients: Circulating Leishmania DNA. Acta Trop 2017; 172: 186–191.
- Costa DLDL, Rocha RLRLRL, Chaves E de BF; et al. Predicting death from kala-azar: Construction, development, and validation of a score set and accompanying software. Rev Soc Bras Med Trop 2016; 49: 728–740.
- Takele Y, Mulaw T, Adem E; et al. Immunological factors, but not clinical features, predict visceral leishmaniasis relapse in patients co-infected with HIV. Cell Reports Med 2022; 3: 100487. [CrossRef]
- Silva-Freitas ML, Cota GF, Machado-de-Assis TS; et al. Immune Activation and Bacterial Translocation: A Link between Impaired Immune Recovery and Frequent Visceral Leishmaniasis Relapses in HIV-Infected Patients. PLoS ONE 2016; 11: e0167512. [CrossRef]
- Gautam S, Kumar R, Singh N; et al. CD8 T Cell Exhaustion in Human Visceral Leishmaniasis. J Infect Dis 2014; 209: 290–299. [CrossRef]
- Silva-Freitas ML, Corrêa-Castro G, Cota GF; et al. Impaired Thymic Output Can Be Related to the Low Immune Reconstitution and T Cell Repertoire Disturbances in Relapsing Visceral Leishmaniasis Associated HIV/AIDS Patients. Front Immunol; 11. Epub ahead of print 20 May 2020. [CrossRef]
- Francois B, Jeannet R, Daix T; et al. Interleukin-7 restores lymphocytes in septic shock: The IRIS-7 randomized clinical trial. JCI Insight; 3. Epub ahead of print 8 March 2018. [CrossRef]
- Szwarcwald CL, Malta DC, Pereira CA; et al. Valores de referência para exames laboratoriais de colesterol, hemoglobina glicosilada e creatinina da população adulta brasileira. Rev Bras Epidemiol; 22. Epub ahead of print 2019. [CrossRef]
- Lal CS, Kumar A, Kumar S; et al. Hypocholesterolemia and increased triglyceride in pediatric visceral leishmaniasis. Clin Chim Acta 2007; 382: 151–153. [CrossRef]
- Grunfeld C, Pang M, Doerrler W; et al. Lipids, lipoproteins, triglyceride clearance, and cytokines in human immunodeficiency virus infection and the acquired immunodeficiency syndrome. J Clin Endocrinol Metab 1992; 74: 1045–1052. [CrossRef]
- Souza SJ, Luzia LA, Santos SS; et al. Lipid profile of HIV-infected patients in relation to antiretroviral therapy: A review. Rev Assoc Med Bras 2013; 59: 186–198. [CrossRef]
- Wallet MA, Buford TW, Joseph A-M; et al. Increased inflammation but similar physical composition and function in older-aged, HIV-1 infected subjects. BMC Immunol 2015; 16: 43. [CrossRef]
- Harhay MOMO, Olliaro PLPL, Vaillant M; et al. Who Is a Typical Patient with Visceral Leishmaniasis? Characterizing the Demographic and Nutritional Profile of Patients in Brazil, East Africa, and South Asia. Am J Trop Med Hyg 2011; 84: 543–550. [CrossRef]
- Grinspoon S, Mulligan K. Weight Loss and Wasting in Patients Infected with Human Immunodeficiency Virus. Clin Infect Dis 2003; 36: S69–S78. [CrossRef]
- Carpentier YA, Scruel O. Changes in the concentration and composition of plasma lipoproteins during the acute phase response. Curr Opin Clin Nutr Metab Care 2002; 5: 153–158. [CrossRef]
- Feingold KR, Grunfeld C. The Effect of Inflammation and Infection on Lipids and Lipoproteins. Epub ahead of print 2000. DOI: 26561701.
- Veiga GRS, Ferreira HS, Sawaya AL; et al. Dyslipidaemia and Undernutrition in Children from Impoverished Areas of Maceió, State of Alagoas, Brazil. Int J Environ Res Public Health 2010; 7: 4139–4151. [CrossRef]
- Verma DGK, Yadav DYS, Yadav DRK; et al. Study of lipid profile levels in malnourished and healthy children: A case control study acquired pneumonia in children. Pediatr Rev Int J Pediatr Res 2018; 5: 156–161.
- Zhang Z, Pereira S, Luo M; et al. Evaluation of Blood Biomarkers Associated with Risk of Malnutrition in Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2017; 9: 829. [CrossRef]
- Stellaard F. From Dietary Cholesterol to Blood Cholesterol, Physiological Lipid Fluxes, and Cholesterol Homeostasis. Nutrients 2022; 14: 1643. [CrossRef]
- Olsson AG, Angelin B, Assmann G; et al. Can cholesterol be too low? Possible risks of extremely low levels. J Intern Med 2017; 281: 534–553. [CrossRef]
- Wu Z, Huang Z, Lichtenstein AH; et al. The risk of ischemic stroke and hemorrhagic stroke in Chinese adults with low-density lipoprotein cholesterol concentrations < 70 mg/dL. BMC Med 2021; 19: 142. [CrossRef]
- Hofmaenner DA, Arina P, Kleyman A; et al. Association Between Hypocholesterolemia and Mortality in Critically Ill Patients With Sepsis: A Systematic Review and Meta-Analysis. Crit Care Explor 2023; 5: e0860. [CrossRef]
Figure 1.
Mean plasma concentration and standard deviation of total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), very low-density (VLDL), and triglycerides (TG) of patients with HIV at the first episode of and with a relapsing course of visceral leishmaniasis. All differences were statistically significant (p-value < 0.05).
Figure 1.
Mean plasma concentration and standard deviation of total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), very low-density (VLDL), and triglycerides (TG) of patients with HIV at the first episode of and with a relapsing course of visceral leishmaniasis. All differences were statistically significant (p-value < 0.05).
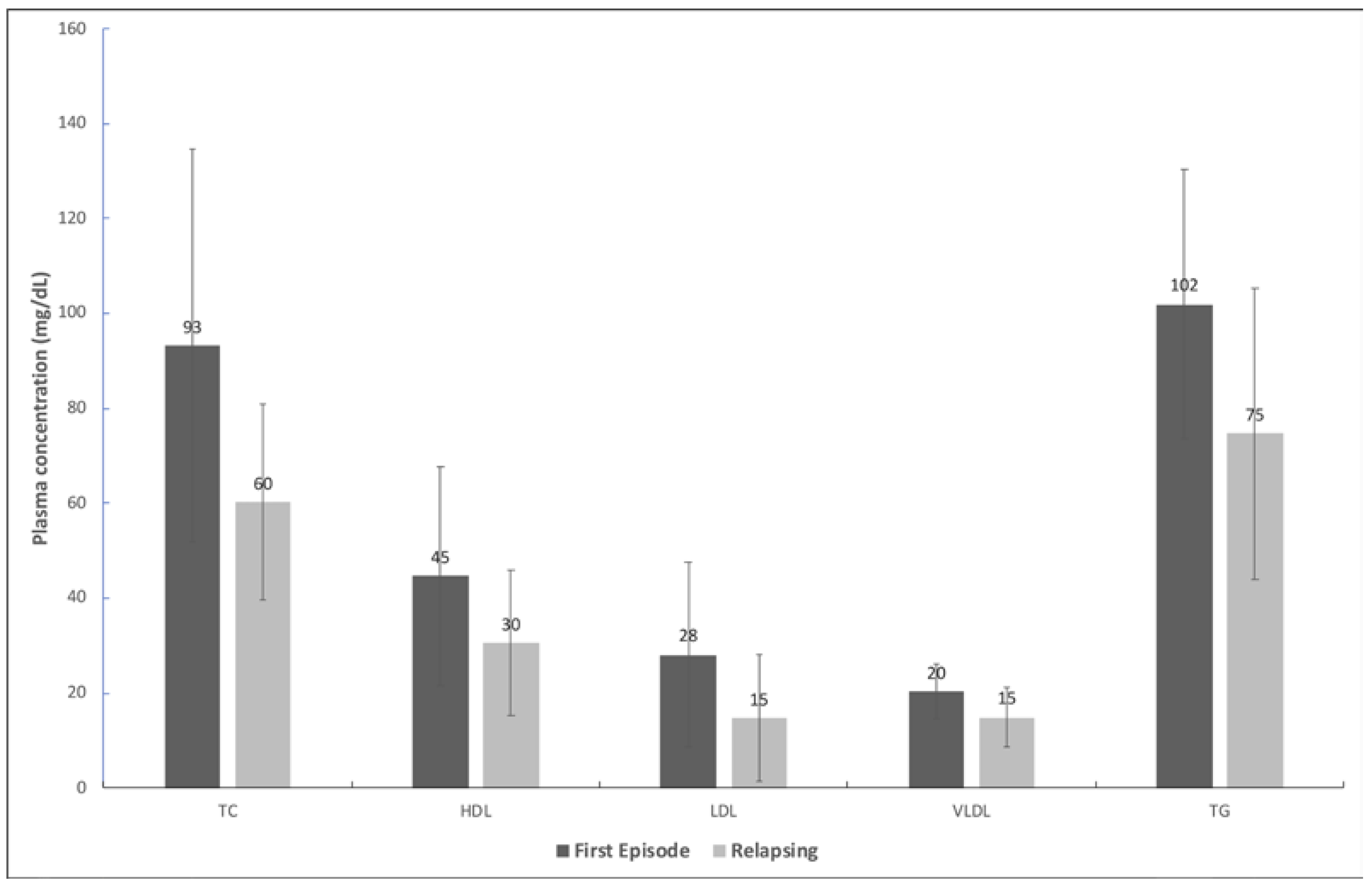
Table 1.
EC50¹ values of promastigotes from isolates taken from individuals with visceral leishmaniasis coinfected with HIV and of promastigotes of a reference strain.
Table 1.
EC50¹ values of promastigotes from isolates taken from individuals with visceral leishmaniasis coinfected with HIV and of promastigotes of a reference strain.
| Patient ID | Mean EC50¹ | Standard error | No. of experiments | No. of previous VL episodes |
| (µM) | (µM) | |||
| 55672 | 0.042 | 0.007 | 5 | 2 |
| 57682 | 0.037 | 0.006 | 5 | 2 |
| 69052 | 0.034 | 0.007 | 4 | 2 |
| 70532 | 0.024 | 0.008 | 5 | 2 |
| 56093 | 0.026 | 0.006 | 4 | 0 |
| MHOM/BR/2005/NLC4 | 0.051 | 0.005 | 3 | - |
¹Half-maximal effective concentration. 2The promastigotes used in the experiment were isolated from patients who were in second episode of visceral leishmaniasis.3The isolate used in the experiment was taken from a patient in the first episode of visceral leishmaniasis. 4Reference isolate.
Table 2.
Demographic and clinical characteristics of individuals with visceral leishmaniasis infected with HIV.
Table 2.
Demographic and clinical characteristics of individuals with visceral leishmaniasis infected with HIV.
| Characteristics | First episode n (%) |
Relapsing n (%) |
p-value |
|---|---|---|---|
| Sex | |||
| Male | 6 (100.0) | 20 (87.0) | |
| Female | 0 (0.0) | 3 (13.0) | 0.350 |
| Age-group | |||
| Up to 40 years old | 4 (66.7) | 8 (34.8) | |
| More than 40 years | 2 (33.3) | 15 (65.2) | 0.158 |
| Symptoms and signs | |||
| Weight loss | 6 (100.0) | 17 (73.4) | 0.160 |
| Pallor | 5 (83.3) | 17 (73.4) | 0.631 |
| Fever | 6 (100.0) | 13 (56.5) | 0.046 |
| Asthenia/weakness | 4 (66.7) | 14 (60.9) | 0.794 |
| Splenomegaly | 3 (50.0) | 13 (56.5) | 0.775 |
| Hepatomegaly | 2 (33.3) | 9 (39.1) | 0.794 |
| Jaundice | 2 (33.3) | 8 (34.8) | 0.947 |
| HAART* | 6/6 (100.0) | 15/23 (0.65) | 0.43 |
| Death | 0 (0.0) | 4 (17.4) | 0.55 |
* Highly-active antiretroviral therapy.
Table 3.
Laboratory data of individuals with visceral leishmaniasis infected with HIV, according to the course of VL (relapsing and first episode).
Table 3.
Laboratory data of individuals with visceral leishmaniasis infected with HIV, according to the course of VL (relapsing and first episode).
| Laboratory data | Course of VL | p-valuec | |||
| First episode (N=6) | Relapsing (N=23) | ||||
| na | Mean (95% CIb) | na | Mean (95% CI) | ||
| Hemoglobin (g/dL) | 5 | 8.0 (3.6; 12.5) |
19 | 7.8 (7.2; 8.4) |
0.522 |
| Leukocytes (per mm³) | 5 | 4.643 (1,060; 4; 8.223) |
21 | 2.397 (1,713; 3.083) |
0.013 |
| Neutrophils (cells/mm³) | 5 | 2,410 (-272; 5092.9) |
19 | 1,409 (889; 1930) |
0.076 |
| Lymphocytes (cells /mm³) | 5 | 1,654 (-88; 3,396) |
19 | 660 (457; 864) |
0.005 |
| Platelets (number/mm³) |
6 | 151,952 (151,952;184,813) |
21 | 190,217 (89.298; 291,135) |
0.297 |
| Albumin (g/dL) | 1 | 1.8 | 10 | 2.7 (1.9; 3.6) |
- |
| Globulin (g/dL) | 1 | 9.9 | 9 | 6.0 (4.8;7.2) |
- |
| CD4+ (cells/mm³) | 5 | 152 (-32; 332) |
15 | 142 (89; 196) |
0.877 |
| CD8+ (cells/mm³) | 5 | 955 (-197.4; 2,106.55) |
14 | 606 (423; 789) |
0.222 |
aNumber of patients with the information available; b95% Confidence interval.; cStudent's t-test.
Table 4.
Association between the lipid profile and the clinical outcome of individuals with visceral leishmaniasis coinfected with HIV according to survival and death.
Table 4.
Association between the lipid profile and the clinical outcome of individuals with visceral leishmaniasis coinfected with HIV according to survival and death.
| Lipid profile | Outcome |
p-value |
|
| Survival (na=25) Mean (95% CIb) |
Death (n=4) Mean (95% CI) |
||
| TCc (mg/dL) | 68.3 (56.1; 80.5) | 60.7 (20.8; 100.7) | 0.633 |
| LDLd (mg/dL) | 20.4 (14.2; 26.7) | 3.6 (-3.8; 10.9) | 0.038 |
| HDLe (mg/dL) | 32.7 (25.3; 40.2) | 37.3 (8.6; 65.9) | 0.644 |
| VLDLf (mg/dL) | 15.2 (12.7; 17.6) | 20.0 (5.7; 34.2) | 0.170 |
| TGg (mg/dL) | 75.8 (63.7; 88.0) | 99.8 (28.4; 171.1) | 0.170 |
aNumber of individuals. b95% confidence interval. cTotal cholesterol. dLow-density lipoprotein. eHigh-density lipoprotein. fVery low-density lipoprotein. gTriglycerides.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated







