1. Introduction
Women are at greater risk for major depression compared to men worldwide and the causes of this discrepancy are still being investigated [
1]. Within the U.S., data from the 2013-2016 National Health and Nutrition Examination Survey (NHANES) showed an almost 2:1 sex ratio difference in depression prevalence [
2]. Biological factors, as well as environmental influences, may contribute to these differences [
1]. In addition to being at higher risk based on gender, some women also experience perinatal depression-related illnesses which may impact the health of mothers and their infants [
3,
4,
5,
6,
7]. Notably, antepartum depression has been associated with increased risk of preterm labor [
3,
5,
7], preeclampsia [
5], reduced fetal development [
3,
5], miscarriage [
5], cesarean sections and instrumental vaginal deliveries [
3], and admission to a neonatal care unit [
3]. Infants whose mother experienced antepartum depression are also at higher risk to have low-birth weight and stunted growth across the first year of life [
5]. Furthermore, the literature indicates a correlation between postpartum depression and child behavioral issues [
4], impaired motor and cognitive development [
6], infant sleep disturbances [
6], and difficulties with mother-infant bonding [
6,
8].
Emerging studies are seeking to evaluate the relationship between vitamin D concentration and mental health [
9,
10,
11,
12]. Vitamin D has several roles in the body namely related to calcium homeostasis, bone health, as well as immune function, gene expression, and neural function [
9,
13,
14]. As such, vitamin D deficiency may contribute to a myriad of diseases, including depression [
9,
13]. One hypothesis examines how vitamin D decreases the heightened neuronal levels of calcium that propel depression [
13]. Although the mechanism of how vitamin D contributes to depression remains unclear, correlations between low vitamin D concentration and depressive symptoms have been established in both men and women [
9], as well as specifically, pregnant [
11,
12,
15] and postpartum mothers [
10,
15]. Notably, to the research team’s knowledge, no study has analyzed breastfeeding status in conjunction with these factors.
The human body acquires vitamin D through dietary intake and endogenous synthesis from adequate sun exposure. Poor dietary patterns and reduced sunlight exposure may consequently lead to vitamin D insufficiency/deficiency. In the United States, the National Center for Health Statistics showed that from 2001-2006, women had a greater risk of vitamin D deficiency compared to men [
16] and another study reported a higher vitamin D concentration in men compared to women worldwide [
17]. Particularly, women of childbearing age exhibit increased risk of vitamin D deficiency compared to men, but pregnant or lactating women have decreased vitamin D deficiency risk compared to other women [
16]. Excluding the elderly population in countries with more supplement use, men have been shown to have increased vitamin D intake through nutrients and supplements compared to women [
18]. To ensure the maintenance of adequate maternal and fetal/infant health, increased dietary and supplemental vitamin D intake is recommended in expecting mothers [
19].
Many disparities exist in the U.S. maternal population with minority groups and lower socioeconomic status women experiencing higher rates of depression during pregnancy [
5]. The social determinants of health contribute to the well-being of family units and involve factors of education access, food security, work and home environment, healthcare access, financial stability, and quality of support systems. The social determinants of health are interconnected, impacting the physical and mental health of communities and therefore may influence the ability of mothers to exclusively breastfeed. Additionally, maternal mental health can not only impact maternal behaviors with the infant but also human milk composition; literature shows that maternal nutrition [
20] and stress levels [
21,
22] are associated with alters in human milk composition. For example, Ziomkiewicz et al found a positive correlation between stress reactivity and milk fat, long-chain unsaturated fatty acids, with a negative correlation between stress reactivity and milk lactose [
22]. With this in mind, infants of different feeding practices and home-life environments could be receiving distinct nutrients from one another, contributing to their overall health. Due to potential changes in milk composition, the impact of maternal vitamin D concentration and postpartum depression may have health implications for infants who are breastfed compared to formula-fed.
Depression is a complex medical condition caused or influenced by many factors.
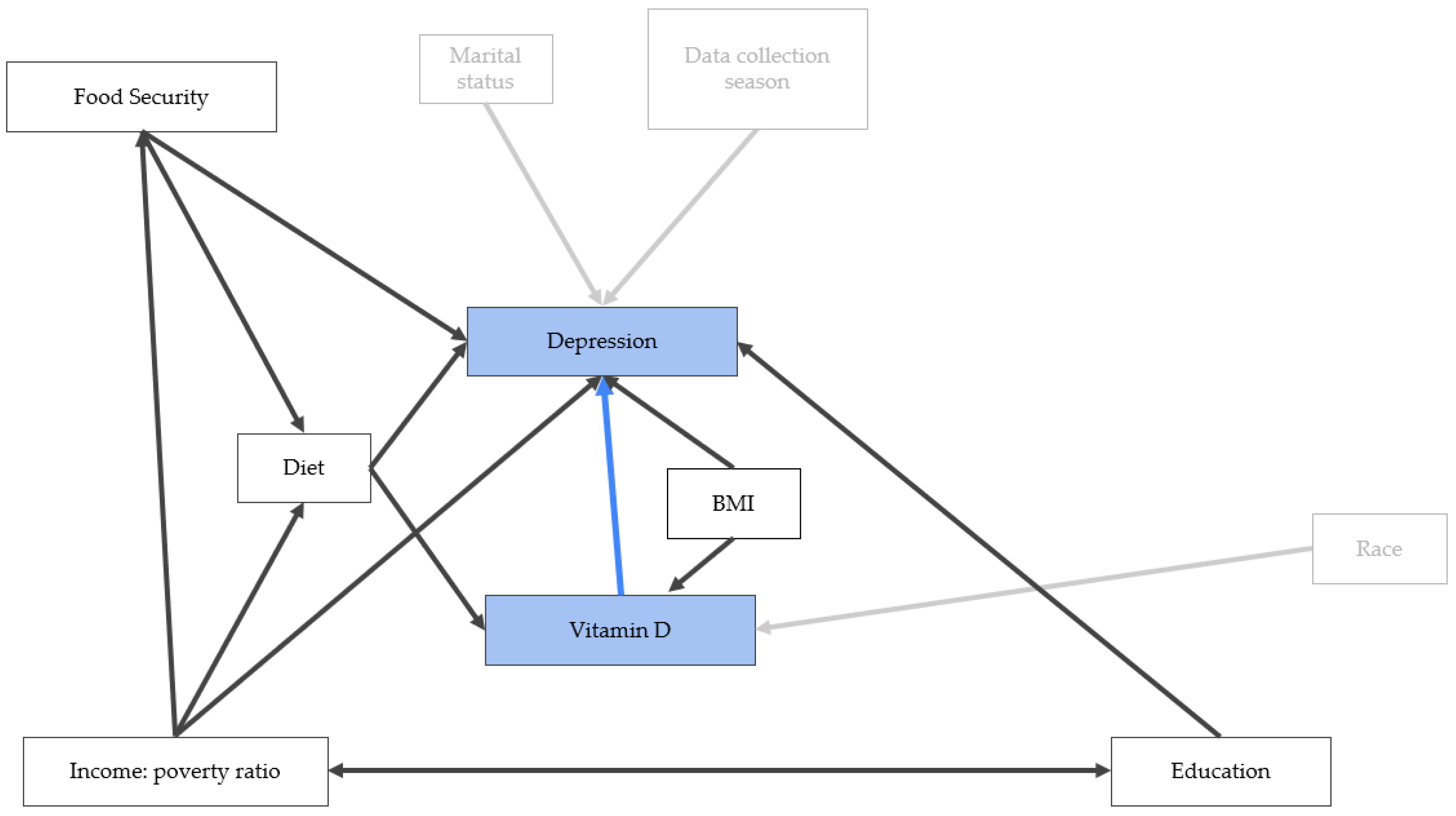
Figure 1 shows the directed acyclic graph created to visualize the relationships between vitamin D, depression and other intervening factors that can impact both depression and vitamin D concentration and hence are possible confounding variables. Diet is a confounding factor, influencing both depression [
23,
24,
25] and vitamin D concentration [
14]. Additionally, diet is a mediating factor for the influence of other variables on depression and vitamin D concentration. For example, food security status has a negative correlation with depression status [
26,
27,
28]. We did not find evidence in the literature that food security is directly influencing vitamin D concentration, but food security was shown to influence diet [
29,
30] and thus can indirectly impact vitamin D concentration. The income-to-poverty ratio may influence a person’s food security [
30] and diet [
31], providing secondary influences to depression and vitamin D concentration. Income-to-poverty ratio and education attainment can both influence one another; generational financial status has implications on educational achievements [
32], while educational achievement further impacts income opportunity. A negative correlation between education level and depression was also identified in the literature [
33,
34]. Marital status, race, and data collection season were not found to be confounding factors. Instead, marital status [
35,
36] and season [
37] were associated with depression, while race was correlated with vitamin D concentration [
38,
39,
40]. Body mass index (BMI) has been positively correlated to depression [
41] and despite negative correlations seen in the literature with BMI and vitamin D concentration [
38,
42,
43,
44], it was not included in the analyses as a confounding variable due to the complexity of influencing factors on BMI, including diet, physical activity, stress, genetics, environment, and more [
45].
Women are at greater risk for depression than men, and some women experience maternal-related impacts on their mental health affecting both themselves and their infants. Vitamin D concentration and depression have been shown to have a negative correlation in several studies and further investigations of this relationship are imperative to understanding populations at greatest risk and health interventions needed. The objective of this study was to investigate associations of serum vitamin D concentration with depressive symptoms and assess the impact serum vitamin D concentration has on the occurrence of depressive symptoms in pregnant mothers, postpartum mothers, women (non-pregnant/postpartum women), and men with a subgroup analysis of postpartum breastfeeding and non-breastfeeding mothers. We hypothesize that serum vitamin D concentration will be negatively correlated with depression risk in all subpopulations and higher vitamin D concentration will more strongly impact participants in the perinatal period. We also hypothesize that breastfeeding mothers will exhibit a lower amount of depression compared to other groups. Although previous studies have evaluated the relationship between vitamin D concentration and depressive symptoms, this study uses an extensive length of data (12 years; NHANES 2007-2018), comparing the four study groups of interest with each other, and incorporates a separate analysis of breastfeeding status in postpartum mothers, which together contribute unique information to better understand maternal and fetal health.
2. Materials and Methods
2.1. Study Populations
The National Health and Nutrition Examination Survey (NHANES) is a U.S. nationally representative series of cross-sectional, continuous surveys that combines interview questionnaires with physical exams and laboratory data collection. Open access data to the public is published every two years by the National Center for Health Statistics in conjunction with the Centers for Disease Control and Prevention. The NHANES participants are randomly selected for recruitment through analyses of U.S. Census information and provide informed consent prior to participation in the study. Approval of the survey cycles are permitted by the National Center for Health Statistics Research Ethics Review Board. The NHANES 2007-2018 survey cycles were chosen for this project because serum vitamin D concentrations were measured using the same method throughout the 12-year period.
This study sought to evaluate how pregnant mothers, postpartum mothers, women (refers to women who are neither pregnant nor within 12 months postpartum), and men compare to each other with a separate, subset analysis of postpartum breastfeeding and non-breastfeeding mothers. Pregnancy status was determined through the NHANES demographic pregnancy status variable which included urine pregnancy test results and/or self-reported status. Pregnancy status information is available for participants aged 20-44 years old; for equal comparative purposes, the study strictly analyzed participants within this age range for all study populations and participants outside 20-44 years old were removed from this study. The research team defined postpartum mothers as having delivered 0-12 months before the time of the interview, presented by the ‘months since last delivery’ question in the reproductive health section. Men were separated from the other study populations through the gender/sex assessment (male or female) in the demographics section. The breastfeeding and non-breastfeeding mothers were evaluated separately as a subset of the postpartum group. The question assessing current breastfeeding activity was provided in the reproductive health section.
2.2. Patient Health Questionnaire
Trained interviewers administered a nine-item depression screening instrument (Patient Health Questionnaire, PHQ-9) to assess self-reported depression symptoms over the previous two weeks, one symptom per question. Participants with missing PHQ-9 data were dropped from this study. The interviewers utilized the Computer-Assisted Personal Interview system throughout this portion of the Mobile Examination Center Interview. The questionnaire incorporates the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders by scoring each of the symptom criteria [
46]. Each question presented a symptom frequency scale ranging from 0 to 3 corresponded with the responses 0 = “not at all”, 1 = “several days”, 2 = “more than half the days”, and 3 = “nearly every day”. These scores were summed across all 9 questions, resulting in a final PHQ-9 depression score that could range from 0-27. The PHQ-9 scores represent the level of depression severity: minimal 0-4; mild 5-9; moderate 10-14; moderately severe 15-19; and severe 20-27 (46). The moderate (10-14), moderately severe (15-19), and severe (20-27) categories were combined into one category to balance sample size across the depression groups, creating three final categories in the analysis: no depression (0-4), mild depression (5-9), moderate to severe depression (10-27).
2.3. Serum Vitamin D Concentrations
Serum samples in NHANES 2007-2018 were evaluated by liquid chromatography-tandem mass spectrometry to quantify total serum vitamin D (25OHD2+25OHD3) with no changes in laboratory method, lab equipment, or lab site across each of the survey cycles. Participants with missing serum vitamin D concentration data were removed from this study.
2.4. Nutrient Intake within the Past 24 Hours
The What We Eat in America questionnaire was used in NHANES 2007-2018 for estimating dietary intake [
47]. Total nutrient intake within the past 24 hours of energy (kcal), protein (gm), carbohydrate (gm), total sugars (gm), total fat (gm), total saturated fatty acids (gm), and total monounsaturated fatty acids (gm), were estimated from the first day of foods, beverages, and water (tap and bottled water) consumed from midnight to midnight preceding the medical examination center interview. Information regarding dietary supplements, antacids, and medications are not included in the total dietary nutrient intake variables. Participants with missing data for nutrient intake described were dropped from this study.
2.5. Food Security
NHANES 2007-2018 provides an adult food security question that places adults within the household into four categories: full; marginal; low; and very low food security. These values were formulated by NHANES from the evaluation of ten questions in the food security questionnaire. The research team dichotomized the values to either secure (full food security) or insecure (marginal, low, and very low food security) to avoid extreme imbalance in sample sizes between categories.
2.6. Demographics
Additional demographic factors of interest include age, the 6-month time period when the examination was performed, race, marital status, and education. The ‘6-month time period when the examination was performed’ divided the year into: November 1 through April 30 (we labeled as winter) and May 1 through October 31 (we labeled as summer). The NHANES race variable divided participants into 5 categories: Mexican American, other Hispanic, Non-Hispanic White, Non-Hispanic Black, and other races including multiracial. The research team re-coded the variables to combine Mexican Americans and other Hispanic. This was done to simplify the categorical options. The inclusion of a non-Hispanic Asian category was not a part of the race variable available spanning the twelve years of collected data. The NHANES marital status included 6 categories: married, widowed, divorced, separated, never married, and living with a partner. The research team re-coded the values to combine married participants and those living with a partner. Widowed, divorced, and separated participants were also combined. This was done to simplify the categories and produce a more even distribution of sample sizes within each category. Education level in adults 20 years and older evaluated the highest grade level of school completed or the highest degree received. This variable was split into five categories within NHANES dataset: Less Than 9th Grade, 9-11th Grade (Includes 12th grade with no diploma), High School Grad/GED or Equivalent, Some College or AA Degree, and College Graduate or Above. The research team re-coded this variable to combine participants with less than 9th-grade education and those with 9-11th grade education for simplification of data and a more even distribution of the sample sizes across the categories. Trained health technicians along with a recorder gathered body measurement data which are presented in the body measures section. This study used information regarding body mass index (kg/m2) across each of the study populations.
2.7. Statistical Analyses
All survey observations were weighted to account for population strata and minimize bias. Following NHANES guidelines, the dietary intake survey weights were used for analysis. Since this study used 6 NHANES survey cycles, the NHANES weights were divided by 6, following the recommendations of the NHANES survey instructions. Participants with missing data across the PHQ-9, serum vitamin D concentration, and diet variables of caloric intake, total fats, total saturated fatty acids, total monounsaturated fatty acids, total sugars, total protein and total carbohydrates were dropped from the analysis. Additionally, survey respondents outside the target age range of 20-44 years old were removed from the data set prior to analyses.
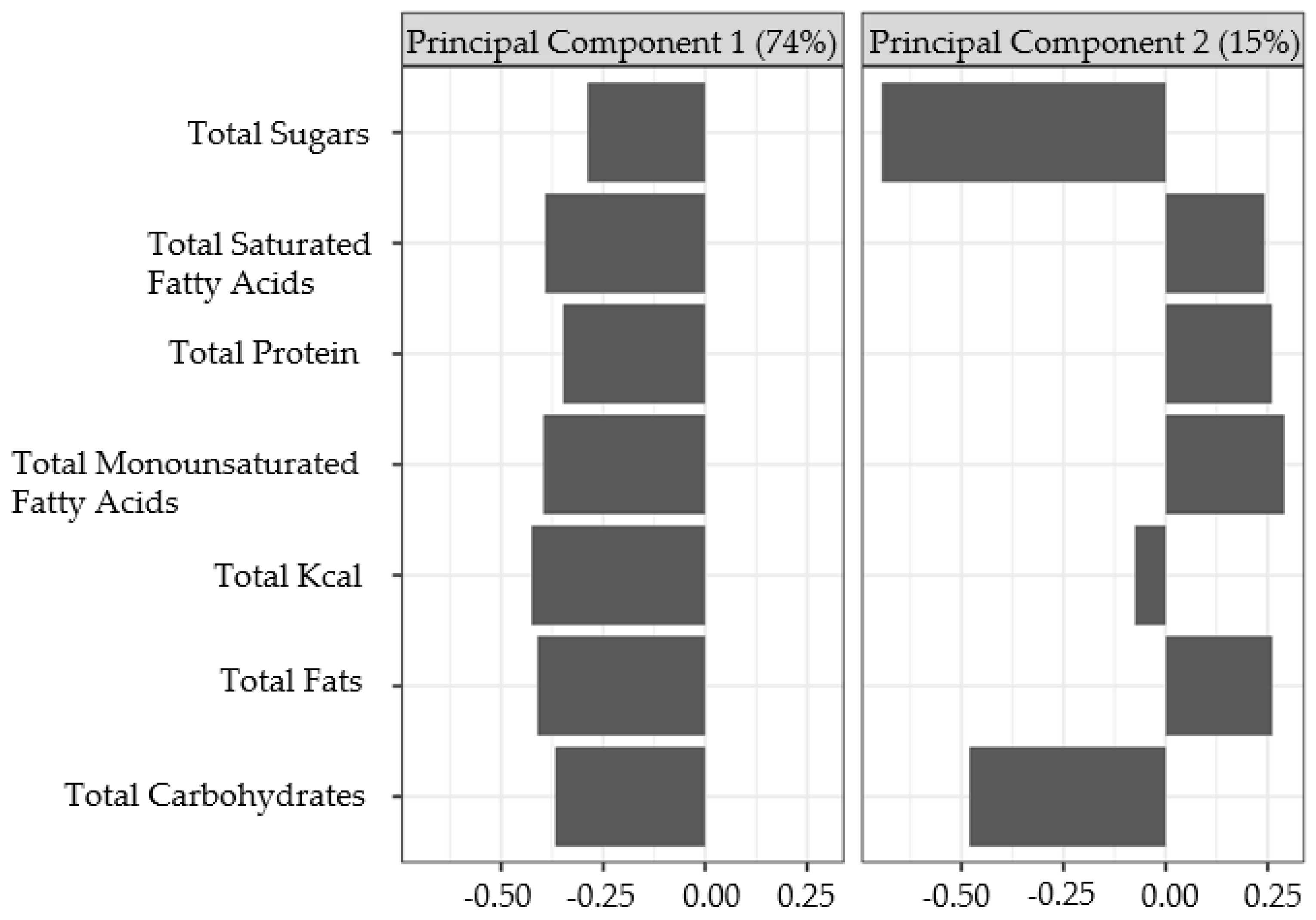
The ‘dagitty’ [
48] package was used to construct a directed acyclic graph (
Figure 1) and identity adjustment sets for estimating the impact of vitamin D on depression severity. Latent variables for diet, “Diet pattern 1” and “Diet pattern 2”, were created by conducting a principal component analysis using total caloric intake, total fats, total saturated fatty acids, total monounsaturated fatty acids, total sugars, total protein and total carbohydrates. These variables were highly correlated with one another, with the majority of pairwise correlation coefficients being above 0.5, except for correlations between sugars with fat and protein variables. The variables were scaled and standardized to have a mean of zero and a standard deviation of one for principal component analysis. The first two components were extracted and used as control variables representing diet. The R package ‘survey’ [
49,
50] was used for estimating population weighted means cross tabulations and conducting chi-square contingency tests.
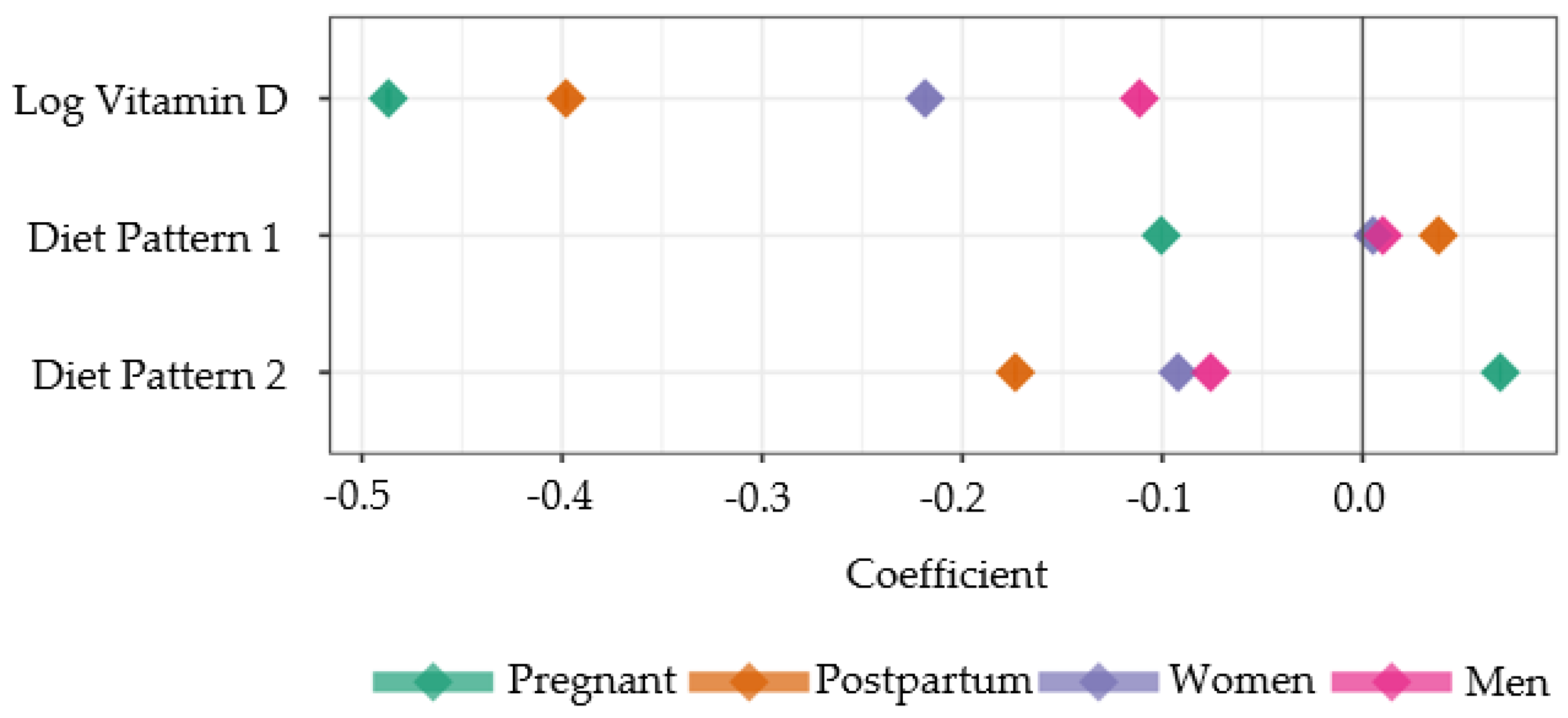
A Bayesian multinomial model was fit to predict depression outcomes for each cohort separately. These outcomes were estimated using cumulative probit and logit models as a function of the natural log of vitamin D and the two latent variables for diet, Diet pattern 1 and Diet pattern 2. The observations were weighted by their NHANES weights, and the model was fit using the R package ‘brms’ [
51,
52,
53] for 4 chains of 2000 iterations each, with 1000 iterations reserved for warmup. Vitamin D was transformed with the natural log to introduce more symmetry into that variable and reduce the influence of extremely large values. The postpartum subpopulation analysis followed a similar form with the following exceptions: (1) separate slopes were estimated for the breastfeeding and non-breastfeeding groups; and (2) unequal variance of the breastfeeding groups was assumed and incorporated into the model.
Model fit for all populations and subpopulations analyses were evaluated by comparing the WAIC and leave-one-out statistics for the logit and probit models. Convergence and model quality was evaluated for each model by inspecting the trace plots of the chains and the values for R-hat and effective sample size for each parameter. Post Hoc hypothesis tests were conducted to evaluate if the Vitamin D slope parameters were less than zero, indicating that as vitamin D concentration increased, the probability of depression decreased. The statistical software R v4.2 or higher was used for all analysis [
54].
4. Discussion
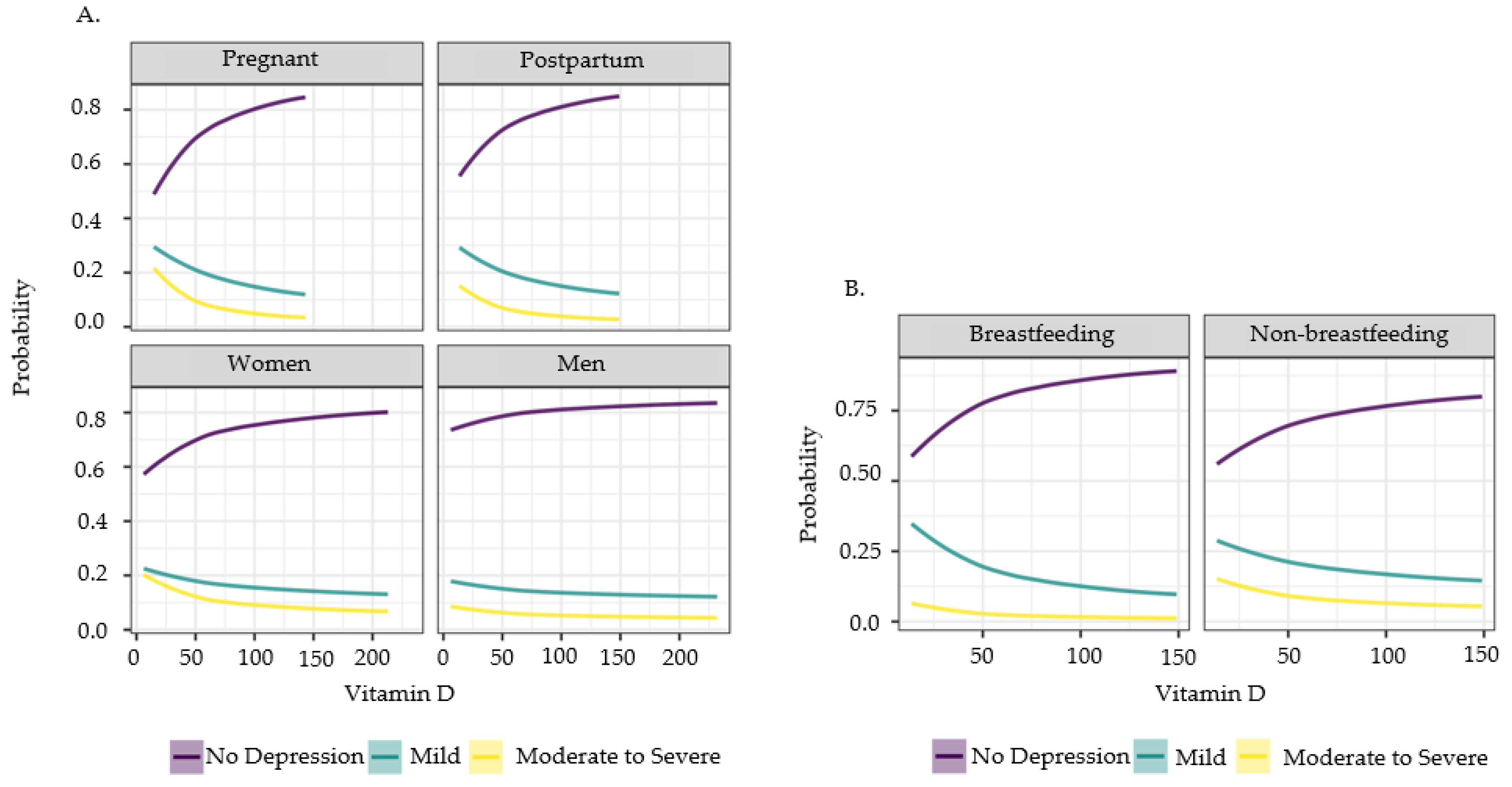
From the 12 years of cross-sectional data collected by NHANES, we confirmed similar findings from previous publications as well as gathered new information to advance maternal and fetal health. Consistent with previous studies [
9,
10,
11,
12,
15], vitamin D concentration had a significant negative correlation to depressive symptoms in pregnant, postpartum, women, and men populations; a higher vitamin D concentration indicates an increased probability of no depression, while a lower vitamin D concentration predicts a higher chance of depression within the severity scale. However, the influence of vitamin D concentration on depression revealed a range of strength within the subpopulations. Specifically, the Bayesian analysis illustrated that vitamin D concentration more profoundly impacts pregnant mothers than the other subpopulations. After pregnant mothers, postpartum mothers had the next greatest impact from vitamin D concentration, then women, and finally men. Although vitamin D concentration impacts men’s depressive symptoms, it is not as influential compared to any of the women subpopulations.
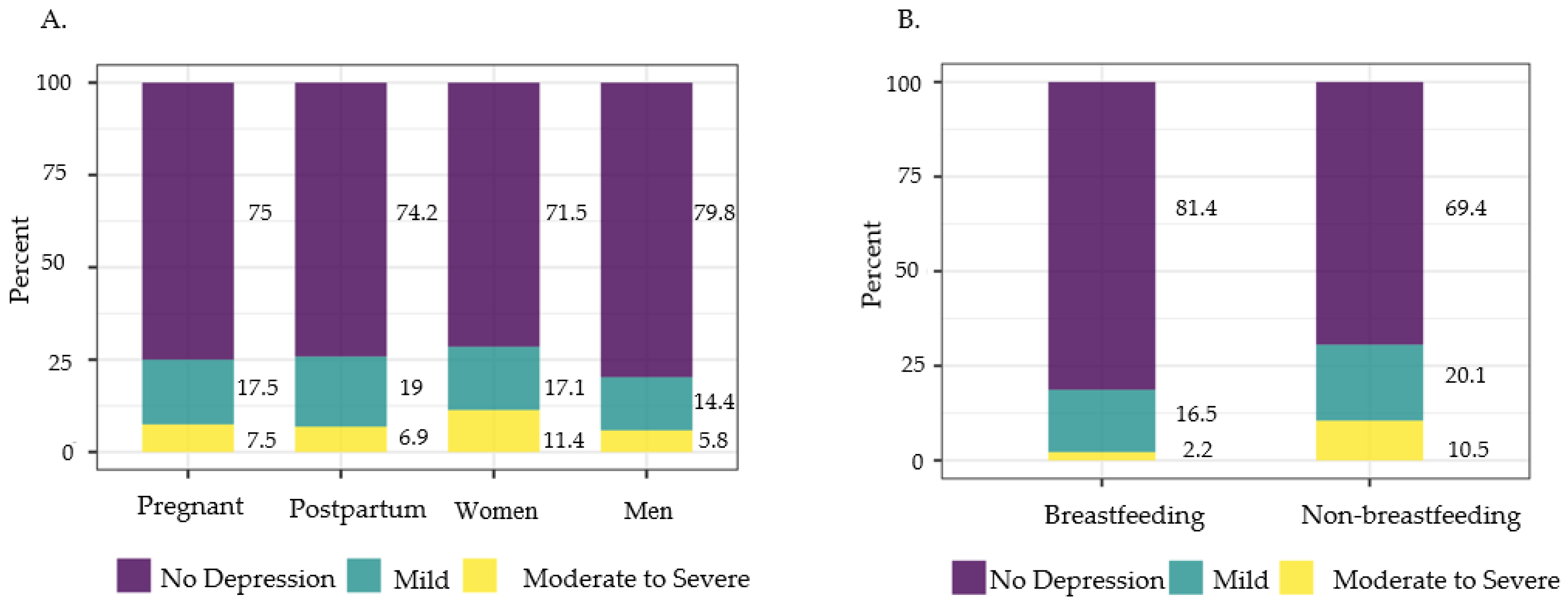
Perinatal depression alters health outcome risks in infants [
3,
4,
5,
6,
7] and vitamin D concentration was shown to be an influential factor on depression in pregnant and postpartum mothers. This suggests adequate vitamin D concentration throughout pregnancy and after delivery may be particularly crucial to the health of the mothers and infants. Our study also analyzed how depression risk among breastfeeding and non-breastfeeding postpartum mothers are impacted by vitamin D concentration. A novelty found in this study through the Bayesian model was that the beneficial effects of vitamin D on depression are more enhanced in breastfeeding mothers than non-breastfeeding mothers. Specifically, breastfeeding mothers showed the lowest percentages of moderate to severe depression and highest percentage of participants with no depression compared to all other groups, suggesting that postpartum breastfeeding mothers are more impacted by the benefits of vitamin D on depressive symptoms compared to non-breastfeeding mothers. The NHANES reproductive health questionnaire doesn’t specify whether the breastfeeding mothers are exclusively breastfeeding or mix feeding with formula, but since this group shows the lowest weighted percentage of no depression, at least some breastfeeding activity appears to enhance the benefits of higher vitamin D concentration. This, again, points to the importance of maintaining adequate vitamin D concentration while the mothers’ bodies are an active source of nutrition for infants, during pregnancy and while breastfeeding.
To account for confounding factors, diet was another variable that advanced to the final analysis of this study because it affects vitamin D concentration and depression [
14,
23,
24,
25]. Diet pattern 1, having higher summative calories and intake of all macronutrients, indicated a positive relationship with depression in postpartum mothers. Interestingly, pregnant mothers had decreased depressive symptoms risk with this diet pattern. Diet pattern 1 closely simulates the typical Western diet, showing the adverse health effects of excess food intake. Pregnant mothers were the only group that exhibited lower depression with Diet pattern 1 likely due to their increased dietary needs during pregnancy. Diet pattern 2, which encompassed a lower caloric, sugar and carbohydrate intake and/or increased protein and fat intake, showed a decreased risk of depression in postpartum mothers, women, and men. Pregnant mothers again echoed another divergence, where following the Diet pattern 2 predicted increased risk of depression. Diet pattern 2 has similarities to the paleo diet and our results show decreased depression risk with this diet for all the study populations, except pregnant mothers. Our study demonstrates how pregnant mothers need different diet plans than postpartum mothers, women, and men, to better support their mental health and potential impacts on fetal health. During pregnancy, based on the increased overall caloric and macronutrient needs to support tissue deposition and optimize placental-fetal nutrient transfer, Diet pattern 1 ensures adequate nutritional provision. Indeed, pregnancy induces insulin resistance to maximize glucose transport to the fetus, thus a diet with higher total calories and overall macronutrients would be conducive in supporting optimal placental-fetal glucose transfer. However, the threshold between the two diet patterns, to avoid over-abundance of intake inducing obesity risk, and risk for depression in pregnant mothers still needs to be investigated. For example, Parrettini et al reviewed several studies and illustrated how obesity and excessive weight gain presents higher risk of maternal/fetal health issues in the short and long term [
55]. Finding an appropriate nutritional balance for expecting mothers will require a multifactorial approach, assessing body composition, morbidities, and socioeconomic barriers to a healthy diet. It is interesting that postpartum women (including breastfeeding women) did not share the same relationship patterns with pregnant women in relation to diet patterns even though breastfeeding women also require additional caloric intake. However, our subpopulation of postpartum women included both breastfeeding and non-breastfeeding women, and the actual amount of breastfeeding was not clearly quantified in the NHANES data to better assess the impact of these Diet patterns on breastfeeding women.
Although our study includes an extensive length of NHANES data, the cross-sectional design does not allow for repeated measures of vitamin D concentrations nor depression scores in individual participants over time. We simply have a snapshot of how vitamin D concentrations are associated with depression risk in pregnant mothers, not how this relationship may change over the pregnancy course. Another survey limitation involves breastfeeding status reported in the reproductive health questionnaire. The question for the NHANES participants only inquires if the mother is currently breastfeeding, not specifying exclusive breastfeeding or actual amount of breastfeeding. As we know, exclusive breastfeeding during the first 6 months of life is recommended for all infants [
56] and future studies following mothers could benefit from quantifying exclusive breastfeeding and amount of breastfeeding to better understand human milk’s protective effects. Additionally, our sample sizes for participants with moderate to severe depression were limited and our pregnant/postpartum groups were much smaller than our women and men groups. A larger pool of pregnant and postpartum participants and participants experiencing depression would strengthen the results of subsequent studies.
Future research analyzing how human milk composition changes with varying vitamin D concentrations in mothers may provide important health knowledge for breastfed infants. Future studies should also investigate whether vitamin D concentrations are significantly different geographically throughout the United States; Vitamin D concentration is affected by endogenous synthesis through sun exposure, and populations across the US range in the amount of exposure throughout the year. Building on our new found knowledge from this study that pregnant and postpartum mothers display stronger influences from vitamin D concentration, this may inform interventional studies throughout the perinatal period in relation to maternal mental health.
Author Contributions
Conceptualization, V.R.B.B.H. and Y.C.; methodology, V.R.B.B.H., J.L.P., and Y.C.; formal analysis, V.R.B.B.H., and J.L.P.; investigation, V.R.B.B.H., J.L.P., and Y.C.; resources, V.R.B.B.H., J.L.P., and Y.C.; data curation, V.R.B.B.H., and J.L.P.; writing—original draft preparation, V.R.B.B.H.; writing—review and editing, V.R.B.B.H., J.L.P., and Y.C.; visualization, V.R.B.B.H., J.L.P., and Y.C.; supervision, Y.C.; funding acquisition, Y.C. All authors have read and agreed to the published version of the manuscript.
Figure 1.
Directed acyclic graph displaying hypothesized relationships between key variables obtained from NHANES 2007-2018 data. Blue boxes: the study’s main variables of focus; White boxes: other key variables that have influences on the main variables; Blue arrow: the study’s hypothesis of vitamin D concentration impacting depressive symptoms; bolded black arrows: variables that were shown in the literature review to influence more than one factor; faded gray arrows: variables that were shown in the literature review to influence one factor.
Figure 1.
Directed acyclic graph displaying hypothesized relationships between key variables obtained from NHANES 2007-2018 data. Blue boxes: the study’s main variables of focus; White boxes: other key variables that have influences on the main variables; Blue arrow: the study’s hypothesis of vitamin D concentration impacting depressive symptoms; bolded black arrows: variables that were shown in the literature review to influence more than one factor; faded gray arrows: variables that were shown in the literature review to influence one factor.
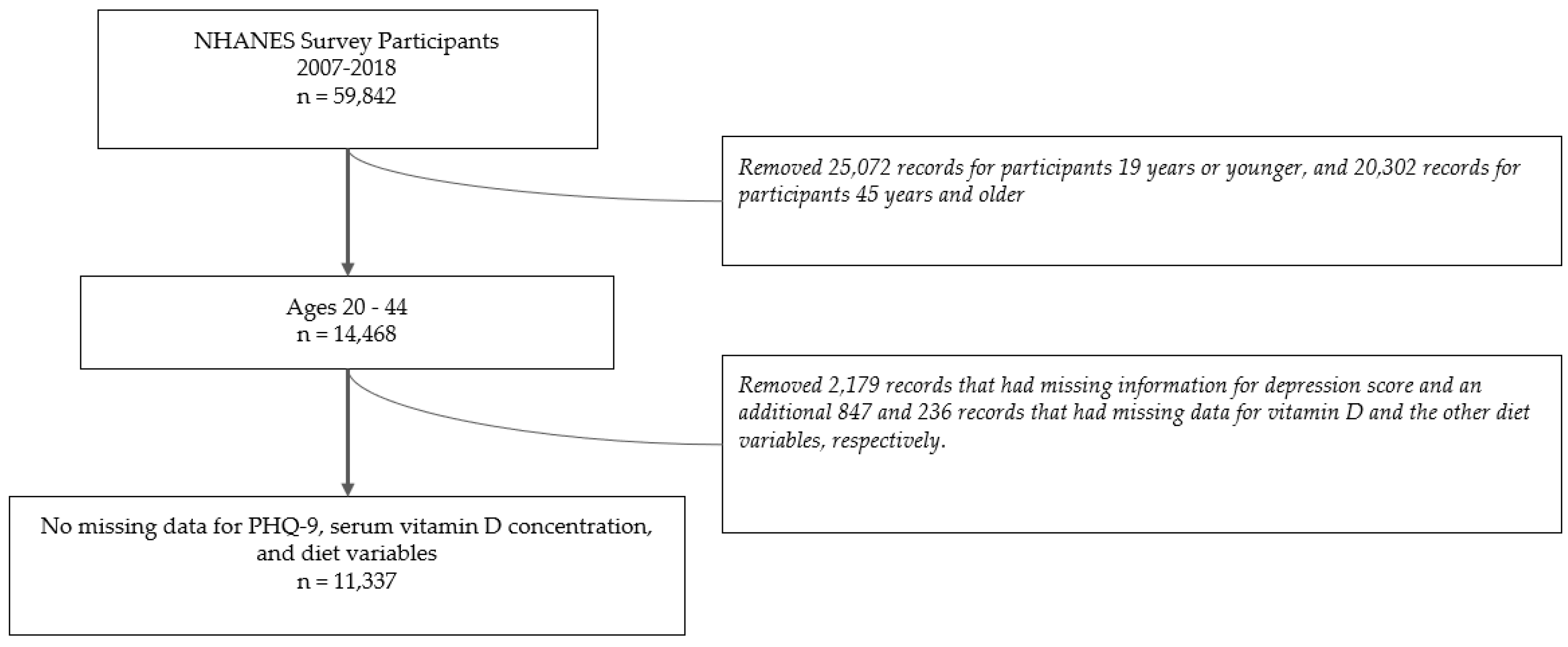
Figure 2.
Flow diagram illustrating how we arrived at our final study population after filtering for the desired age range and removing participants with missing data for the PHQ-9, serum vitamin D concentration, and diet variables of caloric intake, total fats, total saturated fatty acids, total monounsaturated fatty acids, total sugars, total protein and total carbohydrates.
Figure 2.
Flow diagram illustrating how we arrived at our final study population after filtering for the desired age range and removing participants with missing data for the PHQ-9, serum vitamin D concentration, and diet variables of caloric intake, total fats, total saturated fatty acids, total monounsaturated fatty acids, total sugars, total protein and total carbohydrates.
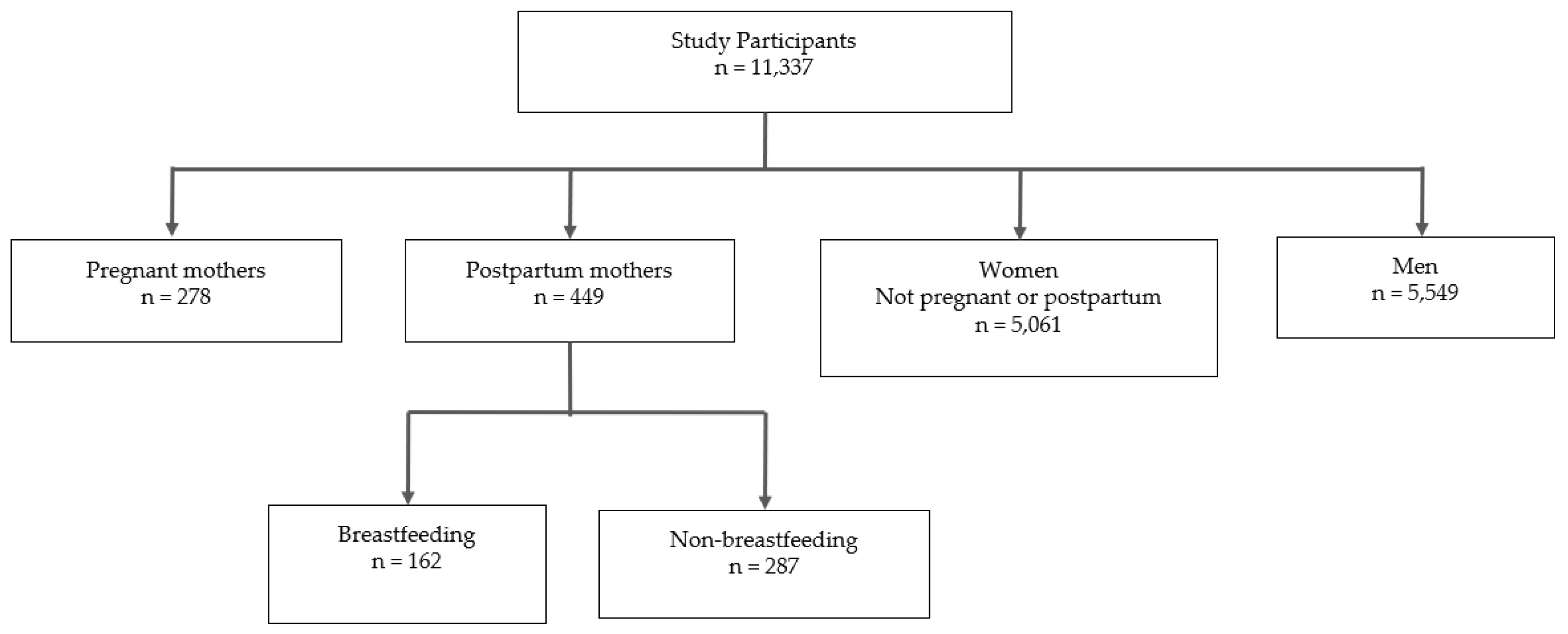
Figure 3.
Flow diagram visualizing the count breakdown of participants into subpopulations (pregnant mothers, postpartum mothers, women, and men) and the postpartum breastfeeding and non-breastfeeding subgroups.
Figure 3.
Flow diagram visualizing the count breakdown of participants into subpopulations (pregnant mothers, postpartum mothers, women, and men) and the postpartum breastfeeding and non-breastfeeding subgroups.
Figure 4.
Weighted percentage of participants with no depression, mild depression, and moderate to severe depression in A) pregnant mothers, postpartum mothers, women, and men; and B) breastfeeding and non-breastfeeding postpartum mothers aged 20-44 years old, NHANES 2007-2018.
Figure 4.
Weighted percentage of participants with no depression, mild depression, and moderate to severe depression in A) pregnant mothers, postpartum mothers, women, and men; and B) breastfeeding and non-breastfeeding postpartum mothers aged 20-44 years old, NHANES 2007-2018.
Figure 5.
Variable loadings for the diet-derived latent variables from principal component analysis. The percentages in parentheses are the percent variation summarized by each latent variable. The loadings from the first component, a latent variable labeled “Diet pattern 1”, negatively weighted all of the (standardized) Diet pattern 1 variables, where lower values for this latent variable indicated higher overall calorie consumption and elevated consumption of protein, fats, carbohydrates, sugars - similar to that of a typical Western Diet. The second principal component loadings (latent variable “Diet pattern 2”) had negative values for sugar and carbohydrates, positive values for all fats variables and protein, while the loading for total calories hovered close to zero. Higher values for Diet pattern 2 among the respondents for this latent variable indicate more fat and protein consumption and lower carbohydrate and sugar consumption.
Figure 5.
Variable loadings for the diet-derived latent variables from principal component analysis. The percentages in parentheses are the percent variation summarized by each latent variable. The loadings from the first component, a latent variable labeled “Diet pattern 1”, negatively weighted all of the (standardized) Diet pattern 1 variables, where lower values for this latent variable indicated higher overall calorie consumption and elevated consumption of protein, fats, carbohydrates, sugars - similar to that of a typical Western Diet. The second principal component loadings (latent variable “Diet pattern 2”) had negative values for sugar and carbohydrates, positive values for all fats variables and protein, while the loading for total calories hovered close to zero. Higher values for Diet pattern 2 among the respondents for this latent variable indicate more fat and protein consumption and lower carbohydrate and sugar consumption.
Figure 6.
Slope parameter estimates from cumulative categorical model for all cohorts, using the model threshold and observed data for diet patterns 1 and 2. The larger the negative value for a group, the more influence high vitamin D concentration had to decrease depression risk. Likewise, the larger the negative value for a group, the more influence following that diet pattern had to decrease depression risk. The 68% and 95% credible intervals are plotted, but cannot be observed because they are less wide than the plotting symbol for each point.
Figure 6.
Slope parameter estimates from cumulative categorical model for all cohorts, using the model threshold and observed data for diet patterns 1 and 2. The larger the negative value for a group, the more influence high vitamin D concentration had to decrease depression risk. Likewise, the larger the negative value for a group, the more influence following that diet pattern had to decrease depression risk. The 68% and 95% credible intervals are plotted, but cannot be observed because they are less wide than the plotting symbol for each point.
Figure 7.
Prediction curve along Vitamin D from item response model in A) Pregnant mothers, postpartum mothers, women, and men; and B) Breastfeeding and non-breastfeeding postpartum mothers aged 20-44 years old, NHANES 2007-2018. Predictions are from the observed data for each cohort, taking into account the diet latent variables and population threshold for the depression categories. The 0.999 prediction interval is plotted, but it is narrower than the plotted line and hence not visible.
Figure 7.
Prediction curve along Vitamin D from item response model in A) Pregnant mothers, postpartum mothers, women, and men; and B) Breastfeeding and non-breastfeeding postpartum mothers aged 20-44 years old, NHANES 2007-2018. Predictions are from the observed data for each cohort, taking into account the diet latent variables and population threshold for the depression categories. The 0.999 prediction interval is plotted, but it is narrower than the plotted line and hence not visible.
Table 1.
Weighted percentages and distributions (mean ± standard deviation) of characteristics among all participants, pregnant, postpartum, women, and men aged 20-44 years old, NHANES 2007-2018.
Table 1.
Weighted percentages and distributions (mean ± standard deviation) of characteristics among all participants, pregnant, postpartum, women, and men aged 20-44 years old, NHANES 2007-2018.
| Variable Description |
All Participants |
Pregnant |
Postpartum |
Women1
|
Men |
| Race |
|
|
|
|
|
| Non-Hispanic White |
58.7 |
51.2 |
55.1 |
59.3 |
58.8 |
| Hispanic |
19.5 |
21.2 |
23.9 |
18.3 |
20.1 |
| Non-Hispanic Black |
12.6 |
15.2 |
13.6 |
13.5 |
11.7 |
| Other Race - Including Multi-Racial |
9.2 |
12.3 |
7.4 |
9 |
9.4 |
| Marital Status |
|
|
|
|
|
| Married/Living with Partner |
56.7 |
78.1 |
75.2 |
56.2 |
54.7 |
| Widowed, Divorced, or Separated |
8.5 |
5 |
6.5 |
11.3 |
6.4 |
| Never Married |
34.8 |
16.9 |
18.3 |
32.5 |
38.9 |
| Education |
|
|
|
|
|
| No High School Diploma |
14.1 |
17.4 |
17.1 |
12.7 |
15 |
| High School Grad/GED or Equivalent |
22.3 |
18.9 |
25.3 |
18.8 |
25.2 |
| Some College or AA degree |
34.4 |
32.7 |
31.9 |
36.9 |
32.6 |
| College Graduate or Above |
29.1 |
31 |
25.6 |
31.5 |
27.3 |
| Adult Food Security Category |
|
|
|
|
|
| Secure |
68.7 |
67.7 |
62.2 |
67.5 |
70.3 |
| Insecure (Marginal to Very Low) |
31.3 |
32.3 |
37.8 |
32.5 |
29.7 |
| Data Collection Season |
|
|
|
|
|
| Summer |
55.8 |
59.8 |
52.9 |
56.3 |
55.5 |
| Winter |
44.2 |
40.2 |
47.1 |
43.7 |
44.5 |
| Age |
31.7 ± 7.2 |
29.1 ± 5.9 |
28.4 ± 5.8 |
32.2 ± 7.4 |
31.5 ± 7.2 |
| BMI |
28.7 ± 7.5 |
29.9 ± 7.1 |
29.7 ± 7.5 |
28.9 ± 8.3 |
28.5 ± 6.6 |
| Income: Poverty Ratio |
2.7 ± 1.6 |
2.8 ± 1.6 |
2.1 ± 1.4 |
2.7 ± 1.6 |
2.8 ± 1.6 |
Table 2.
Counts of depression level in pregnant, postpartum, women, and men aged 20-44 years old, NHANES 2007-2018.
Table 2.
Counts of depression level in pregnant, postpartum, women, and men aged 20-44 years old, NHANES 2007-2018.
| Depression level |
Pregnant |
Postpartum |
Women1
|
Men |
Total |
| None |
194 |
336 |
3570 |
4409 |
8509 |
| Mild |
60 |
83 |
897 |
790 |
1830 |
| Moderate to severe |
24 |
30 |
594 |
350 |
998 |
| Total |
278 |
449 |
5061 |
5549 |
11337 |
Table 3.
Counts of depression level in breastfeeding and non-breastfeeding mothers aged 20-44 years old, NHANES 2007-2018.
Table 3.
Counts of depression level in breastfeeding and non-breastfeeding mothers aged 20-44 years old, NHANES 2007-2018.
| Depression level |
Breastfeeding |
Non-Breastfeeding |
Total |
| None |
127 |
209 |
336 |
| Mild |
29 |
54 |
83 |
| Moderate to severe |
6 |
24 |
30 |
| Total |
162 |
287 |
449 |