1. Introduction
Plants have been humankind’s faithful companions for millennia, fulfilling our basic needs for food and shelter and offering solace in times of illness. Throughout history, various cultures have looked to the natural world for remedies, relying on plants for their medicinal properties (World Health Organization Global Centre for Traditional Medicine, 2023). This dependence on traditional medicine is particularly pronounced in rural areas, where modern healthcare systems may need expanded. The WHO estimates that a staggering 88% of the global population utilizes traditional medicine as their primary healthcare option (WHO GCTM 2023).
This intricate relationship between humans and plants has shaped human civilization, particularly in medicine (World Health Organization 2019). Even today, the tradition of using wild plants for medicinal purposes continues to thrive in small, rural communities, especially among those societies that bridge the gap between past and present cultural practices. Indigenous knowledge about medicinal plants holds immense value for discovering novel and effective drugs (Kunwar, 2016). Numerous active natural products with therapeutic potential have been unearthed from medicinal plants thanks to ethnobotanical surveys (Timmermans 2003).
The enduring appeal of traditional medicine lies in its affordability and efficacy. These practices passed down through generations, are a cornerstone of healthcare in many communities (Huai & Pei 2002). Medicinal plants are a treasure trove of bioactive compounds with various pharmacological activities. Their use extends beyond rural areas, increasing acceptance in urban settings across developed and developing nations (Huai & Pei 2002). Importantly, research has demonstrated the safety and efficacy of plant-derived medicinal products, offering solutions for various health concerns without causing adverse effects (Singh & Ahirwar 2018).
Natural plant resources are critical in traditional herbal medicine, fostering better health and contributing to local communities’ economic well-being (Everest & Ozturk 2005, Joshi & Joshi 2006; Yaseen et al. 2015). Tribal societies, in particular, depend profoundly on forest resources for their livelihoods and healthcare needs. These communities act as custodians of traditional knowledge and cultural practices, transmitting this invaluable heritage through oral traditions (Jain 2004, Maharjan et al. 2021). However, sociocultural transformations, human migration, and limited knowledge transfer threaten the continuation of these practices (Kunwar et al. 2016).
Geography, ethnicity, age, occupation, education, and cultural background all significantly influence traditional ethnomedicinal knowledge (Joshi et al., 2020). Therefore, ethnomedicinal research serves a crucial purpose in preserving and promoting the cultivation of medicinal plants and the associated understanding (Ford et al., 2020; Kumar et al., 2021). Natural products derived from plants have been instrumental in drug development, accounting for over 50% of the clinical drugs used in the pharmaceutical industry (Ghimire et al., 2012). Ethnobotanical studies documenting the medicinal uses of plants pave the way for developing contemporary drugs and treatments and contributing to plant conservation efforts (Heinrich, 2000; Calzada, 2020).
With its rich heritage of traditional medicine systems, India is recognized as a significant center for the origin and diversification of domesticated plant varieties (Siva, 2007). According to an All India coordinated project sponsored by the Ministry of Environment and Forest (MoEF), 40% of India’s 16,000 recorded flowering plants possess ethnomedicinal value. In the Indian subcontinent, 84% of the tribal population relies on forest resources for their livelihood (Harris & Mohammed, 2003; Mehta & Shah, 2003).
There are approximately 550 tribal communities spread across 227 ethnic groups residing in different forest regions of India (Sikarwar, 2002). These communities possess unique diagnostic and treatment methods based on traditional knowledge. Unfortunately, much ethnomedicinal information remains undocumented due to communication gaps, specific to limited communities or regions (Nisha & Sivadasan, 2007). However, there has been a recent surge in the screening of medicinal plant preparations, leading to a rise in the availability of herbal medicines, medicinal plants, and nutraceuticals in the market (Subramanyam, 2007).
India boasts 8% of the world’s total biodiversity and is among 12 megadiversity countries. Tropical forests are among the most productive ecosystems, covering only ~6% of the world’s surface area (Pan, 2013). These forests are known to harbor numerous medicinal plants (Rosero-Toro et al. 2018), which are currently disappearing at alarming rates due to natural and man-made disturbances and overexploitation of forest resources (Shanley and Luz 2003; Prajapati et al. 2018)
India’s Uttar Pradesh state harbors significant floristic diversity, particularly in the Terai and Vindhyan regions (Anonymous 2005). The Terai region boasts exceptional plant richness due to its favorable climate and edge effect (Bajpai et al. 2015). While indigenous knowledge regarding medicinal plant use exists, a comprehensive ethnomedicinal study of India’s moist deciduous forests, especially those within Uttar Pradesh’s Terai region, still needs to be included.
This study focuses on the Suhelwa Wildlife Sanctuary, a haven of tropical moist deciduous forest (TMDF) within the Terai region. We aim to document the indigenous knowledge held by local and traditional healers concerning the wild medicinal plants employed in phytotherapy within the sanctuary. We will utilize quantitative indices like Use Value (UV), Informant Consensus Factor (ICF), and Fidelity Level (FL) to analyze the ethnobotanical information gathered. Furthermore, we will compare our findings with data from other regions to identify novel medicinal plant uses. This enriched database can serve as a valuable resource for future pharmacological research.
The selection of the Suhelwa Wildlife Sanctuary as our study area is particularly compelling due to its diverse geographical and climatic conditions, fostering a remarkable variety of medicinal plants. This research delves into the knowledge of local healers, aiming to not only document traditional practices but also evaluate the potential of this region’s medicinal flora for drug discovery and as a sustainable source of income for local communities.
2. Material and Methods
2.1. Study Area
Nestled in the districts Sravasti, Balrampur, and Gonda of Uttar Pradesh lies the Suhelwa Wildlife Sanctuary (also known as Soheldeo Wildlife Sanctuary since 2002). Established in 1988, this sanctuary forms a crucial part of the Bhabher-Tarai ecosystem, renowned for its rich biodiversity. Spanning an area of 452 square kilometers, the sanctuary boasts five ranges: Tulsipur, Barahawa, Bankatwa, East Suhelwa, and West Suhelwa. A 220 square kilometer buffer zone further enhances its ecological significance. The Shivalik Hills of the Himalayas border the sanctuary, adding to its scenic beauty. Suhelwa experiences a unique climate, transitioning between the Gangetic plains and the Terai region. From July to September, the monsoon season brings an average annual rainfall of 1700 mm. Winters are cool and dry, with temperatures ranging from a minimum of 4°C to a maximum of 40°C.
2.2. Data Collection and Identification of Medicinal Plants
To ensure transparency and respect for participants, we clearly explained the study’s purpose, methods, and potential risks before each interview. All participants provided voluntary oral consent and were free to discontinue the interview at any point. We conducted semi-structured and structured face-to-face interviews to gather ethnobotanical data on medicinal plant use among local inhabitants. These interviews were conducted during multiple visits to the research area. 86 informants (57 male and 29 female) participated in the current study. Focusing on traditional healers with expertise in local medicine, we employed a purposive sampling technique to select participants. After the interviews, all collected data was securely stored. We adhered to the ethical guidelines established by the International Society of Ethnobiology (ISE) Code of Ethics throughout the research process. This ensured that our study posed no harm to the local community.
Furthermore, we followed the recommended standards for conducting ethnobotanical research (Weckerle et al. (2018). The interviews centered on the local population’s traditional knowledge regarding using wild plants for treating various ailments. Additionally, we meticulously verified the correct taxonomic classification and nomenclature of all identified vascular plants using the World Flora Online (WFO) database (
www.worldfloraonline.org). Finally, herbarium specimens with corresponding voucher numbers were deposited in the Jawaharlal Nehru University, New Delhi, India, for future reference.
2.3. Demography of Informants
To identify participants with deep knowledge of medicinal plants, we utilized a “snowball” sampling technique. This method involves initially selecting a random villager as the first informant. Subsequent participants are then recruited based on recommendations and referrals provided by the initial informant. This approach is particularly beneficial for reaching isolated or hard-to-reach populations that might be hesitant to participate in sociological studies.
The study area is home to various ethnicities and religions, with Hindi as the dominant language. We ensured participant inclusion from both genders and focused on individuals permanently residing in the villages under study. Seventy-two participants were interviewed, including 47 men and 25 women. The age range spanned from 30 to 75 years, with the majority (59.72%) falling between 40 and 60 (
Table 1). We documented each participant’s gender, age, education level, and occupation. Our participant pool encompassed individuals from various backgrounds, including farmers, homemakers, medicinal plant collectors, and traditional healers, ensuring a well-rounded representation of the local knowledge of medicinal plants.
2.4. Data Analysis
The gathered data were revised and organized using MS Excel following use reports. Scientific and local names, habits, parts used, modes of preparation, and medicinal uses are included in each column as attributes of that reference. SPSS software was used for statistical analyses.
2.5. Use Value (UV)
Use value (UV) was used to determine the relative importance of the medicinal plants (Phillips & Gentry 1993).
Ui is the number of use reports, citations, or mentions by each informant for a particular species, and N is the total number of informants who participated in the study. Low numbers signify fewer mentions or citations, whereas high values show a significant volume of use reports or citations from the informants. It counts as one use report or citation each time an informant identifies or describes a species of medicinal plant that is being used to treat a condition or for another reason.
2.6. Relative Frequency Citation (RFC)
The relative frequency of citation (RFC) was computed to know the importance of the species. The relative frequency citation (RFC) is used to determine the relative frequency of reference or mention from the study participants who served as informants were calculated using the formula:
Where FC is the number of informants cited or mentioned a plant, and N is the total number of informants (Tardio et al. 2008). The values closest to 1 show that nearly all informants mentioned a medicinal plant used to treat a particular illness. Low scores show that the usage or purpose of a medicinal plant species is mentioned by few, or occasionally by one, informant.
2.7. Informant Consensus Factor (ICF)
The informant consensus factor (ICF) was used to assess the homogeneity or degree of agreement of the informant’s knowledge about medicinal plants and calculated as follows:
where Nur represents the number of use reports or citations for each illness category, and Nt represents the number of species utilized in that specific category (Heinrich 1998).
2.8. Fidelity Level (FL)
The percentage of the most popular and valuable medicinal plant for a specific condition or use category was calculated using fidelity level (FL) using the formula:
where NP is the proportion of informants who cited or discussed using a medicinal plant to treat a specific disease category, and N is the total number of informants who cited the plant for any other use or purpose (Friedman J 1986). A medicinal plant with a high value will likely have many citations and be the most popular species for treating a specific condition.
2.9. The Jaccard Similarity Coefficient or Jaccard Index (JI):
This index is used to compare study data with other ethnobotanical studies conducted in other parts of India and other countries worldwide. The formula to evaluate the JI index (González-Tejero et al., 2008) was:
where “a” is the recorded number of species of the study area “A,” “b” is the documented number of species of the area “B,” and “c” is the common number of species in both areas “A” and “B.” In the case of indigenous communities, “a” is the number of species reported by an indigenous community “A,” “b” is the number of species cited by the indigenous community “B” and c is the number of species reported by both “A” and “B.”
3. Results
3.1. Demographic Characteristics
The study included 72 informants, and their information on age, gender, educational level, and healing experience are shown in
Table 1. Men represented 65.27% of informants, and women 34.72%. Based on age, informants were classified into three major categories, i.e., above 60, between 40 and 60, and less than 40. Elders (age above 60) had more plant knowledge than young people (age less than 40). Another reason for the lower understanding of young informants was their limited interest in herbal preparations due to changes in lifestyle with the advent of industrialization and modernization. Informants were from different educational backgrounds (
Table 2), with the majority (36.12%) being educated up to the secondary level. The results showed that informants with a high school degree mentioned more plant names than those with a graduate degree. Highly educated informants usually relied on allopathic medicines for their immediate healthcare and had the slightest knowledge about herbal drugs and their preparation methods. Out of 72 informants, 21 were traditional healers (Key informants). There was a difference between key and general informants; the key informants had higher levels of knowledge than general informants. Likewise, traditional health practitioners had a broad conventional understanding of the medicinal uses of plants compared to other professions.
3.2. Diversity and Growth Form of Medicinal Plants
The analysis of the field documentation revealed that the indigenous people of the Suhelwa region used 137 medicinal plants from 55 plant families. With a total of 16 species (11.68%).
The analysis of the field documentation revealed that the indigenous people of the Suhelwa region used 137 medicinal plants from 55 plant families. With 16 species (11.68%), the Fabaceae family had the most representation and was followed by 13 species (9.56%) of Poaceae, seven species (5.10%) of Asteraceae and Moraceae, six species (4.36%) of Apocynaceae and Acanthaceae, Combretaceae, Euphorbiaceae and Malvaceae have five species each (
Table 2). Herbs, shrubs, trees, climbers, and liana were the preferred growth forms of the therapeutic plants in the study area.
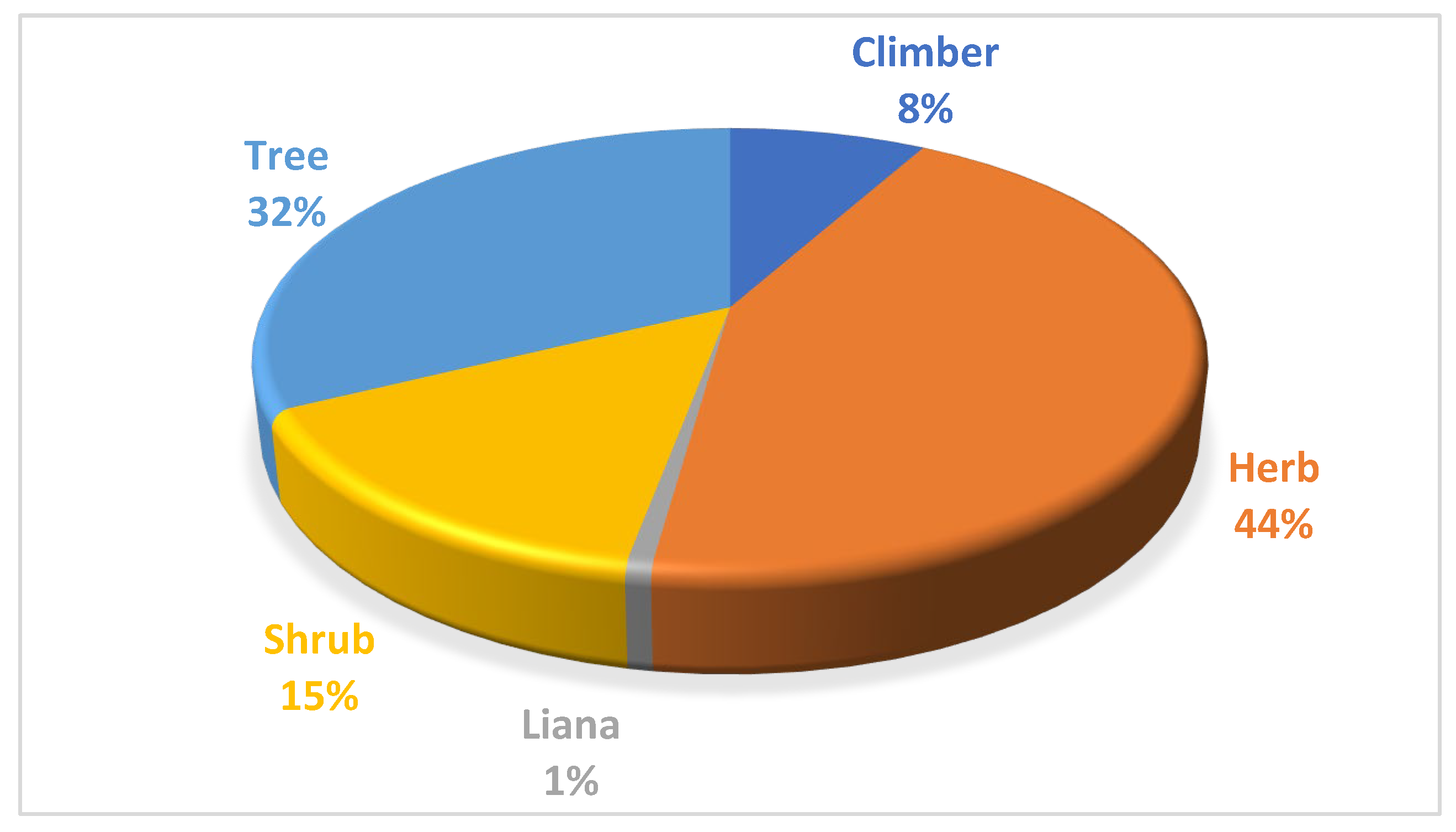
The herbaceous life form was dominantly (60 sp.; 44%) used in herbal preparation, followed by 45 species (32%)) of trees, 20 species of shrubs (15%), 11 species (8%) of climbers, and one species of liana (
Figure 1).
3.3. Plant Part Used
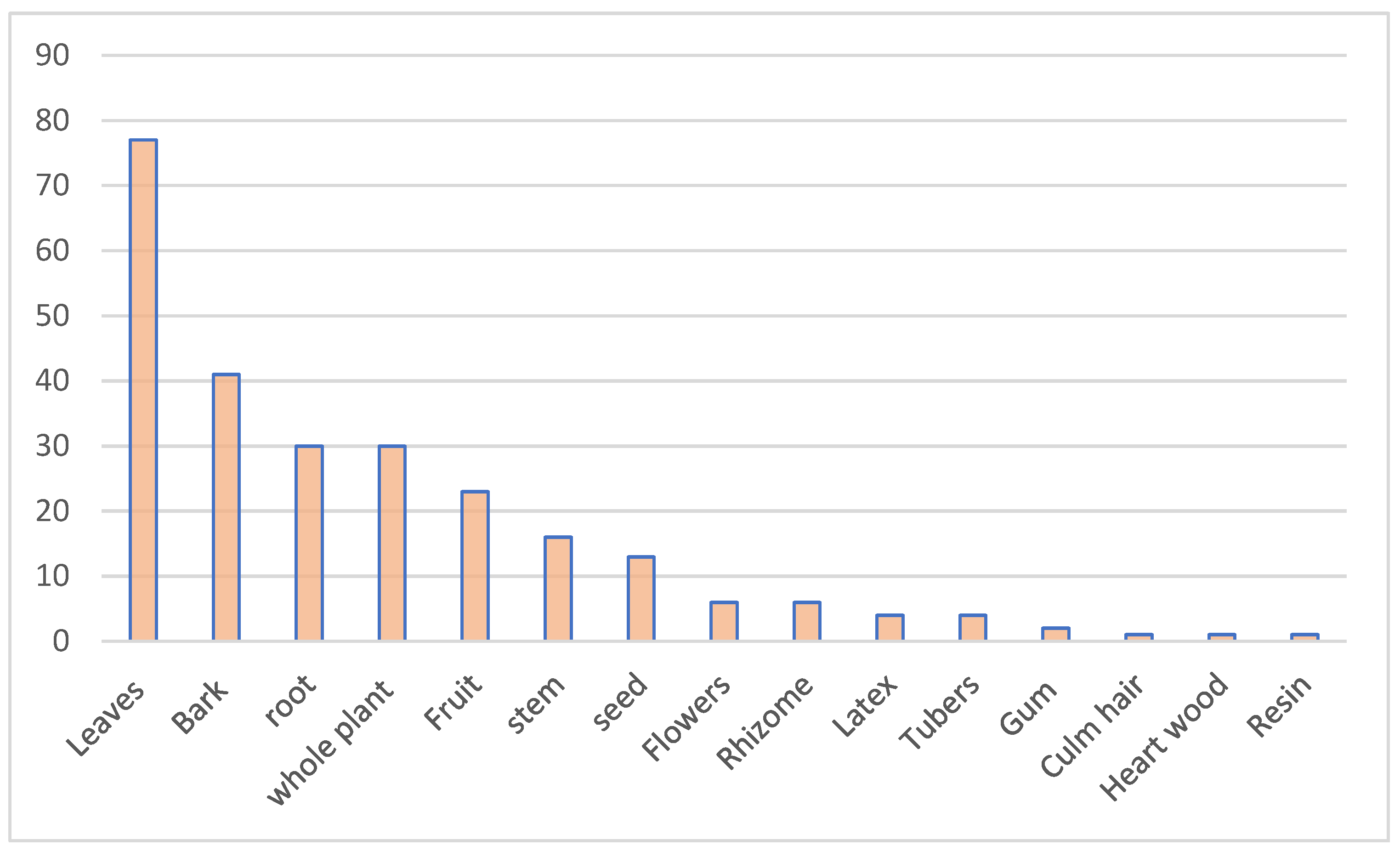
Different plant components, such as bark, flowers, fruits, leaves, rhizomes, roots, seeds, stems, tubers, whole plants, latex, tubers, gum, culm hair, heartwood, and resin, are utilized in traditional medicine in the study area. The majority of plant parts employed were the leaves from 75 species (54.74%), bark from 41 species (29.92%), roots and whole plants from 30 species (21.89%) (
Figure 2).
3.4. Mode of Preparation and Administration
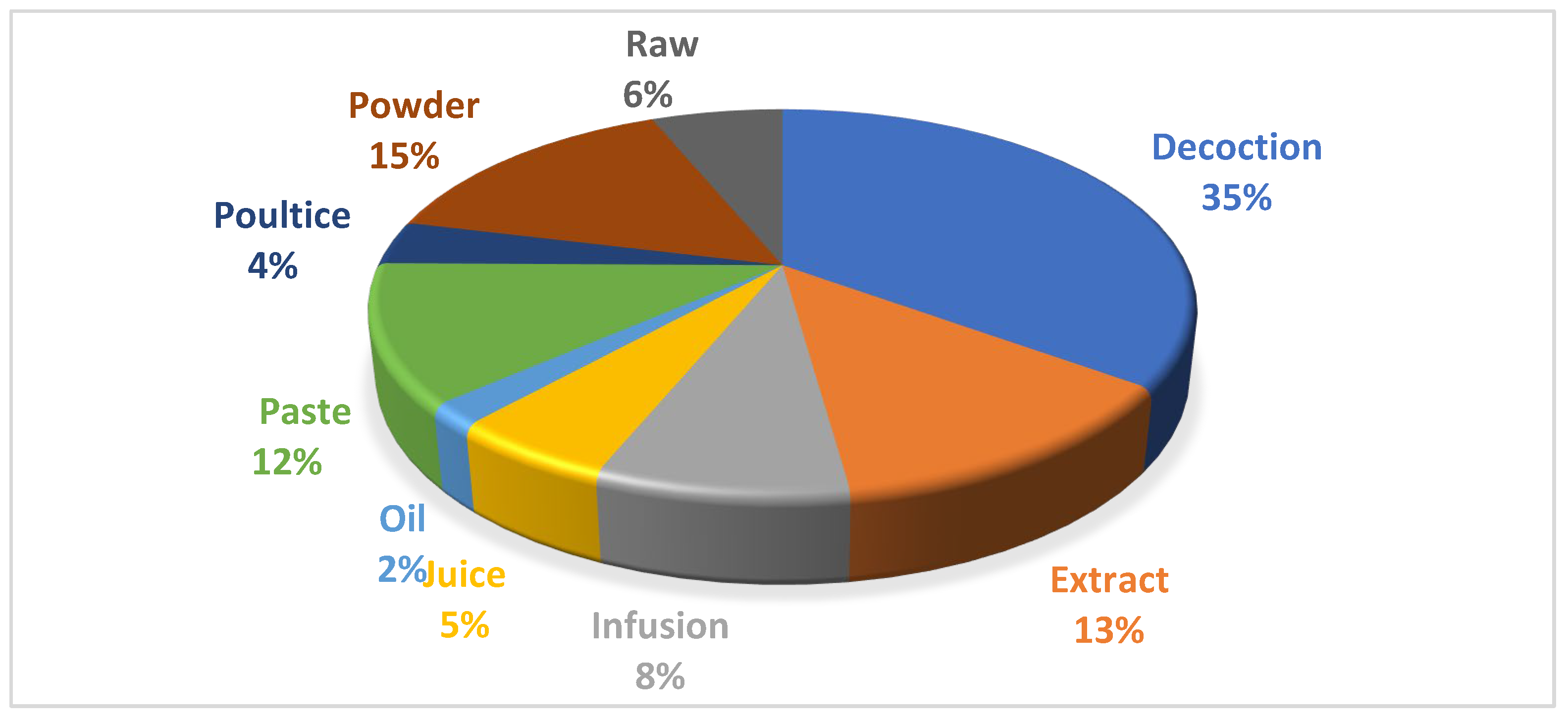
The indigenous people from the study area prepared different recipes from medicinal plants using various methods based on the type of disease treated. The decoction was the most common method (96 sp.; 35%) for the preparation of herbal recipes, followed by powder (41 sp.; 15%), extract (35 sp.; 13%), Paste (32 12%), and Infusion (23 sp.; 8%) (
Figure 3). Traditional medicines can be delivered orally, topically, by fumigation, or inhalation. Oral uptake was the main route of administration in the study area.
3.5. Informant Consensus Factor (ICF)
The informant consensus factor was analyzed based on disease categories, as a single plant might be used to treat 3–4 or more disease categories. Ailments were classified into 16 categories to develop informant consensus. The ICF value ranged from 0.86 to 0.96. The maximum value of ICF was estimated for the digestive disease category (0.96), followed by skin problems, respiratory disorders, and general symptoms (0.94) each (
Table 3). The general system listed diseases included body pain, inflammation, dandruff, Allergies, Heat stroke, and fever. While the neoplasms had the lowest ICF score (0.86), the listed diseases included Cancer and tumors.
3.6. Relative Frequency of Citation (RFC) and Use Value (UV)
The RFCvalueC ranged between 0.99 and 0.04. Azadiracta indica had highest RFC value (0.99). Other plant species with significant RFC values (>0.90) were Acacia catechu, Accacia nilotica, Asparagus racemosus, Ficus religeosa, Shorea robusta, Syzygium cumini, Tinospora cardifolia, Vetiveria zizanioides, and Xanthium strumarium (annexure 1). The lowest RFC value (0.04) was reported for Mimosa himalayana.
To determine the use value (UV) of the documented medicinal plants, we employed the use report (UR), which revealed the preferred medicinal plants used by the people of study area (annexure 1). The use value ranged between 1.24 and 0.04. Azadiracta indica had the highest UV(1.24). Other plant species with UV (> 1or =1) are Ocimum basilicum, Syzygium cumini, Tinospora cardifolia, Acacia catechu, Asparagus racemosus, Shorea robusta, Ficus religeosa, Accacia nilotica, Annona squamosal, Ficus racemosa and Vetiveria zizanioides. While other species with significantly high use value were Xanthium strumarium (0.95), Terminallia belerica (0.95), Physalis miniama (0.93), Hygrooryza ariatata(0.91), Haldina cardifolia(0.90), and Cassia fistula(0.90).
3.7. Jaccard Index
A comparison with data reported by ethnobotanists from other regions of India and internationally was performed using the Jaccard Index (
Table 4). The original application information of ethnomedicinal plants within our study was compared with 11 previous ethnobotanical research studies published from different countries including India. The JI ranged from 0.43 to 19.39. The top three highest degree of similarities was recorded from India with studies conducted by Upadhyay D (2016) with a JI of 19.39, followed by Ahirwar and Gupta (2024) with a JI of 14.41 and Prajapati et. al. (2018) with a JI of 10.82 (Table 5). Among other countries, the highest similarity was recorded from Pakistan with a JI of 2.95 and Sudan with JI 2.08.
4. Discussion
The indigenous and local knowledge of medicinal plant use is still higher among the older (age groups > 40) than among the younger across ethnic groups (Tamene et al. 2024 ; Beltrán-Rodríguez et al. 2014; Sharma et al. 2019). According to Silva et al. (2011) older people have more opportunities for cultural interaction and familiarity with plants and their therapeutic benefits than younger. Another reason for the lower knowledge of young informants was their limited interest in herbal preparations due to changes in lifestyle with the advent of industrialization and modernization (Regassa, 2013). The results showed that informants with a high school degree mentioned much more plants than those with graduate. Illiterate and lower-grade informants have reported more medicinal plants than higher-grade informants (Tamene et al. 2024; Kutal D et el 2021). Highly educated informants usually relied on allopathic medicines for their immediate healthcare and had the least knowledge about herbal medicines and their preparation methods. There was a difference between key and general informants; the key informants had higher levels of knowledge than general informants. Traditional healers had a broad conventional understanding of the medicinal uses of plants compared to other professions. Traditional healers are involved in the care of all types of diseases, both psychological and somatic (Denise Baratti-Mayer 2019; Ralte L 2024).
As shown in the present study’s findings, the use of plant species indicated that local people had good ethnobotanical knowledge about the specific plants and plant parts to use for their daily healthcare purposes. Other studies in India have found similar findings. For example, Meena & Yadav (2010) listed 31 plants from 22 families in the southern part of Rajasthan; Upadhyay (2016) documented 60 plants from 30 families in the Katarniaghat Wildlife Sanctuary situated in the Terai region of Uttar Pradesh. Singh et al. (2017) found 73 medicinal plant species belonging to 46 families in the Rudraprayag district, western Himalaya. In addition, several similar studies were conducted in protected areas in other parts of the world; for example, Kose et al. (2015) documented 80 medicinal plant species in the Maseru district of Lesotho; Mechaala et al. (2022) enlisted 60 local medicinal plant species in the El Kantara’s area (Algerian Sahara gate); while Polat R (2019) reported 93 medicinal plant species around a traditional protected area in the Bingöl region of Turkey. Furthermore, Mincheva et al. (2022) documented 114 medicinal plant species in Bulgarian Mountain Rhodopes; Amjad et al. (2020) recorded 150 medicinal plants in Harighal, Azad Jammu & Kashmir, Pakistan; and Dery et al. (2023) reported 94 species in Sissala East municipality of the Upper West region, Ghana. In the present study, survey data and field observation confirmed that.
The analysis of the field documentation revealed that with 16 species (11.68%), the Fabaceae family had the most representation and was followed by Poaceae, Asteraceae, and Moraceae (
Table 3). Our findings agree with previous reports (Tamene et al. 2024; Teshome et al. 2023). The prevalence of these families might be due to their abundance and easy accessibility in the study area. Herbs, shrubs, trees, climbers, and liana were the preferred growth forms of the therapeutic plants in the study area. The herbaceous life form was dominantly used in herbal medicine preparation. These observations are per previous reports (Agize et al. 2022; Faruque 2018; Tamene et al.2024). The availability of herbs throughout the study area and their ease of collection may have been the main reasons for this.
In this study, leaves are the most commonly used plant for herbal medicine preparation. A higher preference for leaves over other plant parts could be due to ease of preparation and better treatment of a disease. While using leaves for medicinal preparations may not pose a significant threat to plant species, utilizing other parts, such as roots, bark, and stems, can have negative consequences. The overharvesting of these plant parts can disrupt the ecological balance and potentially endanger the survival of medicinal plant species. Therefore, it is crucial to implement proper conservation and sustainable measures to protect these plants and ensure their long-term viability. This finding aligns with the results of other ethnobotanical studies (Faruque et al., 2018; Teshome et al., 2023; Tamene et al. 2024), which reported that leaves were the most cited plant parts used in remedy preparations.
The indigenous people from the study area prepared different recipes from medicinal plants using different methods based on the type of disease treated. Decoction was the most common method (96 sp.; 35%) for the preparation of herbal recipes; informants reported that most medicinal plants are used in decoction to dissolve the chemicals of the material and extract its constituents using water (Agize et al., 2022; Zaigham et al., 2019). It was found that many respondents take these medicinal plants orally, which is consistent with previous research in other parts of the world where oral intake was reported as the main route of administration (Mood 2008; Kadir et al. 2012; Rehman et al. 2017). Most medicinal plants are ingested as decoctions and juices, whereas for the treatment of external ailments such as wounds, sores, and skin rashes, ground plant parts are made into a paste (Kose et al. 2015). The informant consensus factor (ICF) value shows the high dependence of local inhabitants on medicinal plants (Uddin and Hassan 2014), and low ICF values indicate less steadiness of the informant’s knowledge.
The informant consensus factor (ICF) value was analyzed based on disease categories, as a single plant might be used to treat 3–4 or more disease categories. As in the present study, the maximum ICF for digestive diseases was reported by other studies (Singh et al. 2012; Umair et al. 2017; Amjad et al. 2020; Dery et al. 2023) in their investigated area. The second-highest ICF was recorded for respiratory disorders, possibly due to the prevalence of cold and moist conditions in the study area (Amjad et al., 2020). Gastrointestinal (GIT) disorders (i.e., constipation, indigestion, gastric trouble, dysentery, acidity, and stomach ulcer), skin diseases (pimples, pustules, and ringworm), respiratory tract infections (bronchitis, asthma, pneumonia), were the common health problems. The prevalence of gastrointestinal (GI) disorders may be attributed to poor available hygiene. The harsh and hostile weather might contribute to respiratory infections, and the limited sanitary facilities might contribute to intestinal problems (Bibi et al., 2022).
Relative frequency of citation (RFC) is used to identify the significant species in various ailments as cited by local people (Vitalini et al. 2013). The score varies from 0 to 1; implying that the informants provided more knowledge about a plant species (Medeiros et al. 2011). More plant species with high RFC value in the study area indicate that the local people were much familiar with their ethnomedicinal uses over a long period. The highest RFC reported for
A. indica is reported for curing diabetes, skin problems, wounds, and piles, supported by previous studies (Sujarwo et al. 2016; Reddy & Neelima 2022). The second top RFC-valued plant is
S. cumin (0.98), which is also very important and is reported for diabetes, Sore throat, bronchitis, asthma, thirst, biliousness, dysentery, and ulcers burns, cuts and wounds, pain, piles, etc. that is supported by the previous studies (Ayyana and Subash-Babu 2012). To determine the use value (UV) of the documented medicinal plants, we employed the use report (UR), which revealed the preferred medicinal plants used by the people of the study area (Table 5). Plant species with more use reports have high use values and vice versa (Qaseem et al. 2019; Amjad et al. 2017). The high use of these plant species indicates the common occurrence and importance among healers as they frequently use these plants in herbal therapies for various ailments. The UV indicates the local importance of plant species against different ailments. The plants with the most minor UV, as indicated in
Table 2, were more effective against various ailments and could be used in other therapeutic uses. Hence, these plants can be used to develop human pharmaceuticals (Rehman et al. 2017).
The RFC and UV are constant in particular areas. However, they may change according to the variation in the knowledge of indigenous people from area to area or within the area (Amjad et al., 2020). Species with high RFC and UV are prioritized for conservation and sustainable use; otherwise, they will be extinct from the area shortly (Farooq et al., 2019) Therefore, the medicinal plants with high UV scores and RFC values should be further evaluated for their phytochemically and phytopharmacologically important substances to identify their active constituents for discovering new drugs (Vitalini et al., 2009; Kayani et al., 2014; Mukherjee, 2012; Amjad et al., 2020).
The high similarity in the Jaccard Index reflects similar cultures, traditions, vegetation, and geography among the areas. In contrast, JI’s high differences or lowest value of JI reflects that areas do not share common cultural values. Further, ethnoecological knowledge is often influenced explicitly by the origin and culture of indigenous communities.
5. Conclusion
An extensive survey of medicinal plants and traditional healthcare practices among indigenous communities revealed their exclusive reliance on plant-based ethnomedicine for daily healthcare needs. Sustainable harvesting and cultivation practices are crucial for conserving these invaluable plant species. Collaboration between various stakeholders can boost medicinal plant production and usage, which is essential for rural sustainable development. Traditional medicine practices, passed down through generations, face challenges from modern medicine. Documenting the knowledge of senior citizens is vital, as younger generations need more understanding due to the availability of modern drugs—quantitative indices aid in identifying valuable plants and developing conservation strategies. The high informant consensus factor underscores the reliability of gathered data for future ethnopharmacological research. Further studies are recommended to validate and explore the therapeutic potential of cited plants for developing alternative drugs.
Acknowledgments
We warmest thanks to the School of Environmental Sciences, Jawaharlal Nehru University, for the valuable support.
References
- Abu-Odeh, A.M.; Talib, W.H. Middle East Medicinal Plants in the Treatment of Diabetes: A Review. Molecules 2021, 26, 742. [Google Scholar] [CrossRef] [PubMed]
- et al. Journal of Ethnobiology and Ethnomedicine (2020) 16:65.
- Ahirwar, R.K.; Gupta, V.K. Quantitative ethnomedicinal investigation of medicinal plants used by traditional healers to treat various diseases in the district Dindori, Madhya Pradesh, India. Ethnobot. Res. Appl. 2024, 28, 1–31. [Google Scholar] [CrossRef]
- Amjad MS, 2017 Faisal Qaeem M, Ahmad I, Khan SU, Chaudhari SK, Malik NZ, Shaheen H, Khan AM. Descriptive study of plant resources in the context of the ethnomedicinal relevance of indigenous flora: A case study from Toli Peer National Park, Azad Jammu and Kashmir, Pakistan. PlosOne. 2017;12(2):e0171896].
- Amjad1M S, Zahoor U, Bussmann RW, Altaf M, Gardazi S M H, Abbasi A M (2020) Ethnobotanical survey of the medicinal flora of Harighal, Azad Jammu & Kashmir, Pakistan Journal of Ethnobiology and Ethnomedicine 16:65.
- Axiotis, E.; Halabalaki, M.; Skaltsounis, L.A. An Ethnobotanical Study of Medicinal Plants in the Greek Islands of North Aegean Region. Front. Pharmacol. 2018, 9, 409. [Google Scholar] [CrossRef] [PubMed]
- Bajpai, O.; Kushwaha, A.K.; Srivastava, A.K.; Pandey, J.; Chaudhary, L.B. Phytosociological Status of a Monotypic Genus Indopiptadenia: A Near Threatened Tree from the Terai-Bhabar Region of Central Himalaya. Res. J. For. 2015, 9, 35–47. [Google Scholar] [CrossRef]
- Beltrán-Rodríguez, L.; Ortiz-Sánchez, A.; A Mariano, N.; Maldonado-Almanza, B.; Reyes-García, V. Factors affecting ethnobotanical knowledge in a mestizo community of the Sierra de Huautla Biosphere Reserve, Mexico. J. Ethnobiol. Ethnomedicine 2014, 10, 14–14. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Sharma, A.; Cooper, R.; Bhardwaj, G.; Gaba, J.; Mutreja, V.; Chauhan, A. A comprehensive phytochemical, ethnomedicinal, pharmacological ecology and conservation status of Picrorhiza kurroa Royle ex Benth.: An endangered Himalayan medicinal plant. Process. Biochem. 2021, 109, 72–86. [Google Scholar] [CrossRef]
- Bibi F(2022, Abbas Z, Harun N, Perveen B, Bussmann RW (2022) Indigenous knowledge and quantitative ethnobotany of the Tanawal area, Lesser Western Himalayas, Pakistan. PLoS ONE 17(2): e0263604.
- Boudjelal A, C. Henchiri, M. Sari, D. Sarri, N. Hendel, A. Benkhaled, G. Ruberto, Herbalists and wild medicinal plants in M’Sila (North Algeria): an ethnopharmacology survey, J. Ethnopharmacol. 148 (2013) 395–402. [CrossRef]
- WHO. Traditional medicine: growing needs and potentials. 2002.
- Calzada, F.; Bautista, E. Plants used for the treatment of diarrhoea from Mexican flora with amoebicidal and giadicidal activity, and their phytochemical constituents. J. Ethnopharmacol. 2020, 253, 112676. [Google Scholar] [CrossRef]
- Chander MP, C. Kartick, J. Gangadhar, P. Vijayachari, Ethno medicine and healthcare practices among Nicobarese of Car Nicobar - an indigenous tribe of Andaman and Nicobar Islands, J. Ethnopharmacol. 158 (2014) 18–24. [CrossRef]
- Debnath P, Rathore S, Walia S, Kumar M, Devi R, Kumar R (2020) Picrorhiza kurroa: a promising traditional therapeutic herb from higher altitude of western Himalayas. J Herb Med 23:100358.
- Baratti-Mayer, D.; Daou, M.B.; Gayet-Ageron, A.; Jeannot, E.; Pittet-Cuénod, B. Sociodemographic Characteristics of Traditional Healers and Their Knowledge of Noma: A Descriptive Survey in Three Regions of Mali. Int. J. Environ. Res. Public Heal. 2019, 16, 4587. [Google Scholar] [CrossRef] [PubMed]
- Dery G , Dzitse S, Tom-Dery D(2023)Ethnobotanical survey of medicinal plants in Sissala East municipality of the upper West region, Ghana Phytomedicine Plus 3 100461.
- Emre, G.; Dogan, A.; Haznedaroglu, M.Z.; Senkardes, I.; Ulger, M.; Satiroglu, A.; Emmez, B.C.; Tugay, O. An Ethnobotanical Study of Medicinal Plants in Mersin (Turkey). Front. Pharmacol. 2021, 12. [Google Scholar] [CrossRef]
- Everest, A.; Ozturk, E. Focusing on the ethnobotanical uses of plants in Mersin and Adana provinces (Turkey). J. Ethnobiol. Ethnomedicine 2005, 1, 6–6. [Google Scholar] [CrossRef]
- Farooq, A.; Amjad, M.S.; Ahmad, K.; Altaf, M.; Umair, M.; Abbasi, A.M. Ethnomedicinal knowledge of the rural communities of Dhirkot, Azad Jammu and Kashmir, Pakistan. J. Ethnobiol. Ethnomedicine 2019, 15, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Faruque MO, Uddin SB, Barlow JW, Hu S, Dong S, Cai Q, Li X and Hu X (2018) Quantitative Ethnobotany of Medicinal Plants Used by Indigenous Communities in the Bandarban District of Bangladesh. Front. Pharmacol. 9:40. [CrossRef]
- Ghimire BK, Tamang JP, Yu CY, Jung SJ, Chung IM. Antioxidant, antimicrobial activity and inhibition of α-glucosidase activity by Betula alnoides Buch. bark extract and their relationship with polyphenolic compounds concentration. Immunopharmacol Immunotoxicol. 2012;34:824–31. [CrossRef]
- González-Tejero, M.; Casares-Porcel, M.; Sánchez-Rojas, C.; Ramiro-Gutiérrez, J.; Molero-Mesa, J.; Pieroni, A.; Giusti, M.; Censorii, E.; de Pasquale, C.; Della, A.; et al. Medicinal plants in the Mediterranean area: Synthesis of the results of the project Rubia. J. Ethnopharmacol. 2008, 116, 341–357. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, M. Ethnobotany and its role in drug development. Phytotherapy Res. 2000, 14, 479–488. [Google Scholar] [CrossRef]
- Harris, F. Mohammed S.. 2003. Relying on nature: Wild foods in Northern Nigeria. Ambio 32: 24–29.
- Heinrich, M. Ethnobotany and its role in drug development. Phytotherapy Res. 2000, 14, 479–488. [Google Scholar] [CrossRef]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: healers' consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Yaniv, Z.; Dafni, A.; Palewitch, D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J. Ethnopharmacol. 1986, 16, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Huai HY, Pei SJ. Medicinal ethnobotany and its advances. Chin Bull Bot. 2002;2(19):129–36.
- Jain, S. K. (Ed.) 2004. A Manual of Ethnobotany.: Scientific Publishers, Jodhpur, India.
- Joshi, A.R. , Joshi, K., 2006. Trend of ethnobotanical research and conservation of useful species in Nepal. Bionotes 9, 6.
- Joshi, N.; Ghorbani, A.; Siwakoti, M.; Kehlenbeck, K. Utilization pattern and indigenous knowledge of wild medicinal plants among three ethnic groups in Makawanpur district, Central Nepal. J. Ethnopharmacol. 2020, 262, 113219. [Google Scholar] [CrossRef]
- et al. 2014, Ahmad M, Zafar M, Sultana S, Khan MPZ, Ashraf MA, Hussain J, Yaseen G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, Northern Pakistan. J Ethnopharmacol. 2014;156:47–60.
- Kunwar, R.M.; Baral, K.; Paudel, P.; Acharya, R.P.; Thapa-Magar, K.B.; Cameron, M.; Bussmann, R.W. Land-Use and Socioeconomic Change, Medicinal Plant Selection and Biodiversity Resilience in Far Western Nepal. PLOS ONE 2016, 11, e0167812. [Google Scholar] [CrossRef] [PubMed]
- Kunwar, R.M.; Baral, K.; Paudel, P.; Acharya, R.P.; Thapa-Magar, K.B.; Cameron, M.; Bussmann, R.W. Land-Use and Socioeconomic Change, Medicinal Plant Selection and Biodiversity Resilience in Far Western Nepal. PLOS ONE 2016, 11, e0167812. [Google Scholar] [CrossRef]
- Ford, J.D.; King, N.; Galappaththi, E.K.; Pearce, T.; McDowell, G.; Harper, S.L. The Resilience of Indigenous Peoples to Environmental Change. One Earth 2020, 2, 532–543. [Google Scholar] [CrossRef]
- Kumar, M.; Radha; Devi, H. ; Prakash, S.; Rathore, S.; Thakur, M.; Puri, S.; Pundir, A.; Bangar, S.P.; Changan, S.; et al. Ethnomedicinal Plants Used in the Health Care System: Survey of the Mid Hills of Solan District, Himachal Pradesh, India. Plants 2021, 10, 1842. [Google Scholar] [CrossRef] [PubMed]
- Kutal, D.; Kunwar, R.M.; Baral, K.; Sapkota, P.; Sharma, H.P.; Rimal, B. Factors that influence the plant use knowledge in the middle mountains of Nepal. PLOS ONE 2021, 16, e0246390. [Google Scholar] [CrossRef] [PubMed]
- Macuja, J.C.O.; Ruedas, L.N.; España, R.C.N. Utilization of Cellulose fromLuffa cylindricaFiber as Binder in Acetaminophen Tablets. Adv. Environ. Chem. 2015, 2015, 1–8. [Google Scholar] [CrossRef]
- Maharjan R, Thapa R, Nagarkoti S, Sapkota P. Ethnobotanical uses of home garden species around Lalitpur district, Nepal. Asian J Pharmacogn. 2021;4(2):10–22.
- Meena KL & Yadav BL (2010) Some ethnomedicinal plants of Southern Rajasthan. Indian Journal of Traditional Knowledge Vol. 9 (1), January, pp.
- Medeiros MFT, Silva O, Albuquerque U (2011) Quantification in ethnobotanical research: an overview of indices used from 1995.
- to 2009. Sitientibus Sér Ci Biol 11:211–230.
- Mehta, A. K. & Shah A.. 2003. Chronic poverty in India: Incidence, causes and policies. World Development 31: 491–511.
- et al. , 2021Mechaala, S., Bouatrous, Y., Adouane, S., 2021. Traditional knowledge and diversity of wild medicinal plants in El Kantara’s area (Algerian Sahara gate): an ethnobotany survey. Acta Ecol. Sin. 42 (1), 33–45. [CrossRef]
- Moghadam, E.T.; Yazdanian, M.; Tahmasebi, E.; Tebyanian, H.; Ranjbar, R.; Yazdanian, A.; Seifalian, A.; Tafazoli, A. Current herbal medicine as an alternative treatment in dentistry: In vitro, in vivo and clinical studies. Eur. J. Pharmacol. 2020, 889, 173665. [Google Scholar] [CrossRef] [PubMed]
- Muhakr M AY M, Ahmed I M, El hassan G O M, Yagi S (2024) Ethnobotanical study on medicinal plants in Melit area (North Darfur), Western Sudan. 3: Journal of Ethnobiology and Ethnomedicine 20.
- Mukherjee, P.K.; Nema, N.K.; Venkatesh, P.; Debnath, P.K. Changing scenario for promotion and development of Ayurveda – way forward. J. Ethnopharmacol. 2012, 143, 424–434. [Google Scholar] [CrossRef] [PubMed]
- Nisha, V. M. & M. Sivadasan. 2007. Ethnodermatologically significant plants used by traditional healers of Wayanad district, Kerala. Ethnobotany 19: 55–61.
- Pan Y, R.A. Birdsey, O.L. Phillips, R.B. Jackson, The structure, distribution, and biomass of the world’s forests, Annu. Rev. Ecol. Evol. Syst. 2013. [Google Scholar]
- https://doi.org/10.1146/annurev-ecolsys-110512-135914. [CrossRef]
- Phillips, O.; Gentry, A.H. The useful plants of Tambopata, Peru: I. Statistical hypotheses tests with a new quantitative technique. Econ. Bot. 1993, 47, 15–32. [Google Scholar] [CrossRef]
- Prajapati SK, Sharma K, Singh P K (2018) Plant diversity in tropical dry deciduous forests of Jashpur, Chhattisgarh with special reference to their ethnomedicinal uses Tropical Ecology 59(3): 505–514, ISSN 0564-3295.
- Qaseem MF, Qureshi R, Amjad MS, Waseem M, Sajid A. Ethnobotanical evaluation of tridational medicinal plants among thre rular communities of Goi and Dhanwa union council, District Kotli, Azad Jammu & Kashmir. Appl Ecol Environm Res. 2019;6(2):340–9.
- Rahman S, Jan G, Jan F G, Jawairya S, Hashmi, Rahim H U (2024) Exploration of ethnomedicinal plants, diversity and their practices in human healthcare in Tehsil Mandan, District Buner, Khyber Pakhtunkhwa, Pakistan Ecological Frontiers Volume 44, Issue 1, February, Pages 143-154.
- Rawat R, Vashistha DP (2011) Common herbal plant in Uttarakhand, used in the popular medicinal preparation in Ayurveda. Int J Pharmacognosy Phytochem Res 3(3):64–73.
- Ralte et al. Ralte L 1, Sailo H Singh Y. T(2024) 2Ethnobotanical study of medicinal plants used by the indigenous community of the western region of Mizoram, India Journal of Ethnobiology and Ethnomedicine 20.
- Regassa, R. “Assessment of indigenous knowledge of medicinal plant practice and mode of service delivery in Hawassa city, southern Ethiopia,” Journal of Medicinal Plants Research, vol. 7, no. 9, pp. 517–535, 2013.
- Rehman MN, Ahmad M, Sultana S, Zafar M, Edwards S (2017) Relative popularity level of medicinal plants in Talagang, Punjab Province, Pakistan. 7: Rev Bras Farmacogn 27.
- Rosero-Toro, J.H.; Romero-Duque, L.P.; Santos-Fita, D.; Ruan-Soto, F. Cultural significance of the flora of a tropical dry forest in the Doche vereda (Villavieja, Huila, Colombia). J. Ethnobiol. Ethnomedicine 2018, 14, 22. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Thakur, D.; Uniyal, S.K. Plant-derived utility products: knowledge comparison across gender, age and education from a tribal landscape of western Himalaya. J. Ethnobiol. Ethnomedicine 2019, 15, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.d.S.; Ramos, M.A.; Hanazaki, N.; de Albuquerque, U.P. Dynamics of traditional knowledge of medicinal plants in a rural community in the Brazilian semi-arid region. Rev. Bras. de Farm. 2011, 21, 382–391. [Google Scholar] [CrossRef]
- Shanley, P. , Luz, L., 2003. The impacts of forest degradation on medicinal plant use and implications for health care in Estern Amazonia. Bioscience 53, 573–584.
- Singh A, Nautiyal MC Kunwar R M., Bussmann R W. (2017) Ethnomedicinal plants used by local inhabitants of Jakholi block, Rudraprayag district, western Himalaya, India. Journal of Ethnobiology and Ethnomedicine 13:49.
- Singh GK, Ahirwar RK. 2018. Phyto-diversity of Ethnomedicinal plants of Chanda forest range district Dindori, Madhya Pradesh. International Journal of Science and Research 6(1):213-216.
- Siva, R. 2007. Status of natural dyes and dye-yielding plants in India. Current Science 92: 916–925.
- Sikarwar, R. L. S. 2002. Ethnogynaecological uses of plants new to India. Ethnobotany 14: 112–115.
- Subramanyam, R., S. G. Newmaster, G. Paligath, & C. B. Newmaster. 2007. Exploring ethnobiological classifications for novel alternative medicine: A case study of Cardiospermum helicacabum L. (‘Madakathon’ Balloon vine) as a traditional herb for treating rheumatoid arthritis. Ethnobotany 19: 1–16.
- Singh J S and Chaturvedi R K (2017) Diversity of Ecosystem Types in India: A Review, Proc Indian Natn Sci Acad 83 No. 3 September pp.
- Tamene S, Mesele N, Fortunatus B M & Chiwona-Karltun L (2024). Influence of socio-demographic factors on medicinal plant knowledge among three selected ethnic groups in south-central Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2024, volume 20, Article number: 29.
- Tardio J, Pardo de Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain). Econ Bot. 2008;62:24–39.
- Teshome, M.; Kebede, F.; Yohannes, T. An Ethnobotanical Survey of Indigenous Knowledge on Medicinal Plants Used by Communities to Treat Various Diseases around Ensaro District, North Shewa Zone of Amhara Regional State, Ethiopia. Scientifica 2023, 2023, 1–19. [Google Scholar] [CrossRef]
- The ISE code of ethics, international society of ethnobiology, 2006. http://ethnobiology.net/code-of-ethics/.
- Timmermans, K. Intellectual property rights and traditional medicine: policy dilemmas at the interface. Soc. Sci. Med. 2003, 57, 745–756. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay D 2016 Ethnobotanicaly useful plants of Katarniaghat Wildlife Sanctuary, Uttar Pradesh, IndiaIJAR; 2(2): 24-29.
- Kose LS, Moteetee A, Vuuren SV. (2015) Ethnobotanical survey of medicinal plants used in the Maseru district of Lesotho Journal of Ethnopharmacology 170184–200.
- Vitalini, S.; Iriti, M.; Puricelli, C.; Ciuchi, D.; Segale, A.; Fico, G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—An alpine ethnobotanical study. J. Ethnopharmacol. 2012, 145, 517–529. [Google Scholar] [CrossRef] [PubMed]
- Weckerle, C.S.; de Boer, H.J.; Puri, R.K.; van Andel, T.; Bussmann, R.W.; Leonti, M. Recommended standards for conducting and reporting ethnopharmacological field studies. J. Ethnopharmacol. 2018, 210, 125–132. [Google Scholar] [CrossRef] [PubMed]
- World Health. WHO global report on traditional and complementary medicine 2019.World Health Organization (2019).
- World Health Organization (WHO) Global Centre for Traditional Medicine. Available online: www.who.int/initiatives/who-global-centre-for-traditional-medicine (accessed on 28 November 2023).
- World Health Organization (WHO) Global Centre for Traditional Medicine. 2023.
- Yaseen, G.; Ahmad, M.; Sultana, S.; Alharrasi, A.S.; Hussain, J.; Zafar, M.; Rehman, S.U. Ethnobotany of Medicinal Plants in the Thar Desert (Sindh) of Pakistan. J. Ethnopharmacol. 2015, 163, 43–59. [Google Scholar] [CrossRef]
- Zaigham H, Abdullah T, Akhtar A. Recent trend in traditional medicine dosage form and present status of Unani and Ayurvedic Medicine. IJPSR. 2019;10(4):1640–9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).