1. Introduction
Healthcare systems can be classified into two main categories: 1) conventional medicine (also referred to as modern, Western, mainstream, or allopathic), and 2) traditional medicine (encompassing indigenous medicine and Complementary and Alternative Medicine)[
1]. Conventional medicine can be understood as a system that relies on a Western medical concept that prevents, treats and rehabilitates symptoms and diseases through evidence-based practices, including drugs, radiation or surgical procedures [
2]. Complementary and Alternative Medicine (CAM) has been defined by the World Health Organization (WHO) [
3], as a broad set of healthcare practices that are not part of the conventional health system practices and are not fully integrated into the dominant healthcare system [
3].
However, controversies exist regarding the terminologies given the lack of homogeneous international health policies and the differences amongst national healthcare systems and cultural perceptions particularly applicable to non-Western countries. For instance, the national health system in China has two variables equally accepted and supported by governmental policies and regulations: Western medicine and Traditional Chinese medicine [
4,
5,
6,
7]. As Traditional Chinese medicine is a key element of the national health system, practices encompassed within Traditional Chinese medicine (such as acupuncture, Tai Chi, and herbs) are not perceived as CAM practices but as mainstream practices [
6,
7]. Thus, for the purposes of this review, the main difference between conventional and unconventional medicine is whether the practice is formally integrated into the dominant healthcare system of a nation (conventional) or not (unconventional).
Definitions have had a dynamic pattern fluctuating throughout the years; between 1990 and 2013, the terms "complementary" and "alternative" were prevalent in the literature as separate terminologies [
8]. In addition to the aforementioned terms, the concept of "integrative medicine" has a notable role within this topic. It is considered integrative medicine when both conventional and unconventional medicine are combined [
8]. The term CAM, which includes both complementary and alternative medicine, has gained more acceptance since 2000, and it is now the most widely recognised term [
8]. CAM consists of a set of medical practices, products, or systems, but approaches to these unconventional practices differ and are still largely unregulated globally [
9].
CAM practices have been present in the healthcare systems worldwide since ancient times [
10]. It has become a global tendency to use CAM, with prevalence rates ranging from 8% to 76% in the general population [
11]. Regarding the paediatric population, in 2013, an estimated 52% of European children used CAM therapies [
12], and available data indicates an increase in the popularity of CAM methods worldwide [
13]. Likewise, the WHO estimates that parents' prevalence of using CAM therapies for their children varies geographically, ranging from 10% to as high as 80% [
14].
Several studies have published favourable results regarding the use of CAM; however, non-rigorous and unclear methodologies have been identified. Such inconsistent results contrast other scientific evidence following rigorous methodologies [
15].
The heterogeneity in existing trials, together with inconclusive results about CAM effectivity and safety, has led health providers and scientists to adopt different positions to recommend CAM or not, creating, at the same time, confusion amongst CAM users in the general population[
15]. This heterogeneity within healthcare providers hinders the formality of reporting adverse events. Despite the many-sidedness, the number of case reports of adverse events is growing and varies from mild and self-limited effects to fatal outcomes leading to death[
16]. Hence, concerns regarding patients' well-being have arisen within the scientific community, and CAM interventions' effectiveness and safety have been highly questioned. This lack of consensus regarding the use of CAM affects primarily vulnerable populations, such as the elderly and children, given that their health is mostly dependent on their caregivers and guardians, who rely on different socio-cultural and geographical contexts. Thus, high-quality research examining the effectiveness and safety of CAM therapies is crucially needed.
This review aims to provide an overview of CAM around the globe as well as to explore the applications, mechanisms of action, and adverse effects of CAM therapies in the paediatric population. The study employed Google Scholar, PubMed, and The Cochrane Library for academic searches, using keywords and topical research. Initially, broad terms like "complementary and alternative medicine in children" were used, but later, they were refined to specific topics. Eligible articles included systematic reviews, meta-analyses, randomised controlled trials (RCT), observational studies, literature reviews, case reports, and discussion articles. Only English language studies published between 2010 and 2024 were considered, with exceptions made for relevant older studies or when recent data was lacking. Preclinical studies were included to explore mechanisms of action, and there were no geographical limitations to ensure a global perspective on CAM and children. When a lack of paediatric evidence was identified, considerations were given to studies performed in animal and adult populations, as there are often common underlying mechanisms and therapeutic strategies.
2. National Healthcare Systems and CAM
The architecture of a typical healthcare system is contingent upon distinct factors, each intrinsic to the particular country in question. These factors encompass the climate and natural environment, geography, population density and demographics, history, socio-cultural ideologies, political, and economic status[
17]. These elements collectively delineate a unique framework and national context that significantly shapes healthcare systems' governance and financial structuring. National authorities subsequently formulate criteria and strategic frameworks for resource allocation, with the primary goal of facilitating the provision of healthcare services, including health promotion initiatives, disease prevention measures, curative interventions, rehabilitation programs, and palliative care [
17]. The dissemination of these services to the population at large is facilitated through the deployment of healthcare personnel, the availability of medical products, adherence to established service standards, and the dissemination of pertinent health-related information [
17].
CAM occupies a significant role within the socio-cultural ideologies that mould and influence national healthcare systems across various levels. Epidemiological data reveal a notable global surge in CAM utilisation [
18,
19]. Notably, in Europe, research indicates that approximately 29% of the population used CAM therapies in 2014[
20]. Similarly, in the United States of America (USA), CAM usage escalated by 17.5% between 2002 (19.2%) and 2022 (36.7%) [
21].
This trend may have influenced government resource allocation, prompting augmented funding for CAM research; illustrating this financial impact, in the USA, the National Institutes of Health (NIH) report highlights a substantial increase in budgetary provisions for the National Center for Complementary and Integrative Health (NCCIH), whose NIH congressional appropriation increased approximately 40% since the last decade (
$121, 373 dollars in thousands in 2013 vs. 170,384 in 2023) [
22]. However, in 2019, the NCCIH total reported budget was
$517,246 dollars in thousands, which represents an increase of 253% of the congressional appropriation reported in the same year (
$146,473 dollars in thousands)[
23].
In some other countries, the increased prevalence of CAM not only may have impacts on the financial resources of a healthcare system, but it also has elicited changes in particular settings such as cancer: in Malaysia, where the prevalence of CAM users was approximately 46.5%, a multi-centre cross-sectional study reported that in patients with breast cancer, the use of CAM was associated with delays in presentation (OR 1.65; 95% CI: 1.05-2.59), diagnosis (OR 2.42; 95% CI: 1.56-3.77) and treatment of breast cancer (OR 1.74; 95% CI: 1.11- 2.72) [
24]. Similar results have been reported in the paediatric population; according to an Indonesian study in a cohort of oncologic paediatric patients, authors reported an association between CAM users and a delay in the diagnosis of solid tumours (OR = 1.86, 95% CI: 1.13–3.08, p = .015) with a median delay of 14 days [
25].
Regardless of the objectivity of these data, it is worth considering Western medicine's heterogeneous national health coverage, particularly in remote areas where CAM are the most available or affordable healthcare. The integration of well-established policies and strategies for CAM regulation into crucial infrastructure components of national healthcare systems may contribute to advancing the particular health system in terms of quality, safety, and efficacy.
Despite an increase in CAM usage in the paediatric population [
26,
27], little has been investigated concerning its global impact, which opens avenues for further exploration of this healthcare concern.
3. Paediatric Population and CAM
The prevalence of CAM therapies in paediatric populations varies widely according to cultural and geographical contexts. Still, it is estimated that over the world, overall rates of CAM use in children range from 10.9% to 87.6% depending on the country and socio-cultural factors of the parents [
28].
Lately, it has become a widespread practice for parents to use CAM therapies for their children rather than conventional medicine [
29]. In previous years, in the USA, the number of children taken to be consulted by CAM providers was higher than the number of children taken to conventional practitioners [
30]. In the past, American parents' estimated amount of money spent on CAM therapies for their children annually in the whole country was more significant than the money spent on hospitalisations (
$13.7 billion, compared to
$12.8 billion, respectively) [
30].
Currently, studies have shown that vulnerable children, such as those with chronic, recurrent or incurable conditions that are difficult to manage or children taking prescription medication [
31], are more likely to seek CAM alternatives than others [
32,
33,
34]. Rates of children with such conditions are estimated to be greater than 50% of the total of children using CAM, with oncology patients leading the list with 63% [
35,
36]. Other common conditions that were found to be linked to higher use of CAM are asthma and mental health conditions such as autism spectrum disorder, attention deficit hyperactivity disorder (ADHD), depression, and anxiety [
32,
37]. Furthermore, parents predominately choose CAM to treat specific symptoms of their children such as headaches, neck or back pain, colic, and respiratory symptoms like chest cold [
13,
37], running nose, cough, and sore throat [
38].
Despite the large number of studies supporting the strong link between CAM usage and chronic illnesses, some studies have not found a correlation in the therapeutic approach. Instead, they suggest that CAM is used for children to increase physical fitness [
39], prevent or maintain good health, and deal with symptoms such as vomiting or abdominal pain[
31]. Unlike four- to eleven-year-olds, for whom the main reason for using CAM is to treat vomiting or abdominal pain, adolescents aged 11 to 17 are more likely to use CAM to control their weight and improve their personal image or body shape [
13,
39,
40].
4. Factors Influencing CAM Usage in the Paediatric Population
The factors that lead caregivers or legal guardians to use CAM can be classified into the following categories: socio-cultural, economic, and educational [
28,
41,
42].
4.1. Socio-Cultural Factors
The use of complementary therapies strongly relies on the socio-cultural and ethnic contexts. In European countries, where the official national healthcare system is mainly based on a Western medical approach, CAM use rates among children range from 25% to 50% [
43]; in contrast, Traditional Chinese Medicine (TCM) is a pillar of the national healthcare system, and the prevalence of parents using CAM for their children is by far the highest in the world, reaching approximate 76%, with rates as high as 96% in paediatric oncologic patients [
44,
45].
Furthermore, some caregivers decide to use CAM in their dependents simply because it is an inherited tradition [
46], whereas some other caregivers rely on the conviction that CAM methods or therapies are natural or use natural components; hence, they are innocuous and safe [
46]. It has also been reported that children whose parents/caregivers are CAM users are more likely to use CAM in their descendants/dependents as well [
31,
47,
48]. Some parents choose CAM therapies to be considered "good parents" [
46], which eases their sense of agency over their offspring. For other parents, choosing CAM for their children is related to superstition and beliefs [
49].
Parents/caregivers commonly decide to use CAM in cases where children face chronic, incurable, or terminal pathologies. Therefore, guardians feel helpless, and the active and personal seeking of an alternative to improve the condition becomes imperative [
50]. Moreover, it has been observed that parents decide to use CAM when they lack an accurate diagnosis of their child's condition. Consequently, parents' decision to give their child CAM is often taken out of despair to find a solution to their child's problem, based on a felt failure and concerns related to the side effects of conventional medical treatments [
46].
As previously explained, cultural factors highly influence the selection and transmission of CAM therapies; this inherited "CAM culture" promotes seeking and using these therapies in each generation, consequently impacting the national health systems.
4.2. Economical and Educational Factors
It is generally accepted that broad access to CAM and affordability for the general population account for some of the primary causes of CAM use [
11]. Nevertheless, controversies exist regarding the association of CAM, education, and income. On the one hand, some academics support the idea that easy access to CAM and the low costs of such interventions are associated with higher rates of CAM use [
46,
49]. On the other hand, existing literature suggests that people with a higher educational level, who tend to have higher incomes, are more likely to afford to become CAM users [
49]. Still, some evidence shows that a higher educational level outweighs wealth in the decision to use CAM; however, the available literature supporting any of the aforementioned perspectives is insufficient to favour one over another.
Despite the lack of consensus regarding the role of educational and income level influencing the incidence and prevalence of CAM use, there is a growing body of objective evidence suggesting that these two factors are strong determinants in selecting the type or modality of CAM. For example, acupuncture and relaxation were associated with higher educational levels, whereas chiropractic was associated with lower educational levels [
51]. Then, chronic illnesses and children's poor health prognosis, along with household income, educational level, and socio-geographical factors, all together account for the major premises that encourage parents/caregivers to use CAM therapies for themselves and their dependents.
In an attempt to wrap up a Western prototype of a typical CAM child patient, some literature reflecting data from the USA and Germany states that the classical paediatric patient under CAM interventions would be a non-Hispanic white adolescent living in a house with high income and whose parents have a higher educational level [
32,
34]. These findings were also confirmed by The National Health Statistics Report in the USA (2015), where the paediatric population with the lowest prevalence of CAM usage were Hispanic and African American children[
13].
Whatever the reasons or motivations that lead parents or adolescents to seek CAM, the high rates of their popularity urge us to examine whether these interventions are indeed effective and safe.
5. CAM Classification
Therapies included in the definition of CAM are deliberately broad since practices considered complementary or traditional in one country or a particular culture might be regarded as part of conventional medicine in a different one [
51]. Thus, several classifications of the therapies considered as CAM have been proposed by different scholars. The NCCIH proposes three categories based on their therapeutic input: physical (e.g. massage, acupuncture), nutritional (e.g. probiotics, herbal therapy), and psychological (e.g. hypnosis, spiritual healing/prayer) [
52].
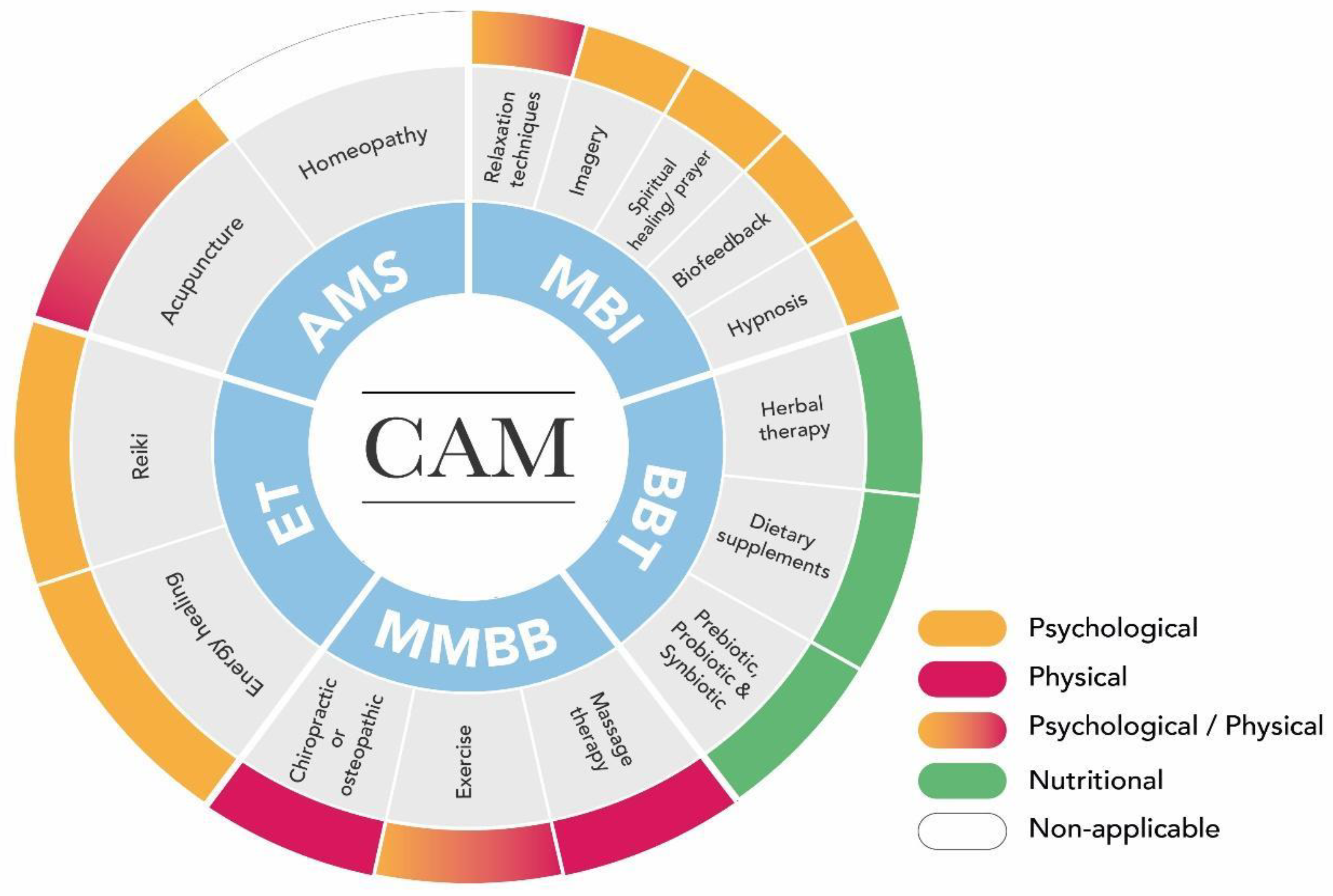
However, Mollaoğlu and Aciyurt [
53] suggested the following classification: 1) Alternative and medical system (AMS): acupuncture and homoeopathy. 2) Mindbody interventions (MBI): relaxation techniques, imagery, spiritual healing/prayer, biofeedback, hypnosis. 3) Biologically based therapies (BBT): Herbal therapy, dietary supplements. 4) Manipulative and body-based methods (MBBM): massage therapy, exercise chiropractic or osteopathic. 5) Energy therapies (ET): energy healing, Reiki.
Considering that the vast majority of CAM interventions share input features, one single CAM intervention may fall within different categories; hence, the following adjusted classification and categorisation are proposed (
Figure 1).
Then, it is vital to determine the specific features and mechanisms of action of each CAM, given that every intervention may impact distinctly the physiological and psychological domains of each CAM user.
6. CAM Mechanisms of Action, Applications and Adverse Effects
6.1. Acupuncture Overview and Mechanism of Action
Acupuncture is an ancient Chinese medicine component that works with the "chi" (qi) or vital energy flowing in channels/meridians through the human body [
54]. According to this practice, a body becomes sick when the flow of "chi" is blocked or disrupted. Hence, acupuncture aims to restore the vital energy flow, stimulating certain meridian points [
35,
36].
Acupuncture is widely used around the world, producing numerous variations of the acupuncture therapy technique and its principles. However, the most used method is the collocation of solid-core and small needles that penetrate the skin, collocate alongside the body and are stimulated manually [
32]. In TCM, the stimulation of the needling sites, or acupoints, leads to the sensation of numbness, distension, or tingling at the needling site [
55]. This sensation is referred to as "de-qi", which radiates along to the corresponding meridian, inducing the desired effect. Acupressure is a different modality that interacts with the vital energy flowing in the meridians using the hands or fingers of the therapist. It has its origins in China and is based on the same principle as acupuncture [
51].
The effects of acupuncture are explained mainly by the diffuse noxious inhibitory control (DNIC) that involves the activation of the first neuron through mechanical, thermic, or chemical stimuli of nociceptors and polymodal receptors (PMR) [
56]. Primary nociceptive neuron depolarisation propagates through A-δ and C-afferent fibres, whereas PMR signals at the dorsal horn through A-β, A-δ and C-afferent fibres[
57,
58,
59]. These first neurons will then activate secondary afferent neurons in the spinal cord, depolarising tertiary neurons at superior brain structures such as the thalamus and the hypothalamus [
57,
60].
The local application of the needle primarily activates nociceptors and PMR, but it can also activate local vascular processes and inflammatory responses (e.g. mast cells) [
56,
61]. The literature demonstrates that several molecules are involved in the positive effects of acupuncture [
57,
61,
62]. For instance, P2X3 and TRPV1 receptors play a significant role in nerve conduction. In contrast, the inflammatory response is mediated by mast cells, microglia, astrocytes, and oligodendrocytes expressing OX-42, matrix metalloproteinase (MMP)-9/MMP-2, TNF-α, IL-1β, IL-6, and IL-10. Lastly, cell adaptation relies on the activation of CXCL1, p38MAPK, ERK, and C-Jun/N-terminal kinase signalling [
56,
60,
63].
Regarding the modulation of pain, mood, and behaviour in the CNS, acupuncture induces positive effects, most likely by the releasement of endogenous opioids (e.g. endorphins, enkephalins, dynorphins, nociceptin/orphanin) and neurotransmitters (e.g. 5-hydroxytryptamine, Noradrenaline, dopamine) [
55,
64,
65,
66]
Applications and Adverse Effects
Acupuncture is used to treat and manage a vast number of conditions and illnesses. Acute pain (e.g. postoperative pain, labour pain, dysmenorrhea, and migraine), chronic pain (e.g. low back pain, osteoarthritis, knee pain, neck pain, chronic shoulder pain), and behavioural conditions such as insomnia, anxiety, and depression are amongst the most common indications in the general population for the use of acupuncture [
62].
Unlike adults, because children often fear needles, acupuncturists stimulate acupoints and meridians using non-needle methods, such as heat, magnets, lasers, and massages [
35,
36]. Thus, acupressure is commonly used for children [
32,
67]. Among the wide list of conditions and illnesses in children treated with acupuncture, some studies have suggested positive outcomes for acupuncture. A systematic review evaluating RCT reported that acupuncture significantly reduced the incidence of nausea and vomiting in patients undergoing surgery [
68]. Alike, some studies, such as double-blind RCT conducted in children with headaches, found laser acupuncture to be superior to placebo in decreasing the number of headaches per month and severity [
69]. As well, clinical guidelines such as the NICE in young people and adults in the UK recommend acupuncture as prophylactic treatment for primary headache disorders such as tension type headache and migraine [
70]. Positive outcomes for acupuncture and conditions such as infant colic, nocturnal enuresis, dysmenorrhea, pain management, and allergic rhinitis have been described in other reviews [
71].
Regarding the safety of acupuncture for children, systematic reviews have shown that it is usually safe when practised by licensed and trained acupuncturists who follow studied and detailed protocols [
72,
73,
74]. Furthermore, the severe adverse effects of such practices are limited, suggesting that it is a relatively safe-practice [
32,
72,
75]. Confirming that acupuncture is a safe practice, Adams et al. (2011) [
72] found in a systematic review that most of the adverse effects were mild and included crying, pain, bruising, numbness, and haemorrhage in the site where the needles were placed. Also, dizziness and nausea were reported, whereas severe adverse effects were limited and linked to technical errors and unskilled practitioners rather than risks related to the procedure itself [
72]. Other severe adverse effects were reported in pneumothorax, nerve injury, vasovagal reaction, and, in some cases, cross infection when the needle is reused with an improper sterilisation technique[
54,
56].
6.2. Massage and Bodywork Overview and Mechanism of Action
Massage therapy is an ancient Chinese practice defined as the manipulation of soft tissue and muscles of the human body. It aims to enhance emotional and physical health [
75]. Massages are most commonly performed on the acupuncture/meridian points [
75]. However, the alternatives encompassed in massage and bodywork vary widely depending on the cultural and geographical background since most cultures have their own traditional massage methods [
35,
36].
Massage is believed to heal by raising the temperature in the manipulated tissues by promoting the targeted tissues' metabolism. That causes dilation of capillaries and fastens the circulation of blood and lymph. It also enhances the supply of nutrients in the surrounding muscles and tissues, promoting at the same time their growth and development [
76,
77].
The general physiological effects of massage remain unclear, but a possible explanation is based on the increase in blood circulation, a decrease in cortisol levels and an increase in the endogenous levels of serotonin; hence, a relaxation stage is reached, loosening muscles and joints and enhancing the overall feeling of well-being [
35,
36].
Application and Adverse Effects
Massage therapy is offered as support for a broad spectrum of health conditions; it has been reported that massage reduces gastrointestinal issues such as constipation and acute diarrhoea [
78], ameliorates asthma symptoms, reduces pain, and improves vascular circulation [
35,
36].
The available evidence, including systematic reviews and meta-analysis, heavily supports massage care as a suitable treatment for infants to treat conditions mainly related to improving growth rate and weight gain in premature infants [
79,
80,
81,
82,
83]. For instance, an RCT conducted on Indian neonates found that massage therapy can help premature infants gain around 476.76 g within 28 days in newborns with a birth weight of less than 1800 g [
84]. The stimulation of the vagal activity explains the beneficial effects of massage on newborns' weight gain. Hence, the levels of insulin-like growth factor-1 (IGF-1) increase as well as the gastric motility; consequently, there is a maturation of the sleep-wake state behaviour and an increase in the infant's weight [
81].
Additionally, promising results were found in a meta-analysis that analysed 26 studies encompassing 2,644 paediatric patients with the diagnosis of acute diarrhoea, where it was shown that massage care was clinically more effective than pharmacotherapy in treating paediatric acute diarrhoea (p<0.01) [
75]. The exact physiological mechanism of how massage might clinically improve acute diarrhoea is still not fully elucidated. Still, it is hypothesised that massage, as described before, enhances gastric motility and influences the secretion of hormones, cytokines, and gastric acid. Consequently, the spontaneous movements of the bowels are rhythmically enhanced [
75].
Still, in favour of massages, evidence suggests massage as a promising treatment for jaundice in newborns. An RCT studying 40 newborns of 34 to 36 weeks of gestation without any disease at birth found a decrease in the transcutaneous bilirubin levels of premature neonates who received massage interventions starting from the 3rd and 4th day (
p=0.003 and
p<0.001, respectively) when compared with the control group. Similarly, statistically significant differences were noted in the increasing stool frequency in favour of the massage group (
p=0.002) [
85]. The decreased levels of bilirubin and the increase in stool frequency are explained again by the stimulation of the vagal nerves and the stimulation of the gastric motility, which is caused by the release of gastrointestinal hormones, specifically gastrin and cholecystokinin, due to the stimulation of the peripheral nerves. Consequently, the digestion is accelerated, and therefore, the excretion of bilirubin through the stools [
85].
Concerning pain management, an RCT performed with 52 hospitalised children aged ten to 18 years suggested that massage therapy is useful in reducing the overall pain of children with cancer after each massage session (
p<0.001), as well as decreasing the pain related to walking (
p<0.05) [
77]. Pain improvement was measured using the Visual Analogue Scale (VAS). The positive effects of massage on decreasing pain have been attributed to the enhancement of blood circulation and lymphatic flow, as well as the reduced levels of stress-related hormones that induce a state of body relaxation and increase muscle tone and range [
77]. However, this is a single-blinded study limited to a small sample. Hence, more research exploring children's pain management is needed before drawing conclusions.
In summary, massage's most robust evidence suggests that this practice increases weight gain in premature infants [
79,
80,
81,
82,
83] and also reduces anxiety and suffering in hospitalised children and adolescents with psychiatric disorders [
35,
36].
6.3. Mind-Body Therapies
Mind-body therapies (MBT) can be generically conceptualised as any therapy that combines brain, mind, body and behaviours with the purpose of healing [
86]. These practices acknowledge that emotional, mental, social and spiritual factors directly impact health. MBT includes Tai Chi, Qigong, Yoga, meditation, and other types of relaxation (e.g. biofeedback, neurofeedback) [
87].
Given that MBT encompasses a broad variety of practices, describing a unique mechanism of action is complex; thus, the molecular and cellular effects of these practices over health will be described separately. Based on the available information, Yoga, meditation, and Tai Chi will be covered.
6.3.1. Yoga Overview and Mechanism of Action
Yoga is an ancient Hindu practice that has become more popular in Western countries in recent years. Yoga is generally used as a form of exercise and movement, whereas therapeutic Yoga works by uniting the mind, the body, and the spirit through conscious breathing and body postures [
88]. It is believed that Yoga influences the parasympathetic nervous system, reducing cortisol levels [
89] and heart rate [
88].
In 2012, according to the National Health Survey, in the USA, Yoga was positioned among the top five most commonly used CAM methods for children between two and 17 years old; the prevalence has increased from 3.1% in 2012 to 8.4% in 2017 [
13]. Within the paediatric population with mental health conditions, Yoga was found to occupy the third place of most common CAM therapies [
44].
Children facing mental health difficulties may seek Yoga because of the essential effects it has on psychological functioning. From a physiological perspective, RCT have suggested that the positive impact of Yoga might be linked to the effects on the sympathetic nervous system and the regulations of the hypothalamus-pituitary-adrenal axis. Systemically, Yoga decreases serum levels of IL-6, TNF-𝛂, and glucocorticoids [
86].
The aforementioned systemic changes can be molecularly explained by a yoga-induced decrease of NF-𝛋B activity and activation of glucocorticoid receptors; in consequence, heart rate decreases, tissular perfusion increases, and the overall mood is enhanced [
32,
86].
Yoga Applications and Adverse Effects
Having explained the physiological mechanism of Yoga, it is not surprising that a body of evidence evaluating systematic reviews, meta-analyses, and RCT interventions of Yoga in children has indicated positive effects mainly in behavioural conditions, control of anger, anxiety, stress, body dissatisfaction, control over emotions, self-esteem, and resilience [
32,
89].
Apart from enhancing mental well-being, a systematic review analysing 15 trials identified Yoga as a beneficial treatment for specific paediatric conditions such as asthma, irritable bowel syndrome (IBS), eating disorders, juvenile idiopathic arthritis, and fibromyalgia. Furthermore, it was found to improve some metabolic and hormonal parameters and chronic pain [
90].
The overall benefits of Yoga for conditions like IBS and eating disorders have also been mainly related to the decrease in anxiety and control over negative emotions caused by the course of the conditions. For instance, an RCT evaluating the effect of Yoga on 54 patients aged 11 to 21 years old with diagnosed eating disorders found decreased scores in their anxiety, depression, and food preoccupation. Consequently, the enhanced mental well-being facilitated the total clinical recovery of preexisting eating disorders [
91].
Although some studies conclude that Yoga might be promising, for instance, an exploratory and experimental study performed on children with Autism Spectrum Disorder (ASD) reported that Yoga intervention significantly reduces sleep, gastrointestinal and behavioural problems [
92]. Regarding paediatric cancer, pilot non-RCTs have supported the safety and efficacy of Yoga [
93]. At the same time, some other systematic reviews show inconclusive results in recommending Yoga as an effective mental health intervention in children, given the identified heterogeneity in measured outcomes and the diverse and non-comparable populations [
94,
95].
When assessing Yoga's safety, the existing literature identifies a few adverse effects of this practice. According to evidence, Yoga and MBT are considered relatively safe practices in the general population [
32]. A systematic review and meta-analysis of RCT investigating the safety of Yoga found that 57% of the trials did not report any adverse effect, and from the reported adverse events, only 2.2% were classified as intervention-related. Among these effects, 10.9% were non-serious events (e.g. musculoskeletal injuries), and 0.6% were severe events (e.g. permanent physical disabilities and injuries needing surgical interventions). The systematic review also reported low bias risk and low heterogeneity of trials [
96]. Similarly, more systematic reviews have concluded that Yoga is safe and effective [
96,
97].
Considering the evidence mentioned above, it can be concluded that Yoga is a safe and cost-effective practice that can be a reasonable method to improve overall well-being and enhance mental health conditions, stress, and anxiety in children.
6.3.2. Meditation Overview and Mechanism of Action
Meditation practices are part of the mind-body therapies that originally came from traditional contemplative practices used in ancient cultures under a spiritual basis with a focus on gaining body consciousness [
88].
Meditation encompasses different practices (
Table 1) that generally work with concentration and attention. However, providing a specific definition is complex since there is a wide variety of techniques and types, each with its own characteristics and definition. However, all forms have a common component: training the mind [
98].
As observed with other already discussed CAM interventions, meditation techniques have recently gained popularity. In the USA, for example, in 2012, approximately 0.6% of children aged 4 to 17 years practised any form of meditation, whereas, in 2017, 5.4% of children were found to use meditation [
99].
Unlike ancient meditation practices, nowadays, meditation has been incorporated into modern practices and cultures without spirituality and religious settings [
98]. Within the modern meditation practices, and despite the different techniques used to meditate, they all fundamentally increase the awareness and the sense of self through intentional practices such as breathing, listening, specific movements, and sounds [
100].
Little is known about the physiological effects of mediation practices among children. Still, a systematic review and meta-analysis suggests that meditation decreases physiological stress-related substances, such as cortisol, C-reactive protein, triglycerides, and TNF-𝛂. A relaxation state induced by meditation decreases heart rate, blood pressure, and expression of inflammatory cytokines, leading to feelings of well-being [
101].
Meditation Applications
The positive effects of meditation on children's mental well-being have drawn research attention to the possible impact on meditating children's cognitive functioning and behavioural improvements, specifically Mindfulness [
102]. A single-blinded RCT study conducted in 32 Italian children comparing mindfulness-oriented meditation (MOM) versus active control conditions without meditation found that Mindfulness can effectively improve cognitive, emotional, and social abilities in children [
102]. The importance of such results centres on the possibilities of reaching clinical improvements in mental conditions such as ADHD, autism spectrum, and behavioural disorders of children, which are generally difficult to treat by mainstream medicine [
102]. Focusing on children with ADHD, a systematic review and meta-analysis evaluating RCTs reported that mindfulness-based therapies improved ADHD symptoms (
p = 0.006). However, significant heterogeneity in the measured outcomes (e.g. effects on internalising behavioural problems, externalising behavioural problems, parental stress) was also reported, portraying the overall complexity when interpreting the possible benefits of mindfulness-based interventions [
103].
Besides, some authors have suggested that meditation should be included in academic curricula to help children improve their attention and help children with behavioural difficulties [
98,
100]. However, research exploring the link between improved cognitive functions has recently emerged. Hence, more trials are still needed to analyse the benefits of mindfulness. Despite being promising, available evidence still does not warrant the effectiveness of Mindfulness for such conditions [
102,
103].
6.3.3. Tai Chi Overview and Mechanism of Action
Tai Chi is a mind-body exercise rooted in Chinese culture; it literally translates to "Grand Ultimate,' and is considered a philosophical and theoretical practice that seeks balance (Qi balance) between interactive dualistic phenomena through meditative movement. The practice involves dynamic dance-like postures, relaxation and breathing control [
104,
105].
Traditional Tai Chi has three fundamental principles: body, breath, and mind focus. Typically, Tai Chi consists of a complex series of sequenced and choreographed movements, meditation, visualisation, and deep abdominal breathing techniques that induce a relaxation state leading to health enhancement [
104].
It has been suggested that Tai Chi has multiple central and peripheral effects, mainly influencing the autonomous nervous and immune systems [
106]. However, Tai Chi effects are not limited to the systems mentioned earlier; it has also been reported that Tai Chi practices also impact neurological function [
107] and musculoskeletal systems in children and young population [
108,
109,
110].
As a consequence of the stimulation of the autonomic nervous system, Tai Chi reduces heart frequency and improves tissue perfusion; this last effect is mediated by both the recruitment of reserve capillaries and the increase of the VO
2 peak [
111]. Neurological effects are mediated by the modulation of neurotransmitters (e.g. dopamine, serotonin, and adrenaline) and neuromodulators (e.g. endorphins, brain-derived neurotrophic factor (BDNF) and insulin-like growth factor (IGF)) that in conjunction can elicit neuroplasticity with structural and functional brain changes [
108].
Regarding the immune system, Tai Chi has been shown to decrease inflammatory cytokines (e.g. IL-6, IL-8) and other inflammatory markers (e.g. cortisol and C-reactive protein) [
106,
108]. Additionally, it has been reported that after Tai Chi is practised, monocytes decrease the expression of TNF-𝛂 and IL-6; the described modulation is also associated with the upregulation of the interferon regulatory factor (IRF) family and the downregulation of NF-𝛋B transcription factors resulting in the modulation of the inflammatory response [
86].
Moreover, Tai Chi also exerts effects on oxidative stress, including the increase of glutathione peroxidase, catalase, and superoxide dismutase levels. Such enzymes, classified as scavengers, positively enhance the total antioxidant capacity [
112].
Tai Chi Applications
In the general population, Tai chi has been used to treat a wide variety of conditions and illnesses. Existing scientific evidence suggests that Tai Chi is useful for decreasing pain, increasing range of motion, improving proprioception, and enhancing mental health and well-being. Additionally, Tai Chi is used to treat respiratory diseases and as an additional treatment for cardiovascular conditions such as hypertension and heart failure [
104].
Supporting the beneficial effects of Tai Chi on cardiovascular function, some studies have reported decreased systolic and diastolic blood pressure in hypertensive patients and a delay in heart failure progression [
9,
111,
113]. Moreover, other studies have suggested that Tai Chi reduces serum levels of the B-type natriuretic peptide and levels of serum lipids, including total cholesterol, total triglycerides, and low-density lipoproteins type C [
111,
113].
Regarding the paediatric population, literature reports that children commonly practise Tai Chi as a general physical practice aiming to decrease obesity and overweight and to improve well-being and physical fitness. Also, some RCTs have shown positive effects on respiratory fitness, balance, coordination of upper limbs, and functional mobility, particularly in patients with intellectual disabilities and children with balance disorders [
110,
114,
115].
In conclusion, Tai Chi's strongest scientific evidence in children favours its practice as a general physical activity with beneficial effects on overall fitness and body weight, particularly applicable to children with coordination disorders. Based on the results mentioned earlier regarding studies conducted in adults, the positive results impacting cardiovascular and respiratory function should be explored and evaluated in the paediatric population.
6.4. Herbal Medicine Overview and Mechanism of Action
Herbal medicine is defined as all those products made exclusively of active herbal substances [
116]. Medicinal treatments include various components of the plants encompassing their specific parts, such as the root, leaves, seeds, fruits or flowers, or the dried plant [
117]. Some of these components can be prepared as an infusion, tea, pill, extract, oil, and cream [
117].
Herbs' medicinal properties have been used for centuries, especially in indigenous cultures, to treat several children's symptoms and illnesses [
118]. Places such as China, India, and Egypt were pioneers in herbal medicine, and in Western countries, herbs were commonly used during mediaeval times [
117].
Similar to many other therapies, the tendency to use herbal medicine is rising in some countries, such as the USA [
119]. The general population's global rate of using herbal remedies is around 80% of adults and children, with an estimated prevalence of 18% among the paediatric population [
120]. According to the USA national survey in 2012, herbal remedies accounted for the most used CAM method, with 3.9% of children under CAM treatment [
13].
Unlike herbal medicine, a drug is defined as anything that enters the body and produces physiological changes that are used for prevention (e.g. vaccines, vitamins, diet) or to treat pathological conditions (e.g. hypothyroidism, malnutrition, diabetes) [
121]. Taking into account this pharmacological principle, herbs cannot be prescribed as if they were an "active drug principle", given that herbs components broadly differ due to several intrinsic and extrinsic factors such as circadian rhythm, type of species, seasonal variations, soil, geographical conditions, harvesting and processing methods [
122].
Unlike herbal medicine, "active drug principles" have a well-defined physicochemical profile, pharmacokinetics, bioavailability, and posology. In herbal medicine, many species' pharmacological profiles and active compounds are not properly elucidated [
123]. Since herbal medicines are a collection of multiple molecules in a single plant fragment, elucidating the mechanisms of action and precise posology remains remarkably challenging [
124].
Herbal medicine practitioners and academics suggest that herbolary's prophylactic and therapeutic properties are influenced by the synergistic effect of the multiple herb compounds [
123]. Hence, rather than using a single active drug principle as in Western medicine, the selected herb fragment should be utilised as a whole under the premise that such plant parts have greater therapeutic properties than the individual sum of its compounds [
125].
Applications and Adverse Effects
Despite the vast number of plants and their possible properties, parents often seek herbal remedies to treat their children for conditions such as upper respiratory tract infections, cough, "common colds", noninfective gastroenteritis and colitis, pain in throat and chest, asthma, cancer, neurologic disorders, atopic dermatitis, abdominal pain, and prophylactic treatments for different conditions [
118,
126,
127].
Parents usually choose herbal medicine for their children under the generic belief that they are effective and safe because herbal remedies come from natural sources [
127]. Nevertheless, many herbs' therapeutic actions have been poorly understood because some active substances have not yet been identified as chemical-defined ingredients; hence, examining the properties of herbs and conducting clinical trials testing their effectiveness is complex [
126]. Besides, due to the lack of knowledge of the active substances, herbs' dosage is based on subjective perceptions, signifying a potential risk of adverse effects, overdoses, and poisoning [
118].
Available evidence of some commonly used herbs such as
Gingko biloba,
Zingiber officinale (ginger), peppermint oil, and Echinacea suggests promising and beneficial effects among the paediatric population. In some RCTs conducted on children and adolescents with ADHD using herbs such as
Gingko biloba and
Valeriana officinalis, it was reported that such herbs might ameliorate ADHD symptoms [
128,
129]. However, systematic reviews and meta-analyses assessing the possible effects of herbs on children with ADHD have concluded that available evidence is inconclusive and insufficient to recommend herbs as an alternative treatment for ADHD [
130,
131,
132,
133].
Some other herbal compounds, such as peppermint oil and ginger, have been evaluated as possible treatments for gastrointestinal disorders, including functional abdominal pain, irritable bowel symptoms and gastroenteritis in children [
133,
134,
135,
136,
137]. An RCT conducted in 75 children with acute gastroenteritis found that ginger is an effective intervention to improve vomiting compared to placebo (
p = 0.003) [
135]. Still, in gastrointestinal disorders, RCT assessing the effects of peppermint oil in irritable bowel syndrome reported that peppermint oil is only effective in decreasing abdominal pain intensity compared to placebo (
p=0.001) [
138]. However, peppermint oil did not show significant changes when assessing belching, abdominal distention, heartburn, gas, or abdominal rumbling. Similar results were found in other RCT, showing no significant differences in gut motility, gastric emptying, and contractility when using pepper mint oil in children with functional abdominal pain [
136].
Some other herbs, such as
Echinacea spp. and
Astragalus spp., have been used as treatment interventions for respiratory conditions in the paediatric population [
139,
140,
141,
142]. For instance, in an RCT evaluating Echinacea's effectiveness in preventing viral respiratory tract infections in children, Echinacea appeared to be effective in reducing episodes of viral respiratory tract infections compared to vitamin C (
p = 0.021) [
140]. Another mini-review of RCT evaluating Echinacea's effect against coronavirus in children and adults agrees that Echinacea may exhibit antiviral activity[
141].
Despite a number of clinical trials reporting positive effects for different herbs such as the aforementioned, it is fundamental to acknowledge that results should be interpreted with caution, given that their validity and generalizability to the paediatric population are commonly hampered by methodological heterogeneity, lack of long-term follow-ups, small sample sizes and absence of common clinical and objective measurements as concluded in available systematic reviews [
130,
131,
132,
133,
143]. Further research is needed in this area to address knowledge gaps and establish the efficacy and safety profiles of herbal treatments, thus potentially providing alternative treatment approaches for consideration in clinical practice.
6.5. Energy Therapy
6.5.1. Reiki Overview and Mechanism of Action
Reiki is an energy healing or biofield therapy rooted in Japan around the late 19th century. Literally speaking, "Rei" means universal and "ki" life energy, and the term can be translated into "universal life energy" [
144,
145].
Reiki sustains the idea that universal energy directly supports the human body's ability to heal; hence, this technique seeks to send energy through the therapist's hands to the sick body, enhancing its innate ability to heal and restore its natural balance [
144,
146].
Given this energetical practice's nature and characteristics, elucidating the exact mechanism of action is complex. Studies conducted in animal models have not shown enough scientific evidence suggesting direct induction of physiological changes by Reiki practice; however, it has been proposed that Reiki activates the parasympathetic nervous system through the induction of a relaxation status resulting in reduced cortisol, heart rate, and blood pressure [
144,
147]. Still, these effects remain highly controversial since some other authors have found no correlation between reductions in neither heart rate nor blood pressure and Reiki in animal models. For instance, a study described that those rats who received 15 minutes of Reiki showed a decreased heart rate compared with rats receiving sham Reiki (individuals who mimic Reiki movements without proper formation in Reiki). However, no significant changes in blood pressure were found; hence, results cannot be extrapolated to the general population [
148]. Additionally, another study conducted on 189 oncologic patients found similar results for the sham Reiki placebo and Reiki concerning well-being and comfort, concluding that neither sham Reiki placebo nor Reiki alters the physical well-being of oncologic patients. However, this study has highlighted the effect of "being with", defined as being emotionally present to others, implying that Reiki therapy has a positive psychological impact on the sense and feeling of receiving extra attention, caring, and privacy, as a consequence, enhances the patient's perception of well-being [
149].
In summary, Reiki's effects on health remain controversial, and scientific evidence yields paradoxical results; documented psychological effects such as well-being, relaxation, and comfort outweigh the objective physiological effects of Reiki.
Reiki Applications
In the general population, Reiki therapy has been used as a treatment or as a supportive measure for several conditions, mainly within palliative care in patients with end-stage cancer and severe pain. For instance, It has been reported that Reiki may have a significant effect on pain relief in the areas of dental surgery, chronic pain, abdominal hysterectomies, post-caesarean surgeries, and neuropathic pain [
146].
In an RCT, it was found that patients with a diagnosis of cancer who used Reiki as a supportive therapy reported a positive experience concerning mood-related symptoms, including a decrease in anxiety, reduced isolation and loneliness, better attitude, improved appetite, and quality of sleep [
150,
151,
152]. Likewise, Reiki has been used in the field of mental health and well-being, showing beneficial results in decreasing depression, anxiety, and stress symptoms in non-related oncological patients [
149,
153].
In the paediatric population, literature is scarce. However, some pilot studies have been conducted in children with a diagnosis of cancer and hematopoietic stem-cell transplantation patients, showing promising results in reducing pain. Still, the authors conclude that there is no statistical significance in relation to objective variables; however, an overall improvement in pain perception was achieved [
152,
154].
In summary, Reiki has not shown statistically significant effects over physiological pathways and variables, but a trend towards pain improvement and overall well-being has been suggested.
7. Conclusion, Limitations & Future Perspectives
It has been documented that CAM therapies are rooted in ancient cultures with a predominant influence from Oriental countries. However, nowadays, the prevalence of CAM users is increasing worldwide, particularly in Western countries. That tendency leads to a shift towards a global healthcare paradigm in relation to Western healthcare practices and the acceptance of CAM within the formal healthcare systems.
The nature of this paradigm relies on controversies between different CAM scientific perspectives. On the one hand, some scholars suggest CAM "might" be helpful and safe for certain conditions if prescribed and supervised by health professionals. On the other hand, conservative scholars have suggested that CAM interventions lack scientific evidence supporting its use as an isolated or adjunctive therapy, given that the offered evidence fails to prove objective and statistically significant results over physiological or pathophysiological processes. This paradigm highlights the need for new research to evaluate these practices' efficacy, safety, and cultural integration in international and national healthcare settings.
The vast majority of existing studies assessing children and CAM have focused on particular conditions or diseases among children or within specific cultures or geographical regions. Therefore, conclusions regarding the effectiveness and safety of CAM interventions are broad. Amongst the CAM therapies covered in this review (
Table 2), acupuncture, Tai Chi, Yoga, meditation, massage, and bodywork have stood out, given the scientific rigour and objectivity of the evidence supporting their use for the general and paediatric population.
Evidence favouring the aforementioned therapies suggests that positive effects are mainly related to relaxation status and modulation of the Autonomic Nervous System that positively impact overall well-being and improve mood behavioural conditions (e.g. anxiety, stress, insomnia, depression) and enhance pain relief. Within specific non-objective parameters, CAM therapies improve the perception of overall body shape, disease-related symptoms, comfort, mental well-being, and quality of life. However, for some of the described CAM therapies, scientific evidence mostly failed to demonstrate tangible effects over physiological pathways and biological processes.
Despite our extensive literature review, it is challenging to determine a global consensus on integrating CAM as a single and homogeneous concept due to the internal idiosyncrasies and cultural perceptions of each country implementing CAM in their healthcare systems and the diverse public health regulations. Moreover, the lack of consensus and polarised positions among conventional professionals regarding mechanisms of action, applications, and effectiveness of CAM makes it challenging to draw firm conclusions. This situation highlights the need for high-quality research examining the efficacy and safety of CAM therapies in vulnerable populations, such as children.
Another potential limitation of this manuscript is the variability in the quality and methodology of the studies included in this review, which might hinder the direct comparison of outcomes and generalisation of findings. Lastly, the potential lack of long-term longitudinal studies limits understanding of the long-term impact of CAM therapies on paediatric health, especially regarding side effects, drug interactions, and long-term health outcomes.
Therefore, obtaining more knowledge and scientific evidence of CAM's effectiveness and safety will help decrease morbidity and mortality rates related to ineffective and unsafe health practices. CAM practitioners and mainstream healthcare professionals require a collaborative effort with a multidisciplinary approach to improve conventional medical practices and patients' overall well-being. This multidisciplinary and collaborative approach allows holistic and personalised therapies to fulfil each child's physical, psychological, and mental needs.
Our research highlights the need for further investigation into CAM in paediatric care, as it opens up new questions that warrant exploration. This study lays the groundwork for future inquiries, emphasising the importance of addressing critical issues such as CAM therapies' safety, efficacy, and mechanisms of action and their integration into clinical settings. Additionally, it underscores the importance of launching scientific awareness campaigns aimed at healthcare personnel to clearly define CAM's objective capabilities and limitations in the clinical context. It also advocates CAM researchers and practitioners prioritising objective and rigorous evaluation methods, thereby fostering an informed and holistic approach to paediatric healthcare. This holistic approach should integrate evidence-based practices, combining scientific evidence, the patient's values and beliefs, and clinical expertise.
An evidence-based healthcare system, anchored in primary healthcare, directs its structures and functions towards the values of equity and social solidarity without distinction, suggesting adherence to the highest standards of quality and safety and implementing intersectoral interventions.
Furthermore, a multidisciplinary and collaborative approach must be integrated at all healthcare levels. This approach involves distinct healthcare professionals such as physicians, nutritionists, psychologists, odontologists, CAM and Traditional Medicine practitioners, and active participation from paediatric patients and their guardians. Embracing diverse expertise ensures a comprehensive and inclusive healthcare strategy that addresses the holistic well-being of individuals across various medical disciplines.
In conclusion, even though there are promising results in favour of CAM, this literature review shows and concludes that available scientific evidence is significant enough to only recommend CAM as a complementary therapy rather than an alternative to enhance mental well-being and physical fitness in the paediatric population.
Author Contributions
PAR-G developed the idea. PAR-G and SQR-L accomplished the review framework. PAR-G, SQR-L, SR-P, JJM-G, JAC-M, SG-S wrote the first draft of the manuscript. PAR-G, SQR-L, SR-P, JJM-G, JAC-M, SG-S, and SK supervised manuscript writing and performed the final editing. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
We extend our gratitude to Daniel Ayala-Moreno, Digital Content Designer at the Department of Communication and Marketing, Universidad Autónoma de Guadalajara, for his valuable contribution to the figure's design in this manuscript.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Glossary
| Glossary |
| Acupuncture |
An occupational discipline of the traditional Chinese methods that comprises the insertion of needles along specific pathways or meridians. The placement varies with the disease being treated. |
| Being with |
Perception of being emotionally accompanied by other. |
| CAM practitioner |
A CAM practitioner is someone who delivers a range of healthcare services and therapies that are beyond the scope of conventional medical treatment. Unlike conventional healthcare professionals, the training requirements for those who practice CAM often vary considerably. There are various means by which these practitioners obtain their skills such as certificate programs, apprenticeships, workshops, or self-study |
| Comfort |
Patient care intended to prevent or relieve suffering in conditions that ensure optimal quality living. (MeSH). |
| Complementary and alternative medicine |
Broad set of healthcare practices that are not part of the conventional health system practices. |
| Dependents |
A child or other individual who relies on a parent, relative, or other person for support in the domain of care to carry out a set of activities necessary for the maintenance of life, health, and well-being, compensating a self-care deficit. |
| Herbal Medicine |
The study of medicines derived from botanical sources. (MeSH definition). |
| Integrative medicine |
Combination of conventional and unconventional medicine that addresses the biological, psychological, social, and spiritual aspects of health and illness. |
| Mandala |
Mandala is a Sanskrit term which translates to circle, sphere, integrity, and completion. These geometrical figures are traditionally used as an aide to meditation by drawing the eye to the centre of the sphere. |
| Massage |
The systematic and methodical manipulations of body tissues best performed with the hands for the purpose of affecting the nervous and muscular systems and the general circulation (MeSH definition). |
| Meditation |
A state of consciousness that trains the mind to eliminate the external stimuli and focus on an isolated entity eliciting stress relief and relaxation. |
| Mindfulness |
The practice of being aware of your body, mind, and feelings in the present moment, thought to create a feeling of calm. (Cambridge dictionary). |
| Randomised control trial |
It is an experimental study in which subjects are randomly assigned to two distinct groups, experimental (receiving the intervention that is being tested) and control (receiving an alternative treatment). |
| Reiki |
Energy healing or biofield therapy that consists in placing the hands of the healer upon the clients with the intent to be cured with spiritual energetic healing. |
| Sham |
Something that is not what it seems to be and is intended to deceive, or someone who pretends to be something they are not. (Cambridge dictionary). |
| Tai Chi |
Mind-body meditative exercise that involves dynamic dance-like postures, relaxation and breathing control. |
| Tonglen practice |
The Tibetan term "Tonglen" translates to "sending and taking." It is an ancient type of meditation that centres on breathing techniques and compassion. |
| Traditional Chinese Medicine |
It represents an ancient medical model characterised by an emphasis on the maintenance of mind-body homeostasis and the intricate interplay between the human body and its surrounding environment. Rooted in a personalised and holistic framework, TCM addresses pathological states by employing a wide range of psychological and physical strategies that may include natural therapeutic agents customised to individual symptomatology. |
| Traditional medicine |
It is the sum of the knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures, which may not be explained by modern medicine, used in the maintenance of health and the prevention, diagnosis, improvement or treatment of physical and mental illness. (modified from World health organisation). |
| Vipassana |
type of meditation that focuses on mental training with the purpose of improving the proprioceptive and somatic awareness impacting the attentional style. |
| Well-being |
The state of healthiness and happiness covering the physical and mental conditions of an individual. |
| Yoga |
Hindu philosophical practice that works by uniting the mind, the body, and the spirit through conscious breathing and body postures. |
References
- Xue, C.C. Traditional, complementary and alternative medicine: policy and public health perspectives. Bulletin of the World Health Organization: International Journal of Public Health 2008, 86, 77-77.
- Mortada, E.M. Evidence-Based Complementary and Alternative Medicine in Current Medical Practice. Cureus 2024, 16, e52041. [CrossRef]
- World Health Organization (WHO) Traditional, Complementary and Integrative Medicine. Available online: https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine#tab=tab_1 (accessed on.
- Lue, H.-C.; Su, Y.-C.; Lin, S.J.-S.; Huang, Y.-C.; Chang, Y.-H.; Lin, I.H.; Yang, S.-P. Taipei consensus on integrative traditional Chinese and Western Medicine. Journal of the Formosan Medical Association 2021, 120, 34-47. [CrossRef]
- Hao, X.U.; Keji, C. The integration of traditional Chinese medicine and Western medicine. European Review 2003, 11, 225-235. [CrossRef]
- Jun, R.; Xun, L.; Jin, S.; Mei, H.; Guo-Yan, Y.; Wen-Yuan, L.; Nicola, R.; George, L.; Jian-Ping, L. Is traditional Chinese medicine recommended in Western medicine clinical practice guidelines in China? A systematic analysis. BMJ Open 2015, 5, e006572. [CrossRef]
- Qian, Z.; Wang, G.Y.; Henning, M.; Chen, Y. Understanding health literacy from a traditional Chinese medicine perspective. Journal of Integrative Medicine 2023, 21, 215-220. [CrossRef]
- Ng, J.Y.; Dhawan, T.; Fajardo, R.-G.; Masood, H.A.; Sunderji, S.; Wieland, L.S.; Moher, D. The Brief History of Complementary, Alternative, and Integrative Medicine Terminology and the Development and Creation of an Operational Definition. Integrative Medicine Research 2023, 12, 100978. [CrossRef]
- Chow, S.L.; Bozkurt, B.; Baker, W.L.; Bleske, B.E.; Breathett, K.; Fonarow, G.C.; Greenberg, B.; Khazanie, P.; Leclerc, J.; Morris, A.A.; et al. Complementary and Alternative Medicines in the Management of Heart Failure: A Scientific Statement From the American Heart Association. 2023, 147, e4-e30. [CrossRef]
- Bataller-Sifre, R.; Bataller-Alberola, A. What does "integrative medicine" provide to daily scientific clinical care? Revista Clinica Espanola 2015, 215, 451-453. [CrossRef]
- Tangkiatkumjai, M.; Boardman, H.; Walker, D.-M. Potential factors that influence usage of complementary and alternative medicine worldwide: a systematic review. BMC Complementary Medicine and Therapies 2020, 20, 363. [CrossRef]
- Zuzak, T.J.; Bonkova, J.; Careddu, D.; Garami, M.; Hadjipanayis, A.; Jazbec, J.; Merrick, J.; Miller, J.; Ozturk, C.; Persson, I.A.L.; et al. Use of complementary and alternative medicine by children in Europe: Published data and expert perspectives. Complementary Therapies in Medicine 2013, 21, S34-S47. [CrossRef]
- Black, L.I.; Clarke, T.C.; Barnes, P.M.; Stussman, B.J.; Nahin, R.L. Use of complementary health approaches among children aged 4-17 years in the United States: National Health Interview Survey, 2007-2012. National health statistics reports 2015, 1-19.
- Mosavat, S.H.; Heydari, M.; Hashempur, M.H.; Dehghani, S.M. Use of complementary and alternative medicine among paediatric patients with hepatogastrointestinal diseases. Eastern Mediterranean Health Journal 2018, 24, 1018-1025. [CrossRef]
- Pineiro Perez, R.; Nunez Cuadros, E.; Rodriguez Marrodan, B.; Garcia Cabrera, L.; Manzano Blanco, S.; Escrig Fernandez, R.; Calvo, C. Position Statement From The Spanish Association Of Paediatrics Medicines Committee Concerning The Use Of Alternative Medicine And Pseudo-Science In Children. Anales de pediatria (Barcelona, Spain : 2003) 2019, 91, 272.e271-272.e275. [CrossRef]
- Lim, A.; Cranswick, N.; South, M. Adverse events associated with the use of complementary and alternative medicine in children. Archives of Disease in Childhood 2011, 96, 297. [CrossRef]
- Park, Y.L.; Canaway, R. Integrating Traditional and Complementary Medicine with National Healthcare Systems for Universal Health Coverage in Asia and the Western Pacific. Health Systems & Reform 2019, 5, 24-31. [CrossRef]
- Møller, S.R.; Ekholm, O.; Christensen, A.I. Trends in the use of complementary and alternative medicine between 1987 and 2021 in Denmark. BMC Complementary Medicine and Therapies 2024, 24, 23. [CrossRef]
- Kollikowski, A.; Gabriel, K.M.A.; Schiffmann, L.; Gágyor, I.; Güthlin, C.; Heuschmann, P.U.; Langhorst, J.; Keil, T.; Löffler, C. Complementary Medicine in Acute Care Hospitals: Questionnaire Survey with Heads of Bavarian Hospitals. Complementary Medicine Research 2023, 30, 415-423. [CrossRef]
- Kemppainen, L.M.; Kemppainen, T.T.; Reippainen, J.A.; Salmenniemi, S.T.; Vuolanto, P.H. Use of complementary and alternative medicine in Europe: Health-related and sociodemographic determinants. 2018, 46, 448-455. [CrossRef]
- (NIH), N.C.f.C.a.I.H. Use of Complementary Health Approaches for Pain by U.S. Adults Increased From 2002 to 2022. Available online: https://www.nccih.nih.gov/research/research-results/use-of-complementary-health-approaches-for-pain-by-us-adults-increased-from-2002-to-2022 (accessed on 22 feb 2024).
- (NIH), N.C.f.C.a.I.H.o.o.b. Appropriations History by Institute/Center (1938 to Present). Available online: https://officeofbudget.od.nih.gov/approp_hist.html (accessed on 24/03/2024).
- (NIH), N.C.f.C.a.I.H. Complementary and Alternative Medicine Funding by NIH Institute/Center. Available online: https://www.nccih.nih.gov/about/budget/complementary-and-alternative-medicine-funding-by-nih-institutecenter (accessed on.
- Mohd Mujar, N.M.; Dahlui, M.; Emran, N.A.; Abdul Hadi, I.; Wai, Y.Y.; Arulanantham, S.; Hooi, C.C.; Mohd Taib, N.A. Complementary and alternative medicine (CAM) use and delays in presentation and diagnosis of breast cancer patients in public hospitals in Malaysia. PLoS One 2017, 12, e0176394. [CrossRef]
- Sari, N.M.; Devansyah, S.; Modjaningrat, I.; Suryawan, N.; Susanah, S.; Rakhmillah, L.; Wahyudi, K.; Kaspers, G.J.L. Type of cancer and complementary and alternative medicine are determinant factors for the patient delay experienced by children with cancer: A study in West Java, Indonesia. 2023, 70, e30192. [CrossRef]
- Kranjcec, I.; Abdovic, S.; Buljan, D.; Matijasic, N.; Slukan, M.; Stepan, J. Complementary Medicine Practice and Use of Dietary Supplements in Pediatric Cancer Patients in Croatia. Cureus 2022, 14, e30246. [CrossRef]
- Stampini, V.; Bortoluzzi, S.; Allara, E.; Amadori, R.; Surico, D.; Prodam, F.; Barone-Adesi, F.; Faggiano, F. The use of Complementary and Alternative Medicine (CAM) among Italian children: A cross-sectional survey. Complementary Therapies in Medicine 2019, 47, 102184. [CrossRef]
- Italia, S.; Wolfenstetter, S.B.; Teuner, C.M. Patterns of Complementary and Alternative Medicine (CAM) use in children: a systematic review. European Journal of Pediatrics 2014, 173, 1413-1428. [CrossRef]
- Hunt, K.; Ernst, E. The evidence-base for complementary medicine in children: a critical overview of systematic reviews. Archives of Disease in Childhood 2011, 96, 769-776. [CrossRef]
- Complementary, C.o.t.U.o.; Public, A.M.b.t.A. Complementary and alternative medicine in the United States; National Academies Press: 2005.
- Birdee, G.S.; Phillips, R.S.; Davis, R.B.; Gardiner, P. Factors associated with pediatric use of complementary and alternative medicine. Pediatrics 2010, 125, 249-256. [CrossRef]
- McClafferty, H.; Vohra, S.; Bailey, M.; Brown, M.; Esparham, A.; Gerstbacher, D.; Golianu, B.; Niemi, A.-K.; Sibinga, E.; Weydert, J.; et al. Pediatric Integrative Medicine. Pediatrics 2017, 140. [CrossRef]
- Italia, S.; Bruske, I.; Heinrich, J.; Berdel, D.; von Berg, A.; Lehmann, I.; Standl, M.; Wolfenstetter, S.B. Complementary and Alternative Medicine Use Among Chronically Ill Adolescents from 2 German Birth Cohorts. Forsch Komplementmed 2016, 23, 246-252. [CrossRef]
- Ventola, C.L. Current Issues Regarding Complementary and Alternative Medicine (CAM) in the United States: Part 1: The Widespread Use of CAM and the Need for Better-Informed Health Care Professionals to Provide Patient Counseling. P T 2010, 35, 461-468.
- Kathi J Kemper, M., MPH. Complementary and integrative health in pediatrics. UpToDate 2023, 2023.
- Mora, D.C.; Kristoffersen, A.E.; Overvag, G.; Jong, M.C.; Mentink, M.; Liu, J.; Stub, T. Safety of Complementary and Alternative Medicine (CAM) treatment among children and young adults who suffer from adverse effects of conventional cancer treatment: A systematic review. Integr Cancer Ther 2022, 21, 15347354221105563. [CrossRef]
- Snyder, J.; Brown, P. Complementary and alternative medicine in children: an analysis of the recent literature. Curr Opin Pediatr 2012, 24, 539-546. [CrossRef]
- Lucas, S.; Leach, M.; Kumar, S. Complementary and alternative medicine utilisation for the management of acute respiratory tract infection in children: A systematic review. Complement Ther Med 2018, 37, 158-166. [CrossRef]
- Kim, J.-H.; Nam, C.-M.; Kim, M.-Y.; Lee, D.-C. The use of complementary and alternative medicine (CAM) in children: a telephone-based survey in Korea. BMC Complementary and Alternative Medicine 2012, 12, 46. [CrossRef]
- Wilson, K.M.; Klein, J.D.; Sesselberg, T.S.; Yussman, S.M.; Markow, D.B.; Green, A.E.; West, J.C.; Gray, N.J. Use of complementary medicine and dietary supplements among U.S. adolescents. J Adolesc Health 2006, 38, 385-394. [CrossRef]
- Rossler, W.; Lauber, C.; Angst, J.; Haker, H.; Gamma, A.; Eich, D.; Kessler, R.C.; Ajdacic-Gross, V. The use of complementary and alternative medicine in the general population: results from a longitudinal community study. Psychol Med 2007, 37, 73-84. [CrossRef]
- Cincotta, D.R.; Crawford, N.W.; Lim, A.; Cranswick, N.E.; Skull, S.; South, M.; Powell, C.V. Comparison of complementary and alternative medicine use: reasons and motivations between two tertiary children's hospitals. Arch Dis Child 2006, 91, 153-158. [CrossRef]
- Shih, V.; Chiang, J.Y.; Chan, A. Complementary and alternative medicine (CAM) usage in Singaporean adult cancer patients. Ann Oncol 2009, 20, 752-757. [CrossRef]
- Wang, C.; Preisser, J.; Chung, Y.; Li, K. Complementary and alternative medicine use among children with mental health issues: results from the National Health Interview Survey. Bmc Complementary and Alternative Medicine 2018, 18. [CrossRef]
- Wang, C.; Li, K.; Gaylord, S. Prevalence, patterns, and predictors of meditation use among US children: Results from the National Health Interview Survey. Complementary Therapies in Medicine 2019, 43, 271-276. [CrossRef]
- Gad, A.; Al-Faris, E.; Al-Rowais, N.; Al-Rukban, M. Use of complementary and alternative medicine for children: a parents' perspective. Complement Ther Med 2013, 21, 496-500. [CrossRef]
- Richmond, E.; Adams, D.; Dagenais, S.; Clifford, T.; Baydala, L.; King, W.J.; Vohra, S. Complementary and alternative medicine: A survey of its use in children with chronic respiratory illness. Can J Respir Ther 2014, 50, 27-32.
- Kalaci, O.; Giangioppo, S.; Leung, G.; Radhakrishnan, A.; Fleischer, E.; Lyttle, B.; Price, A.; Radhakrishnan, D. Complementary and alternative medicine use in children with asthma. Complement Ther Clin Pract 2019, 35, 272-277. [CrossRef]
- Bishop, F.L.; Lewith, G.T. Who Uses CAM? A Narrative Review of Demographic Characteristics and Health Factors Associated with CAM Use. Evid Based Complement Alternat Med 2010, 7, 11-28. [CrossRef]
- Isaac-Otero G, Molina-Alonso D, Asencio-López L, et al. Uso de la medicina alternativa y complementaria (MAC) en el cáncer infantil: encuesta de 100 casos en un instituto de tercer nivel de atención. Gac Med Mex. 2016;152(1):7-12.
- Smith, C.A.; Collins, C.T.; Levett, K.M.; Armour, M.; Dahlen, H.G.; Tan, A.L.; Mesgarpour, B. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020, 119. [CrossRef]
- National Center for Complementary and Integrative Health (NIH) Complementary, Alternative, or Integrative Health: What’s In a Name? Available online: https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name (accessed on.
- Mollaoglu, M.; Aciyurt, A. Use of complementary and alternative medicine among patients with chronic diseases. Acta Clin Croat 2013, 52, 181-188.
- Lam, C.F.D.; Leung, K.S.; Heng, P.A.; Lim, C.E.D.; Wong, F.W.S. Chinese Acupuncture Expert System (CAES)—A Useful Tool to Practice and Learn Medical Acupuncture. Journal of Medical Systems 2012, 36, 1883-1890. [CrossRef]
- Chen, T.; Zhang, W.W.; Chu, Y.-X.; Wang, Y.-Q. Acupuncture for Pain Management: Molecular Mechanisms of Action. 2020, 48, 793-811. [CrossRef]
- Kawakita, K.; Okada, K. Acupuncture therapy: mechanism of action, efficacy, and safety: a potential intervention for psychogenic disorders? BioPsychoSocial Medicine 2014, 8, 4. [CrossRef]
- Bing, Z.; Villanueva, L.; Le Bars, D. Acupuncture-evoked responses of subnucleus reticularis dorsalis neurons in the rat medulla. Neuroscience 1991, 44, 693-703. [CrossRef]
- Kagitani, F.; Uchida, S.; Hotta, H. Afferent nerve fibers and acupuncture. Auton Neurosci 2010, 157, 2-8. [CrossRef]
- Le Bars, D.; Dickenson, A.H.; Besson, J.-M. Diffuse noxious inhibitory controls (DNIC). I. Effects on dorsal horn convergent neurones in the rat. 1979, 6, 283-304. [CrossRef]
- Chen, T.; Zhang, W.W.; Chu, Y.X.; Wang, Y.Q. Acupuncture for Pain Management: Molecular Mechanisms of Action. Am J Chin Med 2020, 48, 793-811. [CrossRef]
- Mingfu, L.; Xiaotong, D.; Xiaojing, S.; Jin, J.; Jinling, Z.; Ying, H. Study on the Dynamic Compound Structure Composed of Mast Cells, Blood Vessels, and Nerves in Rat Acupoint. Evidence-Based Complementary and Alternative Medicine 2013, 2013, 160651. [CrossRef]
- Lin, J.G.; Kotha, P.; Chen, Y.H. Understandings of acupuncture application and mechanisms. Am J Transl Res 2022, 14, 1469-1481.
- Choi, D.C.; Lee, J.Y.; Lim, E.J.; Baik, H.H.; Oh, T.H.; Yune, T.Y. Inhibition of ROS-induced p38MAPK and ERK activation in microglia by acupuncture relieves neuropathic pain after spinal cord injury in rats. Experimental Neurology 2012, 236, 268-282. [CrossRef]
- Liu, L.; Pei, P.; Zhao, L.-P.; Qu, Z.-Y.; Zhu, Y.-P.; Wang, L.-P. Electroacupuncture Pretreatment at GB20 Exerts Antinociceptive Effects via Peripheral and Central Serotonin Mechanism in Conscious Migraine Rats. Evidence-Based Complementary and Alternative Medicine 2016, 2016, 1846296. [CrossRef]
- Tang, Q.; Jiang, Q.; Sooranna, S.R.; Lin, S.; Feng, Y.; Zhang, Q.; Wang, M.; Wang, Y. Effects of Electroacupuncture on Pain Threshold of Laboring Rats and the Expression of Norepinephrine Transporter and <i>α</i>2 Adrenergic Receptor in the Central Nervous System. Evidence-Based Complementary and Alternative Medicine 2016, 2016, 9068257. [CrossRef]
- Shou, Y.; Yang, Y.; Xu, M.-S.; Zhao, Y.-Q.; Ge, L.-B.; Zhang, B.-M. Electroacupuncture Inhibition of Hyperalgesia in Rats with Adjuvant Arthritis: Involvement of Cannabinoid Receptor 1 and Dopamine Receptor Subtypes in Striatum. Evidence-Based Complementary and Alternative Medicine 2013, 2013, 393460. [CrossRef]
- Tsai, S.-L.; Reynoso, E.; Shin, D.W.; Tsung, J.W. Acupuncture as a Nonpharmacologic Treatment for Pain in a Pediatric Emergency Department. 2021, 37, e360-e366. [CrossRef]
- Lee, A.; Chan, S.K.C.; Fan, L.T.Y. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2015. [CrossRef]
- Gottschling, S.; Meyer, S.; Gribova, I.; Distler, L.; Berrang, J.; Gortner, L.; Graf, N.; Shamdeen, M.G. Laser acupuncture in children with headache: A double-blind, randomized, bicenter, placebo-controlled trial. Pain 2008, 137, 405-412. [CrossRef]
- Halsall, D.; Guideline Dev, G. Diagnosis and management of headaches in young people and adults: summary of NICE guidance (vol 345, e5795, 2012). British Medical Journal 2012, 345. [CrossRef]
- Brittner, M.; Le Pertel, N.; Gold, M.A. Acupuncture in Pediatrics. Current Problems in Pediatric and Adolescent Health Care 2016, 46, 179-183. [CrossRef]
- Adams, D.; Cheng, F.; Jou, H.; Aung, S.; Yasui, Y.; Vohra, S. The safety of pediatric acupuncture: a systematic review. Pediatrics 2011, 128, e1575-1587. [CrossRef]
- Ernst, E.; White, A.R. Prospective studies of the safety of acupuncture: a systematic review. The American Journal of Medicine 2001, 110, 481-485. [CrossRef]
- Yang, C.; Hao, Z.; Zhang, L.-L.; Guo, Q. Efficacy and safety of acupuncture in children: an overview of systematic reviews. Pediatric Research 2015, 78, 112-119. [CrossRef]
- Gao, L.; Jia, C.H.; Huang, H.W. Paediatric massage for treatment of acute diarrhoea in children: a meta-analysis. Bmc Complementary and Alternative Medicine 2018, 18. [CrossRef]
- Taspinar, F.; Aslan, U.B.; Sabir, N.; Cavlak, U. Implementation of matrix rhythm therapy and conventional massage in young females and comparison of their acute effects on circulation. J Altern Complement Med 2013, 19, 826-832. [CrossRef]
- Batalha, L.M.D.; Mota, A. Massage in children with cancer: effectiveness of a protocol. Jornal De Pediatria 2013, 89, 595-600. [CrossRef]
- Nam, M.J.; Bang, Y.I.; Kim, T.I. Effects of Abdominal Meridian Massage with Aroma Oils on Relief of Constipation among Hospitalized Children with Brain related Disabilities. Journal of Korean Academy of Nursing 2013, 43, 247-255. [CrossRef]
- Gonzalez, A.P.; Vasquez-Mendoza, G.; Garcia-Vela, A.; Guzman-Ramirez, A.; Salazar-Torres, M.; Romero-Gutierrez, G. Weight Gain in Preterm Infants following Parent-Administered Vimala Massage: A Randomized Controlled Trial. American Journal of Perinatology 2009, 26, 247-252. [CrossRef]
- Li, X.W.; Zhong, Q.L.; Tang, L.H. A Meta-Analysis of the Efficacy and Safety of Using Oil Massage to Promote Infant Growth. Journal of Pediatric Nursing-Nursing Care of Children & Families 2016, 31, E313-E322. [CrossRef]
- Lu, L.C.; Lan, S.H.; Hsieh, Y.P.; Lin, L.Y.; Chen, J.C.; Lan, S.J. Massage therapy for weight gain in preterm neonates: A systematic review and meta-analysis of randomized controlled trials. Complementary Therapies in Clinical Practice 2020, 39. [CrossRef]
- Mrljak, R.; Arnsteg Danielsson, A.; Hedov, G.; Garmy, P. Effects of Infant Massage: A Systematic Review. 2022, 19, 6378.
- ÖZDEMİR, S.; YILDIZ, S.J.J.o.T.M.C.T. The Effects of Massage on the Weight Gain of Preterm Infants: A Systematic Review. 2019, 2.
- Kumar, J.; Upadhyay, A.; Dwivedi, A.K.; Gothwal, S.; Jaiswal, V.; Aggarwal, S. Effect of Oil Massage on Growth in Preterm Neonates Less than 1800 g: A Randomized Control Trial. Indian Journal of Pediatrics 2013, 80, 465-469. [CrossRef]
- Basiri-Moghadam, M.; Basiri-Moghadam, K.; Kianmehr, M.; Jani, S. The effect of massage on neonatal jaundice in stable preterm newborn infants: a randomized controlled trial. Journal of the Pakistan Medical Association 2015, 65, 602-606.
- Bower, J.E.; Irwin, M.R. Mind–body therapies and control of inflammatory biology: A descriptive review. Brain, Behavior, and Immunity 2016, 51, 1-11. [CrossRef]
- Fogaca, L.Z.; Portella, C.F.S.; Ghelman, R.; Abdala, C.V.M.; Schveitzer, M.C. Mind-Body Therapies From Traditional Chinese Medicine: Evidence Map. Front Public Health 2021, 9, 659075. [CrossRef]
- McClafferty, H.; Sibinga, E.; Bailey, M.; Culbert, T.; Weydert, J.; Brown, M.; Sect Integrative, M. Mind-Body Therapies in Children and Youth. Pediatrics 2016, 138. [CrossRef]
- Nanthakumar, C. The benefits of yoga in children. Journal of Integrative Medicine-Jim 2018, 16, 14-19. [CrossRef]
- Rosen, L.; French, A.; Sullivan, G. Complementary, Holistic, and Integrative Medicine: Yoga. Pediatrics in Review 2015, 36, 468-474. [CrossRef]
- Carei, T.R.; Fyfe-Johnson, A.L.; Breuner, C.C.; Brown, M.A. Randomized controlled clinical trial of yoga in the treatment of eating disorders. J Adolesc Health 2010, 46, 346-351. [CrossRef]
- Narasingharao, K.; Pradhan, B.; Navaneetham, J. Efficacy of Structured Yoga Intervention for Sleep, Gastrointestinal and Behaviour Problems of ASD Children: An Exploratory Study. J Clin Diagn Res 2017, 11, VC01-VC06. [CrossRef]
- Danhauer, S.C.; Addington, E.L.; Sohl, S.J.; Chaoul, A.; Cohen, L. Review of yoga therapy during cancer treatment. Support Care Cancer 2017, 25, 1357-1372. [CrossRef]
- Khunti, K.; Boniface, S.; Norris, E.; De Oliveira, C.M.; Nicola, S. The effects of yoga on mental health in school-aged children: A Systematic Review and Narrative Synthesis of Randomised Control Trials. Clin Child Psychol Psychiatry 2023, 28, 1217-1238. [CrossRef]
- James-Palmer, A.; Anderson, E.Z.; Zucker, L.; Kofman, Y.; Daneault, J.F. Yoga as an Intervention for the Reduction of Symptoms of Anxiety and Depression in Children and Adolescents: A Systematic Review. Front Pediatr 2020, 8, 78. [CrossRef]
- Cramer, H.; Ward, L.; Saper, R.; Fishbein, D.; Dobos, G.; Lauche, R. The Safety of Yoga: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. American Journal of Epidemiology 2015, 182, 281-293. [CrossRef]
- Roberta Crevelário de, M.; Aline Ângela Victoria, R.; Cézar, D.L., Jr.; Maritsa Carla de, B.; Tereza Setsuko, T.; Jorge Otávio Maia, B. Effectiveness and safety of yoga to treat chronic and acute pain: a rapid review of systematic reviews. BMJ Open 2021, 11, e048536. [CrossRef]
- Simkin, D.R.; Hudziak, J.J.; Pradhan, B. MEDITATION/MINDFULNESS: USE IN CLINICAL PRACTICE. Journal of the American Academy of Child and Adolescent Psychiatry 2017, 56, S128-S128. [CrossRef]
- Black, L.I.; Barnes, P.M.; Clarke, T.C.; Stussman, B.J.; Nahin, R.L. Use of Yoga, Meditation, and Chiropractors Among U.S. Children Aged 4-17 Years. NCHS data brief 2018, 1-8.
- Sibinga, E.M.S.; Kemper, K.J. Complementary, Holistic, and Integrative Medicine: Meditation Practices for Pediatric Health. Pediatrics in Review 2010, 31, E91-E103. [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Jenkins, Z.M.; Ski, C.F. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. Journal of Psychiatric Research 2017, 95, 156-178. [CrossRef]
- Crescentini, C.; Capurso, V.; Furlan, S.; Fabbro, F. Mindfulness-Oriented Meditation for Primary School Children: Effects on Attention and Psychological Well-Being. Frontiers in Psychology 2016, 7. [CrossRef]
- Lee, Y.-C.; Chen, C.-R.; Lin, K.-C. Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. 2022, 19, 15198.
- Li, J.X.; Hong, Y.; Chan, K.M. Tai chi: physiological characteristics and beneficial effects on health. British Journal of Sports Medicine 2001, 35, 148. [CrossRef]
- Jahnke, R.; Larkey, L.; Rogers, C.; Etnier, J.; Lin, F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot 2010, 24, e1-e25. [CrossRef]
- Liao, P.-C.; Lin, H.-H.; Chiang, B.-L.; Lee, J.-H.; Yu, H.-H.; Lin, Y.-T.; Yang, Y.-H.; Li, P.-Y.; Wang, L.-C.; Sun, W.-Z. Tai Chi Chuan Exercise Improves Lung Function and Asthma Control through Immune Regulation in Childhood Asthma. Evidence-Based Complementary and Alternative Medicine 2019, 2019, 9146827. [CrossRef]
- Tabeshian, R.; Nezakat-Alhosseini, M.; Movahedi, A.; Zehr, E.P.; Faramarzi, S. The Effect of Tai Chi Chuan Training on Stereotypic Behavior of Children with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders 2022, 52, 2180-2186. [CrossRef]
- Yao, Y.; Ge, L.; Yu, Q.; Du, X.; Zhang, X.; Taylor-Piliae, R.; Wei, G.-X. The Effect of Tai Chi Chuan on Emotional Health: Potential Mechanisms and Prefrontal Cortex Hypothesis. Evidence-Based Complementary and Alternative Medicine 2021, 2021, 5549006. [CrossRef]
- Riskowski, J.L.; Almeheyawi, R. Effects of Tai Chi and Qigong in Children and Adolescents: A Systematic Review of Trials. Adolescent Research Review 2019, 4, 73-91. [CrossRef]
- Fong, S.S.M.; Chung, L.M.Y.; Schooling, C.M.; Lau, E.H.Y.; Wong, J.Y.H.; Bae, Y.-H.; Chung, J.W.Y. Tai chi-muscle power training for children with developmental coordination disorder: a randomized controlled trial. Scientific Reports 2022, 12, 22078. [CrossRef]
- Cheng, D.; Wang, B.; Li, Q.; Guo, Y.; Wang, L. Research on Function and Mechanism of Tai Chi on Cardiac Rehabilitation. Chinese Journal of Integrative Medicine 2020, 26, 393-400. [CrossRef]
- Rosado-Pérez, J.; Castelán-Martínez, O.D.; Mújica-Calderón, A.J.; Sánchez-Rodríguez, M.A.; Mendoza-Núñez, V.M. Effect of Tai Chi on Markers of Oxidative Stress: Systematic Review and Meta-Analysis. 2021, 18, 3458.
- Liang, H.; Luo, S.; Chen, X.; Lu, Y.; Liu, Z.; Wei, L. Effects of Tai Chi exercise on cardiovascular disease risk factors and quality of life in adults with essential hypertension: A meta-analysis. Heart Lung 2020, 49, 353-363. [CrossRef]
- Cetin, S.Y.; Erel, S.; Bas Aslan, U. The effect of Tai Chi on balance and functional mobility in children with congenital sensorineural hearing loss. Disability and Rehabilitation 2020, 42, 1736-1743. [CrossRef]
- Kong, Z.; Sze, T.-M.; Yu, J.J.; Loprinzi, P.D.; Xiao, T.; Yeung, A.S.; Li, C.; Zhang, H.; Zou, L. Tai Chi as an Alternative Exercise to Improve Physical Fitness for Children and Adolescents with Intellectual Disability. 2019, 16, 1152.
- Li, F.S.; Weng, J.K. Demystifying traditional herbal medicine with modern approaches. Nature Plants 2017, 3. [CrossRef]
- Licata, A.; Macaluso, F.S.; Craxi, A. Herbal hepatotoxicity: a hidden epidemic. Internal and Emergency Medicine 2013, 8, 13-22. [CrossRef]
- Marquardt, P.; Kaft, K.; Nieber, K. Clinical trials with herbal medicinal products in children: a literature analysis. Wiener Medizinische Wochenschrift 2015, 165, 236-242. [CrossRef]
- Clarke, T.C.; Black, L.I.; Stussman, B.J.; Barnes, P.M.; Nahin, R.L. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report 2015, 1-16.
- Ghorani-Azam, A.; Sepahi, S.; Riahi-Zanjani, B.; Ghamsari, A.A.; Mohajeri, S.A.; Balali-Mood, M. Plant toxins and acute medicinal plant poisoning in children: A systematic literature review. Journal of Research in Medical Sciences 2018, 23. [CrossRef]
- Bent, S. Herbal Medicine in the United States: Review of Efficacy, Safety, and Regulation. Journal of General Internal Medicine 2008, 23, 854-859. [CrossRef]
- Awang, D.V.C. Quality Control and Good Manufacturing Practices: Safety and Efficacy of Commercial Herbals. Food and Drug Law Journal 1997, 52, 341-344.
- Al-Worafi, Y.M. Chapter 14 - Herbal medicines safety issues. In Drug Safety in Developing Countries, Al-Worafi, Y., Ed.; Academic Press: 2020; pp. 163-178.
- Efferth, T.; Kaina, B. Toxicities by Herbal Medicines with Emphasis to Traditional Chinese Medicine. Current Drug Metabolism 2011, 12, 989-996.
- Shetti, S.; Kumar, C.D.; Sriwastava, N.K.; Sharma, I.P. Pharmacovigilance of herbal medicines: Current state and future directions. Pharmacogn Mag 2011, 7, 69-73. [CrossRef]
- Du, Y.; Wolf, I.-K.; Zhuang, W.; Bodemann, S.; Knoess, W.; Knopf, H. Use of herbal medicinal products among children and adolescents in Germany. Bmc Complementary and Alternative Medicine 2014, 14. [CrossRef]
- Smolinske, S.C. Dietary Supplements in Children. Pediatric Clinics of North America 2017, 64, 1243-1255. [CrossRef]
- Shakibaei, F.; Radmanesh, M.; Salari, E.; Mahaki, B. Ginkgo biloba in the treatment of attention-deficit/hyperactivity disorder in children and adolescents. A randomized, placebo-controlled, trial. Complementary Therapies in Clinical Practice 2015, 21, 61-67. [CrossRef]
- Razlog, R.; Pellow, J.; White, S.J. A pilot study on the efficacy of <i>Valeriana officinalis</i> mother tincture and <i>Valeriana officinalis</i> 3X in the treatment of attention deficit hyperactivity disorder : original research. 2011, 17, 1-7. [CrossRef]
- Dutta, T.; Anand, U.; Mitra, S.S.; Ghorai, M.; Jha, N.K.; Shaikh, N.K.; Shekhawat, M.S.; Pandey, D.K.; Prockow, J.; Dey, A. Phytotherapy for Attention Deficit Hyperactivity Disorder (ADHD): A Systematic Review and Meta-analysis. Front Pharmacol 2022, 13, 827411. [CrossRef]
- Golsorkhi, H.; Qorbani, M.; Sabbaghzadegan, S.; Dadmehr, M. Herbal medicines in the treatment of children and adolescents with attention-deficit/hyperactivity disorder (ADHD): An updated systematic review of clinical trials. Avicenna J Phytomed 2023, 13, 338-353. [CrossRef]
- Catala-Lopez, F.; Hutton, B.; Nunez-Beltran, A.; Page, M.J.; Ridao, M.; Macias Saint-Gerons, D.; Catala, M.A.; Tabares-Seisdedos, R.; Moher, D. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PLoS One 2017, 12, e0180355. [CrossRef]
- Anheyer, D.; Lauche, R.; Schumann, D.; Dobos, G.; Cramer, H. Herbal medicines in children with attention deficit hyperactivity disorder (ADHD): A systematic review. Complement Ther Med 2017, 30, 14-23. [CrossRef]
- Thapa, S.; Luna, R.A.; Chumpitazi, B.P.; Oezguen, N.; Abdel-Rahman, S.M.; Garg, U.; Musaad, S.; Versalovic, J.; Kearns, G.L.; Shulman, R.J. Peppermint oil effects on the gut microbiome in children with functional abdominal pain. 2022, 15, 1036-1049. [CrossRef]
- Nocerino, R.; Cecere, G.; Micillo, M.; De Marco, G.; Ferri, P.; Russo, M.; Bedogni, G.; Berni Canani, R. Efficacy of ginger as antiemetic in children with acute gastroenteritis: a randomised controlled trial. Aliment Pharmacol Ther 2021, 54, 24-31. [CrossRef]
- Shulman, R.J.; Chumpitazi, B.P.; Abdel-Rahman, S.M.; Garg, U.; Musaad, S.; Kearns, G.L. Randomised trial: Peppermint oil (menthol) pharmacokinetics in children and effects on gut motility in children with functional abdominal pain. Br J Clin Pharmacol 2022, 88, 1321-1333. [CrossRef]
- Chumpitazi, B.P.; Kearns, G.L.; Shulman, R.J. Review article: the physiological effects and safety of peppermint oil and its efficacy in irritable bowel syndrome and other functional disorders. 2018, 47, 738-752. [CrossRef]
- Kline, R.M.; Kline, J.J.; Di Palma, J.; Barbero, G.J. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr 2001, 138, 125-128. [CrossRef]
- Su, G.; Chen, X.; Liu, Z.; Yang, L.; Zhang, L.; Stålsby Lundborg, C.; Wen, Z.; Guo, X.; Qin, X.; Liang, J.; et al. Oral Astragalus (Huang qi) for preventing frequent episodes of acute respiratory tract infection in children. Cochrane Database Syst Rev. 2016. [CrossRef]
- Ogal, M.; Johnston, S.L.; Klein, P.; Schoop, R. Echinacea reduces antibiotic usage in children through respiratory tract infection prevention: a randomized, blinded, controlled clinical trial. Eur J Med Res 2021, 26, 33. [CrossRef]
- Nicolussi, S.; Ardjomand-Woelkart, K.; Stange, R.; Gancitano, G.; Klein, P.; Ogal, M. Echinacea as a Potential Force against Coronavirus Infections? A Mini-Review of Randomized Controlled Trials in Adults and Children. 2022, 10, 211.
- Wang, W.; Jing, W.; Liu, Q. Astragalus Oral Solution Ameliorates Allergic Asthma in Children by Regulating Relative Contents of CD4(+)CD25(high)CD127(low) Treg Cells. Front Pediatr 2018, 6, 255. [CrossRef]
- Ernst, E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John's Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 2002, 136, 42-53. [CrossRef]
- Bat, N. The effects of reiki on heart rate, blood pressure, body temperature, and stress levels: A pilot randomized, double-blinded, and placebo-controlled study. Complementary Therapies in Clinical Practice 2021, 43, 101328. [CrossRef]
- Zadro, S.; Stapleton, P. Does Reiki Benefit Mental Health Symptoms Above Placebo? Front Psychol 2022, 13, 897312. [CrossRef]
- Billot, M.; Daycard, M.; Wood, C.; Tchalla, A. Reiki therapy for pain, anxiety and quality of life. 2019, 9, 434-438. [CrossRef]
- McManus, D.E. Reiki Is Better Than Placebo and Has Broad Potential as a Complementary Health Therapy. J Evid Based Complementary Altern Med 2017, 22, 1051-1057. [CrossRef]
- Reiki Improves Heart Rate Homeostasis in Laboratory Rats. 2008, 14, 417-422. [CrossRef]
- Catlin, A.; Taylor-Ford, R.L. Investigation of standard care versus sham Reiki placebo versus actual Reiki therapy to enhance comfort and well-being in a chemotherapy infusion center. Oncol Nurs Forum 2011, 38, E212-220. [CrossRef]
- Alarcão, Z.; Fonseca, J.R.S. The effect of Reiki therapy on quality of life of patients with blood cancer: Results from a randomized controlled trial. European Journal of Integrative Medicine 2016, 8, 239-249. [CrossRef]
- Lopes-Junior, L.C.; Urbano, I.R.; Schuab, S.; Pessanha, R.M.; Rosa, G.S.; Lima, R.A.G. Effectiveness of complementary therapies for the management of symptom clusters in palliative care in pediatric oncology: a systematic review. Rev Esc Enferm USP 2021, 55, 03709. [CrossRef]
- Konuk, D. Use of Traditional and Complementary Medicine Methods in Children: Is It Effective and Safe? 2022, 19, 456-465. [CrossRef]
- Morero, J.A.P.; Pereira, S.d.S.; Esteves, R.B.; Cardoso, L. Effects of Reiki on Mental Health Care: A Systematic Review. 2021, 35, 191-198. [CrossRef]
- Zucchetti, G.; Candela, F.; Bottigelli, C.; Campione, G.; Parrinello, A.; Piu, P.; Vassallo, E.; Fagioli, F. The Power of Reiki: Feasibility and Efficacy of Reducing Pain in Children With Cancer Undergoing Hematopoietic Stem Cell Transplantation. J Pediatr Oncol Nurs 2019, 36, 361-368. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).