1. Historical Perspective
The cardiopulmonary Resuscitation (CPR) procedure is practiced worldwide as a lifesaving skill. If initiated earlier in cardiac arrest, CPR can improve chances of survival [
1]. Historically, any attempt to revive the moribund was deemed unethical, even blasphemous in society, as the reversal of death was considered the divine ability of God despite resuscitation by humans well documented and supported in religious books [
2,
3]. The ancient writings by the Egyptians and Greeks around the 30
th century BCE (Before Common Era) described theories of respiration and revival techniques such as inversion or rectal fumigation. These scripts are highlighting human desire to prevent the loss of life and loved ones despite contrary beliefs and superstitions, as described by William Shakespeare in his phenomenal play: "O, that I could call these dead to life!" [
2]. In the Hebrew Bible, around 8
th century BCE, the first written account of a resuscitation attempt is attributed to the Prophet Elijah [
4], who delivered rescue breaths from his mouth into the mouth of a child who was dying; "And when Elisha came into the house, behold, the child was dead and laid upon his bed… He went up, and lay upon the child, and put his mouth upon his mouth … and the flesh of the child waxed warm… and the child opened his eyes." (Kings 4:34-35). Among the other religious doctrines, The Holy Quran outlines the broad principle in the verse…...whoever saved a single life, it is as if he’d saved the entire mankind " [The Qur'an, 5:32] [
5]. Hippocrates (460-375 BCE) advocated for cannulation (tracheal tubing) whereas Galen described the heart was the furnace of the heat required for the continuity of life [
6]. Based on similar observations, it was concluded that the body became lifeless once cold hence, connecting heat with life was integral part of human saving. Flagellation (whipping) was based on the same principle to compress the chest to save the victim
2. Around 1000 CE (Common Era), the first case of an ‘oral airway’ was experimented by Ibn-e-Sina (Avicenna) and reported as; "When necessary, a cannula of gold, silver or another suitable material is advanced down the throat to support inspiration." [
7]
The first recorded mouth-to mouth resuscitation in the medical literature was done by surgeon William Tossach on patient James Blair [
8]. Mouth-to-mouth breathing for resuscitation of drowning victims was officially recommended in 1740 for the first time in history by the Paris Academy of Sciences [
9]. Philippus Paracelsus (1493-1541) used a bag-like device to blow air (Fire Bellows) into the lungs through the patient's mouth which credited him the pioneer of first mechanical ventilator in the history [
10]. Working along the same lines, the first ‘tracheostomy’ was performed by a famous anatomist Vesalius A [
11]. In 1628 William Harvey an English Physician, was the first person to notice the cardiac systole and diastole [
12]. However, even in those days, the medical authorities seemingly unaware of the anatomy of the respiratory system did not appreciate the need to extend the victim's neck and lift the jaw to obtain a clear airway.
2. Methods: SMEAR Classification System
The conventional CPR is based on performing manual chest compressions while maintaining airway and delivering effective breaths. Over the last few decades, however, a new era of medical advancements has been ushered in, pioneered by the availability of state-of-the-art resources including virtual techniques and artificial intelligence. Despite these advancements, a comprehensive and unified system categorizing the diverse CPR techniques and devices is notably absent in existing medical literature. This gap presents a challenge, hindering consistent understanding and communication of these lifesaving procedures within academia and public at large.
To address this deficiency, we conducted an extensive review of current literature, utilizing databases such as PubMed, Scopus, Web of Science, MEDLINE, and Cochrane Library. This search was conducted in October and November of 2022, focused on gathering comprehensive data about existing CPR techniques, devices, and biotechnological advancements. Additionally, we conducted google searches to identify the manufacturers of the devices summarized in
Table 1.
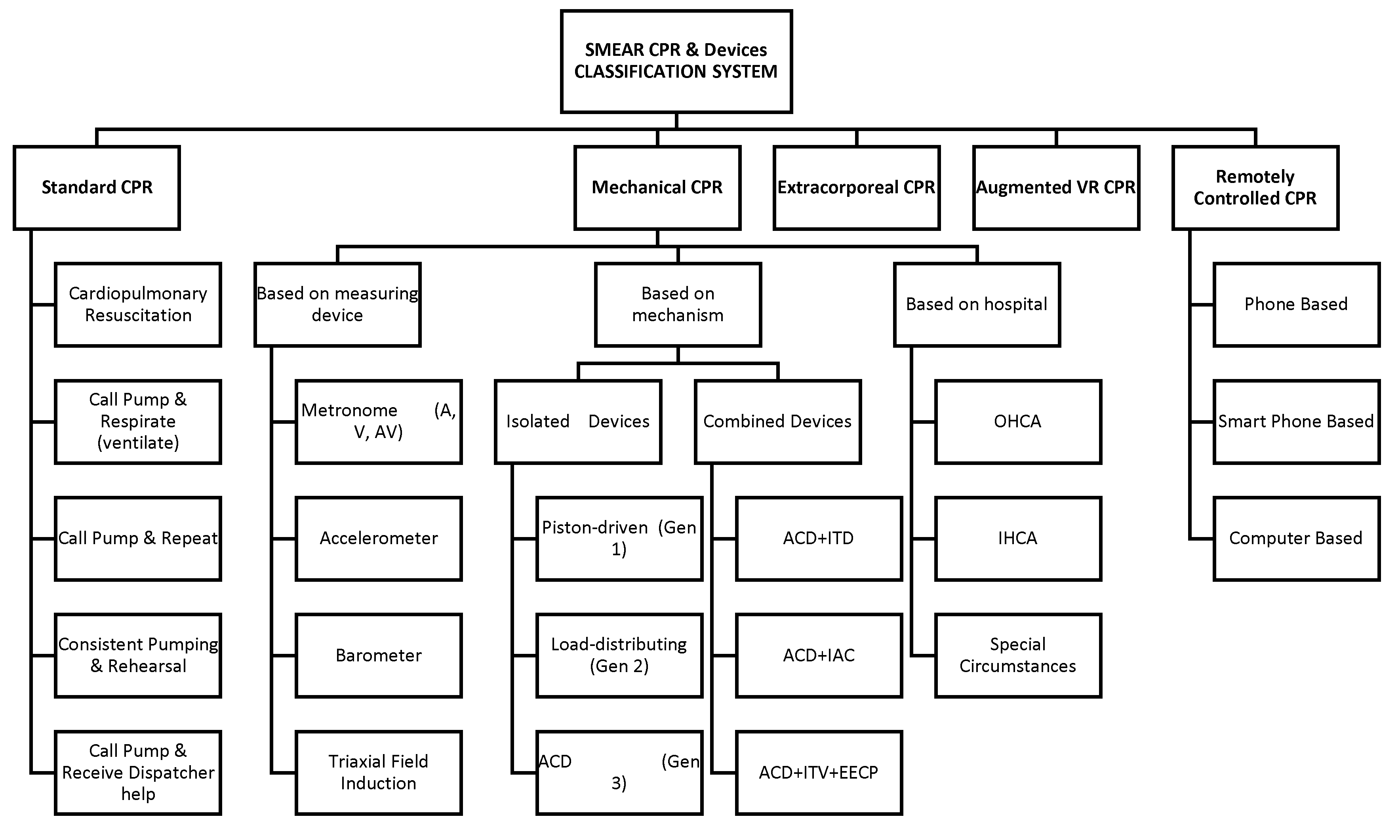
Our proposed mnemonic-based classification system, SMEAR (Standard, Mechanical, ECMO assisted, Augmented and virtual and Remote) fills this gap effectively, offering a comprehensive, easy-to-memorize model that considers recent advancements in CPR delivery mechanisms (
Figure 1). This represents a significant stride forward, streamlining education, practice, and research in resuscitation methods.
2.1. Standard CPR (S-CPR)
Standard cardiopulmonary resuscitation (S-CPR) combines external chest compressions with sustained positive pressure ventilation to preserve blood flow and oxygenation to essential organs following cardiac arrest [
13]. This technique was initially delineated by Kouwenhoven in 1960 [
14]. While some reviewers employ the term S-CPR to refer to Active Compression-Decompression (ACD), in our work, we use it exclusively to describe manual CPR to eliminate ambiguity. Despite the advances in resuscitation medicine, only marginal improvements in survival rates have been observed, leading researchers to investigate alternative CPR methods and devise supportive ventilation and circulatory devices [
15]. A significant challenge in this realm is conveying this knowledge to the public in a manner that is straightforward, comprehensible, and pragmatic. Consequently, we recommend distinct CPR terminologies based on the individual’s background and expertise:
Cardiopulmonary Resuscitation
For trained medical professionals, such as doctors, nurses & paramedics, in a well-equipped environment.
Call Pump & Respirate (Ventilate)
Aimed at less experienced medical staff or those with limited medical training (e.g., allied health staff) and those lacking specialized facilities. Also appropriate for laypeople with formal CPR training and foundational understanding.
Call Pump & Repeat
Intended for general public without prior experience or foundational knowledge in CPR.
2.2. Mechanical CPR
High-quality CPR is paramount for survival following cardiac arrest [
16]. However, manual chest compressions frequently fall short due to reasons such as fatigue, inconsistency, or practical challenges. Mechanical CPR devices can overcome these obstacles with the potential of achieving improved outcomes [
17].
We have categorized mechanical devices based on three distinct criteria. Effective chest compressions remain the cornerstone of successful CPR as they significantly influence both survival rates and neurological outcomes. According to guidelines, adults necessitate chest compressions that are 5 cm deep at rate of 100 per minute, a task that is physically strenuous. Without any real time-feedback, even the experienced emergency responders can only maintain 40% of their compressions at optimal level due to fatigue [
18]. In this context, the specific devices can provide important feedback which can help deliver high quality CPR.
2.2.1. AED-Associated & Non-Associated Active Compression & Passive Decompression (ACPD) Devices
Non-Automated External Defibrillator (AED) devices employ Active chest Compression, and passive Decompression (ACPD). The technologies supporting these devices vary widely, from a simple metronome to sophisticated electromagnetic sensing. To date, nine such feedback devices have been tested in both simulation and clinical settings. Integrating these devices with AED can improve outcomes. The audio-visual feedback system of AEDs has shown to elevate the quality of CPR during both training and clinical practice [
19,
20]. These AED-integrated devices can be further classified based on feedback sensor and compression mechanisms.
2.2.2. Classification Based on Feedback Sensor
Metronome (Audio, Visual, Audiovisual)
A Metronome is a device that produces rhythmic beats at regular intervals. Maintaining the optimal compression rate of 100 to 120 per minute can be challenging without feedback. Metronomes embedded in CPR devices can help healthcare professionals maintain this recommended pace. These come in three variations, i.e., audio, visual, and audio-visual. The Pocket CPR and Voice Advisory manikin-VAM (Laerdal, Orpington, UK) are examples of audio-centric devices, while the Anne Skillmeter (Laerdal, Orpington, UK) is visually oriented. Devices like CPR RsQ Assist [
21] combine both modalities.
Accelerometer
Accelerometers in CPR devices help enable feedback on the rate and depth of chest compressions based on their ability to sense small tilt changes in the CPR device using the narrow bandwidths typical of human motion. CPR devices that are accelerometer-based include Q-CPR, from Philips, and CPR-D-Padz, from Zoll.
Barometer
A single-barometer-air-chamber design used by Wan et al [
18] is small, simple, and low-cost. Not only it can be easily integrated into established emergency first aid kits and AED boxes, it can also be incorporated into small personal items like keychains for better accessibility. Embedding the device into manikins, which currently have limited feedback [
18], could enhance training efficacy.
Triaxial Field Induction (TFI)
The TrueCPR provides high-quality feedback both in real-time and post-resuscitation . It utilizes novel Triaxial Field Induction (TFI) technology, shown to provide precise depth measurement and help guide rescuers to perform compressions of at least 2 inches (5 centimetres) in depth. TFI measures changes in a very low-energy 3-D magnetic field generated by a reference pad placed beneath the patient and a sensor on the patient’s chest, continuously calculating the changing distance between the two points as a caregiver performs manual chest compressions. Unlike accelerometer-based devices, which have been shown to overestimate chest compression depth on soft surfaces, TrueCPR measures the relative distance from the chest sensor to reference pad, regardless of underlying texture and patient movement. Thus, it can be used on surfaces such as a hospital gurney, mattress or in a moving ambulance [
22].
2.2.3. Based on Compression Mechanism
While sensors in devices are primarily for feedback, the actual chest compression is facilitated through distinct mechanisms. Accordingly, these devices are further subclassified into “isolated” and “combined” based on their built-in-mechanisms.
2.3. Isolated Devices
Piston-driven (1st Generation)
This is a first-generation mechanical device based on the cardiac pump theory. It employs single-point active compression/decompression (Piston driven-CPR) on the sternum antero-posteriorly using a piston mounted on an arm. It is operated either through a battery or pneumatic power derived from compression [
23], Life-Stat, formerly known as Thumper [
24], is the commonly known piston device [
25].
Load-distributing (2nd Generation)
The second-generation load-distributing bands operate based on the thoracic pump theory. These devices achieve circumferential thoracic compression on the anterior-anterolateral thorax. This compression alters intra-thoracic pressures, facilitating flow of blood [
26].
ACD (3rd Generation)
The Active Compression-Decompression (ACD) device is a hand-held device equipped with a suction cup that adheres to the chest. It also has a gauge to indicate the force required for effective compression and decompression. The ACD CPR device, when used, creates a vacuum within the thorax with each chest wall decompression. However, the hemodynamic advantages of this vacuum can be compromised by the influx of inspiratory gas [
27].
2.4. Combination Devices
ACD+ITD
The Impedance Threshold Device (ITD) is a small, 35-mL, device that fits on a face mask or an endotracheal tube. The pressure-sensitive valves within the ITD impedes the influx of inspiratory gas during chest wall decompression, thereby augmenting the amplitude and duration of the vacuum within the thorax [
28,
29,
30,
31]. This vacuum draws more venous blood back into the heart, resulting in increased cardiac preload, followed by improved cardiac output and vital organ perfusion. ResQPump (ZOLL) is an active compression-decompression (ACD) hand- held device and ResQPod (ZOLL) is an inspiratory impedance threshold valve device (ITD).
ACD+IAC
The Interposed Abdominal Compression CPR (IAC) has been discussed in a case report published in the Western Journal of Emergency Medicine for out of hospital cardiac arrest victim failing Traditional CPR and documented survival of recipient [
32]. The procedure requires two providers: one for chest compressions and other for abdominal compressions. The abdominal compressor performs CPR with their hands about 5cm above the umbilicus and compressing about as deep as you would need to palpate the abdominal aorta pulse. Both operators compress at the same rate and alternate their compressions. Theoretically, the abdominal compressor is acting as an external intra-aortic balloon pump. By compressing the aorta during diastole there is retrograde blood flow back into the coronaries and brain [
33]. Additionally, abdominal compression increases venous return and promotes forward flow of the intrathoracic blood pool [
34]. Also abdominal compression increases venous return and improves stroke volume [
35]. Most reported cases have shown minimal intra-abdominal injuries, with the exception of one paediatric traumatic pancreatitis case [
36]. A recent review in Resuscitation highlighted the potential of IAC-CPR in achieving a higher rate of return in spontaneous circulation (ROSC) compared to standard CPR [
37].
ACD+ITV+EECP
The Enhanced External Counter Pulsation (EECP) treatment is an FDA-approved outpatient therapy for chronic stable angina. It uses pressure on the lower limbs to improve blood flow in patients with long-term symptoms of heart disease, such as angina [
38]. It has been added to CPR device and has led to improved outcome in animal studies [
39]. The ITV (Inspiratory Impedance threshold Valve) is inserted within the respiratory circuit, between the ventilation bag and the endotracheal tube, face mask, esophageal tracheal airway (Combitube) or Laryngeal Mask Airway (LMA). The ITV enhances venous return during the chest recoil phase of CPR and thus primes the heart for the subsequent CPR compression. Additionally, it is equipped with a safety check valve that activates if patients initiates independent breathing.
Mechanical devices may be a useful alternative or addition to manual chest compressions when it is challenging to deliver high-quality manual without interruptions. Mechanical devices are not associated with better survival when used during transport in a meta-analysis [
26]. In a study conducted in Taiwan however demonstrated increased rate of ROSC [
40] in patient suffering out of hospital cardiac arrest. Mechanical devices are associated with better survival in prolonged resuscitation, but worse survival when fibrinolytics are used for coronary events [
41]. Conflicting results are available for mechanical CPR in special circumstances like organ donation [
42], mechanical CPR before Extracorporeal CPR cannulation and earlier vs late deployment of mechanical CPR. In any context where mechanical devices are utilized, clinicians should prioritize uninterrupted chest compressions [
17].
2.5. Extracorporeal CPR (ECPR)
Extracorporeal-CPR (ECPR), incorporates Extracorporeal membrane oxygenation (ECMO) into CPR process, is being increasingly used in out of hospital cardiac arrest [
43,
44,
45]. Its therapeutic benefits are linked to instant and uninterrupted chest compressions (CC), besides early implementation. Mechanical CCs can alleviate some of the limitations of traditional manual methods, such as operator fatigue and intensive manual effort, ensuring consistent blood perfusion to vital organs. ECPR’s successful deployment demands skilled staff and state of the art transportation system supported by ECPR cardiac arrest center [
46]. However, recent randomized controlled trials on ECPR however have shown mixed results in terms of survival and neurologic outcomes [
47,
48,
49].
2.6. Augmented VR CPR
Augmented Virtual Reality (VR) CPR is used to develop an augmented reality version of Hands-Only CPR delivery. This also offers a cost-effective method for public education. This can be facilitated using cutting-edge Virtual devices or Virtual CPR trainers. There are two main categories of Augmented Reality (AR): marker-less AR, and marker-based AR. By definition, marker-less AR is technology that does not need any specific point beforehand for locating the virtual object [
50]. The location for placing the virtual object is from the real-world environment, such as the coordinates from GPS devices or the sensor in visual devices. In contrast, marker-based AR is technology that requires a pre-assigned location embedded into the physical object, the marker, for locating the position of the virtual object [
51]. There are many types of virtual reality scenarios that can incorporate this, such as Augmented (Enhanced) Reality, Virtual Reality, Desktop Virtual Reality (Non-Immersive VR), Immersive Virtual Reality, QuickTime Virtual Reality (QTVR), and Telepresence. A notable application of Augmented VR CPR is the Hands-Only CPR Augmented Reality application developed, collaboratively by American Heart Association (AHA) and Level Ex (Chicago, IL) [
52] for training and delivery of CPR.
2.7. Remotely Controlled or Tele-Assisted CPR
Technological advances have expanded the avenues for initiating and guiding CPR remotely, particularly for untrained bystanders. These mechanisms span from the simplicity of a 911 call to intricate applications delineating CPR techniques in-depth.
Pertinent apps/software include CPR through mHealth [
53], Pocket CPR for smartphones [
54], and PulsePoint [
55] to find the nearest AED/trained rescuer. Online CPR Training, provided by organizations like American Health Training [
56] and American Red Cross [
57] remains the invaluable resource available to larger audiences for either voluntary or mandatory trainings.
3. Limitations
Certain innovative methods such as augmented virtual reality CPR are primarily being used for training purposes, with limited application currently in actual resuscitative events. Our classification system does not account for emerging technologies and methods that are still under investigation. Although our literature review was comprehensive, it mainly focuses on the devices and techniques that are currently in use without individual and head-to-head comparison of their effectiveness. Hence, it inherently excludes promising experimental advancements that could influence future resuscitation practices.
4. Conclusion
Over last few decades there have been advancements in the CPR techniques and innovations in the biotechnology led to introduction of devices that can improve outcomes in victims of cardiac arrest. We propose mnemonic based SMEAR classification (Summarized in
Table 1) which can be used for academic reference, aiming to educate audiences on the diverse CPR techniques and devices with their respective applications.
Author Contributions
MI and LI: Literature review, drafted manuscript. SH and MH: Critical review of the manuscript. All authors contributed to the editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Ethical Statements
Development of this manuscript required extensive literature review and did not involve any human research subject, hence is exempt for review from Institution Ethical Committee/Institutional Review Board (IRB) This is original review article. There is no intentional overlap with previous publications. All sources of information are appropriately cited. Manuscript, including related data, figures and tables have not been published previously. Manuscript is not under consideration elsewhere.
Non-standard Abbreviations and Acronyms
CPR: Cardiopulmonary Resuscitation
S-CPR: Standard Cardiopulmonary Resuscitation
ACD: Active Compression-Decompression
TFI: Triaxial Field Induction
PD: Piston Driven
LDB: Load Distributing Band
CC: Chest Compression
ITD: Impedance Threshold Device
LMA: Laryngeal Mask Airway
IAC: Interposed Abdominal Compression
TFI: Triaxial Field Induction
EECP: Enhanced External Counter Pulsation
ECPR: Extracorporeal Cardiopulmonary Resuscitation
ECMO: Extracorporeal Membrane Oxygenation
VR: Virtual Reality
AR: Augmented Reality
AHA: American Heart Association
OHCA: Out of Hospital Cardiac Arrest
IHCA: In-Hospital Cardiac Arrest
RCA: Refractory Cardiac Arrest
QTVR: QuickTime Virtual Reality
AED: Automated External Defibrillator
ITV: Impedance Threshold Valve
References
- Part 1: Introduction. Circulation. 2005;112(24_supplement):IV-1. [CrossRef]
- Evolution of Cardiopulmonary Resuscitation * An Historical. studylib.net. Accessed December 20, 2022. https://studylib.net/doc/7045389/evolution-of-cardiopulmonary-resuscitation---an-historical.
- Eisenberg MS. History of the Science of Cardiopulmonary Resuscitation. In: Ornato JP, Peberdy MA, eds. Cardiopulmonary Resuscitation. Humana Press; 2005:1-9. [CrossRef]
- Eisenberg MS, Baskett P, Chamberlain D. A history of cardiopulmonary resuscitation. In: Chamberlain DA, Halperin HR, Kern KB, Paradis NA, Wenzel V, eds. Cardiac Arrest: The Science and Practice of Resuscitation Medicine. 2nd ed. Cambridge University Press; 2007:3-25. [CrossRef]
- Surah Ma’idah Ayat 32 (5:32 Quran) With Tafsir. My Islam. Accessed December 20, 2022. https://myislam.org/surah-maidah/ayat-32/.
- Aird WC. Discovery of the cardiovascular system: from Galen to William Harvey. J Thromb Haemost. 2011;9(s1):118-129. [CrossRef]
- Szmuk P, Ezri T, Evron S, Roth Y, Katz J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the Space Age. Intensive Care Med. 2008;34(2):222-228. [CrossRef]
- History of CPR. cpr.heart.org. Accessed December 20, 2022. https://cpr.heart.org/en/resources/history-of-cpr.
- Baker AB. Artificial respiration, the history of an idea. Med Hist. 1971;15(4):336-351.
- Davis A. Paracelsus: a quincentennial assessment. J R Soc Med. 1993;86(11):653-656.
- Zampieri F, ElMaghawry M, Zanatta A, Thiene G. Andreas Vesalius: Celebrating 500 years of dissecting nature. Glob Cardiol Sci Pract. 2015;2015(5):66. [CrossRef]
-
On the Motion of the Heart and Blood in Animals. Accessed December 20, 2022. https://universitypressofamerica.com/ISBN/9780879758547/On-the-Motion-of-the-Heart-and-Blood-in-Animals.
- Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR Overview. Circulation. 2010;122(18_suppl_3):S676-S684. [CrossRef]
- Kouwenhoven WB, Jude JR, Knickerbocker GG. CLOSED-CHEST CARDIAC MASSAGE. JAMA. 1960;173(10):1064-1067. [CrossRef]
- Cave DM, Gazmuri RJ, Otto CW, et al. Part 7: CPR Techniques and Devices. Circulation. 2010;122(18_suppl_3):S720-S728. [CrossRef]
- Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the HospitalCirculation . 2013;128(4):417-435. [CrossRef]
- Poole K, Couper K, Smyth MA, Yeung J, Perkins GD. Mechanical CPR: Who? When? How? Crit Care. 2018;22(1):140. [CrossRef]
- Wan Q, Vogt D, Dubrovsky Z. Low-Cost, Small-Footprint, Barometer-Based CPR Feedback Device1. J Med Devices. 2014;8(3):030950. [CrossRef]
- Fischer H, Gruber J, Neuhold S, et al. Effects and limitations of an AED with audiovisual feedback for cardiopulmonary resuscitation: a randomized manikin study. Resuscitation, 2011;82(7):902-907. [CrossRef]
- Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation, 2009;80(7):743-751. [CrossRef]
- Yuksen C, Prachanukool T, Aramvanitch K, Thongwichit N, Sawanyawisuth K, Sittichanbuncha Y. Is a mechanical-assist device better than manual chest compression? A randomized controlled trial. Open Access Emerg Med OAEM, 2017;9:63-67. [CrossRef]
- Beesems SG, Koster RW. Accurate feedback of chest compression depth on a manikin on a soft surface with correction for total body displacement. Resuscitation. 2014;85(11):1439-1443. [CrossRef]
- Aygun M, Erten Yaman H, Genc A, Karadagli F, Baris Eren N. Mechanical Chest Compression Devices: Historical Evolution, Classification and Current Practices, A Short Review. Eurasian J Emerg Med. 2016;15(2):94-104. [CrossRef]
- Lu X guang, Kang X, Gong D bo. The clinical efficacy of Thumper modal 1007 cardiopulmonary resuscitation: a prospective randomized control trial. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue Chin Crit Care Med Zhongguo Weizhongbing Jijiuyixue. 2010;22(8):496-497.
- Leong SHB. Mechanical CPR. Singapore Med J. 2011;52(8):592-595.
- Ong MEH, Mackey KE, Zhang ZC, et al. Mechanical CPR devices compared to manual CPR during out-of-hospital cardiac arrest and ambulance transport: a systematic review. Scand J Trauma Resusc Emerg Med. 2012;20(1):39. [CrossRef]
- FACEP RJF MD. Improving Survival from Cardiac Arrest Using ACD-CPR + ITD. JEMS: EMS, Emergency Medical Services - Training, Paramedic, EMT News. Published November 23, 2014. Accessed December 20, 2022. https://www.jems.com/patient-care/improving-survival-cardiac-arrest-using-0/.
- Lurie KG, Zielinski T, McKnite S, Aufderheide T, Voelckel W. Use of an inspiratory impedance valve improves neurologically intact survival in a porcine model of ventricular fibrillation. Circulation. 2002;105(1):124-129. [CrossRef]
- Aufderheide TP, Lurie KG. Vital organ blood flow with the impedance threshold device. Crit Care Med. 2006;34(12 Suppl):S466-473. [CrossRef]
- Yannopoulos D, Sigurdsson G, McKnite S, Benditt D, Lurie KG. Reducing ventilation frequency combined with an inspiratory impedance device improves CPR efficiency in swine model of cardiac arrest. Resuscitation. 2004;61(1):75-82. [CrossRef]
- Aufderheide TP, Nichol G, Rea TD, et al. A Trial of an Impedance Threshold Device in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2011;365(9):798-806. [CrossRef]
- Westjem. Interposed Abdominal Compression CPR for an Out-of-Hospital Cardiac Arrest Victim Failing Traditional CPR. The Western Journal of Emergency Medicine. [CrossRef]
- Sack JB, Kesselbrenner MB, Bregman D. Survival From In-Hospital Cardiac Arrest With Interposed Abdominal Counterpulsation During Cardiopulmonary Resuscitation. JAMA. 1992;267(3):379-385. [CrossRef]
- Rudikoff MT, Maughan WL, Effron M, Freund P, Weisfeldt ML. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation. 1980;61(2):345-352. [CrossRef]
- 35. Ward KR, Sullivan RJ, Zelenak RR, Summer WR. A comparison of interposed abdominal compression CPR and standard CPR by monitoring end-tidal PCO2. Ann Emerg Med, 1989;18(8):831-837. [CrossRef]
- 36. Waldman PJ, Walters BL, Grunau CFV. Pancreatic injury associated with interposed abdominal compressions in pediatric cardiopulmonary resuscitation. Am J Emerg Med, 1984;2(6):510-512. [CrossRef]
- Ghanbari Khanghah A, Moghadamnia MT, Panahi L, Pouy S, Aghajani Nargesi M, Kazemnezhad Leyli E. Effect of Interposed Abdominal Compression on Cardiopulmonary Resuscitation Outcomes; a Randomized Clinical Trial. Arch Acad Emerg Med. 2022;10(1):e57. [CrossRef]
- Arora RR, Chou TM, Jain D, et al. The multicenter study of enhanced external counterpulsation (MUST-EECP): effect of EECP on exercise-induced myocardial ischemia and anginal episodes. J Am Coll Cardiol. 1999;33(7):1833-1840. [CrossRef]
- Xiong J, Zhang W, Wei H, Li X, Dai G, Hu C. Enhanced external counterpulsation improves cardiac function in Beagles after cardiopulmonary resuscitation. Braz J Med Biol Res. 2020;53(1):e9136. [CrossRef]
- Chen YR, Liao CJ, Huang HC, et al. The Effect of Implementing Mechanical Cardiopulmonary Resuscitation Devices on Out-of-Hospital Cardiac Arrest Patients in an Urban City of Taiwan. Int J Environ Res Public Health. 2021;18(7):3636. [CrossRef]
- Gässler H, Kurka L, Rauch S, Seewald S, Kulla M, Fischer M. Mechanical chest compression devices under special circumstances. Resuscitation. 2022;179:183-188. [CrossRef]
- Mateos A, Navalpotro JM, Andres A, Abradelo M, Rio FD, Calatayud J. Mechanical CPR devices in donors after cardiac death. Resuscitation. 2014;85:S88. [CrossRef]
- Dennis M, Lal S, Forrest P, et al. In-Depth Extracorporeal Cardiopulmonary Resuscitation in Adult Out-of-Hospital Cardiac Arrest. J Am Heart Assoc. 2020;9(10):e016521. [CrossRef]
- Dennis M, Buscher H, Gattas D, et al. Prospective observational study of mechanical cardiopulmonary resuscitation, extracorporeal membrane oxygenation and early reperfusion for refractory cardiac arrest in Sydney: the 2CHEER study. Crit Care Resusc J Australas Acad Crit Care Med. 2020;22(1):26-34.
- Bartos JA, Carlson K, Carlson C, et al. Surviving refractory out-of-hospital ventricular fibrillation cardiac arrest: Critical care and extracorporeal membrane oxygenation management. Resuscitation. 2018;132:47-55. [CrossRef]
- Sinning C, Ahrens I, Cariou A, et al. The cardiac arrest centre for the treatment of sudden cardiac arrest due to presumed cardiac cause - aims, function and structure: Position paper of the Association for Acute CardioVascular Care of the European Society of Cardiology (AVCV), European Association of Percutaneous Coronary Interventions (EAPCI), European Heart Rhythm Association (EHRA), European Resuscitation Council (ERC), European Society for Emergency Medicine (EUSEM) and European Society of Intensive Care Medicine (ESICM). Eur Heart J Acute Cardiovasc Care. 2020;9(4_suppl):S193-S202. [CrossRef]
- Suverein MM, Delnoij TSR, Lorusso R, et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N Engl J Med. 2023;388(4):299-309. [CrossRef]
- Belohlavek J, Smalcova J, Rob D, et al. Effect of Intra-arrest Transport, Extracorporeal Cardiopulmonary Resuscitation, and Immediate Invasive Assessment and Treatment on Functional Neurologic Outcome in Refractory Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2022;327(8):737-747. [CrossRef]
- Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet Lond Engl. 2020;396(10265):1807-1816. [CrossRef]
- Schechter S. What is markerless Augmented Reality? 3D Cloud by Marxent. Published May 10, 2014. Accessed December 20, 2022. https://www.marxentlabs.com/what-is-markerless-augmented-reality-dead-reckoning/.
- Boonbrahm PB Charlee Kaewrat, Salin. Interactive Marker-based Augmented Reality for CPR Training. IJTech - International Journal of Technology. Accessed December 20, 2022. https://ijtech.eng.ui.ac.id/article/view/3267.
- Augmented Reality (AR) Hands-Only CPR Trainer. Center for Health Technology & Innovation. Published March 20, 2018. Accessed December 20, 2022. https://ahahealthtech.org/augmented-reality-ar-hands-only-cpr-trainer/.
- Müller SD, Lauridsen KG, Palic AH, Frederiksen LN, Mathiasen M, Løfgren B. Mobile App Support for Cardiopulmonary Resuscitation: Development and Usability Study. JMIR MHealth UHealth. 2021;9(1):e16114. [CrossRef]
- British Heart Foundation’s PocketCPR Mobile Application for iPhone and Android | Accella Accella. Accessed December 20, 2022. https://accella.net/knowledgebase/mobile-application-development/mobile-app-development-portfolio/british-heart-foundations-pocketcpr-mobile-application/.
- Building informed communities. PulsePoint. Accessed December 20, 2022. https://www.pulsepoint.org/.
- CPR Certification. American Health Training. Accessed December 20, 2022. https://www.americanhealthtraining.com/cpr-certification/.
- Red Cross Training | Take a Class | Red Cross. Accessed December 20, 2022. https://www.redcross.org/take-a-class?scode=PSG00000E017&cid=generator&med=cpc&source=google&gclid=Cj0KCQiA14WdBhD8ARIsANao07jjgA7f1_qQR7Lie8tltN6cBG3RYOA91iJM5Ghn_gAZM1NzaXfm0XYaAqWPEALw_wcB&gclsrc=aw.ds.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).