1. Introduction
Xylitol is a well-known, preventative product used in dentistry for decades [
1]. Erythritol and xylitol are polyols extensively researched and demonstrated to have notable anti-cariogenic and anti-periodontal disease properties with appropriate use [
2,
3,
4]. Polyols have been used traditionally (for about 80 years) to replace sugar in sweet foods to block tooth enamel demineralization and to reduce postprandial blood glucose surges. However, the benefits of added dietary polyols go beyond removing sugar. Emerging evidence shows that xylitol and erythritol can play several functional roles in actively supporting oral and systemic health maintenance with anti-biofilm, antioxidant, and anti-diabetic effects. Xylitol and erythritol disrupt keystone oral disease initiators such as S. mutans (caries) and P. gingivalis (periodontal disease) while acting as prebiotics and helping to balance and maintain a healthy microbiome, beginning with the oral gateway microbiome, which supports innate immunity and disease resistance [
5,
6,
7,
8,
9,
10,
11,
12,
13,
14].
The role of the microbiome in cancer development and treatment is now well-recognized 15. Indeed, the interactions between microbiome and cancer have generated research into the complex microbial communities and the possible mechanisms through which the microbiota influence cancer prevention, carcinogenesis, and anti-cancer therapy. In addition, developing next-generation prebiotics and probiotics designed to target specific diseases is considered extremely urgent [
16]. Ideally, healthcare providers will one day optimally implant effective prebiotics, probiotics, and the derived postbiotics to ameliorate disease [
17]. Immune elimination and immune escape are reported as hallmarks of cancer, and both can be partly bacteria-dependent, with the shaping of immunity by mediating host immunomodulation. In addition, host immunity regulates the microbiome by altering bacteria-associated signaling to influence tumor surveillance. Cancer immunotherapy, including immune checkpoint blockade (ICB), appears to have heterogeneous therapeutic effects in different individuals, partially attributed to the microbiota [
18]. In the era of personalized medicine, the microbiota and its interactions with cancer must be better understood, and manipulating the gut microbiota to improve cancer therapeutic responses could be necessary for future cancer treatment [
19].
Research demonstrates the inhibitory property of xylitol with many cancer cell lines when administered both dietary and systemically [
20,
21,
22]. Because xylitol exhibits almost no side effects and is safely utilized by healthy human cells, it could be a beneficent natural supplement for potentially inhibiting cancer cell proliferation [
23,
24]. Additionally, xylitol inhibits angiogenesis, thereby decreasing the vascularization of the tumor [
25]. Increased vascularization would support tumor growth and possibly cancer metastasis. Interestingly, the typical human is reported to endogenously produce approximately 15 gm per day in the liver, making xylitol endogenous [
26]. Indeed, xylitol is utilized by the mitochondria of cells as the precursor to the first step in the tricarboxylic acid cycle (also known as the citric acid cycle or the Krebs cycle), with xylitol dehydrogenase on the cristae converting xylitol to d-xylulose which then converts NADP to NADPH [
27]. In addition to the liver production of xylitol, many plants, such as blueberries, strawberries, plums, cauliflower, and even oats, have substantial amounts of xylitol naturally present [
28]. There is considerable overlap when comparing the list of xylitol-containing foods to the American Heart Association's “heart-friendly” foods list. Xylitol has been utilized even in diabetes prevention and as an anti-inflammatory [
29,
30].
Previous research with xylitol supplementation in animal models has had positive results in inhibiting cancer cell lines and xenografts [
31,
32]. Combination treatments with xylitol have also been reported as successful [
33]. Animal models are considered the first phase of cancer research, looking for potential therapeutic agents [
34]. This research study intends to use two mouse models to evaluate the efficacy of different concentrations and the modality of delivery of xylitol in cancer.
Metabolomics can be used to identify cancer biomarkers and the drivers of tumorigenesis [
35]. Metabolism is dysregulated in cancer cells to support uncontrolled cell proliferation [
36]. This dysregulation of cellular metabolism leads to specific metabolic phenotypes. These metabolic phenotypes can be used for earlier cancer diagnosis, clinical trials, patient selection, and/or as biomarkers of treatment response. Drugs that selectively target metabolic enzymes and, with precision medicine and nutrition, can affect cancer-related unique metabolic dependencies [
37]. Cancer outcomes and the patient's quality of life may be affected by cancer and cancer treatments in individual and complex manners due to the whole-body interaction and the influences of diet and exercise [
38].
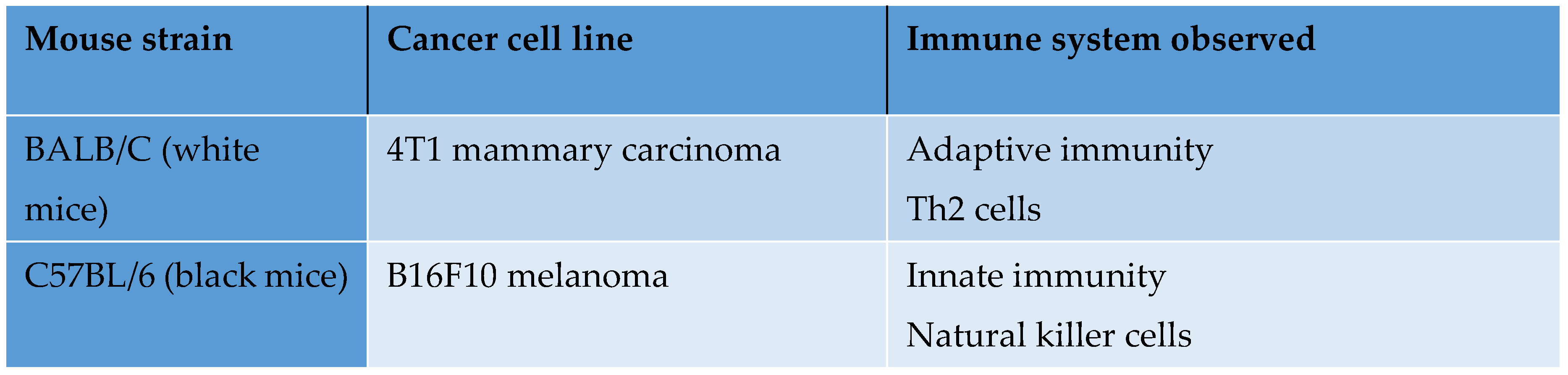
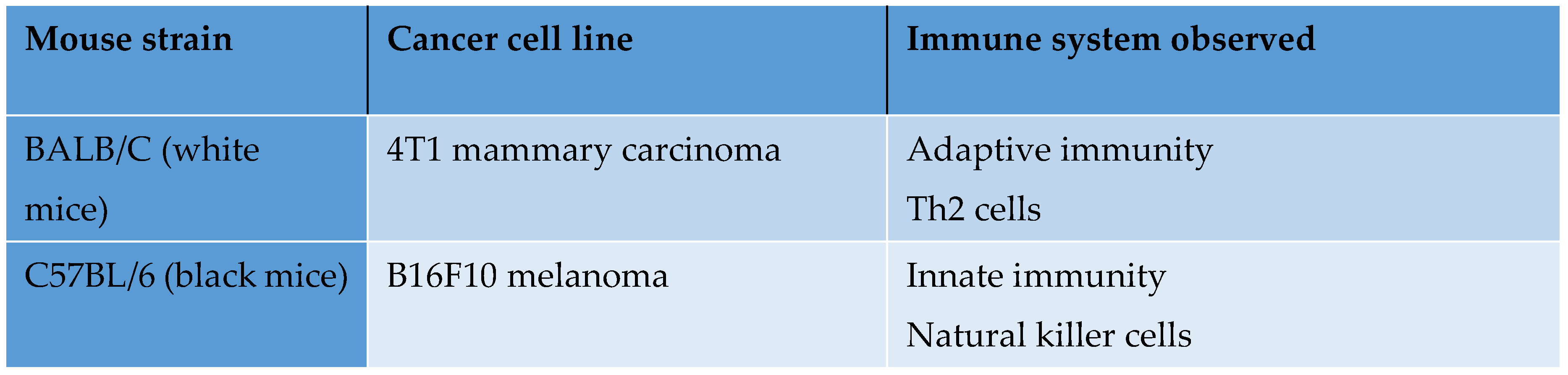
The purpose was to evaluate the effects, including cell line inhibition of xylitol on tumor progression, in two syngeneic mouse cancer models. Specifically, this pilot study measured tumor inhibition from two cancer cell line implantations in two syngeneic mouse cancer models, 4T1 mammary carcinoma and B16F10 melanoma, with 20% xylitol (prebiotic) solution intratumorally administered daily. Institutional (IACUC) approval was obtained for this study.
2. Materials and Methods
This study included two strains of immunocompetent female mice: 20 C57BL/6 and 20 BALB/c mice for a total of 40 mice. The BALB/c group was injected with 4T1 mammary carcinoma cells (1 x 10^6 cells into the 4th mammary gland), and the C57BL/6 group was injected with B16F10 melanoma cells (1 x 10^6 cells into the flank). When tumor sizes reached 50 to 100 mm3, both treatment groups (10 each) were injected daily with 20% xylitol solution intratumorally and subcutaneously. Control mice received sterile saline (10 each) with the same daily treatment frequency (Monday – Sunday) as the xylitol group. The treatment route was subcutaneous (SQ) - ~75% of volume Intra-tumoral (IT)- with the remaining 25% peri-tumorally. Tumor tissue and terminal blood were collected for pharmacokinetic, metabolomic, and histopathologic analyses upon mouse euthanasia.
Euthanization protocol:
All mice were euthanized when control tumor volumes were equal to or larger than 2000 mm3 or if mice lost more than 20% of their original body weight. In addition, euthanization was performed if there are other severe clinical health issues (e.g., paralysis) that would cause undue discomfort. Xylitol was given daily until significant changes in the tumor sizes were observed (the study terminated if no changes were seen). Euthanasia was performed according to IACUC protocol. Animals were not combined from different cages, and when euthanizing some of the mice from a cage, the rest of the animals remained in their original cage. The maximum number of mice per cage was five, and the CO2 flow rate per mouse cage was 3 L/min until one minute after breathing stopped. Euthanasia was confirmed by cervical dislocation.
Data:
All mice's body weight and Tumor volume were measured every other day. After the study terminated, tumor tissue and blood were collected for the following analyses: pharmacokinetic, metabolomic (tissue flash frozen in liquid nitrogen), and histopathology—tissue placed in formalin (for H&E staining for general morphology, IHC staining for microvascular density).
3. Results
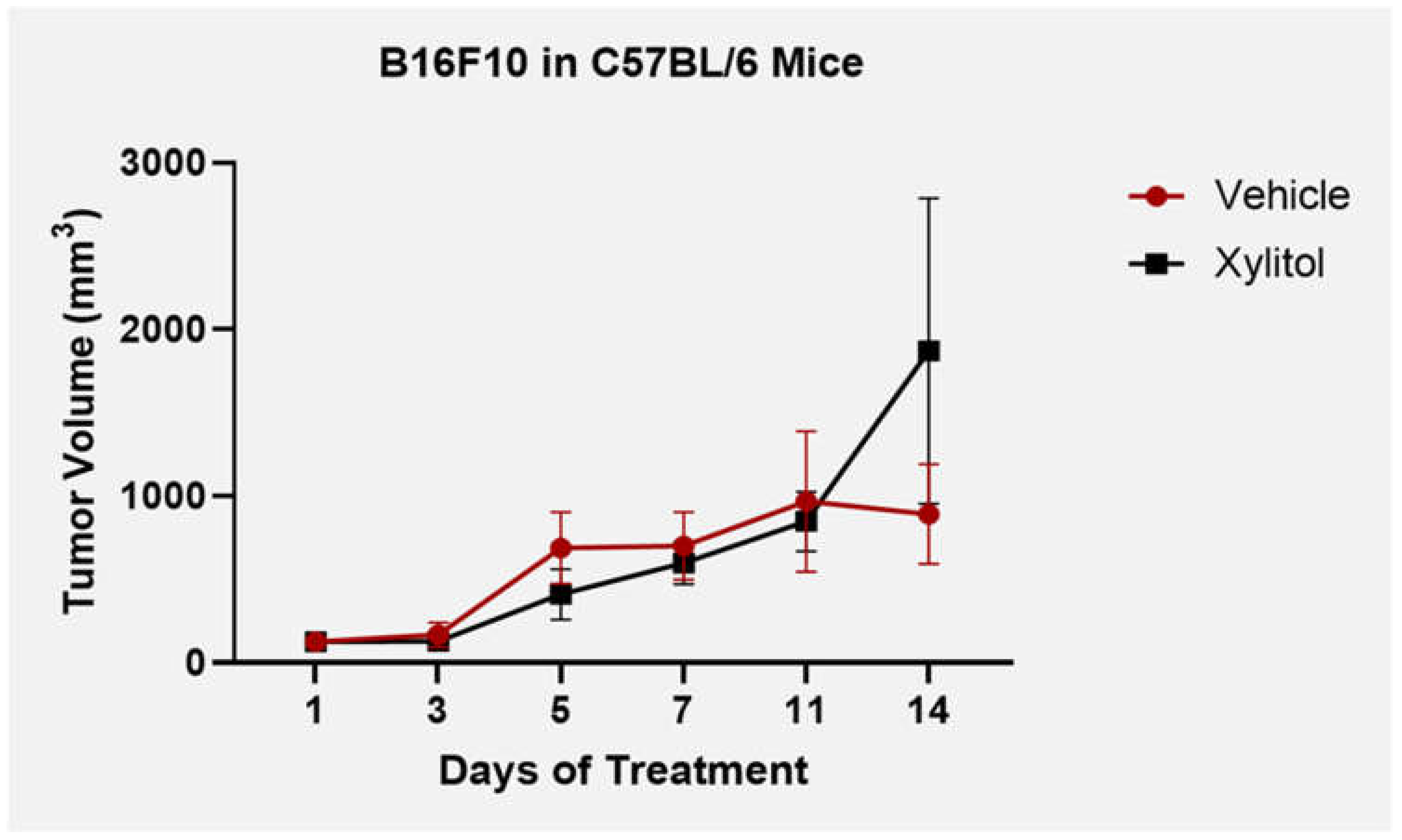
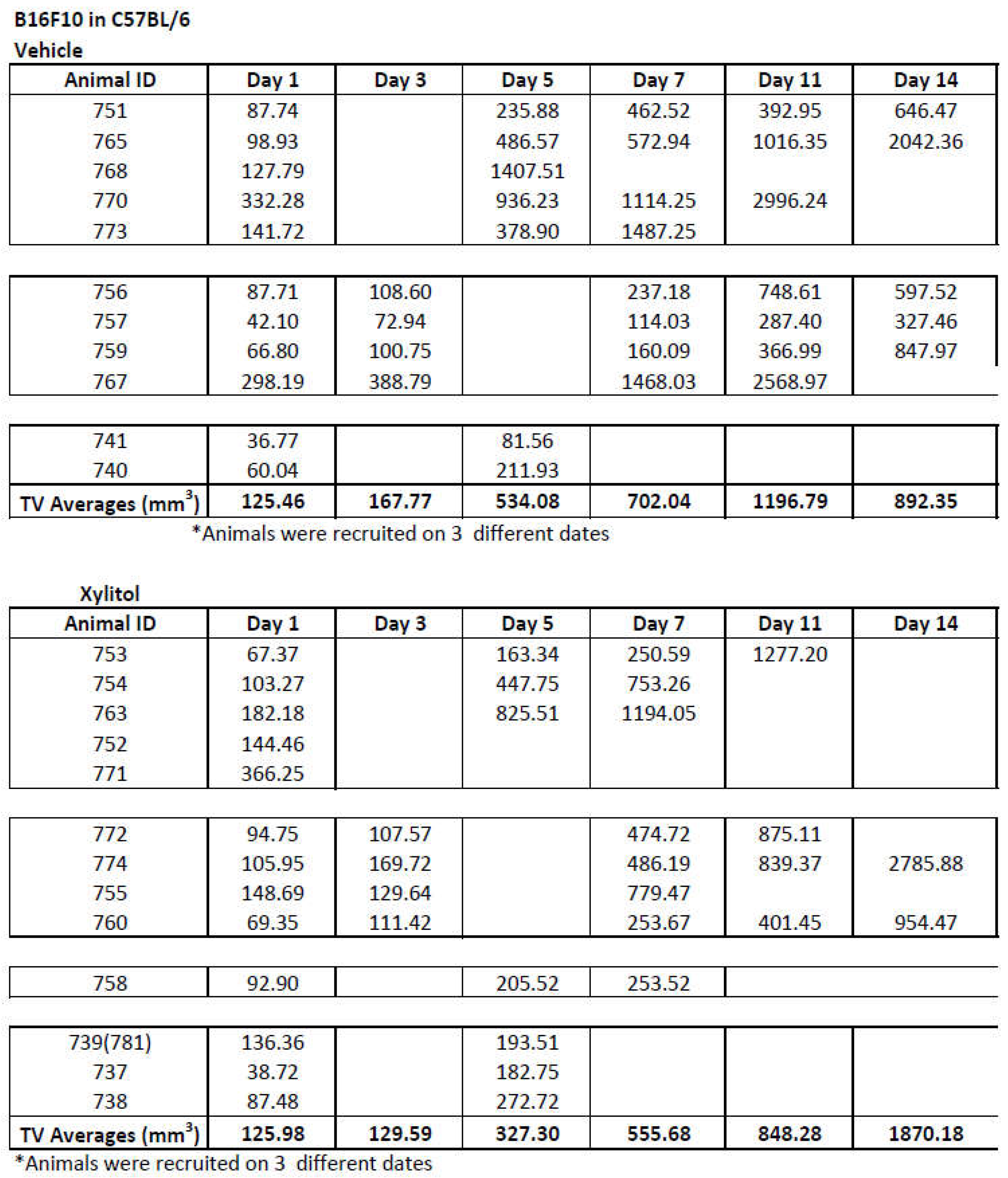
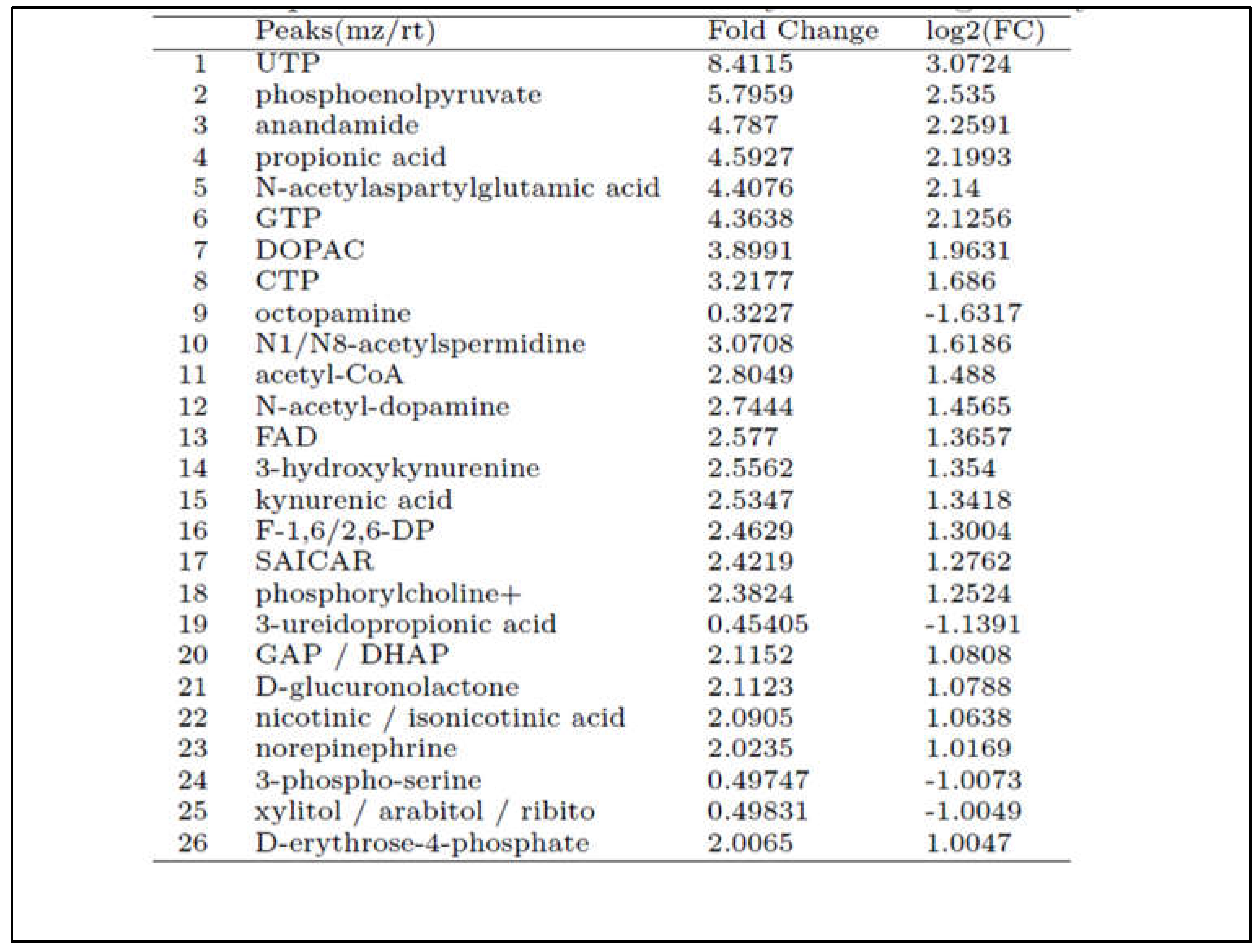
After five days of 20% xylitol injections, tumor volumes were reduced by 40% in the C57BL/6 group injected with B16F10 melanoma cells (see
Figure 1), but with the BALB/c + 4T1 cancer line (adaptive immunity), the tumor reduction was insignificant. With repeated intra-tumoral injections, the tumor stroma deteriorated in the B16F10 tumors, resulting in substantial xylitol leaking onto the skin surface. Afterward, experimental and control tumor volumes would become clinically comparable by study termination at day 14 (see
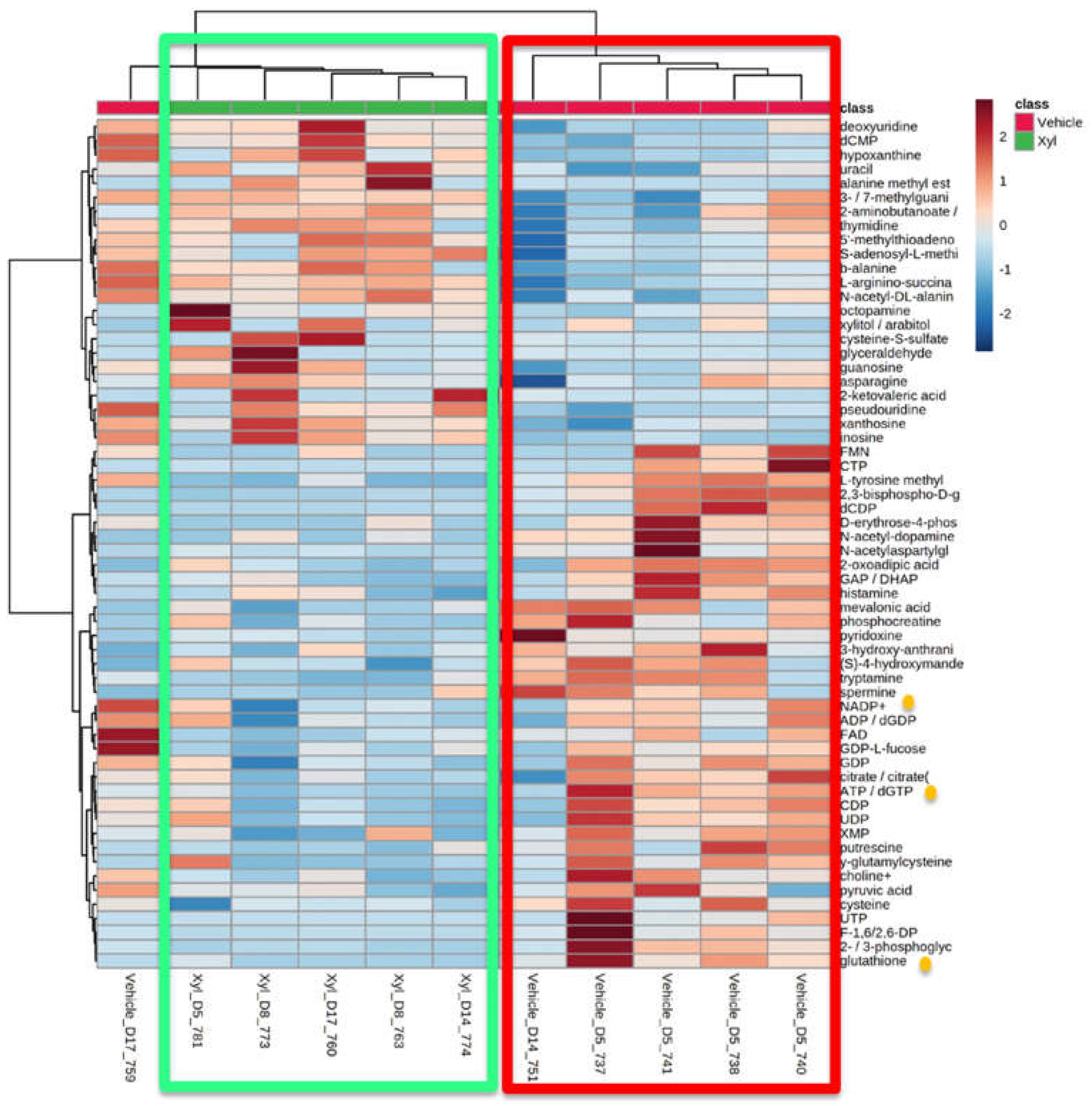
Table 1). Interstitial tumor pressure increased, preventing sufficient injection of the solution after five days. Metabolomic analysis revealed apparent differences between experimental and control tumor cellular metabolism. Lymph node histological analysis demonstrated metastasis in both groups by the time of euthanasia. The metabolomic analysis demonstrates that intratumoral xylitol reduces tumor cell production of histamine, NADP+, ATP, and glutathione, thereby affecting the availability of reactive oxidative species and the host immune response (see
Figure 2). The xylitol group showed significantly decreased phosphocreatine, citrate, and pyruvic acid levels, signifying metabolic stress likely due to inhibiting mitochondrial metabolism within the tumor cells. Notably, xylitol levels were increased in tumors, demonstrating that xylitol accumulates in cancer cells and suggests that the effects of xylitol are likely due to cancer cell-intrinsic effect on metabolism (see
Table 2). In addition, a decrease in tumor glutathione may affect the innate immune response, enhancing the effect of reactive oxidative species.
4. Discussion
The data denotes that xylitol inhibits both cancer cell lines, although only significantly in the melanoma group (syngeneic model C57L/C, B16F10- innate immunity). Cancer cells cannot utilize xylitol as can normal human cells (as do rodents such as rats and mice) in their mitochondria for energy [
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39]. Most cancer cells utilize glycolysis and mitochondrial metabolism to sustain growth in vivo [
40]. Certain animal species cannot correctly utilize xylitol, especially carnivores that have not been evolutionarily exposed to plants as foods 41. Tubers were once a significant source of food for homo sapiens and still a survivor food for hunter-gatherers, such as the Hadza tribe [
42,
43]. The microbiome of hunter-gatherers and traditional tribal people maintains specific bacterial taxa that can utilize complex carbohydrates and polyols [
44,
45]. One can theorize that homo sapiens cell mitochondria may have rapidly evolved to metabolize xylitol due to its presence in several survival foods, especially during periods of scarcity [
46]. Cockroaches, mice, rats, swine, and humans can metabolize xylitol [41,42 and 46].
Xylitol enhances the innate immune system response to cancer cells. Cancer cell lines are effectively more sensitive to ROS the killer T-cells produce [
47]. Results from metabolomics support the theory. The metabolomic values were different between the vehicle and xylitol groups. Specifically, tumor cell production of glutathione and histamine was reduced by xylitol. Glutathione is an antioxidant that reduces the reactive oxygen species (ROS) effect on tumor cells [
48,
49]. Xylitol reduction of histamine may hypothetically reduce metastasis by reducing vascularization and proliferation [
50,
51]. In addition, mitochondrial metabolism is necessary to determine stem cell fate. Mitochondrial metabolism is responsible for the production of ATP and maintains the tricarboxylic acid (TCA) cycle. The metabolites of the TCA cycle support stem cell survival and growth. Recent evidence shows that mitochondria control mammalian stem cell’s fate and function through reactive oxygen species (ROS) generation, TCA cycle metabolite production, NAD+/NADH ratio regulation, pyruvate metabolism, and mitochondrial dynamics [
52]. Xylitol affects the mitochondria and the TCA cycle, apparently with anti-oncogenic properties.
Our first protocol utilized intra-tumor injections, which proved less effective due to loss of stroma. Lack of structural integrity, interstitial fluid pressure, and possibly tumor trauma resulted in xylitol solution leaking from the tumor, allowing for tumor progression [
53]. This exact mechanism was reported with previous intra-tumoral injections using chemotherapeutics, such as 5 fluorouracil, until the development of smart hydrogels [
54]. Studies in progress at the Developmental Therapeutics Core utilize Alzet mini osmotic pumps that deliver a consistent concentration of xylitol to the subject animals [
55,
56]. Our research team is now cautiously optimistic that this approach will advance techniques used in previously published studies with IV xylitol, which could be more challenging to implement in an animal group [
21].
The human microbiota and microbiome have many biological functions, including food digestion, synthesis of various vitamins, protection from pathogen colonization, and resistance against systemic infections [
57]. The gut microbiota also plays a crucial role in immune system development, and its alteration can cause immune dysregulation, which can lead to autoimmune diseases [
58]. The role of microbiome in cancer development/progression via several mechanisms, including immune response modulation and the promotion of a pro-inflammatory tumor environment, has been very well studied and established [
59].
It has also been noted that xylitol significantly affects the composition of the gut microbiota, stimulates the propagation of beneficial bacteria, and produces short-chain fatty acids (SCFAs) [
60,
61]. This altered metabolism of xenobiotic xylitol can potentially influence cancer growth and progression [
62].
5. Conclusions
Our study offers novel insights into the potential therapeutic role of xylitol in cancer treatment, specifically in melanoma. Treatment with a 20% xylitol solution demonstrated a significant reduction in the initial growth of B16F10 melanoma tumors in syngeneic mouse models, highlighting xylitol's potential as an adjunctive treatment in oncology. Notably, this effect was predominantly observed in the melanoma model, indicating a potential cancer-type specificity or differential mechanism of action. The efficacy of the xylitol injections decreased after five days due to melanoma tumor stroma degradation, and the tumors re-commenced growth.
The findings underscore the intricate relationship between metabolic interventions and tumor progression. Xylitol's impact on tumor metabolism, specifically its influence on reducing tumor cell production of crucial metabolites like histamine, NADP+, ATP, and glutathione, paves the way for further exploration into its role as a metabolic modulator in cancer therapy. This is particularly relevant given the growing interest in metabolic pathways as targets for cancer treatment.
Moreover, the differential responses observed between the 4T1 mammary carcinoma and B16F10 melanoma models illuminate the complex nature of cancer biology and the necessity for targeted therapeutic strategies. Our study also brings to light the challenges associated with intratumoral drug delivery, as evidenced by the complications in maintaining the structural integrity of the tumor stroma during xylitol administration.
Future research should focus on optimizing the delivery method of xylitol to enhance its therapeutic efficacy. Extending these findings to other cancer models and eventually to clinical trials will be crucial to fully understanding xylitol's potential in cancer treatment. Our research lays the groundwork for such future investigations, with the hope of contributing to more effective and targeted cancer therapies.
Data Availability
All data is published in this and subsequent articles.
Ethics Statement
This research was conducted in strict accordance with ethical standards and guidelines for animal experimentation. All procedures performed in animal studies complied with the ethical standards of the institution where the studies were conducted. Efforts were made to minimize animal suffering and reduce the number of animals used.
Author Contributions
Conceptualization, M.C. and N.G.; methodology, N.G.; validation, A.C., F.P. and F.R.; formal analysis, N.C.; investigation, M.C.; resources, L.T.; data curation, L.T.; writing—original draft preparation, M.C.; writing—review and editing, M.T.; visualization, A.C.; supervision, M.C.; project administration, N.G.; funding acquisition, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Developmental Therapeutics Core at Northwestern University and the Robert H. Lurie Comprehensive Cancer Center support grant (NCI CA060553). Funding provided by the Swanson Fund with special thanks to Drs. Lon Jones, and R. William Cornell for their contributions.
Acknowledgments
Metabolomics services were performed by the Metabolomics Core Facility at Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nayak, P. A., Nayak, U. A., & Khandelwal, V. (2014). The effect of xylitol on dental caries and oral flora. Clinical, cosmetic and investigational dentistry, 6, 89–94. [CrossRef]
- Janakiram C., Deepan Kumar C. V., Joseph J., Xylitol in preventing dental caries: A systematic review and meta-analyses. J Nat Sci Biol Med. 2017 Jan-Jun; 8(1): 16–21.
- Kõljalg S, Smidt I, Chakrabarti A, Bosscher D, Mändar R. Exploration of singular and synergistic effect of xylitol and erythritol on causative agents of dental caries. Sci Rep. 2020 Apr 14;10(1):6297. [CrossRef] [PubMed] [PubMed Central]
- Mäkinen KK (2017) Sugar alcohols and prevention of oral diseases – comments and rectifications. Oral Health Care 2. [CrossRef]
- Salli, K., Lehtinen, M. J., Tiihonen, K., & Ouwehand, A. C. (2019). Xylitol's Health Benefits beyond Dental Health: A Comprehensive Review. Nutrients, 11(8), 1813. [CrossRef]
- de Cock P. Erythritol Functional Roles in Oral-Systemic Health. Adv Dent Res. 2018 Feb;29(1):104-109. doi: 10.1177/0022034517736499. PMID: 29355425.
- Bettina K. Wölnerhanssen, Anne Christin Meyer-Gerspach, Christoph Beglinger & Md. Shahidul Islam (2020) Metabolic effects of the natural sweeteners’ xylitol and erythritol: A comprehensive review, Critical Reviews in Food Science and Nutrition, 60:12, 1986-1998, DOI: 10.1080/10408398.2019.1623757.
- Cannon ML, Merchant M, Kabat W, Catherine L, White K, Unruh B, Ramones A. In Vitro Studies of Xylitol and Erythritol Inhibition of Streptococcus Mutans and Streptococcus Sobrinus Growth and Biofilm Production. J Clin Pediatr Dent. 2020 Sep 1;44(5):307-314. [CrossRef] [PubMed]
- Sánchez M.C., Romero-Lastra P., Ribeiro-Vidal H., et al. Comparative gene expression analysis of planktonic Porphyromonas gingivalis ATCC 33277 in the presence of a growing biofilm versus planktonic cells. BMC Microbiol. 2019;19(1):58. Published 2019 Mar 12. [CrossRef]
- Badet C., Furiga A., Thébaud N. Effect of xylitol on an in vitro model of oral biofilm. Oral Health Prev Dent. 2008;6(4):337-41.
- 11. Marleen Marga Janus, Catherine Minke Charlotte Volgenant, Bernd Willem Brandt, Mark Johannes Buijs, Bart Jan Frederik Keijser, Wim Crielaard, Egija Zaura & Bastiaan Philip Krom (2017) Effect of erythritol on microbial ecology of in vitro gingivitis biofilms, Journal of Oral Microbiology, 9:1. [CrossRef]
- Söderling E., Hietala, Lenkkeri A.M. (2010) Xylitol and erythritol decrease adherence of polysaccharide-producing oral streptococci. Curr Microbiol 60: 22-29.
- S. Ferreira, Aline; F. Silva-Paes-Leme, Annelisa; R.B. Raposo, Nadia; S. da Silva, Silvio. By Passing Microbial Resistance: Xylitol Controls Microorganisms Growth by Means of Its Anti-Adherence Property. Current Pharmaceutical Biotechnology, Volume 16, Number 1, January 2015, pp. 35-42(8).
- Bahador, A., Lesan, S., & Kashi, N. (2012). Effect of xylitol on cariogenic and beneficial oral streptococci: a randomized, double-blind crossover trial. Iranian journal of microbiology, 4(2), 75–81.
- Meng, C., Bai, C., Brown, T. D., Hood, L. E., & Tian, Q. (2018). Human Gut Microbiota and Gastrointestinal Cancer. Genomics, proteomics & bioinformatics, 16(1), 33–49. [CrossRef]
- Tsai, Y. L., Lin, T. L., Chang, C. J., Wu, T. R., Lai, W. F., Lu, C. C., & Lai, H. C. (2019). Probiotics, prebiotics and amelioration of diseases. Journal of biomedical science, 26(1), 3. [CrossRef]
- Yadav, M. K., Kumari, I., Singh, B., Sharma, K. K., & Tiwari, S. K. (2022). Probiotics, prebiotics and synbiotics: Safe options for next-generation therapeutics. Applied microbiology and biotechnology, 106(2), 505–521. [CrossRef]
- Zhou, C. B., Zhou, Y. L., & Fang, J. Y. (2021). Gut Microbiota in Cancer Immune Response and Immunotherapy. Trends in cancer, 7(7), 647–660. [CrossRef]
- Ting, N. L., Lau, H. C., & Yu, J. (2022). Cancer pharmacomicrobiomics: targeting microbiota to optimise cancer therapy outcomes. Gut, 71(7), 1412–1425. [CrossRef]
- Park, E., Park, M. H., Na, H. S., & Chung, J. (2015). Xylitol induces cell death in lung cancer A549 cells by autophagy. Biotechnology letters, 37, 983-990.
- Tomonobu, N., Komalasari, N. L. G. Y., Sumardika, I. W., Jiang, F., Chen, Y., Yamamoto, K. I., ... & Sakaguchi, M. (2020). Xylitol acts as an anticancer monosaccharide to induce selective cancer death via regulation of the glutathione level. Chemico-Biological Interactions, 324, 109085.
- Sahasakul, Y., Angkhasirisap, W., Lam-Ubol, A., Aursalung, A., Sano, D., Takada, K., & Trachootham, D. (2022). Partial Substitution of Glucose with Xylitol Prolongs Survival and Suppresses Cell Proliferation and Glycolysis of Mice Bearing Orthotopic Xenograft of Oral Cancer. Nutrients, 14(10), 2023. [CrossRef]
- Mehnert, H., Förster, H., & Dehmel, K. H. (1969). The effect of intravenous administration of xylitol solutions in normal persons and in patients with liver diseases and diabetes mellitus. In International Symposium on Metabolism, Physiology, and Clinical Use of Pentoses and Pentitols: Hakone, Japan, August 27th–29th, 1967 (pp. 293-302). Springer Berlin Heidelberg.
- Sato, J., Wang, Y. M., & van Eys, J. (1981). Metabolism of xylitol and glucose in rats bearing hepatocellular carcinomas. Cancer Research, 41(8), 3192-3199.
- Yi, E. Y., & Kim, Y. J. (2013). Xylitol inhibits in vitro and in vivo angiogenesis by suppressing the NF-κB and Akt signaling pathways. International Journal of Oncology, 43(1), 315-320.
- Ylikahri, R. H., & Leino, T. (1979). Metabolic interactions of xylitol and ethanol in healthy males. Metabolism: clinical and experimental, 28(1), 25–29. [CrossRef]
- Hutchenson, R. M., Reynolds, V. H., & Touster, O. (1956). The reduction of L-xylulose to xylitol by guinea pig liver mitochondria. The Journal of biological chemistry, 221(2), 697–709.
- Ahuja, V., Macho, M., Ewe, D., Singh, M., Saha, S., & Saurav, K. (2020). Biological and Pharmacological Potential of Xylitol: A Molecular Insight of Unique Metabolism. Foods (Basel, Switzerland), 9(11), 1592. [CrossRef]
- Islam M. S. (2011). Effects of xylitol as a sugar substitute on diabetes-related parameters in nondiabetic rats. Journal of medicinal food, 14(5), 505–511. [CrossRef]
- Wada, T., Sumardika, I. W., Saito, S., Ruma, I. M. W., Kondo, E., Shibukawa, M., & Sakaguchi, M. (2017). Identification of a novel component leading to anti-tumor activity besides the major ingredient cordycepin in Cordyceps militaris extract. Journal of chromatography. B, Analytical technologies in the biomedical and life sciences, 1061-1062, 209–219. [CrossRef]
- Park, E., Na, H. S., Kim, S. M., Wallet, S., Cha, S., & Chung, J. (2014). Xylitol, an anticaries agent, exhibits potent inhibition of inflammatory responses in human THP-1-derived macrophages infected with Porphyromonas gingivalis. Journal of periodontology, 85(6), e212–e223. [CrossRef]
- Trachootham, D., Chingsuwanrote, P., Yoosadiang, P., Mekkriangkrai, D., Ratchawong, T., Buraphacheep, N., ... & Tuntipopipat, S. (2017). Partial substitution of glucose with xylitol suppressed the glycolysis and selectively inhibited the proliferation of oral cancer cells. Nutrition and cancer, 69(6), 862-872.
- Qusa, M. H., Siddique, A. B., Nazzal, S., & El Sayed, K. A. (2019). Novel olive oil phenolic (−)-oleocanthal (+)-xylitol-based solid dispersion formulations with potent oral anti-breast cancer activities. International journal of pharmaceutics, 569, 118596.
- Ireson, C. R., Alavijeh, M. S., Palmer, A. M., Fowler, E. R., & Jones, H. J. (2019). The role of mouse tumour models in the discovery and development of anticancer drugs. British journal of cancer, 121(2), 101-108.
- Rinschen, M. M., Ivanisevic, J., Giera, M., & Siuzdak, G. (2019). Identification of bioactive metabolites using activity metabolomics. Nature reviews. Molecular cell biology, 20(6), 353–367. [CrossRef]
- Vander Heiden, M. G., & DeBerardinis, R. J. (2017). Understanding the Intersections between Metabolism and Cancer Biology. Cell, 168(4), 657–669. [CrossRef]
- Vernieri, C., Casola, S., Foiani, M., Pietrantonio, F., de Braud, F., & Longo, V. (2016). Targeting Cancer Metabolism: Dietary and Pharmacologic Interventions. Cancer discovery, 6(12), 1315–1333. [CrossRef]
- Schmidt, DR, Patel, R, Kirsch, DG, Lewis, CA, Vander Heiden, MG, Locasale, JW. Metabolomics in cancer research and emerging applications in clinical oncology. CA Cancer J Clin. 2021. [CrossRef]
- Ylikahri R. (1979). Metabolic and nutritional aspects of xylitol. Advances in food research, 25, 159–180. [CrossRef]
- DeBerardinis RJ, Chandel NS. We need to talk about the Warburg effect. Nat Metab. 2020 Feb;2(2):127-129. [CrossRef] [PubMed]
- Cortinovis, C., & Caloni, F. (2016). Household Food Items Toxic to Dogs and Cats. Frontiers in veterinary science, 3, 26. [CrossRef]
- Iannotti, L. L., Gyimah, E. A., Reid, M., Chapnick, M., Cartmill, M. K., Lutter, C. K., Hilton, C., Gildner, T. E., & Quinn, E. A. (2022). Child dietary patterns in Homo sapiens evolution: A systematic review. Evolution, medicine, and public health, 10(1), 371–390. [CrossRef]
- Marlowe, F. W., & Berbesque, J. C. (2009). Tubers as fallback foods and their impact on Hadza hunter-gatherers. American journal of physical anthropology, 140(4), 751–758. [CrossRef]
- Olm, M. R., Dahan, D., Carter, M. M., Merrill, B. D., Yu, F. B., Jain, S., Meng, X., Tripathi, S., Wastyk, H., Neff, N., Holmes, S., Sonnenburg, E. D., Jha, A. R., & Sonnenburg, J. L. (2022). Robust variation in infant gut microbiome assembly across a spectrum of lifestyles. Science (New York, N.Y.), 376(6598), 1220–1223. [CrossRef]
- De Filippo, C., Cavalieri, D., Di Paola, M., Ramazzotti, M., Poullet, J. B., Massart, S., Collini, S., Pieraccini, G., & Lionetti, P. (2010). Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proceedings of the National Academy of Sciences of the United States of America, 107(33), 14691–14696. [CrossRef]
- Marean C. W. (2010). When the sea saved humanity. Scientific American, 303(2), 54–61. [CrossRef]
- Trachootham, D., Alexandre, J., & Huang, P. (2009). Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach?. Nature reviews. Drug discovery, 8(7), 579–591. [CrossRef]
- Niu, B., Liao, K., Zhou, Y., Wen, T., Quan, G., Pan, X., & Wu, C. (2021). Application of glutathione depletion in cancer therapy: Enhanced ROS-based therapy, ferroptosis, and chemotherapy. Biomaterials, 277, 121110. [CrossRef]
- Wen, Y., Chen, H., Zhang, L., Wu, M., Zhang, F., Yang, D., Shen, J., & Chen, J. (2021). Glycyrrhetinic acid induces oxidative/nitrative stress and drives ferroptosis through activating NADPH oxidases and iNOS, and depriving glutathione in triple-negative breast cancer cells. Free radical biology & medicine, 173, 41–51. [CrossRef]
- Hellstrand, K., Brune, M., Naredi, P., Mellqvist, U. H., Hansson, M., Gehlsen, K. R., & Hermodsson, S. (2000). Histamine: a novel approach to cancer immunotherapy. Cancer investigation, 18(4), 347–355. [CrossRef]
- Stoyanov, E., Uddin, M., Mankuta, D., Dubinett, S. M., & Levi-Schaffer, F. (2012). Mast cells and histamine enhance the proliferation of non-small cell lung cancer cells. Lung cancer (Amsterdam, Netherlands), 75(1), 38–44. [CrossRef]
- Chakrabarty, R. P., & Chandel, N. S. (2021). Mitochondria as Signaling Organelles Control Mammalian Stem Cell Fate. Cell stem cell, 28(3), 394–408. [CrossRef]
- Simonsen, T. G., Gaustad, J. V., Leinaas, M. N., & Rofstad, E. K. (2012). High interstitial fluid pressure is associated with tumor-line specific vascular abnormalities in human melanoma xenografts. PloS one, 7(6), e40006. [CrossRef]
- Shin, G. R., Kim, H. E., Kim, J. H., Choi, S., & Kim, M. S. (2021). Advances in Injectable In Situ-Forming Hydrogels for Intratumoral Treatment. Pharmaceutics, 13(11), 1953. [CrossRef]
- Gould, H. J., 3rd, & Paul, D. (2022). Targeted Osmotic Lysis: A Novel Approach to Targeted Cancer Therapies. Biomedicines, 10(4), 838. [CrossRef]
- Liu, Y. X., Liu, W. J., Zhang, H. R., & Zhang, Z. W. (2018). Delivery of bevacizumab by intracranial injection: assessment in glioma model. OncoTargets and therapy, 11, 2673–2683. [CrossRef]
- Algrafi, A. S., Jamal, A. A., & Ismaeel, D. M. (2023). Microbiota as a New Target in Cancer Pathogenesis and Treatment. Cureus, 15(10), e47072. [CrossRef]
- Wu, H. J., & Wu, E. (2012). The role of gut microbiota in immune homeostasis and autoimmunity. Gut microbes, 3(1), 4–14. [CrossRef]
- Halley, A., Leonetti, A., Gregori, A., Tiseo, M., Deng, D. M., Giovannetti, E., & Peters, G. J. (2020). The Role of the Microbiome in Cancer and Therapy Efficacy: Focus on Lung Cancer. Anticancer research, 40(9), 4807–4818. [CrossRef]
- Zuo, Q. L., Cai, X., Zheng, X. Y., Chen, D. S., Li, M., Liu, Z. Q., Chen, K. Q., Han, F. F., & Zhu, X. (2021). Influences of Xylitol Consumption at Different Dosages on Intestinal Tissues and Gut Microbiota in Rats. Journal of agricultural and food chemistry, 69(40), 12002–12011. [CrossRef]
- Xiang, S., Ye, K., Li, M., Ying, J., Wang, H., Han, J., Shi, L., Xiao, J., Shen, Y., Feng, X., Bao, X., Zheng, Y., Ge, Y., Zhang, Y., Liu, C., Chen, J., Chen, Y., Tian, S., & Zhu, X. (2021). Xylitol enhances synthesis of propionate in the colon via cross-feeding of gut microbiota. Microbiome, 9(1), 62. [CrossRef]
- Koppel, N., Maini Rekdal, V., & Balskus, E. P. (2017). Chemical transformation of xenobiotics by the human gut microbiota. Science (New York, N.Y.), 356(6344), eaag2770. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).