1. Introduction
The opioid crisis refers to the extensive misuse and addiction to opioids, which covers both prescription medications and illegal substances synthesized or derived from the opium poppy plant [
1]. It consists of an escalation in overdose deaths: first driven by natural and semi-synthetic opioids like oxycodone until 2010, followed by a spike in heroin deaths post-2010, and more recently dominated by illicit synthetic opioids since 2013, with stimulants now also playing a significant role [
2,
3,
4]. Opioid use disorder (OUD) is a chronic condition with persistent opioid consumption and detrimental consequences to the user [
5]. Over 2.1 million individuals in the United States are affected by OUDs, with an annual death toll of approximately 80,000 linked to opioid misuse [
5,
6].
In response to the crisis, several states have enacted regulations, including Prescription Drug Monitoring Program (PDMP), opioid prescribing guidelines, and prescription-limit laws [
7,
8], aiming to minimize opioid analgesic exposure and prevent the onset of OUD. However, the widespread illicit supplies and varying results from these interventions have hindered their ability to consistently decrease opioid overdoses [
9]. In tandem with these measures, numerous states have also implemented regulations to enhance access to overdose prevention strategies. These efforts include increasing the availability and utilization of naloxone, a substance used to reverse opioid overdoses [
10], as well as expanding the accessibility of Medications for Opioid Use Disorder (MOUD) [
11].
There are three main MOUDs approved by FDA: methadone, buprenorphine, and extended-release naltrexone. Buprenorphine helps reduce drug use and offers protection from overdoses. It is popular because it requires less monitoring and can be given by qualified primary care doctors. Methadone helps lessen cravings and withdrawal from heroin, but due to its associated risks, it is only dispensed through certified Opioid Treatment Programs (OTPs) by the Substance Abuse and Mental Health Services Administration (SAMHSA). Naltrexone aids in preventing relapses after detox. It is safe with no overdose risk, has effects lasting up to 30 days with just one dose, and is available through certain primary care providers [
12,
13,
14,
15].
MOUDs are vital in preventing overdoses and related care complications, but issues like diagnosis, treatment initiation, and patient commitment can limit their impact. This emphasizes the importance of broader adoption and better training for healthcare providers in OUD care [
16,
17]. Over the past decade,efforts have been made to expand MOUD availability [
18]. As a result, 42% of the U.S. population could access all three types of treatments within a 10-mile radius by the end of 2020 [
19]. Yet, despite these advances, gaps in accessibility persist. These gaps are notably pronounced in various geographic locations, including both state and county levels, with rural areas facing particular challenges [
20]. To address these disparities, numerous studies have explored MOUD availability [
21,
22,
23], their effect on overdose rates [
24], and the correlation with community-level socio-demographic factors [
25].
Building on this, a recent study correlated county-level MOUD availability with overdose rates, creating a straightforward classification system that categorizes counties into high and low risk groups. High-risk counties are those with lower level of access to MOUDs than the national average, coupled with higher-than-average overdose rates [
26]. The authors went on to compare the socio-economic and demographic profiles of these county groups, which are key factors in determining opioid demand [
27]. While this approach provides valuable insights into the demand side of the opioid crisis through its focus on characteristics, there is a noticeable gap in research regarding the legal supply side, represented by opioid prescription records. To our knowledge, no study has yet explored legal prescription data in relation to MOUD access and overdose rates.
Our study aims to fill this gap by examining the legal supply side of the opioid crisis using county-level data for South Carolina from 2017 to 2021. The increasing prominence of synthetic opioids like fentanyl in overdose deaths, especially during the fourth wave of the opioid crisis, motivates our first hypothesis: that these potent synthetic opioids are more frequently prescribed in high-risk counties [
3,
28]. Further, based on our prior studies, we observe a trend where patients increasingly seek prescriptions from out-of-state doctors, pharmacies, and retail entities following the implementation of local opioid policies [
29,
30]. We suspect that this behavior is especially prevalent among patients who are likely to have OUD and, therefore, may be more common in high-risk counties. Confirmation of these patterns could result in significant policy implications not just on MOUD access, but also on the regulation of opioid supply.
2. Methodology
2.1. Overview
We start by examining the state-level data to gain a broader perspective on opioid prescription rates and overdose occurrences in South Carolina. This statewide data provides an initial context for the more detailed county-level analysis that ensues. Following this initial step, we utilize the classification method outlined by Haffajee et al. [
26] to categorize counties into high-risk and low-risk based on the availability of MOUDs and the rates of overdose deaths. Subsequently, our study adopts two primary analytical approaches: one that does not consider time and another that explores changes over time. The non-temporal analysis employs a two-way t-test to compare prescription patterns between the high-risk and low-risk counties, focusing on the type of opioids prescribed, the locations of prescribing entities, and the types of dispensing entities. Following this, the temporal analysis utilizes linear regression models to understand how these prescription patterns have evolved over time, particularly in high-risk counties.
2.2. Overdose Deaths and Opioid Treatment Facilities’ Data
This study leverages a dataset aggregated from the South Carolina Department of Health and Environmental Control (SCDHEC), the National Vital Statistics System, and the CDC WONDER database to examine instances of fatal drug overdoses between 2017 and 2021 [
6,
31,
32,
33,
34,
35]. In compiling this dataset, deaths resulting from drug overdoses are categorized by the SCDHEC using ICD-10 codes X40–X44, X60–X64, X85, and Y10–Y14, with a principal emphasis placed on fatalities related to opioids, among other substances.
To categorize specific drug types, SCDHEC employs distinct ICD-10 codes.“Prescription Drugs” are identified through codes T36.0–T39.9, T40.2–T40.4, T41.0–T43.5, and T43.7–T50.8, while “Opioids” are differentiated using codes T40.0 –T40.6. Additionally, natural and semi-synthetic opioids like morphine, codeine, oxycodone, hydrocodone, hydromorphone, and oxymorphone are distinguished from fentanyl, which is highlighted as a prevalent synthetic opioid [
36].
Normalizing the overdose deaths by population is essential to accurately compare across counties. Without such normalization, a mere comparison of raw numbers would lack meaningful context. By using the drug overdose death rate, we ensure that the data is adjusted based on each county’s population, making comparisons more relevant and insightful.
Furthermore, in this study, we analyze three specific medications for OUDs: methadone, buprenorphine, and naltrexone. We extract data regarding methadone by examining the availability of OTPs as listed on the SAMHSA website [
37]. Although it is important to acknowledge that OTPs may dispense additional medications, methadone is singularly dispensed through OTPs that have received certification from SAMHSA. The presence of buprenorphine providers is likewise determined via the SAMHSA website [
38]. In contrast, the availability of naltrexone is assessed through the prevalence of VIVITROL, a brand that signifies an extended-release formulation of naltrexone, information about which is publicly provided by Alkermes Inc., the manufacturer of the drug [
39]. As of the end of 2021, our data indicated the existence of 24 fully certified OTPs, 647 buprenorphine providers, and 41 naltrexone providers in the state of South Carolina.
2.3. Risk Status Classification of Counties
To formulate a risk profile for each county, we adopt the methodology suggested by Haffajee et al. [
26]. We first compute the per capita average of each medication’s providers within the state and then label each county as "low" or "high" risk based on comparison with the state average. To be more precise, we have 0.36 SAMHSA-approved OTPs per 100,000 residents in South Carolina, 0.6 naltrexone providers per 100,000 people, and 9.32 per capita buprenorphine providers. Following this phase, we categorize counties as either high or low risk concerning the availability of each treatment. The ultimate MOUD status is determined by majority rule; that is, if more than one treatment falls into the low category, the overall MOUD status is deemed low, and vice versa. This diverges from the approach suggested by Haffajee et al., who combine all three metrics and compare them to the state average. We argue that our methodology is more equitable as typically OTPs or naltrexone providers are less numerous, and their scale is vastly different from buprenorphine providers. Thus, lumping all metrics together seems to reflect the number of buprenorphine providers more than the other two treatments.
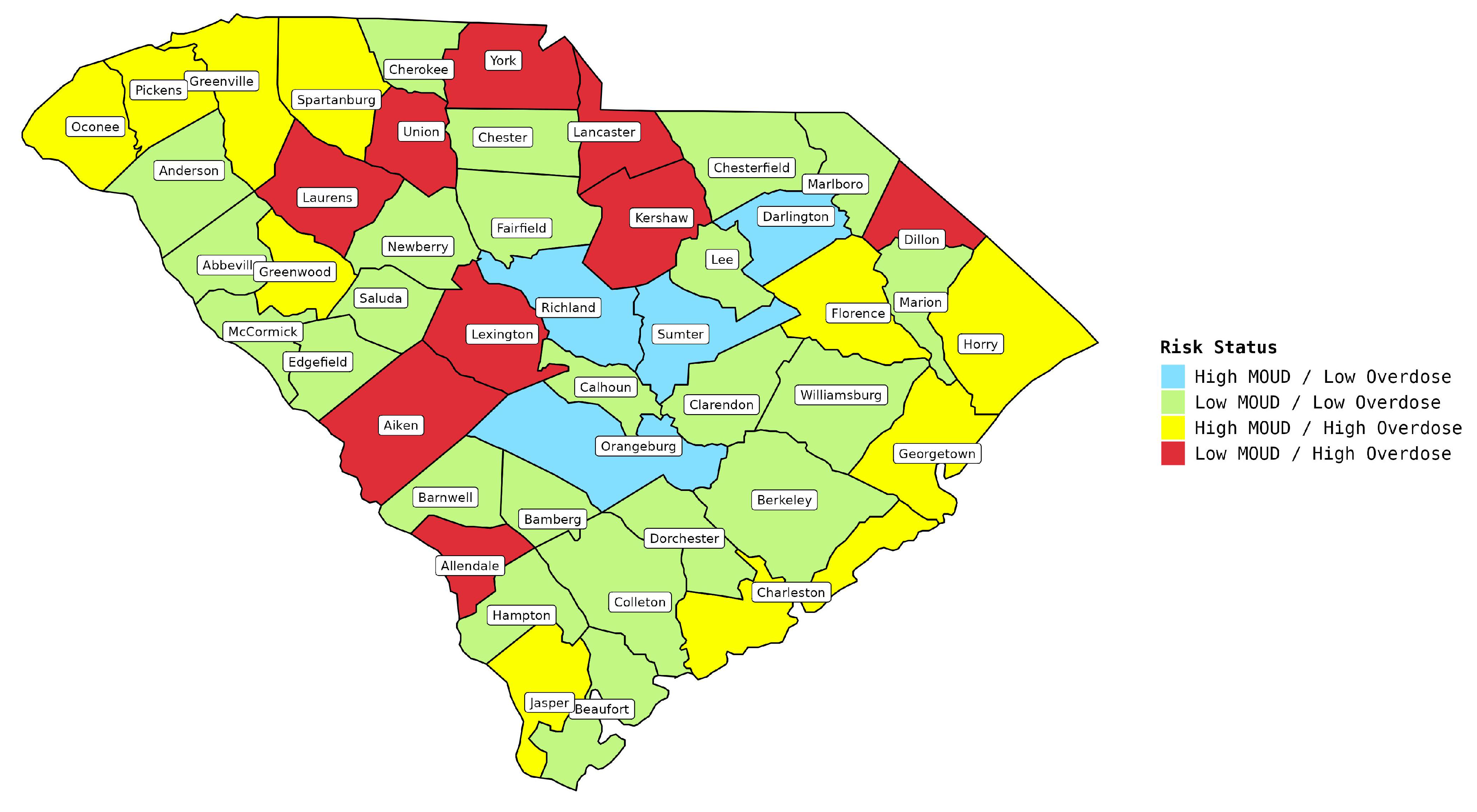
Furthermore, in order to determine the risk level for each county, we combine the per capita overdose death rates with the availability of MOUD, creating a four-category risk status index. The state’s yearly average overdose rate per 100,000 residents stands at 19.02. Consequently, any overdose rate lower than this figure is categorized as low, while rates exceeding it are considered high. This comprises: 1) Counties with high availability of MOUD providers but low overdose rate, 2) Counties with high availability of MOUD providers but high overdose rate, 3) Counties with low availability of MOUD providers but low overdose rate, and finally 4) Counties with low availability of MOUD providers but high overdose rate. These four categories are illustrated in
Figure 1. Evidently, the final category is the most concerning and warrants comprehensive comparison with the other groups. As a result, we further designate the final category as "High Risk" and the remaining three as "Low Risk" counties. Subsequently, we aim to compare prescription patterns between these categorized counties. Additional details pertaining to each treatment and county can be found in the supplemental materials.
2.4. Opioid Prescription Data
The research uses data from the South Carolina Prescription Tracking System, known as SCRIPTS. This large database has about 43 million prescription records from 2014 to 2022. The focus is on the years 2017 to 2021 so that it matches up with the overdose data that is also available for those years. The SCRIPTS database encompasses multiple dimensions such as prescription attributes (e.g., drug name, volume, days supply, and refill status), drug characteristics (e.g., National Drug Code), and details on the prescriber, dispenser, and patient.
Three main areas are looked at in this study: 1) Type of drug, 2) Prescriber’s geographical location, and 3) Type of dispensing institution.
2.4.1. Type of Drug
The drugs of interest in this study are opioids, particularly fentanyl, oxycodone, and hydrocodone. These substances constitute roughly 77% of the opioid prescriptions in our dataset. Our focus on these specific opioids is twofold: firstly, oxycodone and hydrocodone are predominant in opioid prescriptions, rendering other types less relevant for this investigation. Secondly, emerging evidence indicates that fentanyl plays a critical role in overdose incidents, corroborated by the available overdose data [
16]. It is important to note that stimulants, which have been implicated in overdose rates in recent literature, are not included in our dataset [
3].
2.4.2. Prescriber Location
Our emphasis lies on comparing in-state and out-of-state prescribers. Prior research suggests that out-of-state prescribers are more strongly correlated with suspicious prescribing patterns [
29,
30].
2.4.3. Type of Dispenser
The predominant sources for prescriptions are retail and chain pharmacies. Hence, our analysis focuses on these two dispensing categories.
To clarify, the difference between retail and chain pharmacies is as follows:
Retail Pharmacies: These are typically independent pharmacies owned by individuals or small groups. They often serve local communities and may provide more personalized services tailored to their clientele. These pharmacies are stand-alone, meaning they are not part of a larger chain of stores.
Chain Pharmacies: These are part of a large network of stores under a single brand or corporate entity. Examples include CVS, Walgreens, and Rite Aid. Chain pharmacies can be found nationwide, offering standardized services and products.
2.4.4. Doctor Shopping
“Doctor Shopping” refers to the practice of seeking treatment from multiple healthcare providers, either within a single illness episode or with the intention of obtaining prescription medications unlawfully [
40]. In our study, “Doctor Shopping” refers to patients who seek controlled substance prescriptions from several providers, often not for genuine medical reasons. Engaging in this behavior exposes individuals to risks such as OUD and deadly overdoses, and they often simultaneously face mental health challenges, alcohol struggles, and come from lower economic backgrounds [
41,
42,
43,
44]. Given the severe consequences, both health-wise and legally, identifying “doctor shoppers” is vital for healthcare and law enforcement. In our research, while the SCRIPT data does not explicitly label "doctor shopping", we extract instances of this behavior according to the widely accepted definition where patients obtain medication from at least four different prescribers and four dispensers within a year. This approach was chosen based on its frequent use, as pointed out by [
45].
2.5. Statistical Analysis
To identify differences between high-risk and low-risk counties, we utilize the two-sample t-Test and linear regression, each tailored to the specific data and research question. The details are as follows:
Two-Sample T-Test: This test compares the mean per capita prescription rates from
Table 3. It is used for continuous, normally distributed variables to determine if differences between the high-risk and low-risk group means are statistically significant or merely due to random chance. In essence, it evaluates if elements like fentanyl prescriptions or out-of-state prescriptions differ meaningfully between high-risk and low-risk counties. A resulting p-value below 0.05 indicates a statistically significant difference in means.
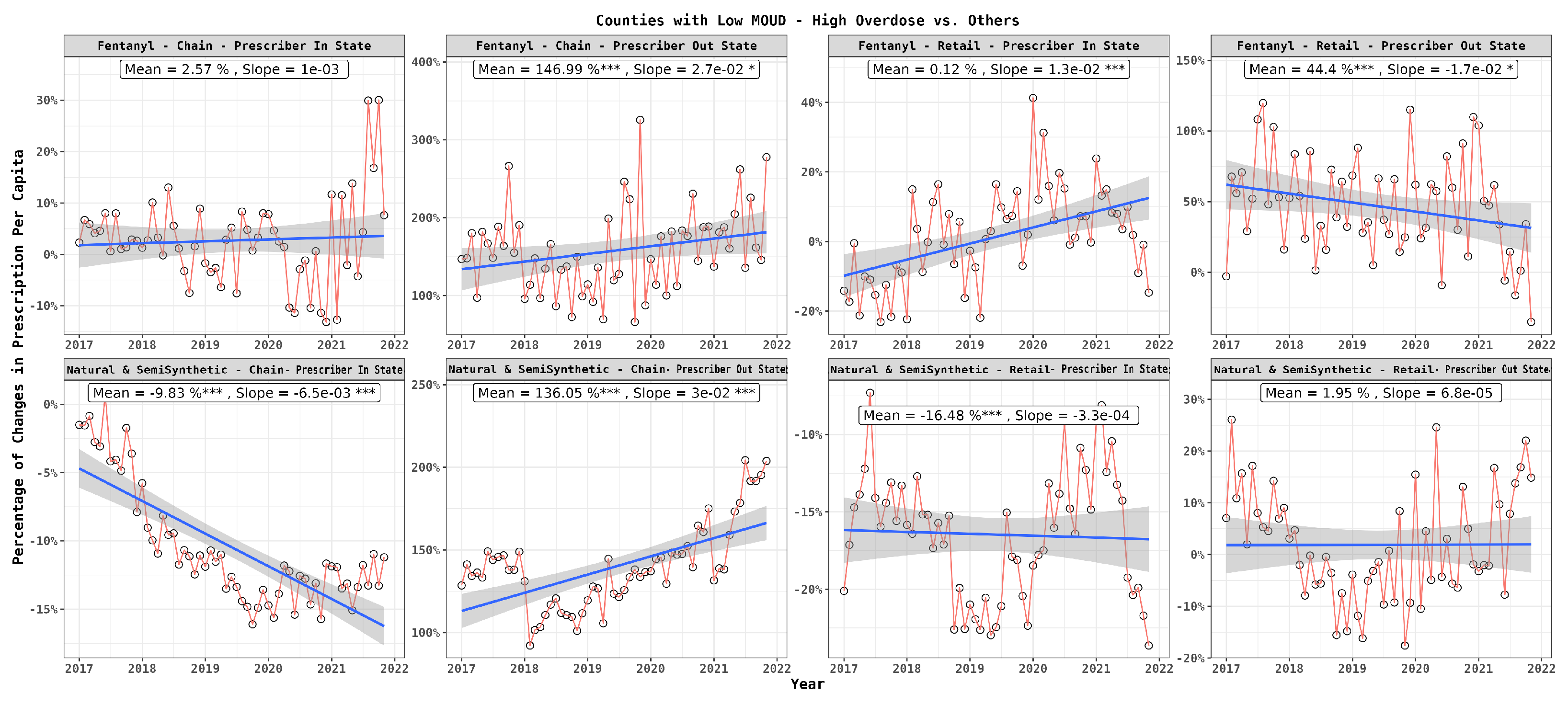
Linear Regression for Trend Analysis: This method assesses how a dependent variable, like the difference in per capita prescription, varies with an independent variable, often time, spanning 2017 to 2021. It is demonstrated in
Figure 3 to
Figure 6. The regression line’s slope signifies the rate of change: a positive slope indicates an increase, while a negative one indicates a decrease. A p-value less than 0.05 confirms the trend’s statistical significance.
By using these two statistical methods in combination, we are able to conduct a nuanced analysis that looks at both the current state and trends over time in high-risk and low-risk counties.
3. Results
3.1. Opioid Trends in South Carolina: Setting the Stage for County Prescription Comparisons
Before we dive into county-specific details, we focus on the high-level metrics of opioid use in South Carolina. From 2017 to 2021, the rate of opioid prescriptions per 100,000 residents drops from 64,223 to 41,214. This happens even though the state issues more than 13 million opioid prescriptions in total. As shown in
Table 1, prescriptions for all types of opioids are on a downward trend. In contrast, overdose deaths, particularly from fentanyl, are on the rise, as
Table 2 shows. Deaths from natural and semi synthetic opioids like methadone, hydrocodone and oxycodone also increase but not as much. These contrasting trends make it crucial to examine what happens at the county level.
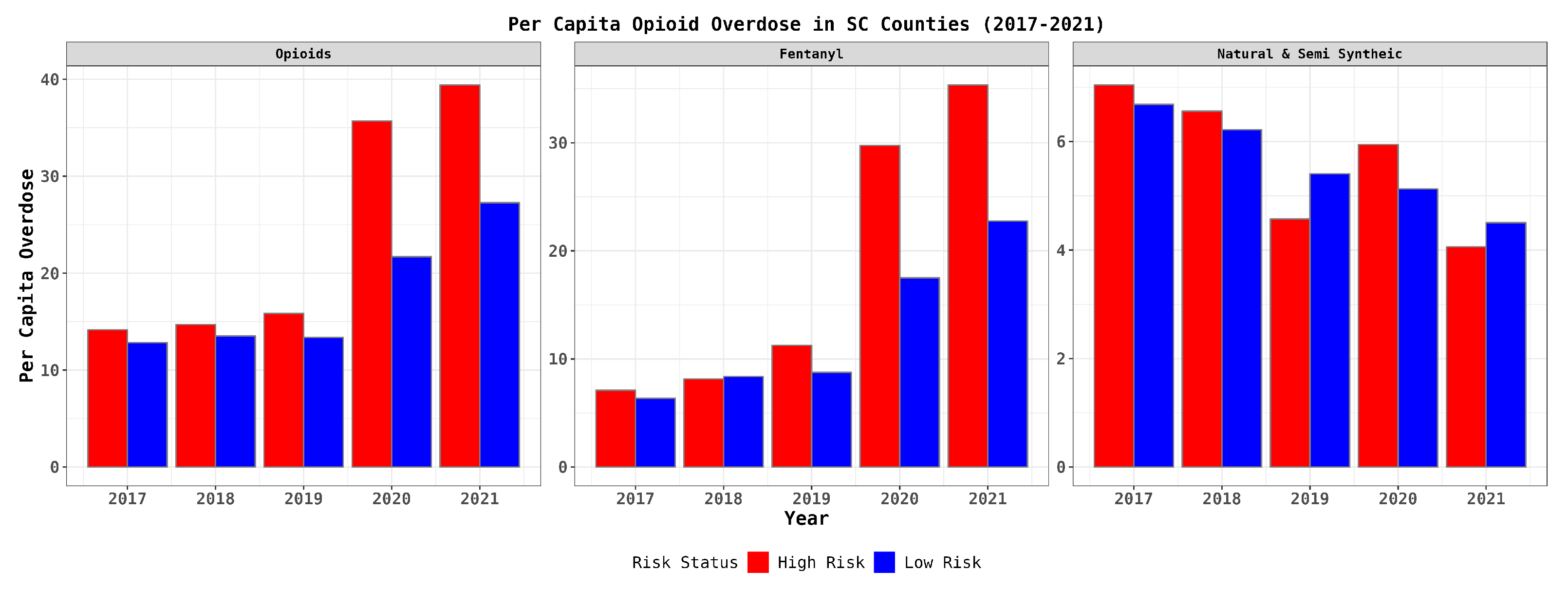
As depicted in
Figure 1, nine counties exhibit below-average MOUD availability coupled with above-average overdose rates, positioning them in a high-risk category, whereas 37 counties do not fall into this category.
Figure 2 visualizes the annual overdose death rates, aligning with the broader statewide trends. Notably, overdoses linked to fentanyl have seen an increase, predominantly in high-risk counties, with a marked rise in 2020 and 2021. In contrast, overdoses resulting from natural and semi-synthetic opioids have remained relatively stable, and their prevalence has reduced over time, persisting in both high-risk and low-risk counties.
These patterns suggest that counties identified as high-risk are grappling with distinct challenges, particularly those related to fentanyl overdoses. Subsequently, we aim to investigate whether insights can be derived from the analysis of legal opioid prescriptions within these counties to further comprehend these variances.
It is important to mention that the overdose data includes both legal and illegal drugs. Since we only have access to data on legally-prescribed opioids, our research only considers the correlation between legal prescriptions and county risk status.
Table 1.
Opioid prescription rates per 100,000 residents during years 2017 to 2021 - State of South Carolina
Table 1.
Opioid prescription rates per 100,000 residents during years 2017 to 2021 - State of South Carolina
| Drug Class |
Year |
Change (%) |
| |
2017 |
2018 |
2019 |
2020 |
2021 |
|
| Opioids |
64223 |
54778 |
50514 |
47686 |
41214 |
-35.83 % |
| Natural & Semi Synthetic |
58294 |
49437 |
45467 |
42957 |
37310 |
-35.99% |
| Fentanyl |
1490 |
1206 |
1097 |
970 |
772 |
-48.19 % |
Table 2.
Opioid overdose deaths during years 2017 to 2021 - State of South Carolina
Table 2.
Opioid overdose deaths during years 2017 to 2021 - State of South Carolina
| Drug Class |
Year |
Change (%) |
| |
2017 |
2018 |
2019 |
2020 |
2021 |
|
| Total Drug Overdose |
1001 |
1103 |
1131 |
1734 |
2168 |
117 % |
| Prescription Drugs |
782 |
863 |
923 |
1463 |
1853 |
137 % |
| Opioids |
748 |
816 |
876 |
1400 |
1733 |
131 % |
| Natural & Semi Synthetic |
315 |
332 |
349 |
418 |
373 |
18% |
| Fentanyl |
362 |
460 |
537 |
1100 |
1494 |
312 % |
Figure 2.
Temporal trend of county level overdose by underlying cause of death during years 2017 to 2021 - State of South Carolina
Figure 2.
Temporal trend of county level overdose by underlying cause of death during years 2017 to 2021 - State of South Carolina
3.2. Comparing Prescription Patterns in High and Low-Risk Counties
Our analysis of prescription data reveals key differences between high-risk and low-risk counties when it comes to opioid use, as shown in
Table 3. Even though patients in both high-risk and low-risk counties get about the same number of opioid prescriptions per person, there is a key difference: patients in high-risk counties have 17% more fentanyl prescriptions per person. Statistical tests confirm that this is a significant difference. On the other hand, prescriptions for natural and semi-synthetic opioids are about the same in both types of counties.
In addition, in high-risk counties, patients are 75% more likely to get prescriptions from out-of-state doctors which is statistically significant too. When it comes to prescriptions from doctors within the state, the rates are about the same for both high-risk and low-risk counties. When it comes to picking a pharmacy, there is not a big difference. Patients in high-risk areas use retail pharmacies about 12% more, but this is not a statistically significant difference. The use of chain pharmacies is about the same in both high-risk and low-risk counties.
Table 3.
Comparison of Characteristics Between High Risk and Low Risk Counties
Table 3.
Comparison of Characteristics Between High Risk and Low Risk Counties
| Characteristic |
Mean (SD) |
P-value |
| |
All Counties |
High Risk Counties |
Low Risk Counties |
|
| Per Capita Opioid Prescription |
|
|
|
|
| Drug Type |
|
|
|
|
| All opioids |
57625 (17154) |
58974 (16736) |
57250 (17295) |
0.5243 |
| Natural & Semi Synthetic |
52439 (1550) |
51060(13906) |
52774(16426) |
0.4769 |
| Fentanyl |
1295 (539) |
1465 (603) |
1248 (512) |
0.0233 |
| Prescriber Location |
|
|
|
|
| In State Doctors |
52604 (17500) |
51427 (20002) |
52932 (16787) |
0.6282 |
| Out State Doctors |
5020 (5127) |
7547 (6698) |
4319 (4367) |
0.0020 |
| Dispenser Type |
|
|
|
|
| Retail |
16356 (9372) |
17915 (9823) |
15923 (9224) |
0.2029 |
| Chain |
32796 (132389) |
32713 (9559) |
32819 (14114) |
0.9505 |
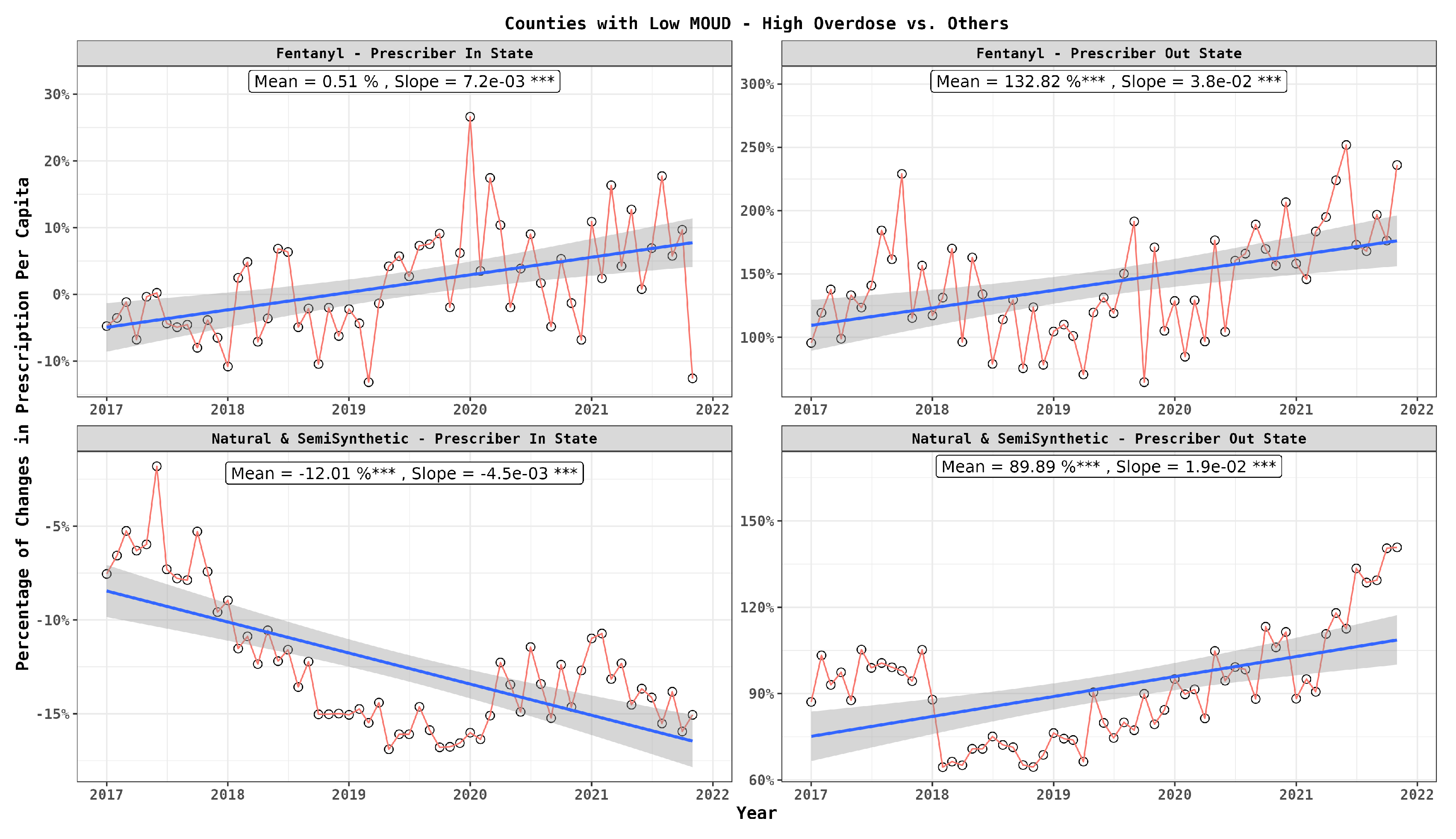
Next, we considered time and the interaction between each pair of characteristics listed in
Table 3. To come up with a metric that applies to both high-risk and low-risk counties, we calculated what we call the "Differential Percentage." This metric captures the difference in average per capita prescriptions between high-risk and low-risk areas, normalized by the average per capita prescription in low-risk areas and multiplied by 100.
3.2.1. Opioid Type and Prescriber Location
In
Figure 3, each point represents the Differential Percentage, as defined in the previous section, for fentanyl prescriptions obtained from in-state and out-of-state doctors. In each subplot, we also provide two indicators: the mean and the slope. The mean reflects the average of the Differential Percentage, with its significance determined through a t-test. The slope indicates the coefficient in a linear regression, offering insight into whether the differential percentage is increasing or decreasing over time. This figure illustrates a higher prevalence of opioid prescriptions, particularly fentanyl, in high-risk counties from out-of-state prescribers, aligning with insights from
Table 3. This figure denotes a rising trend for fentanyl in high-risk regions over time. In contrast, natural and semi-synthetic opioids reveal a similar trend only when prescribed by out-of-state practitioners.
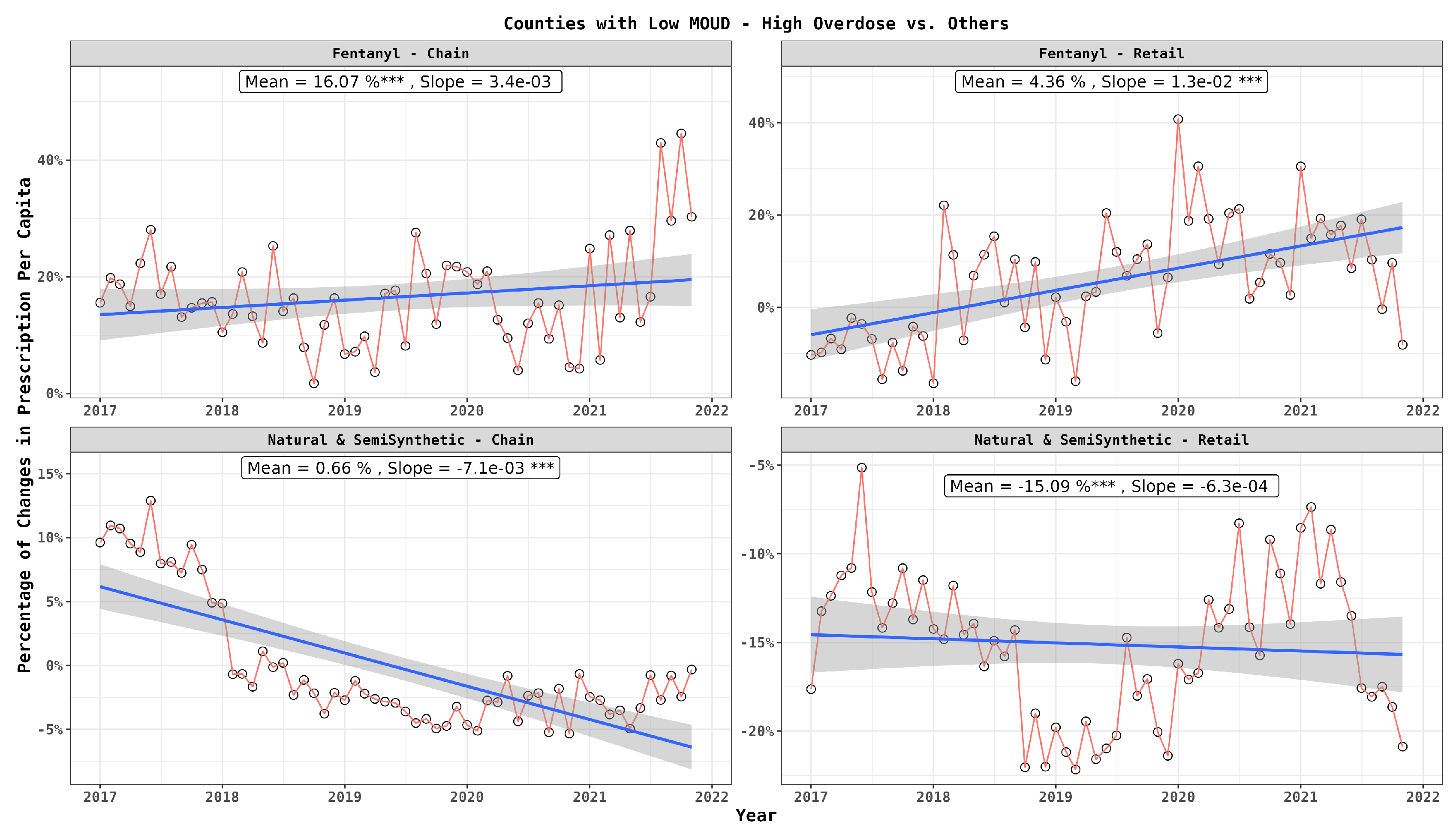
3.2.2. Opioid Type and Pharmacy Type
Analyzing the influence of pharmacy type,
Figure 4 underscores the augmented dispensation of fentanyl in high-risk areas by both chain and retail pharmacies, with the role of chain pharmacies being more crucial. In contrast, for natural and semi-synthetic opioids, a reduced dispensation is observable in high-risk areas by both pharmacy types, with chain pharmacies uniquely exhibiting a declining trend, indicating a receding dependency on them for such drugs.
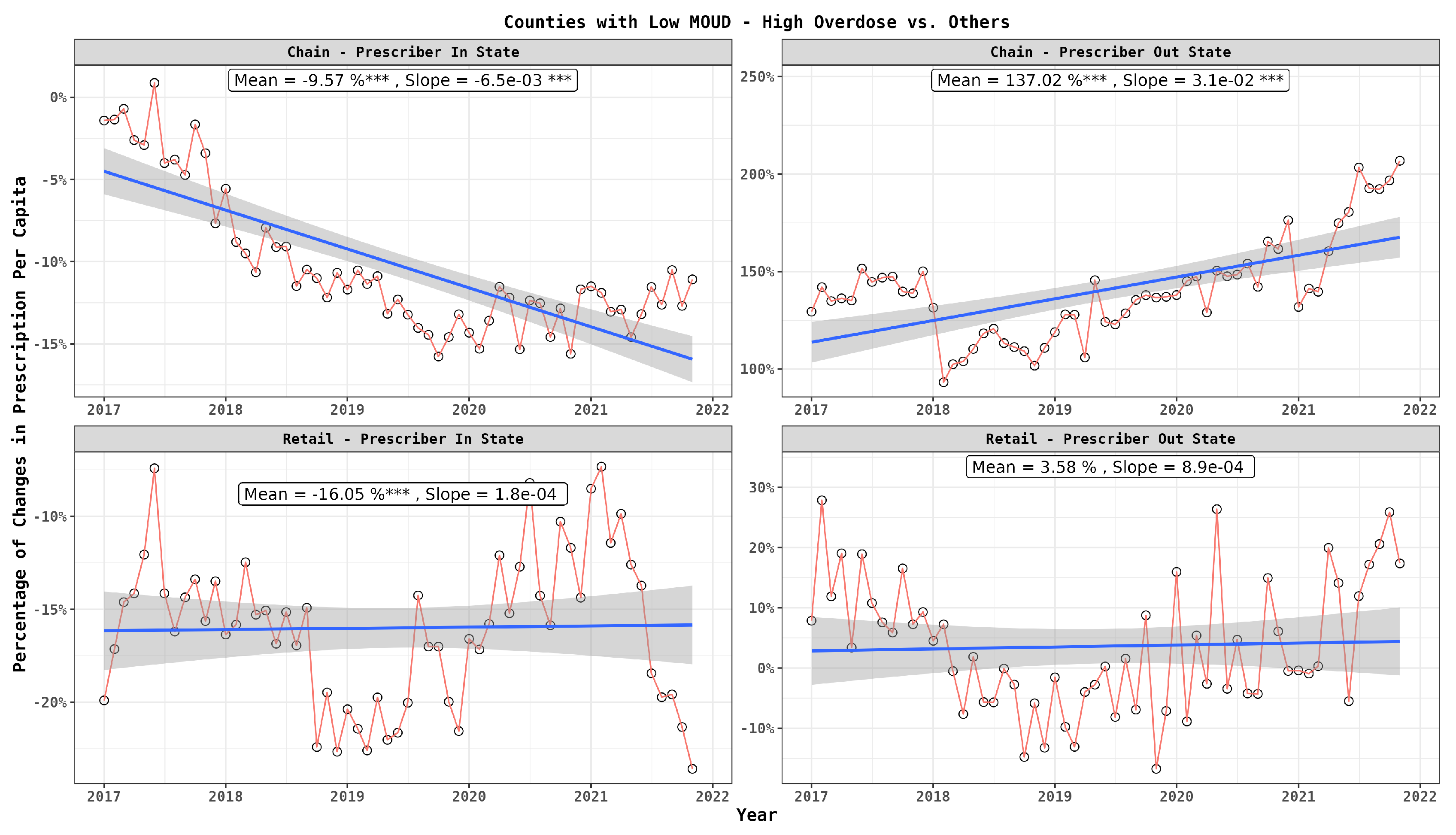
3.2.3. Pharmacy Type and Prescriber Location
Incorporating prescriber location,
Figure 5 reveals an interesting dynamic; chain pharmacies are notably accommodating more prescriptions from out-of-state doctors, while retail pharmacies maintain a more steady approach. Notably, there is a discernible decline in prescriptions from in-state doctors, primarily seen in chain pharmacies.
3.2.4. Multifactorial Analysis
Figure 6 depicts how the percentage difference in per capita prescriptions between low and high-risk counties change over time (calculated on a monthly basis) with respect to drug type and prescriber location. The results reaffirm the pronounced preference of high-risk patients for out-of-state doctors and the prominent role of chain pharmacies in filling such prescriptions, especially for fentanyl, displaying an escalating trend over time. In contrast, retail pharmacies maintain a stable approach, primarily with fentanyl prescriptions from out-of-state doctors. Additionally, there is a marginal inclination for acquiring fentanyl from in-state doctors irrespective of pharmacy type; however, this upward trajectory is significantly noticeable in retail pharmacies. Meanwhile, for natural and semi-synthetic opioids prescribed by in-state doctors, a decreasing trend is more visible, notably in chain pharmacies.
Our analysis demonstrates that high-risk counties have a growing predilection for fentanyl, notably from out-of-state prescribers, and chain pharmacies are increasingly central to this pattern. While retail pharmacies exhibit a more balanced and consistent behavior across different opioids and prescriber locations, the overall multifactorial analysis elucidates nuanced trends and preferences in opioid prescriptions in high-risk counties.
3.2.5. Impact of Health Infrastructure Accessibility
Throughout our study, we have extensively examined legal prescription data, and identified distinctions between high and low-risk counties in South Carolina, with high-risk counties characterized by below-average access to medications for Opioid Use Disorder (OUD) and above-average overdose rates.
A pivotal finding is the prevalent tendency of individuals in high-risk counties to consult with out-of-state doctors, likely attributed to the insufficient and fragile health infrastructure in these regions. This is corroborated by lower availability of medications for OUD and lower MD density, with the state average being 161.45 doctors per 100,000 residents. In high-risk areas, this number dwindles to 137.36, while in low-risk areas, it increases to 167.31. The associated P-value of 0.0440 signifies a statistically significant disparity in MD density between high and low-risk areas.
Additionally, our analysis suggests doctor shopping may be more prevalent in high-risk counties, predominantly involving out-of-state doctors. On average, there are 80.89 instances of per capita doctor shopping out-of-state, but in high-risk counties, this figure significantly surges to 90.92, while in low-risk counties, it is approximately 78.45, with a p-value of 0.006 confirming a statistically significant difference. Lastly, it is crucial to acknowledge that not all overdoses are attributed to prescribed medications; a substantial part is due to illegal supplies, a facet not considered in this analysis.
Figure 3.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, prescriber location
Figure 3.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, prescriber location
Figure 4.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, dispenser type
Figure 4.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, dispenser type
Figure 5.
Monthly per capita prescription differences among patients in high risk and low risk counties: dispenser type, prescriber location
Figure 5.
Monthly per capita prescription differences among patients in high risk and low risk counties: dispenser type, prescriber location
Figure 6.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, dispenser type, prescriber location
Figure 6.
Monthly per capita prescription differences among patients in high risk and low risk counties: drug type, dispenser type, prescriber location
4. Discussion
Our research delves into the multifaceted nature of South Carolina’s opioid crisis using data spanning from 2017 to 2021. Consistent with prior studies, we observe a decline in opioid prescriptions statewide; however, there has been a notable increase in opioid-related overdose deaths [
46]. Of particular concern is the rise in fatalities associated with fentanyl, a potent synthetic opioid. While fentanyl is prescribed less frequently compared to natural and semi-synthetic opioids like hydrocodone, oxycodone, and methadone, its associated fatalities have significantly risen. This surge in deaths linked to synthetic opioids, primarily fentanyl and its analogs, alongside methamphetamine, marks what has been termed the "fourth wave" of the opioid crisis [
47]. Our study reveals that between 2017 and 2021, opioid prescriptions decreased from 64,223 to 41,214 per 100,000 residents, while fentanyl-related overdose deaths increased by 312%. High-risk counties exhibited notably higher rates of fentanyl prescriptions and relied more on out-of-state doctors. Additionally, they demonstrated elevated instances of doctor shopping, fewer medical doctors per capita, and limited access to MOUD. To effectively address the opioid crisis, we advocate for enhanced local healthcare infrastructure, expanded treatment access, tighter management of out-of-state prescriptions, and meticulous tracking of prescription patterns. Tailored local strategies are vital for mitigating the opioid epidemic in these communities.
Examining the situation at the county level introduces additional layers of complexity, confirming earlier observations [
48]. High-risk counties are distinctive in the manner in which opioids are sourced and consumed. A notable difference is the increase in prescriptions originating from out-of-state physicians. This increasing trend suggests that individuals are expanding their networks beyond state lines to obtain opioids. The weaker health systems and a shortage of doctors in high-risk counties likely play a role in this reliance on out-of-state prescribers. There is an urgent need to strengthen the health care systems in these high-risk counties, making health care services more available and reducing the reliance on external prescribers.
Our findings also suggest the possibility of unauthorized activities like doctor shopping. This behavior calls for actions that extend beyond the boundaries of South Carolina. Supported by our previous studies, these out-of-state resources often exhibit more lenient regulations, introducing an additional layer of risk [
29,
30]. Furthermore, the presence or absence of MOUD is key to understanding these supply trends. The restricted access to MOUD in high-risk counties, even when people are ready to seek treatment, underscores the imbalance between supply and demand in treatment options, potentially escalating the opioid issue (see [
26]).
Regarding pharmacies, the prominent role of chain pharmacies in filling fentanyl prescriptions from out-of-state sources and the consistent rate at retail pharmacies underscore the significance of pharmacy chains in these regions. As this trend is only apparent for fentanyl and not for natural and semi-synthetic drugs, it necessitates closer scrutiny and enhanced regulations on synthetic opioids in high-risk areas. Strengthening local regulations could be a quicker solution compared to expanding health infrastructure. This trend contradicts previous findings suggesting a decrease in opioid distribution when an independent pharmacy becomes part of a chain [
49].
Our study does have its limitations. The absence of patient-level data prevents us from drawing firm conclusions regarding the occurrence and specifics of Opioid Use Disorder (OUD). Additionally, the lack of data on illegal drug supply hampers our comprehensive understanding of the opioid issue, given the study focuses solely on legal prescriptions.
5. Conclusion
In summary, our study reveals a complex landscape of opioid use in South Carolina from 2017 to 2021. Despite a statewide decrease in opioid prescriptions, overdose fatalities—particularly from fentanyl—have surged. High-risk counties, distinguished by limited access to MOUD, exhibit unique trends: a greater percentage of fentanyl prescriptions and a significant reliance on out-of-state doctors for opioid prescriptions. This raises concerns about the efficacy of state-level interventions alone and suggests the need for broader, possibly national, strategies to address the crisis, focusing not just on regulating the supply but also on improving MOUD accessibility.
Author Contributions
A.S.-F. and A.H.S.: Conceptualization, Methodology, Data curation, Statistical Analysis, Writing—original draft, Visualization. R.H.: Resources, Conceptualization, Writing—review and editing. E.K.-Z.: Methodology Validation, Conceptualization, Resources, Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval are not applicable (due to use of a de-identified dataset).
Informed Consent Statement
Not applicable.
Acknowledgments
We thank our colleagues from Supply Chain Resource Cooperative (SCRC) at North Carolina State University who provided insight and expertise that greatly assisted the research, although they may not agree with all of the interpretations/conclusions of this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Soelberg, C.D.; Brown, R.E.; Du Vivier, D.; Meyer, J.E.; Ramachandran, B.K. The US opioid crisis: current federal and state legal issues. Anesthesia & Analgesia 2017, 125, 1675–1681. [CrossRef]
- Kiang, M.V.; Basu, S.; Chen, J.; Alexander, M.J. Assessment of changes in the geographical distribution of opioid-related mortality across the United States by opioid type, 1999-2016. JAMA network open 2019, 2, e190040–e190040. [CrossRef]
- Ciccarone, D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Current opinion in psychiatry 2021, 34, 344. [CrossRef]
- Salmond, S.; Allread, V. A population health approach to America’s opioid epidemic. Orthopedic nursing 2019, 38, 95. [CrossRef]
- Dydyk, A.M.; Jain, N.K.; Gupta, M. Opioid use disorder. In StatPearls [Internet]; StatPearls Publishing, 2022.
- Ahmad, F.B.; Rossen, L.M.; Sutton, P. Provisional drug overdose death counts. National center for health statistics 2021, 12.
- Lee, B.; Zhao, W.; Yang, K.C.; Ahn, Y.Y.; Perry, B.L. Systematic evaluation of state policy interventions targeting the US opioid epidemic, 2007-2018. JAMA network open 2021, 4, e2036687–e2036687. [CrossRef]
- Howard, R.; Waljee, J.; Brummett, C.; Englesbe, M.; Lee, J. Reduction in opioid prescribing through evidence-based prescribing guidelines. JAMA surgery 2018, 153, 285–287. [CrossRef]
- Chen, Q.; Larochelle, M.R.; Weaver, D.T.; Lietz, A.P.; Mueller, P.P.; Mercaldo, S.; Wakeman, S.E.; Freedberg, K.A.; Raphel, T.J.; Knudsen, A.B.; et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA network open 2019, 2, e187621–e187621. [CrossRef]
- Abouk, R.; Pacula, R.L.; Powell, D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA internal medicine 2019, 179, 805–811. [CrossRef]
- Donroe, J.H.; Socias, M.E.; Marshall, B.D. The deepening opioid crisis in North America: historical context and current solutions. Current Addiction Reports 2018, 5, 454–463. [CrossRef]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC clinical practice guideline for prescribing opioids for pain—United States, 2022. MMWR Recommendations and Reports 2022, 71, 1. [CrossRef]
- Blanco, C.; Volkow, N.D. Management of opioid use disorder in the USA: present status and future directions. The Lancet 2019, 393, 1760–1772. [CrossRef]
- Levin, F.R.; Bisaga, A.; Sullivan, M.A.; Williams, A.R.; Cates-Wessel, K. A review of a national training initiative to increase provider use of MAT to address the opioid epidemic. The American journal on addictions 2016, 25, 603–609. [CrossRef]
- Mauro, P.M.; Gutkind, S.; Annunziato, E.M.; Samples, H. Use of medication for opioid use disorder among US adolescents and adults with need for opioid treatment, 2019. JAMA network open 2022, 5, e223821–e223821. [CrossRef]
- Strang, J.; Volkow, N.D.; Degenhardt, L.; Hickman, M.; Johnson, K.; Koob, G.F.; Marshall, B.D.; Tyndall, M.; Walsh, S.L. Opioid use disorder. Nature reviews Disease primers 2020, 6, 3. [CrossRef]
- Wakeman, S.E.; Larochelle, M.R.; Ameli, O.; Chaisson, C.E.; McPheeters, J.T.; Crown, W.H.; Azocar, F.; Sanghavi, D.M. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA network open 2020, 3, e1920622–e1920622. [CrossRef]
- Krawczyk, N.; Rivera, B.D.; Jent, V.; Keyes, K.M.; Jones, C.M.; Cerdá, M. Has the treatment gap for opioid use disorder narrowed in the US?: A yearly assessment from 2010 to 2019”. International Journal of Drug Policy 2022, 110, 103786. [CrossRef]
- Cantor, J.; Powell, D.; Kofner, A.; Stein, B.D. Population-based estimates of geographic accessibility of medication for opioid use disorder by substance use disorder treatment facilities from 2014 to 2020. Drug and alcohol dependence 2021, 229, 109107. [CrossRef]
- Mitchell, P.; Samsel, S.; Curtin, K.M.; Price, A.; Turner, D.; Tramp, R.; Hudnall, M.; Parton, J.; Lewis, D. Geographic disparities in access to Medication for Opioid Use Disorder across US census tracts based on treatment utilization behavior. Social Science & Medicine 2022, 302, 114992. [CrossRef]
- Tabatabai, M.; Cooper, R.L.; Wilus, D.M.; Edgerton, R.D.; Ramesh, A.; MacMaster, S.A.; Patel, P.N.; Singh, K.P. The Effect of Naloxone Access Laws on Fatal Synthetic Opioid Overdose Fatality Rates. Journal of Primary Care & Community Health 2023, 14, 21501319221147246. [CrossRef]
- Andrilla, C.H.A.; Moore, T.E.; Patterson, D.G.; Larson, E.H. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. The Journal of Rural Health 2019, 35, 108–112. [CrossRef]
- Jones, C.W.; Christman, Z.; Smith, C.M.; Safferman, M.R.; Salzman, M.; Baston, K.; Haroz, R. Comparison between buprenorphine provider availability and opioid deaths among US counties. Journal of substance abuse treatment 2018, 93, 19–25. [CrossRef]
- Krawczyk, N.; Jent, V.; Hadland, S.E.; Cerdá, M. Utilization of medications for opioid use disorder across US states: relationship to treatment availability and overdose mortality. Journal of Addiction Medicine 2022, 16, 114–117. [CrossRef]
- Corry, B.; Underwood, N.; Cremer, L.J.; Rooks-Peck, C.R.; Jones, C. County-level sociodemographic differences in availability of two medications for opioid use disorder: United States, 2019. Drug and Alcohol Dependence 2022, 236, 109495. [CrossRef]
- Haffajee, R.L.; Lin, L.A.; Bohnert, A.S.; Goldstick, J.E. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA network open 2019, 2, e196373–e196373. [CrossRef]
- Fink, D.S.; Keyes, K.M.; Branas, C.; Cerdá, M.; Gruenwald, P.; Hasin, D. Understanding the differential effect of local socio-economic conditions on the relation between prescription opioid supply and drug overdose deaths in US counties. Addiction 2023. [CrossRef]
- Sadeghi, A.; Sahebi-fakhrabad, A.; Handfield, R. The Effect of Opioid Legislation on Supply Chain Stakeholders’ Behavior: South Carolina Case Study.
- Sahebi-Fakhrabad, A.; Sadeghi, A.H.; Handfield, R. Evaluating state-level prescription drug monitoring program (PDMP) and pill mill effects on opioid consumption in pharmaceutical supply chain. In Proceedings of the Healthcare. MDPI, 2023, Vol. 11, p. 437. [CrossRef]
- Sahebi-Fakhrabad, A.; Sadeghi, A.H.; Kemahlioglu-Ziya, E.; Handfield, R.; Tohidi, H.; Vasheghani-Farahani, I. The Impact of Opioid Prescribing Limits on Drug Usage in South Carolina: A Novel Geospatial and Time Series Data Analysis. In Proceedings of the Healthcare. MDPI, 2023, Vol. 11, p. 1132. [CrossRef]
- South Carolina Department of Health and Environmental Control. Drug Overdose Deaths - South Carolina 2017, 2017. Accessed: Novermber 11, 2022. Available at: https://scdhec.gov/sites/default/files/media/document/Drug%20Overdose%20Deaths%20-%20South%20Carolina%202017.pdf.
- South Carolina Department of Health and Environmental Control. Drug Overdose Deaths - South Carolina 2018, 2018. Accessed: Novermber 11, 2022. Available at: https://scdhec.gov/sites/default/files/media/document/SC-drug-overdose-report-2018.pdf.
- South Carolina Department of Health and Environmental Control. Drug Overdose Deaths - South Carolina 2019, 2019. Accessed: Novermber 11, 2022. Available at: https://scdhec.gov/sites/default/files/media/document/2019_South_Carolina_Drug_Overdose_Deaths.pdf.
- South Carolina Department of Health and Environmental Control. Drug Overdose Deaths - South Carolina 2020, 2020. Accessed: Novermber 11, 2022. Available at: https://scdhec.gov/sites/default/files/media/document/Drug%20overdose%20report_2020_V1.pdf.
- South Carolina Department of Health and Environmental Control. Drug Overdose Deaths - South Carolina 2021, 2021. Accessed: Novermber 11, 2022. Available at: https://scdhec.gov/sites/default/files/media/document/Drug%20Overdose%20Deaths%20-%20South%20Carolina%202021.pdf.
- Rudd, R.A.; Seth, P.; David, F.; Scholl, L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morbidity and mortality weekly report 2016, 65, 1445–1452.
- Substance Abuse and Mental Health Services Administration. Opioid Treatment Program Directory, 2021. Accessed: Januray 15, 2022. Available at: https://dpt2.samhsa.gov/treatment/directory.aspx.
- Substance Abuse and Mental Health Services Administration. Buprenorphine Practitioner Locator, 2021. Accessed: Januray 20, 2022. Available at: https://www.samhsa.gov/medication-assisted-treatment/find-treatment/treatment-practitioner-locator.
- Alkermes Inc. Vivitrol. Find a Treatment Provider, 2021. Accessed: Januray 20, 2022. Available at: https://www.vivitrol.com/opioid-dependence/find-a-provider.
- Sansone, R.A.; Sansone, L.A. Doctor shopping: a phenomenon of many themes. Innovations in clinical neuroscience 2012, 9, 42.
- Hall, A.J.; Logan, J.E.; Toblin, R.L.; Kaplan, J.A.; Kraner, J.C.; Bixler, D.; Crosby, A.E.; Paulozzi, L.J. Patterns of abuse among unintentional pharmaceutical overdose fatalities. Jama 2008, 300, 2613–2620. [CrossRef]
- Peirce, G.L.; Smith, M.J.; Abate, M.A.; Halverson, J. Doctor and pharmacy shopping for controlled substances. Medical care 2012, pp. 494–500.
- Dhalla, I.A.; Mamdani, M.M.; Sivilotti, M.L.; Kopp, A.; Qureshi, O.; Juurlink, D.N. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. Cmaj 2009, 181, 891–896. [CrossRef]
- Biernikiewicz, M.; Taieb, V.; Toumi, M. Characteristics of doctor-shoppers: a systematic literature review. Journal of market access & health policy 2019, 7, 1595953. [CrossRef]
- Delcher, C.; Bae, J.; Wang, Y.; Doung, M.; Fink, D.S.; Young, H.W. Defining “Doctor Shopping” with Dispensing Data: A Scoping Review. Pain Medicine 2022, 23, 1323–1332. [CrossRef]
- Ball, S.J.; Simpson, K.; Zhang, J.; Marsden, J.; Heidari, K.; Moran, W.P.; Mauldin, P.D.; McCauley, J.L. High-Risk Opioid Prescribing Trends: Prescription Drug Monitoring Program Data from 2010–2018. Journal of public health management and practice: JPHMP 2021, 27, 379. [CrossRef]
- Han, B.; Einstein, E.B.; Jones, C.M.; Cotto, J.; Compton, W.M.; Volkow, N.D. Racial and ethnic disparities in drug overdose deaths in the US during the COVID-19 pandemic. JAMA network open 2022, 5, e2232314–e2232314. [CrossRef]
- Romeiser, J.L.; Labriola, J.; Meliker, J.R. Geographic patterns of prescription opioids and opioid overdose deaths in New York State, 2013-2015. Drug and alcohol dependence 2019, 195, 94–100. [CrossRef]
- Janssen, A.; Zhang, X. Retail pharmacies and drug diversion during the opioid epidemic. American Economic Review 2023, 113, 1–33.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).