1. Introduction
Currently, according to the World Health Organization (WHO), 2.2 billion people in the world suffer from some visual impairment, of these, 1 billion are preventable or treatable causes [
1]. Glaucoma, age-related macular degeneration (AMD), and diabetic retinopathy are among the major causes of blindness. All of these can have their morbidity reduced with early detection through retinography and/or retinal mapping, thus permitting appropriate intervention [
2].
The estimate of blindness in Brazil is 1.559 million people, and the main causes are in accordance with WHO’s declaration: cataracts, glaucoma, AMD, and diabetic retinopathy [
3]. Brazil has as unbalanced geographical distribution of ophthalmologists, the predominance of the specialty in concentrated in Southeast and there is a huge deficit in the Northern region, particularly in communities outside the state capital [
3].
Conventional instruments for fundus evaluation (e.g.: indirect ophthalmoscope and slit lamp) are difficult to handle, require extensive prior training and are examiner dependent, not allowing, in most cases, photographic recording of the retina. With traditional fundus cameras it is possible to take wide field high resolution pictures of the retina – imaging with an angular field of view over 50 degrees [
4] –, allowing different examiners evaluation and fundus record for follow up, however they have elevated acquisition cost and logistical problems for transportation [
5]. Capturing retinal images is important in ophthalmic practice, since it permits to evaluate more details of the retina, to monitor diseases progression, to apply analysis software and artificial intelligence, and it also plays a key role in the training of new doctors [
5,
6].
Nowadays, different smartphone-based devices make it possible to easily capture high quality images of the retina. These devices are light, small, less examiner depend, and, although still expensive, are much more affordable than the traditional fundus cameras [
6]. Moreover, most do not require mydriasis, shortening the examination time and avoiding adverse effects, such as visual discomfort, photophobia, keratitis, and increased intraocular pressure [
7]. With the advent of telemedicine and cloud-based data records, images are automatically sent to an online network, a secure database with access restricted to those involved in the exam and the responsible doctor, enabling a specialized ophthalmologist to analyze them from anywhere in the world, bringing the patient a more reliable diagnosis and supporting local physicians to choose the most appropriate and up to date management [
8].
Regarding the reality of telemedicine in Brazil, it is known that its introduction in the country is recent and it was only regulated during the COVID-19 pandemic in 2020 [
9]. Its dissemination throughout the country faces several obstacles, such as structural barriers – lack of access to internet and digital technologies – and techniques – few people have the necessary knowledge to effectively insert telemedicine into daily care [
10]. This difference is even more important when we consider teleophthalmology, since this is one of the areas of telemedicine that most needs high technology density [
11].
In wealthy regions these interfaces are not major obstacles since there is enough investment to purchase modern devices and access to specialized professionals [
5]. However, even in high income countries, millions of people live in low-income areas without access to ophthalmologists and technology, hence are left unattended and develop various blinding conditions. Added to the lack of access, these patients are also unaware of the need for early detection and treatment to improve life quality [
12]. New smartphone-based fundus camera and telemedicine, combined, show a promising opportunity for accessing ocular health inequalities in vulnerable populations. Thus, this study had the objective to evaluate the retina of a semi-isolated river side community in the Amazon Forest, to investigate the prevalence of retinal findings, and to propose strategies to enhance ocular health through telemedicine in unaided populations.
2. Materials and Methods
A cross sectional study was conducted in the community of Calama – Rondônia, Brazil, which is a 2,000 people riverside community in the Amazon Forest located around 15 hours by boat away from the closest ophthalmology service. The STROBE reporting guideline was followed [
13]. The study was performed in accordance with the ethical standards of The Declaration of Helsinki and approved in the Local Research Ethics Committee (number 5.325.976), informed consent was verbal. Participants included adults randomly selected in home visits or at the local general care clinic during January-February 2022; to avoid bias, it was excluded from the sample patients under 18 years old, with anterior segment opacities, and who looked for the clinics with known eye diseases. In siting position, two retinal photos were captured from each eye: i) posterior pole, and ii) optic disc. After photo acquisition, participants were questioned about age, sex, and self-reported comorbidities, no ethnic information was collected during the study. All photos and data were automatically sent to an online encrypted data base (EyerCloud, Phelcom Thecnologies
®, SP-Brazil).
Photos were captured by four previously trained 5th year medical students using a portable non-mydriatic smartphone-based fundus camera (Eyer, Phelcom Thecnologies®, SP-Brazil). Interns were trained in a four-hour lection including theoretical aspects (e.g.: physics of the device, ophthalmological basic anamneses and exam, and retinal pathology) and practical activity in a simulation-based scenario.
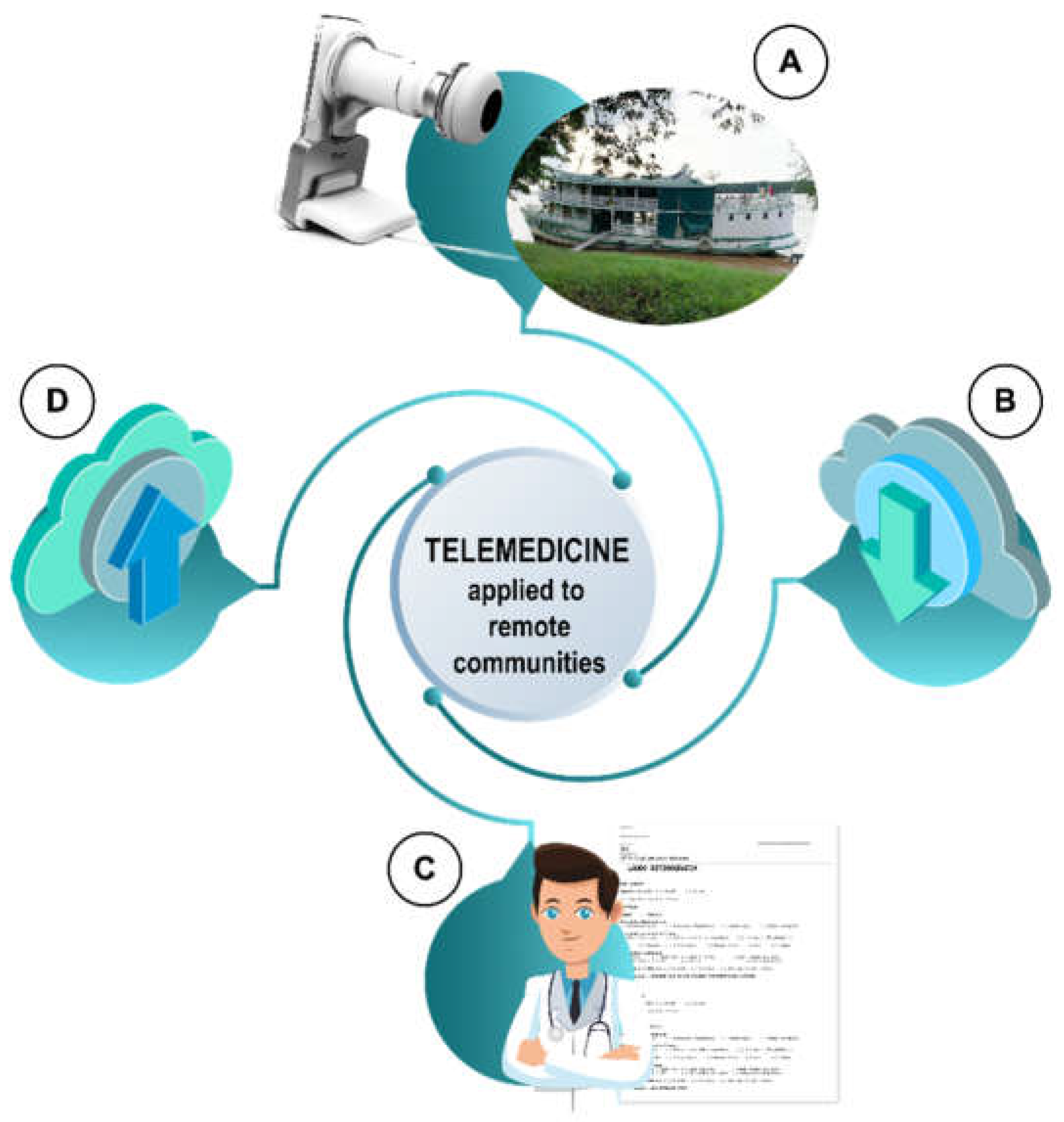
A single retina specialist located more than 3,000km away received all data remotely, checked all exams for retinal alterations, and, through the data base, sent back the signed results. All participants were properly referred or oriented according to the final diagnosis given through telemedicine (
Figure 1). Transportation of all referred patients was guaranteed by the local health secretary.
Epithelial changes were considered as areas of altered hyper or hypo pigmentation in the epithelium without visual alteration or known cause. Chorioretinal scars were considered as areas of pigmentary change or fibrosis resulting from an uncomplete healing of the retina, showing a possible participation of the retinal pigmented epithelium (RPE) in process that affect the retina and choroid. Dry AMD was considered the presence of drusen in the macula without neovascularization. Enlarged optic discs were considered disc relation > 0.50. Hypertensive retinopathy was considered as widening of the arteriole reflex, arteriovenous crossing signs, and copper or silver wire arterioles (copper or silver colored arteriole light reflex), or constricted and tortuous arterioles, retinal hemorrhage, or hard exudates in patients with known history of arterial hypertension. Non proliferative diabetic retinopathy was considered as the presence of microaneurysms, dot-blot hemorrhages, cotton wool spots and hard exudates without neovascularization in patients with known diabetes.
Statistical analyses were performed using IBM SPSS® 28.0.1 (IBM, Inc, Chicago, IL-USA). Continuous variables were compared between groups with Mann–Whitney U test for non-parametric independent samples, and nominal variables were compared with Chi-squared test. Proportion 95% Confidence Intervals (CI) were calculated considering a=0.05 and binomial distributions.
3. Results
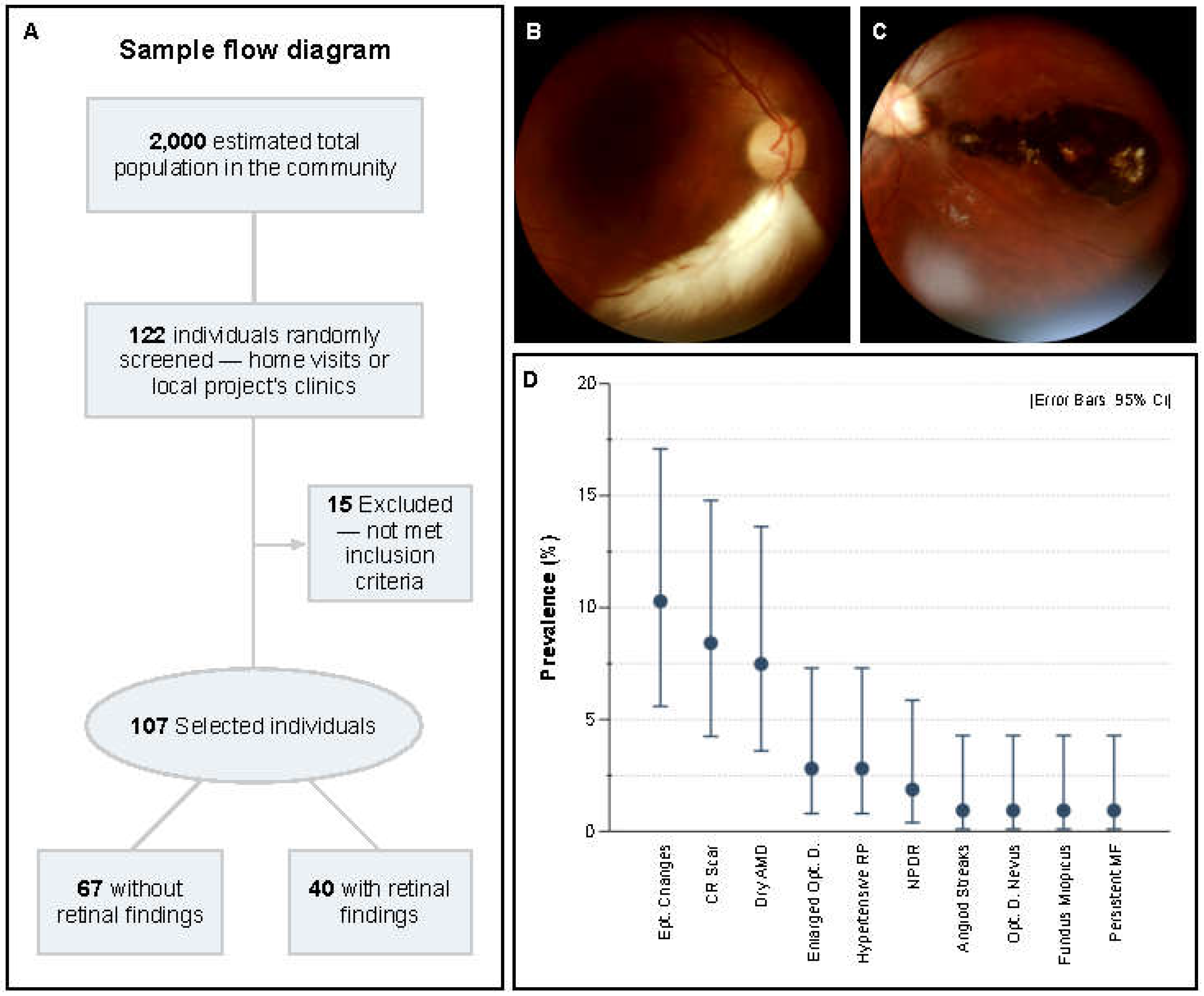
During the study, 122 individuals were screened for retinal alterations, 15 were excluded for not meeting including criteria (
Figure 2A). Final sample was composed by 107 participants, aged mean 52±17.7 years (range 18 to 88), and 57.9% female. Comorbidities were found in 46.7% of the sample and were systemic arterial hypertension (SAH), Type 2 Diabetes Mellitus (DM2), and dyslipidemia, 22.4% had more than one comorbidity associated. Patient’s demographics are shown in
Table 1, altered retina were considered patients with a retinal alteration in fundus photography in at least one eye.
Most of the population did not have any identifiable retinal alterations, 62.6%, CI [53.2, 71.3], however findings were detected in 37.4%, CI [28.7, 46.8], of the sample. A large set of alterations were identified, ranging from non-visual threatening to severe blindness (e.g., inferior temporal persistent myeline fibers vs. large macular chorioretinal scar;
Figure 2B-C). Interestingly, the three main retinal findings were epithelial changes (10.3%, CI [5.6, 17.1]), chorioretinal scars (8.4%, CI [4.2, 14.8]), and dry Age-related Macular Degeneration (dAMD; 7.5%, CI [3.6, 13.6]). In lower rates, enlarged optic disc (2.8%, CI [0.8, 7.3]), hypertensive retinopathy (2.8%, CI [0.8, 7.3]), and non-proliferative diabetes retinopathy (NPDR; 1.9%, CI [0.4, 5.9]) were also identified. Other alterations appeared only once, 0.9%, CI [0.1, 4.3]—angioid streaks, fundus miopicus, optic disc nevus, and persistent myeline fibers (
Figure 2D). All patients that showed NPDR had confirmed Type 2 Diabetes Mellitus (DM2), the prevalence of NPDR among DM2 participants was 8.0%, CI [1.7, 23.3]. Other ophthalmological findings that were not in the retina (e.g., refractive errors, pterygium, cataract, etc) were not considered in the study.
Among the sample, participants with retinal alterations were significantly older (p<0.001), however, as expected, when adjusted by age and in pairwise comparison with retinal findings, only dAMD had statistical significance (p<0.001), other findings had no correlation with age (p>0.05). SAH was the only comorbidity that showed higher prevalence among participants with retinal findings (52.5%; CI 37.3, 67.3, p=0.008). Sex, DM2, dyslipidemia and smoking showed no impact on the findings (p>0,05).
4. Discussion
Through telemedicine and a smartphone-based device, our study detected retinal alterations in 37.4% of the population in a remote riverside community at the Amazon Forest, a prevalence which is among the average of other underresourced areas [
14]. The most prevalent retinal finding was epithelial changes (10.3%), which is a non-specific sign that could be related to a variety of diseases, e.g., light toxicity, macular dystrophies, and early stage pachychorid [
15,
16,
17] etiologies probably related to community’s social conditions, such as intense sun exposition and high rates of consanguinity. However, complementary exams are necessary to clearly state the management of the findings—OCT, blood testing, genetic panels, etc.; in this study, the only available tool was a portable fundus camera.
Interestingly, the prevalence of chorioretinal scars was 8.4%, similar to other studies, which showed a prevalence of 1.0% to 17.7%, depending on the design and characteristics of the population [
18,
19]. It is known that ocular toxoplasmosis is one of the most frequent causes of posterior uveitis worldwide, and it is the leading cause of childhood blindness in Brazil, since, when not treated, it may leave typical chorioretinal scars [
20]. Toxoplasma gondii, the parasite associated with the zoonosis, is endemic in the region, and its main source of dissemination is contaminated water, undercooked meat, and vertically during pregnancy—risk factors which the population of this study is largely exposed [
21]. This finding highlights the necessity of intensive measures to early detect contaminated pregnant women, to increase access to treated water, and to intensify public policies aiming prophylaxis.
The riverside community of Calama is in a remote region of the Brazilian Amazon Forest, which the only way to reach it is by boat through The Madeira River. As in other isolated communities, it is marked by difficult displacement caused by territorial dimension, lack of transport system, and low concentration of health professionals [
22,
23]. This study shows that telemedicine, local support with distant specialists, is a huge opportunity to address health inequities, especially in ophthalmology, which is a medical field that demands long term trained professionals and high-cost equipment.
The recognition of risk factors for non-preventable diseases are conducted by general doctors in the primary health care scenario, which are, in most of the places, represented by recently graduated physicians. However, studies showed that those doctors manifest a huge deficit in ophthalmology knowledge during medical school and insecurity to initially assist and/or refer ophthalmological cases, compromising the proper approach of the patients [
24,
25,
26]. This problem is possibly correlated to the exclusion of ocular health as a mandatory subject in the Brazilian medical curriculum, and less than half have the option of undertaking an elective clerkship in ophthalmology, increasingly distancing the specialty from the reality of the general practitioner [
27,
28]. Easy handling devices, artificial intelligence, and telemedicine can support medical education, and bring back clinicians’ security for initially managing and referring patients with risk factors for blinding ocular condition. Extracurricular activities are also an important opportunity to support medical education and encourage knowledge developed outside the university walls, a fact highlighted by the exponential growth of The Brazilian Association of Ophthalmology Academic Leagues (ABLAO), an association that develops multicenter extension, research, and teaching activities, bringing together students interested in ophthalmology and providing opportunities for social impact and improvement of medical education [
27].
5. Conclusions
In this study, we showed that, through relatively low-cost and portable devices, distant high specialized professionals can guarantee and support effective clinical decisions in remote areas with low health access. However, it is possible to conclude that maintaining assistance after initial implementation is still a challenge, since the visit of trained health professionals is periodic, and some conditions demand frequent follow-up. We suggest enhancing medical education in the recognition of ocular pathologies, training local non-specialized health professionals for risk assessment, device handling, and data base use to ensure early diagnosis and follow-up after project implementation. Apart from that, we also suggest the development of new research aiming unexplored portable devices (e.g., OCT, visual field) and larger investigations with a broader spectrum of exams to support public policies in blindness prevention.
Author Contributions
Conceptualization, J.S., L.E.S., J.V.M.L., L.R.S., I.U.N., C.P.C., A.C.F.A., A.M., E.L.D. and L.F.M.L.; methodology, J.S. and L.E.S.; software, L.E.S.; validation, A.M., E.L.D. and L.F.M.L.; formal analysis, J.S. and L.F.M.L.; investigation, J.S., L.E.S., J.V.M.L., L.R.S., I.U.N., C.P.C. and A.C.F.A.; resources, J.S., L.E.S., A.M., E.L.D. and L.F.M.L.; data curation, J.S. and L.E.S.; writing—original draft preparation, J.S., L.E.S., J.V.M.L., L.R.S., I.U.N., C.P.C. and A.C.F.A.,; writing—review and editing, J.S., A.M., E.L.D. and L.F.M.L.; visualization, J.S., L.E.S., E.L.D. and L.F.M.L.; supervision, A.M., E.L.D. and L.F.M.L.; project administration, E.L.D. and L.F.M.L.; funding acquisition, J.S., L.E.S, A.M., E.L.D. and L.F.M.L. All authors have read and agreed to the published version of the manuscript.
Funding
this study was funded by the Cultural and Extension Dean’s Office of the University of São Paulo. LES and LRS are supported by São Paulo Research Foundation (respectively, grants number 2020/0365-8 and 2021/09023-0).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Hospital de Reabilitação de Anomalias Craniofaciaias da Universidade de São Paulo – HRAC USP protocol code 5.325.976 from 1st of April 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Direct information and requests for resources or data to Josmar Sabage (josmar.sabage@usp.br).
Acknowledgments
We would like to acknowledge Letícia Leite, Magali Caldana and José R. M. Basto, coordinators of the project “Bauru School of Dentistry - Rondônia”, all members of the expedition, and Luiz F. F. Silva for the material, logistic and administrative support; Marisa Romangnolli for the technical and design support; the Cultural and Extension Dean’s Office of the University of São Paulo for the financial and administrative support; and Phelcom Technologies for the material and technical support.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M. V; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global Causes of Blindness and Distance Vision Impairment 1990-2020: A Systematic Review and Meta-Analysis. Lancet Glob Health 2017, 5, e1221–e1234. [CrossRef]
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study Causes of Blindness and Vision Impairment in 2020 and Trends over 30 Years, and Prevalence of Avoidable Blindness in Relation to VISION 2020: The Right to Sight: An Analysis for the Global Burden of Disease Study. Lancet Glob Health 2021, 9, e144–e160. [CrossRef]
- Umbelino, C.C.; Avlia, M. As Condições de Saúde Ocular No Brasil; Umbelino, C.C., Avlia, M., Eds.; 1st ed.; Conselho Brasileiro de Oftalmologia: São Paulo, 2023;
- Lucente, A.; Taloni, A.; Scorcia, V.; Giannaccare, G. Widefield and Ultra-Widefield Retinal Imaging: A Geometrical Analysis. Life 2023, 13, 202. [CrossRef]
- Garg, S.J. Applicability of Smartphone-Based Screening Programs. JAMA Ophthalmol 2016, 134, 158–159. [CrossRef]
- Wintergerst, M.W.M.; Jansen, L.G.; Holz, F.G.; Finger, R.P. A Novel Device for Smartphone-Based Fundus Imaging and Documentation in Clinical Practice: Comparative Image Analysis Study. JMIR Mhealth Uhealth 2020, 8, e17480. [CrossRef]
- Hong, D.; Tripathy, K. Tropicamide. 2023 Aug 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. PMID: 31082113.
- Jin, K.; Lu, H.; Su, Z.; Cheng, C.; Ye, J.; Qian, D. Telemedicine Screening of Retinal Diseases with a Handheld Portable Non-Mydriatic Fundus Camera. BMC Ophthalmol 2017, 17, 89. [CrossRef]
- Lisboa, K.O.; Hajjar, A.C.; Sarmento, I.P.; Sarmento, R.P.; Gonçalves, S.H.R. A História Da Telemedicina No Brasil: Desafios e Vantagens. Saúde e Sociedade 2023, 32. [CrossRef]
- Nakayama, L.F.; Binotti, W.W.; Link Woite, N.; Fernandes, C.O.; Alfonso, P.G.; Celi, L.A.; Regatieri, C.V. The Digital Divide in Brazil and Barriers to Telehealth and Equal Digital Health Care: Analysis of Internet Access Using Publicly Available Data. J Med Internet Res 2023, 25, e42483. [CrossRef]
- Grisolia, A.B.D.; Abalem, M.F.; Lu, Y.; Aoki, L.; Matayoshi, S. Teleophthalmology: Where Are We Now? Arq Bras Oftalmol 2017, 80. [CrossRef]
- Lodhia, V.; Karanja, S.; Lees, S.; Bastawrous, A. Acceptability, Usability, and Views on Deployment of Peek, a Mobile Phone MHealth Intervention for Eye Care in Kenya: Qualitative Study. JMIR Mhealth Uhealth 2016, 4, e30. [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. The Lancet 2007, 370, 1453–1457. [CrossRef]
- Jacobsen, B.H.; Shah, A.A.; Aggarwal, S.; Mwanansao, C.; McFadden, M.; Zouache, M.A.; Shakoor, A. Prevalence of Retinal Diseases and Associated Risk Factors in an African Population From Mwanza, Tanzania. Ophthalmic Surg Lasers Imaging Retina 2020, 51, S17–S25. [CrossRef]
- Youssef, P.N.; Sheibani, N.; Albert, D.M. Retinal Light Toxicity. Eye 2011, 25, 1–14. [CrossRef]
- Warrow, D.J.; Hoang, Q. v; Freund, K.B. Pachychoroid Pigment Epitheliopathy. Retina 2013, 33, 1659–1672. [CrossRef]
- Halford, S.; Liew, G.; Mackay, D.S.; Sergouniotis, P.I.; Holt, R.; Broadgate, S.; Volpi, E. v.; Ocaka, L.; Robson, A.G.; Holder, G.E.; et al. Detailed Phenotypic and Genotypic Characterization of Bietti Crystalline Dystrophy. Ophthalmology 2014, 121, 1174–1184. [CrossRef]
- de Amorim Garcia, C.A.; Oréfice, F.; de Oliveira Lyra, C.; Gomes, A.B.; França, M.; de Amorim Garcia Filho, C.A. Socioeconomic Conditions as Determining Factors in the Prevalence of Systemic and Ocular Toxoplasmosis in Northeastern Brazil. Ophthalmic Epidemiol 2004, 11, 301–317. [CrossRef]
- Glasner, P.D.; Silveira, C.; Kruszon-Moran, D.; Martins, M.C.; Burnier, M.; Silveira, S.; Camargo, M.E.; Nussenblatt, R.B.; Kaslow, R.A.; Belfort, R. An Unusually High Prevalence of Ocular Toxoplasmosis in Southern Brazil. Am J Ophthalmol 1992, 114, 136–144. [CrossRef]
- de Angelis, R.E.; Veronese Rodrigues, M. de L.; Passos, A.D.C.; Bollela, V.R.; Freitas E Silva, M.S.; Vieira, B.R.; de Lucena, M.M.; Moralles, T.D.; de Morais Vicente, L.; de Melo Rocha, G.; et al. Frequency and Visual Outcomes of Ocular Toxoplasmosis in an Adult Brazilian Population. Sci Rep 2021, 11, 3420. [CrossRef]
- Strang, A.G.G.F.; Ferrari, R.G.; do Rosário, D.K.; Nishi, L.; Evangelista, F.F.; Santana, P.L.; de Souza, A.H.; Mantelo, F.M.; Guilherme, A.L.F. The Congenital Toxoplasmosis Burden in Brazil: Systematic Review and Meta-Analysis. Acta Trop 2020, 211, 105608. [CrossRef]
- Franco, E.C.; Santo, C. do E.; Arakawa, A.M.; Xavier, A.; França, M. de L.; Oliveira, A.N. de; Machado, M.A.M. de P.; Bastos, R. da S.; Bastos, J.R. de M.; Caldana, M. de L. Promoção Da Saúde Da População Ribeirinha Da Região Amazônica: Relato de Experiência. Revista CEFAC 2015, 17, 1521–1530. [CrossRef]
- Leite, L. de A. Levantamento Dos Fatores de Risco Para o Acidente Vascular Cerebral Em Sujeitos Adultos de Diferentes Regiões Do Estado de Rondônia, Assistidos Pelo Projeto \"FOB-USP Em Rondônia\", Universidade de São Paulo: Bauru, 2022.
- Espíndola, R.F. de; Teixeira, F.C.; Yamakami, I.M.; Silva, H.R.F. da; Freitas, J.A.H. de Análise Dos Conhecimentos Básicos Sobre Urgências Oftalmológicas Em Plantonistas Não-Oftalmologistas. Arq Bras Oftalmol 2006, 69, 11–15. [CrossRef]
- Rached, C.R.; Oliveira, T.C. de; Sousa, C.L.M. de M.; Escudeiro, I.M.; Mori, L.P.; Ferreira, F.P.; Xavier, J.C.B.; Milioni, B.H. de M.; Figueiredo, R.R. de; Paula, M.A. de Avaliação Do Conhecimento Sobre Urgências Oftalmológicas Dos Acadêmicos Da Faculdade de Medicina Da Pontifícia Universidade Católica de Campinas. Rev Bras Oftalmol 2012, 71, 100–105. [CrossRef]
- Cobbs, L.; Tsui, E.; Haberman, I.; Kim, E.; Sperber, L.; Wu, M.; Schuman, J. Student Perceptions of the Ophthalmology Curriculum in Medical School. Journal of Academic Ophthalmology 2018, 10, e79–e82. [CrossRef]
- Gameiro, G.R.; Gameiro, G.R. Ligas Acadêmicas de Oftalmologia: Gerando Impacto Na Educação Médica. Arq Bras Oftalmol 2020, 83. [CrossRef]
- Ferreira, M. de A.; Gameiro, G.R.; Cordeiro, F. de M.; Santos, T.V.; Hilarião, A.A.V.B.P.; Souza, G.M.; Nassaralla Neto, J.J.; Carricondo, P.C.; Portes, A.J.F.; Portes, A.L.F. Perfil Multicêntrico Do Acadêmico de Medicina e Suas Perspectivas Sobre o Ensino Da Oftalmologia. Rev Bras Oftalmol 2019, 78, 315–320. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).