Introduction
Medication Related Osteonecrosis of the jaws (MRONJ) is a rare but serious adverse effect associated with numerous medications including bisphosphonates, denosumab and possibly antiangiogenics. The American Association of Oral and Maxillofacial Surgeons (AAOMS) states that “The case definition of MRONJ includes all the following elements: current or previous treatment with antiresorptive therapy alone or in combination with immune modulators or antiangiogenic medications, exposed bone or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region that has persisted for more than eight weeks and no history of radiation therapy to the jaws or metastatic disease to the jaws”[
1].
In 2007, the AAOMS introduced a staging system for MRONJ, which was subsequently refined in the 2022 position paper [1-3]. The current classification system consists of the following stages: “Stage 0” - Patients with no clinical evidence of necrotic bone but who present with nonspecific symptoms or clinical and radiographic findings, “Stage 1” - Exposed and necrotic bone or fistula that probes to the bone in patients who are asymptomatic and have no evidence of infection/inflammation, “Stage 2” - Exposed and necrotic bone, or fistula that probes to the bone, with evidence of infection/inflammation, “Stage 3” Exposed necrotic bone extending beyond the region of alveolar bone or pathologic fracture or extraoral fistula or oral antral/oral-nasal communication [
1].
Although, there is a consensus on the significance of imaging in evaluating the extent of MRONJ, the precise role of radiologic findings in MRONJ patients and its contribution to clinical staging remain unclear [
4,
5]. Radiologic findings of MRONJ may include lytic changes, sclerosis, sequestrations and periosteal bone formation. All these findings are not specific and can be seen in other conditions such as osteoradionecrosis, osteomyelitis and jaw metastatic disease [6-8].
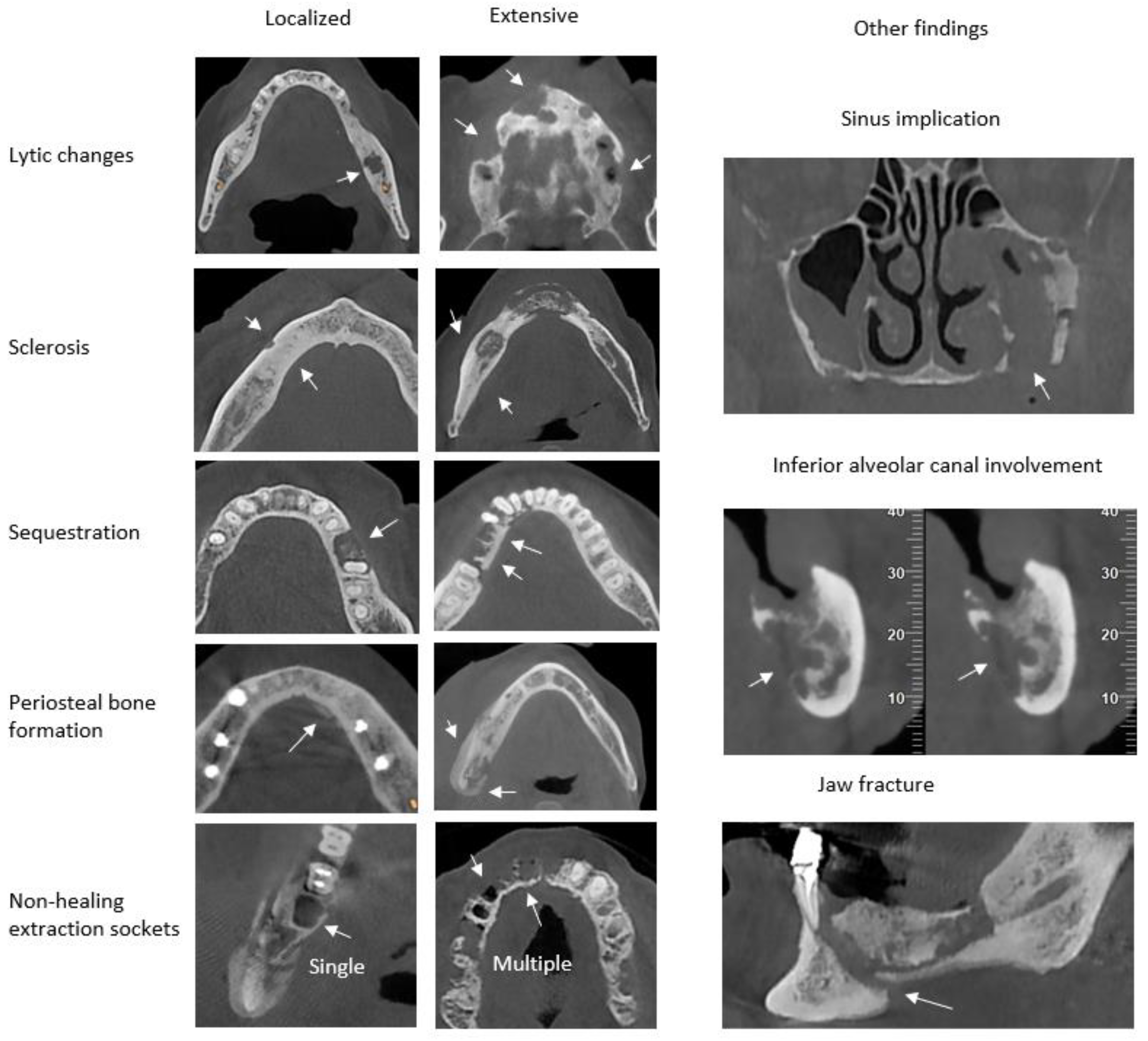
Recently, in the study of Yfanti Z. et al, the presence and the extent of radiologic findings of medication related osteonecrosis of the jaws, osteoradionecrosis, osteomyelitis and jaw metastatic disease was evaluated with the use of a new modified index (CRIm) [
8]. The Composite Radiographic Index modified (CRIm) [
8], based on the Composite Radiographic Index (CRI) that was introduced by Walton K [
6], classified and evaluated eight radiologic features, common in the above-mentioned diseases which include: lytic changes, sclerosis, periosteal bone formation, sequestration, non-healing extraction sockets and other findings (maxillary sinus implication, inferior alveolar canal involvement and jaw fracture) [
8]. Lytic changes, sclerosis, periosteal bone formation and sequestration were scored as (0) when absent, (1) as localized when the lesions extended up to 1 cm and (2) extensive when the lesions extended those dimensions or in cases of multiple lesions. Extraction sockets showing no sign of healing were evaluated only if they were near the lesion and scored as (0) absent if no sockets were present, (1) localized if one socket was present, and (2) extensive if multiple sockets were present. The other findings were individually scored as (0) when absent and (1) when present [
8] (
Figure 1).
The purpose of this study is to apply the CRIm index in Cone Beam Computed Tomography (CBCT) scans of patients with MRONJ in order to detect its validity and correlate the radiologic findings with the staging of the disease.
Materials and Methods
A total of 43 patients who had attended NKUA School of Dentistry from 2019 to 2023 with a definite diagnosis of MRONJ who were referred for CBCT examinations, were included in this study. This study was approved by the Research Ethics Committee of the NKUA, School of Dentistry with protocol number 99126. Consensus form was signed by all patients. Patient data included: age, gender, underlying primary disease, date of initial consultation, antiresorptive medication and location and size of the exposed bone.
Clinical staging for every patient (Stage 0-3) was provided by the Department of Oral Pathology & Hospital Dentistry according to AAOMS 2022 guidelines [
1]. In cases of patients with both jaws affected, each jaw was evaluated separately. Follow up examinations of the same patients were excluded, except in cases where documented disease progression with new radiological characteristics was observed. Additionally, patients with a history of head or neck radiation were not included in the study.
As a result, a total of 52 CBCT scans of MRONJ matched the inclusion criteria and were evaluated. The CBCT scans were performed with the NewTom VGi CBCT scanner (Cefla, Imola, Italy) and were accepted if diagnostic quality was optimal or adequate. The exposure settings were 110 kV and 3–5 mA with 3,6 sec. exposure time.
The selected CBCT scans underwent anonymization and two observers [a PhD Candidate in Oral and Maxillofacial Radiology (Z.Υ.) and a senior Oral and Maxillofacial Radiologist (K.E.A.)] evaluated all the scans under identical-standardized viewing conditions. Both observers were trained and calibrated prior to the evaluation. Localization was categorized into maxillary anterior, maxillary posterior, mandibular anterior, and mandibular posterior sextants. Anterior sextants of the maxilla and the mandible were classified as regions within the canines. Lesions that extended in both anterior and posterior regions were recorded in both corresponding sextants.
Each observer was provided with a special answer sheet for each CBCT scan, and noted the location, pertinent radiologic features of pathologic findings and the final value of the CRIm index [
8]. CRIm index was constructed by summing up the individual scores for each radiologic feature for every jaw examined, yielding a theoretical range of 0–12. All CBCT scans were classified in three groups according to their CRIm scores: low (0–3), medium (4–8) and high (9–12). In cases where there was a difference of more than 1 in the CRIm index between the 2 observers, both observers re-evaluated the CBCT scans in order to achieve consensus. If there was a disagreement between the two observers, a third observer (K.T., experienced specialist in Oral and Maxillofacial Radiology) assessed the CBCT scans under identical viewing conditions.
Statistical Analysis
The collected data was analyzed with descriptive statistics by means of frequency, incidence rate, mean values and standard deviation (SD). All statistical analyses were performed using IBM SPSS software version 25 (SPSS Inc., 2003, Chicago, USA). The Fisher’s exact test and Spearman’s correlation coefficient were applied for correlation of both the radiologic features and CRIm index with the clinical stage. P-values< 0,05 were considered statistically significant. Kappa statistics was performed in order to evaluate the agreement between the 2 observers.
Results
A total of 43 patients were evaluated in this study (17 males and 26 females), with an average age of 65.4 years and Standard Deviation (SD) of 11.2 years. Age ranged from 39 to 87 y.o. The agreement rate between the 2 observers was recorded as excellent both for localization (Kappa 0.944-1), and for radiologic features (Kappa 0.961-1). From the 43 patients 52 CBCT scans with radiologic findings were acquired and evaluated accordingly.
Table 1 presents the localization of MRONJ in maxilla and mandible divided in sextants (13 maxillas and 39 mandibles). The most common localization was in the posterior sextants of the mandible (63,5%) followed by the anterior sextants of the mandible (34,6%), posterior sextants of the maxilla (21,2%) and finally anterior sextants of the maxilla (13,5%).
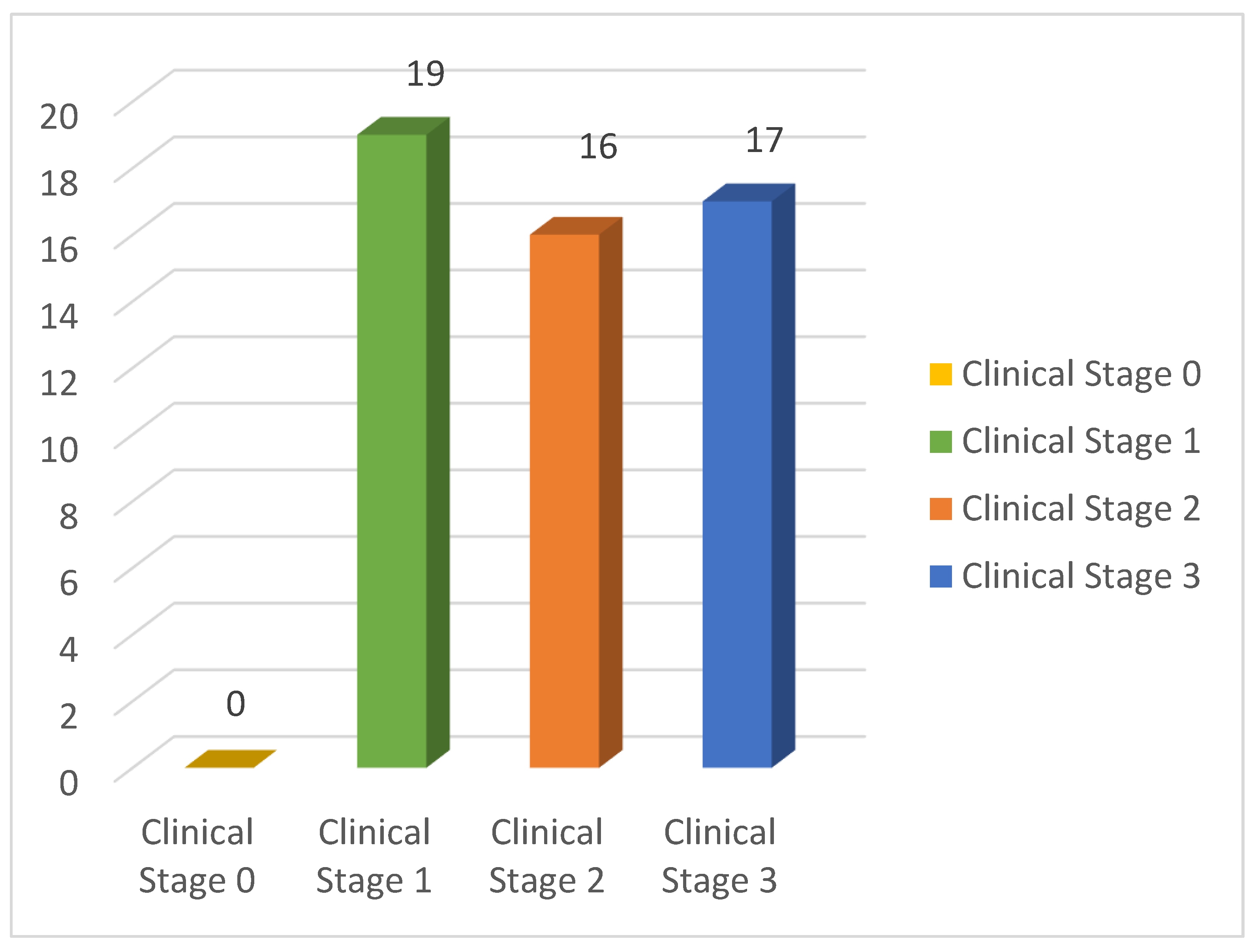
Figure 2 presents the distribution of the 52 CBCT scans with MRONJ findings according to the clinical stage of the disease. No affected jaws were recorded with Stage 0. Clinical Stage 1 consisted of 19 jaws (36,5% of the sample), Stage 2 of 16 jaws (30,8%) and Stage 3 of 17 jaws (32,7%).
Table 2 presents the results of the correlation of the clinical stage of MRONJ with the radiologic features. A statistically significant association of clinical stage with lytic changes, sequestration and inferior alveolar canal involvement was found (p-value<0,05). Extensive lytic changes, sclerosis, sequestration and periosteal bone formation were mostly observed in clinical Stage 3. Also, inferior alveolar canal involvement is mainly observed in clinical Stage 3.
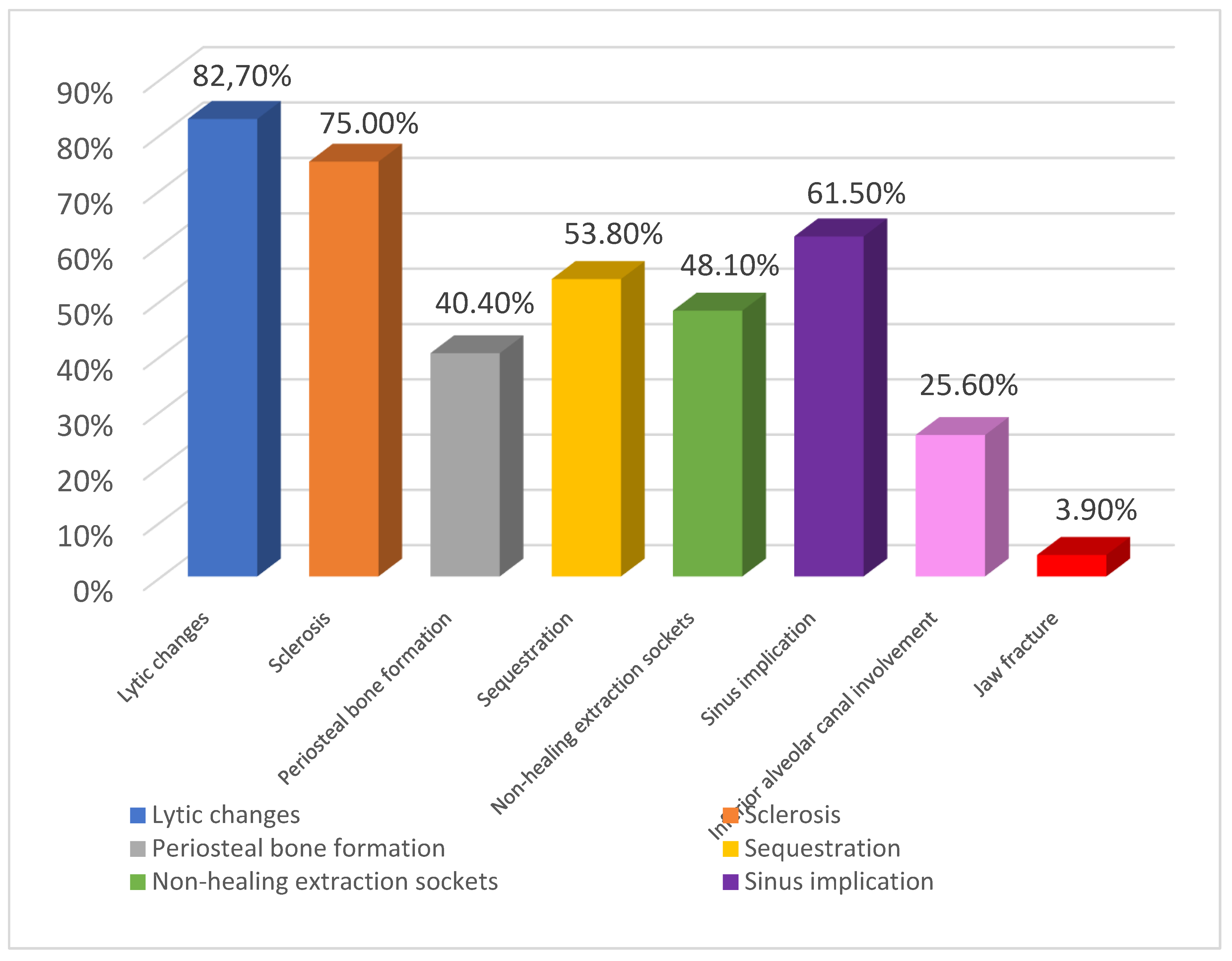
Figure 3 presents the distribution of all the radiologic features for MRONJ affected jaws.
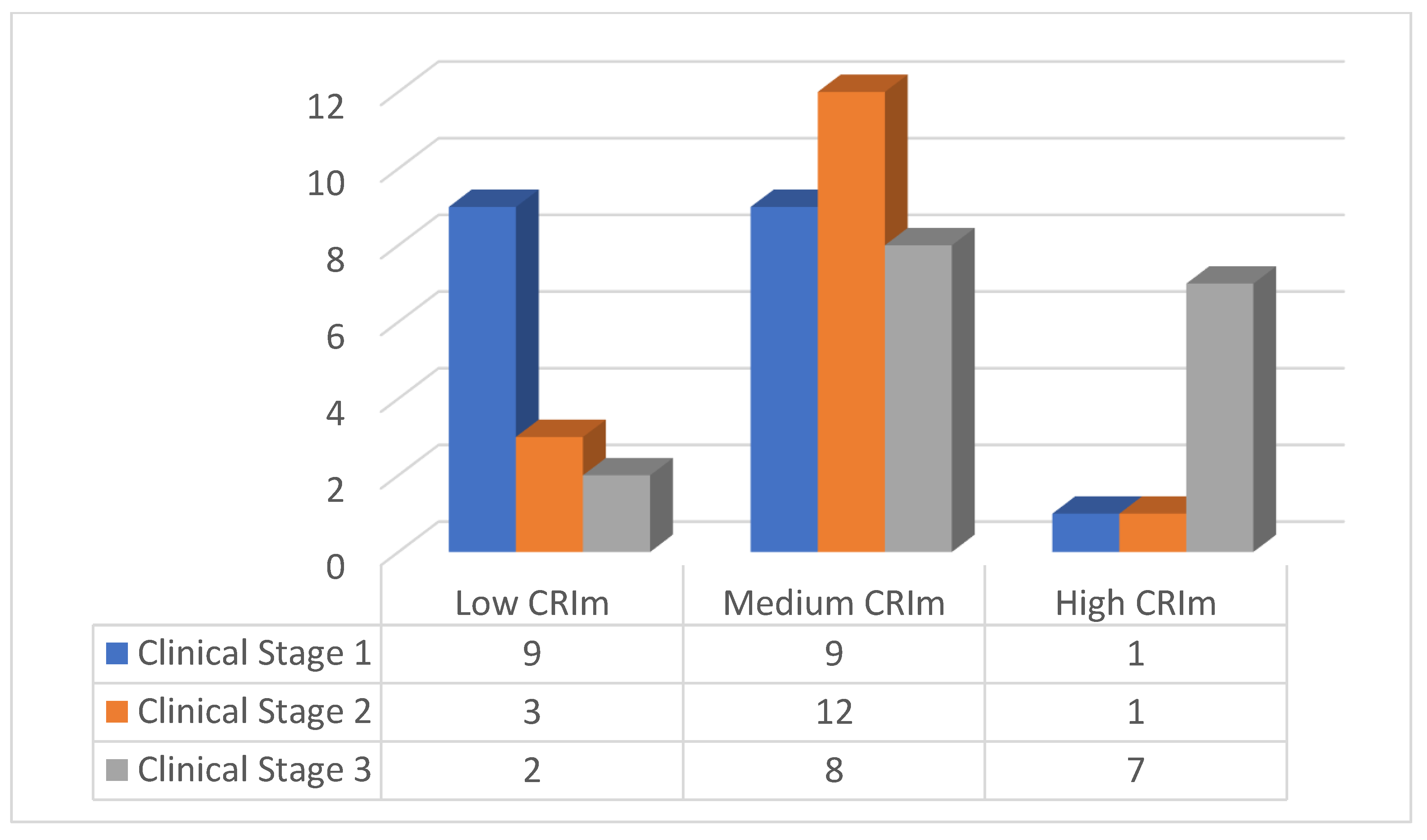
Table 3 demonstrates the results of the correlation of the clinical stage with the CRIm index. In clinical Stage 1 approximately half of the affected jaws (47.4%) were classified in the low CRIm group, 75% of the Clinical stage 2 cases were classified in the medium CRIm group, while 41.2% of the clinical stage 3 cases were classified in the high CRIm group. In addition, a statistically significant moderate correlation of clinical stage with CRIm index classification is obtained (rho= 0.446 & p-value< 0.001).
Figure 4 shows the distribution of the classification of the CRIm index into 3 groups, according to the clinical stage.
Discussion
Medication-related osteonecrosis of the jaw (MRONJ) is a rare but serious complication in patients undergoing treatment for bone malignancy or osteoporosis. MRONJ presents as nonhealing exposed bone in patients who have been treated with antiresorptive or antiangiogenic medications, without prior radiation to the head and neck region [
9,
10].
The current AAOMS staging system classifies MRONJ patients to different stages based mostly on clinical signs and symptoms [
1]. However, clinical examination cannot always provide the full extent of the condition beneath the mucosal tissue, while the radiological examination can offer a more accurate estimation of its real extent [
11,
12].
The modified Composite Radiographic Index (CRIm) that was introduced in the study of Yfanti Z et al 2023, was a modified index based on the CRI index of Walton K et al 2019 that was constructed in order to evaluate the extent of the radiographic findings in MRONJ patients. CRIm was classified in low (0-3), medium (4-8) and high (9-12) scores.
In this context, the results of this study aim to correlate the current clinical staging system to the CRIm index in order to provide a more comprehensive radiographic evaluation of MRONJ patients.
As far as it concerns clinical appearance, MRONJ’s initial presentation may vary from asymptomatic patients to patients with extensive lesions and bone exposure leading to a pathological fracture [
13].
In the present study, the majority of MRONJ patients were females (60%), which is in agreement with findings from similar studies [
8,
14,
15]. This is probably due to the higher prevalence of osteoporosis treatment among female patients.
In the literature, it is indicated that the mandible is most affected, at a 2:1 proportion compared with the maxilla [
16]. In our study, it was observed that 66% of the MRONJ cases affected the mandible. Interestingly, 12% of the patients in our study presented with MRONJ both in maxilla and mandible, which is considered uncommon [
6,
17].
In contrast to traditional 2D imaging such as with panoramic radiographs, CBCT can provide a comprehensive assessment to the actual extent of MRONJ [18-20]. CBCT is a valuable imaging technique in oral and maxillofacial surgery as it is increasingly used in evaluating oral pathology even in early stages of detection [
21] with substantially reduced radiation exposure than Multi-detector computed tomography (MDCT) [
22].
In our study the most common radiographic feature were lytic changes. Osteolysis was observed in 82,7% of the cases and this is in agreement with other MRONJ related studies where osteolysis is generally observed [
7,
8]. The second most common finding was sclerosis which is considered an important bone alteration in MRONJ patients [
23,
24]. In our study, sclerosis appeared in 75% of the affected jaws in all the 3 clinical stages, a finding that is also common in other studies [6-8].
The results of our research show that MRONJ presented a high occurrence of multiple or extensive bone sequestrations (53,8%) in all 3 clinical stages. These findings are in agreement with other MRONJ related studies that demonstrate the frequent presence of bone sequestration in MRONJ [
7,
25].
The results of this study show that more than half of the cases were classified in the CRIm medium group (4-8) which is in agreement with the results of other studies [
6,
8].
It was observed that in MRONJ clinical Stage 1 approximately half of the cases had low CRIm scores. In clinical Stage 2 the majority of the cases had medium CRIm scores and finally in clinical Stage 3 most cases had high CRIm scores. This proves a progression of the CRIm as it tends to increase as the clinical stages advance and this was found to be statistically significant. This indicates a correlation between MRONJ clinical and radiographic appearance which is in agreement with other MRONJ related studies [
6,
12,
23].
The main limitation of this study was the small sample size. Further studies with a larger sample size of documented cases of MRONJ must be performed in order to evaluate and validate the effectiveness of the CRIm index.
Conclusions
The CRIm is a valid indicator of the progress of MRONJ by means of extent of bone involvement. Moreover, the CRIm tends to increase with the advancement of MRONJ’s clinical stages.
Author Contributions
Writing - Original Draft Preparation: Z.Y. Methodology: Z.Y., K.E.A. Investigation: Z.Y., K.E.A., E.V. Visualization: Z.Y. Supervision: S.T., K.T., C.A. Resources: N.G.N., K.T. Writing - Review & Editing: C.A., K.T. Conceptualization: K. T. The final version of the manuscript has been reviewed and approved by all authors prior to the publication.
Institutional Review Board Statement
Approval by the Research Ethics Committee of the NKUA, School of Dentistry with protocol number 99126.
Informed Consent Statement
Consensus form was signed by all patients.
Data Availability Statement
The datasets are available from the corresponding author upon reasonable request due to privacy/ethical restrictions.
Conflicts of Interest
No conflicts of interest.
References
- Ruggiero S. L., Dodson T. B., Aghaloo T., Carlson E. R., Ward B.B., Kademani D. American Association of Oral and Maxillofacial Surgeons’ Position Paper on medication-related osteonecrosis of the jaw–2022 update. J Oral Maxillofac Surg2022, 80, 920-943. [CrossRef]
- Ruggiero S. L., Dodson T. B., Fantasia J., Goodday R., Aghaloo T., Mehrotra B., O'Ryan F. "American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg2014, 72,10:1938-1956. [CrossRef]
- Advisory Task Force on Bisphosphonate-Related Osteonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg2007, 65(3),369-376.
- Kämmerer P.W., ThiemD., Eisenbeiß C., Dau M., Schulze R.K., Al-Nawas B., Draenert F.G. Surgical evaluation of panoramic radiography and cone beam computed tomography for therapy planning of bisphosphonate-related osteonecrosis of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol, 2016, 121(4), 419-24. [CrossRef]
- Izzetti R., Gennai S., De Francesco P., Carli E., Graziani F., Nisi M. Panoramic Radiography Features of Medication-Related Osteonecrosis of the Jaws (MRONJ), Int. J. Dent, (2023) 2023.
- Walton K., Grogan T.R., Eshaghzadeh E., Hadaya D., Elashoff D.A., Aghaloo T.L., Tetradis S. Medication related osteonecrosis of the jaw in osteoporotic vs oncologic patients-quantifying radiographic appearance and relationship to clinical findings. Dentomaxillofac. Radiol. 2019, 48, 20180128. [CrossRef]
- Gaêta-Araujo H., Vanderhaeghen O., Vasconcelos K.F., Coucke W., Coropciuc R., Politis C., Jacobs R. Osteomyelitis, osteoradionecrosis, or medication-related osteonecrosis of the jaws? Can CBCT enhance radiographic diagnosis? Oral. Dis. 2021, 27, 312-319.
- Yfanti Z., Tetradis S., Nikitakis N.G., Alexiou K. E., Makris N., Angelopoulos C., Tsiklakis K. Radiologic findings of osteonecrosis, osteoradionecrosis, osteomyelitis and jaw metastatic disease with cone beam CT. Eur J Radiol. 2023, 165, 110916. [CrossRef]
- Favia G., Tempesta A., Limongelli L., Crincoli V., Maiorano E. Medication-Related Osteonecrosis of the Jaws: Considerations on a New Antiresorptive Therapy (Denosumab) and Treatment Outcome after a 13-Year Experience. Int J Dent. 2016, 2016, 1801676. [CrossRef]
- AlDhalaan N. A., BaQais A., Al-Omar A. Medication-related Osteonecrosis of the Jaw: A Review. Cureus2020, 12, e6944. [CrossRef]
- Bedogni A., Blandamura S., Lokmic Z., Palumbo C., Ragazzo M., Ferrari F. Biphosphonate-associated jawbone osteonecrosis: a correlation between imaging techniques and histopathology. Oral Surg Oral Med Oral Pathol Oral Endod. 2008, 105, 358–364.
- Wilde F., Heufelder M., Lorenz K., Liese S., Liese J., Helmrich J., Schramm A., Hemprich A., Hirsch E., Winter K. Prevalence of cone beam computed tomography imaging findings according to the clinical stage of bisphosphonate-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 2012, 114, 804-811. [CrossRef]
- Thomas J. G., Ouanounou A., Medication-related osteonecrosis of the jaw: a narrative review of risk factors, diagnosis, and management. Front Oral Maxillofac Med2023, 5. [CrossRef]
- Grisar K., Schol M., Schoenaers J., Dormaar T., Coropciuc R., Vander Poorten V., Politis C. Osteoradionecrosis and medication-related osteonecrosis of the jaw: similarities and differences, Int. J. Oral Maxillofac. Surg. 2016, 45, 1592-1599. [CrossRef]
- Soundia A., Hadaya D., Mallya S.M., Aghaloo T.L., Tetradis S. Radiographic predictors of bone exposure in patients with stage 0 medication-related osteonecrosis of the jaws. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 537-544. [CrossRef]
- Ruggiero S.L., Fantasia J., Carlson E. Bisphosphonate-related osteonecrosis of the jaw: background and guidelines for diagnosis, staging and management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006,102, 433–41. [CrossRef]
- Saad F., Brown J. E., Van Poznak C., Ibrahim T., Stemmer S.M., Stopeck A.T., DielI. J., Takahashi S., Shore N., Henry D. H., Barrios C. H., Facon T., Senecal F., Fizazi K., Zhou L., Daniels A., Carrière P., Dansey R. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012, 23, 1341-1347. [CrossRef]
- Gönen Z. B., Yillmaz Asan C., Zararsiz G., Kiliç E., Alkan A. Osseous changes in patients with medication-related osteonecrosis of the jaws. Dentomaxillofac Radiol 2018, 47,20170172. [CrossRef]
- Stockmann P., Hinkmann F. M., Lell M.M., Fenner M., Vairaktaris E., Neukam F.W., Nkenke E. Panoramic radiograph, computed tomography or magnetic resonance imaging. Which imaging technique should be preferred in bisphosphonate-associated osteonecrosis of the jaw? A prospective clinical study. Clin Oral Invest 2010, 14,311–317. [CrossRef]
- Cardoso C. L., Barros C.A., Curra C., Fernandes L.M., Franzolin S.O., Júnior J.S., De Antoni C.C., Curi M.M. Radiographic Findings in Patients with Medication-Related Osteonecrosis of the Jaw. Int J Dent. 2017, 2017, 3190301. [CrossRef]
- Grassi R., Guerra E., Berritto D. Bone fractures difficult to recognize in emergency: May be cone beam computed tomography (CBCT) the solution? Radiol Med. 2023, 128, 1-5.
- Adibi S., Zhang W., Servos T., O'Neill P. N. Cone beam computed tomography in dentistry: what dental educators and learners should know. J Dent Educ2012, 76,1437–42. [CrossRef]
- Bagan J.V., Cibrian R.M., Lopez J., Leopoldo-Rodado M., Carbonell E., Bagán L., Utrilla J., Scully C. Sclerosis in bisphosphonate-related osteonecrosis of the jaws and its correlation with the clinical stages: study of 43 cases. Br J Oral Maxillofac Surg 2015, 53, 257-262. [CrossRef]
- Mallya S.M., Tetradis S. Imaging of Radiation- and Medication-Related Osteonecrosis. Radiol Clin North Am. 2018, 56, 77-89. [CrossRef]
- KwonT. G., Choi S. Y., Ahn B. C., An C. H. Comparison of chronic osteomyelitis versus bisphosphonate-related osteonecrosis of the jaws in female patients without malignant bone disease J. Oral Maxillofac. Surg. Med. Pathol. 2013, 25, 214-220.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).