1. Introduction
Hydrotherapy as a method for managing pain during childbirth has been used for thousands of years, and its exact origin is unknown [
1]. Currently, many women seek non-pharmacological methods for pain relief during labor. The use of hydrotherapy can provide natural pain relief because warm water helps relax muscles and can reduce the sensation of pain, allowing women to better manage contractions [
1,
2].
The use of warm water can help reduce anxiety and stress, promoting a state of calm that facilitates the birthing process. The option to choose hydrotherapy for pain management during labor can give women a sense of control and empowerment over their birthing experience [
3]. It allows them to actively participate in their care and make informed decisions about pain management. It is important to consider that each woman has her own preferences and needs during labor, and the decision to use hydrotherapy should be individualized [
4].
In 2022, the Health Technology Assessment Service of the Basque Country (OSTEBA), supported by the Spanish Ministry of Health, published a comprehensive report on water immersion during labor. This study focused on two main aspects: evaluating the efficacy, effectiveness, and safety of water immersion during labor, and understanding the values and preferences of women who had experienced this birthing method. Given existing concerns, particularly regarding the safety of the newborn, the report aimed to analyze the available evidence to determine the safety and efficacy of water immersion during labor for both the mother and the neonate [
5].
According to the literature review, various studies have been conducted to demonstrate the efficacy of therapeutic showers during labor for pain relief, compared to women who do not use water during the birthing process [
6,
7]. However, as of our review, we have not found specific studies that directly compare therapeutic showers and bathtubs in this context. Nevertheless, there are articles that compare therapeutic showers with other non-pharmacological methods, such as the use of perineal exercises with a Swiss ball during the dilation phase. These studies have yielded equally interesting results, demonstrating that the combination of therapeutic showers with these exercises is associated with reduced pain during labor and greater comfort for the mother [
8].
In a pretest-posttest design study with a single group of 24 women who used the therapeutic shower for 30 minutes, numerical pain rating scales were evaluated before and after use. A significant decrease in both pain perception and levels of tension and anxiety was observed after the intervention [
9].
Currently, in Spain, maternity units are incorporating bathtubs in their delivery rooms, but not all hospitals in the country can offer these services due to a lack of necessary infrastructure, specifically bathtubs for water immersion use by pregnant women during labor. Some delivery rooms have therapeutic showers available, but these do not provide full water immersion. The purpose of the present study was to compare whether therapeutic showers can be as effective as bathtubs regarding labor duration, use of analgesia, pain relief, and maternal and fetal outcomes.
Objectives
To evaluate and compare the effects of using a bathtub and a therapeutic shower during labor on pain perception, the use of epidural analgesia, labor duration, and maternal and fetal outcomes.
2. Materials and Methods
2.1. Study Design
This is a retrospective cohort study of women who chose to use hydrotherapy during their labor. The report of this research follows the STROBE guidelines for observational studies. The study was conducted in accordance with the Declaration of Helsinki for research involving humans and was approved by the Ethics Committee of Hospital Costa del Sol (002_oct18_PI-hydrotherapy in labor) in November 2018.
2.2. Setting
These are secondary outcomes from a study that evaluated the use of hydrotherapy during labor. The initial study included women who gave birth at Hospital Costa del Sol, Málaga (Spain), during the period between January 2010, when hydrotherapy began to be offered during labor at the hospital, and December 2020. In this hospital, the use of hydrotherapy is indicated in the first stage of labor, either through a therapeutic shower or by immersion in a bathtub. Data were collected from each woman’s partogram as well as from the medical records of both the mother and the newborn.
2.3. Participants
Our study included women with low-risk pregnancies and labors, which means they had a healthy singleton pregnancy, a body mass index of 30 kg/m² or less, cephalic presentation, spontaneous onset of labor, a gestational age between 37+0 and 41+6 weeks, and a normal cardiotocographic record upon admission. Women with multiple pregnancies and those who gave birth before 37 weeks or after 42 weeks were excluded. According to the protocol of our Labor Unit, all admitted women were offered the option to use hydrotherapy during the labor process.
2.4. Variables and Data Sources
The study meticulously planned data coding in advance, extracting data directly from medical records into a structured database. It analyzes a variety of variables related to labor and hydrotherapy. Regarding pain relief during labor, pain perception was assessed using the visual analogue scale (VAS) in both the therapeutic shower group and the bathtub group, as well as comparing the median pain scores before and after the use of each method. Regarding labor duration, dilation times and overall labor time were examined in both groups. The use of epidural analgesia during labor was also recorded. In terms of delivery types, the proportion of spontaneous and operative deliveries in each group was observed. Additionally, various maternal outcomes were explored, including the incidence of postpartum hemorrhage, perineal status, presence of hypotension, maternal fever, and breastfeeding. As for neonatal outcomes, APGAR scores, fetal heart rate, fetal complications, and neonatal unit admission were analyzed.
2.5. Bias
To mitigate potential biases, the study established precise inclusion and exclusion criteria for participants, ensured data anonymity, and conducted meticulous data coding. Additionally, confounding variables were controlled through multivariable statistical analysis. These measures ensured the validity and reliability of the findings obtained in this retrospective cohort study.
2.6. Study Size
The sample size calculation for the primary study was conducted using the systematic review by Cluett et al. [
1] as a reference. For the main objective of the study, the calculated sample size is 248 pregnant women, including a control group of 124 women and 124 women in the hydrotherapy group.
2.7. Statistical Methods
Descriptive analysis was performed using measures of central tendency, dispersion, and position (median and interquartile range (P75–P25)) for quantitative variables and frequency distribution for qualitative variables. To assess differences between study groups (bath vs. shower), the chi-squared test (or Fisher’s exact test if expected frequencies were less than 5) was used for qualitative variables, while Student’s t-test (or Mann–Whitney U test if the distribution was non-normal) was used for quantitative variables. Using pain as the outcome variable, a multivariate linear regression model was employed, including unbalanced independent variables from previous bivariate analysis, selecting variables with a criterion of p < 0.05, and describing the Beta coefficient (β) with respective 95% confidence intervals (CI95%). This involved checking for normality, homoscedasticity, and multicollinearity.
For all analyses, the level of statistical significance was set at p < 0.05. The analysis was performed using SPSS vs. 28.0 program for Windows (IBM Corporation, Armonk, NY, USA) statistical software.
2.8. Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki for research involving human subjects. The Ethics Committee of the Costa del Sol Hospital approved the study in November 2018 under reference number 002_oct18_PI-hydrotherapy birth, ensuring the ethical compliance of the research.
No personal or identifying information was collected. Anonymity was guaranteed by the research service of Hospital Costa del Sol, which anonymized the personal or identifying data of the women involved in the study. Additionally, the data were stored on a password-protected personal computer.
3. Results
The results examined the effect of hydrotherapy, both in the form of a bathtub and a therapeutic shower, in relation to pain relief during labor, its duration, the use of pharmacological analgesia, and delivery types. Additionally, maternal and fetal outcomes were analyzed based on whether water immersion in a bathtub or use of water in a therapeutic shower was performed.
For this study, a convenience sample of 124 laboring women was recruited. This included 44 women (35.5%) who used the therapeutic shower and 80 women (64.5%) who used the bathtub, in which water immersion was present. To determine if there were significant differences between the groups, the obstetric characteristics of the sample were evaluated, which are presented in
Table 1:
These results demonstrate the distribution of key obstetric characteristics between women who used a therapeutic shower and those who used a bathtub during labor. No statistically significant differences were found between the groups in terms of age, grouped gestation, history of abortions, or the number of previous children.
3.1. Pain Relief
The initial findings of this study revealed statistically significant differences between the use of hydrotherapy during labor compared to non-use, regardless of whether therapeutic shower or bathtub was utilized during labor [
10]. At this juncture, we have scrutinized the sensation of pain in the bathtub versus the therapeutic shower.
Our sample, comprised of 124 pregnant women, furnishes comparative data on perceived pain during the use of therapeutic shower and bathtub. In the therapeutic shower group, 8 cases were lost, while in the bathtub group, 5 cases were lost due to lack of recording.
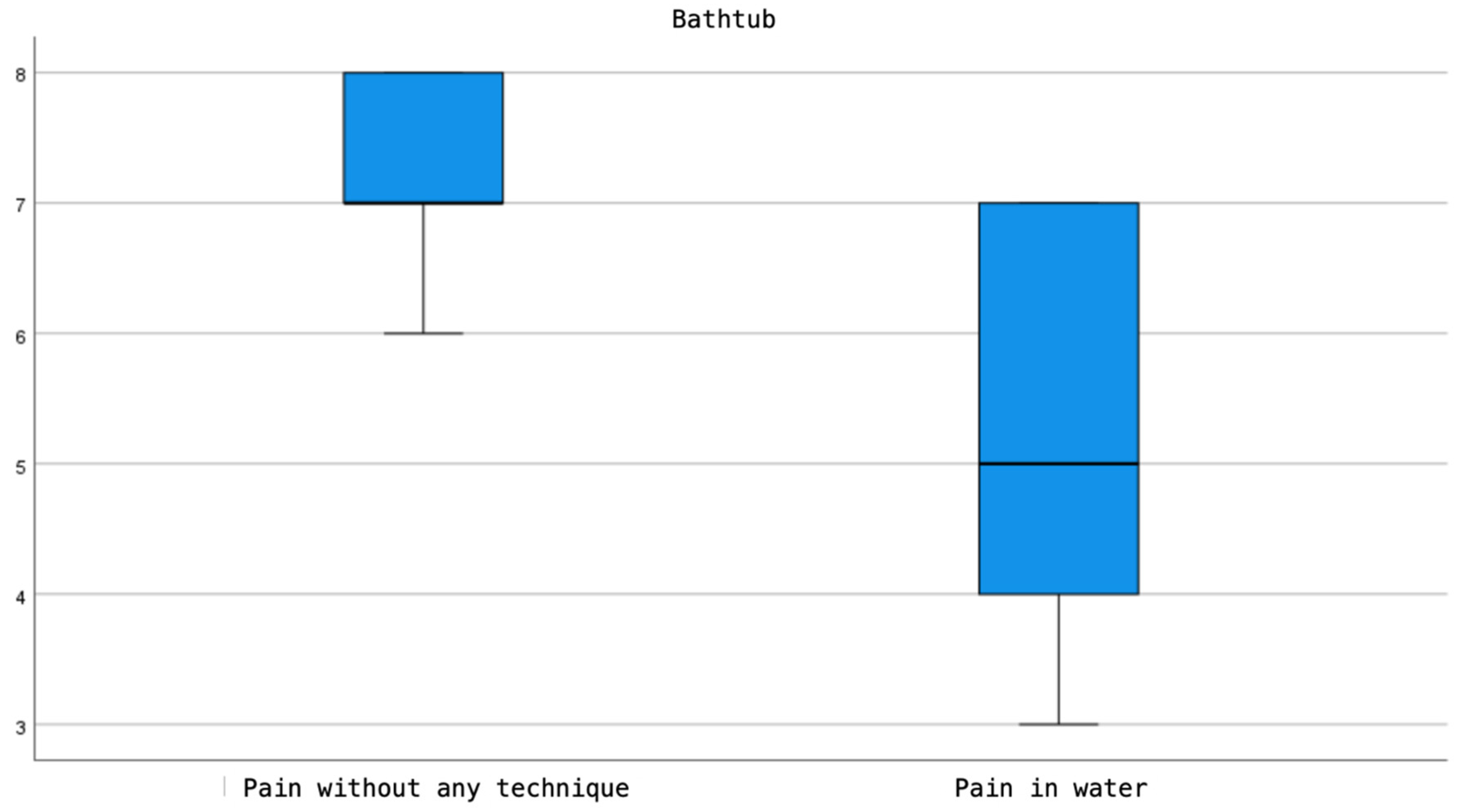
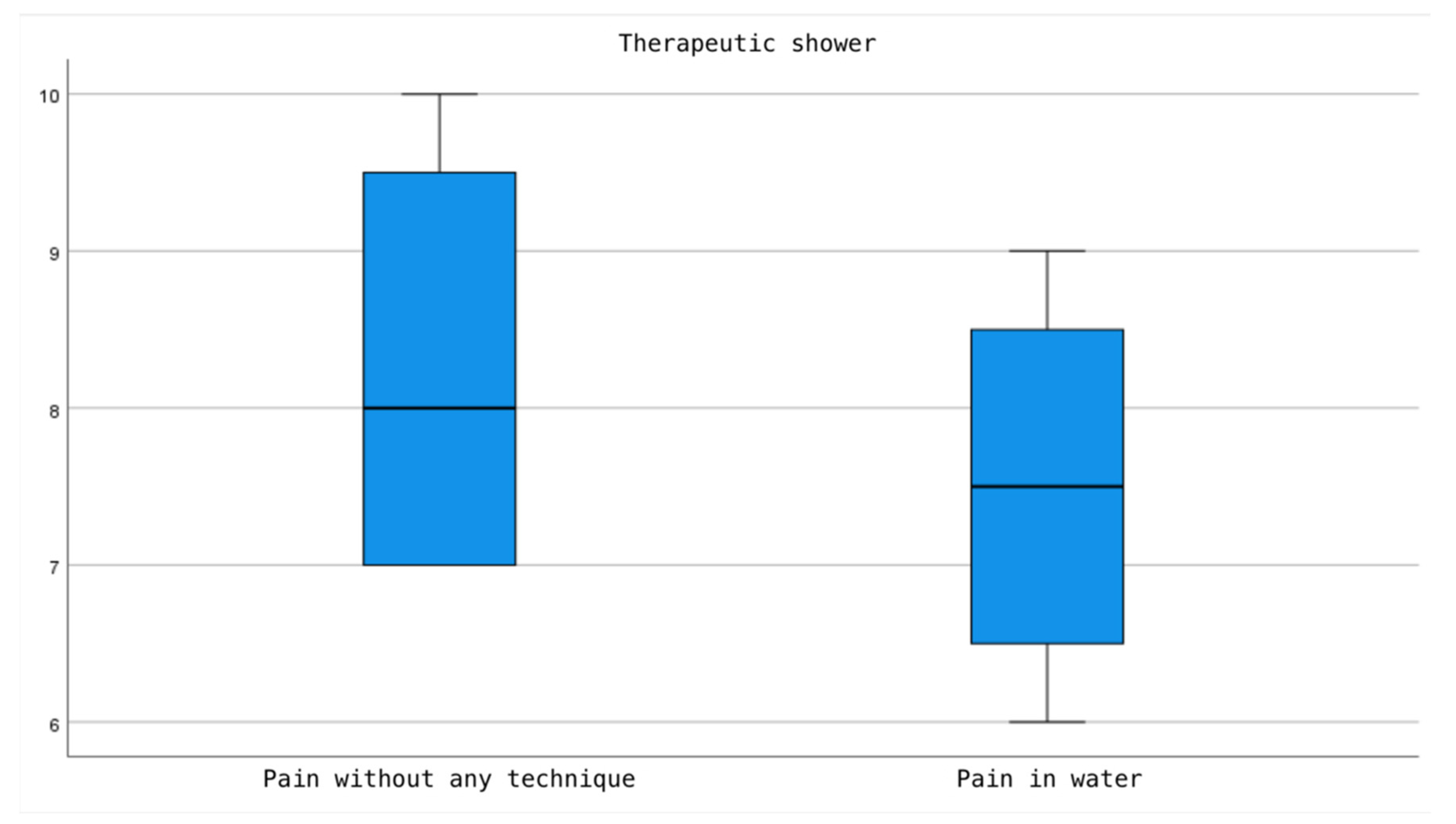
According to the presented results, both the use of therapeutic shower and bathtub exhibit a reduction in pain perception compared to the sensation of pain prior to their use. However, this decrease is more pronounced in the bathtub group, where a median of 7 IQR (7-8) on the VAS scale is recorded before use and a score of 5 IQR (4-7) on VAS after use, with the difference in pain perception scale before and after use being statistically significant (p=0.003). In contrast, in the therapeutic shower group, an average of 8 IQR (7-9) VAS score is observed before use and 7.5 IQR (6.25-8.75) on VAS after use, although a reduction in pain perception is noted, this difference does not reach statistical significance (p=0.083) (
Figure 1 and
Figure 2).
3.2. Duration of Labor
Upon examining the results between the group using the therapeutic shower and the group using the bathtub, it was found that dilation times and overall labor duration showed significant differences between the two groups, favoring the group that used the therapeutic shower (
Table 2).
3.3. Duration of Labor
This indicates that women in the group using the therapeutic shower gave birth in a shorter time compared to those who used the bathtub. Women who used the therapeutic shower had a reduced overall labor time.
3.4. Use of Analgesia
A total of 99 pregnant women did not use epidural analgesia, representing 79.8% of the 124 women in our study. Conversely, 25 pregnant women did use epidural analgesia, which equals 20.2%. The result of p=0.521 indicates no significant association between epidural use and the bathing method, whether therapeutic shower or bathtub. In the therapeutic shower group, 37 women did not use analgesia, while 7 used epidural analgesia, representing 84.1% and 15.9%, respectively. In the bathtub group, 18 women used analgesia and 62 did not, corresponding to 22.5% and 77.5%, respectively, of the 80 women in this group. These data suggest that analgesia was not frequently used by women using the bathtub.
3.5. Types of Delivery
The data comparing the therapeutic shower group and the bathtub group, as well as the types of delivery, are very similar. According to the p-values obtained, none of the statistical tests performed indicate a statistically significant association between the type of delivery and the bathing method. All p-values are well above the 0.05 threshold. Therefore, no significant differences were found between the use of the bathtub and the therapeutic shower concerning the types of delivery. The analysis indicates that in the therapeutic shower group, 2.3% of deliveries were operative vaginal and operative cesarean, while 97.7% were spontaneous vaginal. In the bathtub group, 2.5% of deliveries were operative vaginal and operative cesarean, and 97.5% were spontaneous vaginal.
3.6. Maternal Outcomes
The effect of the therapeutic shower and bathtub on various maternal parameters has been investigated:
3.6.1. Postpartum Hemorrhage
There were 2 cases of postpartum hemorrhage in the therapeutic shower group and 4 cases in the bathtub group, representing 4.5% and 5.0% of the sample, respectively. However, no statistically significant differences were found regarding this variable.
3.6.2. Postpartum Perineal Status
The study results indicate a statistically significant decrease in the frequency of 1st, 2nd, and 3rd-degree tears, as well as episiotomies, in favor of the group that used the therapeutic shower. In the therapeutic shower group, 45.5% of women had an intact perineum after delivery, compared to 23.8% in the bathtub group. The incidence of 1st, 2nd, and 3rd-degree tears and episiotomies was 54.5% and 76.3%, respectively. The p-value of 0.022 suggests that the use of the therapeutic shower was associated with a lower incidence of tears and episiotomies compared to the use of the bathtub.
3.6.3. Maternal Hypotension
It was observed that 9.1% of women in the therapeutic shower group experienced hypotension, compared to 3.8% of women who used the bathtub. However, the p-value of 0.244 does not show statistically significant differences between the groups.
3.6.4. Maternal Fever
In the therapeutic shower group, no cases of fever were recorded, while in the bathtub group, there was one case with a fever above 38°C. No significant differences were found between the groups concerning this variable.
3.6.5. Breastfeeding
No statistically significant differences were recorded (p=1.000); both percentages were high, with 95.5% for women who used the therapeutic shower compared to 96.3% for those who used the bathtub.
3.7. Neonatal Outcomes
Regarding fetal parameters, the analysis between the groups revealed no significant differences in APGAR scores at 1 and 5 minutes, except for one case in the bathtub group with an APGAR score at 1 minute below 7. Fetal heart rate (FHR) was normal in 94.4% of cases in both groups. Specifically, in the therapeutic shower group, 6.8% had a non-reassuring fetal cardiotocographic record (FCTG), while in the bathtub group, this percentage was 5%. No significant differences were found in the APGAR and FCTG variables.
Regarding fetal complications and neonatal unit admissions (NICU), 119 newborns did not have complications, and 118 did not require NICU admission, representing 96% and 95.2% of the sample, respectively. Fetal complications occurred in 5% of the newborns in the bathtub group and 2.3% of the newborns in the therapeutic shower group. NICU admission occurred in 5% of the newborns in the bathtub group and 4.5% of the newborns in the therapeutic shower group. No significant differences were found for these two variables, thus no relationship could be established between the method of water use during labor and the presence of fetal complications or NICU admissions.
4. Discussion
We focused on investigating the effect of hydrotherapy during labor, according to the use of a bathtub or therapeutic shower, in relation to perceived pain, labor duration, analgesia use, and maternal and neonatal outcomes. The objective is to contribute to the scientific evidence by comparing these two groups, which is uncommon due to the scarcity of literature addressing this comparison.
Pain management is a fundamental aspect of labor care, which is why it has been the subject of numerous scientific investigations studying its relationship with non-pharmacological methods such as hydrotherapy. Publications analyzing both the therapeutic shower and the bathtub, encompassed in hydrotherapy in general, emphasize how the sensation of pain can decrease through the use of hydrotherapy. Our study also corroborates these findings: the comparison between the groups shows that the bathtub reduces the sensation of pain by one point more on the visual analog scale (VAS) compared to the therapeutic shower. Other studies, such as the one conducted by Davim et al. [
11], have observed that pain relief increases as dilation progresses during labor when using the therapeutic shower. In a clinical trial conducted by Lee et al. [
6], it was demonstrated that the therapeutic shower is a cost-effective, comfortable, and easy-to-perform non-pharmacological method for reducing pain, with positive results on a visual analog pain scale. A systematic review by Vargens, Silva, and Progianti [
3] compiled 21 articles on the use of hydrotherapy and concluded that both the bathtub and the therapeutic shower effectively reduce pain during labor.
Our study also shows that the therapeutic shower results in a shorter labor duration compared to the use of the bathtub. Numerous studies discuss the use of the bathtub as a pain relief method [
12,
13,
14,
15,
16], while there are also studies addressing the use of the therapeutic shower [
6,
7,
11,
12,
17]. A decrease in dilation time and total labor duration has been observed when using the therapeutic shower as a method. Gallo et al. [
12] detailed in their randomized trial how a warm shower at more than 7 centimeters dilation, combined with exercises on a Swiss ball and lumbosacral massage before 7 centimeters, yielded significant benefits, such as a reduction of 72 minutes compared to the group that did not use non-pharmacological techniques during labor, as well as differences in faster expulsion times.
Regarding specific research on analgesia use, the systematic review by Cluett et al. [
1] revealed discrepancies in the use of epidural analgesia among women who opted for water immersion during the first stage of labor and those who did not. It was observed that in the group of women who experienced water labor, a smaller proportion opted for epidural analgesia compared to the groups that did not use water as a pain relief method. However, no significant differences were found in the use of epidural analgesia or the use of pethidine/narcotics between the different groups. In our study, we found a significant association between the use of epidural and the use of hydrotherapy, either in a bathtub or therapeutic shower, considering that the majority of pregnant women who used the therapeutic shower or bathtub did not use epidural analgesia. Authors like Gallo et al. [
12] and Stark [
7] describe the therapeutic shower as one of the beneficial non-pharmacological interventions, with few side effects or contraindications, allowing for a reduction in pain perception and even reducing the use of epidural analgesia, although Stark’s study [
7] found similar use of epidural analgesia in both the therapeutic shower group and the control group.
The randomized trial by Gallo et al. [
12] not only studied variables such as pain and labor duration in women who used the therapeutic shower but also examined other parameters similar to those measured in our study. However, it is important to note that Gallo et al.‘s study compared the use of the therapeutic shower with exercises on a Swiss ball and lumbosacral massage. Among the results, neonatal effects stood out: the experimental group had a lower risk of respiratory distress and significantly better Apgar scores. Although no significant differences were observed regarding delivery types, perineal status, or obstetric complications. In our study, we also evaluated these parameters and found no significant differences, except in postpartum perineal status, where we observed a decrease in the frequency of tears and episiotomies in the group that used the therapeutic shower.
The main limitation was the lack of exhaustive records in medical histories, leading to a sample of sixteen pregnant women, as previous information was not typically recorded in these histories. Another limitation was the absence of data related to the water temperature of the bathtub or therapeutic shower, information that would have been useful to assess its possible impact on the health of pregnant women and fetal development. Water temperature could influence various physiological factors, such as blood circulation and muscle relaxation, in addition to preventing risks associated with extreme temperatures, such as overheating or thermal shock.
5. Conclusions
The conclusions of this study suggest that both the therapeutic shower and the bathtub are effective in alleviating pain during the first stage of labor. Both methods demonstrated a significant reduction in pain perception, as evidenced by the visual analog scale (VAS). However, the bathtub showed a greater reduction in pain intensity compared to the therapeutic shower. Additionally, the use of the therapeutic shower was associated with a shorter labor duration compared to the bathtub, suggesting that the therapeutic shower may be more effective in this aspect.
Regarding the use of epidural analgesia, it was found that the majority of pregnant women who used the therapeutic shower or the bathtub did not require epidural analgesia, suggesting that hydrotherapy can be an effective alternative for pain relief without the need for medication.
No significant differences were found between the use of the therapeutic shower and the bathtub in terms of types of delivery, such as spontaneous or operative delivery. This suggests that both methods of hydrotherapy do not influence the choice of delivery type.
In terms of maternal outcomes, it was observed that the use of the therapeutic shower was associated with a lower incidence of tears and episiotomies compared to the use of the bathtub, indicating a potential additional benefit of the therapeutic shower for maternal health.
Regarding neonatal outcomes, no significant differences were found between the use of the therapeutic shower and the bathtub in terms of APGAR scores, fetal heart rate, fetal complications, or neonatal unit admissions. This suggests that both methods of hydrotherapy are safe for neonatal well-being.
In summary, this study provides evidence that both the therapeutic shower and the bathtub are effective in pain relief during labor and do not pose significant risks to the mother or baby. However, the therapeutic shower may be preferable in terms of shorter labor duration and lower incidence of tears and episiotomies.
Author Contributions
Conceptualization, R.R.-B., J.C.-M., E.M.-G. and J.C.S.-G.; data curation, J.C.-M., L.D.-R., J.C.S.-G. and J.C.H.M.; formal analysis, F.R.R., J.C.S.-G.; investigation, R.R.-B., L.D.-R., E.M.-G. and J.C.S.-G.; methodology, F.R.R., E.M.-G., R.R.-B. and L.D.-R.; project administration, R.R.-B., B.P.-S., J.C.-M. and J.C.S.-G.; resources, E.M.-G., J.C.S.-G., R.R.-B. and L.D.-R.; supervision, L.D.-R. and R.R.-B.; validation, R.R.-B., J.C.-M., L.D.-R., B.P.-S. and E.M.-G.; visualization, R.R.-B., J.C.-M. and L.D.-R.; writing—original draft preparation, J.C.-M., R.R.-B., E.M.-G. and J.C.S.-G.; writing—review and editing, R.R.-B., J.C.-M., B.P.-S., E.M.-G., L.D.-R. and J.C.S.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Ethics Committee of the Hospital Costa del Sol approved this study in November 2018 under reference number 002_oct18_PI-hydrotherapy birth, thus ensuring the ethical compliance of the research in question.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data regarding this study are available upon request from the corresponding author.
Acknowledgments
This study was carried out within the framework of the research project “Effects of hydrotherapy during labour in terms of maternal and neonatal health”, which is part of the Doctoral Programme in Clinical Medicine and Public Health at the University of Granada. We are grateful to the Official College of Nursing of Granada (CODEGRA) for their help in the research support program, and to the Chair of Research in Nursing Care of the University of Granada and the Official College of Nursing of Granada. We thank the Research and Innovation Unit of the Costa del Sol Universitary Hospital for their help in obtaining the data related to the study. We thank our medical translator Megan Berry for her services and comments that contributed to improving this manuscript for publication.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Cluett, E.R.; Burns, E.; Cuthbert, A. Immersion in Water during Labour and Birth. Cochrane Database of Systematic Reviews 2018, CD000111. [Google Scholar] [CrossRef] [PubMed]
- Benko A Waterbirth: Is It a Real Choise. Midwifery matters 2009, 122, 9–12.
- Vargens, O.M.C.; Silva, A.C.V.; Progianti, J.M. Non-Invasive Nursing Technologies for Pain Relief during Childbirth—The Brazilian Nurse Midwives’ View. Midwifery 2013, 29, e99–e106. [Google Scholar] [CrossRef] [PubMed]
- Fair, C.D.; Crawford, A.; Houpt, B.; Latham, V. “After Having a Waterbirth, I Feel like It’s the Only Way People Should Deliver Babies”: The Decision Making Process of Women Who Plan a Waterbirth. Midwifery 2020, 82, 102622. [Google Scholar] [CrossRef] [PubMed]
- Reviriego Rodrigo E; Ibargoyen-Roteta N; Carreguí Vilar S; Mediavilla Serrano L; Montero Carcaboso S; Ares Mateos G; Castelló Zamora B; Moreno Rodríguez A; Hernández Tejada N; Koetsenruyter C Inmersión En Agua Durante El Parto. Informes de Evaluación de Tecnologías Sanitarias; Vitoria-Gasteiz, 2022.
- Lee, S.; Liu, C.; Lu, Y.; Gau, M. Efficacy of Warm Showers on Labor Pain and Birth Experiences During the First Labor Stage. Journal of Obstetric, Gynecologic & Neonatal Nursing 2013, 42, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Stark, M.A. Testing the Effectiveness of Therapeutic Showering in Labor. Journal of Perinatal & Neonatal Nursing 2017, 31, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, M.; Henrique, A.J.; Chors, F.M.; Maia, N. de L.; Gabrielloni, M.C. Warm Shower Aspersion, Perineal Exercises with Swiss Ball and Pain in Labor. Acta Paul Enferm 2013, 26, 478–484.
- Stark, M.A. Therapeutic Showering in Labor. Clin Nurs Res 2013, 22, 359–374. [Google Scholar] [CrossRef] [PubMed]
- Mellado-García, E.; Díaz-Rodríguez, L.; Cortés-Martín, J.; Sánchez-García, J.C.; Piqueras-Sola, B.; Higuero Macías, J.C.; Rodríguez-Blanque, R. Effects of Hydrotherapy on the Management of Childbirth and Its Outcomes — A Retrospective Cohort Study. Nursing Report 2024, 14, 1251–1259. [Google Scholar] [CrossRef]
- Davim, R.M.B.; Torres, G.D.V.; Dantas, J.D.C.; de Melo, E.S.; Paiva, C.P.; Vieira, D.; Costa, I.K.F. Showering as a Non Pharmacological Strategy to Relief the Parturients Pain. Revista Eletrônica de Enfermagem 2008, 10, 600–609. [Google Scholar] [CrossRef]
- Gallo, R.B.S.; Santana, L.S.; Marcolin, A.C.; Duarte, G.; Quintana, S.M. Sequential Application of Non-Pharmacological Interventions Reduces the Severity of Labour Pain, Delays Use of Pharmacological Analgesia, and Improves Some Obstetric Outcomes: A Randomised Trial. J Physiother 2018, 64, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Ulfsdottir, H.; Saltvedt, S.; Georgsson, S. Women’s Experiences of Waterbirth Compared with Conventional Uncomplicated Births. Midwifery 2019, 79. [Google Scholar] [CrossRef] [PubMed]
- Camargo, J.C.S.; Varela, V.; Ferreira, F.M.; Pougy, L.; Ochiai, A.M.; Santos, M.E.; Grande, M.C.L.R. The Waterbirth Project: São Bernardo Hospital Experience. Women and Birth 2018, 31, e325–e333. [Google Scholar] [CrossRef] [PubMed]
- Zanetti-Daellenbach, R.A.; Tschudin, S.; Zhong, X.Y.; Holzgreve, W.; Lapaire, O.; Hösli, I. Maternal and Neonatal Infections and Obstetrical Outcome in Water Birth. European Journal of Obstetrics & Gynecology and Reproductive Biology 2007, 134, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Nutter, E.; Meyer, S.; Shaw-Battista, J.; Marowitz, A. Waterbirth: An Integrative Analysis of Peer-Reviewed Literature. J Midwifery Womens Health 2014, 59, 286–319. [Google Scholar] [CrossRef] [PubMed]
- Benfield, R.; Heitkemper, M.M.; Newton, E.R. Culture, Bathing and Hydrotherapy in Labor: An Exploratory Descriptive Pilot Study. Midwifery 2018, 64, 110–114. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).