1. Introduction
Nutritional research currently focuses on dietary patterns rather than individual nutrients or foods [
1]. The Mediterranean diet (MD) is the most well-known and researched dietary pattern worldwide. It is characterized by the consumption of a wide variety of foods, such as extra virgin olive oil, legumes, cereals, nuts, fruits, vegetables, dairy, fish and wine [
2]. Many of these foods provide various phytonutrients, among which polyphenols and vitamins play an important role. It is currently one of the healthiest dietary patterns, mainly due to its antioxidant and anti-inflammatory effects 5/13/24 [
1,
3,
4]. Numerous studies, systematic reviews, and meta-analyses have established the protective effects of the Mediterranean diet against several chronic diseases, including diabetes, obesity, cardiovascular disease, cancer, aging disorders, and overall mortality [
1,
2,
4,
5,
6,
7,
8,
9,
10,
11,
12]. All this is related to a better lipid profile, lower blood pressure (BP), blood sugar and obesity [
4,
13].
Metabolic syndrome (MetS) is made up of multiple risk factors for atherosclerosis, including obesity, high BP, elevated fasting plasma glucose (FPG), and atherogenic dyslipidemia [
14]. MetS has become a major health problem in the world. Its prevalence is rising due to the increase in the consumption of fast food (high in calories and low in fiber) and the decrease in physical activity resulting from mechanized transport and sedentary activities during leisure time [
15]. MetS doubles the risk of morbidity and mortality from cardiovascular disease and multiplies the risk of all-cause mortality by 1.5 times [
16,
17,
18].
Healthy lifestyle factors, such as physical activity and MD, decrease the likelihood of developing MetS. Thus, a recent study showed that participants with higher MetS followed a pro-inflammatory dietary pattern and tended to have lower adherence to DM, showing lower intake of carbohydrates and nuts and higher intake of proteins, saturated fatty acids, cholesterol, red and processed meat products, and oils other than olive oil [
19]
However, the effect of MD on the prevalence of this disease and each of its components is not fully established in the Caucasian population. For this reason, this study has the following objectives: first, to investigate the relationship of MD with MetS and its components in Caucasian subjects between 35 and 74 years; second, to analyze sex differences.
2. Materials and Methods
2.1. Design
A descriptive cross-sectional study was carried out with data from the EVA study [
20] (NCT02623894), the MARK study [
21] (NCT01428934) and EVIDENT study [
22] (NCT0108308).
2.2. Study Population
All studies were conducted in primary care, involving a total of 3471 subjects between the ages of 35 and 75 who had recorded all the variables necessary to carry out this study. Specifically, the following were included: 491 of the 501 subjects recruited in the EVA study [
20], selected by random sampling from the urban population without cardiovascular disease (reference population 43,946), 2330 of the 2475 subjects recruited in the MARK study [
21], selected by random sampling among the subjects consulted in 7 urban health centers and with inert cardiovascular risk, and 650 subjects from the EVIDENT study [
22], selected by random sampling among the subjects consulted in a primary care center.
A detailed description of the methodology of the studies, as well as the inclusion and exclusion criteria, can be found in the protocols of the three studies [
20,
21,
22].
2.3. Variables and Measuring Instruments
2.3.1. Adherence to the Mediterranean Diet
Adherence to the MD was evaluated with a 14-item questionnaire, validated in Spain and used in the PREDIMED study [
23]. The questionnaire includes 12 questions on the frequency of food consumption and two questions on typical eating habits of the Spanish population. Each question was rated with zero or one point. One point was given for: use of olive oil as the main fat for cooking, daily consumption of four or more tablespoons (one tablespoon = 13.5 g) of olive oil (including oil used for frying, salad dressing, etc.), two or more servings of vegetables, three or more pieces of fruit, less than one serving of red or processed meat, less than one serving of animal fat, less than one cup (one cup = 100 ml) of carbonated beverages or sugar, and intake of white meat to a greater extent than red meat. A point was also given for the weekly consumption of seven or more glasses of wine, three or more servings of legumes, three or more servings of fish, three or more servings of nuts or dried fruit, two or more servings of sofrito (a traditional sauce made with tomato, garlic, onion or leeks and sautéed with olive oil), and less than two baked goods. The final score range was from 0 to 14 points, with scores above the median (7) being considered as adherence to the Mediterranean diet [
23].
2.3.2. Diagnostic Criteria of Metabolic Syndrome
According to the international consensus in the Joint Scientific Statement National Cholesterol Education Program III [
14], MetS was defined as the presence of three or more of the following five components: waist circumference (WC) ≥88 cm in women and ≥102 cm in men); elevated triglycerides (TGC) ≥150 mg/dL (or drug treatment for elevated TGC); high-density lipoprotein (HDL) cholesterol <40 mg/dL in men or <50 mg/dL in women; high blood pressure (systolic blood pressure (SBP) ≥130 mmHg or diastolic blood pressure (DBP) ≥85 mmHg, or antihypertensive drug treatment), and fasting plasma glucose (FPG) ≥100 mg/dL (or drug treatment for elevated glucose).
2.3.3. Anthropometric Measurements and Cardiovascular Risk Factors
Body weight was determined on two occasions using a homologated electronic scale (Seca 770; Medical scale and measurement systems, Birmingham, United Kingdom) following due calibration (precision ± 0.1 kg), with the patient wearing light clothing and shoeless. These readings were rounded to 100 g. Height in turn was measured with a portable system (Seca 222; Medical scale and measurement systems, Birmingham, United Kingdom), recording the average of two readings, and with the patient shoeless in the standing position. The values were rounded to the nearest centimeter. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Waist circumference was measured according to the 2007 recommendations of the Spanish Society for the Study of Obesity [
24].
Office blood pressure measurement involved three measurements of systolic blood pressure (SBP) and diastolic blood pressure (DBP), using the average of the last two, with a validated OMRON model M10-IT sphygmomanometer (Omron Health Care, Kyoto, Japan), by following the recommendations of the European Society of Hypertension [
25]. Subjects were considered to have hypertension if they were taking antihypertensive drugs or had blood pressure values ≥140/90 mmHg; to have diabetes if taking hypoglycaemic agents or with fasting plasma glucose ≥126 mg/dl or HbA1c ≥6.5%; to have dyslipidaemia if taking lipid-lowering drugs or with fasting total cholesterol ≥240 mg/dl, low density lipoprotein cholesterol (LDL-c) ≥160 mg/dl, high density lipoprotein cholesterol (HDL-c) <40 mg/dl in men and <50 mg/dl in women, or triglycerides ≥150 mg/dl. A value of BMI ≥30 kg/m2 was used to define obesity [
26].
2.4. Statistical Analysis
Data are presented using means ± standard deviations and numbers or percentages according to whether they are continuous or categorical variables. The comparison between men and women was performed using chi-square tests for percentages and Student’s t for continuous variables. The Pearson correlation was used to analyze the relationship between continuous variables.
To analyze the association between average score value of MD and the number of MetS components and with each of the MetS components, seven multiple linear regression models were performed (ENTER method) using MD as the independent variable and the number of MetS components, SBP in mmHg, DBP in mmHg, FPG in mg/dl, Triglycerides in mg/dl, HDL cholesterol in mg/dl and WC in cm as dependent variables.
To analyze the association between adherence to the Mediterranean diet and the presence of MetS and each of its components, we used six logistic regression models. MD adherence was the independent variable (encoded as MD adherence = 1, MD non-adherence = 0. MetS components were the dependent variables (encoded as yes = 1, no = 0), BP ≥130/85 mmHg (yes = 1, no = 0), FPG ≥100 mg/dL (yes = 1, no = 0), TGC ≥150 mg/dL (yes = 1, no = 0), HDL-C mg/dL <40 in men, <50 mg/dL in women (yes = 1, no = 0), and WC ≥88 cm in women, ≥102 cm in men (yes = 1, no = 0). All models included the adjustment variables of age, sex, and consumption of antihypertensive drugs, hypoglycemic and lipid-lowering agents.
All analyses were performed globally and by sex. The SPSS Statistics program for Windows, version 28.0 (IBM Corp, Armonk, NY, USA) was used. We considered a value of p <0.05 as a statistical significance limit.
2.5. Ethical Principles
The research protocols for the studies incorporated into this pooled analysis were duly approved by the Drug Research Ethics Committee of Salamanca, with registration numbers PI15/01039 and PI20/10569 (EVA study [
20]), PI10/02043 (MARK study [
21]), and PI83/06/2018 (EVIDENT study [
22]). All subjects participating in these studies provided written informed consent. During the development of the study, the standards of the Declaration of Helsinki [
27] and the WHO standards for observational studies were followed. The confidentiality of the subjects included was always guaranteed in accordance with the provisions of Organic Law 3/2018, of 5 December, on Personal Data Protection and guarantee of digital rights and Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on Data Protection (RGPD).
3. Results
3.1. Demographic and Clinical Characteristics of the Included Subjects
The characteristics, cardiovascular risk factors, and drug use are described globally and by sex in
Table 1. The mean age was 60.14 ± 9.77 years, with no differences observed between sexes (p=0.543). Men made up a greater proportion of the sample (57%), and showed higher BP, LDL cholesterol, TGC, FPG and WC values than women. Women had higher total cholesterol and HDL cholesterol values than men.
3.2. Mediterranean Diet and Metabolic Syndrome
Table 1 shows the values for Mediterranean diet and MetS. The mean value of the total MD score was 5.83 ± 2.04 (women 6.04 ± 1.99, men 6.67 ± 2.06). The adherence to MD percentage was 36.8% (women 40.3%, men 34.3). The percentage of subjects with MetS was 41.6% (women 45.2%, men 39.0%) and the mean number of MetS components was 2.28±1.33 (women 2.33±1.44, men 2.24±1.25). When analyzing each of the components, women had a higher percentage of WC (69.3 vs 48.6) and HDL_C (37.2 vs 21.9) and a lower percentage of FPG (34.2 vs 40.6), BP (68.0 vs 80.2) and TGC (24.1 vs 32.6) than men.
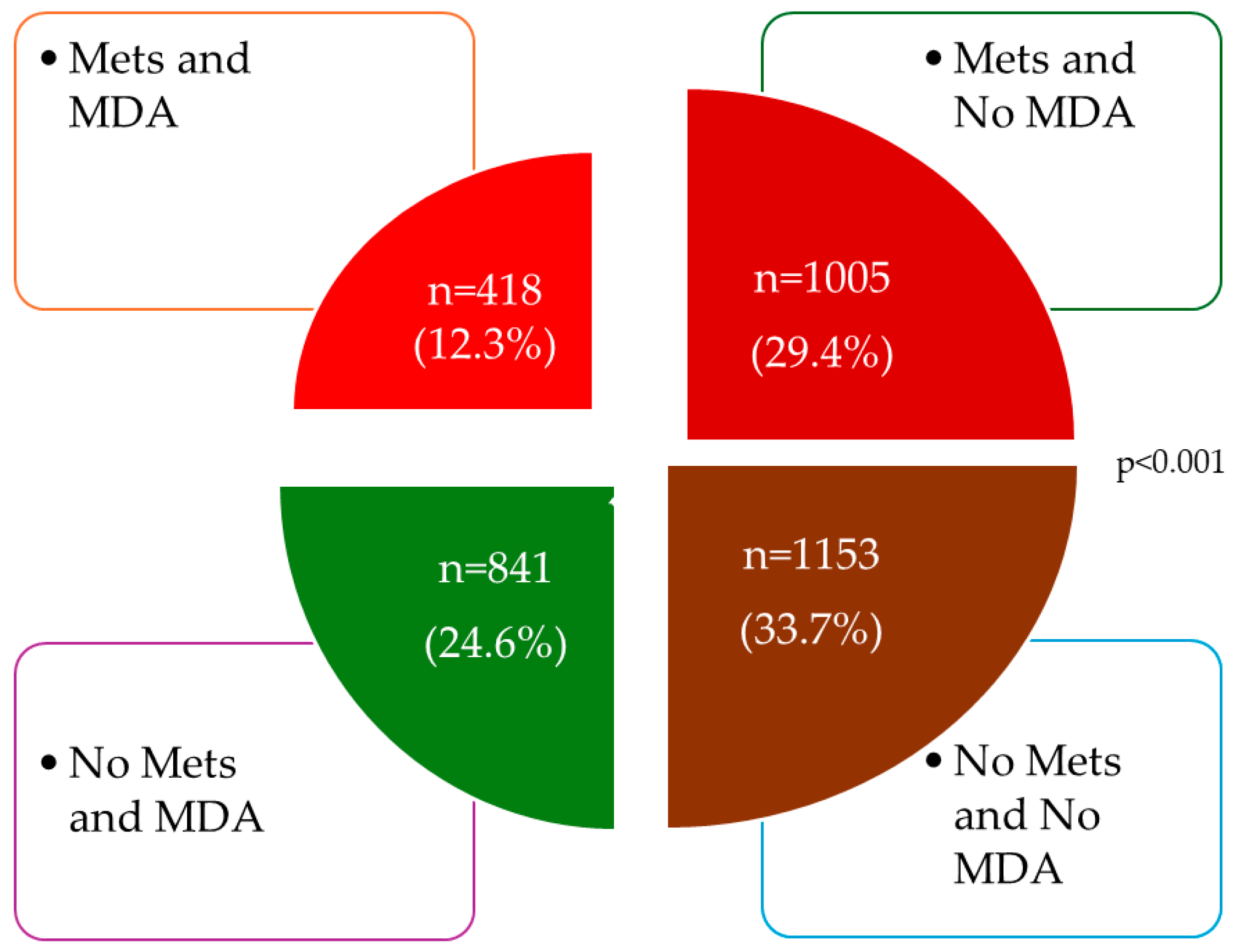
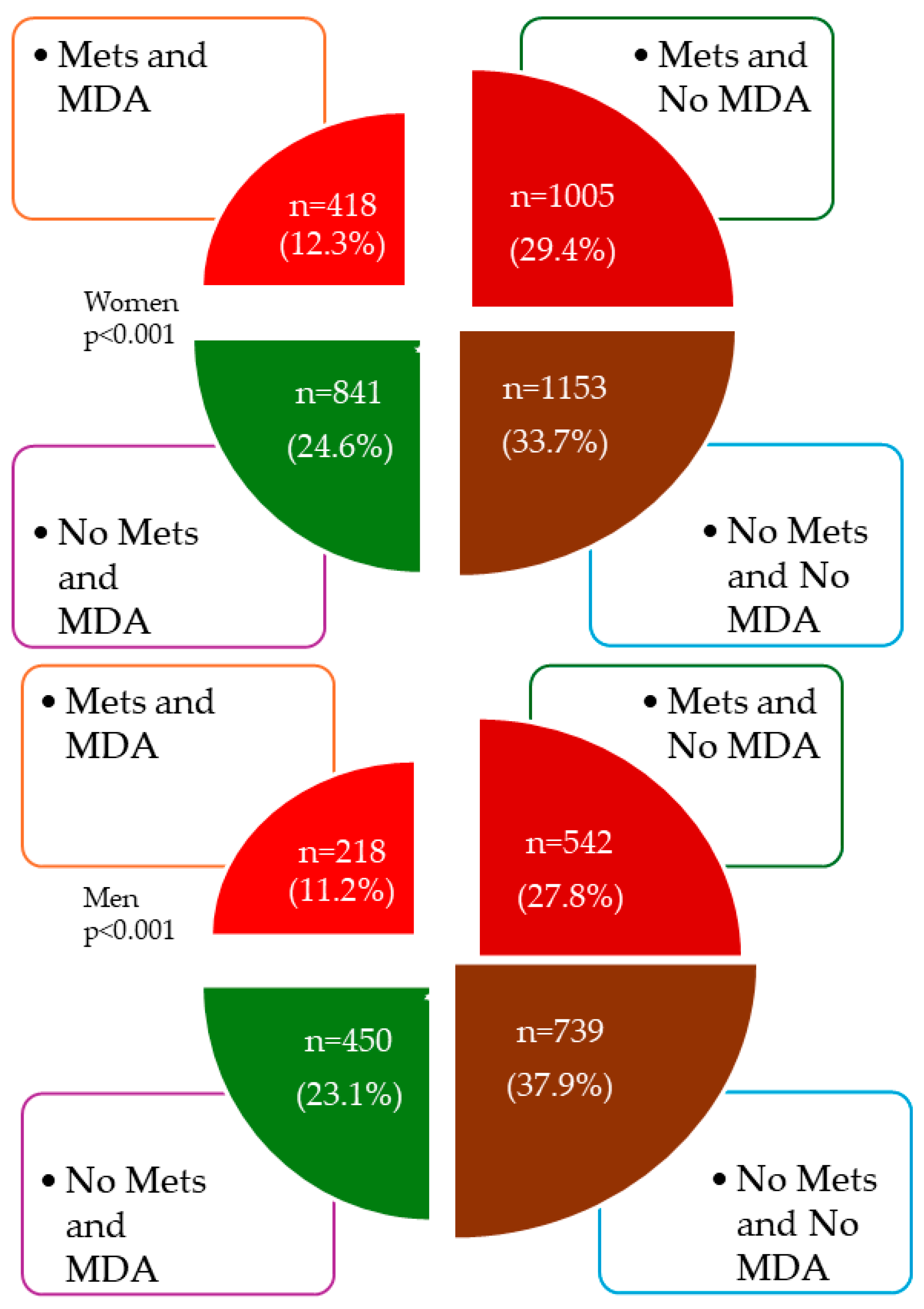
Figure 1 shows the overall distribution of subjects according to whether they have MetS or adherence to MD, and
Figure 2 shows the distribution by sex.
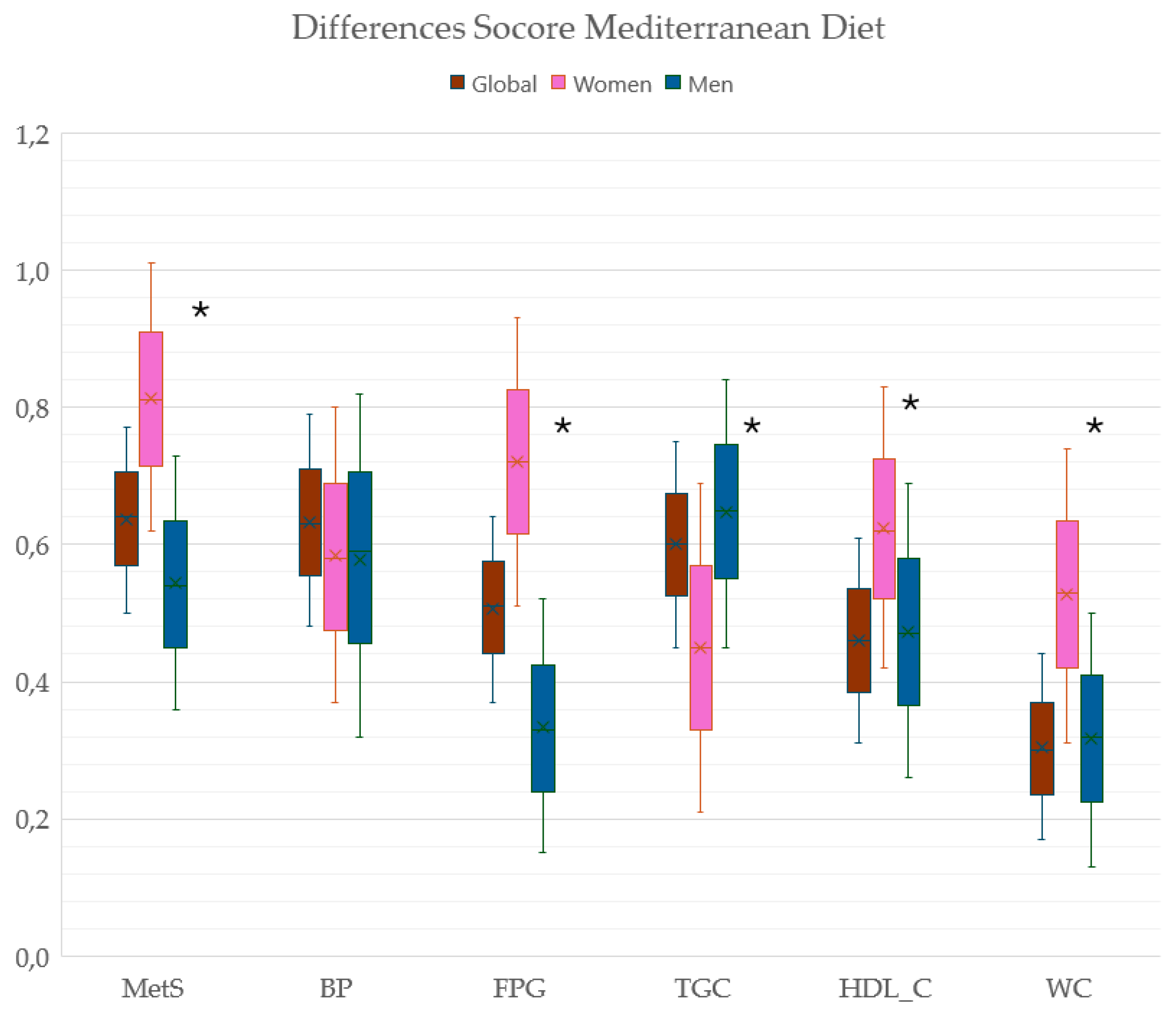
Figure 3 shows the difference in the mean value of the MD score between subjects with and without MetS and without each of the components of MetS and with MetS overall and by sex. In MetS, FPG, HDL_C and WC components, the difference was greater in women and in TGC the difference was greater in men (p<0.05).
3.3. Correlation between the Mediterranean Diet and MetS and Its Components
The mean value of MD showed a negative correlation with the number of MetS components r=-0.196 (women r=-0.220; men r=-0.185), and with all MetS components in the overall analysis and by sex, except for HDL_C, which showed a positive correlation r=0.171 (women r=0.179; men r=0.130) (
Table 2).
3.4. Association between Adherence to the Mediterranean Diet and MetS and Its Components
In the multiple regression analysis after adjusting for possible confounders, the mean value of MD showed a negative association with the number of MetS components (β=-0.336, 95% CI -0.393 to -0.280), and with the different MetS components: SBP (β=-0.011, 95% CI -0.015 to -0.008), DBP (β=-0.029, 95% CI -0.035 to -0.022), FPG (β=-0.009, 95% CI -0.012 to -0.006), TGC (β=-0.004, 95% CI -0.004 to -0.003), WC (β=-0.026, 95% CI -0.032 to -0.020), except with the HDL-cholesterol value which showed a positive association (β=0.021, 95% CI 0.018 to 0.028). The results by sex were similar (
Table 3).
Table 4 shows the results of the logistic regression analysis overall and by sex. The adjusted logistic regression models showed that an increase in MD adherence decreases the probability of MetS (OR =0.555, 95% CI 0.477 to 0.650) and its components: BP ≥130/85 mmHg (OR = 0.634, 95% CI 0.522 to 0.771), FPG ≥100 mg/dL (OR = 0.615, 95% CI 0.511 to 0.740); TGC ≥150 mg/dL (OR = 0.641, 95% CI 0.546 to 0.753); WC ≥88 cm in women and ≥102 cm in men (OR = 0.741, 95% CI 0.639 to 0.859), and increases HDL cholesterol <40 mg/dL in men or <50 mg/dL in women (OR = 1.700), 95% CI 1.442 to 2.005 (p<0.001 in all cases). The results by sex were similar.
4. Discussion
The results of this study carried out in 3417 Caucasian subjects show that approximately 4 out of 6 people have MetS and adherence to MD, with a differing ratio between the sexes. While the percentage of men with MetS is higher than in women, the percentage of MD adherence is higher in women than in men, which contrasts with other studies [
28,
29,
30,
31]. The percentage of each of the components of the MetS varied according to sex. The presence of MetS and all components showed an association with MD overall and by sex.
The prevalence of MetS in this study was 41% (45% in men and 39% in women) and is higher than that found in other studies conducted in Spain. Thus, in the ENRICA study [
30], which included 11149 representatives individuals of the Spanish population aged over 18 years, the prevalence in the 45-64 age group was 31% (36% men and 25% women), and increased with age and in the communities of southern Spain. In the DARIOS study [
31], which included 24,670 people aged between 35 and 74 years from 10 autonomous communities, the prevalence of MetS was 31% (32% in men and 29% in women). In the same vein, the prevalence of MetS was higher than in the United States: 34% (36% in men and 32% in women) [
32]. When analyzing each of the components, as well as the results found in this study, the percentage of fasting plasma glucose ≥100 mg/dL and TGC ≥150 mg/dL was higher in men. The percentage of subjects with HDL-C <40 mg/dL in men, <50 mg/dL in women and WC ≥88 cm in women, ≥102 cm in men was higher in women. There is considerable variation in prevalence depending on the geographical area, age, sex, level of education, degree of obesity and the definition used for diagnosis [
30,
31,
33]. Therefore, these data are not directly comparable because they correspond to different age groups, and subjects from the different studies had different characteristics; in our case a significant percentage of those from the MARK study [
21] were subjects with intermediate cardiovascular risk, while those from the EVIDENT [
22] study were selected by random sampling among the subjects consulted, and subjects from a population-based sample were only included in the EVA study [
20]. Moreover, while the ENRICA study [
30] included subjects from all over Spain over 18 years of age, the DARIOS study [
31] only included data from 10 autonomous communities and from subjects aged between 35-75 years.
However, there are fewer data in longitudinal studies on the effect of MD on the incidence of MetS. Some longitudinal studies have examined the importance of Mediterranean lifestyles, as measured with the adherence to the Mediterranean lifestyle (MEDLIFE) questionnaire. A 5-year follow-up of the subjects included in the CORDIOPREV study showed that those with greater adherence to the Mediterranean lifestyle had a lower incidence of MetS (odds ratio 0.37; 95% CI: 0.19-0.75) and a higher probability of reversing MetS (odds ratio 2.08; 95% CI 1.11-3.91) compared to participants in the low adherence group of MEDLIFE [
34]. Similarly, with the cohort of the ENRICA study at 8.7 years of follow-up, assessing the Mediterranean lifestyle with the MEDLIFE index showed that greater adherence to it was associated with a lower incidence of MetS [
35]. The MEDLIFE index, representing the Mediterranean lifestyle, includes food consumption as well as other dietary habits and healthy behaviors (living together, eating in company, rest and social habits) characteristic of traditional Mediterranean culture and supports the importance of cultural habits, beyond mere eating habits, as strong determinants of health. The aforementioned studies did not evaluate the isolated effects of each item but rather the joint, and possibly synergistic, effect of the combination of several behaviors related to traditional Mediterranean culture. For this reason, prospective studies are needed to specifically analyze the effect of adherence to MD on MetS.
In this study, we found an association between the variables that define MD and MetS as continuous variables (in multiple regression analysis) and categorical variables (in logistic regression analysis). This association differs from that found in other studies, so a study conducted on 1,404 adults in Luxembourg only found a significant association between MD and MetS when used as a continuous score, based on the weighting of the compounds by exploratory factor analysis with MetS, but not when used as categorical variables [
36]. However, the PREDIMED-PLUS study that included 5739 overweight/obese participants with MetS characteristics (aged 55 to 75 years) showed that participants with MetS tended to have lower adherence to MD [
19]. In the study carried out by Hassani, S et al. [
37], adherence to MD was not associated with MetS, presenting an association only with fasting blood glucose (OR: 0.57, CI: 0.33-0.97) and abdominal obesity (OR: 0.42, CI: 0.20-0.87) in women. In 1972, Greek schoolchildren aged 9 to 13 years with a logistic regression analysis revealed that “poor” adherence to MD was associated with an increased likelihood of central obesity (OR 1.31; 95% CI: 1.01-1.73) and hypertriglyceridemia (OR 2.80; 95% CI: 1.05-7.46), after adjusting for several possible confounders [
38]. Finally, a meta-analysis that included 58 studies and analyzed the relationship between adherence to MD and the components of MetS found that WC β= -0.20, (95% CI: -0.40, -0.01) and TGC β= -0.27 (95% CI: -0.27, -0.11) were lower and HDL-C β=-0.28 (95% CI: 0.07, 0.50) was higher in the group with high adherence to MD without finding an association with FBG and BP [
39].
In summary, high adherence to MD can have a positive impact on MetS parameters. However, this may vary from one component to another, probably explained by the heterogeneity in the studies in terms of subjects included, analyses performed, associated pathologies or concomitant treatments. More research is therefore needed in this field.
Limitations and Strengths
This study has a number of limitations and strengths. The main limitation is the analysis of cross-sectional data, which prevents us from establishing causality. Another limitation is that the people included in the analysis come from three studies with very different characteristics, including the largest number of subjects in the MARK study (MetS). Among the strengths of the study are the size of the sample and the fact that all the criteria that define MetS, such as anthropometry and blood pressure, were carried out under standardized conditions and with validated devices. In addition, all analytical measurements were performed in laboratories with adequate quality controls.
5. Conclusions
The results of this study suggest that greater adherence to the Mediterranean diet decreases the probability of presenting MetS and each of its components globally and by sex. This suggests the need to improve adherence to the Mediterranean diet in primary health care in order to reduce the prevalence of MetS and the health problems it causes.
Author Contributions
Conceptualization, M.A.G.-M. and L.G.-S.; methodology, M.A.G.-M. G.O.-L and M.G.-S.; formal analysis, M.A.G.-M. and L.G.-O.; investigation, L.G.-S., M.G.-S., C.L.-S., O.T.-M., S.G.-S. and M.Ll.-R.; data curation, M.A.G.-M., E.R.-S., and M.L.-R.; writing—original draft preparation, L.G.-S. and M.G.-S.; writing—review and editing, project administration, M.A.G.-M., L.G.-O and M.Ll.-R.; funding acquisition, M.A.G.-M; L.G.-O and M.Ll.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by this project was financed by the Carlos III Health Institute of the Ministry of Health of Spain (FIS:PI13/00618, PI13/01526, PI13/00058, PI13/01635, PI13/02528, PI12/01474, (PI10/01088, PI10/02077, PI10/02043). Regional Health Management of the Junta de Castilla y León through research projects (GRS 1193/B/15; GRS2303/B/21); the Instituto de Salud Carlos III (ISCIII) of the Ministry of Science and Innovation, through RD21/0016/0010 (Red de Investigación en Cronicidad, Atención Primaria y Promoción de la Salud (RICAPPS), which is funded by the European Union-Next Generation EU. Facility for Recovery and Resilience (MRR) and PI21/00454 was co-funded by the European Union and also contributed to the funding of the project. Human resources were also obtained from the research programme of the Junta de Castilla y León (INT/M/02/17 and INT/M/04/15), the Instituto de Investigación Biomedico de Salamanca (IBSAL) (IBI21/00001), and the Instituto de Salud Carlos III (INT22/00007). None of them played any role in the study design, data analysis, reporting results, or the decision to submit the manuscript for publication.
Informed Consent Statement
This project was approved by the ethics committee for research with medicines of the health area of Salamanca, the baseline assessment dated on 4 May 2015, and the follow-up assessment on 13 November 2020 (CEIm reference code. PI 2020 10 569). Before the start of the study, all participants signed the informed consent form. The standards of the Declaration of Helsinki were followed during the conduct of the study [
31] and the WHO standards for observational studies were followed. Subjects were informed of the aims of the project and the risks and benefits of the examinations performed. The study did not contemplate any intervention involving a risk greater than the minimal risk involved in performing the different tests. All information generated in this study was stored, coded, and used exclusively for the purposes specified here. Both the samples and the data collected are associated with a code, kept under appropriate security conditions, and it is guaranteed that the subjects cannot be identified through means considered reasonable by persons other than those authorized. The confidentiality of the subjects included has been guaranteed at all times in accordance with the provisions of Organic Law 3/2018, of 5 December, on the Protection of Personal Data and guarantee of digital rights and Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on Data Protection (RGPD).
Data Availability Statement
The variables used in the analyses carried out to obtain the results of this work are available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Martini, D. Health Benefits of Mediterranean Diet. Nutrients 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Román, G.C.; Jackson, R.E.; Reis, J.; Román, A.N.; Toledo, J.B.; Toledo, E. Extra-virgin olive oil for potential prevention of Alzheimer disease. Rev Neurol (Paris) 2019, 175, 705–723. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Martinez-Gonzalez, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med 2014, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2019, 3, Cd009825. [Google Scholar] [CrossRef] [PubMed]
- Kiani, A.K.; Medori, M.C.; Bonetti, G.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Stuppia, L.; Connelly, S.T.; Herbst, K.L.; et al. Modern vision of the Mediterranean diet. J Prev Med Hyg 2022, 63, E36–E43. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Veronese, N.; Di Bella, G.; Cusumano, C.; Parisi, A.; Tagliaferri, F.; Ciriminna, S.; Barbagallo, M. Mediterranean diet in the management and prevention of obesity. Exp Gerontol 2023, 174, 112121. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Kaddoumi, A.; Denney, T.S., Jr.; Deshpande, G.; Robinson, J.L.; Beyers, R.J.; Redden, D.T.; Praticò, D.; Kyriakides, T.C.; Lu, B.; Kirby, A.N.; et al. Extra-Virgin Olive Oil Enhances the Blood-Brain Barrier Function in Mild Cognitive Impairment: A Randomized Controlled Trial. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style Diet for the Primary and Secondary Prevention of Cardiovascular Disease: A Cochrane Review. Glob Heart 2020, 15, 56. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Di Bella, G.; Veronese, N.; Barbagallo, M. Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity. Nutrients 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Mazza, E.; Ferro, Y.; Pujia, R.; Mare, R.; Maurotti, S.; Montalcini, T.; Pujia, A. Mediterranean Diet In Healthy Aging. J Nutr Health Aging 2021, 25, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2019, 3, CD009825. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed]
- Kotani, K.; Satoh-Asahara, N.; Nakakuki, T.; Yamakage, H.; Shimatsu, A.; Tsukahara, T. Association between metabolic syndrome and multiple lesions of intracranial atherothrombotic stroke: a hospital-based study. Cardiovasc Diabetol 2015, 14, 108. [Google Scholar] [CrossRef]
- Jiang, B.; Li, B.; Wang, Y.; Han, B.; Wang, N.; Li, Q.; Yang, W.; Huang, G.; Wang, J.; Chen, Y.; et al. The nine-year changes of the incidence and characteristics of metabolic syndrome in China: longitudinal comparisons of the two cross-sectional surveys in a newly formed urban community. Cardiovasc Diabetol 2016, 15, 84. [Google Scholar] [CrossRef]
- Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Mascaró, C.M.; Montemayor, S.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; et al. Leisure-Time Physical Activity, Sedentary Behaviour and Diet Quality are Associated with Metabolic Syndrome Severity: The PREDIMED-Plus Study. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Gomez-Marcos, M.A.; Martinez-Salgado, C.; Gonzalez-Sarmiento, R.; Hernandez-Rivas, J.M.; Sanchez-Fernandez, P.L.; Recio-Rodriguez, J.I.; Rodriguez-Sanchez, E.; García-Ortiz, L. Association between different risk factors and vascular accelerated ageing (EVA study): study protocol for a cross-sectional, descriptive observational study. BMJ Open 2016, 6, e011031. [Google Scholar] [CrossRef]
- Martí, R.; Parramon, D.; García-Ortiz, L.; Rigo, F.; Gómez-Marcos, M.A.; Sempere, I.; García-Regalado, N.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Feuerbach, N.; et al. Improving interMediAte risk management. MARK study. BMC Cardiovasc Disord 2011, 11, 61. [Google Scholar] [CrossRef]
- Recio-Rodríguez, J.I.; Martín-Cantera, C.; González-Viejo, N.; Gómez-Arranz, A.; Arietaleanizbeascoa, M.S.; Schmolling-Guinovart, Y.; Maderuelo-Fernandez, J.A.; Pérez-Arechaederra, D.; Rodriguez-Sanchez, E.; Gómez-Marcos, M.A.; et al. Effectiveness of a smartphone application for improving healthy lifestyles, a randomized clinical trial (EVIDENT II): study protocol. BMC Public Health 2014, 14, 254. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama 2013, 310, 2191–2194. [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Rubio, M.A.; Barbany, M.; Moreno, B. [SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria]. Med Clin (Barc) 2007, 128, 184–196, quiz 181 p following 200. [Google Scholar] [CrossRef]
- O’Brien, E.; Asmar, R.; Beilin, L.; Imai, Y.; Mancia, G.; Mengden, T.; Myers, M.; Padfield, P.; Palatini, P.; Parati, G.; et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005, 23, 697–701. [Google Scholar] [CrossRef]
- 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013, 31, 1925–1938. [CrossRef]
- GómezSánchez, M.; Gómez Sánchez, L.; Patino-Alonso, M.C.; Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Lugones-Sánchez, C.; Rodríguez Sánchez, E.; García Ortiz, L.; Gómez-Marcos, M.A. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Caparello, G.; Galluccio, A.; Giordano, C.; Lofaro, D.; Barone, I.; Morelli, C.; Sisci, D.; Catalano, S.; Andò, S.; Bonofiglio, D. Adherence to the Mediterranean diet pattern among university staff: a cross-sectional web-based epidemiological study in Southern Italy. Int J Food Sci Nutr 2020, 71, 581–592. [Google Scholar] [CrossRef]
- Guallar-Castillón, P.; Pérez, R.F.; López García, E.; León-Muñoz, L.M.; Aguilera, M.T.; Graciani, A.; Gutiérrez-Fisac, J.L.; Banegas, J.R.; Rodríguez-Artalejo, F. Magnitude and management of metabolic syndrome in Spain in 2008-2010: the ENRICA study. Rev Esp Cardiol (Engl Ed) 2014, 67, 367–373. [Google Scholar] [CrossRef]
- Fernández-Bergés, D.; Cabrera de León, A.; Sanz, H.; Elosua, R.; Guembe, M.J.; Alzamora, M.; Vega-Alonso, T.; Félix-Redondo, F.J.; Ortiz-Marrón, H.; Rigo, F.; et al. Metabolic syndrome in Spain: prevalence and coronary risk associated with harmonized definition and WHO proposal. DARIOS study. Rev Esp Cardiol (Engl Ed) 2012, 65, 241–248. [Google Scholar] [CrossRef]
- Ford, E.S.; Li, C.; Zhao, G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes 2010, 2, 180–193. [Google Scholar] [CrossRef]
- Alipour, P.; Azizi, Z.; Raparelli, V.; Norris, C.M.; Kautzky-Willer, A.; Kublickiene, K.; Herrero, M.T.; Emam, K.E.; Vollenweider, P.; Preisig, M.; et al. Role of sex and gender-related variables in development of metabolic syndrome: A prospective cohort study. Eur J Intern Med 2024, 121, 63–75. [Google Scholar] [CrossRef]
- Romero-Cabrera, J.L.; García-Ríos, A.; Sotos-Prieto, M.; Quintana-Navarro, G.; Alcalá-Díaz, J.F.; Martín-Piedra, L.; Torres-Peña, J.D.; Luque, R.M.; Yubero-Serrano, E.M.; Delgado-Lista, J.; et al. Adherence to a Mediterranean lifestyle improves metabolic status in coronary heart disease patients: A prospective analysis from the CORDIOPREV study. J Intern Med 2023, 293, 574–588. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Ortolá, R.; Ruiz-Canela, M.; Garcia-Esquinas, E.; Martínez-Gómez, D.; Lopez-Garcia, E.; Martínez-González, M.; Rodriguez-Artalejo, F. Association between the Mediterranean lifestyle, metabolic syndrome and mortality: a whole-country cohort in Spain. Cardiovasc Diabetol 2021, 20, 5. [Google Scholar] [CrossRef]
- Al Kudsee, K.; Vahid, F.; Bohn, T. High adherence to the Mediterranean diet and Alternative Healthy Eating Index are associated with reduced odds of metabolic syndrome and its components in participants of the ORISCAV-LUX2 study. Front Nutr 2022, 9, 1087985. [Google Scholar] [CrossRef]
- Hassani Zadeh, S.; Salehi-Abargouei, A.; Mirzaei, M.; Nadjarzadeh, A.; Hosseinzadeh, M. The association between dietary approaches to stop hypertension diet and mediterranean diet with metabolic syndrome in a large sample of Iranian adults: YaHS and TAMYZ Studies. Food Sci Nutr 2021, 9, 3932–3941. [Google Scholar] [CrossRef]
- George, E.S.; Gavrili, S.; Itsiopoulos, C.; Manios, Y.; Moschonis, G. Poor adherence to the Mediterranean diet is associated with increased likelihood of metabolic syndrome components in children: the Healthy Growth Study. Public Health Nutr 2021, 24, 2823–2833. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Chrysoula, L.; Kotzakioulafi, E.; Theodoridis, X.; Chourdakis, M. Impact of the Level of Adherence to Mediterranean Diet on the Parameters of Metabolic Syndrome: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2021, 13. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).