Submitted:
04 May 2024
Posted:
06 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Inclusion/Exclusion Criteria
2.3. Data Extraction
2.4. Methodological Quality Evaluation
3. Results
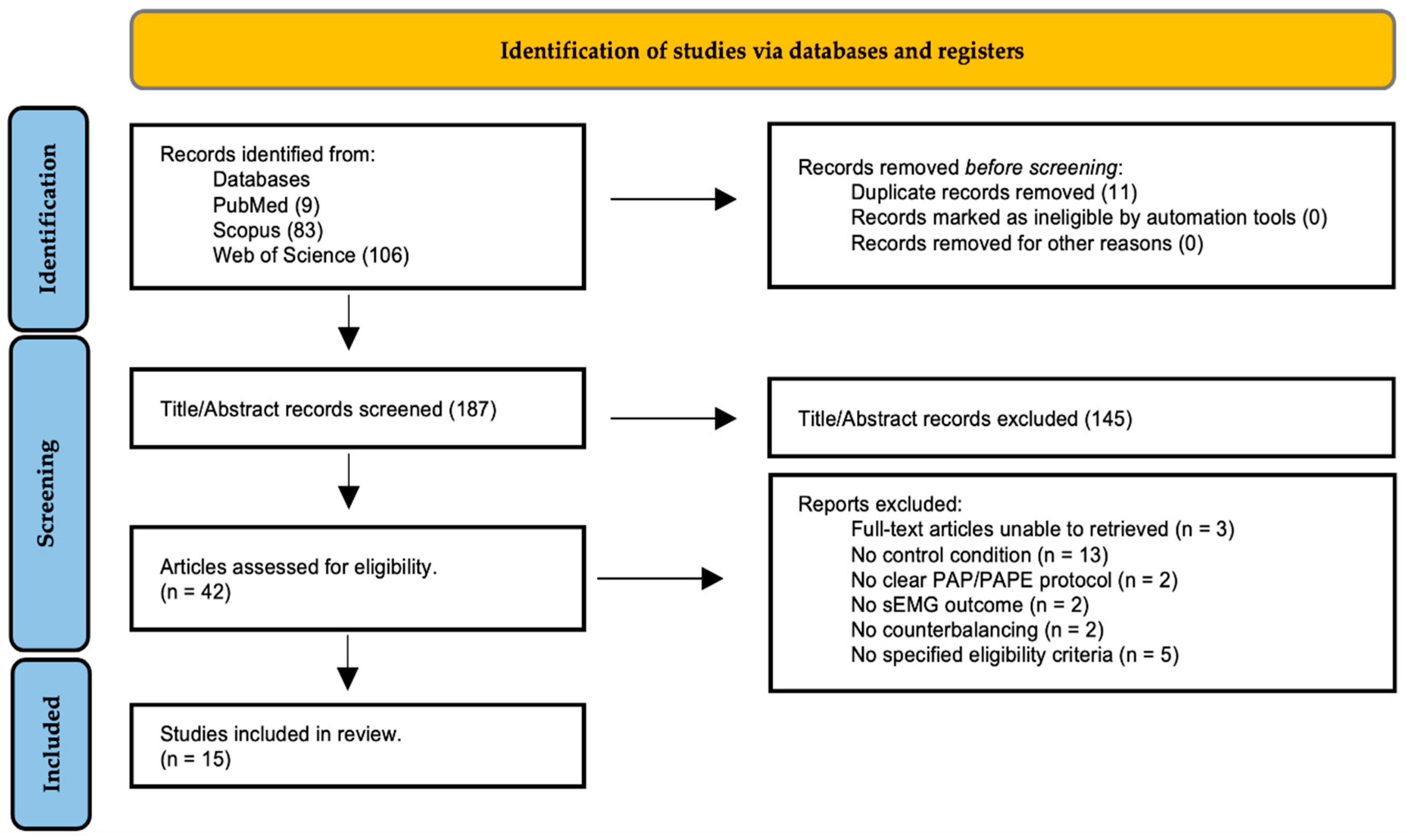
3.1. Study Selection and Results of Literature Retrieval
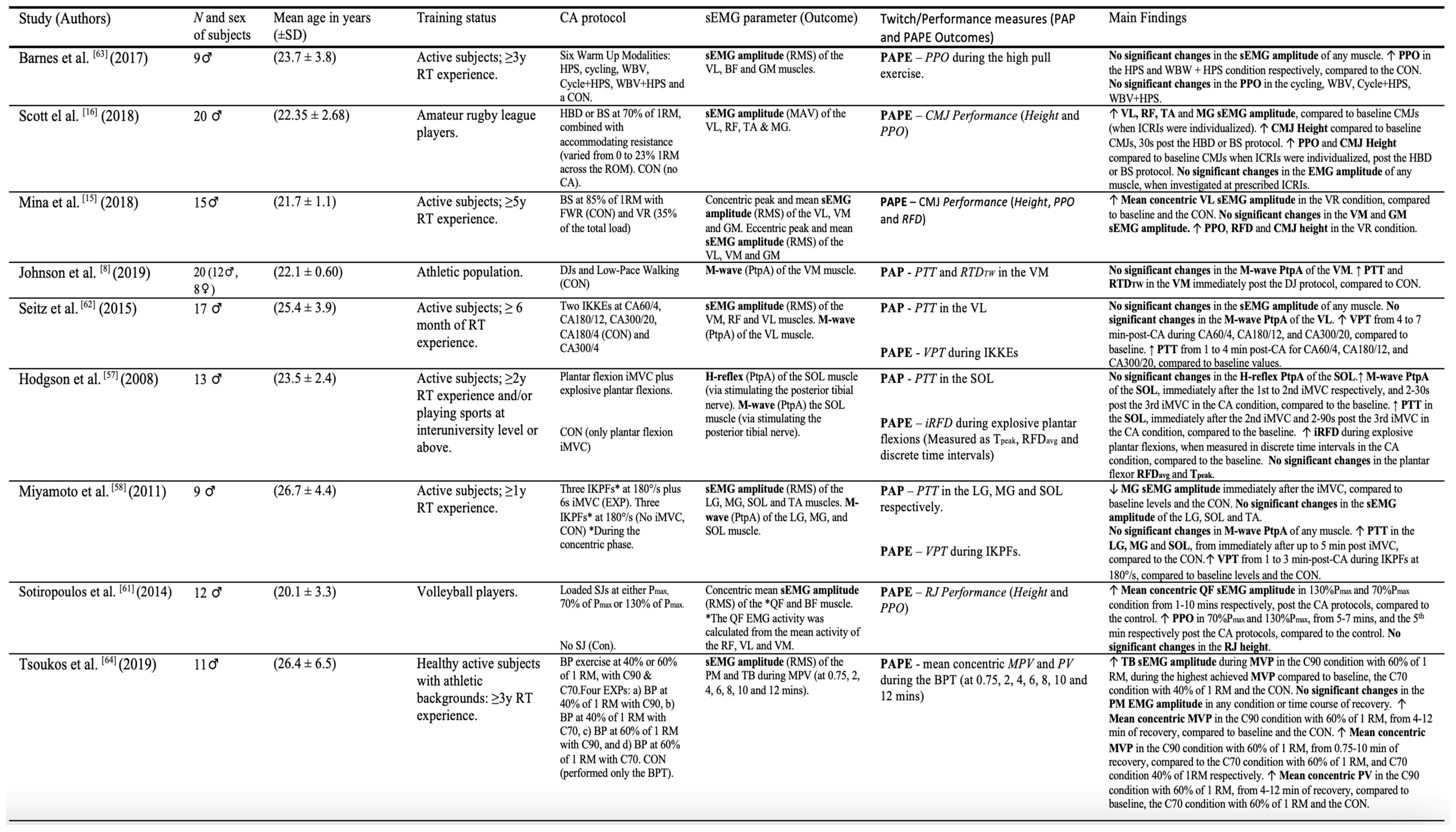
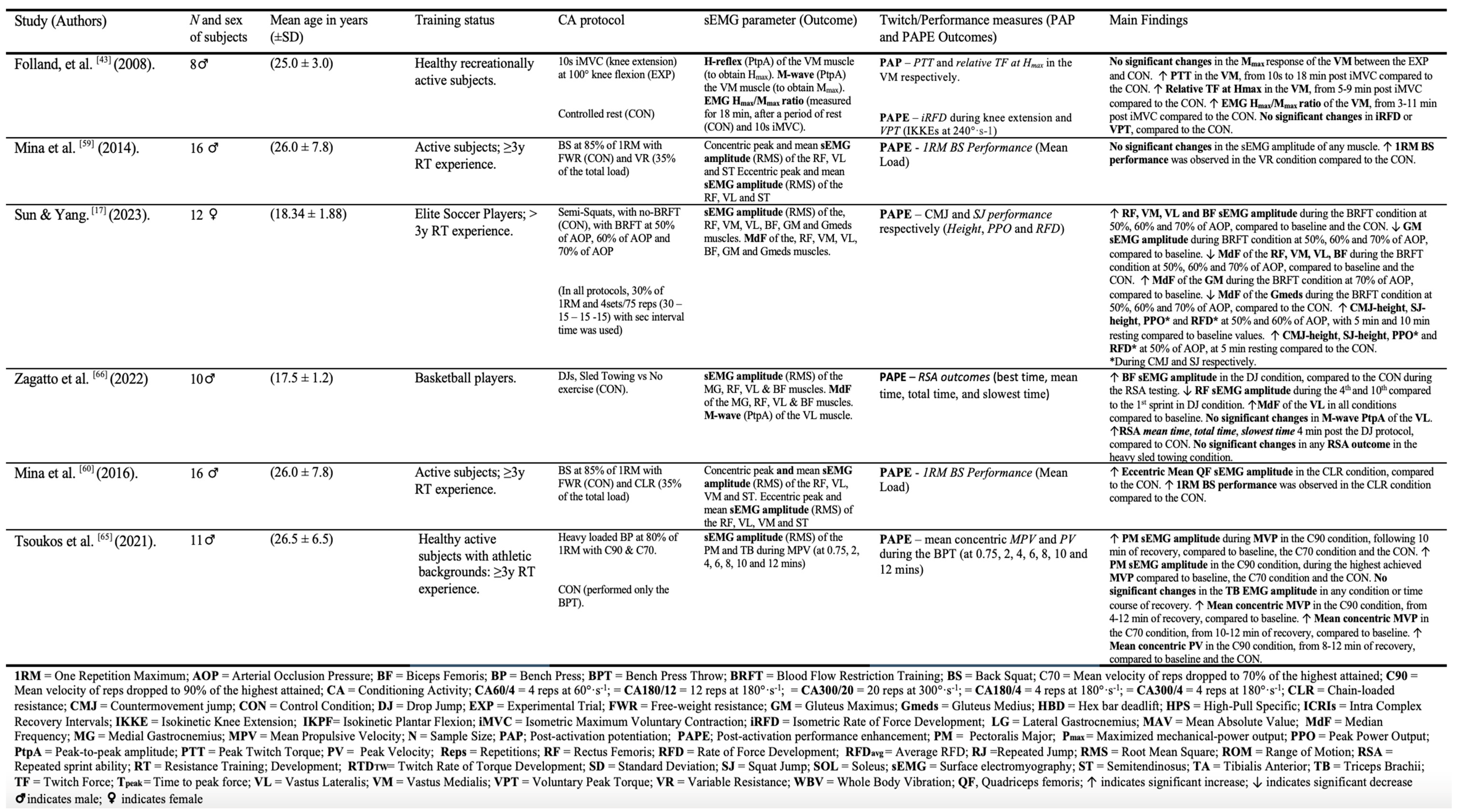
3.2. Characteristics of Studies Included.
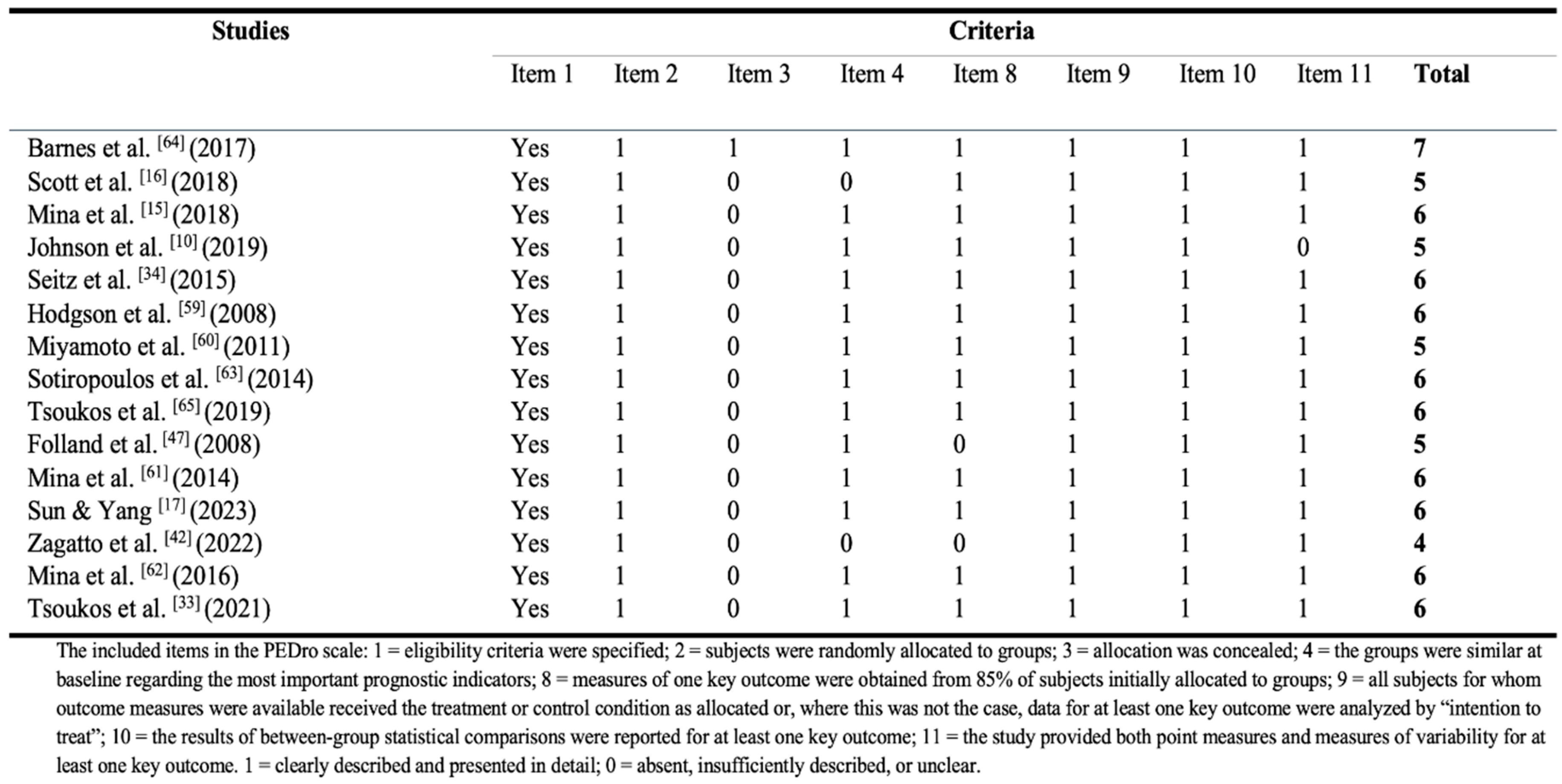
3.3. Quality of the Studies (Risk of Bias)
3.4. Synthesis of Results
- Changes in sEMG parameters and twitch/performance outcomes between different CA protocols were examined. The evidence was summarized for conditions were sEMG parameters indicative of acute improvements in twitch/performance outcomes (PAP and PAPE respectively) in healthy athletic adults, but also incidents where they were deemed as unrelated.
3.4.1. The sEMG Amplitude (RMS and MAV) and PAP/PAPE
3.4.2. The MdF and PAP/PAPE
3.4.3. The M-Wave and PAP/PAPE
3.4.4. The H-Reflex and PAP/PAPE
3.4.5. The EMG Hmax/Mmax Ratio and PAP/PAPE
4. Discussion
4.1. Limitations and Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Safran, M.R.; Garrett, W.E.; Seaber, A.V.; Glisson, R.R.; Ribbeck, B.M. The role of warmup in muscular injury prevention. Am. J. Sports Med. 1988, 16, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Noonan, T.J.; Best, T.M.; Seaber, A.V.; Garrett, W.E. Thermal effects on skeletal muscle tensile behavior. Am. J. Sports Med. 1993, 21, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Shellock, F.G.; Prentice, W.E. Warming-Up and Stretching for Improved Physical Performance and Prevention of Sports-Related Injuries. Sports Med. 1985, 2, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Chang, C.-K.; Tseng, W.-C.; Chiu, C.-H.; Dai, X.; Ye, X. Acute Effects of Different Warm-up Protocols on Sports Performance in Elite Male Collegiate Handball Players. J. Strength Cond. Res. 2022, 36, 2262–2267. [Google Scholar] [CrossRef] [PubMed]
- McGowan, C.J.; Pyne, D.B.; Thompson, K.G.; Rattray, B. Warm-Up Strategies for Sport and Exercise: Mechanisms and Applications. Sports Med. Auckl. NZ 2015, 45, 1523–1546. [Google Scholar] [CrossRef] [PubMed]
- Blazevich, A.J.; Babault, N. Post-activation Potentiation Versus Post-activation Performance Enhancement in Humans: Historical Perspective, Underlying Mechanisms, and Current Issues. Front. Physiol. 2019, 10, 1359. [Google Scholar] [CrossRef]
- Hamada, T.; Sale, D.G.; MacDougall, J.D.; Tarnopolsky, M.A. Postactivation potentiation, fiber type, and twitch contraction time in human knee extensor muscles. J. Appl. Physiol. 2000, 88, 2131–2137. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, H.B.; MacIntosh, B.R.; Dal Pupo, J. Does postactivation potentiation (PAP) increase voluntary performance? Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metab. 2020, 45, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Gago, P.; Zoellner, A.; Cézar Lima da Silva, J.; Ekblom, M.M. Post Activation Potentiation and Concentric Contraction Performance: Effects on Rate of Torque Development, Neuromuscular Efficiency, and Tensile Properties. J. Strength Cond. Res. 2020, 34, 1600–1608. [Google Scholar] [CrossRef]
- Johnson, M.; Baudin, P.; Ley, A.L.; Collins, D.F. A Warm-Up Routine That Incorporates a Plyometric Protocol Potentiates the Force-Generating Capacity of the Quadriceps Muscles. J. Strength Cond. Res. 2019, 33, 380–389. [Google Scholar] [CrossRef]
- Zhi, G.; Ryder, J.W.; Huang, J.; Ding, P.; Chen, Y.; Zhao, Y.; Kamm, K.E.; Stull, J.T. Myosin light chain kinase and myosin phosphorylation effect frequency-dependent potentiation of skeletal muscle contraction. Proc. Natl. Acad. Sci. USA 2005, 102, 17519–17524. [Google Scholar] [CrossRef]
- Stull, J.T.; Kamm, K.E.; Vandenboom, R. Myosin light chain kinase and the role of myosin light chain phosphorylation in skeletal muscle. Arch. Biochem. Biophys. 2011, 510, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.; Dantzig, J.A.; Hollingworth, S.; Baylor, S.M.; Goldman, Y.E.; Mitchison, T.J.; Straight, A.F. A small-molecule inhibitor of skeletal muscle myosin II. Nat. Cell Biol. 2002, 4, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Maloney, S.J.; Turner, A.N.; Fletcher, I.M. Ballistic Exercise as a Pre-Activation Stimulus: A Review of the Literature and Practical Applications. Sports Med. 2014, 44, 1347–1359. [Google Scholar] [CrossRef] [PubMed]
- Mina, M.A.; Blazevich, A.J.; Tsatalas, T.; Giakas, G.; Seitz, L.B.; Kay, A.D. Variable, but not free-weight, resistance back squat exercise potentiates jump performance following a comprehensive task-specific warm-up. Scand. J. Med. Sci. Sports 2018, sms.13341. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.J.; Ditroilo, M.; Marshall, P. Effect of Accommodating Resistance on the Postactivation Potentiation Response in Rugby League Players. J. Strength Cond. Res. 2018, 32, 2510–2520. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Yang, T. Semi-Squat Exercises with Varying Levels of Arterial Occlusion Pressure during Blood Flow Restriction Training Induce a Post-Activation Performance Enhancement and Improve Vertical Height Jump in Female Football Players. J. Sports Sci. Med. 2023, 212–225. [Google Scholar] [CrossRef]
- Wyland, T.P.; Van Dorin, J.D.; Reyes, G.F.C. Postactivation Potentation Effects From Accommodating Resistance Combined With Heavy Back Squats on Short Sprint Performance. J. Strength Cond. Res. 2015, 29, 3115–3123. [Google Scholar] [CrossRef]
- Andersen, E.; Lockie, R.G.; Dawes, J.J. Relationship of Absolute and Relative Lower-Body Strength to Predictors of Athletic Performance in Collegiate Women Soccer Players. Sports (Basel) 2018, 6, 106. [Google Scholar] [CrossRef]
- Gossen, E.R.; Sale, D.G. Effect of postactivation potentiation on dynamic knee extension performance. Eur. J. Appl. Physiol. 2000, 83, 524–530. [Google Scholar] [CrossRef]
- Pearson, S.J.; Hussain, S.R. Lack of association between postactivation potentiation and subsequent jump performance. Eur. J. Sport Sci. 2014, 14, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Leavitt, V.M.; DeLuca, J. Central fatigue: issues related to cognition, mood and behavior, and psychiatric diagnoses. PM R 2010, 2, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, A.; Behan, P.O. Fatigue and basal ganglia. J. Neurol. Sci. 2000, 179, 34–42. [Google Scholar] [CrossRef]
- Taylor, J.L.; Amann, M.; Duchateau, J.; Meeusen, R.; Rice, C.L. Neural Contributions to Muscle Fatigue: From the Brain to the Muscle and Back Again. Med. Sci. Sports Exerc. 2016, 48, 2294–2306. [Google Scholar] [CrossRef] [PubMed]
- Schillings, M.L.; Hoefsloot, W.; Stegeman, D.F.; Zwarts, M.J. Relative contributions of central and peripheral factors to fatigue during a maximal sustained effort. Eur. J. Appl. Physiol. 2003, 90, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Neyroud, D.; Cheng, A.J.; Bourdillon, N.; Kayser, B.; Place, N.; Westerblad, H. Muscle Fatigue Affects the Interpolated Twitch Technique When Assessed Using Electrically-Induced Contractions in Human and Rat Muscles. Front. Physiol. 2016, 7, 252. [Google Scholar] [CrossRef] [PubMed]
- Gandevia, S.C. Spinal and supraspinal factors in human muscle fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef]
- Zhang, Q.; Iyer, A.; Lambeth, K.; Kim, K.; Sharma, N. Ultrasound Echogenicity as an Indicator of Muscle Fatigue during Functional Electrical Stimulation. Sensors 2022, 22, 335. [Google Scholar] [CrossRef]
- Guilherme H., Elcadi; Forsman, M.; Crenshaw, A.G. The relationship between oxygenation and myoelectric activity in the forearm and shoulder muscles of males and females. Eur. J. Appl. Physiol. 2011, 111, 647–658. [Google Scholar] [CrossRef]
- Toro, S.F.D.; Santos-Cuadros, S.; Olmeda, E.; Álvarez-Caldas, C.; Díaz, V.; San Román, J.L. Is the Use of a Low-Cost sEMG Sensor Valid to Measure Muscle Fatigue? Sensors 2019, 19, 3204. [Google Scholar] [CrossRef]
- Scano, A.; Pirovano, I.; Manunza, M.E.; Spinelli, L.; Contini, D.; Torricelli, A.; Re, R. Sustained fatigue assessment during isometric exercises with time-domain near infrared spectroscopy and surface electromyography signals. Biomed. Opt. Express 2020, 11, 7357–7375. [Google Scholar] [CrossRef] [PubMed]
- Ament, W.; Bonga, G.J.; Hof, A.L.; Verkerke, G.J. EMG median power frequency in an exhausting exercise. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 1993, 3, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Tsoukos, A.; Brown, L.E.; Terzis, G.; Veligekas, P.; Bogdanis, G.C. Potentiation of Bench Press Throw Performance Using a Heavy Load and Velocity-Based Repetition Control. J. Strength Cond. Res. 2021, 35, S72–S79. [Google Scholar] [CrossRef] [PubMed]
- Seitz, L.B.; Trajano, G.S.; Dal Maso, F.; Haff, G.G.; Blazevich, A.J. Postactivation potentiation during voluntary contractions after continued knee extensor task-specific practice. Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metab. 2015, 40, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Johnson, P.W. Fatigue development in the finger flexor muscle differs between keyboard and mouse use. Eur. J. Appl. Physiol. 2014, 114, 2469–2482. [Google Scholar] [CrossRef] [PubMed]
- Chiu, L.Z.F.; Fry, A.C.; Weiss, L.W.; Schilling, B.K.; Brown, L.E.; Smith, S.L. Postactivation Potentiation Response in Athletic and Recreationally Trained Individuals. J. Strength Cond. Res. 2003, 17, 671. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.M.; Duncan, N.M.; Marin, P.J.; Brown, L.E.; Loenneke, J.P.; Wilson, S.M.C.; Jo, E.; Lowery, R.P.; Ugrinowitsch, C. Meta-Analysis of Postactivation Potentiation and Power: Effects of Conditioning Activity, Volume, Gender, Rest Periods, and Training Status. J. Strength Cond. Res. 2013, 27, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Seitz, L.B.; Trajano, G.S.; Haff, G.G.; Dumke, C.C.L.S.; Tufano, J.J.; Blazevich, A.J. Relationships between maximal strength, muscle size, and myosin heavy chain isoform composition and postactivation potentiation. Appl. Physiol. Nutr. Metab. 2016, 41, 491–497. [Google Scholar] [CrossRef]
- Baudry, S.; Duchateau, J. Postactivation potentiation in a human muscle: effect on the rate of torque development of tetanic and voluntary isometric contractions. J. Appl. Physiol. Bethesda Md 1985 2007, 102, 1394–1401. [Google Scholar] [CrossRef]
- Vargas, L.; Baratta, J.; Hu, X. Distribution of M-Wave and H-Reflex in Hand Muscles Evoked via Transcutaneous Nerve Stimulation: A Preliminary Report. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. IEEE Eng. Med. Biol. Soc. Annu. Int. Conf. 2021, 2021, 5897–5900. [Google Scholar] [CrossRef]
- Fukutani, A.; Miyamoto, N.; Kanehisa, H.; Yanai, T.; Kawakami, Y. Influence of the intensity of a conditioning contraction on the subsequent twitch torque and maximal voluntary concentric torque. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2012, 22, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Zagatto, A.M.; Claus, G.M.; Dutra, Y.M.; De Poli, R.A.; Lopes, V.H.F.; Goodall, S.; Loturco, I.; Boullosa, D. Drop jumps versus sled towing and their effects on repeated sprint ability in young basketball players. BMC Sports Sci. Med. Rehabil. 2022, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Maffiuletti, N.A.; Martin, A.; Babault, N.; Pensini, M.; Lucas, B.; Schieppati, M. Electrical and mechanical H(max)-to-M(max) ratio in power- and endurance-trained athletes. J. Appl. Physiol. (1985) 2001, 90, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.L.; Stull, J.T. Myosin light chain phosphorylation in fast and slow skeletal muscles in situ. Am. J. Physiol. 1984, 247, C462–471. [Google Scholar] [CrossRef] [PubMed]
- Inns, T.B.; McCormick, D.; Greig, C.A.; Atherton, P.J.; Phillips, B.E.; Piasecki, M. Factors associated with electrical stimulation-induced performance fatigability are dependent upon stimulation location. Exp. Physiol. 2021, 106, 828–836. [Google Scholar] [CrossRef]
- Rodriguez-Falces, J.; Malanda, A.; Navallas, J.; Place, N. M-wave changes caused by brief voluntary and stimulated isometric contractions. Eur. J. Appl. Physiol. 2023, 123, 2087–2098. [Google Scholar] [CrossRef] [PubMed]
- Folland, J.P.; Wakamatsu, T.; Fimland, M.S. The influence of maximal isometric activity on twitch and H-reflex potentiation, and quadriceps femoris performance. Eur. J. Appl. Physiol. 2008, 104, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, R.M.; Ingersoll, C.D.; Hoffman, M.A. The hoffmann reflex: methodologic considerations and applications for use in sports medicine and athletic training research. J. Athl. Train. 2004, 39, 268–277. [Google Scholar] [PubMed]
- Racinais, S.; Girard, O.; Micallef, J.P.; Perrey, S. Failed excitability of spinal motoneurons induced by prolonged running exercise. J. Neurophysiol. 2007, 97, 596–603. [Google Scholar] [CrossRef]
- McNeil, C.J.; Butler, J.E.; Taylor, J.L.; Gandevia, S.C. Testing the excitability of human motoneurons. Front Hum Neurosci [Internet]. 2013 [cited 2023 Jun 13];7. Available from: http://journal.frontiersin.org/article/10.3389/fnhum.2013.00152/abstract. [CrossRef]
- Bergmann, J.; Kramer, A.; Gruber, M. Repetitive hops induce postactivation potentiation in triceps surae as well as an increase in the jump height of subsequent maximal drop jumps. PloS One 2013, 8, e77705. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Paternoster, F.K. Post-Activation-Performance Enhancement: Possible Contributing Factors. J. Sports Sci. Med. 2024, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Soler, E.; Paredes, X.; Carballeira, E.; Márquez, G.; Fernández-Del-Olmo, M. Effect of intensity and duration of conditioning protocol on post-activation potentiation and changes in H-reflex. Eur. J. Sport Sci. 2011, 11, 33–38. [Google Scholar] [CrossRef]
- Rodriguez-Falces, J.; Duchateau, J.; Muraoka, Y.; Baudry, S. M-wave potentiation after voluntary contractions of different durations and intensities in the tibialis anterior. J. Appl. Physiol. 2015, 118, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Larsson, S.C. Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism 2023, 144, 155533. [Google Scholar] [CrossRef]
- Kupa, E.J.; Roy, S.H.; Kandarian, S.C.; De Luca, C.J. Effects of muscle fiber type and size on EMG median frequency and conduction velocity. J. Appl. Physiol. Bethesda Md 1985 1995, 79, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Gerdle, B.; Karlsson, S.; Crenshaw, A.G.; Elert, J.; Fridén, J. The influences of muscle fibre proportions and areas upon EMG during maximal dynamic knee extensions. Eur. J. Appl. Physiol. 2000, 81, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, n71. [Google Scholar] [CrossRef]
- Coar, J.T.; Sewell, J.P. Zotero: harnessing the power of a personal bibliographic manager. Nurse Educ. 2010, 35, 205–207. [Google Scholar] [CrossRef]
- Hodgson, M.J.; Docherty, D.; Zehr, E.P. Postactivation potentiation of force is independent of h-reflex excitability. Int. J. Sports Physiol. Perform. 2008, 3, 219–231. [Google Scholar] [CrossRef]
- Miyamoto, N.; Kanehisa, H.; Fukunaga, T.; Kawakami, Y. Effect of postactivation potentiation on the maximal voluntary isokinetic concentric torque in humans. J. Strength Cond. Res. 2011, 25, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Mina, M.A.; Blazevich, A.J.; Giakas, G.; Kay, A.D. Influence of variable resistance loading on subsequent free weight maximal back squat performance. J. Strength Cond. Res. 2014, 28, 2988–2995. [Google Scholar] [CrossRef] [PubMed]
- Mina, M.A.; Blazevich, A.J.; Giakas, G.; Seitz, L.B.; Kay, A.D. Chain-loaded variable resistance warm-up improves free-weight maximal back squat performance. Eur. J. Sport Sci. 2016, 16, 932–939. [Google Scholar] [CrossRef]
- Sotiropoulos, K.; Smilios, I.; Douda, H.; Christou, M.; Tokmakidis, S.P. Contrast Loading: Power Output and Rest Interval Effects on Neuromuscular Performance. Int. J. Sports Physiol. Perform. 2014, 9, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.J.; Petterson, A.; Cochrane, D.J. Effects of different warm-up modalities on power output during the high pull. J. Sports Sci. 2017, 35, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Tsoukos, A.; Brown, L.E.; Veligekas, P.; Terzis, G.; Bogdanis, G.C. Postactivation Potentiation of Bench Press Throw Performance Using Velocity-Based Conditioning Protocols with Low and Moderate Loads. J. Hum. Kinet. 2019, 68, 81–98. [Google Scholar] [CrossRef] [PubMed]
- Caterini, D.; Gittings, W.; Huang, J.; Vandenboom, R. The effect of work cycle frequency on the potentiation of dynamic force in mouse fast twitch skeletal muscle. J. Exp. Biol. 2011, 214, 3915–3923. [Google Scholar] [CrossRef] [PubMed]
- Xeni, J.; Gittings, W.B.; Caterini, D.; Huang, J.; Houston, M.E.; Grange, R.W.; Vandenboom, R. Myosin light-chain phosphorylation and potentiation of dynamic function in mouse fast muscle. Pflugers Arch. 2011, 462, 349–358. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Mills, K.R. The relationship between mean power frequency of the EMG spectrum and muscle fibre conduction velocity. Electroencephalogr. Clin. Neurophysiol. 1985, 60, 130–134. [Google Scholar] [CrossRef]
- Komi, P.V.; Tesch, P. EMG frequency spectrum, muscle structure, and fatigue during dynamic contractions in man. Eur. J. Appl. Physiol. 1979, 42, 41–50. [Google Scholar] [CrossRef]
- Beretta-Piccoli, M.; D’Antona, G.; Barbero, M.; Fisher, B.; Dieli-Conwright, C.M.; Clijsen, R.; Cescon, C. Evaluation of central and peripheral fatigue in the quadriceps using fractal dimension and conduction velocity in young females. PloS One 2015, 10, e0123921. [Google Scholar] [CrossRef]
- Linssen, W.H.; Stegeman, D.F.; Joosten, E.M.; Merks, H.J.; ter Laak, H.J.; Binkhorst, R.A.; Notermans, S.L. Force and fatigue in human type I muscle fibres. A surface EMG study in patients with congenital myopathy and type I fibre predominance. Brain J. Neurol. 1991, 114 Pt 5, 2123–2132. [Google Scholar] [CrossRef] [PubMed]
- Bilodeau, M.; Houck, J.; Cuddeford, T.; Sharma, S.; Riley, N. Variations in the relationship between the frequency content of EMG signals and the rate of torque development in voluntary and elicited contractions. J. Electromyogr. Kinesiol. 2002, 12, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.K.; Timothy, G.F.; Yeow, C.H. Comparison of mean frequency and median frequency in evaluating muscle fiber type selection in varying gait speed across healthy young adult individuals. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. IEEE Eng. Med. Biol. Soc. Annu. Int. Conf. 2016, 2016, 1725–1728. [Google Scholar] [CrossRef]
- Bobbert, M.F.; van Ingen Schenau, G.J. Coordination in vertical jumping. J. Biomech. 1988, 21, 249–262. [Google Scholar] [CrossRef] [PubMed]
- McComas, A.J.; Galea, V.; Einhorn, R.W. Pseudofacilitation: a misleading term. Muscle Nerve 1994, 17, 599–607. [Google Scholar] [CrossRef]
- Hicks, A.; Fenton, J.; Garner, S.; McComas, A.J. M wave potentiation during and after muscle activity. J. Appl. Physiol. Bethesda Md 1985 1989, 66, 2606–2610. [Google Scholar] [CrossRef]
- Casabona, A.; Polizzi, M.C.; Perciavalle, V. Differences in H-reflex between athletes trained for explosive contractions and non-trained subjects. Eur. J. Appl. Physiol. 1990, 61, 26–32. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





