1. Introduction
The obstructive sleep apnea (OSA) syndrome is a pathological condition characterized by recurrent episodes of collapse of the upper airways, leading to a reduction in blood oxygen levels and usually culminating in a transient awakening episode; It is a major risk factor for the development of cardiovascular and metabolic diseases resulting in reduced life expectancy and significant economic and social implications [
1]
The symptomatology that most frequently describes this syndrome is both nocturnal and diurnal: snoring, the witnessed apnoeas and daytime drowsiness are the pivotal symptoms. The crucial instrumental examination for studying sleep disorders is Polysomnography that documents the pattern and changes in a few physiological parameters during different stages of sleep. The pathogenesis of OSAS is related to several factors some of which are in turn associated with dento-skeletal malformations, conditions caused by non-harmonic development of the upper jaw and/or mandible that lead a narrowing of the upper airways and that exposed to the risk of developing this syndrome [
2].
It is estimated that nearly 1 billion adults between the ages of 30 and 69 worldwide are affected by obstructive sleep apnea. In Italy, according to Benjafield’s study the 20.5% of the population between 30 and 69 years old has an AHI (Apnoea-Hypopnoea index) of five events per hour and 12% has an AHI of fifteen or more events per h. Apnea was characterized by the absence of airflow for more than 10 seconds. Hypopneas were defined as any reduction in airflow exceeding 50%, lasting longer than 10 seconds, and leading to either arousal or oxyhemoglobin desaturation. The presence of OSAS is not always correlated to the presence of symptoms of which the patient is aware, which is why it’s ad under-diagnosed and under-treated condition. Many studies shows that patients affected by a dentoskeletal malocclusion have a major risk to suffer from OSAS or from a chronic sleep-breathing disorder (SBD) [
3].
Ristow et al. affirmed that patient facial profile is a pivotal element in determining the risk of OSAS and that many patients with OSA present maxillary or mandibular hypoplasia [
4].
Most of the studies that describe the connection between OSAS and dentoskeletal malformation refers to patient affected by severe OSA case(AHI < 5)) [
5], less is known about the incidence of silent OSAS in patient affected from a dentoskeletal malformation candidate for a surgical correction.
Posnick’s study found “silent” obstructive sleep apnea to be frequent in the maxilla-mandibular malformed patients; The prevalence in subjects with retrusive jaw patterns surpassed the estimated prevalence of OSA in the general population) [
6].
The purposes of this observational retrospective study was to evaluate the incidence of silent Obstructive Sleep Apnea in patients with dento-skeletal malformation that undergo Orthognathic Surgery and the potential change in AHI pre and post-operatively.
Orthognathic surgery is designed to reposition the jaw, mandible, and chin with the purpose of enhancing facial balance and proportions and it’s known that skeletal base movements can have a significant impact on the upper airway volume, which is highly influenced by anatomical structures, therefore, the study of the airway becomes essential in successful surgical planning
2. Materials and Methods
A retrospective cohort study was designed. The study considered 71 patients treated for dento-skeletal malformation by the Complex Operating Unit of Maxillofacial Surgery at the IRCCS Policlinico Universitario Agostino Gemelli Foundation in Rome between January 1, 2020 and December 31, 2022.
The inclusion criteria were:
-Patients affected by a dento-skeletal malformation;
-Patients candidated to orthognathic surgery;
-Patients older than 18 years of age;
And exclusion criteria:
-Anamnesis of respiratory system diseases;
-Diagnosis of OSA;
-Patients with previously treated dento-skeletal malformations, related to genetic syndromes, post-traumatic or related to neoplastic diseases.
-Patient with BMI variation between pre and post operative phase.
All patients underwent surgery of LeFort I osteotomy, bilateral mandibular sagittal osteotomy, and possibly associated genioplasty. The surgeries were combined in various ways depending on the surgical schedule.
All patients underwent Epworth Sleepness Scale (ESS) testing and Polysomnography evaluating the AHI (Apnea-Hypopnea Index) and RDI (Respiratory Distress Index) indices. BMI (Body-Mass-Index) was also calculated.
At least 6 months after surgery, patients underwent Polysomnography again to assess any improvement or worsening of the AHI index.
General parameters such as sex, age, and general medical history were collected. A standard medical checkup was then performed.
Each patient was given an identification code so that the data could be processed anonymously.
The results of the study visit were entered into a database (Microsoft Excel - Microsoft 365) so that statistical analysis could then be carried out.
Predictive variables were chosen for our study and were grouped into the following categories:
-Age at the time of intervention.
-Gender.
-Pattern of dento-skeletal deformity.
-Presence or absence of maxillary hypoplasia.
-BMI
-Apnea-Hypopnea Index (AHI) pre orthognathic surgery.
-Apnea-Hypopnea Index (AHI) post orthognathic surgery.
We used the following AHI evaluation criteria:
-AHI > 5 patient with OSA
-4<AHI<5 Borderline patient
-AHI< 4 non-OSA patient
The prevalence of undiagnosed OSAS in subjects evaluated for dento-skeletal malformations and the prevalence of OSAS in subjects undergoing orthognathic surgery compared with the general population.
Our analysis refers to two specific periods, the pre- and postoperative periods.
In the pre-surgery period:
-Relationship between AHI between general cohort and general population
-Relationship between AHI > 5 and malformations, for both DSC IIs and DSC IIIs
-Relationship between AHI > 5 and malformed, in III DSC with maxillary hypoplasia, both compared to III CDS and to the general cohort
-Relationship between 4<AHI<5 and malformed, for both II DSC and III DSC
-Relationship between AHI 4<AHI<5 and malformed, in III DSC with maxillary hypoplasia, both compared with III DSC and with the cohort overall
In the post-surgery period:
-Relationship between AHI between general cohort and general population
-Relationship between AHI > 5 and malformations, both for II DSC and III DSC
-Relationship between AHI > 5 and malformed, in III DSC with maxillary hypoplasia, both compared to III DSC and to the general cohort
-Relationship between 4<AHI<5 and malformed, for both II DSC and III DSC
-Relationship between 4<AHI<5 and malformed, in III DSC with maxillary hypoplasia, both compared with III DSC and compared with the cohort in general.
After that in order to express quantitatively the presence and any intensity of the link between two variables, the correlation index was calculated.
The variables considered were:
-Patients with AHI>5 and dento-skeletal class II or III
-Patients with AHI<5 but >4 (borderline) and dento-skeletal class II or III
The correlation array, also called the covariance array, was then used to calculate the multiple correlation between:
-DSC II, BMI, age and AHI
-DSC III, BMI, age and AHI
Moreover, the presence of any difference between pre- and post-surgery AHI was examined and the percentage of patients whose AHI value worsened post orthognathic surgery was calculated.
Linear plots were constructed based on the data that emerged.
3. Results
In total, we considered 71 patients including 35 men and 36 women ranging in age from 18 to 55 years with a mean age of 26.2 years. 21 patients (29.5%) had class II dento-skeletal malformation according to Angle. 50 (70.5%) patients had class III dento-skeletal malformation according to Angle. Of these, 6 (8.4% of the general cohort and 12% of patients with III DSC) had maxillary hypoplasia calculated on cephalometric criteria [
7].
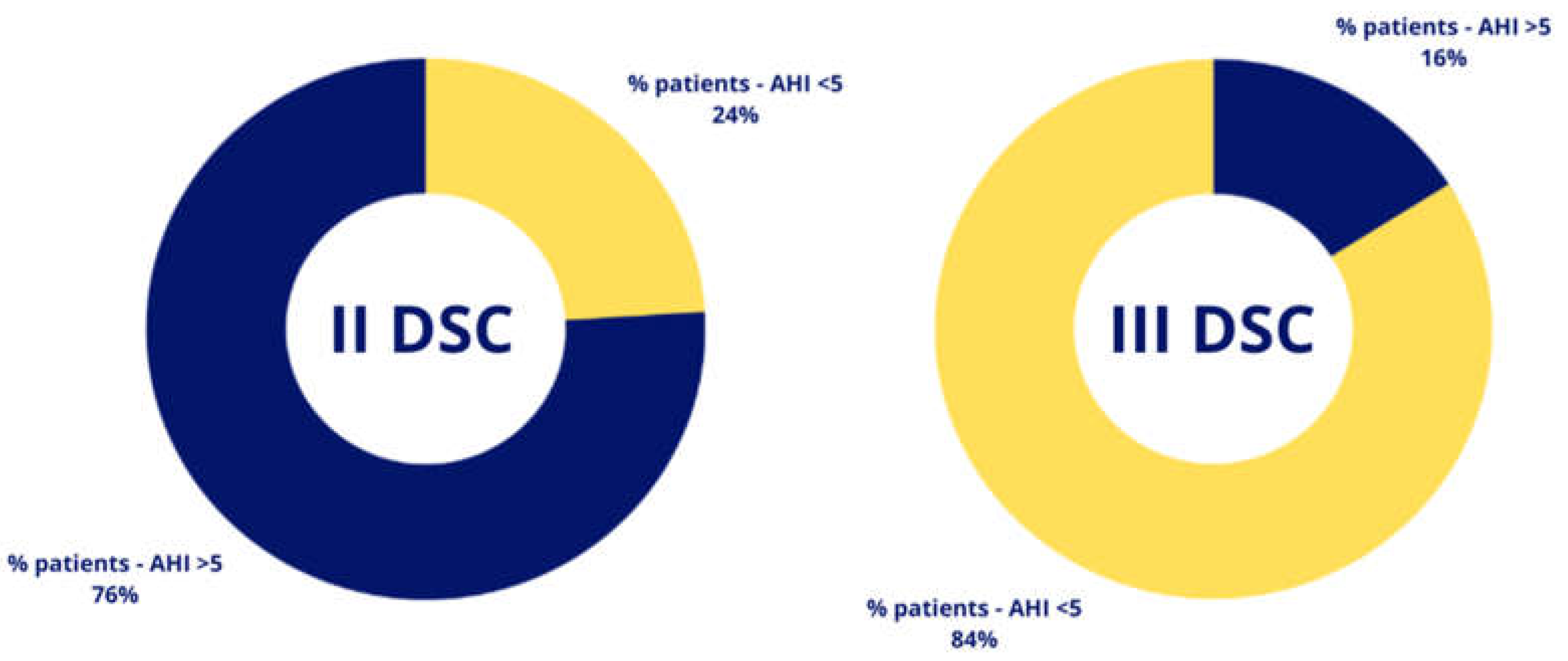
Pre Surgery
We calculated the number of malformed patients examined who had AHI>5 and a percentage of 33% resulted.
In particular 16 II DSC (76%) patients had an AHI>5 and 8 patients with III DSC (16%) had an AHI>5.
Of the patients with III DSC, we also highlighted the possible presence of maxillary hypoplasia and calculated the percentage of patients with AHI>5 falling into this category compared with the total number of patients with III DSC in the study and compared with the total number of malformed patients considered in the study.
It was found that 62% of patients with III DSC and AHI>5 were affected by maxillary hypoplasia. Next, calculating the ratio of patients with maxillary hypoplasia to the general cohort with AHI>5 showed that 25% had maxillary hypoplasia.
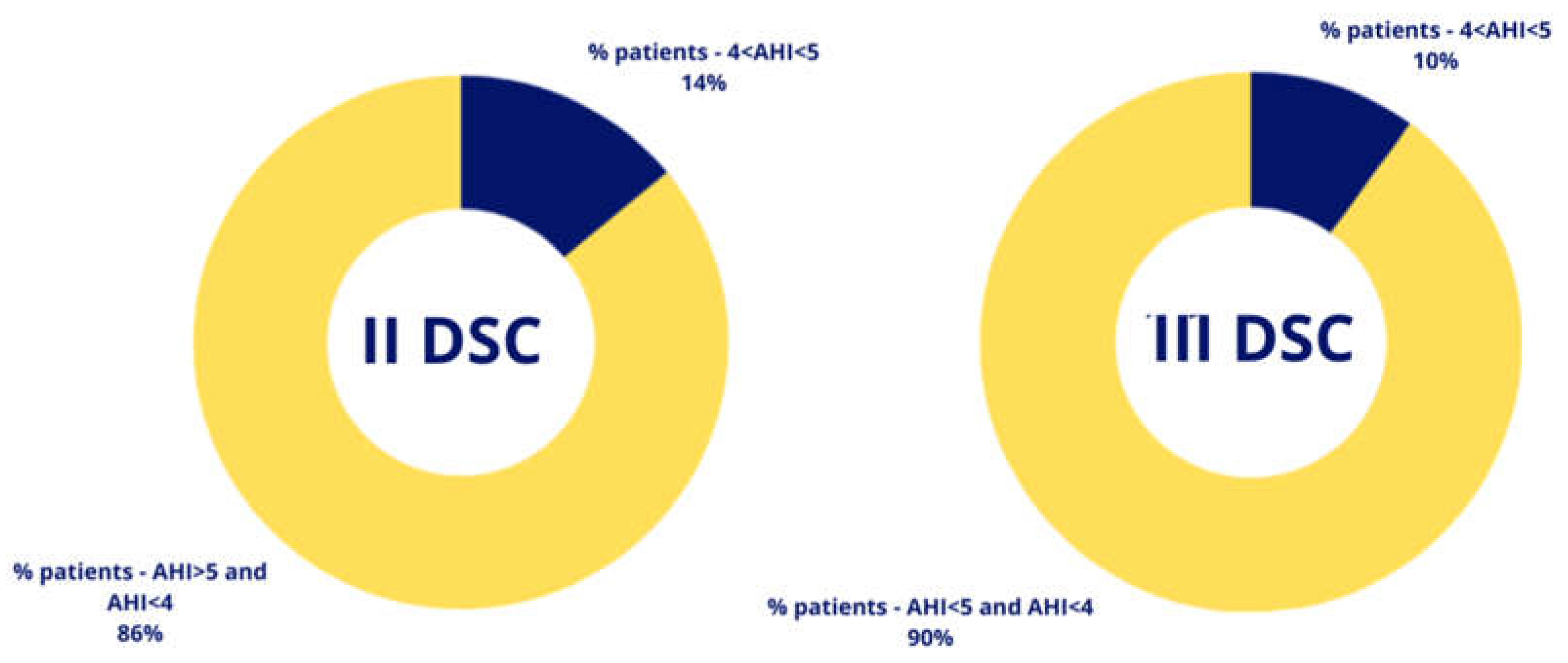
We also considered an AHI that was not strictly pathological but at the borderline <5 but >4 and it turned out that of 21 patients with II DSC, 3 had a 4<AHI<5 so 14% while out of 50 patients with III DSC 5 had a 4<AHI<5 so 10%.
Among the patients with III DSC and borderline AHI only one out of 5 also had maxillary hypoplasia and compared to the total malformed patients taken into the study with borderline AHI it was found that 12.5% of the patients also had maxillary hypoplasia.
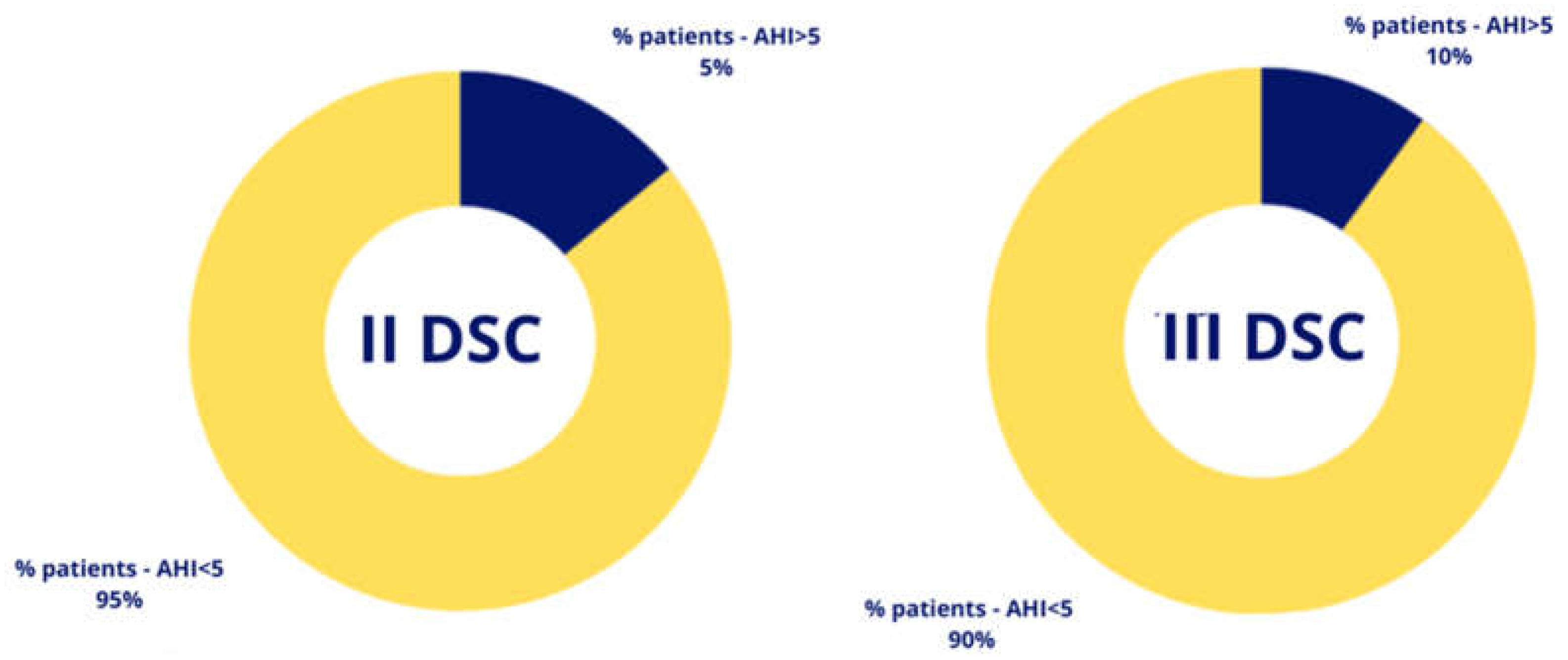
Post Surgery
8% of the malformed patients examined had an AHI>5.
Out of 21 patients with II DSC only one presents in the postoperative period with an AHI>5 thus representing a percentage of 5%
Out of 50 patients with III CDS, 5 of them have an AHI>5 in the postoperative representing a percentage of 10%.
Considering the patients with III DSC and AHI>5 in the postoperative period 80% of the patients have maxillary hypoplasia (4 out of 5 patients) while considering the total malformed patients examined with AHI>5 in the postoperative period, the percentage is 66% (4 out of 6 patients).
Out of 21 patients with II DSC two of them have borderline postoperative AHI thus 9.5%.
Among 50 patients with III DSC four of them have borderline postoperative AHI thus 8%.
Among the patients with III DSC and borderline post-operative AHI 2 out of 4 also had maxillary hypoplasia thus 50% while compared to the total malformed patients examined with borderline post-operative AHI it was found that 2 out of 6 patients also had maxillary hypoplasia thus 33%.
Considering the postoperative AHI also showed that 1 of 71 patients examined had worsened: his original AHI was 4.8 and after orthognathic surgery it increased to 6.3 so it increased by about 3%.
This patient belongs to the CDS III group and has maxillary hypoplasia.
Calculating the correlation between AHI >5 and dento-skeletal malformation, considering DSC II and III, a significant correlation coefficient of -0.58 results. This means that there is an inverse correlation where an AHI>5 is correlated more with a DSC II than with a DSC III.
In contrast, the correlation calculated between AHI<5 but >4 and dento-skeletal malformation classes was -0.06 so it was not significant. In terms of the covariance matrix, the only significant value emerges in the correlation between BMI and AHI>5 in patients with DSC II. No kind of significant correlation value was found in patients with DSC III.
Finally, estimating the regression model relating the variable AHI with the covariates: Sex, age, BMI and DSC showed that there is the presence of a linear relation between BMI and AHI but also between AHI and DSC class, confirming the previous analyses.
As BMI increases by one point, AHI will increase by 0.18 while if the patient belongs to the third class, AHI will decrease by 3.38. The effects of the other covariants are inconsistent.
Therefore, we can conclude that it is more likely that a patient with AHI>5 belongs to CDS II than to CDS III.
In support of this argument, we consider the R-square, a statistical index for assessing the accuracy of the model, which in this case is about 54%
4. Discussion
Several reports show that OSAS affects 5-20% of the adult population, some reports indicate an incidence of up to 26%. OSAS seems to be three times more common in men than in women [
7,
8].
As reported in the literature 50% of OSAS patients are underdiagnosed and that represents a major public health problem [
7].
From the data that emerged as a result of our statistical analyses, there is a significant percentage (33%) of patients who undergo orthognathic surgery with an AHI>5 and also a percentage of patients (11%) who are “borderline.” These rates are higher than the universally accepted proportion of the general population with moderate and severe apnea and the limits of the prevalence of OSAS in individuals over 18 years of age and AHI>5 according to the Benjafield study, which is 20.5% [
9].
In our study, we considered two classes of dento-skeletal malformations: Class II and Class III according to Angle’s classification; in class III, we also considered the presence of maxillary hypoplasia, which is particularly at risk of presenting OSAS.
The results shows a significantly higher percentage (75%) of II CDS patients with AHI>5 than III CDS patients with AHI>5 but when considering also maxillary hypoplasia,it turns out to be a risk factor in III CDS patients in the development of Obstructive Sleep Apnea, in fact although the percentage of the latter with AHI>5 is only 16% in our study, 62% turn out to have maxillary hypoplasia.
Instead, considering the borderline AHI values (>4 but <5), the percentage 14% of patients with II DSC is also higher here compared to 10% of patients with III CDS.
Of the patients with III CDS only one out of 5 also has maxillary hypoplasia so the data in this case are less significant.
Our results confirm that the pattern most at risk is the one characterized by retruded maxilla and patients with dento-skeletal class II.
This finding was previously documented in literature, in 2007 George affirmed the patients with diagnosis of OSAS usually display a class II malocclusion and a retrusive profile [
10].
As already widely reported in the literature, another significant data that emerged from the statistical analysis carried out is the correlation between BMI and the AHI index which demonstrates how patients with a higher BMI are more at risk of developing apneas and hypopneas during sleep [
11].
The statistical analysis we performed shows that after surgery for correction of a dentoskeletal malformation only 8% of malformed patients present an AHI > 5, compared to 20.5% described in the Italian population [
9].
We also described a patient with worsening of the AHI value; the patient underwent the correction of a DSC III and maxillary hypoplasia.
This data is in agreement with other literature reports which indicate this pattern as the most subject to OSAS [
12].
It is therefore possible to hypothesize that there is an increased risk of worsening for patients in this category.
This could be especially true in case of surgical planning that involves only modest maxillary advancement with substantial mandibular retraction. These surgical procedures actually reduced the airway volume, which can be already inadequate in these patients.
From our study it emerges that in some types of malformations, the risk of treating not only a dysmorphic patient but also a patient with OSA is high, in these patients pre surgical planning should comprehend polysomnography evaluation.
In particular, the surgeon must consider the augmented risk of silent OSAS especially in patients with dento-skeletal class II and dento-skeletal class III with maxillary hypoplasia.
In patients with hypo-development of the mandible (II CDS) generally a reduction in sagittal diameter at the oro-pharyngeal and hypo-pharyngeal levels is the reason for stenosis. In these cases usually mandibular advancement improves these air spaces.
In patients with DSC III and maxillary hypoplasia the upper third of upper airway column is hypo-represented while the middle and lower third upper airway column is normo- or hypo-represented. The aesthetic conformation of the patient might tempt planning to retract the mandible, and this surgical movement would certainly go even further to reduce the volume of the upper airway. In this type of patient, airway study is mandatory before proceeding with any surgical programming.
From our results and the evidence present in the literature it is clear that patients suffering from dentoskeletal class II malocclusions are more often, even unconsciously, affected by OSAS; It is useful to remember how, in patients suffering from mandibular retrusion, mandibular advancement devices can represent a valid tool for verifying possible post-surgical improvements of AHI.
The same cannot be said of patients suffering from maxillary retrusion; this component of malocclusion should always be kept in mind when considering upper airway changes related to scheduled surgical moves [
5].
Scheduled surgery not taking into account airway volumes may result in the occurrence or worsening of obstructive airway disease during sleep, this risk is much lower in patients with III CDS from sagittal overdevelopment of the mandible, and in fact we did not observe the increase in AHI value after surgery in any patient.
Although this study has some limitations, such as the absence of CT control for airway study, a non-homogeneous sample, and non-consideration of the extent of surgical movements, it highlights how the frequency of silent osas in the patients we treat for surgical correction of dentoskeletal malformations is high.
It also shows how there is generally an improvement in AHI values although in rare cases there could be a worsening which could for example lead to a clinical picture of OSAS.
It therefore appears clear that the polysomnographic study is essential in the pre-operative study of the patient.
5. Conclusions
From the evidence that emerged in this study, some conclusions can be highlighted.
In malformed patients who receive orthognathic surgery for correction of facial dysmorphosis, the presence of Obstructive Sleep Apnea is significantly higher than in the general population.
Obstructive Sleep Apneas are mainly present in patients with sagittal hypodevelopment of the mandible (II CDS) and in patients with sagittal hypodevelopment of the upper jaw (III CDS with maxillary hypoplasia) where the presence of silent OSA should always be suspected.
The necessity of polysomnographic examination in patients who are about to undergo a process of resolution of facial dysmorphia should be essential as the risk of silent OSA is real and much higher than in the general population.
It is evident from our study that there is a possibility of worsening respiratory function after orthognathic surgery performed without regard to the patient’s AHI value;
When surgically correcting a dentoskeletal malformation, the surgeon must aim not only to a satisfying aesthetics, but also to a proper stomatognathic and respiratory function, this cannot be done without taking polysomnography information into account [
14].
Author Contributions
Conceptualization, G.G., B.C. and G.DA.; methodology, M.T. P.DA.; software, G.S.; validation, G.G., G.S. M.T. and A.M.; formal analysis, F.A. P.DA.; investigation, F.A., B.C.; resources, G.G.; data curation, G.G, P.DA; writing—original draft preparation, M.T., G.DA.; writing—review and editing, G.G., G.DA.; visualization, G.G, P.DA.; supervision, G.G. A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available from the corresponding authors upon reasonable request.
Acknowledgments
Not applicable
Conflicts of Interest
The authors declare no conflicts of interest
References
- Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK, Lavie L, Pépin JL. Obstructive sleep apnoea syndrome. Nat Rev Dis Primers. 2015 Jun 25;1:15015. PMID: 27188535. [CrossRef]
- Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an american academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. [CrossRef]
- Giralt-Hernando M, Valls-Ontañón A, Guijarro-Martínez R, Masià-Gridilla J, Hernández-Alfaro F. Impact of surgical maxillomandibular advancement upon pharyngeal airway volume and the apnoea-hypopnoea index in the treatment of obstructive sleep apnoea: systematic review and meta-analysis. BMJ Open Respir Res. 2019 Oct 9;6(1):e000402. PMID: 31673361; PMCID: PMC6797338. [CrossRef]
- Ristow O, Rückschloß T, Berger M, Grötz T, Kargus S, Krisam J, Seeberger R, Engel M, Hoffmann J, Freudlsperger C. Short- and long-term changes of the pharyngeal airway after surgical mandibular advancement in Class II patients-a three-dimensional retrospective study. J Craniomaxillofac Surg. 2018 Jan;46(1):56-62.
- Dicus Brookes CC, Boyd SB. Controversies in Obstructive Sleep Apnea Surgery. Oral Maxillofac Surg Clin North Am. 2017;29(4):503–13.
- Jeffrey C. Posnick, Anayo Adachie, Neeru Singh, Elbert Choi,“Silent” Sleep Apnea in Dentofacial Deformities and Prevalence of Daytime Sleepiness After Orthognathic and Intranasal Surgery,Journal of Oral and Maxillofacial Surgery,Volume 76, Issue 4,2018,Pages 833-843,ISSN 0278-2391. [CrossRef]
- Steiner CC. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod 1960;46(;721-54.
- Durán J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnoea-hypopnoea and rela ted clinical features in a population-based sample of subjects aged 30 to 70 years. Am J Respir Crit Care Med. 2001;163(3):685–9.
- Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R. Clinical Practice Guide line for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. 2017;13(3):479–504.
- Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687-698.
- George LT, Barber HD, Smith BM. Maxillomandibular advancement surgery: an alternative treatment option for obstructive sleep apnoea. Atlas Oral Maxillofac Surg Clin North Am 2007;15:163-77. 5 Goodday R. Treatment of obstructive sleep apnoea by immediate surgical lengthening of the maxilla and mandible. In: Bell WH, Guerrero CA, editors. Distraction Osteogenesis of the Facial Skeleton. Hamilton, ON, Canada: Decker; 2007. p. 438.
- Wittels EH, Thompson S. Obstructive sleep apnea and obesity. Otolaryngologic Clinics of North America. 1990 Aug;23(4):751-760. PMID: 2199906.
- Quo S, Lo LF, Guilleminault C. Maxillary protraction to treat pediatric obstructive sleep apnea and maxillary retrusion: a preliminary report. Sleep Med. 2019 Aug;60:60-68. Epub 2018 Dec 26. PMID: 30642692 . [CrossRef]
- Capasso B, Saponaro G, Gasparini G. Title of Thesis: “Obstructive Sleep Apnea in maxilla-mandibular patients undergoing to orthognatic surgery”. Medicine and Surgery degree. Catholic University Medical School. Rome. Italy. 25 october 2023.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).