1. Introduction
Compared to urban populations, consistent evidence shows a health disadvantage associated with living in rural areas, a trend observed across developed countries [
1,
2]. In Canada, research consistently reports higher mortality rates, decreased life expectancy, greater incidence and prevalence of morbidity, and poorer self-reported health status in rural populations compared to their urban counterparts [
3,
4,
5,
6,
7]. Several explanations for this difference have been proposed, including a higher likelihood of smoking, alcohol use, and obesity [
4,
8], patterns of health service use [
9,
10], and socioeconomic factors such as lower levels of education, income instability, and exposure to hazardous environmental and occupational conditions [
11,
12]. Within rural areas exist one sub-population, farmers, who report concerning levels of poor physical and mental health. Given the difficulty of engaging with farmers on mental health issues [
13], we aimed to explore the issues influencing mental help-seeking among farmers from the perspectives of mental healthcare providers. We were also interested to understand the strategies these providers used to navigate these issues to effectively engage with this vulnerable population.
In 2021, nearly one-fifth of Canadians (18%) lived in a rural area [
14]. The term "rural" is complex and socially constructed, with no universal definition [
15]. For our study, we applied a broad definition that considers rural areas as all territory beyond urban areas [
16]. Thus, rural areas can include towns, villages, agricultural spaces, as well as undeveloped and wilderness areas. Although rural areas share some similarities (i.e., small populations, located away from urban areas), they vary greatly in population densities and living conditions [
17]. Moreover, there is growing recognition that rural areas contain sub-populations with distinct health risk factors, highlighting the need for targeted interventions [
18]. One particular rural sub-population at risk for poor physical and mental health is farmers. Agriculture is recognized as one of the most stressful occupations [
19]. Not only must farmers endure daily stressors such as long work hours, manual labor, and time pressure, but they also face factors beyond their control such as fluctuating market prices, environmental regulations, and extreme weather conditions [
19,
20,
21]. Farm stress has been linked to depression, anxiety, and burnout [
22,
23,
24,
25], as well as suicide [
26]. A national study of over 1,000 Canadian farmers revealed that 57.8% were classified with mild to severe depression, 49.2% with mild to severe anxiety, and they had elevated levels of burnout and low levels of resilience compared to the general population rates [
25].
While timely help-seeking can mitigate the adverse effects of poor mental health [
26], farmers have shown a lower propensity to seek treatment for physical or mental health issues compared to the general adult population [
27,
28]. In fact, for many farmers, seeking help often becomes a last resort, if pursued at all [
26,
29]. Apart from the relatively fewer healthcare providers offering mental health services in rural areas compared to urban locales in Canada [
24,
30], farmers exhibit reluctance to seek assistance due to various factors including financial and geographical barriers, uncertainty about where to seek support or assess relevance, concerns regarding anonymity, and the enduring stigma surrounding mental health within farming communities [
28,
31,
32,
33]. A critical consideration for farmers when seeking mental health support is whether the services and providers possess "farm credibility," indicating an understanding of the unique needs and challenges associated with agricultural life [
34]. Such credibility may significantly influence the establishment of a therapeutic alliance, thereby impacting treatment engagement and outcomes.
Given the challenges many Canadians in rural and remote communities face in accessing mental healthcare services, coupled with the pressing issue of poor mental health among farmers, the Canadian healthcare system is actively seeking solutions to ensure equitable access to timely, relevant, and high-quality care [
35]. While existing research on farmers and mental health services has primarily focused on their barriers to care [
31,
32,
33,
34,
36], there has been comparatively little exploration of the perspectives of healthcare providers in rural areas and their strategies for engaging with farmers to address their mental health needs. One study conducted by Vayro et al. [
28] explored how rural clinicians approached mental health issues with their farmer patients. Findings revealed that clinicians found beginning consultations by asking patients if they had other concerns helpful, as it allowed farmers an opportunity to discuss topics such as family or farming stressors. Despite clinicians being a familiar point of contact for farmers [
31], medical doctors typically have limited training in mental health to adequately support the complex mental health needs of farmers [
32,
37].
With a growing interest in expanding healthcare services to rural areas to address the mental health needs of farmers [
35], it is imperative that these services effectively address farmers' barriers to help-seeking and establish credibility within the agricultural industry [
34]. A recent environmental scan of mental health support services in Canada identified several successful initiatives engaging individuals in rural areas, particularly those from farming communities [
30]. However, no study has yet explored help-seeking issues and successful strategies used for farming populations from the perspectives of mental healthcare providers. Therefore, employing a strength-based approach that includes the positive attributes rather than the negative ones [
38], our study aimed to develop an in-depth understanding of the factors influencing mental help-seeking among farmers in rural areas from the viewpoint of mental healthcare providers. Additionally, we sought to explore the strategies used by providers to navigate these challenges and effectively engage with this vulnerable population. Our goal was to use this information to derive a set of lessons learned to inform interventions and practices of other healthcare providers interested in developing programs or services for individuals living in farming communities.
2. Methods
2.1. Design
We employed a descriptive phenomenological research design [
39] to gain a deep understanding of healthcare providers' perspectives and experiences in delivering mental health support to individuals in farming communities. This approach was chosen as it enables us to learn from others' experiences [
39] and explore how various contexts and backgrounds influence providers' understanding. Phenomenology is a valuable qualitative methodology because it requires researchers to set aside their preconceptions to gain new insights through interpreting participants’ experiences. This study was reviewed and approved by the University of Alberta’s human research ethics board (Pro00126443).
2.2. Participants
Drawing from a database that identified mental health support services for individuals residing in rural areas in Alberta, Canada [
30], we randomly selected 25 services out of a possible 217 using a random choice generator. Each service provider received an email invitation from the first author to participate in a one-on-one semi-structured interview, aimed at exploring their perspectives and experiences in delivering mental health services to individuals in farming communities. Additionally, we advertised our study on social media platforms such as Facebook and our program website. Those interested in participating contacted the first author via email to schedule an interview. To be eligible to participate, individuals had to offer direct mental health support, serve a rural area, and have been operational for the past 12 months. We received 17 responses to the email invitations and four responses to our study advertisement. All participants were compensated with a
$20 gift card from an online retailer.
2.3. Data Collection
Each interview began with a review of the study objectives and procedures, and participants provided verbal consent to continue. All interviews (N = 21) were conducted virtually via Zoom, audio-recorded, and lasted approximately 30 minutes. They followed a semi-structured protocol focusing on three main areas: (1) perspectives on the mental health needs of farmers, (2) approaches they used to address farmers’ barriers to mental healthcare, and (3) experiences providing mental health services in rural areas. The interviews were led by the first author, who had extensive experience conducting qualitative interviews. Field notes were taken during each interview, and were added to each transcript as a memo to complement the qualitative analysis. Subsequent to the interviews, participants received a copy of the consent form and a mental health resource sheet tailored for the farming community via email. All interviews were transcribed verbatim.
2.4. Data Analysis
Prior to analysis, all interview transcripts were screened for accuracy and any identifying information was removed to protect the identities of the participants. Transcripts were uploaded to Quirkos qualitative software to facilitate data analysis and data management. The interviews were independently reviewed and analyzed by three of the authors (RP, NR, and AC). Our analysis was guided by Colaizzi’s [
40] seven-step process that included (1) reading and re-reading the transcripts to make sense of them; (2) identifying significant statements and phrases that relate to the topic; (3) describing the meaning from the statements and phrases; (4) moving statements and phrases into common themes and sub-themes; (5) compiling an exhaustive description of the themes and sub-themes; (6) refining and describing the themes so that the fundamental structure of phenomenon emerges; and (7) validating the findings through discussions with three experts who reviewed the findings. Further content validation for our findings came from achieving data saturation. Data saturation occurs when no further issues or insights are identified during data collection, and the data starts to repeat, signally that additional data collection is unnecessary and a sufficient sample size has been achieved [
41]. In our study, data saturation began to occur at approximately participant number 15. The research team met weekly to review the coding process and addressed any discrepancies in coding through consensus.
3. Results
The analysis included interviews conducted with 21 healthcare providers offering mental health services to farmers in rural areas. The sample predominantly comprised women (n = 19, 90.48%), with healthcare providers offering mental health support through various channels: community-based social service agencies (n = 10, 47.61%), private counselling practices (n = 9, 42.88%), or healthcare facilities (n = 2, 9.52%). On average, healthcare providers had been practicing for approximately 9.86 years (SD = 8.60). While all possessed experience living in rural areas, the majority (n = 15, 71.43%) had a background in farming or agriculture, with some being part of a farm family and others having previously worked in agriculture or currently residing on a farm. Analysis of the interview data revealed five major themes that underscored the issues recognized by healthcare providers as needing attention to meet the needs of farmers. Each theme and sub-theme are described in detail below, accompanied by verbatim quotes from the participants.
3.1. Ensuring Accessibility
Participants emphasized the intertwining nature of geographical, technological, temporal, and financial barriers, creating a daunting landscape for farmers to seek help. In their view, many farmers struggled with the dilemma of prioritizing their own mental well-being amidst competing demands and limited resources (e.g., only one vehicle). Moreover, a lack of awareness or recognition of poor mental health symptoms often led farmers to only seek help when they reached a crisis point. For this theme, we identified three sub-themes: geographical proximity, scheduling conflicts, and financial considerations. For each, we highlighted how healthcare providers addressed the concerns.
3.1.1. Geographical Proximity
The geographic isolation of smaller rural towns created a significant challenge for many farmers to access timely mental health services, underscored by the scarcity of specific services tailored to them. For instance, one healthcare provider explained, “Within a smaller community, right, you're very far away from services, there's just no services that are accessible. And the ones that are might not be the ones you need” (Participant 1). Given the distance to services, many clients needed to dedicate part of their day to traveling sometimes long distances to seek professional assistance. One healthcare provider observed, “I think travel is a big concern. I have some people that drive from [location] all the way to see me ... that's a solid commitment and traveling two and a half hours for family counselling” (Participant 21).
3.1.2. Ensuring Service Options
In response to accessibility challenges, many healthcare providers opted to continue offering virtual sessions post-pandemic. However, despite efforts to enhance accessibility, technological barriers such as poor internet connectivity persisted in rural and remote areas. In a digital era where online information is increasingly relied upon, healthcare providers acknowledged the unreliable nature of internet services, which frustrated them and their patients. As articulated by one healthcare provider, “When you get out more west from here, their internet service sucks. It doesn't matter what provider you have, it's terrible. They can’t connect with me and I can’t connect with them” (Participant 5). Moreover, some rural communities such as Hutterite colonies continued to have internet restriction rules, so healthcare providers would sometimes go to these communities or offer telephonic services.
While transitioning out of the pandemic, most service providers have tried to offer a broader range of in-person, telephone, and online options to improve flexibility. While healthcare providers acknowledged that telephonic or online services provided anonymity which was important in smaller rural areas, there was a common belief that farmers preferred in-person services. For example,
“It's a mix. Of course, it was definitely more virtual when we first got started in 2020. But now, there's definitely more people that are wanting to come to our physical office, which is good by us. So I would say it's probably like an 80/20 split of 80% in-person, the other 20% virtual. We do have clients that will swap back and forth, depending on how their day is playing out or where they need to be and that kind of a thing” (Participant 6).
Participants agreed that the job structure of most healthcare providers, especially those working in healthcare organizations or community-based services, operated within standard 9 to 5 business hours, which do not align with farmers' irregular work patterns. Participants stressed the importance of offering sessions outside of regular business hours and having flexible cancellation policies. As one participant highlighted,
“If [farmers] are available, it's not necessarily during regular business hours… [They] might be stuck with seeding all day, or spraying at a very certain time because there’s a very small window for that. …Farming doesn't operate on eight to five.” (Participant 1)
3.1.3. Funding and Insurance Coverage
One of the most prominent issues impacting accessing programs was funding and insurance. From the healthcare providers’ perspective, the concern centered on the high cost of their services and the lack of insurance available for farmer clients to cover them. The limited coverage resulted in financial constraints for farmers, restricting their ability to access necessary counselling sessions or in some cases, limiting the amount of sessions they could have for free. According to one participant,
“[P]sychologists know that they're high in demand, so they're $250 an hour, and then people only have $500 worth of benefits. So I charge $100 an hour, so I could give five sessions. They can only get two from a psychologist.” (Participant 8)
While some participants offered their services on a sliding scale, most emphasized the need for increased government funding to expand access to counselling services, advocating for subsidies or broader insurance coverage that includes non-psychologist services. Moreover, participants urged for a broader definition of mental health to enable community-based organizations to deliver programs beyond traditional counselling, such as recreational programs that incorporated mental health components. As one participant pointed out,
“More money. It always comes down to money. But I think the other thing is that it's important to notice that there has been no increase in our funding since 2016. So populations have increased, the needs of people and community and all communities have astronomically increased, yet the amount of funding for preventative programs has remained the same.” (Participant 12)
3.2. Being Relatable
Participants described the need for healthcare providers to find a way to relate to their patients, and often this meant translating their mental health service in a way that resonated with farmers and worked to establish credibility in the agricultural community. Our analysis revealed two sub-themes: building trust, and connecting culturally.
3.2.1. Building Trust
Participants emphasized how crucial it was to demonstrate an authentic understanding and appreciation of the struggles and stresses inherent in agriculture to establish a solid foundation of trust with farmer patients. For example, many participants explained how farmers often felt that their lifestyle and work was often misunderstood by healthcare providers unfamiliar with rural areas, often referring to them as “outsiders” or “city folk” who “don’t know the first thing about what we do.” As highlighted by one participant who stated,
“I think the relatability is so important. It’s part of the foundation to building trust. So, if someone says ‘I am working 14 hours, and I feel like I'm running on my feet all the time, and I have no time to eat or anything’ and then the therapist says, 'Well, why don't you just hire somebody else?' Like, if that's not always possible depending on the operation or whether it's a family farm.” (Participant 2)
Recognizing this, the healthcare providers we interviewed mentioned how important it was for their services to be tailored with the needs of farmers. They demonstrated that they could relate to farmers by having extended hours of operation, having weekend sessions, and having flexible cancellation policies. Many also mentioned that their website highlighted their background in farming or agriculture. In other words, healthcare providers needed to demonstrate their relatability in their business structure as well as their own knowledge. As one healthcare provider stated,
“There's a lot of centralized programs that are, you know, a one-size-fits-all approach for delivering healthcare. I think farmers can see through that, and they will call bullshit on it. Basically, they’re thinking ‘this is not for me’, but you’re telling me it is. But when I pick up the phone and talk to you, you don't know where I am or what I do” (Participant 5).
Participants highlighted a concerning trend of high turnover among counsellors and healthcare providers in rural areas, which can significantly impact the trust-building process within farming communities. This turnover eroded the continuity of care and could undermine the efforts made by farmers who had invested their time, money, and effort in seeking help. The departure of counsellors for urban opportunities created a revolving-door effect, leaving rural communities feeling abandoned and mistrustful of healthcare providers. Our participants mentioned that maintaining trust required an ongoing effort, and many gained it by being an active member in the community. This point was emphasized by one participant,
“There are some communities that I served that had counsellors come in and then take a position that opened up in the city. It’s a sort of revolving door, so then the community has a hard time trusting as well” (Participant 18).
3.2.2. Connecting Culturally
Healthcare providers unanimously agreed on the importance of establishing cultural connections with farmers to foster trust and encourage service utilization. Several commented how people living in rural areas differed a lot from those living in urban areas, such that the “rural demographic wants a personal touch and wants to know that the person they're talking to is human with their own life and their own problems” (Participant 13). Furthermore, a shared understanding of farming sometimes removed the psychological distance between the client and the provider, allowing them to get right to the issue. For example, one participant explained,
“Patients can talk about farming with me and I get it, right? They can tell me about, you know, seeding being a lot of pressure…. And I can say, ‘Yeah, I totally get that. I'm in an intergenerational farm, so I understand where you're coming from [and] how that’s affecting your life’. Then we can move forward rather than focusing on giving me all the details” (Participant 14).
Relatability was a significant factor in establishing trust among farmers to use the services. For example, farmers were inclined to seek assistance from familiar faces within their community rather than outsiders, highlighting the importance of established relationships and community connections. For example, one participant explained,
“I think people's [family] names really mean a lot too, so there's that automatic trust built in, [because] the person who's doing a program or service has a family name that you recognize.” (Participant 2)
3.3. Addressing Stoicism and Stigma
Healthcare providers acknowledged the concerns about privacy, stigma, cultural attitudes, and the perceived toughness within rural, farming communities. Many observed that farmers, especially men, were reluctant to seek help due to fears of judgment and gossip within close-knit communities. Our analysis revealed two sub-themes: acknowledging farm culture, and managing mental health stigma.
3.3.1. Acknowledging Farm Culture
Participants described how engaging and treating farmers was made easier by having an understanding of what farm culture entailed. In their words, farm culture were deeply-rooted values of independence, stoicism, and toughness. Often, that meant that work came first and their needs second. Participants described how they would expect to have long gaps between patient visits given the seasonal work of farming. Many participants observed that men in rural, farming communities grew up in a culture that valued and practiced self-reliance, determination, and associated hard work with pride. One participant explained that reinforcing a flexible, confidential policy was important, and provided this explanation about farm culture:
“You’ve got to tough it out. They’ll tell themselves [that] it's not anxiety, it's not depression, it's farming. So you’ve got to suck it up and keep going. Don't ask for help. If you ask for help, then there's something wrong with you.” (Participant 7).
While these values were pervasive in farming communities, they were more prominent among men, and often prevented many from seeking help even when they knew they needed it. As one participant explained,
“Men, you know, … they don't want to go to the doctor for help. And especially the older folks, and when there's large distances to cover and so much going on… a lot of these guys are suffering in silence” (Participant 4).
3.3.2. Managing Mental Health Stigma
Some participants explained that their farmer patients often wanted to talk to someone that they could relate to but they simultaneously did not want others to know they were seeking help. With the general agreement that stigma still existed in rural areas, one participant explained, “There's way more fear of reaching out in the community. Because if I'm seen coming in these doors, I'm perceived as weak or less than, and I think that is amplified in the farming community” (Participant 7)
Most healthcare providers approached issues of mental health stigma by taking steps to “disguise” their mental health services if they did not offer online services. For example, one participant explained that if you wanted clients to come to your office, you certainly “wouldn’t have a big sign outside your door” that says “mental health”. She explained, “We have an office inside of the college. So people can park there and go anywhere in the college” (Participant 8). Others explained that because the need for anonymity was strong in farming communities, mental health programming was often embedded into more comfortable venues such as community dinners or wellness workshops.
While these strategies were generally successful at building awareness about mental health, they were not as powerful as word-of-mouth recommendations from farmers to their peers. Indeed, many healthcare providers recognized how powerful peer-influence was in rural communities, and many relied on “having the word spread” about a good experience to decrease stigma and bring in new clients. For example, one participant explained:
“I think one of the first ranchers that I saw, you know, once he kind of put the pieces together like, ‘This is a really good resource’ and ‘Everybody should be doing this’. He would come in [and say] ‘I've been telling all my friends about this’. And then you start to see more of them filter through.” (Participant 6).
3.4. Navigating Dual Relationships
Our participants recognized that living in a rural area meant it was inevitable that they would encounter a patient in the community. All healthcare providers stated that they discussed issues of confidentiality at the outset of their first session, with most telling their patient that if they saw each other in public that they would not initiate a greeting unless the patient did so first. However, in small rural communities, providers often found themselves in situations that tested their boundaries and forced them to maintain professionalism at all times. For example, one participant explained:
“My husband was a big card player. He had a bunch of guys [over] and this guy goes ‘Jeez, I've seen you before. Where have I seen you before?’ And I'm like, I don't know. And all of a sudden it clicked that he was a counselling client. …And then I went upstairs and never went back downstairs after because I knew that he then clicked that we knew each other. So I knew I had to keep my distance…keep my space and let him not feel uncomfortable” (Participant 15).
Most providers believed that managing dual relationships was necessary. In their view, being integrated into the community helped to establish trust. Others mentioned that they would offer workshops and seminars as a way to reach out to residents, and rely on advertisements in local newspapers in addition to social media. One participant explained, “So we have to realize that we maybe need to go out to the community a little bit more, rather than them having to come to us” (Participant 1).
3.5. Community Trauma
Participants described how events traumatic losses, such as the suicide, the mass euthanasia of an entire herd of cattle, or an accident could profoundly affect the entire community. We labeled this theme "community trauma" to reflect the collective psychological impact experienced due to significant and distressing events. The close-knit nature of rural areas often meant that traumatic losses were shared experiences of distress and grief, disrupting the community's social fabric, sense of safety, and trust in institutions. One significant issue highlighted by healthcare providers was the limited mental health resources available in rural areas, often resulting in different patients discussing the same issue. As one participant described, “The amount of opioid deaths that have been going on … and the increase here in the last little while has been felt by the entire community” (Participant 4).
One healthcare provider described how community trauma can bring people together, but the effects are often short-lived and lack any real structure to have a lasting impact. For example, several healthcare providers described offering seminars or workshops, yet, these were often poorly attended and lacked continuity. Often the people who needed the support were not the ones who attended, or the event took place at an inconvenient time for farmers. Working to establish ongoing mental health support was essential. As one participant described,
“You did a one off and everybody's like, great. And then now what and then you have nothing happening after and I think that becomes where you really get a disconnect because like you're doing something and then you stop and then you do something and they stop and then you've like, lost all those people in between” (Participant 1).
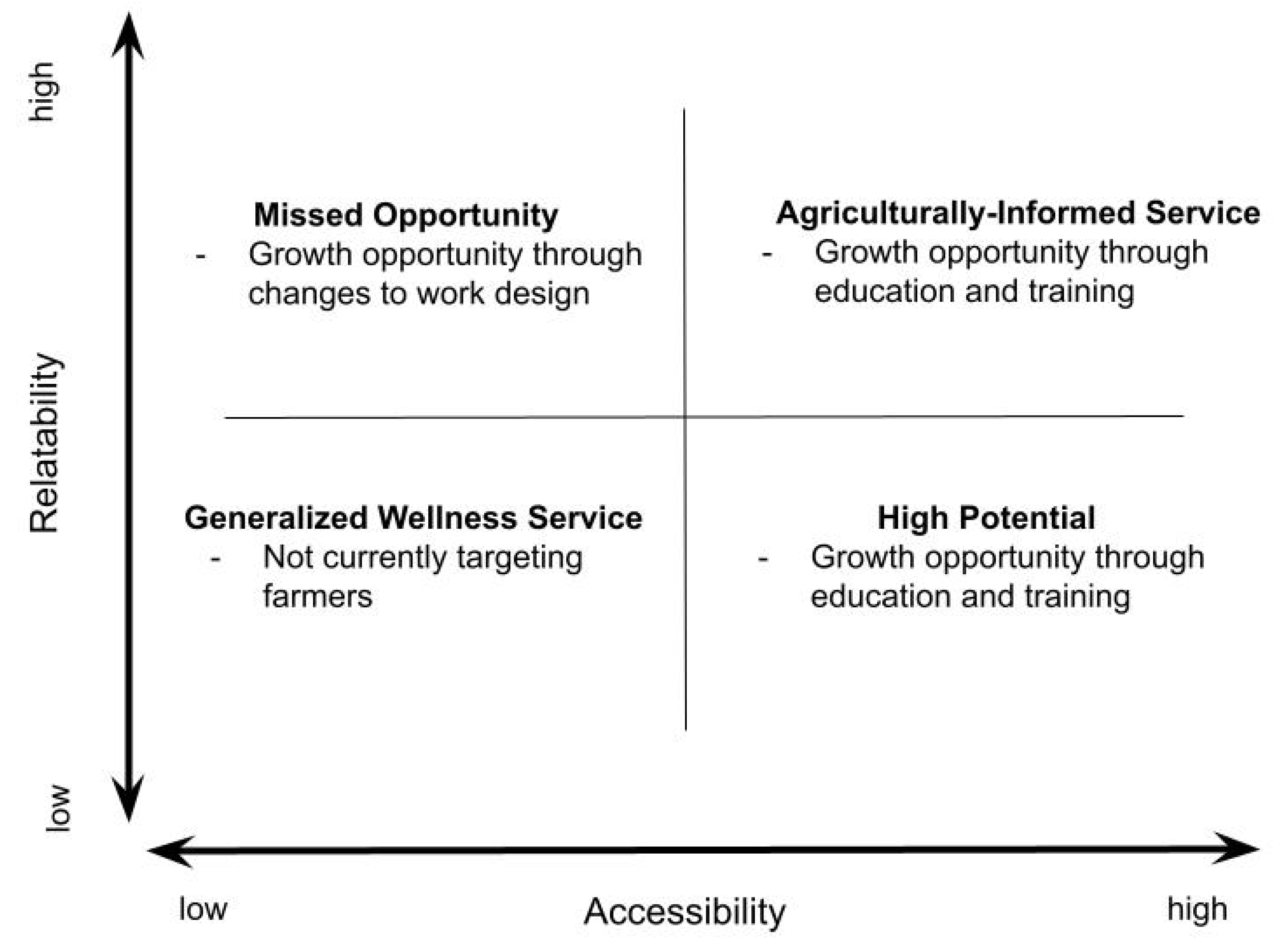
3.6. Four-Quadrant Model
One of the final steps in our analysis involved identifying the fundamental structure of the themes we identified. Upon reviewing our coding, two themes emerged as essential considerations for healthcare providers delivering mental health services to farming populations in rural areas: Relatability and Accessibility. As illustrated in
Figure 1, we represented these themes in a four-quadrant model, which served as a basic framework for identifying the placement of healthcare services concerning the provision of agriculturally-informed rural mental health care. We labeled this model, the
Agriculturally-informed Service Model.
Utilizing this framework, we categorized participants' services into one of the four quadrants, assigning each a label and description. For instance, the Missed Opportunity quadrant (high relatability, low accessibility) encompassed services where mental healthcare providers understood farm culture and could deliver farm-informed care. However, structural barriers such as limited work hours or reliance on virtual care options hindered accessibility. The High Potential quadrant (low relatability, high accessibility) delineated services where mental healthcare providers offered flexible hours and policies. However, they lacked sufficient knowledge of farm culture to confidently provide agriculturally-informed care. The Agriculturally-informed quadrant depicted services where providers possessed a strong understanding of farm culture. Additionally, their service structures were flexible, offering various options and accessible hours.
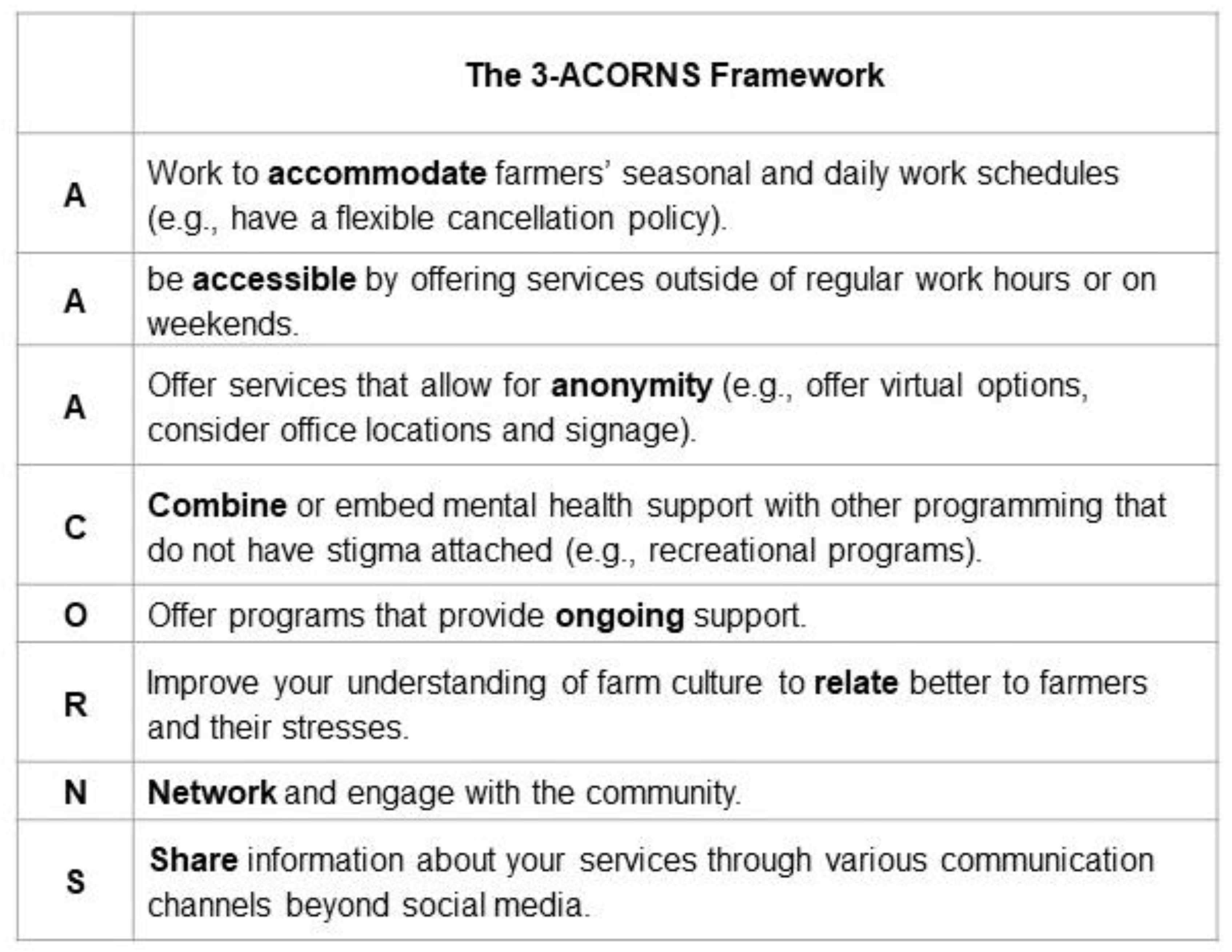
3.7. Evidence-Based Guiding Framework
We identified eight practices associated with healthcare service providers who offered agriculturally-informed services and successfully engaged with farmers (Table 1). We named this framework the 3-ACORNS Framework, representing the acronym AAACORNS. This framework extends our four-quadrant model by aiding mental healthcare providers aspiring to work with farmer clients in identifying aspects of their practice that may require adjustment. The metaphor of "acorns" resonated well in our western Canadian context, drawing parallels with the bur oak, the only oak tree species thriving in the cold prairie climate. Similar to the bur oak's resilience, we found that only agriculturally-informed services demonstrated effective and long-term engagement with farming populations in rural areas.
Figure 2.
Evidence-based 3-ACORNS framework.
Figure 2.
Evidence-based 3-ACORNS framework.
4. Discussion
Healthcare providers acknowledged that farmers constitute a unique subculture, largely because of the occupational demands of the agricultural industry [
19], within rural areas [
36]. Consequently, participants in our study recognized the necessity for a distinct approach to mental health service delivery to address their needs. The current study aimed to understand the factors influencing mental help-seeking among rural-living farmers from the perspective of healthcare providers, while also exploring strategies they used to encourage help-seeking. Our findings offer insights for mental healthcare providers to adopt strategies aimed at improving help-seeking rates among farmers, thereby potentially reducing high levels of poor mental health and elevated suicide rates in this population [
25,
26]. Early engagement with appropriate support has been shown to mitigate distress and suicidality, a pressing concern in farming populations [
42,
43]. Our analysis revealed five major themes among mental healthcare providers: ensuring accessibility, being relatable, addressing stoicism and stigma, navigating dual roles, and understanding community trauma. These themes are interrelated, illustrating how an understanding of these issues can inform the adaptation of healthcare practices to provide more agriculturally-informed services to facilitate farmers' help-seeking.
A prominent theme emerging from our data highlighted the pressing need for accessible mental healthcare services in rural areas. Healthcare providers emphasized the challenges farmers face in accessing these services, citing lengthy travel times on rural and remote roads, a preference for in-person options over internet-based ones, and the financial strain of out-of-pocket expenses. Our findings align with Hagen et al. [
34], who also emphasized the significant barriers posed by financial constraints and geographical distance to accessing mental health services in rural areas. While technology-based services hold promise in addressing accessibility barriers, unreliable internet connections in rural areas continue to hinder the establishment of telemedicine services [
32,
34]. For instance, in Alberta, approximately 67% of rural residents lack access to reliable high-speed internet [
44]. Additionally, Vayro et al. [
32] reported that general practitioners (GPs) were hesitant to refer patients to technology-based solutions due to concerns about their relevance and suitability for farmers. This point highlights the importance of tailoring such services to meet the specific needs and preferences of farming communities to improve help-seeking behavior. To address these challenges, healthcare providers in our study offered several service options, flexible cancellation policies, and extended service hours into evenings and weekends.
Relatability emerged as a significant concern for healthcare providers aiming to encourage farmers to utilize their services. However, ensuring that mental health resources are culturally relevant for farmers has been overlooked. One review found that 62.6% of programs aimed at increasing mental health resources for farmers focused on providing educational materials such as fact sheets, web pages, workshops, conferences, and articles [
45]. As our participants noted, these types of resources are likely to have little or short-term impact because they lack interaction and continuity. While having someone to talk to was deemed important, the review also found that many hotlines or in-person counselling services made available for farmers tended to offer general services instead of ones tailored to their mental health needs [
45]. The importance of ensuring mental health services are delivered by a provider with farm credibility is essential [
34], particularly for individuals at an elevated risk for suicide and psychological distress. Our participants emphasized that being familiar with the community, possessing an understanding of agriculture and farm culture, helped reduce the psychological distance that many of their patients may perceive when seeking professional help.
While opinions regarding the acceptability of dual relationships varied among participants, our findings underscored their importance in rural settings. Consistent with previous research [
46,
47], integrating into the community fostered trust and facilitated cultural competence development among healthcare providers [
48]. Halverson and Brownlee [
47] similarly argued for the necessity of dual relationships in rural areas due to resource limitations. However, participants acknowledged the challenge of maintaining such relationships, given the frequent encounters with patients in various community contexts, although they believed that clear boundaries could mitigate potential issues. Furthermore, the complexity of maintaining dual relationships in rural areas could be exacerbated during critical events such as suicides, which impacted multiple families. Farming communities, often regarded as collectivist societies within the broader individualistic culture [
49], experienced collective grief and loss in such situations. Unlike their urban counterparts, our participants highlighted the need for careful consideration of confidentiality and privacy issues in rural settings.
Our study contributes to a growing body of research aimed at addressing help-seeking behaviors among farming populations in rural areas. A notable strength of our study is the four-quadrant model and the guiding framework. To our knowledge, no such framework not list exists to assist healthcare providers in assessing whether their practices align with agriculturally-informed approaches and what strategies they could adopt to become more agriculturally-informed. However, our study has limitations. Despite using a random sampling approach, there may be a self-selection bias. It is possible that participants who were aware of disparities in urban-rural healthcare services were more inclined to participate. Additionally, our sample included more women participants from a western Canadian province, which may limit generalizability of the findings. Further research is needed to validate our findings across diverse geographical and political contexts. It may also be beneficial for quantitative studies to explore the relative importance of service-related factors in predicting help-seeking behaviors among farmers and identify individual differences variables. Such investigations would further inform the development of tailored approaches to enhance farmers' help-seeking behavior.
Our findings offer implications for intervention development, clinical practice, and future research. First, given the persistent mental health stigma in many rural areas [
51], healthcare providers may need to think creatively about how to incrementally deliver mental health services. For instance, while single workshops or seminars may not be effective in producing long-term change, they can serve as a starting point for spreading awareness and building trust within the community. Additionally, integrating mental health programming within existing services, such as recreational programs, may present an effective strategy to combat stigma while promoting awareness and engagement [
51,
52]. We do, however, recognize that implementing changes to one’s practice is highly dependent on their type of practice. For example, providers who operate a private practice had more flexibility to make changes whereas providers working for a healthcare organization had less. Second, healthcare providers practicing in rural areas should receive training and education related to farmer mental health issues to enhance their cultural competence and ability to detect signs of poor mental health during consultations. Finally, our study focused on the job design factors and work approaches to engaging with farmer clients. While these factors are important to encourage initial help-seeking, more research is needed to understand how to foster trusting relationships in the therapeutic setting so that farmers return to continue their mental health work.
5. Conclusions
In summary, our study provides new insights for improving mental healthcare delivery for farming populations in rural areas. By identifying key strategies and approaches used by mental healthcare providers, our findings contribute to ongoing efforts to improve help-seeking among farmers, with the ultimate goal of reducing the high levels of poor mental health and suicide prevalent in this demographic. Our evidence-based framework, rooted in five major themes, offers a roadmap for adapting mental healthcare services to address the unique challenges faced by farmers. By addressing issues of accessibility, relatability, stoicism, stigma, dual roles, and community trauma, our findings highlight the complexity of delivering mental healthcare in rural areas. Moving forward, understanding and integrating these insights into healthcare practice can significantly impact early engagement with appropriate support, thereby mitigating distress and suicidality among farming populations.
Author Contributions
Conceptualization, R.P.; methodology, R.P.; validation, R.P. and D.H.; formal analysis, R.P, N.R. and A.C.; investigation, R.P.; resources, R.P.; data curation, R.P.; writing—original draft preparation, R.P, N.R. and A.C.; writing—review and editing, R.P. and D.H.; visualization, R.P and N.R.; supervision, R.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Agricultural Research and Extension Council of Alberta and the Alberta Minister of Agriculture and Irrigation (RES0061171).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and reviewed and approved by the University of Alberta’s Health Research Ethics Board (REB) under the Project ID: Pro00126443.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study. No identifiers were used during the interviews while transcribing to maintain the privacy of the participants. Participation in the study was voluntary, and participants knew they could decide to withdraw at any point. The participants provided verbal informed consent before beginning the interviews.
Data Availability Statement
The interview guide and de-identified data presented in this study are available upon request from the corresponding author. The data are not publicly available due to privacy concerns.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Smith, K.B.; Humphreys, J.S.; Wilson, M.G. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Aust J Rural Health 2008, 16, 56–66. [Google Scholar] [CrossRef] [PubMed]
- O'Reilly, G.; O'Reilly, D.; Rosato, M.; Connolly, S. Urban and rural variations in morbidity and mortality in Northern Ireland. BMC Public Health 2007, 7, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute for Health Information. How healthy are rural Canadians? 2006. Available online: https://secure.cihi.ca/free_products/rural_canadians_2006_report_e.pdf (accessed on 13 April 2024).
- Mitura, V.; Bollman, R.D. The health of rural Canadians: a rural–urban comparison of health indicators. Rural Small Town Canada Anal Bull. 2003;4:6. Statistics Canada, Catalogue no. 21-006-XIE.
- Lavergne, M.R.; Kephart, G. Examining variations in health within rural Canada. Rural Remote Health 2012, 12, 34–46. [Google Scholar] [CrossRef]
- Vafaei, A.; Rosenberg, M.W.; Pickett, W. Relationships between income inequality and health: a study on rural and urban regions of Canada. Rural Remote Health 2010, 10, 270–278. [Google Scholar] [CrossRef]
- Pampalon, R.; Martinez, J.; Hamel, D. Does living in rural areas make a difference for health in Québec? Health Place 2006, 12, 421–435. [Google Scholar] [CrossRef] [PubMed]
- Pong, R.W.; DesMeules, M.; Lagacé, C. Rural–urban disparities in health: How does Canada fare and how does Canada compare with Australia? Aust J Rural Health 2009, 17, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Allan, D.; Cloutier-Fisher, D. Health service utilization among older adults in British Columbia: Making sense of geography. Can J Aging 2006, 25, 219–232. [Google Scholar] [CrossRef]
- McDonald, J.T.; Conde, H. Does geography matter? The health service use and unmet health care needs of older Canadians. Can J Aging 2010, 29, 23–37. [Google Scholar] [CrossRef]
- Matz, C.J.; Stieb, D.M.; Brion, O. Urban-rural differences in daily time-activity patterns, occupational activity and housing characteristics. Environ Health 2015, 14, 1–11. [Google Scholar] [CrossRef]
- Bollman, R.D.; Reimer, W. Demographics, employment, income, and networks: differential characteristics of rural populations. J Agromedicine 2009, 14, 132–141. [Google Scholar] [CrossRef]
- Brumby, S.; Smith, A. ‘Train the trainer’ model: implications for health professionals and farm family health in Australia. J Agromedicine 2009, 14, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Population in rural areas. Available online: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-x/2021002/98-200-x2021002-eng.cfm (accessed on 10 April 2024).
- Herron, R.V.; Skinner, M.W. Farmwomen's emotional geographies of care: A view from rural Ontario. Gend Place Cult 2012, 19, 232–248. [Google Scholar] [CrossRef]
- Statistics Canada. Definition of rural. Available online: https://www12.statcan.gc.ca/census-recensement/2021/ref/dict/az/Definition-eng.cfm?ID=geo042 (accessed on 13 April 2024).
- Kulig, J.C.; Williams, A.M. Health in rural Canada; UBC Press, 2011. [Google Scholar]
- Gillespie, J. Health Disparities for Canada's remote and northern residents: Can COVID-19 help level the field? J Bioeth Inq 2023, 20, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.; Hagen, B.N.; Lumley, M.N.; Winder, C.B.; Gohar, B.; Jones-Bitton, A. “An incredible amount of stress before you even put a shovel in the ground”: a mixed methods analysis of farming stressors in Canada. Sustain 2023, 2023 15, 1–23. [Google Scholar] [CrossRef]
- Hagen, B.N.; Albright, A.; Sargeant, J.; Winder, C.B.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. Research trends in farmers’ mental health: A scoping review of mental health outcomes and interventions among farming populations worldwide. PLoS one 2019, 14, e0225661. [Google Scholar] [CrossRef] [PubMed]
- Kearney, G.D.; Rafferty, A.P.; Hendricks, L.R.; Allen, D.L.; Tutor-Marcom, R. A cross-sectional study of stressors among farmers in eastern North Carolina. N C Med J 2014, 75, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Henning-Smith, C.; Alberth, A.; Bjornestad, A.; Becot, F.; Inwood, S. Farmer mental health in the US Midwest: key informant perspectives. J Agromedicine 2022, 27, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Deegan, A.; Dunne, S. An investigation into the relationship between social support, stress, and psychological well-being in farmers. J Community Psychol 2022, 50, 3054–3069. [Google Scholar] [CrossRef] [PubMed]
- Jones-Bitton, A.; Best, C.; MacTavish, J.; Fleming, S.; Hoy, S. Stress, anxiety, depression, and resilience in Canadian farmers. Soc Psychiatry Psychiatr Epidemiol 2020, 55, 229–236. [Google Scholar] [CrossRef]
- Thompson, R.; Hagen, B.N.; Lumley, M.N.; Winder, C.B.; Gohar, B.; Jones-Bitton, A. Mental health and substance use of farmers in Canada during COVID-19. Int J Environ Res Public Health 2022, 19, 13566. [Google Scholar] [CrossRef]
- Purc-Stephenson, R.; Doctor, J.; Keehn, J.E. Understanding the factors contributing to farmer suicide: a meta-synthesis of qualitative research. Rural Remote Health 2023, 23, 1–11. [Google Scholar] [CrossRef]
- Sagar-Ouriaghli, I.; Godfrey, E.; Bridge, L.; Meade, L.; Brown, J.S. Improving mental health service utilization among men: a systematic review and synthesis of behavior change techniques within interventions targeting help-seeking. AJMH 2019, 13, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Brew, B.; Inder, K.; Allen, J.; Thomas, M.; Kelly, B. The health and wellbeing of Australian farmers: a longitudinal cohort study. BMC Public Health 2016, 16, 988. [Google Scholar] [CrossRef]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. A thematic analysis of the personal factors influencing mental health help-seeking in farmers. J Rural Health 2023, 39, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Komiti, A.; Judd, F.; Jackson, H. The influence of stigma and attitudes on seeking help from a GP for mental health problems: a rural context. Soc Psychiatry Psychiatr Epidemiol 2006, 41, 738–745. [Google Scholar] [CrossRef]
- Purc-Stephenson, R.; Roy, N. Supporting farmer mental health: Environmental scan and resource map of mental health support services across rural Alberta. Available online: https://static1.squarespace.com/static/63d44379cabc893dc3c637c9/t/65a1a1f26d4e854942842f51/1705091591257/Research_2023_01_RPS+Environmental+Scan+%26+Resource+Map+Report.pdf (accessed on 12 April 2024).
- Judd, F.; Jackson, H.; Komiti, A.; Murray, G.; Fraser, C.; Grieve, A.; Gomez, R. Help-seeking by rural residents for mental health problems: the importance of agrarian values. Aust N Z J Psychiatry 2006, 40, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. ‘Farming is not just an occupation [but] a whole lifestyle’: a qualitative examination of lifestyle and cultural factors affecting mental health help-seeking in Australian farmers. Sociol Ruralis 2020, 60, 151–173. [Google Scholar] [CrossRef]
- Rose, D.C.; Bradley, F.; O’Connor, D.; Hall, J.; Morrison, R.; Mulkerrins, M.; Nye, C.; Russell, T. The mental wellbeing of young farmers in Ireland and the UK: driving factors, help-seeking, and support. Scott Geogr J 2023, 26, 1–21. [Google Scholar] [CrossRef]
- Hagen, B.N.; Sawatzky, A.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. “Farmers aren’t into the emotions and things, right?”: a qualitative exploration of motivations and barriers for mental health help-seeking among Canadian farmers. J Agromedicine 2022, 27, 113–123. [Google Scholar] [CrossRef]
- Finnigan, P. Mental health: A priority for our farmers. Report of the Standing Committee on Agriculture and Agri-food. https://epe. lac-bac. gc. ca/003/0 0. 2019, 8,19-22.
- Cole, D.; Bondy, M.C. Meeting farmers where they are–rural clinicians’ views on farmers’ mental health. J Agromedicine 2020, 25, 126–134. [Google Scholar] [CrossRef]
- Crowther, A.; Ragusa, A.T. Realities of mental health nursing practice in rural and remote Australia. Issues Ment Health Nurs 2011, 32, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Gharabaghi, K.; Anderson-Nathe, B. Strength-based research in a deficits-oriented context. Child Youth Serv 2017, 38, 177–179. [Google Scholar] [CrossRef]
- Neubauer, B.E.; Witkop, C.T.; Varpio, L. How phenomenology can help us learn from the experiences of others. Perspect Med Educ 2019, 8, 90–97. [Google Scholar] [CrossRef]
- Morrow, R.; Rodriguez, A.; King, N. Colaizzi’s descriptive phenomenological method. Psychologist 2015, 28, 643–644. [Google Scholar]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. SSM 2022, 292, 1–10. [Google Scholar] [CrossRef] [PubMed]
- de Diego-Adeliño, J.; Portella, M.J.; Puigdemont, D.; Pérez-Egea, R.; Álvarez, E.; Pérez, V. A short duration of untreated illness (DUI) improves response outcomes in first-depressive episodes. J Affect Disord 2010, 120, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Oliffe, J.L.; Ogrodniczuk, J.S.; Bottorff, J.L.; Johnson, J.L.; Hoyak, K. “You feel like you can’t live anymore”: Suicide from the perspectives of Canadian men who experience depression. SSM 2012, 74, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Alberta Government. Alberta broadband strategy. https://www.alberta.ca/alberta-broadband-strategy#:~:text=affordability%20and%20quality.-,Access,peers%20living%20in%20urban%20centres.
- Inwood, S.; Becot, F.; Bjornestad, A.; Henning-Smith, C.; Alberth, A. Responding to crisis: Farmer mental health programs in the Extension North Central Region. J Exten 2019, 57, 20–27. [Google Scholar] [CrossRef]
- Doyle, K. Substance abuse counselors in recovery: Implications for the ethical issue of dual relationships. J Couns Dev 1997, 75, 428–432. [Google Scholar] [CrossRef]
- Halverson, G.; Brownlee, K. Managing ethical considerations around dual relationships in small rural and remote Canadian communities. Int Soc Work 2010, 53, 247–260. [Google Scholar] [CrossRef]
- Gingerich, A.; Simpson, C.; Roots, R.; Maurice, S.B. “Juggle the different hats we wear”: enacted strategies for negotiating boundaries in overlapping relationships. Adv Health Sci Educ 2023, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Somasundaram, D. Collective trauma in northern Sri Lanka: a qualitative psychosocial-ecological study. Int J Ment Health Syst 2011, 1, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Skaczkowski, G.; Hull, M.; Smith, A.E.; Dollman, J.; Jones, M.; Gunn, K.M. Understanding farmers’ barriers to health and mental health-related help-seeking: The development, factor structure, and reliability of the Farmer Help-Seeking Scale. J Rural Health 2024, 40, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S. Physical exercise and psychological wellness. Int J Ment Health Promot 2002, 4, 40–46. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).