1. Introduction
HPV genital infections are quite frequent in woman’s life: although they are mostly transient, these infections can cause cervical dysplasia or neoplasia particularly when associated to HR-HPV [1].
Cervical carcinoma represents the most frequent neoplasm of the female genital tract and after breast, colon and lung cancer, being the most frequent cause of illness and death from cancer [2,3]. To prevent cervical cancer, the Lazio Region (Italy), in agreement with the National Cancer Screening program, offers HR-HPV test to all women aged 30-64 years old. During the sampling phase, rare cases of genital malformations, such as double cervix, have been detected. This uterine malformation is due to non-fusion of the Müllerian duct system during embryogenesis and can be associated with various genitourinary system malformations [4].
The aim of this work is to evaluate HR-HPV infections in women with double cervix discovered within the HR-HPV based Cervical Cancer Screening program of the Lazio Region (Italy).
2. Methods
From June 2021 to March 2024 a total of 142,437 samples collected from women aged 30-64 years were analyzed. Samples were collected using the cervix-brush and diluted in ThinPrepR PreservCyt Solution (Hologic, Marlborough, MA, USA).
For each woman identified with a double cervix, two separate samples were taken from both cervixes and these samples were analyzed separately.
DNA extraction, PCR amplification and extended genotyping were performed using automated DNA extraction and PCR setup platform STARlet IVD (Seegene, Seoul, Republic of Korea). Anyplex™ II HR-HPV Detection kit (Seegene, Seoul, Republic of Korea) was applied for HPV DNA detection and genotyping using the CFX96™ Real-time PCR System (Bio-Rad, Berkeley, CA, USA), as already reported [5]. Our molecular platform (the Seegene's proprietary DPO™ and TOCETM technologies), allows the detection and genotyping of the following 14 HR-HPV subtypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59. 66 and 68 [5].
In the Lazio Region, the computerized transmission of results was carried out using SIPSO 2.0 software: our Laboratory is the first applying this informatic tool to manage the overall procedures surrounding HPV screening. The flexibility of the SIPSO software allowed us to accept separately the two samples collected from the double cervix (the same individual with two cervix-brush) on the SIPSO 2.0 software so that we could report the HR-HPV results separately, being sometimes different. In fact, the software does not consider the rare events as double cervix.
The HPV positive cases were sent to cytologic laboratory for the Pap test, according to the Lazio Region algorithms.
3. Results and Discussion
3.1. Results
In total, 27 women (32-64 years old, median age of 45.6 years) with double cervix were identified (0.019%): 20 women (83.3%) tested negative for both cervices, while the remaining four (namely A, B, C and D) (16.7%) resulted as positive (
Table 1).
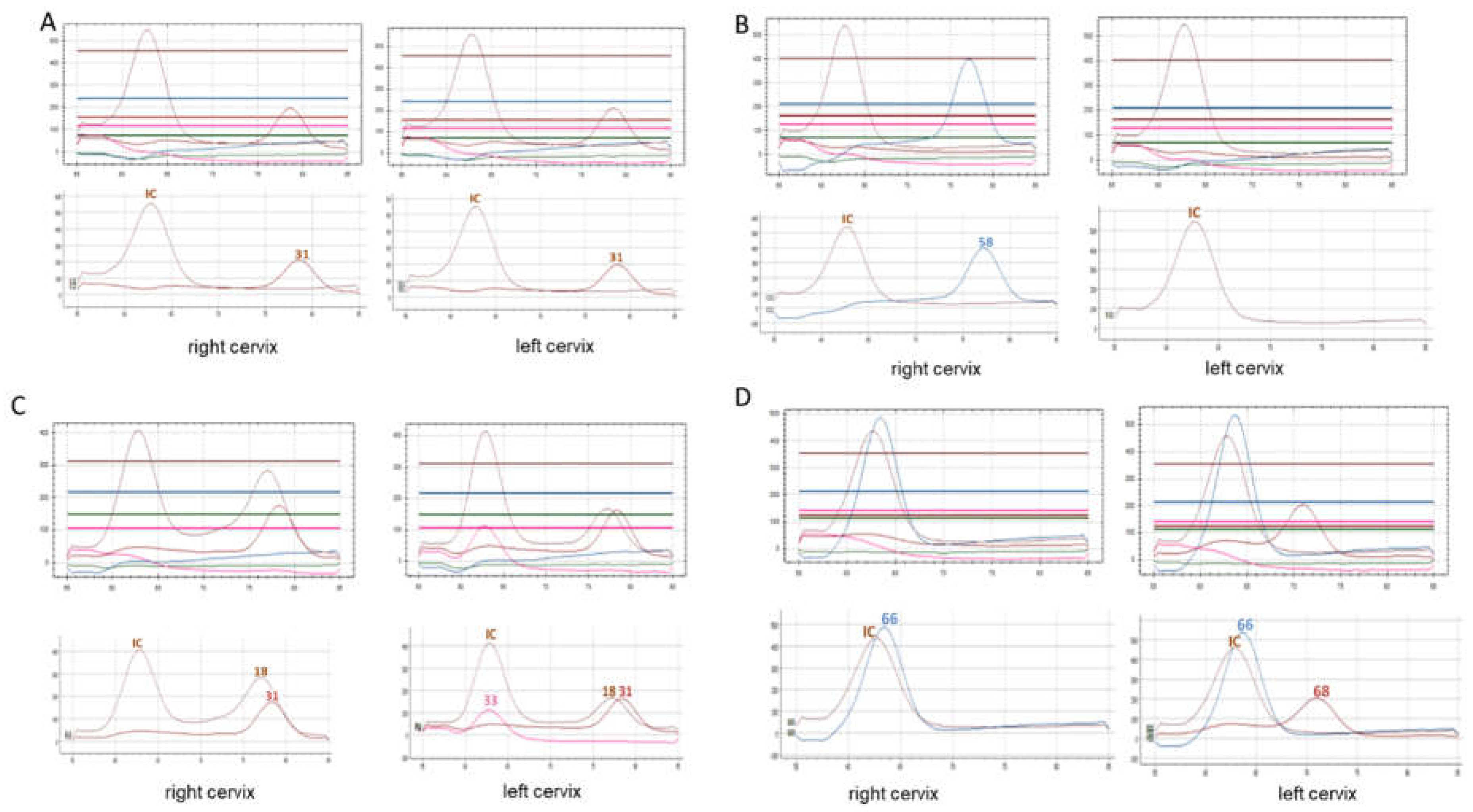
In one woman (A) both cervix samples showed genotype 31 (
Figure 1); in the second woman (B) the left cervix sample was negative while the right sample showed genotype 58; in the third woman (C), the right cervix sample tested positive for HPV 18 and 31, while the left sample for 18, 31 and 33 (
Figure 1). In the last woman (D) one cervix showed genotype 66 while the other one the HPV 66 and 68 (
Figure 1).
In the three cases (women B C D) showing different results on the two brush cervix samples, we repeated the HR-HPV extended genotyping. Repeated HPV test confirmed all the previous results.
The cytologic diagnoses of the positive HR-HPV cases were reported in the
Table 1.
3.2. Discussion
It is known that the main risk factor for development of cervical cancer is HR-HPV infection: therefore, it is preventable and can be easily treated if detected at early stages [6]. To prevent cervical neoplastic pathologies, the Lazio Region, according to the National indications, structured a screening program involving a large number of women [5]. The gynaecological examination followed by cervix-brush performed on a large number of women allowed to identify women with genital malformation such as the double cervix.
This congenital malformation is estimated to have an incidence close to 0.2-0.4% in the general population and a prevalence of around 4-7% [8,9]. Likewise, dysplastic and neoplastic pathologies of the cervix in patients with this malformation are extremely rare, while only few similar findings are described in the literature [4,8] in relationship to HPV-screening.
It is interesting to note that, although several authors describe cases of carcinomas involving both cervices [8,9,10], where the detected neoplasia was present in only one of the cervices [11], other authors report different degrees of dysplastic/malignant lesions in the two cervices [12,13]. Most of these cases reported in the literature were symptomatic and diagnosed only when the women complained genital bleeding or abnormal pain [4].
Fox et al. [14], Loo et al. [15], and Sparic et al. [16] declared that the Pap test of these patients showed cytological atypia, such dyskaryosis and koilocytosis, suggestive of HPV infection.
Only a few authors published data relating to HR-HPV genotypes: Zong et al. [12] reported two HPV-16 positive cervical carcinoma cases, Wang et al. [4] described the case of a woman, with squamous cell carcinoma affecting both cervices, who was HPV-16/18 positive, and Pinto et al. [17] reported a case of double cervix with bilateral High Squamous Intraepithelial Lesion (HSIL) associated in the write cervix with HR-HPV-33 genotype and in the left cervix with HR-HPV-35 genotype.
To our knowledge, there are no works in literature regarding cervical carcinoma screening program of women with congenital malformations such as a double cervix.
The aim of screening campaigns is to monitor the persistence of HR-HPV in order to early diagnose and treat dysplastic lesions before they evolve into an infiltrating neoplasm [5].
Our data shows that 16.7% of the women with double cervix resulted as HR-HPV positives; this percentage is slightly higher than the overall population examined (13.9%) [5], in our Laboratory.
Two of four HPV-positive cases showed discordant genotypes among double cervix: this difference could be due to either low viral load or the contamination occurred during brush sampling with material from the other cervix (C and D females,
Figure 1). In the female B, only one of the two cervices was positive to HPV (
Figure 1). It is interesting to note that the two cervices can be infected by different viral genotypes. Our findings confirm data already reported in a single case [17], also considering that the neoplasm can affect both cervices with lesions of the same or different grade [10,17,18] or only one of the tow cervices [11]. We can speculate that, in women with this malformation, the two cervices may be differently sensitive to the HR-HPV infection with different risk to develop neoplasia. Our data show that cytological findings were the same on both cervix: nevertheless, the only one Low-grade Squamous Intraepithelial Lesion (LSIL) case was associated with multiple HR-HPV infection [19].
4. Conclusion
Our data are in keeping with the literature and confirm that uterine malformations are rare events and can remain unrecognized for several years. The national cervical cancer screening programs in these particular cases are important not only for the early diagnosis and treatment of neoplastic lesions but also to identify these rare abnormalities. Since the two cervices may be differently susceptible to the viral infection, it is necessary to evaluate and analyze separately them to be conclusive in reporting potential risks of infection and cancer, respectively.
Authors Contribution
Tiziana Pisani and Maria Cenci: analyzed the data and wrote the paper; Ettore Domenico Capoluongo: reviewed and supervised the paper.
Acknowledgments
We would like to thank Dr. Francesca Fanfarillo for his support in revising the English. The Authors also express their gratitude to Dr. Eloisa Mania, Dr. Mauro Alderisio, Dr. Valeria Bonanni and Dr. Antonella Di Luzio for providing the cytological diagnoses. Authors thank Arrow Diagnostics for technical support to this work.
Conflicts of Interest
All Authors declare no conflict of interest in relation to this study.
References
- De Sanjosé S, Brotons M, Pavón MA. The natural history of human papillomavirus infection. Best Pract Res Clin Obstet Gynaecol 2018; 47:2-13. [CrossRef]
- Gong M, Chen C, Zhao H, Guo L, Sun M, Song M: Analysis of Distributions of HPV Infection in Females with Cervical Lesions in the Western District of Beijing Chaoyang Hospital. J Healthc Eng 2022; 14. [CrossRef]
- Pimple S, Mishra G. Cancer cervix: Epidemiology and disease burden. Cytojournal 2022; 19: 21. [CrossRef]
- Wang L, Liu Z. Bilateral cervical cancer in a complete septate uterus with a double cervix and vagina: a case report. J Int Med Res 2023;51(3). [CrossRef]
- Cenci M, Rossi F, Pisani T. Detection of 14 High-risk Human Papillomavirus (HPV) Genotypes Within the Italian Cervical Cancer Screening. In Vivo 2023; 37(5):2161-2165. [CrossRef]
- Pimple SA, Mishra GA. Global strategies for cervical cancer prevention and screening. Minerva Ginecol 2019;71(4):313-320. [CrossRef]
- Smith BC, Brown DL, Carter RE, Famuyide AO. Double cervix: clarifying a diagnostic dilemma. Am J Obstet Gynecol 2014; 211(1): 26 e1-5. [CrossRef]
- Gong Y, Xie Y, Chen L, Sui L. Cervical Cancer in a Septate Uterus with Double Cervix and Double Vagina: A Case Report and Review of the Literature. Int J Womens Health 2022;14: 345-351. [CrossRef]
- Gauwerky F. Doppeltes. Portiokarzinom bei Uterus duplex und Vagina subsepta [Double cervical carcinoma in a case of double uterus and subseptate vagina]. Zentralbl Gynakol 1955;77(25):967-71 German. [PubMed]
- Wall RL Jr. Didelphic uterus with carcinoma in situ of both cervices. Am J Obstet Gynecol. 1958;76(4):803-6. [CrossRef]
- Corbett PJ, Crompton AC. Invasive carcinoma of one cervix in a uterus didelphys. Case report. Br J Obstet Gynaecol 1982; 89(2):171-2. [CrossRef]
- Zong L, Wang W, He Y, Cheng N, Xiang Y. Carcinoma of the lower female genital tract in patients with genitourinary malformations: a clinicopathologic analysis of 36 cases. J Cancer 2019; 2; 10(13):3054-3061. [CrossRef]
- Lee CD, Churn M, Haddad N, Davies-Humphries J, Kingston RK, et al. Bilateral radical radiotherapy in a patient with uterus didelphys. Br J Radiol 2000;73(869):553-6. [CrossRef]
- Fox S, Mones JM, Kronstadt R, Saldana MJ. Bilateral and synchronous squamous cell carcinoma of the cervix in a patient with uterus didelphys. Obstet Gynecol 1986; 67(3 Suppl):76S-79S. [CrossRef]
- Loo HW, Locks SM. Squamous cell carcinoma of the cervix: report of an unusual case of bicornuate bicollis uterus treated with bilateral intracavity brachytherapy. Br J Radiol 2010;83(991):e143-6. [CrossRef]
- Sparic R, Dotlic J, Kovac J, Babovic I, Buzadzic S, Mirkovic L, et al. Management of cervical dysplasia in patient with Müllerian anomaly: diagnostic and therapeutic challenges. Eur J Gynaecol Oncol 2017;38(3):469-472. [CrossRef]
- Pinto KR, Lu DW, Rader JS, Dávila RM. Double cervix with bilateral and synchronous HSIL associated with different high-risk HPV types. A case report. Acta Cytol 2004;48(2):273-7. [CrossRef]
- Bakri Y, Salem H, Sadi AR, Mansour M. Bilateral and synchronous cervical carcinoma in situ in a didelphic uterus. Int J Gynaecol Obstet 1992;37(4):289-91. [CrossRef]
- Pisani T, Cenci M. Prevalence of Multiple High Risk Human Papilloma Virus (HR-HPV) Infections in Cervical Cancer Screening in Lazio Region, Italy. Cancer Diagn Progn 2024;3;4(1):42-45. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).