1. Introduction
Poikilodermatous plaque-like hemangioma (PPH) is a recently delineated clinical-pathological entity, with only 18 reported cases in the literature [
1,
2,
3]. PPH is characterized by consistent clinical and histological findings replicated across all cases. Clinically, it is characterized by a plaque-like lesion, atrophic and erythematous, commonly on the lower limbs of males over 50 years. Histologically, there is a diffuse proliferation of thin-walled vessels in the dermis, accompanied by epidermal changes. PPH tends to persist over time with indolent behaviour, but data about long term follow-up are scarce. Understanding PPH is crucial to differentiate it from more consequential lesions, thereby avoiding unnecessary procedures. Here, we present a new case of PPH and provide a comprehensive review of the available literature.
2. Case Report
An 81-year-old male presented with a lesion on the left buttock persisting for the last 2 years, displaying gradual growth. He did not associate it with any treatment, trauma, insect bites or recent foreign travel. Occasional bleeding was reported, unaccompanied by other symptoms. The patient had a medical history of type 2 diabetes treated with sitagliptin, hyperuricemia treated with allopurinol and atrial fibrillation managed with acenocoumarol. No recent changes in medication were noted.
Clinical examination revealed a poikilodermatous, infiltrated erythematous plaque measuring 6 x 4 cm on the left gluteus with marked scaling (
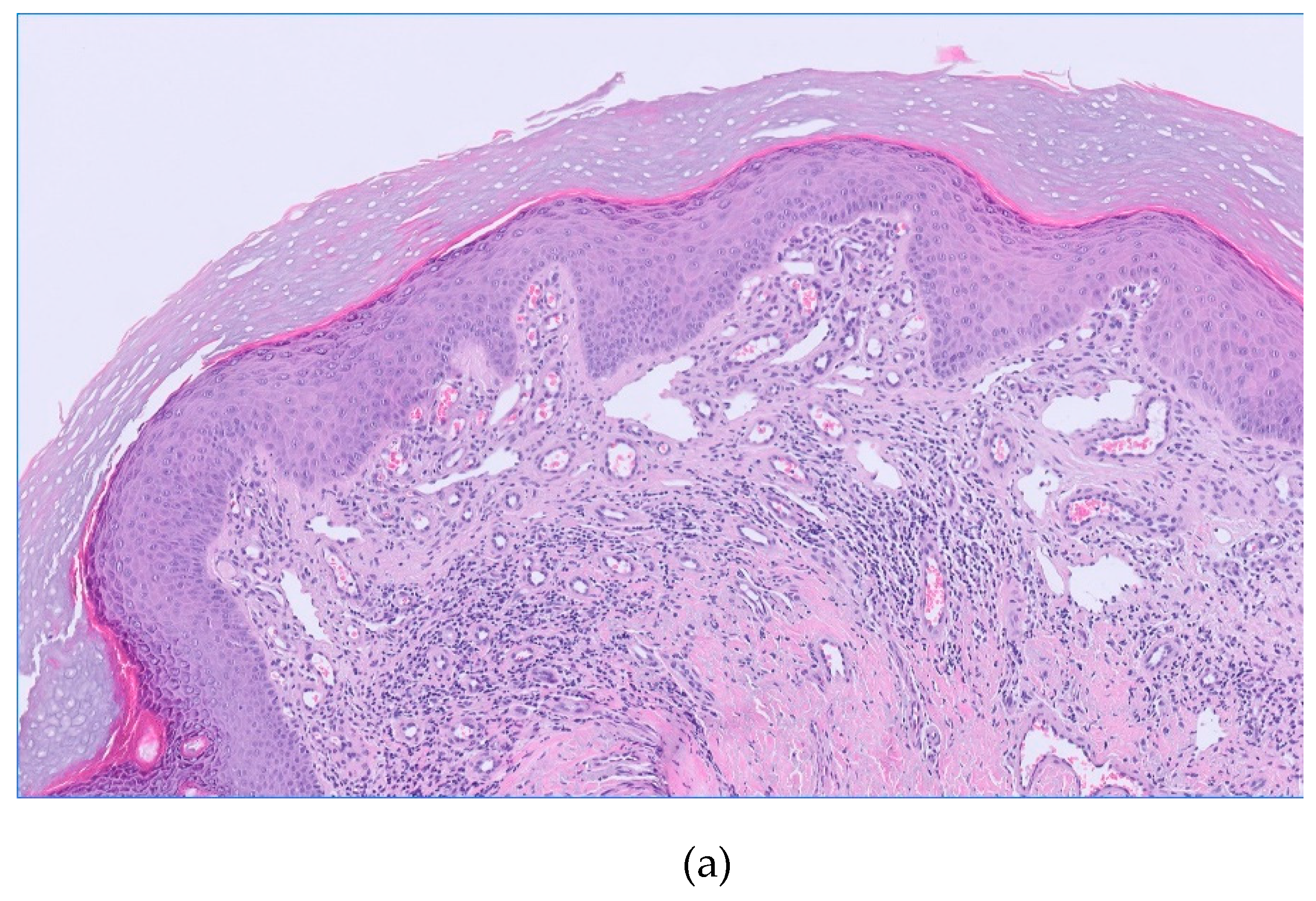
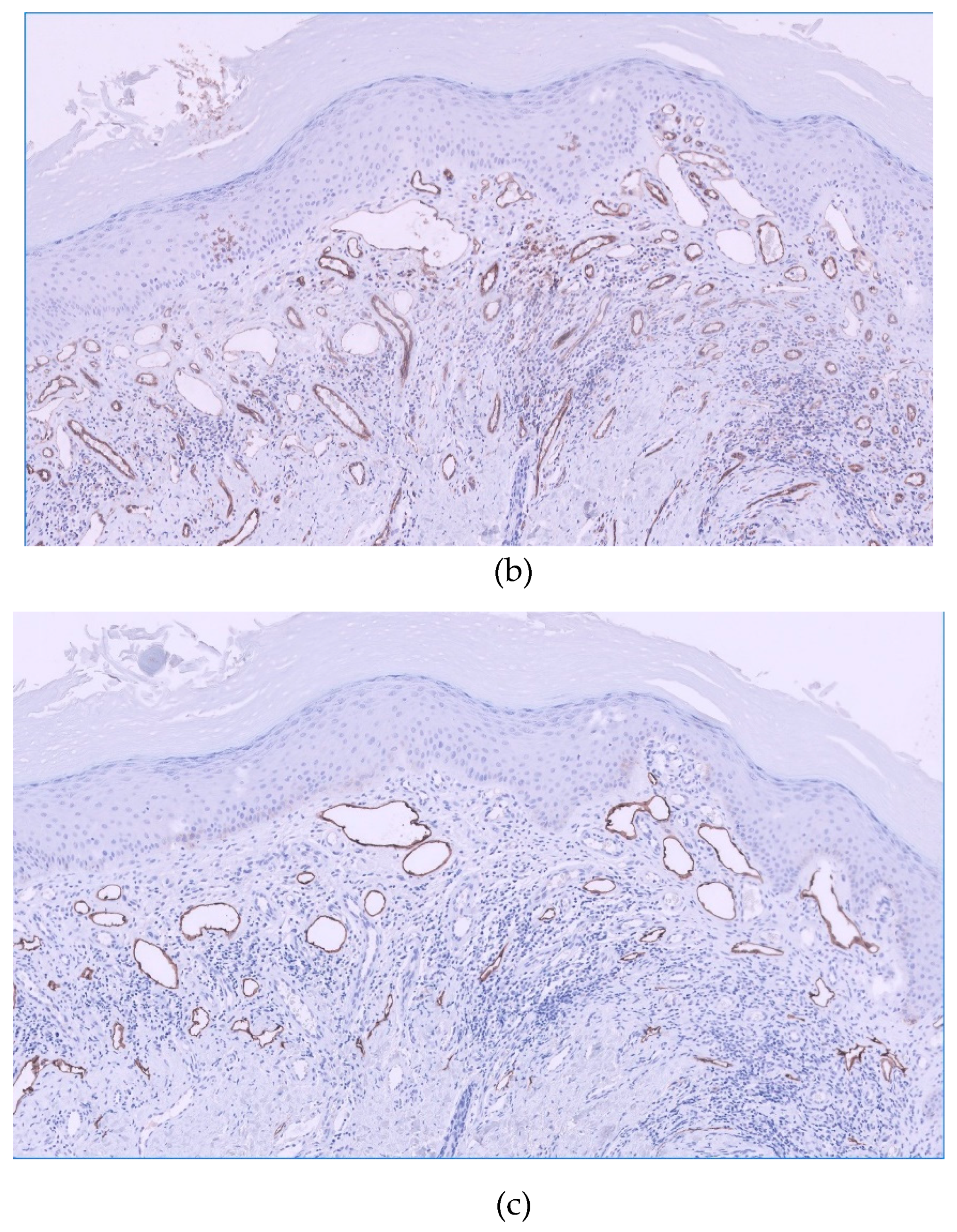
Figure 1). No other lesions were observed. An incisional biopsy, initially suspected as Bowen's disease, revealed orthokeratotic hyperkeratosis and a striking proliferation of microvasculature and vasodilation in the superficial dermis, consistent with PPH (
Figure 2a). Immune CD31 stain confirm vascular origin (
Figure 2b) and D2-40 was negative in the primary vascular proliferation, but positive in background lymphatics (
Figure 2c). No keratinocytic atypia or other suspicious features of malignancy were observed.
Barrier cream therapy was initiated. Over 26 months of follow-up, the lesion stabilized, with no more reported episodes of bleeding or associated symptoms. Reduction in erythema, scaling and infiltration was evident (
Figure 3).
3. Discussion
PPH was described in 2019 in a paper that collected 16 cases from United Kingdom patients [
1]. Since then two more cases have been reported [
2,
3]. The case we present would therefore be number 19. Male involvement predominates (17/19, 89.4%) in all cases. The reported age range is from 58 to 90 years, with a mean age of 72.9 years considering our case.
Clinically, it presents as a solitary plaque several cm in greatest diameter (range 2 to 7 cm) and erythematous to violaceous in color. Two patients have been reported with more than one lesion (2/19, 10.6%) [
1]. The lesions are mostly described as atrophic in appearance, however, they are not usually described as clinically scaly as in our patient, although epidermal changes, including hyperkeratosis and parakeratosis, are characteristic findings on histological examination. This scaly appearance is what led us to make the diagnosis of squamous cell carcinoma in situ, despite not being in a photoexposed area [
4]. The most frequently described sites are the lower limbs, mainly the hip, thigh and calf, although there is one case of involvement of the shoulder, which had two more lesions on the hip and buttocks [
1]. The lesions described to date were asymptomatic and indolent, however, our case presented occasional episodes of bleeding, although without associated pain or pruritus. These episodes occurred in the first months, when the lesion was in the establishment phase and had more scaling. We think that this may be related to the significant scaling that was present, as the scale peeled off may have caused damage to the underlying skin which could have led to the bleeding.
Histopathologically, PPH has constant features clearly described by Semkova et al.[
1]. All cases described to date show a dermal vascular band-like proliferation of thin-walled vessels. The endothelial cells of these vessels lack atypical features and mitotic figures. Epidermal changes are also present. Hyperkeratosis is the most constant finding and is also present in our case. Focal parakeratosis, acanthosis, hypergranulosis, spongiosis, lymphocyte exocytosis and interphase vacuolar dermatitis have also been described. In addition, dermal changes such as fibrosis and edema have been associated. In most cases, interstitial or perivascular lymphohistiocytic infiltrate was reported, as in our case, with no evidence of lymphocyte atypicality. Furthermore, elastic fibers are reduced or absent in the affected dermis.
The etiology of PPH remains unknown, with proposed triggers such as arthropod bites or trauma unconfirmed. Most cases have been reported in Northern England, suggesting possible environmental or infectious factors [
1]. Frequent occurrence on lower limbs, particularly in pressure-prone areas, could imply a role of sustained trauma or pressure in the etiology. Likewise, the peripheral distribution of subcutaneous fat in women provides protection against pressure and trauma and, therefore, this could be the reason why mainly men are affected [
5]. In addition, the fact that older patients are mainly affected may be related to the increased sedentary lifestyle in this age group, and therefore continuous pressure, and loss of fat pad in pressure areas [
6]. The observed reduction in erythema and bleeding with barrier creams in our case supports this hypothesis.
However, factors other than purely mechanical ones must be involved. There are many older patients with sedentary lifestyles [
7], but PPH is an extremely rare diagnosis. On the other hand, we think that this entity may be underdiagnosed, given the indolent course and the localization in generally covered and inconspicuous areas.
Being a recently described entity, there is limited information about the natural history of PPH, especially in the long term. The longest reported follow-up is 6 years. It exhibits an initial phase of gradual growth, accompanied in our case by significant hyperkeratosis and bleeding episodes, followed by a stabilization phase where lesion growth ceases [
1,
2,
3]. Subsequently, the lesion persists, with no reported cases of regression. In our case, a reduction in erythema and scaling post-stabilization may be related to treatment or the natural course of the condition. Establishing hypotheses is challenging due to the scarcity of cases for comparison.
The treatments used in the cases described are topical corticosteroids, oral corticosteroids, topical calcineurin inhibitors and topical antifungals, none of which have been effective in changing the course of the disease [
1,
3]. The wait-and-see approach has been proposed as the most appropriate in this entity, given the indolent course [
2]. Future research should explore emerging therapies and long-term outcomes.
4. Conclusions
We report a new case of PPH. This case underscores the importance of recognizing PPH, a rare but persistent benign entity. Understanding its clinical and histological features is crucial for differentiation from more concerning lesions. Continued reporting and analysis of cases are essential to enrich our understanding of this PPH and establishing effective treatments.
Author Contributions
Conceptualization, F.V.M.; methodology, P.D.C..; investigation, P.D.C., F.V.M. and F.M.R.P..; resources, F.M.R.P.; writing—original draft preparation, P.D.C.; writing—review and editing, F.V.M. and S.A.S.; visualization, F.M.R.P.; supervision, S.A.S.; project administration, S.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Semkova, K.; Carr, R.; Grainger, M.; Green, R.; Hafejee, A.; Makrygeorgou, A.; Melly, L.; Motta, L.; Newsham, J.; Owen, C.; Sillars, J.; Taibjee, S.; Calonje, E. Poikilodermatous plaque-like hemangioma: Case series of a newly defined entity. J Am Acad Dermatol. 2019, 81, 1257–1270. [Google Scholar] [CrossRef]
- Sullivan, M. , Hartman, R., Mahalingam, M. Poikilodermatous plaque-like hemangioma: A benign vasoformative entity with reproducible histopathologic and clinical features. J Cutan Pathol. [CrossRef]
- Salgüero Fernández, I. , Hospital Gil, M., Nájera Botello, L., Roustan Gullón, G. Not All Is Infantile Hemangioma: An Erythematous Plaque in an Adult. Actas Dermosifiliogr. [CrossRef]
- Que, S.K.T. , Zwald, F.O., Schmults, C.D. Cutaneous squamous cell carcinoma: Incidence, risk factors, diagnosis, and staging. J Am Acad Dermatol. [CrossRef]
- Williams, M.J. , Hunter, G.R., Kekes-Szabo, T., Snyder, S., Treuth, M.S. Regional fat distribution in women and risk of cardiovascular disease. Am J Clin Nutr. 1997, 65, 855–60. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, E. , Blume-Peytavi, U., Trojahn, C., Kottner, J. Associations between skin barrier characteristics, skin conditions and health of aged nursing home residents: a multi-center prevalence and correlational study. BMC Geriatr. [CrossRef]
- Hahnel, E. , Lichterfeld, A., Blume-Peytavi, U., Kottner, J. The epidemiology of skin conditions in the aged: A systematic review. J Tissue Viability. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).