4. Discussion
In recent years, the scientific community has shown an increased interest in the phenomenon of dehumanization, which has extensively been examined in the field of social psychology. This is highlighted in multiple recent studies such as those by Haslam et al. (2014, 2016) [
1,
21,
22,
23,
24,
25,
26]. It is well known that healthcare professionals, and especially doctors and nurses, frequently have to face this particularly difficult task. Since health science is a human-centered profession, this dynamic scientific field requires that professionals show a lot of passion and love, to face challenges both psychologically and physically and maintain their integrity over time.
However, dehumanization does not always come from immoral behavior or social rejection. Everyday dehumanization is likely to be unintentional, arising from a variety of factors usually related to structural and organizational aspects of health care [
9,
26,
27]. Unfortunately, multiple difficulties in public hospitals - workplaces, the nature of the profession, as well as the lack of staff and motivation, increase physical and psychological fatigue, which easily leads to real burnout [
9]. We would add that elements of personality, empathy, technology, and the external pressures of everyday life are factors contributing to this behavior among professionals. In this context, dehumanization is a complex psychological defense that ironically helps healthcare providers cope with and survive multiple unpleasant and debilitating personal and professional conditions [
10]. Therefore, it is an emotional regulation strategy used by health care professionals [
9], as it mentally gives them a shield, to alleviate the anxiety and feelings of guilt that may arise from causing pain [
8,
28]. Furthermore, an empirical study of the effect of dehumanization in the era of computerized information was done through Amazon Mechanical Turkish. The results showed that there appears to be a negative effect of the computer on the doctor-patient relationship and the resulting patient care [
29].
The result of all the above observations indicates that in medical environments, multiple behavioral events offend the dignity of patients. Some healthcare professionals use inappropriate communication styles, using baby talk when speaking to elders, while others display various forms of aggressive behavior when interacting with the mentally ill [30, 31, 32].
The main objective of this study was to develop and validate measures for the assessment of both types of dehumanization, namely animalistic and mechanistic dehumanization in the field of healthcare, where dehumanization is a rampant phenomenon [
2,
11]. To the best of our knowledge, there was a lack of validated instruments for measuring dehumanization among healthcare professionals in Greece but also globally, a gap that this research aims to fill. In fact, the lack of validated instruments can lead to under-investigation of the phenomena and research initiatives suspension [
33]. Utilizing the developed questionnaires in our research, both for dehumanization and self-dehumanization will enable researchers to systematically investigate and establish correlations between this phenomenon and other variables, thereby bridging gaps in the existing literature. Also, the thoughtful evaluation of the dehumanization phenomenon can deepen health professionals' understanding of its complexities and guide focused interventions.
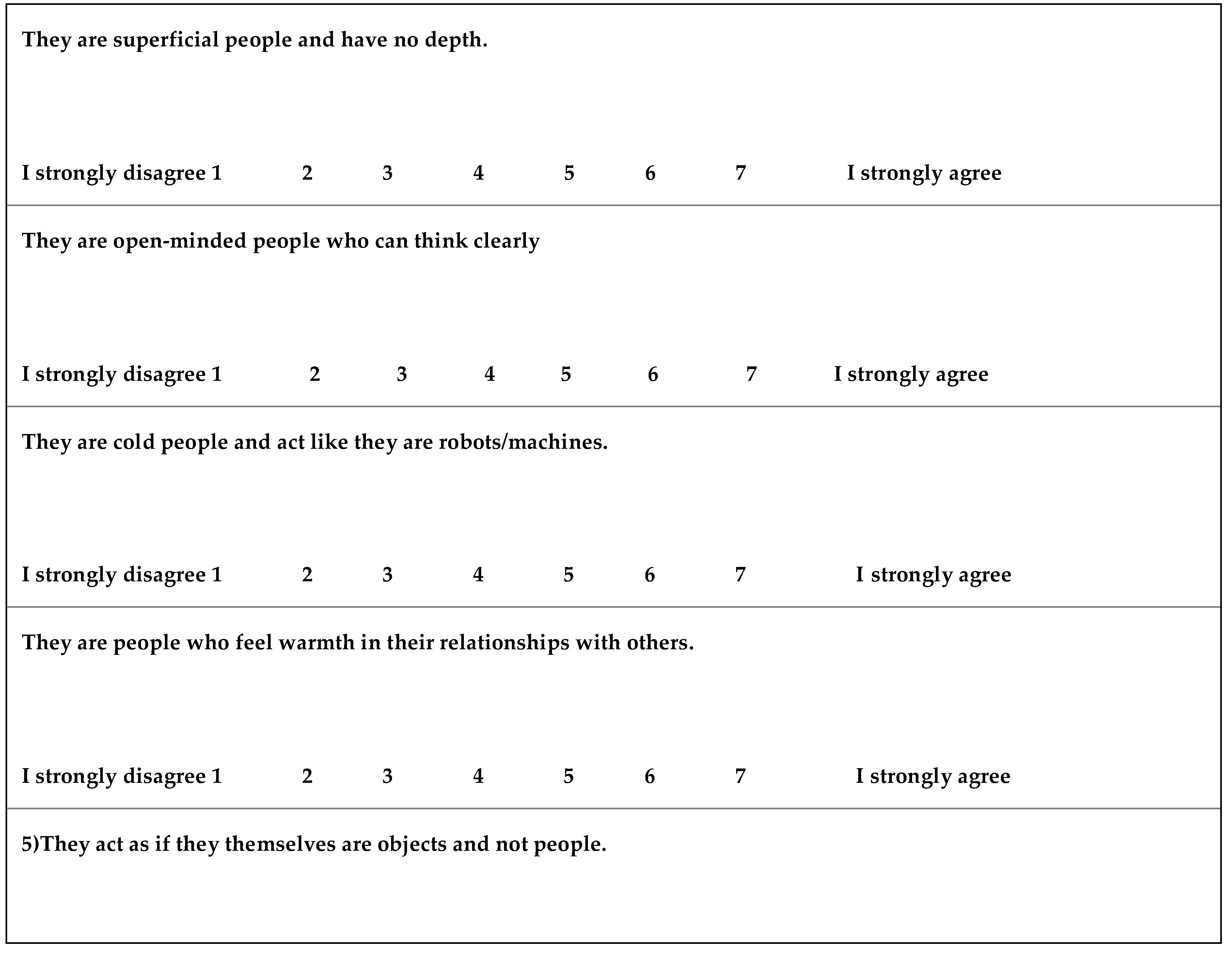
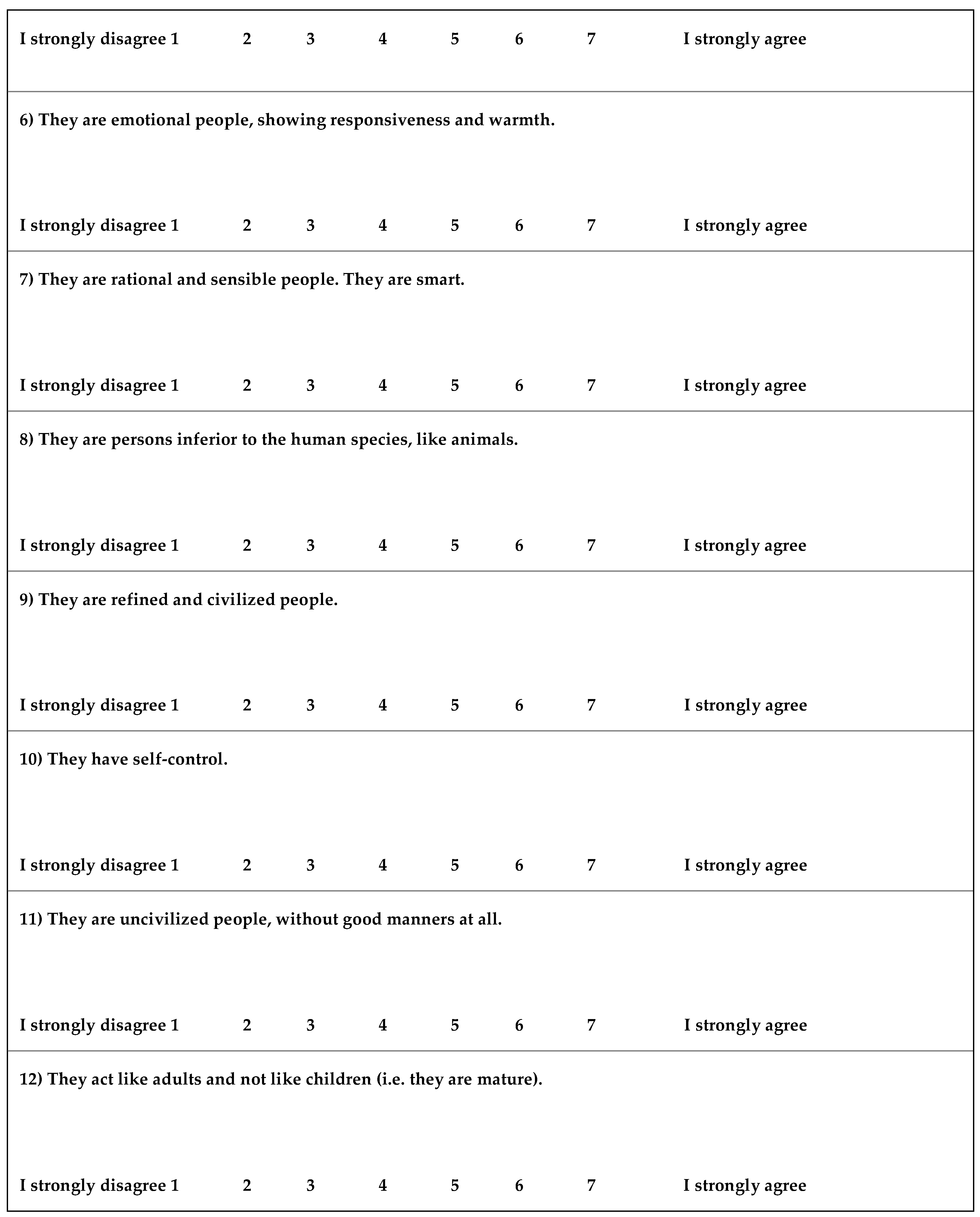
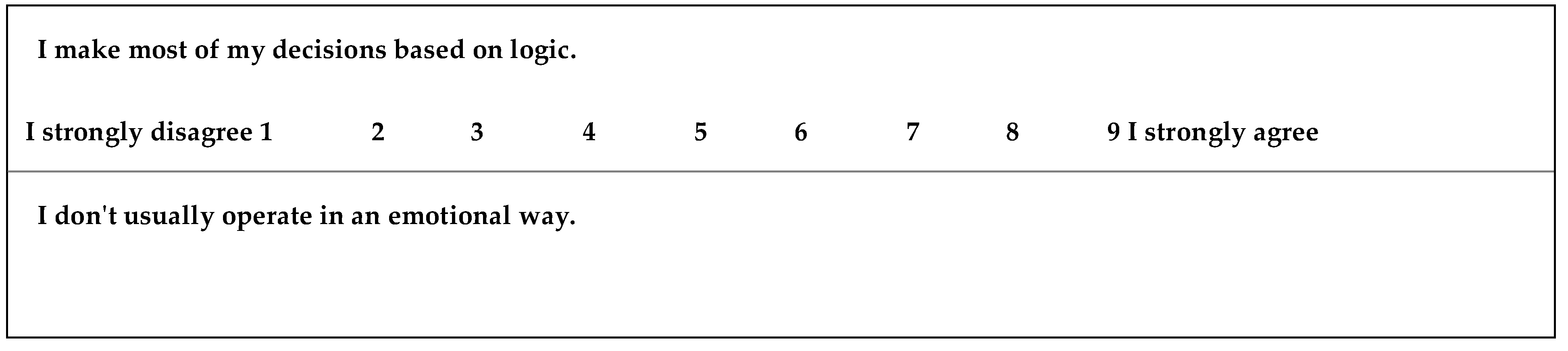
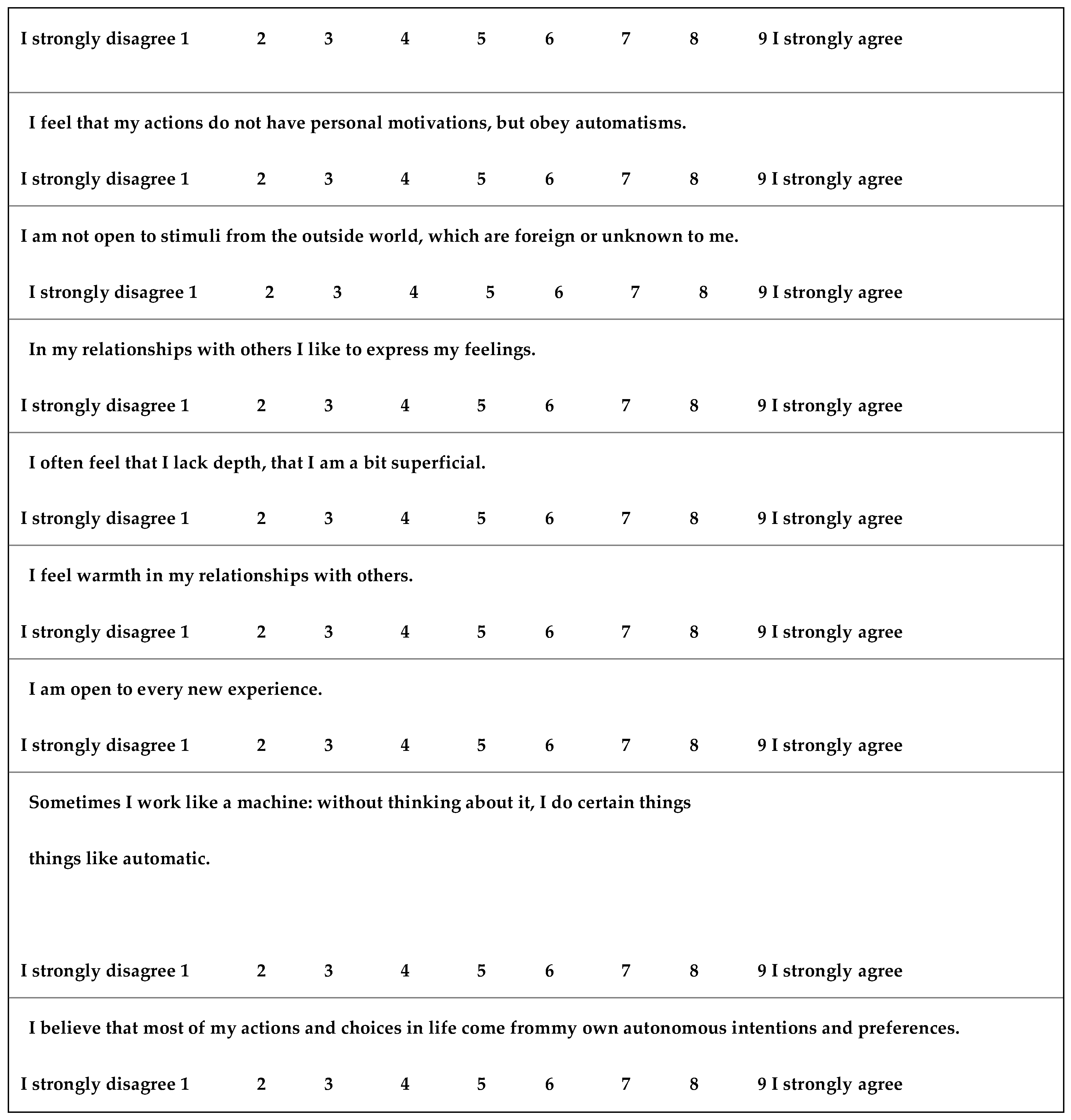
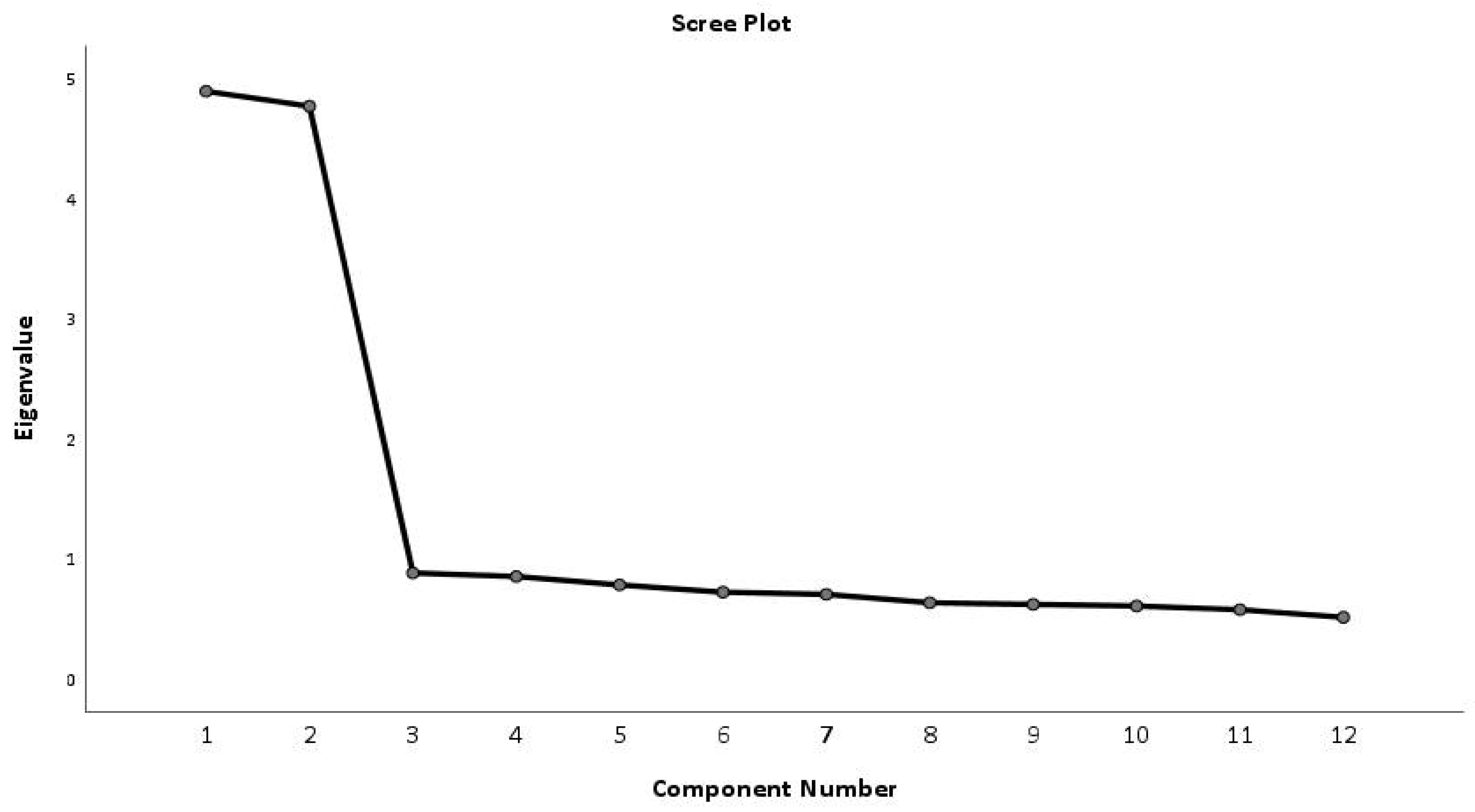
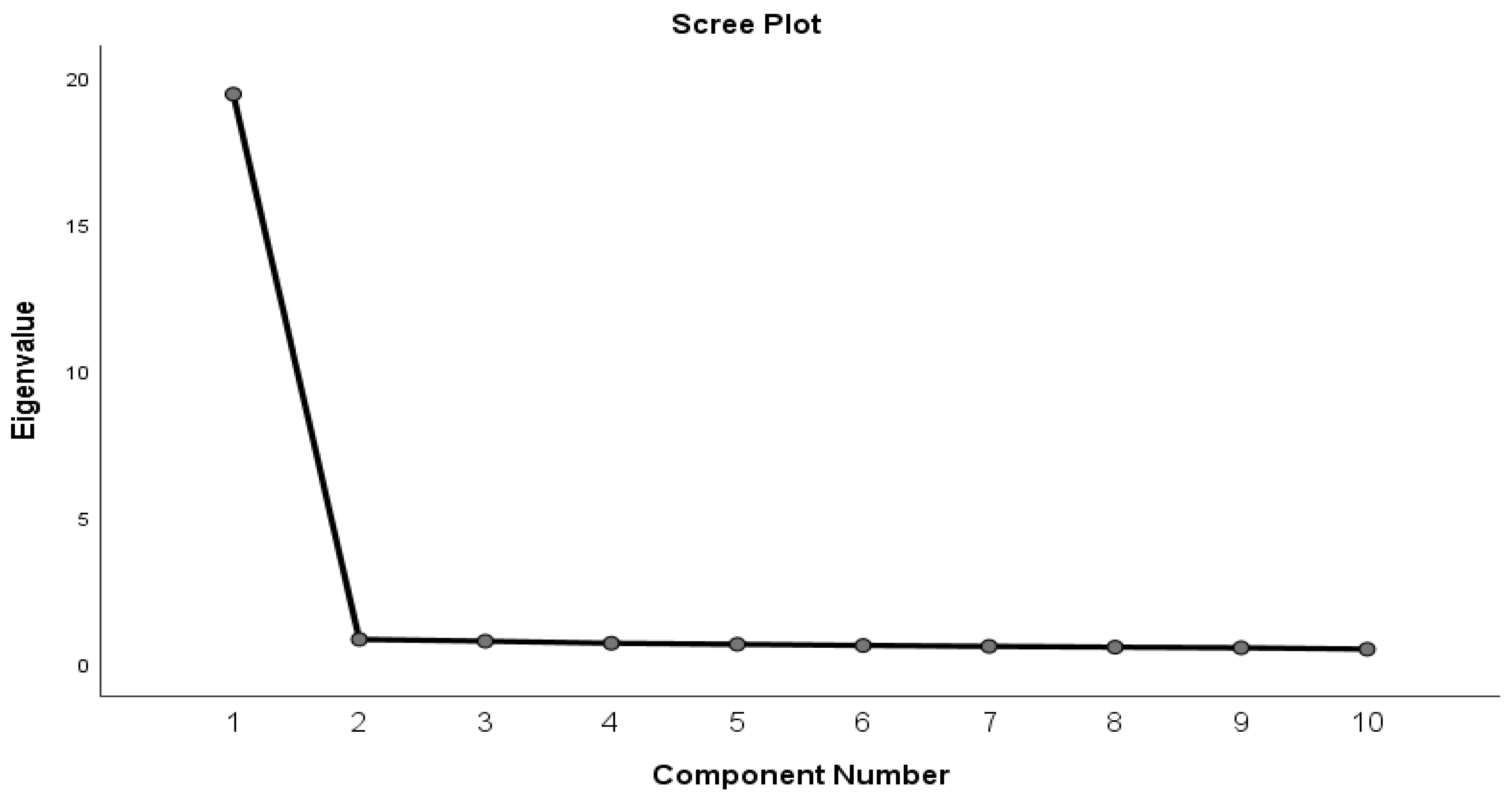
Results of the present study revealed that both newly developed and validated scales are psychometrically sound and theoretically valid measures of dehumanization and self-dehumanization. Factor analysis of the dehumanization scale resulted in a two-factor solution consisting of six items per factor and interpreting 58.35% of the total variance. The two factors were namely mechanistic and animalistic dehumanization. This result is in agreement with the theoretical framework of dehumanization proposed by Haslam (2006) [
2] that distinguishes those two forms of dehumanization [
2]. Furthermore, factor analysis resulted in a one-factor solution for the self-dehumanization scale interpreting 77.0% of the total variance in agreement with the Bastian (2014) theoretical model [
34] and reinforcing previous studies that are considering and investigating self-dehumanization with unidimensional scales. All items in both scales exhibited excellent factor loadings all above the threshold value of 0.30, indicating an acceptable structural validity of the validated instruments [
35]. Factor analysis was used to explore the questionnaire's validity, revealing clear dimensions that accurately represent the underlying concepts we aimed to measure. The high factor loadings indicate that each question effectively contributes to its respective dimension, confirming the questionnaire's validity.
In addition, according to our results, the Cronbach alpha indicator values were acceptable. More specifically the reported values were as follows 0.855 for the “Mechanistic dehumanization” subscale, and 0.858 for the “Animalistic dehumanization” subscale whereas for self-dehumanization the value was equal to 0.966. The mentioned values were above the threshold of 0.70 in indicating good reliability for the values above 0.80 and excellent for those above 0.90 [
36]. This means that the questions consistently measure the intended concepts, making our questionnaire a dependable tool for research.
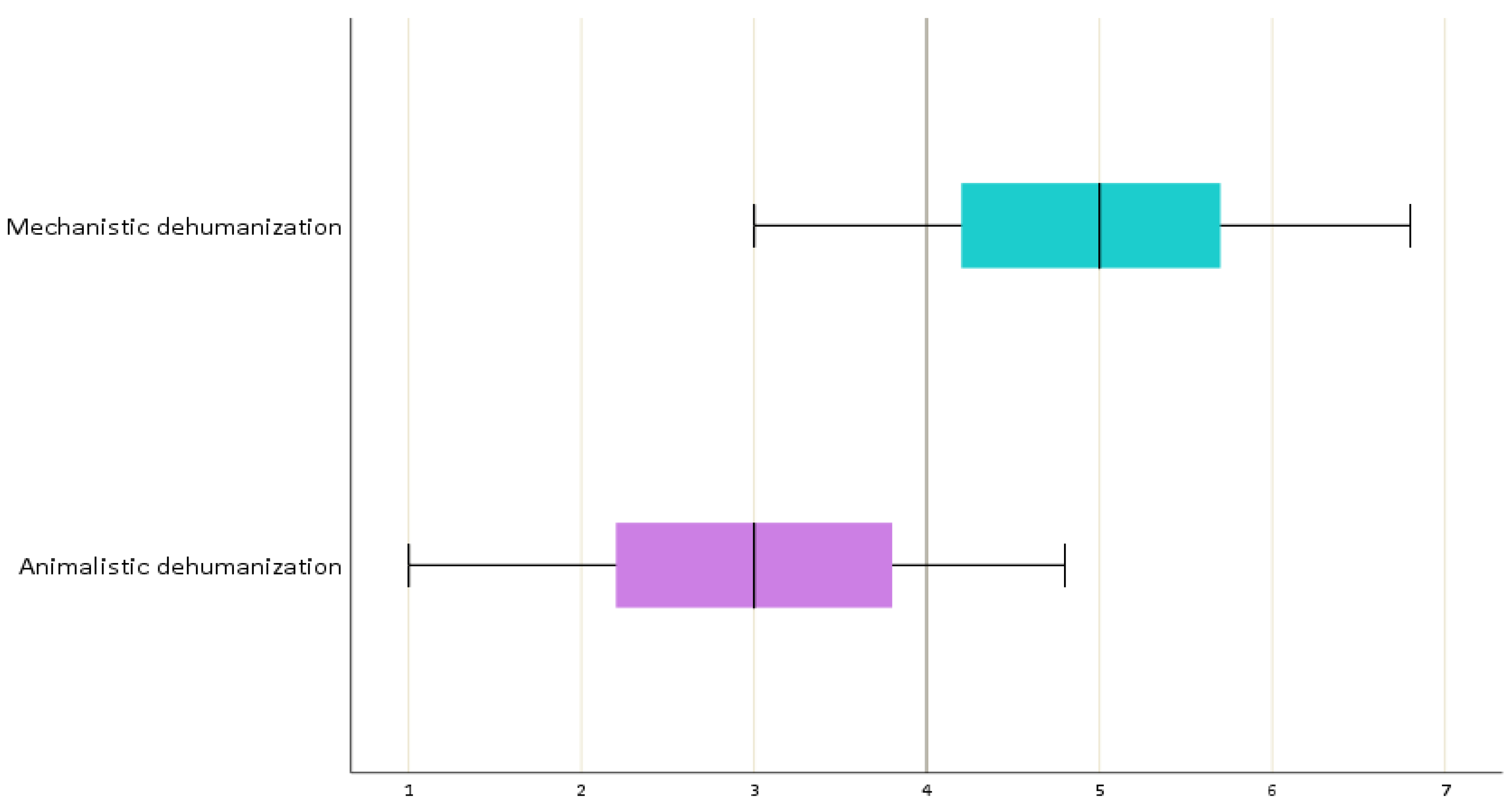
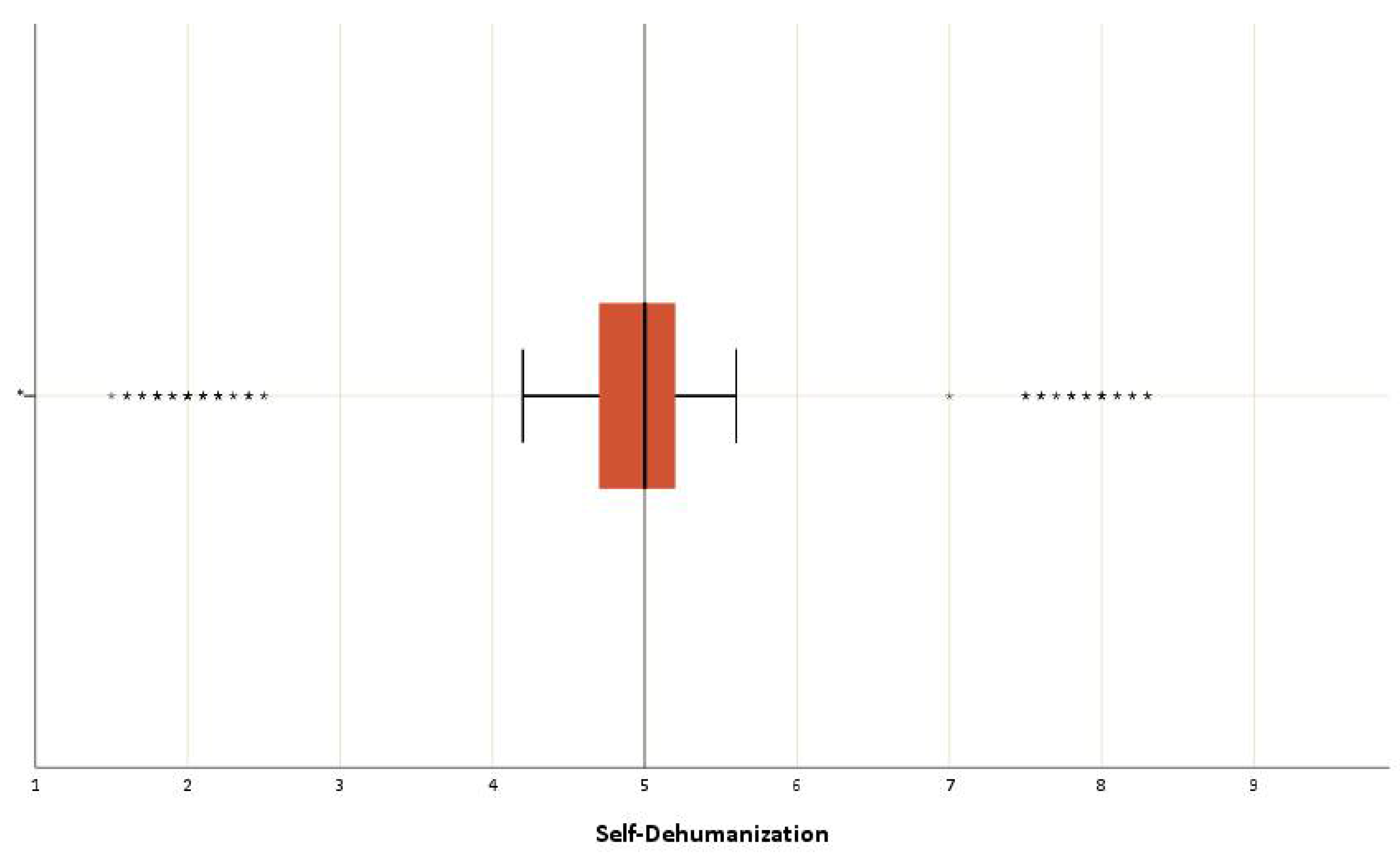
The statistical study’s results showed that doctors and nurses mechanistically dehumanized patients at a moderate to a high level, and also dehumanized themselves at a moderate level. These results are consistent with the existing literature. According to the correlations conducted in our research no socio-demographic and occupational factors were found to be associated with the Mechanistic-Dehumanization and Animalistic-Dehumanization subscales. A significant relationship was found between the Self-Dehumanization scale and: a) years of work in this department (more years correspond to a higher scale score, p = 0.009), b) attending a psychotherapy session (individuals who have attended psychotherapy sessions are associated with higher scores on the scale, p = 0.031). Furthermore, marital status was not found to be associated with any scale.
As aforementioned, more years of experience is a risk factor for increased levels of dehumanization for healthcare professionals. Prolonged exposure to high workloads, stressful environments, and emotionally challenging patient interactions can gradually diminish a healthcare professional's sense of self-esteem leading to feelings of burnout, emotional exhaustion, and a reduced ability to empathize with others. Additionally, although the finding that healthcare providers attending a psychotherapy session seems controversial, it may be reasonable considering that psychological distress and vulnerability, common reasons for seeking therapy, can contribute to the self-dehumanization or dehumanization of others. Also, the therapeutic process itself may lead to increased feelings of shame or inadequacy, feelings that can promote self-dehumanization or hetero-dehumanization as an outcome or a defensive reaction, respectively. The same effect can be triggered by the therapeutic environment which can disclose identity conflicts and internal struggles, exacerbating experiences of dehumanization. A recent study carried out at the Sotiria Hospital in Athens, Greece, showed that healthcare professionals mechanically dehumanize hospitalized patients [
25]. Another study found that nurses stigmatized and dehumanized patients with a psychiatric disorder more often, compared to people without a mental illness [
37]. This occurrence might be related to the cultural stigma associated with mental illness, resulting in unfavorable prejudices and stereotypes. Additionally, the complexities and challenges of managing psychiatric disorders in healthcare settings, combined with potential gaps in mental health education and training, may contribute to elevated stress and frustration among healthcare providers, influencing their attitudes and behaviors towards patients [
37].
Moreover, nurses tended to dehumanize patients more, if they felt dehumanized by their supervisors, and less if they had quality contacts [
37]. This emphasizes the pivotal role of workplace dynamics and organizational culture that influence nurses’ attitudes and behaviors toward patient care. Establishing a supportive and respectful workplace atmosphere is paramount for both fostering an empathetic and compassionate environment for patients and bolstering the overall effectiveness and well-being of nurses.
Self-dehumanization is a phenomenon that can result either from being treated negatively by others or from one’s behavior when it harms others [
1,
2,
25]. We would dare to say that the "offender" is also a "victim". Their character and experiences led them to self-dehumanization and the dehumanization of others. Research studies have shown that self-dehumanization occurs most often when people feel isolated, powerless, or out of control. A literature review of several studies showed that self-dehumanization appears to be due to a sense of helplessness rather than a random change in mood or negative self-esteem [
38]. In another research, it was shown that the suffering experienced by the person and unpleasant situations can cause the rejection of humanity both in ourselves and in others [
1]. In a recent study in Greece, it was confirmed that mental health specialists and hospital workers consider themselves more human compared to the general population, attributing to themselves characteristics of human nature and uniqueness [
25]. However, in some cases, self-dehumanization can encourage the individual to take social initiatives to restore humanity in the eyes of others and their self-concept [
34], which can be a hope for reducing this phenomenon.
4.1. Limitations
The present research faced some limitations. First of all, women outnumbered men in the sample, which is due to the nature of the profession as the majority of nurses are women. Secondly, the collected sample of 400 individuals, although large enough for statistical analysis, was not randomly selected. Finally, the cross-sectional study design limits the ability to establish causal relationships or assess changes over time.
The development of valid questionnaires that are intended to evaluate different aspects of dehumanization among healthcare professionals is the main strength of the present study. Providing precise measures to evaluate dehumanizing actions and attitudes is one of how our research makes a direct contribution to the improvement of patient care and the development of a more compassionate and empathic atmosphere within the healthcare system. These scales not only improve research capacities in the area of studying dehumanization, but they also have practical use in the form of directing interventions and training programs that are targeted at encouraging patient-centered care and professional ethics among healthcare workers.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P.; methodology, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P.; software, A.R., A.P., E.C.F., and E.P.; validation, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P..; formal analysis, A.R., A.P., E.C.F., K.F., and E.P.; investigation, A.R., A.P., K.F., and E.P.; resources, A.R., A.P., and E.P.; data curation, A.R., A.P., K.F., A.L., K.G., and E.P..; writing—original draft preparation, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P.; writing—review and editing, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P.; visualization, A.R., A.P., E.C.F., K.F., A.L., K.G., and E.P.; supervision, A.R., A.P., and E.P. All authors have read and agreed to the published version of the manuscript.” Please turn to the CRediTtaxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.