Submitted:
20 May 2024
Posted:
22 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
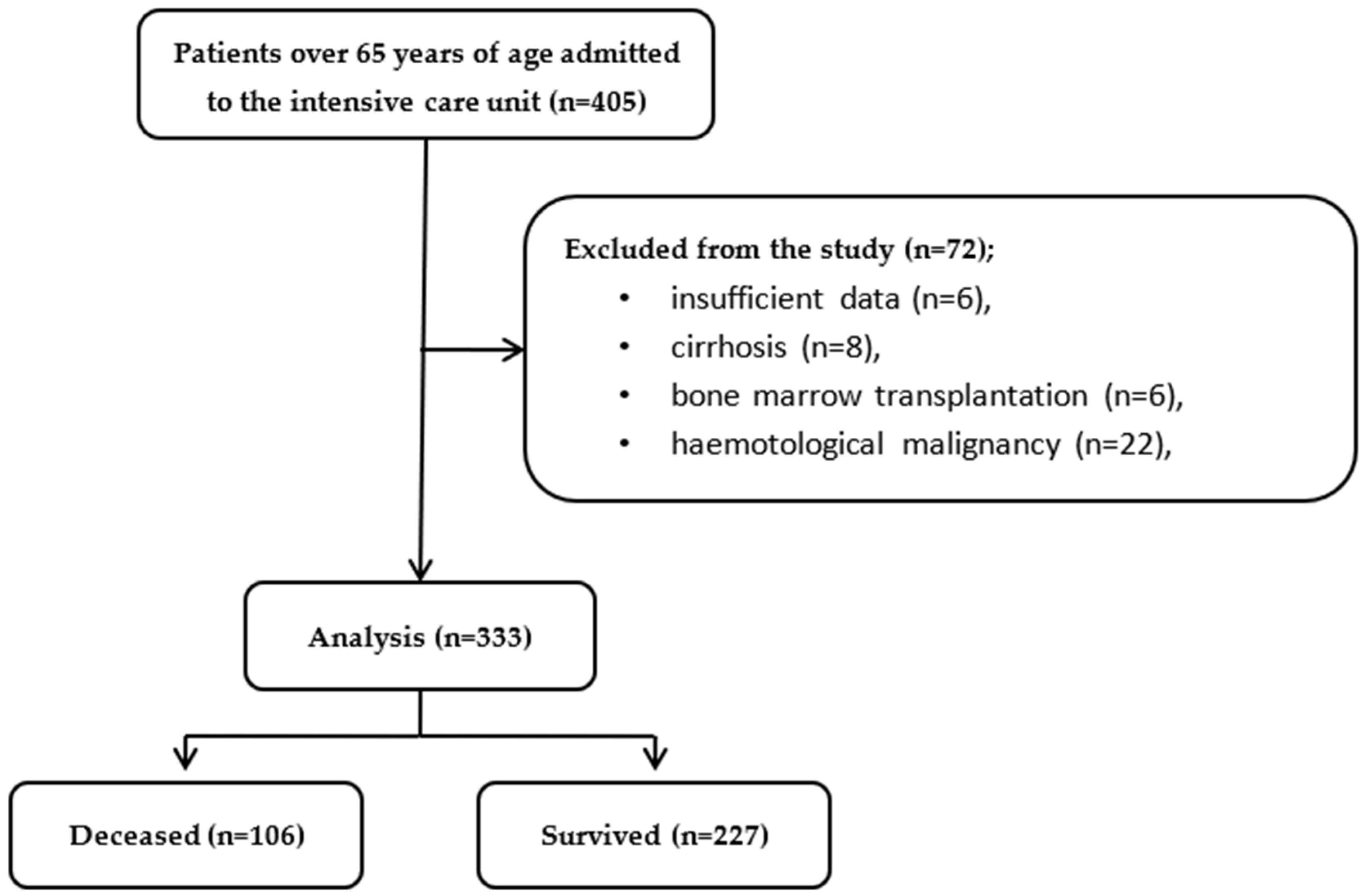
2. Materials and Methods
2.1. Study Location, Duration, and Ethical Approval
2.2. Study Method
2.3. Study Population
2.4. Data Collection Methods
2.5. Blood Measurements and Reference Values
2.6. Data Recording
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sherrington, C.; Fairhall, N.; Kwok, W.; Wallbank, G.; Tiedemann, A.; Michaleff, Z. A.; Ng, C. A. C. M.; Bauman, A. Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2020, 17, 144. [Google Scholar] [CrossRef]
- Flaatten, H.; Beil, M.; Guidet, B. Elderly Patients in the Intensive Care Unit. Semin Respir Crit Care Med. 2021, 42, 10–19. [Google Scholar] [CrossRef]
- Di Rosa, M.; Sabbatinelli, J.; Soraci, L.; Corsonello, A.; Bonfigli, A. R.; Cherubini, A.; Sarzani, R.; Antonicelli, R.; Pelliccioni, G.; Galeazzi, R.; et al. Neutrophil-to-lymphocyte ratio (NLR) predicts mortality in hospitalized geriatric patients independent of the admission diagnosis: a multicenter prospective cohort study. J Transl Med. 2023, 21(1), 835.
- Beniwal, A.; Juneja, D.; Singh, O.; Goel, A.; Singh, A.; Beniwal, H. K. Scoring systems in critically ill: Which one to use in cancer patients? World J Crit Care Med., 2022,11(6), 364–374.
- Celiksoz, A.; Kavak, M.; Tarlacık, A. O. Inflammatory Index as a Predictor of Mortality in Elderly Patients with Intracapsular Femoral Neck Fracture. 2023, Cureus, 15(10), e46318.
- Guven, D. C.; Sahin, T. K.; Erul, E.; Kilickap, S.; Gambichler, T.; Aksoy, S. The Association between the Pan-Immune-Inflammation Value and Cancer Prognosis: A Systematic Review and Meta-Analysis. Cancers (Basel). 2022, 14(11), 2675.
- Yoldas, H.; Karagoz, I.; Ogun, M. N.; Velioglu, Y.; Yildiz, I.; Bilgi, M.; Demirhan, A. Novel Mortality Markers for Critically Ill Patients. J Intensive Care Med. 2020, 35(4), 383–385.
- Turan Y. B. The prognostic importance of the pan-immune-inflammation value in patients with septic shock. BMC Infect Dis. 2024, 24(1), 69.
- Ayrancı, M. K.; Küçükceran, K.; Dundar, Z. D. NLR and CRP to albumin ratio as a predictor of in-hospital mortality in the geriatric ED patients. Am J Emerg Med. 2021, 44, 50–55.
- Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001, 102(1), 5–14.
- Le Tulzo, Y.; Pangault, C.; Gacouin, A.; Guilloux, V.; Tribut, O.; Amiot, L.; Tattevin, P.; Thomas, R.; Fauchet R.; Drénou, B. Early circulating lymphocyte apoptosis in human septic shock is associated with poor outcome. Shock. 2002,18(6), 487–494.
- Miniksar, Ö. H.; Kaçmaz, O. The effect of neutrophil-lymphocyte ratio on admission to postoperative intensive care and mortality in elderly patients undergoing hip fracture surgery with spinal anesthesia. The European Research Journal. 2021, 7, 628–634. [Google Scholar] [CrossRef]
- Zhang, P.; Li, Y.; Zhang, H.; Wang, X.; Dong, L.; Yan, Z.; She, L.; Wang, X.; Wei, M.; Tang, C. Prognostic value of the systemic inflammation response index in patients with aneurismal subarachnoid hemorrhage and a Nomogram model construction. Br J Neurosurg. 2023, 37(6), 1560–1566.
- Hu, B.; Yang, X. R.; Xu, Y.; Sun, Y. F.; Sun, C.; Guo, W.; Zhang, X.; Wang, W. M.; Qiu, S. J.; Zhou, J.; et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014, 20(23), 6212–6222.
- Jomrich, G.; Paireder, M.; Kristo, I.; Baierl, A.; Ilhan-Mutlu, A.; Preusser, M.; Asari, R.; Schoppmann, S. F. High Systemic Immune-Inflammation Index is an Adverse Prognostic Factor for Patients with Gastroesophageal Adenocarcinoma. Ann Surg. 2021, 273(3), 532–541.
- Wang, K.; Diao, F.; Ye, Z.; Zhang, X.; Zhai, E.; Ren, H.; Li, T.; Wu, H.; He, Y.; Cai, S.; et al. Prognostic value of systemic immune-inflammation index in patients with gastric cancer. Chin J Cancer. 2017, 36(1), 75.
- Xie, Q. K.; Chen, P.; Hu, W. M.; Sun, P.; He, W. Z.; Jiang, C.; Kong, P. F.; Liu, S. S.; Chen, H. T.; Yang, Y. Z., et al. The systemic immune-inflammation index is an independent predictor of survival for metastatic colorectal cancer and its association with the lymphocytic response to the tumor. J Transl Med. 2018, 16(1), 273.
- Wang, R. H.; Wen, W. X.; Jiang, Z. P.; Du, Z. P.; Ma, Z. H.; Lu, A. L.; Li, H. P.; Yuan, F.; Wu, S. B.; Guo, J. W.; et al. The clinical value of neutrophil-to-lymphocyte ratio (NLR), systemic immune-inflammation index (SII), platelet-to-lymphocyte ratio (PLR) and systemic inflammation response index (SIRI) for predicting the occurrence and severity of pneumonia in patients with intracerebral hemorrhage. Front Immunol. 2023, 14, 1115031.
- Thijs, L. G.; Hack, C. E. Time course of cytokine levels in sepsis. Intensive Care Med. 1995, 21 Suppl 2, S258–S263. [Google Scholar] [CrossRef]
- Ho, K. M.; Lee, K. Y.; Dobb, G. J.; Webb, S. A. C-reactive protein concentration as a predictor of in-hospital mortality after ICU discharge: a prospective cohort study. Intensive Care Med. 2008, 34(3), 481–487.
- Artero, A.; Zaragoza, R.; Camarena, J. J.; Sancho, S.; González, R.; Nogueira, J. M. Prognostic factors of mortality in patients with community-acquired bloodstream infection with severe sepsis and septic shock. J Crit Care. 2010, 25(2), 276–281.
- Ranzani, O. T.; Zampieri, F. G.; Forte, D. N.; Azevedo, L. C.; Park, M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013, 8(3), e59321.
- Park, J. E.; Chung, K. S.; Song, J. H.; Kim, S. Y.; Kim, E. Y.; Jung, J. Y.; Kang, Y. A.; Park, M. S.; Kim, Y. S.; Chang, J.; et al. The C-Reactive Protein/Albumin Ratio as a Predictor of Mortality in Critically Ill Patients. J Clin Med. 2018, 7(10), 333.
- Oh, J.; Kim, S. H.; Park, K. N.; Oh, S. H.; Kim, Y. M.; Kim, H. J.; Youn, C. S. High-sensitivity C-reactive protein/albumin ratio as a predictor of in-hospital mortality in older adults admitted to the emergency department. Clin Exp Emerg Med. 2017, 4(1), 19–24.
- Casadei Gardini, A.; Scarpi, E.; Valgiusti, M.; Monti, M.; Ruscelli, S.; Matteucci, L.; Bartolini, G.; Vertogen, B.; Pagan, F.; Rovesti, G.; et al. Prognostic role of a new index (multi inflammatory index) in patients with metastatic colorectal cancer: results from the randomized ITACa trial. Ther Adv Med Oncol. 2020, 12, 1758835920958363.
- Dikici S. Novel Indices for Lumbar Discectomy: Systemic Immune Inflammation Index, Systemic Inflammatory Response Index, Multi Inflammatory Index, and Prognostic Nutrition Index. Turk Neurosurg. 2024, 34(2), 243–249.
- Gozdas, H. T.; Kayis, S. A.; Damarsoy, T.; Ozsari, E.; Turkoglu, M.; Yildiz, I.; Demirhan, A. Multi-inflammatory Index as a Novel Mortality Predictor in Critically Ill COVID-19 Patients. J Intensive Care Med. 2022, 37(11), 1480–1485.
- Demirel, M. E.; Akunal Türel, C. The Role of the Multi-Inflammatory Index as a Novel Predictor of Hospital Mortality in Acute Ischemic Stroke. Cureus. 2023, 15(8), e43258.
- Mangalesh, S.; Dudani, S.; Malik, A. The systemic immune-inflammation index in predicting sepsis mortality. Postgrad Med. 2023, 135(4), 345–351.
- Shen, Y.; Huang, X.; Zhang, W. Platelet-to-lymphocyte ratio as a prognostic predictor of mortality for sepsis: interaction effect with disease severity-a retrospective study. BMJ Open. 2019, 9(1), e022896.
- Lu, W.; Zhang, K.; Chang, X.; Yu, X.; Bian, J. The Association Between Systemic Immune-Inflammation Index and Postoperative Cognitive Decline in Elderly Patients. Clin Interv Aging. 2022, 17, 699–705.
| 28-day Mortality | |||
| Deceased (n=106) | Survived (n=227) | p-value | |
| Age, years | 77.2±8.5 | 78.1±8.6 | 0.38 |
| Sex, female | 47 (44.3) | 116 (51.1) | 0.25 |
| Chronic Diseases | |||
| Diabetes mellitus | 43 (40.6) | 86 (37.9) | 0.64 |
| Hypertension | 48 (45.3) | 114 (50.2) | 0.40 |
| Hyperlipidemia | 5 (4.7) | 7 (3.1) | 0.46 |
| Coronary artery disease | 12 (11.3) | 31 (13.7) | 0.55 |
| Atrial fibrillation | 15 (14.2) | 24 (10.6) | 0.34 |
| Chronic kidney disease | 13 (12.3) | 22 (9.7) | 0.48 |
| Pulmonary disease | 19 (17.9) | 46 (20.3) | 0.62 |
| Cerebrovascular disease | 10 (9.4) | 37 (16.3) | 0.94 |
| Multimorbidity | 72 (67.9) | 131 (57.7) | 0.075 |
| Indication of ICU | |||
| Sepsis | 32 (30.2) | 50 (22.0) | 0.11 |
| Acute respiratory failure | 42 (39.6) | 91 (40.1) | 0.94 |
| Acute kidney disease | 12 (11.3) | 16 (7.0) | 0.19 |
| Pancreatitis | 0 | 3 (1.3) | 0.55 |
| Trauma | 1 (0.9) | 7 (3.1) | 0.24 |
| Hepatorenal syndrome | 0 | 1 (0.4) | 0.49 |
| Cardiorenal syndrome | 1 (0.9) | 1 (0.4) | 0.58 |
| Altered conciousness | 24 (22.6) | 40 (17.6) | 0.28 |
| Hemorrhagic shock | 6 (5.7) | 20 (8.8) | 0.32 |
| Postoperative care | 9 (8.5) | 26 (11.5) | 0.41 |
| ICU intensive care unit. | |||
| Deceased (n=106) | Survived (n=227) | p-value | |
| Culture growth | 71 (67.0) | 93 (41.0) | <0.001 |
| Steroid use | 71 (67.0) | 87 (38.3) | <0.001 |
| Platelet tx | 13 (12.3) | 15 (6.6) | 0.083 |
| Erythrocyte tx | 48 (45.3) | 86 (37.9) | 0.20 |
| Sepsis in ICU | 64 (60.4) | 107 (47.1) | 0.024 |
| MV before ICU | 26 (24.5) | 14 (6.2) | <0.001 |
| MV in ICU | 64 (60.4) | 16 (7.0) | <0.001 |
| Day of MV | 3.0 [3.0] | 0.0 [2.0] | <0.001 |
| Day of hospitalization | 13.5 [18.3] | 12.0 [12.0] | 0.68 |
| Day of ICU | 7.0 [10.0] | 6.0 [5.0] | 0.016 |
| Daybefore ICU | 1.5 [11.0] | 0.0 [1.0] | <0.001 |
| Dayafter ICU | 0.0 [0.0] | 4.0 [7.0] | <0.001 |
| SOFA score | 6.0 [4.0] | 3.0 [3.0] | <0.001 |
| APACHE-II score | 24.5 [15.3] | 20.0 [8.0] | <0.001 |
| APACHE Acute Physiologic Asessment and Chronic Health, ICU intensive care unit, MV mechanical ventilation, SOFA Sequantial Organ Failure Assessment, tx transfusion. | |||
| 28-day Mortality | |||
| Deceased (n=106) | Survived (n=227) | p-value | |
| PIV | 1104.3 [2003.4] | 952.0 [1969.8] | 0.47 |
| NLR | 11.6 [20.2] | 9.3 [11.6] | 0.007 |
| MLR | 0.6 [0.6] | 0.5 [0.6] | 0.092 |
| SIRI | 5.8 [11.2] | 4.5 [8.3] | 0.03 |
| PLR | 223.2 [258.8] | 203.5 [240.7] | 0.68 |
| SII | 22.2 [26.6] | 26.7 [29.3] | 0.22 |
| MII1 | 813.8 [2153.1] | 416.3 [1997.1] | <0.001 |
| MII2 | 20182 [46303] | 6993.6 [28048.2] | <0.001 |
| MII3 | 2026.9[4630.6] | 965.5 [3134.3] | 0.006 |
| CRP/Albumin | 4.03 [6.5] | 1.6 [4.7] | <0.001 |
| CRP C-reaktive protein, MII multi-inflamatory index, MLR monocyte-lymphocyte ratio, NLR neutrophil- lymphocyte ratio, PIV pan-immune inflammation, PLR platelet-lymphocyte ratio, SII systemic immune-inflammatory index, SIRI systemic immune response index. | |||
| Hazard Ratio | 95% CI | p-value | |
| NLR | 1.022 | 1.006 to 1.038 | 0.007 |
| MLR | 1.267 | 0.891 to 1.801 | 0.19 |
| SIRI | 1.023 | 1.000 to 1.047 | 0.049 |
| MII1 | 1.0 | 1.0 to 1.0 | 0.32 |
| MII2 | 1.0 | 1.0 to 1.0 | 0.37 |
| MII3 | 1.0 | 1.0 to 1.0 | 0.14 |
| CRP/Albumin | 1.154 | 1.086 to 1.226 | <0.001 |
| CRP C-reaktive protein, MII multi-inflamatory index, MLR monocyte-lymphocyte ratio, NLR neutrophil- lymphocyte ratio, SIRI systemic immune response index. | |||
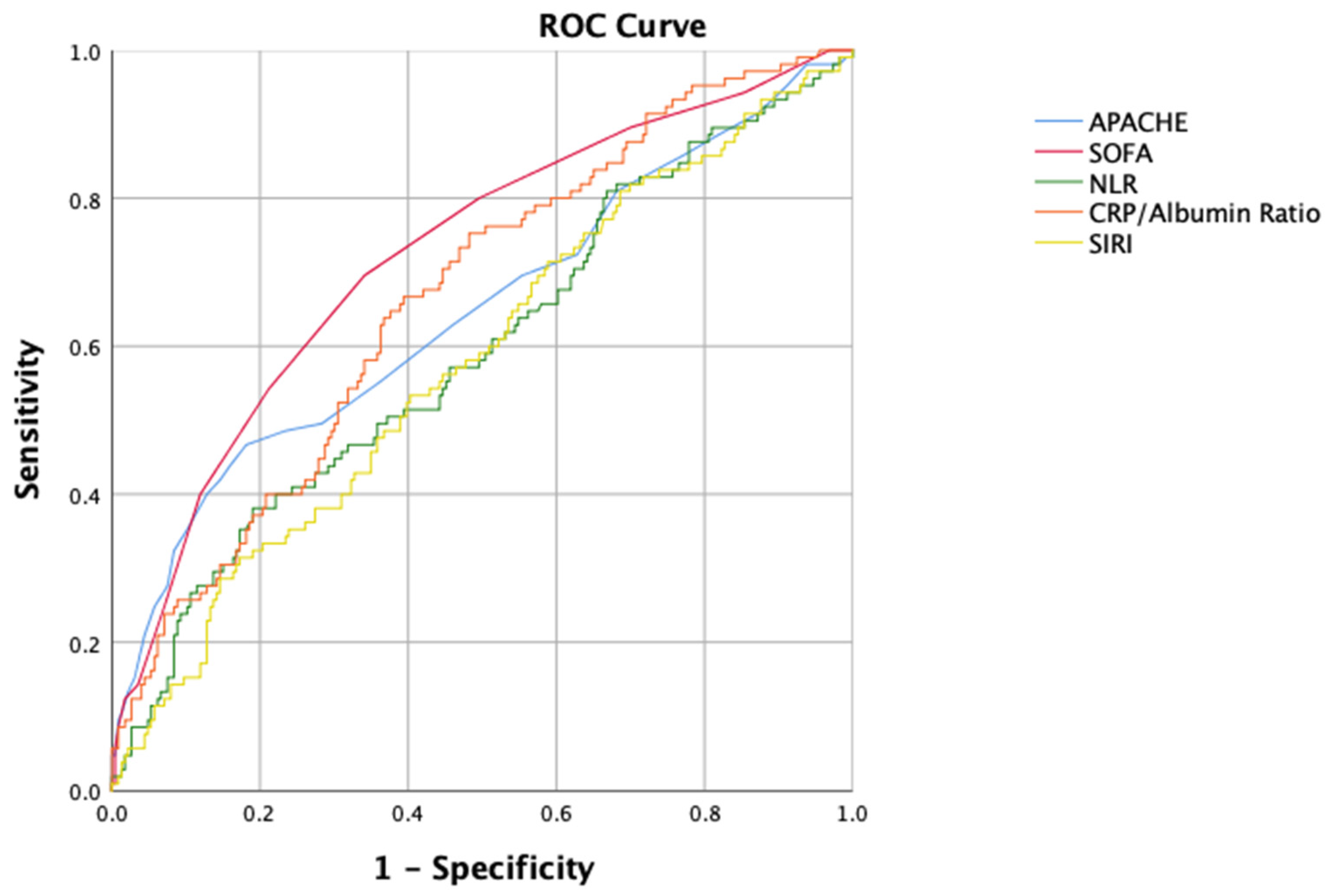
| Cut-off | Sensitivity | Specifity | AUC | 95% CI | p-value | |
| APACHE | 21.5 | 59.0 | 58.8 | 0.647 | 0.579 to 0.714 | <0.001 |
| SOFA | 4.5 | 69.5 | 65.9 | 0.723 | 0.663 to 0.783 | <0.001 |
| NLR | 7.79 | 61.9 | 46.9 | 0.593 | 0.526 to 0.660 | 0.006 |
| SIRI | 5.00 | 56.2 | 54.9 | 0.580 | 0.514 to 0.646 | 0.019 |
| CRP/Albumin | 2.15 | 70.5 | 55.3 | 0.665 | 0.604 to 0.726 | <0.001 |
|
APACHE Acute Physiologic Asessment and Chronic Health, CRP C-reaktive protein, NLR neutrophil- lymphocyte ratio, SIRI systemic immune response index, SOFA Sequantial Organ Failure Assessment. | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





