1. Introduction
The larynx, which is located in the throat over the trachea, is a vital structure in the human body as it plays an important role in breathing, swallowing and in the production of speech sounds. The pathologies of this anatomical site range from benign conditions such as infections and/or inflammation (i.e., laryngitis), benign nodules and/or polyps, to life-threatening pathologies, the most threatening of which is laryngeal cancer. These malignancies can originate from any part of the larynx, including the vocal cords, epiglottis, arytenoid cartilage and other surrounding tissues [
1,
2].
Among the different types of laryngeal cancer, squamous cell carcinoma, which usually arises from the flat, thin cells lining the inside of the larynx, is the most common form and accounts for the vast majority (almost 90%) of malignancies in this anatomical site, followed by less common types of cancers such as adenocarcinoma (which usually arises from the glandular cells of the larynx) and sarcomas (which develop in the connective tissue cells of the larynx, such as muscle, cartilage, or fat) [
3]. Laryngeal cancers can also be classified according to anatomical site (i.e. supraglottic, glottic and subglottic), and are characterized by different pathophysiology and often require different therapeutic management [
3].
The main risk factors for laryngeal cancer include cigarette smoking, tobacco chewing, heavy alcohol consumption, male gender, advanced age, exposure to certain chemicals (like asbestos, nickel, sulphuric acid fumes, formaldehyde, isopropyl alcohol), local infections (especially human papillomavirus [HPV] type 16) and gastroesophageal reflux disease, among others [
3].
The most common symptoms include hoarseness or changes in voice quality lasting longer than 2 to 3 weeks, persistent sore throat or cough, difficulty swallowing, earache, appearance of lumps or masses in the throat, difficulty breathing and even weight loss [
3]. The diagnosis of laryngeal cancer usually involves a combination of physical examination, imaging studies (such as computed tomography [CT] scans or magnetic resonance imaging [MRI]), and local biopsy of the mass [
4]. The prognosis of laryngeal cancer depends on several factors, including the stage of cancer, the patient's health status, early diagnosis and effectiveness of treatment, because it is generally assumed that early detection and treatment are associated with better outcomes. Recent data show that the 5-year survival rate of laryngeal cancer is between 64 and 74% [
5].
Several lines of evidence suggest that the interplay between coronavirus disease 2019 (COVID-19) and laryngeal cancer may have represented a substantial challenge for both patients and healthcare. For example, individuals with early forms of cancer may have developed a weaker immune response against the malignancy due to the direct effect of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on the immune system [
6]. Additional factors include the global disruptions in cancer screening, diagnosis and treatment that may have been associated with significant delay in diagnosis and treatment [
7], but also the increased risk of respiratory complications since laryngeal cancers impair breathing and respiratory function, conditions that could be aggravated by SARS-CoV-2 infection [
8]. Therefore, to garner information on recent mortality for laryngeal cancer, especially during the last years (some of which dominated by the COVID-19 pandemic), we perform an analysis of real-world data made available by the US Centers for Disease Control and Prevention (CDC).
2. Materials and Methods
We accessed the last updated version of the CDC WONDER on-line database, which reports mortality data between the years 2018 and 2022 for the US resident population [
9]. This information is derived from demographic information and death certificates reporting a unique cause of death. The original search was made using “year” as the first variable, combined with the ICD-10 code for laryngeal cancer as the second variable (ICD-10: C32; malignant neoplasm of larynx). The search was then expanded with a sub-analysis of mortality for laryngeal cancer between genders (males and females), and across ten-year age groups, as available in the WONDER database for this type of cancer (35-44, 45-54, 55-64, 65-74, 75-84, +85 years). The final output of the database search includes the total number of deaths for specific ICD-10 codes, the crude or age adjusted mortality rate ×100,000 with 95% confidence interval (95%CI) or standard error (SE). Data were analyzed with one-way analysis of variance (ANOVA) and Tukey post-hoc test (StatPages, Interactive Statistical Calculation). Statistical significance was set at p<0.05. The study was conducted in accordance with the Declaration of Helsinki and in within the terms defined by the local legislation. Since this analysis was based on retrospective data from the freely searchable WONDER anonymized database, no informed consent or ethical committee approval were necessary.
3. Results
The age-adjusted mortality rate ×100,000 for laryngeal cancer was 0.91 (95%CI, 0.84-0.94) in 2018, 0.89 (95%CI, 0.86-0.92) in 2019, 0.89 (95%CI, 0.86-0.92) in 2020, 0.91 (95%CI, 0.88-0.94) in 2021, and 0.91 (95%CI, 0.89-0.92) in 2022. This trend was not statistically significant according to one-way ANOVA (f=0.757; p=0.553). The Tukey post-hoc test revealed no statistically significant differences across multiple comparisons of different years throughout the study period (all p≥0.791).
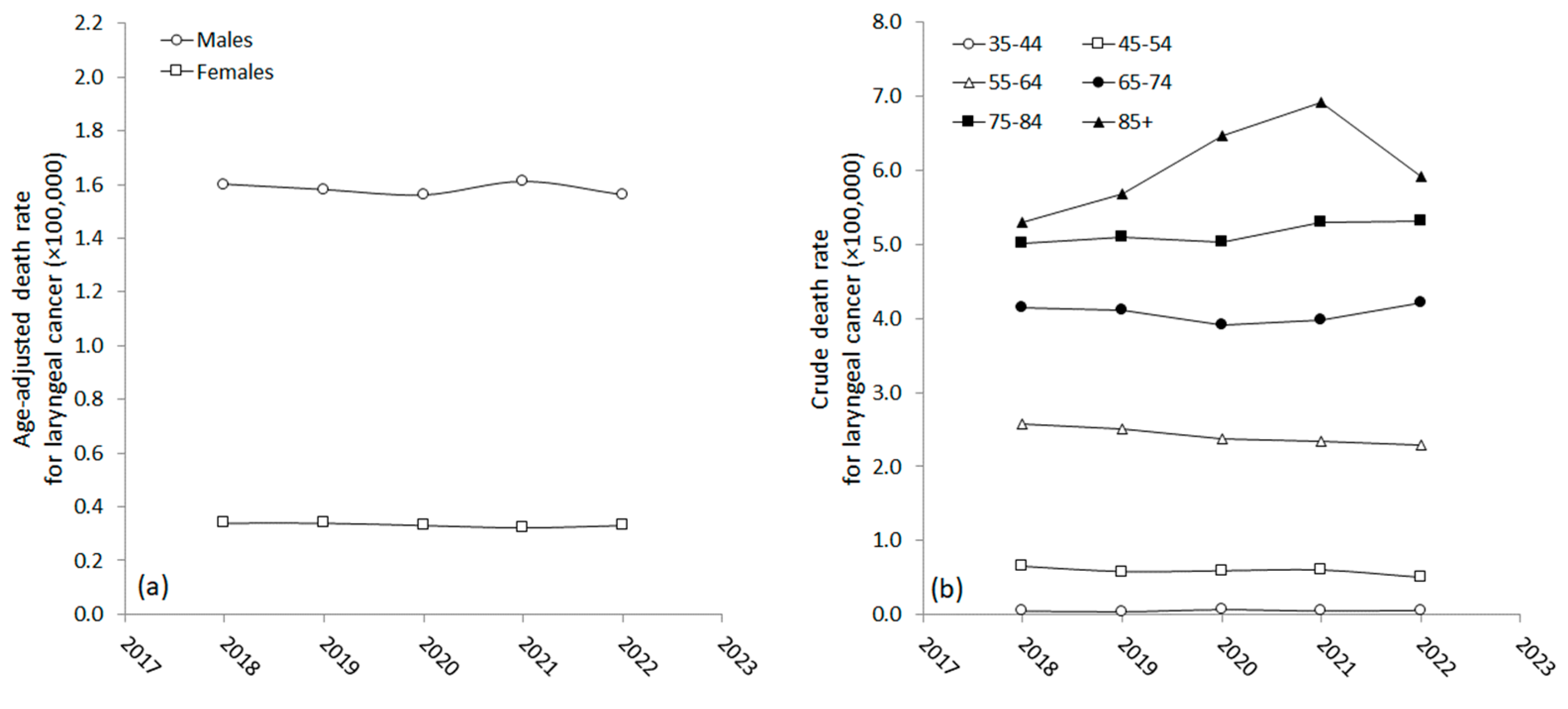
Table 1 and
Figure 2 show the gender- and age-specific mortality trends for laryngeal cancer between 2018 and 2022. Males had consistently higher age-adjusted mortality rates than females, with M/F ratios ranging between 4.6 and 5.0 between 2018 and 2022.
One-way ANOVA revealed no significant differences in mortality trends in both genders before and during the COVID-19 pandemic (males: f=0.58, p=0.676; females: f=0.694, p=0.596). Nonetheless, there were some differences in the age-specific trend of laryngeal cancer mortality between 2018 and 2022. Although the values remained mostly unchanged or only showed minor and non-statistically significant variations in people aged 35-44 years (f=1.24; p=0.300; no significant differences among the different years by Tukey post-hoc test), 45-54 years (f=1.72; p=0.142; no significant differences among the different years by Tukey post-hoc test), 55-64 years (f=2.63; p=0.052; no significant differences among the different years by Tukey post-hoc test), 65-74 years (f=1.23; p=0.296; no significant differences among the different years by Tukey post-hoc test) and 75-84 years (f=0.668; p=0.614; no significant differences among the different years by Tukey post-hoc test), significant variation was found in the older age group. Specifically, in people aged 85 or older, the 2018-2022 trend reached statistical significance by one-way ANOVA (f=3.90; p=0.004), displaying significant increase in mortality rate in 2021 compared to 2018 (p=0.006) and 2019 (p=0.039), respectively (
Figure 2).
4. Discussion
Laryngeal cancer accounts for 30–40% of all head and neck malignancies and continues to impose a major burden on healthcare and society due to its significant impact on quality of life, morbidity and mortality. Although it has previously been demonstrated that mortality from this malignancy has declined in many developed countries in recent decades [
10,
11], COVID-19 may have reversed this positive trend for a variety of reasons other than for the direct interplay of SARS-CoV-2 with the host immune system, including disruption of cancer screening and diagnosis, deferred or even discontinued treatments, surveillance and follow-up, and impeded access to clinical trials and innovative therapies [
12]. The most obvious consequence is the delayed detection of some cancers and the diagnosis of some malignancies at a more advanced stage than in the pre-pandemic period [
13,
14].
Regarding laryngeal cancer, the results of our retrospective analysis of real-world data provided by the US CDC show that the cumulative mortality for this malignancy has not changed significantly during the COVID-19 pandemic, as the age-adjusted death rate has always remained between 0.89-0.91 ×100,000 from 2018 to 2022. There were also no significant variations in the mortality rate for laryngeal cancer between the sexes or in most age groups. However, our analysis also shows that the mortality rate for this cancer has exhibited a significant increase in 2021 in people aged 85 years or older, following a trend that already saw a non-significant increase in 2020. Thereafter, in 2022 the mortality rate in this older population has returned to values comparable to those of 2018-2019, reflecting the lower virulence of SARS-CoV-2, the higher level of herd immunity developed over time (either naturally or through vaccination) and the release of most measures of social restriction (i.e., lockdowns, curfews, quarantines, isolation, etc.) [
15].
5. Conclusions
In conclusion, our analysis of real-world data on laryngeal cancer mortality suggests that the impact of the COVID-19 pandemic may have been relatively modest in the general US population. Nevertheless, one important aspect that has emerged for the future is the need to devote more efforts to the health of older people during similar global tragedies, as the biological consequences of misdiagnosis or mistreating malignancies, including laryngeal cancer, can be enormously amplified in this highly vulnerable part of the general population.
Author Contributions
Conceptualization, R.N., G.L. and C.M.; methodology, G.L.; formal analysis, G.L.; data curation, G.L.; writing—original draft preparation, G.L.; writing—review and editing, R.N. and C.M.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due since this analysis was based on retrospective data from the freely searchable WONDER anonymized database.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Parker DA, Robin PE. Investigation of laryngeal pathology: a review of diagnostic techniques. Clin Otolaryngol Allied Sci 1989;14(1):79-89. [CrossRef]
- Adriaansen A, Van Lierde K, Meerschman I, Claeys S, D'haeseleer E. The Occurrence of Laryngeal Pathologies in a Treatment-Seeking Pediatric Population. J Voice. 2023 Jul 29:S0892-1997(23)00210-2. Epub ahead of print. [CrossRef]
- Koroulakis A, Agarwal M. Laryngeal Cancer. [Updated 2022 Mar 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526076/.
- Itamura K, Hsue VB, Barbu AM, Chen MM. Diagnostic Assessment (Imaging) and Staging of Laryngeal Cancer. Otolaryngol Clin North Am 2023;56(2):215-231. [CrossRef]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70(1):7-30. [CrossRef]
- Wekking D, Senevirathne TH, Pearce JL, Aiello M, Scartozzi M, Lambertini M, De Silva P, Solinas C. The impact of COVID-19 on cancer patients. Cytokine Growth Factor Rev 2024;75:110-118. [CrossRef]
- Allahqoli L, Mazidimoradi A, Salehiniya H, Alkatout I. Impact of COVID-19 on cancer screening: a global perspective. Curr Opin Support Palliat Care 2022;16(3):102-109. [CrossRef]
- Patel ND, Cabrera CI, Fowler NM, Li S, Thuener JE, Lavertu P, Teknos TN, Rezaee RP, Tamaki A. Incidence and medical complications of COVID-19 in the total laryngectomy population: A population-based study. Oral Oncol 2023;139:106353. [CrossRef]
- Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2018-2022 on CDC WONDER Online Database, released in 2024. Data are from the Multiple Cause of Death Files, 2018-2022, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/ucd-icd10-expanded.html (accessed on 4 May 2024).
- Nocini R, Molteni G, Mattiuzzi C, Lippi G. Updates on larynx cancer epidemiology. Chin J Cancer Res 2020;32(1):18-25. [CrossRef]
- Igissin N, Zatonskikh V, Telmanova Z, Tulebaev R, Moore M. Laryngeal Cancer: Epidemiology, Etiology, and Prevention: A Narrative Review. Iran J Public Health 2023;52(11):2248-2259. [CrossRef]
- Richards M, Anderson M, Carter P, Ebert BL, Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nat Cancer 2020;1(6):565-567. [CrossRef]
- Heer E, Ruan Y, Boyne DJ, Jarada TN, Heng D, Henning JW, Morris DM, O'Sullivan DE, Cheung WY, Brenner DR. Impact of the COVID-19 pandemic on cancer diagnoses, stage and survival in Alberta. CMAJ 2023;195(23):E804-E812. [CrossRef]
- Pennisi F, Odelli S, Borlini S, Morani F, Signorelli C, Renzi C. Impact of the Covid pandemic on timely cancer diagnosis across European healthcare settings: a scoping review. Ann Ig 2024;36(2):194-214. [CrossRef]
- Mattiuzzi C, Lippi G. Timeline analysis of clinical severity of COVID-19 in the general population. Eur J Intern Med 2023;110:97-98. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).