1. Introduction
Neurogenic bladder (NB) secondary to spinal cord injury (SCI) leads to complications possibly associated with the pathology of bladder dysfunction itself or with bladder management, thus negatively affecting health and quality of life (QoL)1. These complications include urinary incontinence (UI), urinary tract infections (UTI), kidney stones, high intravesical pressures associated with vesicoureteral reflux, and hydronephrosis2.
UI, defined as involuntary urine leakage during the storage phase of the bladder2, is considered the most unpleasant of these complications and may even negatively affect participation in society3. UI is usually caused by difficulty in bladder storage or voiding due to detrusor hyperactivity or urethral incompetence, detrusor areflexia, or sphincter vesicle dyssynergia4.
Adequate bladder management is an important element of the rehabilitation of SCI, and one of its key objectives is the acquisition of urinary continence5. Despite the impact of this complication on people with SCI, few studies relate UI to bladder-emptying methods or satisfaction with life and mostly mention UI as a secondary outcome that affects QoL6,7.
In Brazil, a study evaluated the effects of UI on the QoL of people with SCI and demonstrated that UI compromises QoL, especially in terms of social life, sexuality, and affectivity8. Another study conducted in Denmark evaluated bladder-emptying methods and UI in individuals with long-term SCI. One of the results found in this study showed that a greater number of participants using clean intermittent catheterization (CIC) reported episodes of UI than participants who used other bladder-emptying methods3.
Thus, considering that UI may be related to the bladder-emptying method and changes in QoL, this study aimed to analyze UI due to NB and its relationship with bladder management, satisfaction, and lifestyle in people with SCI.
2. Materials and Methods
This is a quantitative study with an exploratory, analytical, and cross-sectional design, conducted from February to November 2021, at the Ribeirão Preto School of Nursing, Universidade de São Paulo. Since the records were obtained from a registry of people who voluntarily accepted to participate in research in this area, the scope of this study was nationwide. This study was submitted for approval to the Ethics and Research Committee of the Ribeirão Preto School of Nursing of the Universidade de São Paulo, file CAAE 19748919.3.0000.5393.
The sample included adults, aged 18 years or older, with SCI who enrolled as volunteers to participate in research at the Center for Research and Care in Neuropsychomotor Rehabilitation (NeuroRehab). NeuroRehab, established in 2014, develops studies, technologies, and extension activities in rehabilitation to maximize the autonomy and participation of people with disabilities in society. For this purpose, Neurorehab has a database of people who enrolled as volunteers to participate in research on SCI9.
At the beginning of the survey, the registry had around 1,200 subscribers. Those who did not indicate a mobile phone number or a landline were excluded. The sample size was calculated according to a population equal to 1200 and a p of 0.5. According to the level of significance, the number of participants necessary to achieve the desired margin of error was 290.
First, data were collected by characterizing the clinical profile of the participant based on datasets of the ISCoS (International Spinal Cord Society)10. Furthermore, sociodemographic data were collected according to the variables gender (male and female), date of birth, age, cause, date, and level and classification of SCI. Second, the Bowel and Bladder Treatment Index (BBTI) developed by Tate et al. (2015), translated and validated into Brazilian Portuguese by Braga (2018)11,12. The BBTI is a self-report instrument for patients with SCI. It was developed according to standards of the ISCoS and American Spinal Cord Injury Association (ASIA) for use in patients with SCI during clinical face-to-face or telephone interviews to evaluate bowel and bladder-emptying methods, complications, and impact on QoL, satisfaction, and lifestyle. The BBTI contains 60 items and is divided into sections on the intestine and bladder that address emptying methods, complications, personal satisfaction, and impact on life11.
For this study, the section that evaluates the bladder domain was used to collect data on the impact of bladder function on QoL, the bladder-emptying method, complications of NB, satisfaction with bladder management, and its effect on lifestyle. The sociodemographic profile characterization questionnaire, the BBTI, and the informed consent form were transcribed to the online SurveyMonkey® platform to initiate data collection. A pilot test with 10 participants was previously carried out to verify the adequacy of the collection method. There was no need to change the questionnaire after the pilot test.
The interviews were conducted over the telephone. An invitation explaining the survey and a link with the informed consent form were sent to the mobile phones or by e-mail, depending on the option of respondents at the time of enrollment.
The participants of the registry were divided between 4 researchers to prevent duplicate calls or contact. The calls were made from 8:30 am to 6:00 pm from Monday to Friday and on Saturday from 9:00 am to 12:00 pm. Initially, an attempt was made to contact each participant on the list. If the number of participants was exhausted without having reached the desired sample, the researchers went back to the beginning of the list for the second attempt of telephone contact on different days and times.
For the descriptive statistical analysis of categorical variables (qualitative variables), absolute and relative frequencies were used. In the description of the numerical variables (quantitative variables), measures of position, central tendency, and dispersion were used. To describe the numerical items of the satisfaction and lifestyle instrument and measure central tendency and dispersion, the bootstrap percentile interval of 95% confidence was used. To associate the variables of bladder management, UI, satisfaction, and lifestyle, the Chi-square test, the simulated Chi-square test, and Fisher’s exact test were used in cases of cross-tabulation. When all pairs of characteristics had values greater than 5, the Chi-square test was used. When at least one pair of characteristics obtained a value less than or equal to 5 and the two variables tested had two levels, Fisher’s exact test was used. When at least one pair of characteristics obtained a value less than or equal to 5 and at least one of the variables tested had three levels or more, the simulated Chi-square test was used. The Mann-Whitney test was used to verify the association between two-level categorical variables and numerical variables.
To better evaluate the urinary incontinence variable, the participants were divided into 2 groups. Those who responded having daily leakage at least once a week and at least once a month were included in the incontinence group and those who reported leakage less than once a month and no leakage were included in the continence group. In the variable efficacy of routine bladder management, a Likert scale from 0, very ineffective routine, to 10, very effective routine, was used.
A significance level of <0.05 was adopted in all analyses. The software R (version 3.6.1) was used in the analyses.
3. Results
The sample consisted of 290 participants, 70% male and 30% female. The current mean age of the participants was 41.02 years (SD=10.43).
The mean time of SCI was 139.04 months (SD=106.24) or approximately 12 years. The major causes of SCI were traumatic (79.30%), including traffic accidents (44.1%), automobile and motorcycle accidents, accidents with firearms and knives (14.50%), falls (10.00%), and diving in shallow water (9.00%). Non-traumatic causes totaled 21.70% and included congenital (0.7%), myelopathies (15.50%), related to medical-surgical procedures (3.80%), or other non-traumatic causes (1.7%).
Regarding the classification of SCI, 67.70% reported having paraplegia and 34.40% reported having quadriplegia, with a greater occurrence at the thoracic level (62.80%), followed by cervical level (32.30%) and lumbar level (4.90%). Participants with incomplete SCI totaled 44.13% and complete SCI totaled 35.60%. Moreover, 20.30% of the participants did not know whether the lesion was complete or incomplete.
Table 1 shows the descriptive analysis of bladder management methods. CIC was the most widely used emptying method (74.10%), with 57.20% of the participants performing self-catheterization and 16.90% performing catheterization assisted by third parties. Only one participant reported having a non-continent urinary diversion/ostomy. The methods of anterior sacral root stimulation and Mitrofanoff were not mentioned.
Regarding bladder emptying, almost half of the participants (43.70%) emptied their bladder 5 times a day, 20.50% 4 times a day, 20.50% 6 times a day, 10.80% 7 times or more, and 4.50 1 to 3 times a day. Mean daily bladder emptying according to the method was higher for bladder compression (m=7.40 times/day), followed by normal urination (m=6.72 times/day), and CIC (m=5.05 times/day).
Regarding the frequency of involuntary urine leakage in the last year, 37.00% answered they had leakage daily, 13.10% at least once a week, and 5.50% at least once a month, that is, 55.60% were considered incontinent. In the continence group, 29.10% never had leakage and 15.20% had leakage less than once a month. In this study, 51.00% of the participants used a urinary device, such as a diaper device (65.50%), followed by an external collector (33.80%) and an ostomy bag (0.70%).
When analyzing UI by bladder-emptying method, 86.70% of the participants who performed bladder reflex triggering and 59.10% of the participants who performed CIC were incontinent. Emptying by normal urination and bladder reflex triggering had a statistically significant relationship with UI.
In terms of the odds ratio (OR) of each management method, the chance of continence increases an average of 2.23 times for the participants who perform normal urination (
Table 2).
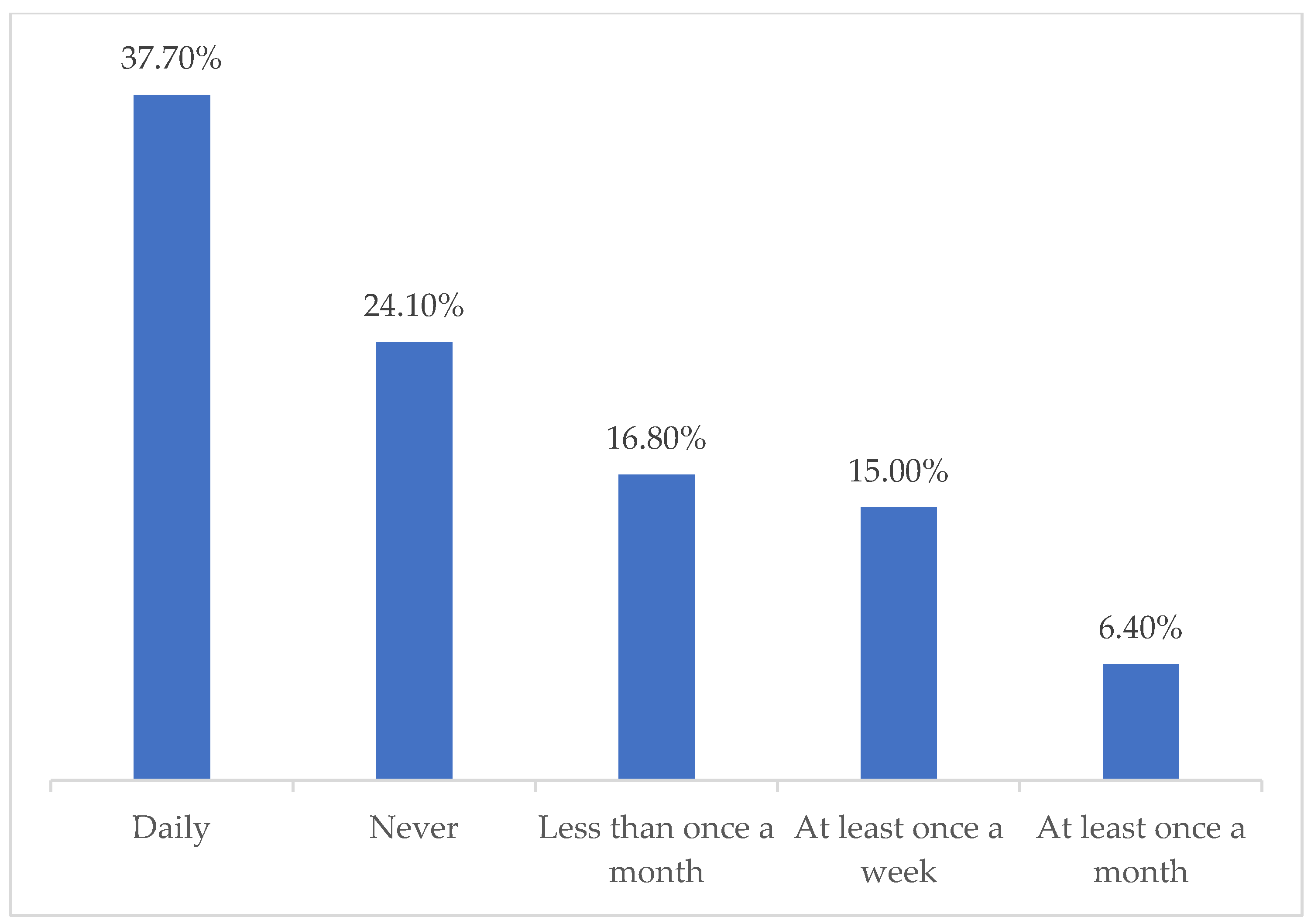
Considering that the vast majority of the sample performed CIC as a bladder–emptying method, a descriptive analysis of urine leakage frequency in this group of participants was performed (Graph 1). In this analysis, 62.30% present with some frequency of urine leakage, and 37.70% have daily leakage.
Figure 1.
- Frequency of urine leakage in the CIC management method, n=220, Brazil, 2021. Source: Prepared by the author
Figure 1.
- Frequency of urine leakage in the CIC management method, n=220, Brazil, 2021. Source: Prepared by the author
Satisfaction and lifestyle and their relationship with UI
When the participants were asked about their level of satisfaction with their bladder-emptying routine, 58.60% responded they were satisfied and very satisfied (Chart 2).
Figure 2.
- Sample distribution according to the level of satisfaction with bladder emptying routine, n=290, Brazil, 2021. Source: Prepared by the author.
Figure 2.
- Sample distribution according to the level of satisfaction with bladder emptying routine, n=290, Brazil, 2021. Source: Prepared by the author.
Although a smaller percentage of the sample (41.40%) stated they were dissatisfied or very dissatisfied with the bladder-emptying routine, when asked about the reason for their dissatisfaction, the second main cause was related to UI (41.70%) (
Table 4).
Table 3.
- Sample distribution according to causes of dissatisfaction with bladder-emptying routine (n=120). Brazil, 2021.
Table 3.
- Sample distribution according to causes of dissatisfaction with bladder-emptying routine (n=120). Brazil, 2021.
| Causes of dissatisfaction with bladder-emptying routine |
N |
% |
| Difficulties related to bladder-emptying method |
59 |
49.1 |
| Related to UI |
50 |
41.7 |
| Architectural difficulties |
19 |
15.8 |
| Psychological difficulties |
13 |
4.5 |
| Related to urinary tract infection |
12 |
4.1 |
The participants were asked about the effectiveness of their bladder-emptying routine on a scale of 0 to 10. The mean was calculated with a bootstrap confidence interval, with an average score of 7.75, (SD=2.12). A statistical significance was observed for the effectiveness of the bladder-emptying routine with UI (p<0.001, Mann-Whitney test) and satisfaction with the bladder-emptying routine (p<0.001, Chi-square test).
Regarding the possible changes in lifestyle in the last year due to urine leakage in the participants with UI, 64.00% stated changes with some level of frequency and only 36.00% reported no changes to lifestyle due to leakage episodes (
Table 4).
Table 4.
- Descriptive distribution of responses on lifestyle changes due to urine leakage in participants with incontinence, n=161, Brazil, 2021.
Table 4.
- Descriptive distribution of responses on lifestyle changes due to urine leakage in participants with incontinence, n=161, Brazil, 2021.
| Lifestyle changes due to urine leakage |
N |
% |
| None |
58 |
36.0 |
| Less than once a month |
22 |
13.7 |
| At least once a month |
17 |
10.6 |
| At least once a week |
19 |
11.8 |
| Daily |
45 |
28.0 |
Statistical analyses were performed relating UI to the categorical variables of satisfaction and lifestyle. An association was observed with the effect of bladder problems on life (p=0.008, simulated Chi-square test), bladder management as an obstacle to working outside the home or doing routine activities (p<0.001, Chi-square test), impaired personal relationships (p = 0.001, Chi-square test), and impaired social life (p-value = 0.002, Chi-square test) (Table 6).
Table 5.
- Association between incontinence and categorical variables of satisfaction and lifestyle, n=290, Brazil, 2021.
Table 5.
- Association between incontinence and categorical variables of satisfaction and lifestyle, n=290, Brazil, 2021.
| Satisfaction and lifestyle\Incontinence |
Yes |
No |
p-value |
| N |
% |
N |
% |
| Effects of bladder problems on QoL |
No effect |
16 |
9.9% |
24 |
18.8 |
0.008 |
| Little effect |
37 |
23.0% |
36 |
28.1 |
| Some effect |
33 |
20.5% |
32 |
25.0 |
| Severe effect |
75 |
46.6% |
36 |
28.1 |
Bladder management prevents me
from working outside the home or doing
routine activities |
Not at all |
55 |
34.2% |
77 |
60.2 |
<0.001 |
| Somewhat |
63 |
39.1% |
35 |
27.3 |
| Very much |
43 |
26.7% |
16 |
12.5 |
Bladder management negatively affects
my personal
relationships |
Not at all |
61 |
37.9% |
76 |
59.4 |
0.001 |
| Somewhat |
55 |
34.2% |
26 |
20.3 |
| Very much |
45 |
28.0% |
26 |
20.3 |
Bladder management
negatively affects
my social life |
Not at all |
56 |
34.8% |
71 |
55.5 |
0.002 |
| Somewhat |
69 |
42.9% |
39 |
30.5% |
| Very much |
36 |
22.4% |
18 |
14.1% |
4. Discussion
This study analyzed UI and its relationship with bladder-emptying methods, personal satisfaction, and lifestyle in people with SCI. In this regard, the prevalent bladder-emptying method among participants was CIC (74.10%). CIC is recommended as the first-choice treatment for neurogenic bladder and is mainly indicated to protect the upper urinary tract, prevent and control UTI, and promote continence5,13,14. The predominance in this study of participants who perform CIC demonstrates that most urologists indicate this method as the gold standard in the treatment of neurogenic bladder.
The mean bladder emptying reported by the participants was 5.4 times a day. However, the mean was higher among participants who performed bladder compression (7.4 times a day). The natural emptying frequency for a typical bladder is 4 to 6 times a day depending on fluid intake and bladder volume. This frequency is also indicated in patients who perform CIC according to urological guidelines5. Therefore, the result is consistent with the mean found in this study for emptying by CIC (5.04). Regarding bladder compression, the participants are expected to perform emptying more times a day because bladder compression does not guarantee complete emptying.
The study revealed that 55.6% of the participants had episodes of incontinence in the last year. Of these participants, 37% have daily leakage and 51% use some device for incontinence, especially diapers. UI was also one of the main causes of dissatisfaction with routine bladder management (41.7%). Previous studies corroborate the findings of this study regarding UI in people with SCI6,15,16,17. A study of the translation, localization, and validation of data sets of the lower urinary tract for people with SCI showed similar results in the use of urinary devices, with diapers as the most frequently used device2.
When comparing each bladder management method, bladder reflex triggering had the highest percentage of individuals with UI (86.7%), followed by CIC (59.1%), and bladder compression (55.5%), which corroborates the results of previous studies 2,8,16. Only emptying by normal urination showed a statistically significant association with urinary continence and bladder reflex triggering with UI.
The relationship between emptying by normal urination and urinary continence is expected since participants may be resuming normal bladder function that involves the coordinated action of the pelvic floor, detrusor muscle, and urethral sphincter resulting from the coordination between the multiple regulatory centers in the brain, spinal cord, and peripheral nerves18. In contrast, the association of bladder reflex triggering with UI is expected because this method involves maneuvers performed by people with SCI or by a caregiver to voluntarily or involuntarily stimulate the detrusor reflex2, often without perception of urine outflow and, thus, without continence control.
In this study, no statistically significant relationship was observed between CIC and UI, although it is the second most widely used method among the participants with incontinence (59.1%). A description of the frequency of UI in CIC users revealed that 37.7% had urine leakage daily, 16.0% had leakage less than once a month, and 24.1% never had leakage. Studies in the literature approximate the percentage of UI in users of CIC16.
One of the objectives of CIC is to improve UI. However, the person often acquires partial continence, as demonstrated in this study, resulting in a decrease in leakage frequency, which improves QoL. In contrast, the entire rehabilitation team should address both the expectations of patients before initiating CIC to minimize the chances of abandoning the technique19,20 and the health education of this population. Insufficient health literacy can affect the patient's ability to take care of themselves and has a direct negative effect on their health, thus increasing the risk of complications21,22.
In the discussion about UI acquisition after CIC, the use of drug therapy for the bladder should be considered as adjuvant in the overall treatment. These drugs assist in the acquisition of continence by decreasing detrusor hyperactivity and increasing bladder capacity or sphincter insufficiency13,23, which reduces leakage.
Satisfaction with the bladder-emptying routine and the effectiveness of this routine were related to urinary continence in this study. One of the objectives of bladder management is the acquisition of urinary continence. Therefore, participants are expected to feel more satisfied with their routine since urinary continence affects the QoL of people with SCI17,18,24.
When asked about possible changes in lifestyle as a result of urine leakage, 64.0% stated they changed their lifestyle with some type of frequency and among these, 28.0% changed their lifestyle daily. The results are similar to the findings of a national study that evaluated the impact of UI on the QoL of people with SCI8. Moreover, another study that compared health-related QoL, daily activities, and the use of health resources between patients with continence and incontinence found that the daily activities of the participants with incontinence were more greatly affected than the daily activities of the patients with continence7.
When relating UI with the variables of satisfaction and lifestyle, it was found that bladder problems had a greater effect on QoL, difficulty working outside the home, performing routine activities, and impaired personal relationships and social life.
Previous studies corroborate these findings concerning the negative effect of UI on the QoL of people with SCI17,18 and impaired social, personal, and affective relationships8. The uncertainty of patients regarding the risk of urine leakage causes social isolation to avoid embarrassment and concerns about UI, as shown in a qualitative study that describes the experiences of bladder and intestinal dysfunction in people with SCI. According to the study, these dysfunctions have a profound effect on relationships and social activities, especially outside the home, also related to the risk of incontinence25,26.
These data reinforce the need and importance of UI control in people with SCI. In this regard, the need to change the entire bladder-emptying routine greatly affects the lifestyle of these people who, when choosing a management method, do not expect further concerns with UI, which is also considered an important factor for resuming their social, work, and affective lives.
Based on the above considerations, nursing professionals should discuss ways to maximize urinary continence and minimize the resulting damage. The rehabilitation nurse should seek care alternatives to ensure people with UI can live to their fullest, with social participation and QoL.
Study Limitations
This study has some limitations. First, the data collected for this study was based on the perception of the participants regarding bladder care. Thus, at the time of the interview, some participants may not remember some information about forms of bladder care and complications. However, memory bias is often present in cross-sectional studies.
Second, the participants may have encountered some difficulties interpreting the questions since the interview was conducted over the telephone. However, to minimize any difficulties, the interviewers were trained to conduct the interviews in a standard manner that was clear and easy to understand. Furthermore, due to social distancing during the COVID-19 pandemic, data collection by telephone ensured the participation of people from all over Brazil with no risk to participants, researchers, and interviewers.
Given the cross-sectional design of this study, changes in the frequency of urinary leakage after initiating CIC were not evaluated. Since one of the objectives of CIC is to reduce urine leakage, longitudinal studies are suggested.
Data on the use of bladder medications would provide valuable insight into the large number of participants with UI, especially among those who perform CIC. Drug therapy associated with the bladder management method reduces the chance of UI in terms of decreasing detrusor hyperactivity, increasing bladder capacity, or sphincter insufficiency. It will be suggested to the authors of the instrument to include this data.
5. Conclusions
The study showed that bladder management is not yet a fully resolved issue when evaluating the relationship with UI. Despite advances in urinary tract protection and the consequent decrease in mortality, UI still has a negative effect on the lives of people with SCI, even with the indicated emptying methods.
CIC was the predominant bladder-emptying method. Despite reducing urine leakage, a considerable number of participants still had frequent leakage, thus preventing the complete acquisition of urinary continence. Bladder emptying with bladder reflex triggering was associated with UI, while normal urination increased the chances of continence.
Satisfaction and lifestyle were strongly affected by UI due to BN in the participants of this study. Moreover, UI negatively affected satisfaction with the bladder management routine, effectiveness of bladder management, QoL, and personal and social relationships.
Given the results obtained in this study, measures should be adopted to minimize the effect of UI on the lives of people with SCI and BN, including longitudinal monitoring of bladder dysfunction and an individualized indication of the bladder-emptying method, considering the expectations of acquiring UI. In addition, continuing education should be provided to rehabilitation professionals, especially nurses, in order to empower patients and manage the physiological and emotional consequences that may result from bladder dysfunction and its complications.
In this regard, future studies are needed to better understand these findings and improve the current methods of managing NB. These improvements include the development of new care technologies that increase the chances of acquiring urinary continence and, consequently, bettering the lives of people with SCI and BN.6. Patents
This section is not mandatory but may be added if there are patents resulting from the work reported in this manuscript.
Author Contributions
Conceptualization, Gomes, Schoeller and Faleiros; Methodology, Gomes, Corbo, Martins, Faleiros and Kappler; Formal Analysis, Gomes, Schoeller, Avila and Faleiros; Investigation, Gomes, Faleiros and Kappler; Resources, Gomes, Avila, Martins, Faleiros, and Kappler; Data Curation, Gomes, Faleiros and Kappler; Writing - Original Draft preparation, Gomes, Corbo, Avila, Martins, Schoeller and Faleiros; editing – Review and editing, Gomes and Corbo; supervision, Faleiros, and Schoeller; Project administration, Gomes and Faleiros; Acquisition of financing Faleiros and Kappler.
Funding
This research received no external funding
Institutional Review Board Statement
This study was submitted for approval to the Ethics and Research Committee of the Ribeirão Preto School of Nursing of the Universidade de São Paulo, file CAAE 19748919.3.0000.5393.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Taweel, W; Seyam, R. Neurogenic bladder in spinal cord injury patients. Research and Reports in Urology, 2015,v.7, o.85-99.
- Cordeiro, A. Tradução, adaptação e validação para o português brasileiro do Data Set do trato urinário inferior para pessoas com lesão medular. Dissertação (Mestrado em Enfermagem) – Escola de Enfermagem, Universidade de São Paulo, Ribeirão Preto, 2017.
- Hansen, R.B.; Biering-Sørensen, F.; Kristensen, J.K. Urinary incontinence in spinal cord injured individuals 10–45 years after injury. Spinal Cord 2009, 48, 27–33, . [CrossRef]
- Chen, S.-F.; Jiang, Y.-H.; Jhang, J.-F.; Lee, C.-L.; Kuo, H.-C. Bladder management and urological complications in patients with chronic spinal cord injuries in Taiwan. Tzu Chi Med J. 2014, 26, 25–28, . [CrossRef]
- Groen, J.; Pannek, J.; Diaz, D.C.; Del Popolo, G.; Gross, T.; Hamid, R.; Karsenty, G.; Kessler, T.M.; Schneider, M.; Hoen, L..; et al. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur. Urol. 2016, 69, 324–333, . [CrossRef]
- Akkoç, Y.; for Neurogenic Bladder Turkish Research Group; Ersöz, M.; Yıldız, N.; Erhan, B.; Alaca, R.; Gök, H.; Zinnuroğlu, M.; A Özçete, Z.; Tunç, H.; et al. Effects of different bladder management methods on the quality of life in patients with traumatic spinal cord injury. Spinal Cord 2012, 51, 226–231, . [CrossRef]
- Tang, D.H.; Colayco, D.; Piercy, J.; Patel, V.; Globe, D.; Chancellor, M.B. Impact of urinary incontinence on health-related quality of life, daily activities, and healthcare resource utilization in patients with neurogenic detrusor overactivity. BMC Neurol. 2014, 14, 74–74, . [CrossRef]
- Meneguessi, GM. Percepção sobre qualidade de vida em pessoas com lesão medular traumática: Um estudo sobre incontinência urinária, 2012.
- Faleiros, F. Pessoas com lesão medular no Brasil: O uso de mídias sociais na investigação do itinerário terapêutico, dificuldades e anseios por pesquisas. Tese de livre-docência, 2019.
- DeVivo, M.J.; Biering-Sørensen, F.; New, P.; Chen, Y. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord 2010, 49, 596–599, . [CrossRef]
- Tate, D. et al. Development of a measure to assess bowel and bladder dysfunction. The 4th ISCoS and ASIA Joint Scientific Meeting. 2015.
- Braga; D. C. O. Disfunção vesical na qualidade de vida de pessoas com lesão medular: Tradução, adaptação e validação de um instrumento. 2018. 117 f. Tese (Doutorado em Enfermagem) - Faculdade de Farmácia, Odontologia e Enfermagem, Universidade Federal do Ceará, Fortaleza, 2018.
- Middleton, J et al. Management of the Neurogenic Bladder for Adults with Spinal Cord Injuries. [s.l: S.n].
- Wyndaele, J.-J. The management of neurogenic lower urinary tract dysfunction after spinal cord injury. Nat. Rev. Urol. 2016, 13, 705–714, . [CrossRef]
- Elmelund, M.; Klarskov, N.; Biering-Sørensen, F. Prevalence of urinary incontinence in women with spinal cord injury. Spinal Cord 2018, 56, 1124–1133, . [CrossRef]
- Biering-Sørensen, F.; Kennelly, M.; Kessler, T.M.; Linsenmeyer, T.; Pannek, J.; Vogel, L.; Wyndaele, J.-J. International Spinal Cord Injury Lower Urinary Tract Function Basic Data Set (version 2.0). Spinal Cord Ser. Cases 2018, 4, 60, . [CrossRef]
- Liu, C.-W.; Attar, K.H.; Gall, A.; Shah, J.; Craggs, M. The relationship between bladder management and health-related quality of life in patients with spinal cord injury in the UK. Spinal Cord 2009, 48, 319–324, . [CrossRef]
- Hicken, B.L.; Putzke, J.D.; Richards, J.S. Bladder Management and Quality of Life After Spinal Cord Injury. Am. J. Phys. Med. Rehabilitation 2001, 80, 916–922, . [CrossRef]
- I Afsar, S.; Yemisci, O.U.; Cosar, S.N.S.; Cetin, N. Compliance with clean intermittent catheterization in spinal cord injury patients: a long-term follow-up study. Spinal Cord 2013, 51, 645–649, . [CrossRef]
- Mizuno, K.; Tsuji, T.; Kimura, A.; Liu, M.; Masakado, Y.; Chino, N. Twenty-seven years of complication-free life with clean intermittent self-catheterization in a patient with spinal cord injury: A case report. Arch. Phys. Med. Rehabilitation 2004, 85, 1705–1707, . [CrossRef]
- Cooper, J.; Chisolm, D.; McLeod, D.J. Sociodemographic Characteristics, Health Literacy, and Care Compliance in Families With Spina Bifida. Glob. Pediatr. Heal. 2017, 4, . [CrossRef]
- Pignone, M et al. Interventions to improve health outcomes for patients with low literacy: A systematic review. Journal of General Internal Medicine, 2005, v.20, n.2, pp:185-192.
- Barboglio, PG et al. Non-surgical urologic management of neurogenic bladder after spinal cord injury. Word Journal of Urology, 2018, n.0123456789.
- Myers, J.B.; Lenherr, S.M.; Stoffel, J.T.; Elliott, S.P.; Presson, A.P.; Zhang, C.; Rosenbluth, J.; Jha, A.; Patel, D.P.; Welk, B.; Neurogenic Bladder Research Group. Patient Reported Bladder Related Symptoms and Quality of Life after Spinal Cord Injury with Different Bladder Management Strategies. J. Urol. 2019, 202, 574–584, . [CrossRef]
- Braaf, S.; Lennox, A.; Nunn, A.; Gabbe, B. Social activity and relationship changes experienced by people with bowel and bladder dysfunction following spinal cord injury. Spinal Cord 2017, 55, 679–686, . [CrossRef]
- Faleiros, F.; Braga, D.C.d.O.; Schoeller, S.D.; Henriques, S.H.; Cunha, N.B.F.; Videira, L.G.N.; Grillo, A.C.L.d.S. Surveying people with spinal cord injuries in Brazil to ascertain research priorities. Sci. Rep. 2023, 13, 1–8, . [CrossRef]
Table 1.
- Sample distribution according to bladder-emptying method in the last 4 weeks (n=290). Brazil, 2021.
Table 1.
- Sample distribution according to bladder-emptying method in the last 4 weeks (n=290). Brazil, 2021.
| Bladder-emptying method |
Main method |
Complementary method |
| N |
% |
N |
% |
| Normal urination |
32 |
11 |
2 |
0.7 |
| Voluntary and involuntary bladder reflex triggering |
14 |
5.1 |
2 |
0.7 |
| Bladder compression through forced effort (abdominal pressure; Valsalva maneuver) and external compression (Credé maneuver, manual pressure in the suprapubic region) |
16 |
4.5 |
11 |
3.4 |
| Clean intermittent catheterization (self-catheterization and assisted catheterization) |
214 |
74.1 |
7 |
2.4 |
| Indwelling transurethral and suprapubic bladder catheterization |
11 |
3.7 |
- |
- |
| Non-continent urinary diversion/ostomy |
1 |
0.3 |
- |
- |
Table 2.
- Association between bladder management methods and continence, n=290, Brazil, 2021.
Table 2.
- Association between bladder management methods and continence, n=290, Brazil, 2021.
| Management method\Incontinence |
Yes |
No |
p-value |
OR |
CI 95% |
| N |
% |
N |
% |
| Normal urination |
13 |
38.2 |
21 |
61.8 |
0.046¹ |
2.23 |
[1.08; 4.77] |
| Bladder reflex triggering |
13 |
86.7 |
2 |
13.3 |
0.015² |
0.18 |
[0.03; 0.67] |
| Bladder compression |
15 |
55.5 |
12 |
44.5 |
0.999¹ |
1.01 |
[0.45; 2.23] |
| Intermittent catheterization |
130 |
59.1 |
90 |
40.9 |
0.054¹ |
0.56 |
[0.32; 0.97] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).