1. Introduction
Breast cancer is the most prevalent cancer among women worldwide, with an estimated 2.3 million new cases diagnosed in 2020 [
1]. Mastectomy, the surgical removal of the entire breast, remains a common treatment option for women with breast cancer. Breast reconstruction, the restoration of the breast form and function following mastectomy, plays a crucial role in the physical and psychological well-being of patients [
2].
The choice between implant-based and autologous reconstruction techniques depends on various factors, including patient preferences, oncologic considerations, and surgeon expertise [
3]. Implant-based reconstruction utilizes silicone or saline implants to recreate the breast mound, while autologous reconstruction employs the patient’s own tissue, such as abdominal tissue or back muscle, to form the breast [
4].
In recent years, there has been a growing trend towards implant-based reconstruction, with studies reporting a steady increase in their utilization.[
5] This trend may be attributed to several factors, including advances in implant technology, improved surgical techniques, and patient preferences for shorter operative times and faster recovery [
6].
The emergence of the COVID-19 pandemic in 2020 has posed unprecedented challenges to healthcare systems globally, potentially influencing decision-making processes and surgical practices in breast reconstruction. The need for resource optimization, minimizing patient exposure during the pandemic, and concerns about potential virus transmission may have affected the choice of reconstruction techniques and timing [
7,
8].
Despite the increasing literature on the pandemic’s impact on various aspects of healthcare, there is limited evidence on how it has affected breast reconstruction trends. This study aims to address this knowledge gap by analyzing the American Society of Plastic Surgeons’ (ASPS) data on breast reconstruction procedures from 2015 to 2022, comparing the pre-pandemic and pandemic periods.
Authors hypothesize that the COVID-19 pandemic has led to a higher proportion of implant-based reconstructions, particularly direct-to-implant procedures, and an increase in immediate reconstructions compared to the pre-pandemic period. This study will provide valuable insights into the impact of the pandemic on breast reconstruction trends and inform future practice and research directions.
2. Materials and Methods
Data Source and Study Design
This retrospective study utilized data from the American Society of Plastic Surgeons’ (ASPS) National Plastic Surgery Statistics, spanning from 2015 to 2022. The dataset, freely accessible on the ASPS statistics website, includes procedural data reported by ASPS member surgeons and other physicians certified by boards recognized by the American Board of Medical Specialties. The comprehensive dataset is anonymized and provided for public access, ensuring compliance with ethical standards for data privacy and confidentiality.
Study Objectives
The study aimed to investigate the impact of the COVID-19 pandemic on breast reconstruction trends in the United States. It specifically focused on examining the utilization rates of implant-based and autologous techniques, as well as comparing the timing of reconstruction—immediate versus delayed. This analysis helps to understand shifts in surgical practices and patient preferences during the pandemic period.
Ethical Considerations
Given the public accessibility and fully anonymized nature of the ASPS data, this study did not require Institutional Review Board (IRB) approval. The data were used strictly within the bounds of ethical guidelines for academic research. By utilizing publicly available data that adhere to stringent privacy standards, this study maintains the highest ethical standards, ensuring that all analyses are performed without compromising individual privacy.
Variables and Definitions
Breast reconstruction procedures were categorized as implant-based (tissue expander/implant and direct-to-implant) or autologous (transverse rectus abdominis myocutaneous [TRAM], deep inferior epigastric perforator [DIEP], latissimus dorsi, and other flaps). Reconstruction timing was classified as immediate (performed at the same time as mastectomy) or delayed (performed after mastectomy).
The study period was divided into pre-pandemic (2015-2019) and pandemic (2020-2022) periods, with 2020 considered the start of the pandemic period, aligning with the World Health Organization’s declaration of the COVID-19 outbreak as a global pandemic in March 2020.
Statistical Analysis
Descriptive statistics were calculated to summarize the annual trends in the number and proportion of implant-based and autologous reconstructions, as well as immediate and delayed procedures. The Shapiro-Wilk test was employed to assess the normality of the data distribution. As the data violated the normality assumption, non-parametric tests were utilized for comparisons between the pre-pandemic (2015-2019) and pandemic (2020-2022) periods. The relative proportions of reconstruction methods (implant-based vs. autologous) and timing (immediate vs. delayed) were compared using chi-square tests. Statistical significance was set at a two-sided p-value < 0.05. All statistical analyses were conducted using SPSS version 29.0.2.0 (IBM Corporation, Armonk, NY).
3. Results
Overall Trends in Breast Reconstruction
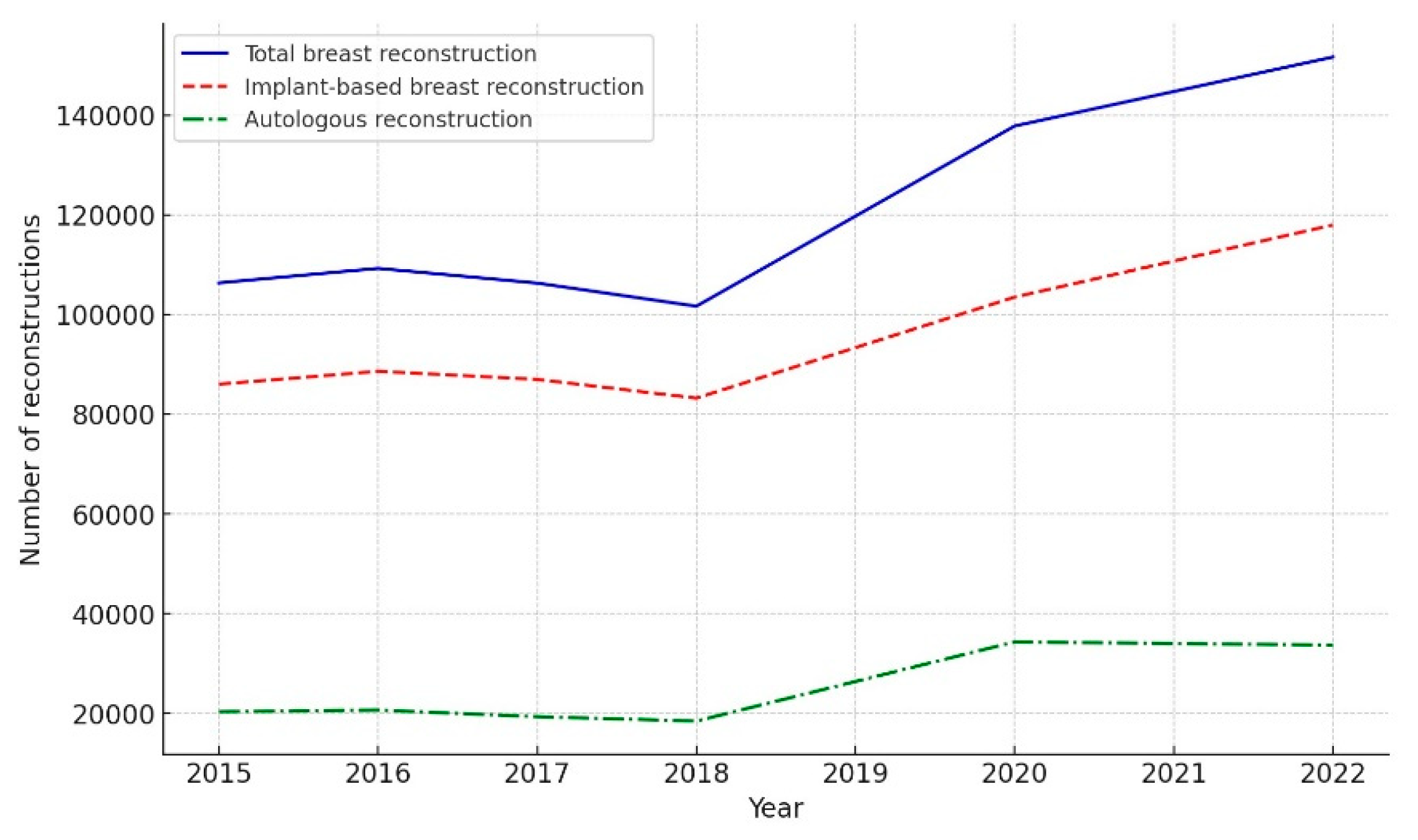
A comprehensive analysis of breast reconstruction procedures in the United States from 2015 to 2022 was conducted using data from the ASPS Database (
Table 1). The findings revealed a significant increase in the annual number of breast reconstructions performed, with a 42.5% rise from 106,338 in 2015 to 151,641 in 2022, highlighting the growing demand for these procedures (
Figure 1).This section may be divided by subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
To better understand the impact of the COVID-19 pandemic on breast reconstruction trends, the data were divided into pre-pandemic (2015-2019) and pandemic (2020-2022) periods (
Table 2). While detailed data on reconstruction type and timing were unavailable for 2019 and 2021, the overall trends could still be observed.
During the pre-pandemic period, implant-based reconstructions accounted for 81.41% of all procedures, with autologous reconstructions making up the remaining 18.59%. However, during the pandemic, the proportion of implant-based reconstructions decreased to 76.51%, while autologous reconstructions increased to 23.49% (p < 0.01).
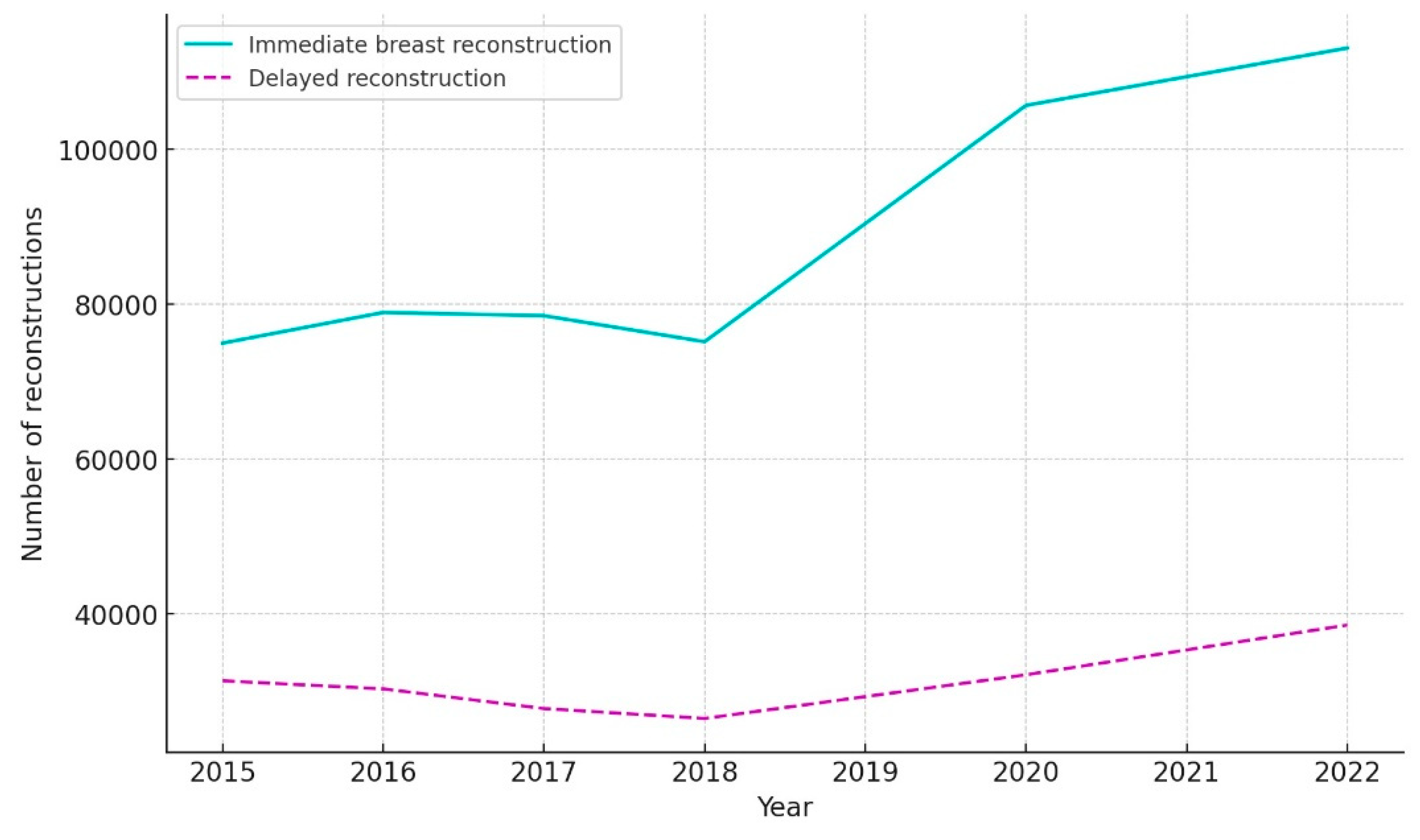
The timing of reconstructions also shifted, with immediate reconstructions increasing from 72.61% in the pre-pandemic period to 75.57% during the pandemic (p < 0.01), and delayed reconstructions decreasing from 27.39% to 24.43% (p < 0.01).
These findings suggest that the COVID-19 pandemic has influenced breast reconstruction trends in the United States, with a notable shift towards autologous reconstructions and immediate procedures.
Implant-Based vs. Autologous Reconstruction
During the COVID-19 pandemic, a notable shift was observed in the adoption of breast reconstruction methods. The proportion of implant-based reconstructions decreased from 81.41% in the pre-pandemic period (2015-2019) to 76.51% during the pandemic (2020-2022) (p < 0.01) (
Table 2). Conversely, autologous reconstructions significantly increased from 18.59% to 23.49% (p < 0.001). This shift suggests a growing preference for autologous tissue reconstruction during the pandemic.
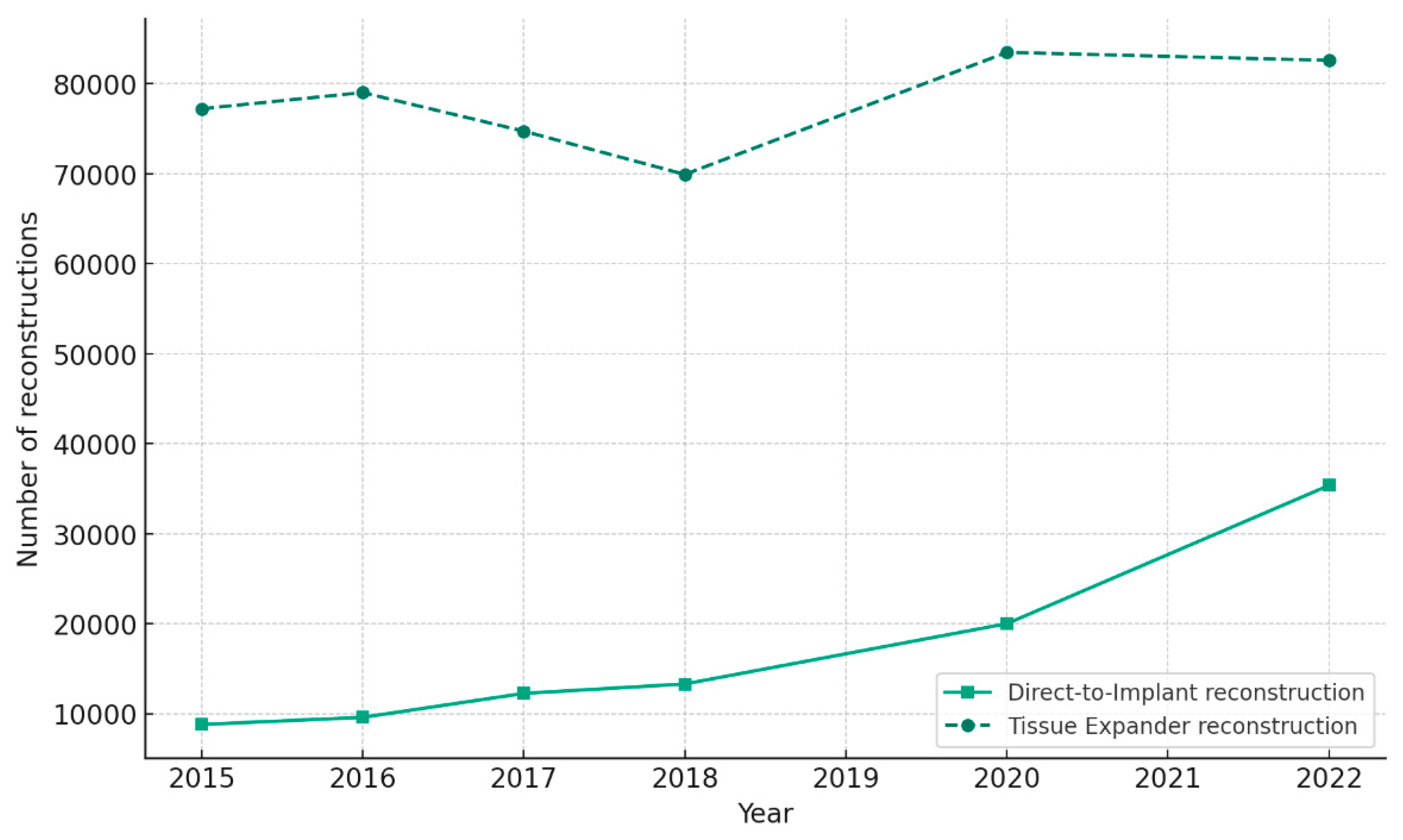
Within the implant-based reconstruction category, a significant shift towards direct-to-implant (DTI) procedures was observed. The proportion of DTI procedures increased from 10.37% to 19.12% during the pandemic (p < 0.001), while tissue expander procedures decreased from 71.05% to 57.38% (p < 0.001) (
Table 2).
Among autologous techniques, DIEP flaps remained the most popular throughout the study period, accounting for 41.60% of all flap-based reconstructions in 2015 and 58.95% in 2022 (
Table 3). The proportion of TRAM flaps decreased from 25.63% in 2015 to 9.68% in 2022, while latissimus dorsi flaps decreased from 29.20% to 15.28% during the same period (
Figure 2). Notably, the proportion of other flaps, which include less common techniques such as superior gluteal artery perforator (SGAP) and transverse upper gracilis (TUG) flaps, increased from 3.57% in 2015 to 16.09% in 2022 (
Table 3). This increase in other flaps may reflect a growing interest in alternative autologous options, possibly due to advancements in microsurgical techniques and a desire for more customized reconstructions.
Trends in Implant-Based Breast Reconstruction Techniques
In the realm of implant-based reconstructions, the data denote a paradigm shift toward single-stage procedures. The incidence of DTI approaches saw a statistically significant increase from 10.37% pre-pandemic to 19.12% during the pandemic (p < 0.001), juxtaposed by a notable decrease in tissue expander/implant procedures from 71.05% to 57.38% (p < 0.001). These trends are quantitatively depicted in
Figure 4 and delineated in
Table 2.
Comprehensive annual data outlined in
Table 5 further illustrates the evolution of DTI and tissue expander/implant case volumes. The proportion of DTI procedures steadily increased from 10.22% in 2015 to 29.98% in 2022, while tissue expander procedures decreased from 89.78% to 70.02% during the same period. Notably, the most prominent shift towards DTI occurred between 2020 and 2022, coinciding with the pandemic period. The total number of implant-based reconstructions also exhibited a consistent growth trend, increasing from 86,013 in 2015 to 117,957 in 2022, despite the challenges posed by the pandemic.
These findings suggest a growing preference for single-stage implant-based reconstruction, particularly DTI, which may be attributed to factors such as advancements in surgical techniques, the use of acellular dermal matrices, and the desire to minimize hospital visits and exposure during the pandemic. The simultaneous decrease in tissue expander procedures further underscores this shift in clinical practice.
4. Discussion
The COVID-19 pandemic has profoundly impacted healthcare delivery across various specialties, necessitating adaptations in surgical practices and decision-making processes [
7]. Our study provides a comprehensive analysis of the pandemic’s influence on breast reconstruction trends in the United States, revealing significant shifts in reconstruction techniques and timing. The most notable changes include a decreased proportion of implant-based reconstructions, an increased adoption of autologous techniques, particularly DIEP flaps, and a higher rate of immediate reconstructions. These findings align with anecdotal reports from plastic surgeons during the pandemic [
9] and highlight the potential impact of pandemic-related factors on breast reconstruction practices [
8].
Implant-Based Reconstruction: Shift Towards Direct-to-Implant Techniques
Although the overall proportion of implant-based reconstructions decreased during the pandemic, a significant shift towards DTI techniques was observed within this category. The proportion of DTI procedures nearly doubled, increasing from 10.37% to 19.12% (p < 0.001), while tissue expander-based reconstructions decreased from 71.05% to 57.38% (p < 0.001) (
Table 2). This trend may be attributed to several factors, including the desire to minimize hospital visits, reduce postoperative complications, and optimize resource utilization during the pandemic [
10].
DTI techniques, particularly prepectoral implant placement with the use of acellular dermal matrices (ADMs), have gained popularity in recent years [
11]. Prepectoral implant placement involves positioning the implant above the pectoralis major muscle, as opposed to the traditional subpectoral placement. ADMs are used to provide additional soft tissue coverage and support, reducing the risk of implant-related complications such as capsular contracture and malposition [
12]. The increased adoption of DTI techniques with ADMs during the pandemic may reflect a preference for a single-stage procedure that minimizes the need for multiple surgeries and hospital visits.
However, it is essential to consider the potential long-term implications of the increased use of DTI techniques. While studies have demonstrated comparable outcomes and patient satisfaction between DTI and two-stage expander/implant reconstructions [
13], long-term data on the safety and effectiveness of prepectoral implant placement with ADMs are still limited [
14]. Future research should focus on evaluating the long-term outcomes, complication rates, and patient-reported outcomes associated with the increased use of DTI techniques during the pandemic.
Rise of Autologous Reconstruction: Emphasis on DIEP Flaps
Our study revealed a significant increase in the proportion of autologous reconstructions during the pandemic, with DIEP flaps being the most popular technique. The proportion of DIEP flaps among all autologous reconstructions increased from 41.60% in 2015 to 58.95% in 2022 (
Table 3). This shift towards autologous reconstruction, particularly DIEP flaps, may be influenced by several factors in the context of the pandemic.
Firstly, autologous reconstruction, especially DIEP flaps, provides a more natural-looking and natural-feeling breast compared to implant-based reconstruction [
3,
15,
16]. The psychological benefits of a more natural reconstruction may be particularly important during a time of heightened stress and uncertainty, as experienced during the COVID-19 pandemic [
17].
Secondly, autologous reconstruction, particularly DIEP flaps, may be associated with a lower risk of post-operative complications and a reduced need for revision surgeries compared to implant-based reconstruction [
18,
19]. In the setting of the pandemic, minimizing the risk of complications and the need for additional surgeries is crucial to reduce patient exposure and optimize healthcare resource utilization [
20].
However, it is important to acknowledge that autologous reconstruction, particularly DIEP flaps, is a more complex and time-consuming procedure compared to implant-based reconstruction [
21]. The increased adoption of DIEP flaps during the pandemic may have implications for surgical training, resource allocation, and patient access. Plastic surgery training programs may need to adapt their curricula to ensure that trainees acquire the necessary skills and experience in microsurgical techniques. Healthcare institutions may need to allocate additional resources, including operating room time, microsurgical equipment, and trained personnel, to support the growing demand for DIEP flaps.
Implications for Clinical Practice and Patient Care
The findings of this study have important implications for clinical practice and patient care in the era of COVID-19. Plastic surgeons should be aware of the shifting trends in breast reconstruction and adapt their practices accordingly. The increased preference for autologous reconstruction, particularly DIEP flaps, may require surgeons to receive additional training or collaborate with microsurgery specialists to meet the growing demand.
Furthermore, the shift towards immediate reconstruction highlights the need for close coordination between the breast cancer treatment team and the reconstructive surgeons. Effective communication and planning are essential to ensure that patients receive the optimal timing and type of reconstruction based on their individual needs and preferences.
Patient education and shared decision-making are also crucial in light of these changing trends. Patients should be provided with comprehensive information about the various reconstruction options, including the benefits and risks of each technique, and the potential impact of the pandemic on their surgical journey. Surgeons should engage in open and honest discussions with patients to help them make informed decisions that align with their values and goals.
Moreover, the increased adoption of DTI techniques with ADMs underscores the importance of long-term follow-up and surveillance. Plastic surgeons should establish appropriate post-operative monitoring protocols to identify and manage any implant-related complications promptly. Patients should be educated about the signs and symptoms of potential complications and encouraged to maintain regular follow-up appointments.
Future Research Directions
The findings of this study provide a foundation for several interesting avenues of future research. Firstly, the long-term outcomes and patient satisfaction associated with the increased use of DTI techniques during the pandemic should be investigated. Prospective studies with extended follow-up periods could evaluate the safety and effectiveness of various DTI approaches, including the use of innovative materials and techniques such as mesh or robotic-assisted surgery. As DTI methods continue to evolve, comparing the outcomes of different surgical approaches and materials will be crucial for guiding evidence-based decision-making and optimizing patient care.
Secondly, the impact of the pandemic on autologous reconstruction, particularly DIEP flaps, warrants further exploration. Future studies could assess the outcomes, complication rates, and patient satisfaction associated with DIEP flaps performed during the pandemic, while also investigating the potential influence of advancements in microsurgical techniques and robotic-assisted surgery on surgical outcomes and efficiency.
Thirdly, the psychosocial impact of the shift towards immediate reconstruction during the pandemic should be examined. Qualitative studies exploring patient experiences, quality of life, and satisfaction with immediate reconstruction in the context of the pandemic could provide valuable insights. Investigating the effectiveness of innovative support interventions, such as online support groups and telemedicine consultations, in promoting patients’ mental well-being and quality of life would also be worthwhile.
Lastly, future research should address the limitations of this study, particularly the missing data for certain years (2019 and 2021) and aim to validate the findings using prospective designs and comprehensive data collection. Researchers should explore strategies to mitigate the impact of missing data, such as imputation methods or sensitivity analyses, to ensure the robustness of the results. Additionally, potential confounding factors, such as changes in patient demographics, cancer stage distribution, and adjuvant therapy trends, should be considered when interpreting the observed shifts in breast reconstruction trends during the pandemic.
By pursuing these research directions and addressing the limitations of the current study, we can gain a more nuanced understanding of the pandemic’s impact on breast reconstruction and identify strategies to optimize patient care and outcomes in the face of future healthcare challenges.
5. Conclusions
The COVID-19 pandemic has significantly influenced breast reconstruction trends in the United States, with notable shifts towards direct-to-implant techniques, autologous reconstruction, particularly DIEP flaps, and immediate reconstruction. These changes reflect adaptations in surgical practice and decision-making processes in response to the unique challenges posed by the pandemic.
As we navigate the ongoing impact of COVID-19, plastic surgeons must remain vigilant, adapt their practices, and prioritize patient safety and outcomes. The findings of this study underscore the importance of patient education, shared decision-making, and long-term follow-up in the context of changing breast reconstruction trends.
Future research should focus on evaluating the long-term outcomes, patient satisfaction, and psychosocial impact associated with the shifts in reconstruction techniques and timing during the pandemic. By understanding the implications of these trends, we can optimize patient care, inform clinical practice guidelines, and ensure that breast cancer patients receive the highest quality of care in the face of the challenges posed by the COVID-19 pandemic.
As we move forward, it is essential for the plastic surgery community to collaborate, innovate, and maintain a strong commitment to patient-centered care. By doing so, we can emerge from this crisis with renewed strength and resilience, better prepared to meet the evolving needs of breast reconstruction patients in the post-pandemic era.
Author Contributions
Conceptualization, D. Kang.; methodology, D. Kang.; software, D. Kang.; validation, SE. Hong., D. Kang.; formal analysis, SE. Hong., D. Kang.; writing—original draft preparation, D. Kang.; writing—review and editing, SE. Hong., D. Kang.; supervision, SE. Hong., D. Kang. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Given the public accessibility and fully anonymized nature of the ASPS data, this study did not require Institutional Review Board approval. The data were used strictly within the bounds of ethical guidelines for academic research.
Informed Consent Statement
Not applicable.
Data Availability Statement
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sedeta, E.T.; Jobre, B.; Avezbakiyev, B. Breast cancer: Global patterns of incidence, mortality, and trends. J. Clin. Oncol. 2023, 41, 10528–10528. [Google Scholar] [CrossRef]
- Zhang, C.; Gomez, D.B.; Abdulwadood, I.B.; Kosiorek, H.; Hammond, J.B.; Cronin, P.M.; Reece, E.M.; Rebecca, A.; Casey, W.; A Pockaj, B. Postoperative complication impact on quality of life after postmastectomy breast reconstruction. J. Am. Coll. Surg. 2023, 237, 319–330. [Google Scholar] [CrossRef] [PubMed]
- von Glinski, M.; Holler, N.; Kümmel, S.; Reinisch, M.; Wallner, C.; Wagner, J.M.; Dadras, M.; Sogorski, A.; Lehnhardt, M.; Behr, B. Autologous Reconstruction After Failed Implant-Based Breast Reconstruction: A Comparative Multifactorial Outcome Analysis. Ann. Plast. Surg. 2023, 91, 42–47. [Google Scholar] [CrossRef]
- Shauly, O.; Olson, B.; Marxen, T.; Menon, A.; Losken, A.; Patel, K.M. Direct-to-Implant vs. Autologous Tissue Transfer: A meta-analysis of patient reported outcomes after immediate breast reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2023, 84, 93–106. [Google Scholar] [CrossRef]
- Yesantharao, P.S.; Arquette, C.; Cheesborough, J.E.; Lee, G.K.M.M.; Nazerali, R.S.M.M. Paradigm shifts in alloplastic breast reconstruction: a nationwide analysis of direct-to-implant trends. Plast. Reconstr. Surg. 2023, 153, 989–998. [Google Scholar] [CrossRef] [PubMed]
- Asaad, M.; Slovacek, C.B.; Mitchell, D.B.; Liu, J.; Selber, J.C.M.; Clemens, M.W.; Chu, C.K.M.; Mericli, A.F.; Butler, C.E. Surgical and patient-reported outcomes of autologous versus implant-based reconstruction following infected breast device explantation. Plast. Reconstr. Surg. 2022, 149, 1080e–1089e. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, R.N.; Stern, C.S.; Graziano, F.D.; Plotsker, E.L.; Haglich, K.; Tadros, A.B.; Allen, R.J.; Mehrara, B.J.; Matros, E.; Nelson, J.A. Decreasing length of stay in breast reconstruction patients: A national analysis of 2019–2020. J. Surg. Oncol. 2023, 128, 726–742. [Google Scholar] [CrossRef]
- Farewell, J.T.; Perez, K.; Henderson, S.; Crook, J.; Hunter, M.; Zhang, A.Y. Psychological impact of the COVID-19 pandemic on breast cancer patients. J. Plast. Reconstr. Aesthetic Surg. 2023, 84, 313–322. [Google Scholar] [CrossRef]
- Aktas, E.H.; Balci, U.D.; Karacaoglu, E. COVID pandemic aftermath: changing dynamics on cosmetic and aesthetic surgery demands. Aesthetic Plast. Surg. 2023, 47, 1658–1665. [Google Scholar] [CrossRef]
- Shivkumar, S.; Mehta, V.; Vaddamanu, S.K.; Shetty, U.A.; Alhamoudi, F.H.; Alwadi, M.A.M.; Aldosari, L.I.N.; Alshadidi, A.A.F.; Minervini, G. SSurgical protocols before and after COVID-19—A narrative review. Vaccines 2023, 11, 439. [Google Scholar] [CrossRef]
- Sohn, S.-M.; Lee, H.-C.; Park, S.-H.; Yoon, E.-S. Difference in the outcomes of anterior tenting and wrapping techniques for acellular dermal matrix coverage in prepectoral breast reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2023, 85, 266–275. [Google Scholar] [CrossRef]
- Samaha, Y.; Chen, J.; Ray, E.C. ADMs and synthetic meshes improve implant-based breast reconstruction aesthetics, but at what cost? J. Plast. Reconstr. Aesthetic Surg. 2023, 80, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Hoque, S.S.B. (.; Zhou, J.M.; Gartoulla, P.; Hansen, J.M.; Farrell, G.M.; Hopper, I.M. Comparing direct-to-implant and two-stage breast reconstruction in the Australian Breast Device Registry. Plast. Reconstr. Surg. 2022, 151, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Vingan, P.S.B.; Haglich, K.; Coriddi, M.; Allen, R.J.; Disa, J.J.; Dayan, J.H.; Matros, E.M.; Mehrara, B.J.; Nelson, J.A. 54. Assessing Long Term Outcomes in Prepectoral Versus Subpectoral Alloplastic Breast Reconstruction. Plast. Reconstr. Surg.-Glob. Open 2023, 11, 26–27. [Google Scholar] [CrossRef]
- Varnava, C.; Wiebringhaus, P.; Kampshoff, D.; Hirsch, T.; Kueckelhaus, M. Use of the superficial inferior epigastric vein in breast reconstruction with a deep inferior epigastric artery perforator flap. Front. Surg. 2023, 10, 1050172. [Google Scholar] [CrossRef] [PubMed]
- Martinez, V.M.B.; Wen, Y.E.B.; Perez, K.M.; Steppe, C.B.; Khan, S.; Haddock, N.; Teotia, S. QS21. Surgical Outcomes of Autologous Breast Reconstruction in Low BMI Patients; Beyond the Gold Standard DIEP Flap. Plast. Reconstr. Surg. - Glob. Open 2022, 10, 102. [Google Scholar] [CrossRef]
- Zwakman, M.; Tan, A.; Boersma, C.; Klinkenbijl, J.; Noorda, E.; de Jong, T.; Francken, A. Long-term quality of life and aesthetic outcomes after breast conserving surgery in patients with breast cancer. Eur. J. Surg. Oncol. (EJSO) 2022, 48, 1692–1698. [Google Scholar] [CrossRef] [PubMed]
- Shatskikh, M.; Coe, L.; McMahon, M.; Kennedy-Williams, S.; Hil, A.; Martin-Smith, J. O080 Evaluation of patient post-operative outcomes after deep inferior epigastric perforator (DIEP) flap surgery. Br. J. Surg. 2023, 110 (Supplement_3), znad101. 080. [Google Scholar] [CrossRef]
- van Rooij, J.A.F.; Bijkerk, E.; van der Hulst, R.R.J.W.; van Kuijk, S.M.J.; Tuinder, S.M.H. Replacing an implant-based with a DIEP flap breast reconstruction: breast sensation and quality of life. Plast. Reconstr. Surg. 2023, 152, 293–304. [Google Scholar] [CrossRef]
- Guru, S.; Gupta, P.; Bakhtavar, J.; Chauhan, G.; Gupta, K. COVID and Perioperative Considerations. J. Card. Crit. Care TSS 2023, 7, 17–20. [Google Scholar] [CrossRef]
- Ahmed, Z.; Ioannidi, L.; Ghali, S.; Hamilton, S.; Shtarbanov, P.; Mosahebi, A.; Nikkhah, D. A single-center comparison of unipedicled and bipedicled diep flap early outcomes in 98 patients. Plast. Reconstr. Surg. - Glob. Open 2023, 11, e5089. [Google Scholar] [CrossRef] [PubMed]
- Delgado, J.A.J.; de Monterrey, M.U.; Echeverría, A.E.N.; Sosa, S.H.R.; Pérez, C.I.R.; Díaz, F.R.E.; Reyna, V.H.S. Importance of Reconstructive Breast Surgery after Mastectomy. Int. J. Med Sci. Clin. Res. Stud. 2023, 03, 878–880. [Google Scholar] [CrossRef]
- Doherty, C.; Pearce, S.; Baxter, N.; Knowles, S.; Ross, D.; McClure, J.A.; Brackstone, M. Trends in immediate breast reconstruction and radiation after mastectomy: A population study. Breast J. 2020, 26, 446–453. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).