Submitted:
17 May 2024
Posted:
20 May 2024
You are already at the latest version
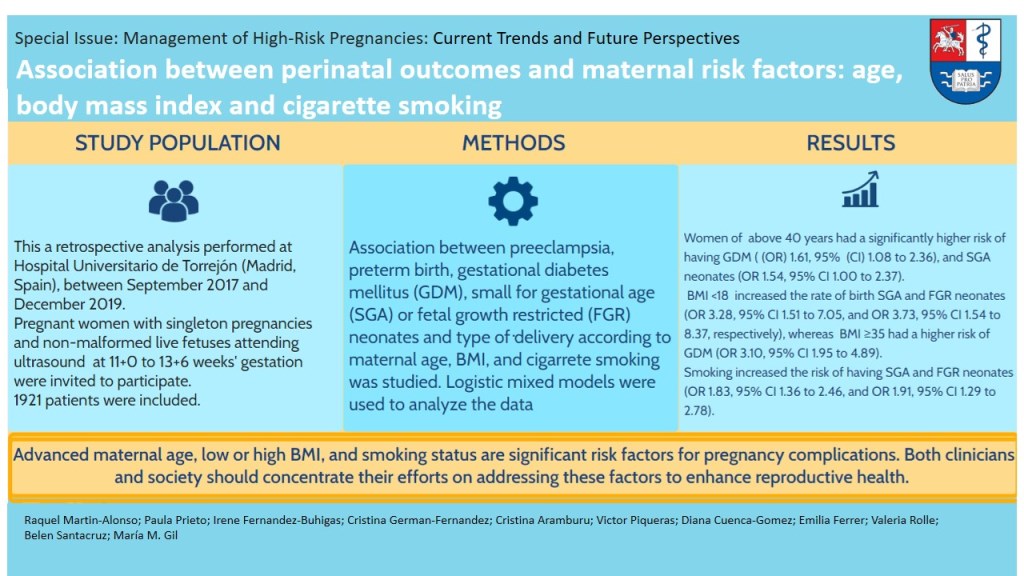
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Pregnancy Outcomes
2.3. Statistical Analysis
3. Results
3.1. Study Population and Pregnancy Outcomes
3.2. Risk Factors for Pregnancy Complications
3.2.1. Maternal Age
3.2.2. Body Mass Index
3.1.3. Smoking
4. Discussion
4.1. Main Findings of the Study
4.2. Comparison with Previous Studies
4.3. Clinical Implications
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tarasi, B.; Cornuz, J.; Clair, C.; Baud, D. Cigarette smoking during pregnancy and adverse perinatal outcomes: a cross-sectional study over 10 years. BMC Public Health. 2022, 22, 2403. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.; Voerman, E.; Amiano, P.; Barros, H.; Beilin, L.J.; Bergström, A.; et al. Impact of maternal body mass index and gestational weight gain on pregnancy complications: an individual participant data meta-analysis of European, North American and Australian cohorts. BJOG Int J Obstet Gynaecol. 2019, 126, 984–995. [Google Scholar] [CrossRef]
- Nakanishi, K.; Saijo, Y.; Yoshioka, E.; Sato, Y.; Kato, Y.; Nagaya, K.; et al. Severity of low pre-pregnancy body mass index and perinatal outcomes: the Japan Environment and Children’s Study. BMC Pregnancy Childbirth. 2022, 22, 121. [Google Scholar] [CrossRef] [PubMed]
- Ko, T.J.; Tsai, L.Y.; Chu, L.C.; Yeh, S.J.; Leung, C.; Chen, C.Y.; et al. Parental Smoking During Pregnancy and Its Association with Low Birth Weight, Small for Gestational Age, and Preterm Birth Offspring: A Birth Cohort Study. Pediatr Neonatol. 2014, 55, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, R.L.; Areia, A.L.; Mota Pinto, A.; Donato, H. Advanced Maternal Age: Adverse Outcomes of Pregnancy, A Meta-Analysis. Acta Médica Port. 2019, 32, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.A.; Hamilton, B.E.; Osterman, M.J.K.; Driscoll, A.K. Births: Final Data for 2019. Natl Vital Stat Rep Cent Dis Control Prev Natl Cent Health Stat Natl Vital Stat Syst. 2021, 70, 1–51. [Google Scholar]
- World Health Organization. Regional Office for Europe. (2008). Atlas of health in Europe: 2nd edition 2008, 2nd ed. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/107365.
- Cnattingius, S.; Forman, M.R.; Berendes, H.W.; Isotalo, L. Delayed childbearing and risk of adverse perinatal outcome. A population-based study. JAMA 1992, 268, 886–890. [Google Scholar] [CrossRef]
- Aldous, M.B.; Edmonson, M.B. Maternal age at first childbirth and risk of low birth weight and preterm delivery in Washington State. JAMA 1993, 270, 2574–2577. [Google Scholar] [CrossRef]
- Cleary-Goldman, J.; Malone, F.D.; Vidaver, J.; Ball, R.H.; Nyberg, D.A.; Comstock, C.H.; et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005, 105, 983–990. [Google Scholar] [CrossRef]
- Khalil, A.; Syngelaki, A.; Maiz, N.; Zinevich, Y.; Nicolaides, K.H. Maternal age and adverse pregnancy outcome: a cohort study: Maternal age and pregnancy complications. Ultrasound Obstet Gynecol. 2013, 42, 634–643. [Google Scholar] [CrossRef]
- Bianco, A.; Stone, J.; Lynch, L.; Lapinski, R.; Berkowitz, G.; Berkowitz, R.L. Pregnancy outcome at age 40 and older. Obstet Gynecol. 1996, 87, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Smithson, S.D.; Greene, N.H.; Esakoff, T.F. Pregnancy outcomes in very advanced maternal age women. Am J Obstet Gynecol 2022, 4, 100491. [Google Scholar] [CrossRef] [PubMed]
- Waldenström, U.; Ekéus, C. Risk of labor dystocia increases with maternal age irrespective of parity: a population-based register study. Acta Obstet Gynecol Scand. 2017, 96, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Callaway, L.K.; Lust, K.; McIntyre, H.D. Pregnancy outcomes in women of very advanced maternal age. Aust N Z J Obstet Gynaecol. 2005, 45, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Edge, V.; Laros, R.K. Pregnancy outcome in nulliparous women aged 35 or older. Am J Obstet Gynecol. 1993, 168, 1881–1884. [Google Scholar] [CrossRef] [PubMed]
- Bayrampour, H.; Heaman, M. Advanced maternal age and the risk of cesarean birth: a systematic review. Birth Berkeley Calif. 2010, 37, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalán, C.; Uauy, R.; Herring, S.; et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016, 4, 1025–1036. [Google Scholar] [CrossRef] [PubMed]
- Ehrenberg, H.M.; Dierker, L.; Milluzzi, C.; Mercer, B.M. Prevalence of maternal obesity in an urban center. Am J Obstet Gynecol. 2002, 187, 1189–1193. [Google Scholar] [CrossRef]
- Sebire, N.J.; Jolly, M.; Harris, J.P.; Wadsworth, J.; Joffe, M.; Beard, R.W.; et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2001, 25, 1175–1182. [Google Scholar] [CrossRef]
- Chu, S.Y.; Callaghan, W.M.; Kim, S.Y.; Schmid, C.H.; Lau, J.; England, L.J.; et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care. 2007, 30, 2070–2076. [Google Scholar] [CrossRef]
- Álvarez Cuenod, J.S.; Sánchez Sánchez, V.; González Martín, J.M.; Emergui Zrihen, Y.; Suarez Guillén, V.; Ribary Domingo, A.; et al. Valores extremos del IMC materno: factores determinantes de peores resultados obstétricos y perinatales. Clínica E Investig En Ginecol Obstet. 2022, 49, 100754. [Google Scholar] [CrossRef]
- McDonald, S.D.; Han, Z.; Mulla, S.; Beyene, J.; Knowledge Synthesis Group. Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta-analyses. BMJ. 2010, 341, c3428. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Aucott, L.S.; Gurung, T.; Smith, W.C.S.; Bhattacharya, S. Obesity as an independent risk factor for elective and emergency caesarean delivery in nulliparous women - systematic review and meta-analysis of cohort studies. Obes Rev. 2009, 10, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Ramsay, J.E.; Ferrell, W.R.; Crawford, L.; Wallace, A.M.; Greer, I.A.; Sattar, N. Maternal obesity is associated with dysregulation of metabolic, vascular, and inflammatory pathways. J Clin Endocrinol Metab. 2002, 87, 4231–4237. [Google Scholar] [CrossRef]
- Delhaes, F.; Giza, S.A.; Koreman, T.; Eastabrook, G.; McKenzie, C.A.; Bedell, S.; et al. Altered maternal and placental lipid metabolism and fetal fat development in obesity: Current knowledge and advances in non-invasive assessment. Placenta 2018, 69, 118–124. [Google Scholar] [CrossRef]
- Han, Z.; Mulla, S.; Beyene, J.; Liao, G.; McDonald, S.D.; Knowledge Synthesis Group. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. 2011, 40, 65–101. [Google Scholar] [CrossRef]
- Liu, P.; Xu, L.; Wang, Y.; Zhang, Y.; Du, Y.; Sun, Y.; et al. Association between perinatal outcomes and maternal pre-pregnancy body mass index. Obes Rev Off J Int Assoc Study Obes. 2016, 17, 1091–1102. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Li, L.; Chen, W.; Liu, Z.B.; Ma, L.; Gao, X.X.; et al. Pre-pregnancy underweight and obesity are positively associated with small-for-gestational-age infants in a Chinese population. Sci Rep. 2019, 9, 15544. [Google Scholar] [CrossRef]
- Rahman, M.M.; Abe, S.K.; Kanda, M.; Narita, S.; Rahman, M.S.; Bilano, V.; et al. Maternal body mass index and risk of birth and maternal health outcomes in low- and middle-income countries: a systematic review and meta-analysis: Body mass index and pregnancy and health outcomes. Obes Rev. 2015, 16, 758–770. [Google Scholar] [CrossRef]
- Banderali, G.; Martelli, A.; Landi, M.; Moretti, F.; Betti, F.; Radaelli, G.; et al. Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. J Transl Med. 2015, 13, 327. [Google Scholar] [CrossRef]
- England, L.; Zhang, J. Smoking and risk of preeclampsia: a systematic review. Front Biosci J Virtual Libr. 2007, 12, 2471–2483. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yang, W.; Xiao, W.; Cao, S. The association between smoking during pregnancy and hypertensive disorders of pregnancy: A systematic review and meta-analysis. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2022, 157, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Gómez, D.; de Paco Matallana, C.; Rolle, V.; Valiño, N.; Revello, R.; Adiego, B.; Mendoza, M.; Molina, F.S.; Carrillo, M.P.; Delgado, J.L.; Wright, A.; Santacruz, B.; Gil, M.M. Performance of first-trimester combined screening for preterm pre-eclampsia: findings from cohort of 10 110 pregnancies in Spain. Ultrasound Obstet Gynecol. 2023, 62, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013, 122, 1122–1131. [Google Scholar]
- Documento de consenso. Asistencia a la gestante con diabetes. Guía práctica clínica actualizada en 2014. Grupo Español de Diabetes y Embarazo (GEDE). Av Diabetol 2015, 31, 45–59. [Google Scholar]
- Nicolaides, K.H.; Wright, D.; Syngelaki, A.; Wright, A.; Akolekar, R. Fetal Medicine Foundation fetal and neonatal population weight charts. Ultrasound Obstet Gynecol. 2018, 52, 44–51. [Google Scholar] [CrossRef] [PubMed]
- [R Core Team (2023). _R: A Language and Environment for Statistical Computing_. R Foundation for Statistical Computing, Vienna, Austria. <https://www.R-project.org/>.].
- Rich B (2023). _table1: Tables of Descriptive Statistics in HTML_. R package version 1.4.3, <https://CRAN.R-project.org/package=table1>.
- Lüdecke D (2023). _sjPlot: Data Visualization for Statistics in Social Science_. R package version 2.8.14, .
- Fulop, T.; Larbi, A.; Douziech, N. Insulin receptor and ageing. Pathol Biol. 2003, 51, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Szoke, E.; Shrayyef, M.Z.; Messing, S.; Woerle, H.J.; Van Haeften, T.W.; Meyer, C.; et al. Effect of Aging on Glucose Homeostasis. Diabetes Care 2008, 31, 539–543. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet Lond Engl. 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Cardona, M.S. ENSE Encuesta Nacional de Salud España 2017, 2017, 37.
- Wei, Y.M.; Yang, H.X.; Zhu, W.W.; Liu, X.Y.; Meng, W.Y.; Wang, Y.Q.; et al. Risk of adverse pregnancy outcomes stratified for pre-pregnancy body mass index. J Matern Fetal Neonatal Med. 2016, 29, 2205–2209. [Google Scholar] [CrossRef]
- Catalano, P.M.; McIntyre, H.D.; Cruickshank, J.K.; McCance, D.R.; Dyer, A.R.; Metzger, B.E.; et al. The Hyperglycemia and Adverse Pregnancy Outcome Study. Diabetes Care 2012, 35, 780–786. [Google Scholar] [CrossRef]
- Hashemi-Nazari, S.S.; Najafi, F.; Rahimi, M.A.; Izadi, N.; Heydarpour, F.; Forooghirad, H. Estimation of gestational diabetes mellitus and dose–response association of BMI with the occurrence of diabetes mellitus in pregnant women of the west of Iran. Health Care Women Int. 2020, 41, 121–130. [Google Scholar] [CrossRef]
- Rezaei, M.; Rajati, F.; Fakhri, N. Relationship between body mass index and gestational diabetes mellitus. Tehran Univ Med J 2019, 77, 246–251. [Google Scholar]
- Kelly, A.C.; Powell, T.L.; Jansson, T. Placental function in maternal obesity. Clin Sci. 2020, 134, 961–984. [Google Scholar] [CrossRef]
- Horta, B.L.; Victora, C.G.; Menezes, A.M.; Halpern, R.; Barros, F.C. Low birthweight, preterm births and intrauterine growth retardation in relation to maternal smoking. Paediatr Perinat Epidemiol. 1997, 11, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Lambers, D.S.; Clark, K.E. The maternal and fetal physiologic effects of nicotine. Semin Perinatol. 1996, 20, 115–126. [Google Scholar] [CrossRef]
- Mantzoros, C.S.; Varvarigou, A.; Kaklamani, V.G.; Beratis, N.G.; Flier, J.S. Effect of Birth Weight and Maternal Smoking on Cord Blood Leptin Concentrations of Full-Term and Preterm Newborns 1. J Clin Endocrinol Metab. 1997, 82, 2856–2861. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Lodge, J.; Flatley, C.; Kumar, S. The burden of adverse obstetric and perinatal outcomes from maternal smoking in an Australian cohort. Aust N Z J Obstet Gynaecol. 2019, 59, 356–361. [Google Scholar] [CrossRef]
- Shah, N.R.; Bracken, M.B. A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. Am J Obstet Gynecol. 2000, 182, 465–472. [Google Scholar] [CrossRef]
- Liu, B.; Xu, G.; Sun, Y.; Qiu, X.; Ryckman, K.K.; Yu, Y.; et al. Maternal cigarette smoking before and during pregnancy and the risk of preterm birth: A dose–response analysis of 25 million mother–infant pairs. PLoS Med. 2020, 17, e1003158. [Google Scholar] [CrossRef]
| Overall (n =1921) | Maternal Age | Body mass index | Smoker | |||||
|---|---|---|---|---|---|---|---|---|
| Less than 40 (n=1776) | 40 or more (n=145) | < 18 (n=29) | 18 to <35 (n=1802) | ≥ 35 | No | Yes | ||
| (n=90) | (n=1647) | (n=274) | ||||||
| Maternal age in years, | 33.6 | 33.1 | 41.2 | 29.8 | 33.7 | 32.8 | 33.8 | 32.3 |
| median (IQR) | (30.0, 36.6) | (29.7, 35.9) | (40.5, 42.2) | (24.5, 33.9) | (30.1, 36.6) | (30, 36) | (30.3, 36.6) | (29.0, 36.0) |
| Body mass index in Kg/m2, median (IQR) | 24.0 | 23.9 | 24.9 | 17.2 | 23.9 | 38.0 | 24.0 | 24.4 |
| (21.7, 27.5) | (21.6, 27.5) | (22.2, 27.5) | (16.87, 17.5) | (21.7, 27) | (36.4, 40.3) | (21.7, 27.5) | (21.8, 27.6) | |
| Smoker, n (%) | 274 (14.3%) | 259 (14.6%) | 15 (10.3%) | 6 (20.7%) | 254 (14.1%) | 14 (15.6%) | 0 | 274 (100%) |
| Race, n (%) | ||||||||
| White | 1873 (97.5%) | 1735 (97.7%) | 138 (95.2%) | 29 (100%) | 1756 (97.4%) | 88(97.8%) | 1601 (97.2%) | 272 (99.3%) |
| Black | 30 (1.6%) | 24 (1.4%) | 6 (4.1%) | 0 | 28 (1.6%) | 2 (2.2%) | 28 (1.7%) | 2 (0.7%) |
| East Asian | 9 (0.5%) | 8 (0.5%) | 1 (0.7%) | 0 | 9 (0.5%) | 0 | 9 (0.5%) | 0 |
| Mixed | 5 (0.3%) | 5 (0.3%) | 0 | 0 | 5 (0.3%) | 0 | 5 (0.3%) | 0 |
| South Asian | 4 (0.2%) | 4 (0.2%) | 0 | 0 | 4 (0.2%) | 0 | 4 (0.2%) | 0 |
| Nulliparity n (%) | 847 (44.1%) | 796 (44.8%) | 51 (35.2%) | 14(48.3%) | 802 (44.5%) | 31(34.4%) | 713 (43.3%) | 134 (48.9%) |
| Conception n (%) | ||||||||
| Spontaneous | 1798 (93.6%) | 1692 (95.3%) | 106 (73.1%) | 29 (100%) | 1683(93.4%) | 86 (95.6%) | 1539 (93.4%) | 259 (94.5%) |
| Assisted reproductive techniques | 123(6.4%) | 84 (4.7%) | 39 (26.9%) | 0 | 119 (6.6%) | 4 (4.4%) | 108 (6.6%) | 15 (5.5%) |
| Chronic hypertension n (%) | 28 (1.5%) | 22 (1.2%) | 6 (4.1%) | 0 | 22(1.2%) | 6(6.7%) | 25 (1.5%) | 3 (1.1%) |
| Diabetes Mellitus n (%) | ||||||||
| Type 1 | 10 (0.5%) | 9 (0.5%) | 1 (0.7%) | 0 | 9 (0.5%) | 1 (1.1%) | 10 (0.6%) | 0 |
| Type 2 | 5 (0.3%) | 4 (0.2%) | 1 (0.7%) | 0 | 5 (0.3%) | 0 | 4 (0.2%) | 1 (0.4%) |
| APS and/or SLE n (%) | 22 (1.1%) | 20 (1.1%) | 1 (1.4%) | 0 | 22 (1.2%) | 0 | 22 (1.3%) | 0 |
| Previous preeclampsia n(%) | 55 (2.9%) | 52 (2.9%) | 3 (2.1%) | 1 (3.2%) | 49 (2.7%) | 5 (5.6%) | 49 (3.0%) | 6 (2.2%) |
| Previous neonate’s birth weight <10th percentile n(%) | 259 (13.5%) | 234 (13.2%) | 25 (17.2%) | 5 (16.1%) | 245(13.6%) | 9(10%) | 213 (12.9%) | 46 (16.8%) |
| Previous neonate’s birth weight <3rd percentile n(%) | 127 (6.6%) | 112 (6.3%) | 15 (10.3%) | 4 (12.9%) | 120 (6.7%) | 3(3.3%) | 102 (6.2%) | 25 (9.1%) |
| Previous Gestational Diabetes n (%) | 67 (3.5%) | 57 (3.2%) | 10 (6.9%) | 0 | 57(3.2%) | 10(11.1%) | 56 (3.4%) | 11 (4.0%) |
| Previous preterm birth n(%) | 83 (4.3%) | 74 (4.2%) | 9 (6.2%) | 1 (3.4%) | 80 (4.4%) | 2 (2.2%) | 69 (4.2%) | 14 (5.1%) |
| Previous fetal weight > 95% percentile n (%) | 34 (3.2%) | 32 (3.3%) | 2 (2.1%) | 0 (0%) | 29 (2.9%) | 5 (8.5%) | 29 (3.1%) | 5 (3.6%) |
| Overall (n=1921) | Maternal Age | Body mass index | Smoker | |||||
|---|---|---|---|---|---|---|---|---|
| Less than 40 (n=1776) | 40 or more (n=145) | < 18 (n=29) | 18 to 35 (n=1802) | ≥ 35 (n=90) | No (n=1647) | Yes (n=274) | ||
| Neonatal outcome, n (%) | ||||||||
| Live birth | 1916 (99.7%) | 1771 (99.7%) | 145 (100%) | 29 (100%) | 1797 (99.7%) | 90 (100%) | 1643 (99.8%) | 273 (99.6%) |
| Neonatal death | 2 (0.1%) | 2 (0.1%) | 0 | 0 | 2 (0.1%) | 0 | 2 (0.1%) | 0 |
| Stillbirth | 3 (0.2%) | 3 (0.2%) | 0 | 0 | 3 (0.2%) | 0 | 2 (0.1%) | 1 (0.4%) |
| Gestational age at birth in weeks, median (IQR) | 39.0 | 39.0 | 39.0 | 39.0 | 39.0 | 39.0 | 39.0 | 39.0 |
| (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | (38.0, 40.0) | |
| Preterm birth n (%) | 118 (6.1%) | 108 (6.1%) | 10 (6.9%) | 4 (13.8%) | 108 (6.0%) | 6 (6.7%) | 104 (6.3%) | 14 (5.1%) |
| Labour onset n (%) | ||||||||
| Spontaneous | 967 (50.3%) | 899 (50.6%) | 68 (46.9%) | 11 (37.9%) | 927 (51.4%) | 29 (32.2%) | 840 (51.0%) | 127 (46.4%) |
| Induced | 817 (42.5%) | 753 (42.4%) | 64 (44.1%) | 14(48.3%) | 749 (41.6%) | 54 (60.0%) | 684 (41.5%) | 133 (48.5%) |
| No labour | 137 (7.1%) | 124 (7.0%) | 13 (9.0%) | 4 (13.8%) | 126 (7%) | 7 (7.8%) | 123 (7.5%) | 14 (5.1%) |
| Mode of delivery n (%) | ||||||||
| Elective cesarean section | 93 (4.8%) | 84 (4.7%) | 9 (6.2%) | 3 (10.3%) | 84 (4.7%) | 6 (6.7%) | 83 (5.0%) | 10 (3.6%) |
| Emergency cesarean section | 288 (15.0%) | 261 (14.7%) | 27 (18.6%) | 1 (3.4%) | 265 (14.7%) | 22 (24.4%) | 244 (14.8%) | 44 (16.1%) |
| Instrumental | 326 (17.0%) | 304 (17.1%) | 22 (15.2%) | 4 (13.8%) | 311 (17.3%) | 11 (12.2%) | 278 (16.9%) | 48 (17.5%) |
| Vaginal | 1214 (63.2%) | 1127 (63.5%) | 87 (60.0%) | 21 (72.4%) | 1142 (63.4%) | 51 (56.7%) | 1042 (63.3%) | 172 (62.8%) |
| Birth weight in grams, | 3200 | 3200 | 3200 | 3030 | 3200 | 3500 | 3210 | 3080 |
| median (IQR) | (2900, 3500) | (2910, 3500) | (2790, 3510) | (2600, 3220) | (2900, 3500) | (3220, 3770) | (2920, 3520) | (2760, 3360) |
| Birth weight percentile | 31.5 | 31.7 | 29.8 | 15.9 | 31.5 | 61.9 | 33.7 | 20.5 |
| Median (IQR) | (12.6, 59.0) | (12.9, 58.8) | (9.75, 59.8) | (2.85, 45.6) | (12.6, 58.8) | (30.2, 79.1) | (14.0, 61.0) | (6.72, 42.1) |
| Birth weight <10th percentile, n (%) | 413 (21.5%) | 375 (21.1%) | 38 (26.2%) | 14 (48.3%) | 385 (21.4%) | 14 (15.6%) | 326 (19.8%) | 87 (31.8%) |
| Birth weight <3rd percentile, n (%) | 186 (9.7%) | 170 (9.6%) | 16 (11.0%) | 9 (31.0%) | 174 (9.7%) | 3 (3.3%) | 143 (8.7%) | 43 (15.7%) |
| Birth weight >95th percentile, n (%) | 38 (2.0%) | 34 (1.9%) | 4 (2.8%) | 0 (0%) | 31 (1.7%) | 7 (7.8%) | 37 (2.2%) | 1 (0.4%) |
| Developed preeclampsia n(%) | 82 (4.3%) | 69 (3.9%) | 13 (9.0%) | 1 (3.4%) | 73(4.1%) | 8 (8.9%) | 73 (4.4%) | 9 (3.3%) |
| Developed pregnancy hypertension n (%) | 43 (2.2%) | 38 (2.1%) | 5 (3.4%) | 0 | 36 (2.0%) | 7 (7.8%) | 36 (2.2%) | 7 (2.6%) |
| Developed gestational diabetes n (%) | 455 (23.7%) | 406 (22.9%) | 49 (33.8%) | 3 (10.3%) | 408 (22.6%) | 44 (48.9%) | 386 (23.4%) | 69 (25.2%) |
| Pregnancy complication | Maternal Age ≥ 40 (n=145) | BMI <18 (n=29) | BMI≥35 (n=90) | Smoking (n=274) | ||||
|---|---|---|---|---|---|---|---|---|
| aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | |
| Preterm delivery | 0.99 (0.45 to 1.96) | 0.970 | 2.67 (0.77 to 7.13) | 0.077 | 1.01 (0.38 to 2.26) | 0.978 | 0.78 (0.42 to 1.36) | 0.415 |
| Cesareansection | 1.13 (0.70 to 1.79) | 0.612 | 0.71 (0.20 to 1.92) | 0.539 | 2.12 (1.25 to 3.54) | 0.005 | 0.97 (0.68 to 1.36) | 0.851 |
| Vaginal delivery | 0.87 (0.57 to 1.32) | 0.504 | 1.35 (0.60 to 3.27) | 0.478 | 0.63 (0.38 to 1.03) | 0.064 | 1.04 (0.78 to 1.40) | 0.786 |
| Birth weight<10th percentile | 1.54 (1.00 to 2.37) | 0.049 | 3.28 (1.51 to 7.05) | 0.002 | 0.73 (0.40 to 1.34) | 0.308 | 1.83 (1.36 to 2.46) | <0.001 |
| Birth weight <3rd percentile | 1.19 (0.63 to 2.11) | 0.569 | 3.73 (1.54 to 8.37) | 0.002 | 0.31 (0.10 to 1.02) | 0.055 | 1.91 (1.29 to 2.78) | 0.001 |
| Birth weight >95th percentile | 1.31 (0.44 to 3.89) | 0.623 | 1.19 (0.07 to 18.84) | 0.908 | 3.50 (1.37 to 8.91) | 0.009 | 0.15 (0.01 to 0.70) | 0.061 |
| Preeclampsia | 2.00 (0.91 to 4.11) | 0.070 | 0.97 (0.05 to 4.85) | 0.977 | 1.94 (0.76 to 4.31) | 0.129 | 0.79 (0.35 to 1.56) | 0.522 |
| Gestational diabetes mellitus | 1.61 (1.08 to 2.36) | 0.018 | 0.32 (0.05 to 1.07) | 0.118 | 3.10 (1.95 to 4.89) | <0.001 | 1.06 (0.76 to 1.45) | 0.745 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





