1. Introduction
Accidental falls are one of the most common health problems related to aging, with falls rate between 28% and 35% in people over 65 years old and around 40% among people over 80 [
1]. These accidents can negatively impact quality of life, socialization, family dynamics, health costs, fear of falling and risk of death [
2,
3]. Falls are associated with multifactorial circumstances that can act in isolation or together, including intrinsic (sarcopenia, functional loss, low visual and auditory acuity, cognitive decline, postural instability, balance and gait impairments, polypharmacy, musculoskeletal pain, chronic diseases), and extrinsic risk factors (such as environmental conditions, uneven and slippery floors, insufficient lighting, arrangement of furniture, steps, public roads and sidewalks with holes and irregularities, lack of handrails and signage) [
4,
5,
6,
7,
8,
9].
Pain is also a significant risk factor for falls. One in two older people with musculoskeletal pain fall each year. This occurs due to neuromuscular control changes and compensatory movements, which impact balance and gait, promote muscle weakness and joint injury and decrease executive function performance [
10]. Furthermore, pain is little investigated among older people, as at least 53% of ambulatory patients with moderate pain and 30% with severe pain do not receive any diagnosis [
11].
Therefore, it is essential to encourage falls prevention programs with available, efficient and low-cost strategies, such as health education, adapting home environment, encouraging physical activity practice, medication review, vitamin D supplementation and health reviews. Multifactorial interventions are important to reduce risk factors for falls and their consequences, to improve physical and cognitive aspects and to promote the aging in place, especially among faller and frail older people [
9,
12,
13,
14,
15,
16,
17].
Multifactorial interventions can prevent and reduce falls risk in community-dwelling older people. When associated with the prescription and performance of specific physical exercises, it can reduce falls rate [
15]. These interventions work with a multidimensional individual assessment to verify modifiable risk factors for falls, and specific referrals and strategies aimed at reducing the identified risk factors for each person [
18]. Physical exercise, when associated with multifactorial interventions, can have better adherence and promote long-term behavior change in older people [
19].
Case management is a new approach of multifactorial intervention, with the possibility of active discussions between participants, caregivers, family members and health care professionals about the risk factors identified in a multidimensional assessment. Also, case management protocols create and implement individualized and personalized plans to reduce risk factors for falls and their consequences [
20,
21]. Although most falls prevention programs include assessment of falls risk factors and physical exercise, they do not include case management as a core element of the intervention program [
21]. Therefore, this study aims to evaluate the effects of a multifactorial falls prevention program, based on case management, on physical performance, presence of pain and risk of falls and fractures in faller older people.
2. Materials and Methods
2.1. Trial Design and Setting
This is a block randomized design (allocation ratio 1:1), parallel group, single-blind (assessors) controlled trial. The trial was approved by the Research Ethics Committee of the Federal University of São Carlos (34350620.7.0000.5504) and it was registered in the Brazilian Registry of Clinical Trials (RBR - 3t85fd). A pilot study was conducted to identify possible barriers and facilitators to adhesion to the program and to standardize all procedures.
2.2. Study Population
Eligible volunteers were Brazilian community-dwelling older adults aged 60 years old and over, non-institutionalized, with a history of falls in the last year. Inclusion criteria were a history of at least two falls in the last year, willing to participate in the interventions and assessments, ability to walk with or without walking devices, familiarity of the volunteer or his/her family with the use of remote devices (self-reported), and availability of telephone contact. Exclusion criteria were severe and uncorrected visual or auditory disorders that affected communication during assessment and intervention, and active inflammatory and neurological diseases that severely interfere with balance performance, including advanced Parkinson disease - stage 5 of the modified Hoehn and Yahr Scale and not being on regular use of antiparkinsonian medications, Multiple Sclerosis, Huntington disease, dementia, uncontrolled vestibulopathy, epilepsy, traumatic brain injury and severe motor sequelae of stroke.
2.3. Power and Sample Size
The sample size was calculated using the G*Power 3.1 software, based on the main variable (Timed up and Go test), the type of study design (two-way ANOVA test), the type I error at 5%, the statistical power of 80% [
2,
9,
13,
15], the moderate effect size (0.20) and the number of groups (2). The total sample size was 42 people, however, taking into account a possible dropout rate of 20%, we recruited 62 community-dwelling older adults.
2.4. Location and Disclosure
The entire research was carried out remotely at the volunteer's home via video calls on Google Meet or telephone.
Volunteers were recruited through referrals from Health Care Network, dissemination on social networks, radio programs throughout Brazil, interviews on television programs, distribution of flyers and posters, promotional emails to higher education institutions and health, educational and social secretariats in all states of Brazil.
2.5. Randomization and Blinding
A researcher not involved in the recruitment, assessments and intervention was responsible for generating a sequence list using the Random Allocation software. According to the randomization sequence, each volunteer corresponded to an opaque and sealed envelope, numbered in order, containing a card that indicated in which group the volunteer would be inserted. After the initial evaluation, the volunteers were allocated (1:1) in 1 of the 2 groups: Intervention Group (IG) and Control Group (CG).
2.6. Assessments
Support materials were sent to the volunteers to facilitate the use of the remote devices and a previous video call was done to explain better the use. The assessment was carried out individually, with the help of a family member or caregiver if necessary, through a video call on google meet. All assessments were recorded according to prior authorization. The recordings and data were stored in Google Drive (virtual file storage service), and only the researchers who carried out the assessment and the coordinators had access to verify information when necessary. The video security guarantee is offered by Google and access to these videos is only released through 2-step authentication, which makes it difficult for hackers to access.
Volunteers were previously instructed to wear comfortable clothing, preferably closed shoes, not to perform vigorous physical exercises the day before the assessment, and to use auditory and/or visual aids when necessary. The assessments were carried out in 4 moments (initial, reassessment after 16 weeks of intervention, short follow-up after 6 weeks of reassessment and long follow-up after 12 months of the initial assessment). The variables evaluated in this study were falls risk, risk of osteoporotic fractures over the next 10 years, physical performance and presence of pain.
The Falls Risk Score was applied to assess falls risk. This scale presents 5 criteria: 1) presence of previous falls, 2) medications used that may increase falls risk, 3) presence of sensory deficit, 4) Mental State through the Mini-Mental State Examination, 5) gait. The scale ranges from zero to 11 points, and scores greater than or equal to 3 points suggest that the person is at high falls risk [
22,
23].
The risk of osteoporotic fractures in the next 10 years was assessed by the clinical FRAX® tool. For this calculation, it is necessary to use body mass index and age values, whether the participant presents previous fractures, whether he/she is a smoker and use of glucocorticoid-type medications. A FRAX® value lower than 5 is considered a low fracture risk. Values between 5 and 7.5 are considered intermediate risk and values greater than 7.5 are considered high risk of osteoporotic fractures [
24,
25].
Physical performance was assessed by the Short Physical Performance Battery (SPPB), the Timed up and Go test (TUG) and TUG with dual task (TUG DT). The SPPB consists of three tests that evaluate static balance (0-4), gait speed (0-4) and lower limb muscle strength (0-4). The final SPPB score is given by the sum of the 3 scores, which can vary between 0 and 12 points: 0 to 3 points indicates disability or poor ability, 4 to 6 points indicates low capacity, 7 to 9 points indicates moderate capacity and 10 to 12 points indicates good capacity [
26]. The TUG requires that the volunteer gets up from a chair, walks 3 meters in a straight line in the usual speed, turns around, walks back the same 3 meters and sits down again [
27]. A time of 12.47 seconds identifies brazilian older people at falls risk [
28]. The TUG DT included the TUG associated with saying names of animals (verbal fluency). A time greater than 15 seconds in the TUG DT indicates greater falls risk in community-dwelling older people [
29,
30].
The presence of pain was assessed by the Brief Pain Inventory, which includes questions about the volunteer's pain during the day, the pain points indicated by a body diagram, the pain intensity, the pain treatment or relief medication and the interference of pain with general activity, mood, ability to walk, work, relationships with other people, sleep and ability to enjoy life [
31].
2.7. Intervention
After randomization, the IG participants received an intervention with individual case management to modify the identified risk factors for falls. The intervention was carried out by two previously trained researchers, weekly through video calls via WhatsApp or phone calls. In the first weeks, the case manager, the participant and their family members established a trusting relationship and discussed the main points identified in the multidimensional assessment and the older adult's goals and preferences. Then, the case managers, with the team of researchers, created a personalized execution plan to be carried out over 16 weeks [
32].
In addition, IG participants were invited to take part in a home-based multicomponent physical exercise program delivered through recorded video guidelines twice a week during the intervention period. The exercise program was developed based on a previous protocol [
33] and in line with the main recommendations [
34,
35]. It was adapted to a remote format and to community-dwelling older adults with a history of falls in the primary health care setting. The progression of physical exercises was individualized. More information about the case management protocol is described by [
32]. The CG received only monthly calls during the 16 weeks to monitor falls and general health status.
2.8. Data Analysis
A significance level of 0.05 and the SPSS software (22.0) were used to perform the statistical tests by intention-to-treat. The Kolmogorov‒Smirnov normality test was applied to all continuous variables to verify data distribution. The chi-square test of association was used for categorical variables to compare groups and assessments. The independent t test was used to compare groups for continuous variables at baseline. The two-way ANOVA was used to test the interaction between groups and assessments. In case of interaction, analyses of simple main effects were performed, with adjustment for multiple comparisons (Bonferroni).
3. Results
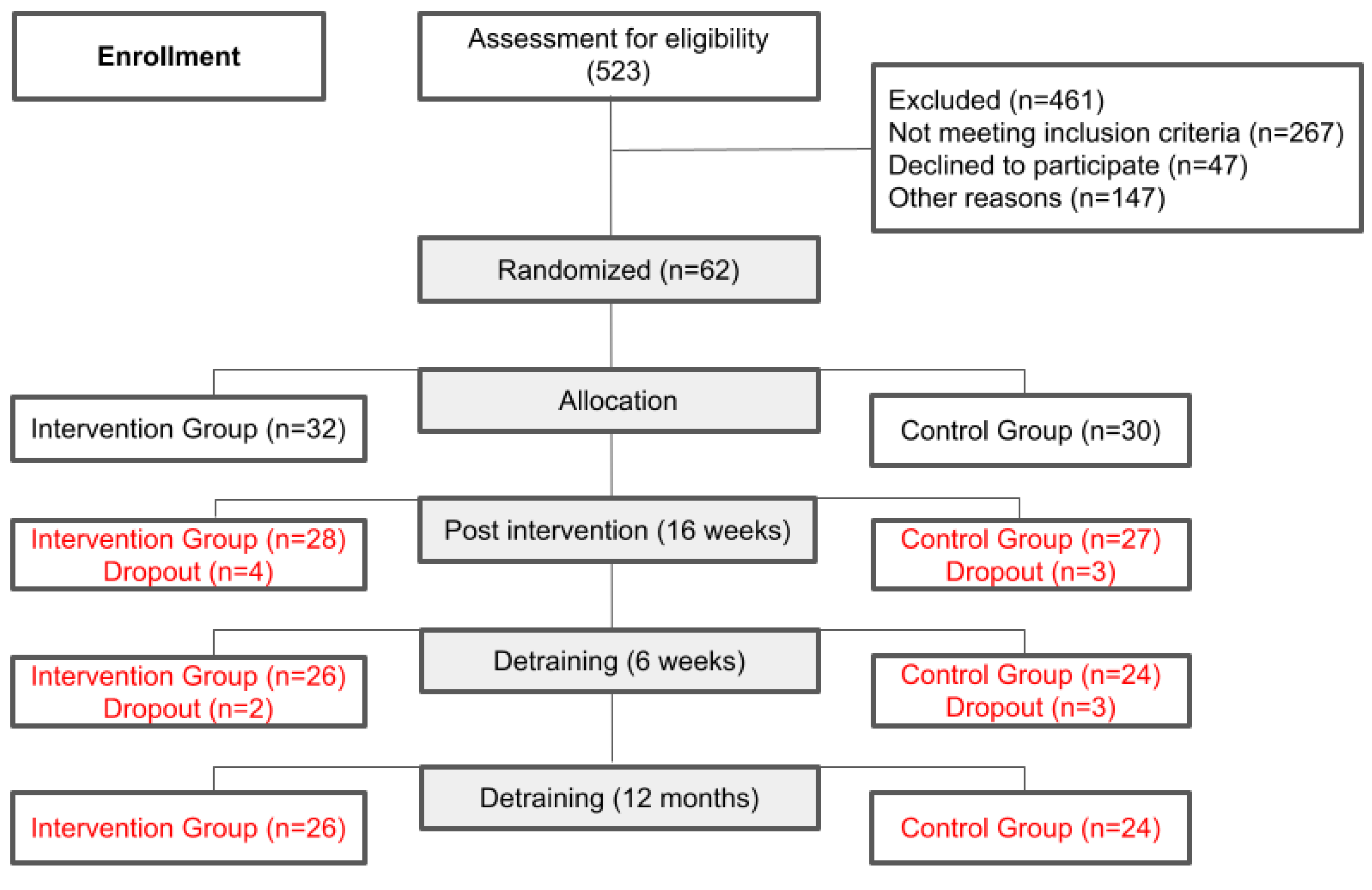
The final sample consisted of 55 participants, with 28 volunteers allocated to the IG and 27 people to the CG (
Figure 1). Eighty-six percent of the volunteers were from the Southeast region of Brazil, 7% from the Northeast region, 5% from the South region and 2% from the Central West region, with no participant from the North region.
We did not find significant differences in sociodemographic characteristics between groups at baseline (
Table 1). The sample was composed of mostly women, mean age of 72-73 years old, mean level of education of 10 years, 2 diseases (mean) and 3 to 4 medications in use (mean).
3.1. Risk of Falls and Fractures
At baseline, the mean number of previous falls in the last 12 months, assessed by the Falls Risk Score, was 2 to 3 falls, which indicates a population at high risk for falls.
The results of the SPPB, TUG, FRAX and BPI tests for each group at each assessment time are presented in table 2.
The FRAX
® presented a mean score of 7 points in the IG and 8 points in the CG at baseline, which means a high risk of fractures. No significant differences were found between groups and assessments (
Table 2).
3.2. Physical Performance
At baseline, the mean SPPB score was 5 points for both groups, indicating declines in physical performance. Also, the IG and CG participants completed the TUG test at baseline in 17 seconds (mean) and 20 seconds (mean), respectively, indicating that both groups are at high risk of falls. In the TUG DT, the average times to complete the test at baseline were 24 seconds and 27 seconds for participants in the IG and CG, respectively, indicating dual task impairments.
There were no significant differences between groups and assessments in any physical performance variable. After 16 weeks of intervention, the short and long follow-up periods, the physical performance scores remained similar in both groups. Despite this, the CG increased the time to perform TUG DT (mean of 33 seconds) after the long follow-up period.
3.3. Presence of Pain
At baseline, 19% of the volunteers in the IG and 29% in the CG reported pain (p=0.811). The most cited part of the body with pain for both groups was the lumbar spine. The mean number of pain sites was 5 for both groups. Pain intensity had an average score of 2 points for the IG and 3 points for the CG, using a scale that ranged from 0 (no pain) to 10 (maximum pain) points. There were no significant differences between groups and assessments regarding presence of pain.
4. Discussion
This randomized controlled trial showed that compared to no intervention, 16 weeks of multifactorial falls prevention program based on case management was not effective in improving physical performance or in reducing presence of pain and risk of falls and fractures in community-dwelling older people with a history of falls. Results of this study do not support our initial hypothesis, in which it was expected that participants who received the intervention based on case management would perform better.
Our findings are in contrast to the results from exercise interventions for preventing falls conducted in older people living in the community [
36]. A systematic review conducted by Sherrington et al. [
36] found that exercise that mainly involved balance and functional training reduced falls compared with an inactive control group. In the present study, the exercise program was provided through recorded videos and participants had to perform the exercises by themselves at home. It is possible that centre-based exercise programs performed with the presence of a health professional may be more effective than home-based exercise programs.
In a recent study, a remote home-based fall prevention exercise program was effective to improve physical function, psychological factors and balance among community-dwelling older adults, who were enrolled at a welfare senior centre [
37]. In the present study, participants had a history of at least two falls in the last year, which characterizes them as a more fragile sample of elderly people. Furthermore, many of them were not aware of the importance of physical exercise in preventing falls, as 11 of the 32 IG participants (34%) did not agree to participate in the physical exercise program during the intervention period.
Another factor that may have also contributed to the lack of improvement on physical performance of the IG participants was the delay in starting the exercise program, which prevented participants from completing all training sessions. Among the 21 participants who agreed to participate in the physical exercise program, 13 managed to complete at least 12 weeks of training. Participants completed an average of 23 sessions and 6 reassessments for progression. This was mainly due to the study design. During the first week of the intervention, participants were invited to take part in a physical exercise program, as a case management approach to prevent future falls. Participants who agreed to take part in the exercise program were required to provide a medical certificate before starting training. The delay in scheduling appointments and exams in primary health care was an issue and delayed the start of the exercise program, preventing many participants from completing the proposed training period.
Although no significant differences were found on pain measures, the assessment allowed identifying the lumbar spine as the part of the body with pain most cited by the participants.Moreover, the number of pain sites decreased over time in both groups. This information may be important to characterize pain in this population and to plan new strategies for managing pain in older people who have suffered falls. The majority of falls prevention programs focus on assessments and interventions related to foot pain, as the feet play an important role in body balance [
38]. In the present study, pain in the lumbar spine was identified as a possible risk factor for falls and, thus, future studies should also target this variable.
There is evidence that a home-based fall prevention Otago Exercise Programme can reduce pain among community-dwelling older adults [
39]. This study used a 1-year exercise intervention in which exercises were individually adjusted by a physical therapist during 6 home visits. Therefore, the presence of a health professional to determine the structure and progression of the individually tailored exercises may be crucial to reducing pain and improving performance.
Results of the present study also suggest a high risk of fractures among the recruited volunteers. The FRAX® algorithm quantifies a patient’s 10-year probability of a hip or major osteoporotic fracture by using data of the individual’s body mass index, age values, previous fractures, whether he/she is a smoker and use of glucocorticoid-type medications. Such variables are not modifiable by a short-term intervention, which can explain the lack of differences between pre and post intervention. It is important to note that this tool does not take balance measurements into account when calculating fracture risk [
24].
Regarding the Falls Risk Score, this proved to be an important tool that can be used in the educational process of the older people at risk of falls. In the present study, assessment results were presented and discussed with participants as a strategy to personalized execution plans. As a result, it was possible to hold conversations related to the concept of falls, the correct use of medications and reflections on the accidents that occurred and the risk factors involved. Therefore, providing guidance on the risk factors involved in fall accidents can be interpreted as an improvement in care and, consequently, a strategy for preventing falls and fractures.
Future studies aiming the development of falls prevention programs should consider the participant's access to health services, familiarity and access to technology, and the inclusion of assessment and management of pain with a higher sample size. Also, it is important to consider effective ways to adapt assessments and physical exercise protocols to the remote context.
Strengths and Limitations
A strength of our study is the remote application of tests and interventions. It is important to highlight that this study was carried out during the COVID-19 pandemic. For this reason, all assessments and interventions were adapted to be carried out via video and telephone calls, thus, we acknowledge that in some way this may have interfered with the results. Also, an important inclusion criteria was that participants should be able to communicate through video calls. This may have limited the possibility of having a more diverse sample of older people. Finally, our sample comprised self-selected volunteers and relatively educated older people (average of 10 years of schooling), so the findings cannot be generalized to less educated older people.
5. Conclusions
The multifactorial falls prevention program based on case management for community-dwelling older people with a history of falls was not effective on improving physical performance, but it was important for the characterization of pain and fracture probability for the next 10 years in this population. Future studies aiming the development of falls prevention programs should consider the inclusion of pain management and fracture prevention strategies.
Author Contributions
Conceptualization, Ansai, JH.; Gramani-Say, K.; and Alberto, SN.; Methodology, Alberto, SN.; Caetano, MJD.; and Novaes, ADC.; Software, Ansai, JH.; Validation, Ansai, JH.; and Alberto, SN.; Formal Analysis, Alberto, SN.; Resources, Gramani-Say, K.; and Ansai, JH.; Data Curation, Ansai, JH.; Alberto, SN.; Gramani-Say, K.; and Novaes, ADC.; Writing – Original Draft Preparation, Alberto, SN.; Novaes, ADC.; Rossi, PG.; Writing – Review & Editing, Novaes, ADC.; Melo, ML.; Ansai, JH.; Gramani-Say, K.; and Caetano, MJD.; Visualization, Novaes, ADC.; and Melo, ML.; Supervision, Gramani-Say, K.; and Ansai, JH.; Project Administration, Novaes, ADC; and Ansai, JH.; Funding Acquisition, Gramani-Say, K.; and Ansai, JH.
Funding
This research was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo - Processo nº 2021/01372-5.
Institutional Review Board Statement
The trial was approved by the Research Ethics Committee of the Federal University of São Carlos (34350620.7.0000.5504 - approved on July 27, 2021) and it was registered in the Brazilian Registry of Clinical Trials (RBR - 3t85fd)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflict of interest.
References
- WINGERTER, Denise Guerra et al. Mortalidade por queda em idosos: uma revisão integrativa. Revista Ciência Plural, v. 6, n. 1, p. 119-136, 2020. Disponível em: <https://periodicos.ufrn.br/rcp/article/view/18366>.
- MEROM, D. et al. Can social dancing prevent falls in older adults? a protocol of the Dance, Aging, Cognition, Economics (DAnCE) fall prevention randomized controlled trial. BMC Public Health, v. 13, n. 1, 2013.
- PIMENTEL, W. R. T. et al. Quedas entre idosos brasileiros residentes em áreas urbanas : ELSI- Brasil. Revista de Saúde Pública, v. 52, n. supl 2:12, p. 1–9, 2018.
- LUSARDI et al. Systematic Reviews Determining Risk of Falls in Community Dwelling Older Adults : A Systematic Review and Meta-analysis Using Posttest Probability. Journal of GERIATRIC Physical Therapy, v. 40, n. 1, p. 1–36, 2017.
- TISSOT, J. T.; VERGARA, L. G. L. Estratégias para prevenção de quedas no ambiente de moradia da pessoa idosa com foco no aging in place. Ambiente Construído, v. 23, p. 25-37, 2023.
- POLASTRI, P. F.; GODOI, D.; GRAMANI-SAY, K. Falls and Postural Stability in Older Individuals: Implications for Activities of Daily Living ´. In: Locomotion and Posture in Older Adults. 1. ed. [s.l.] Springer International Publishing AG, 2017. p. 263–277.
- DE SOUSA, K. C. A.; GARDEL, D. G.; LOPES, A. J. Postural balance and its association with functionality and quality of life in non-hospitalized patients with post-acute COVID-19 syndrome. Physiotherapy Research International, v. 27, n. 4, p. e1967, 2022.
- ALMEIDA, L. M. D. S.; MEUCCI, R. D.; DUMITH, S. C. Prevalência de quedas em idosos: um estudo de base populacional. Revista da Associação Médica Brasileira , v. 65, p. 1397-1403, 2019.
- DOURADO JÚNIOR, FW., et al. Intervenções para prevenção de quedas em idosos na Atenção Primária: revisão sistemática. Acta Paulista de Enfermagem, v. 35, 2022. Disponível em: <https://www.scielo.br/j/ape/a/TqV4k45sTkZYTJW9NGHh5Jj/>.
- HICKS, C. et al. Reduced strength , poor balance and concern about falls mediate the relationship between knee pain and fall risk in older people. BMC Geriatrics, v. 20, n. 94, p. 1–8, 2020.
- MCDONALD, D. D. et al. Older Adult Pain Communication and the Brief Pain Inventory Short Form. Pain Management Nursing, v. 9, n. 4, p. 154–159, 2008.
- BRASIL. Ministério da Saúde. Orientações técnicas para a implementação de Linha de Cuidado para Atenção Integral à Saúde da Pessoa Idosa no Sistema Único de Saúde-SUS. 2018. Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/linha_cuidado_atencao_pessoa_idosa.pdf.
- GUIRGUIS-BLAKE, J. M. et al. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. Jama, v. 319, n. 16, p. 1705-1716, 2018.
- ONG, M. F. et al. Fall prevention education to reduce fall risk among community-dwelling older persons: A systematic review. Journal of nursing management, v. 29, n. 8, p. 2674-2688, 2021.
- HOPEWELL, S., et al. Multifactorial interventions for preventing falls in older people living in the community: a systematic review and meta-analysis of 41 trials and almost 20 000 participants. British journal of sports medicine, v. 54, n. 22, p. 1340-1350, 2020. Disponível em: <https://bjsm.bmj.com/content/54/22/1340.abstract>.
- BÁRRIOS, M. J.; MARQUES, R.; FERNANDES, A. A. Envelhecer com saúde: estratégias de ageing in place de uma população portuguesa com 65 anos ou mais. Revista de Saúde Pública, v. 54, p. 129, 2020.
- DE PAIVA, E. P. et al. Preditores ambientais para quedas em idosos: revisão integrativa. Research, Society and Development, v. 10, n. 1, p. e29410111560-e29410111560, 2021.
- LAMB, S. E. et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials, v. 12, p. 1-8, 2011.
- LORD, S. R.; DELBAERE, K. I. M.; STURNIEKS, D. L. Chapter 10 - AGING. In: Handbook of Clinical Neurology. 3a ed. [s.l.] ELSEVIER, 2018. v. 159p. 157–171.
- LEUNG, A. Y. M. et al. Care Management Service and Falls Prevention : A Case-Control Study in a Chinese Population. Journal of Aging and Health, v. 22, n. 3, p. 348–361, 2010.
- REUBEN, D. B. et al. The STRIDE Intervention: Falls Risk Factor Assessment and Management, Patient Engagement, and Nurse Co-management. J Am Geriatr Soc. 2017 December ; 65(12): 2733– 2739, v. 65, n. 12, p. 2733–2739, 2017.
- SCHIAVETO, F. V. Avaliação do risco de quedas em idosos na comunidade. [Dissertação]. Universidade de São Paulo, Escola de Enfermagem de Ribeirão Preto, p. 117, 2008.
- SMITH, A. DE A. et al. Avaliação do risco de quedas em idosos residentes em domicílio. Revista Latino-Americana de Enfermagem, v. 25, 2017.
- NAJAFI, D. A.; DAHLBERG, L. E.; HANSSON, E. E. A combination of clinical balance measures and FRAX ® to improve identification of high-risk fallers. BMC Geriatrics, v. 16, n. 94, p. 1–7, 2016.
- ZERBINI, C. A. F. FRAX Modelo Brasil : um texto clínico explicativo sobre limiares para intervenção terapêutica. Diagn Tratamento, v. 24, n. 2, p. 41–49, 2019.
- NAKANO, M. M. VERSÃO BRASILEIRA DA SHORT PHYSICAL PERFORMANCE BATTERY – SPPB: ADAPTAÇÃO CULTURAL E ESTUDO DA CONFIABILIDADE. CAMPINAS: [2007].
- SHUMWAY-COOK, A.; BRAUER, S.; WOOLLACOTT, M. Predicting the probability for falls in community-dwelling older adults using the timed up and go test. Physical Therapy, v. 80, n. 9, p. 896– 903, 2000.
- ALEXANDRE, T. S. et al. Accuracy of Timed Up and Go Test for screening risk of falls among community-dwelling elderly. Brazilian Journal of Physical Therapy, v. 16, n. 5, p. 381–388, 2012.
- JEHU, D. A.; PAQUET, N.; LAJOIE, Y. Balance and mobility training with or without concurrent cognitive training improves the timed up and go (TUG), TUG cognitive, and TUG manual in healthy older adults: an exploratory study. Aging Clinical and Experimental Research, v. 29, n. 4, p. 711–720, 2017.
- STEFFEN, T. M.; HACKER, T. A.; MOLLINGER, L. Berg Balance Scale , Timed Up & Go. v. 82, n. 2, p. 128–137, 2002.
- FERREIRA, K. A. et al. Validation of brief pain inventory to Brazilian patients with pain. Supportive Care in Cancer, v. 19, n. 4, p. 505–511, 2011.
- ALBERTO, S. N. et al. A case management program at home to reduce fall risk in older adults (the MAGIC Study): protocol for a single-blind randomized controlled trial. JMIR research protocols, v. 11, n. 6, p. e34796, 2022.
- BUTO, M. et al. Pre-Frail multicomponent training intervention project for complexity of biological signals, functional capacity and cognition improvement in pre-frail older adults: a blinded randomized controlled study protocol. Geriatr. Gerontol, p. 1–6, 2019.
- American College of Sports Medicine. Exercise and physical activity for older adults. Med Sci Sport Exerc. 2009;41:1510–1530.
- GARBER, C. E. et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Medicine and Science in Sports and Exercise, v. 43, n. 7, p. 1334–1359, 2011.
- SHERRINGTON, C. et al. New Cochrane review assesses the benefits and harms of exercise for preventing falls in older people living in the community. Saudi Medical Journal, v. 40, n. 2, p. 204– 205, 2019.
- YI, D.; YIM, J. Remote Home-Based Exercise Program to Improve the Mental State, Balance, and Physical Function and Prevent Falls in Adults Aged 65 Years and Older during the COVID-19 Pandemic in Seoul, Korea. Medical Science Monitor, v. 27, 2021.
- STUBBS, B. et al. Pain is associated with recurrent falls in community-dwelling older adults: evidence from a systematic review and meta-analysis. Pain Medicine, v. 15, n. 7, p. 1115-1128, 2014.
- CEDERBOM, S.; ARKKUKANGAS, M. Impact of the fall prevention Otago Exercise Programme on pain among community-dwelling older adults: a short-and long-term follow-up study. Clinical interventions in aging, p. 721-726, 2019.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).