Submitted:
28 May 2024
Posted:
29 May 2024
You are already at the latest version
Abstract
Keywords:
1. The Significance of Repurposing
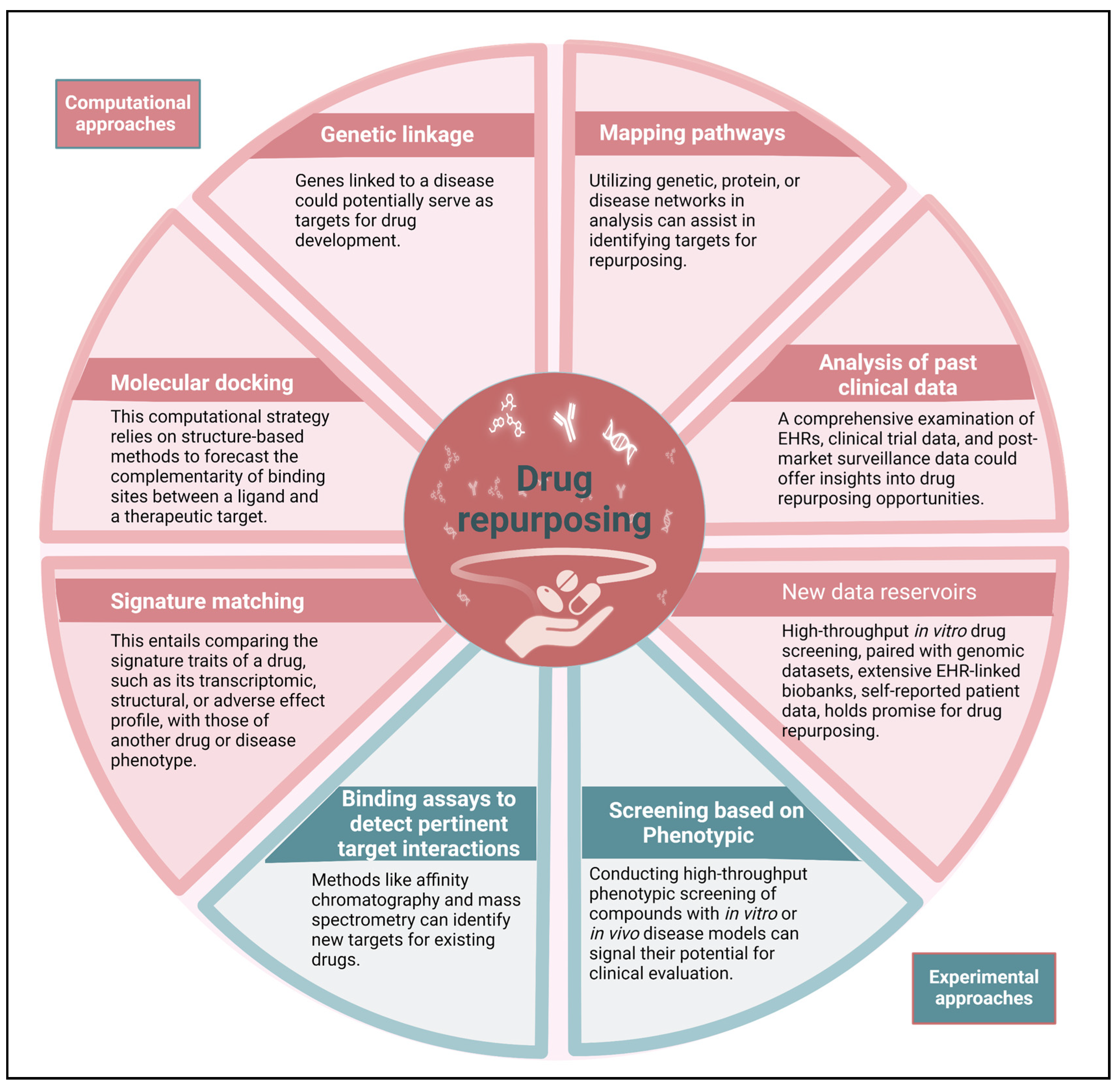
2. Pharmacological Repurposing Strategies and Tools
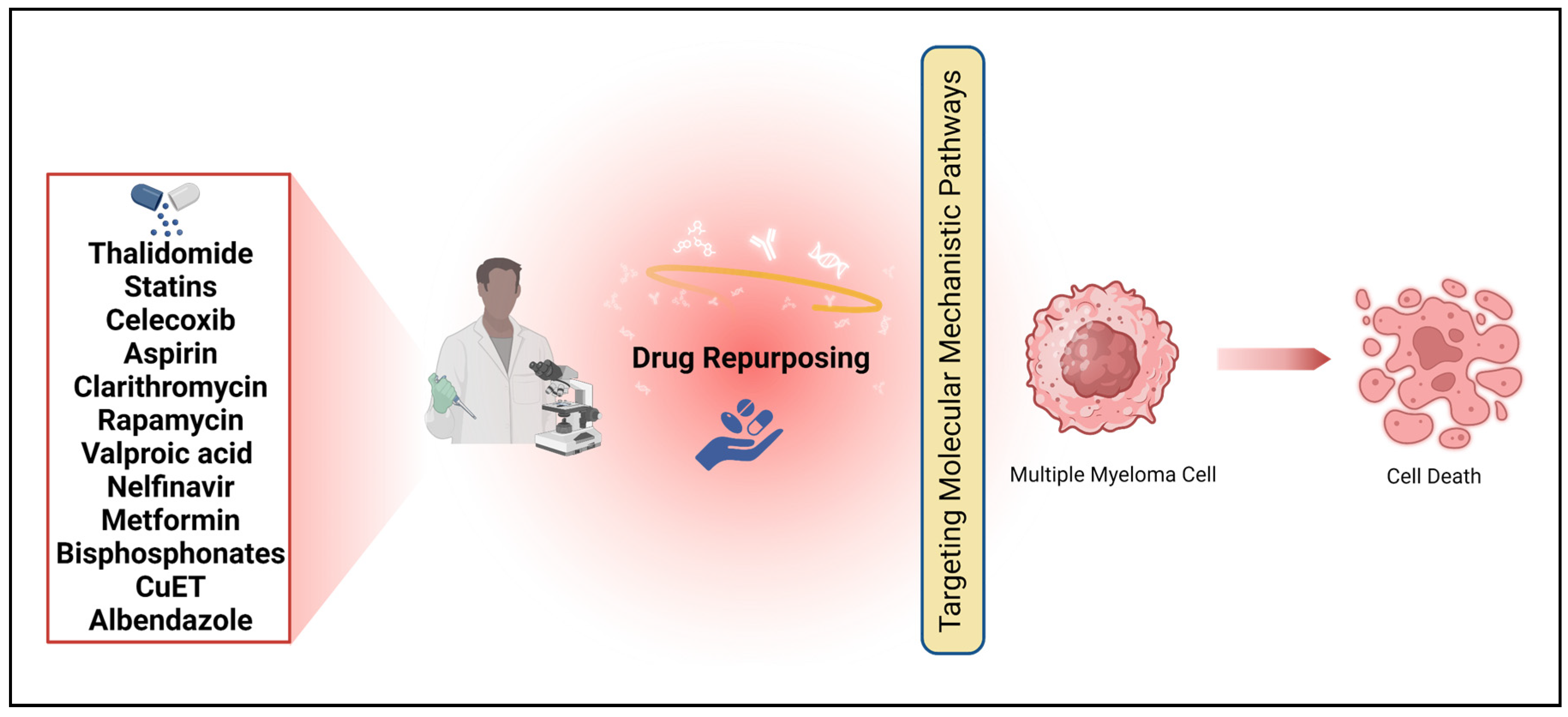
3. Medicines That Could Be Repurposed to Treat MM
3.1. Thalidomide
3.2. Statins
3.3. Celecoxib
3.4. Aspirin
3.5. Clarithromycin
3.6. Rapamycin
3.7. Valproic Acid
3.8. Nelfinavir
3.9. Metformin
3.10. Bisphosphonates
3.11. CuET
3.12. Albendazole
4. Conclusions and Future Prospectives
- Practice points
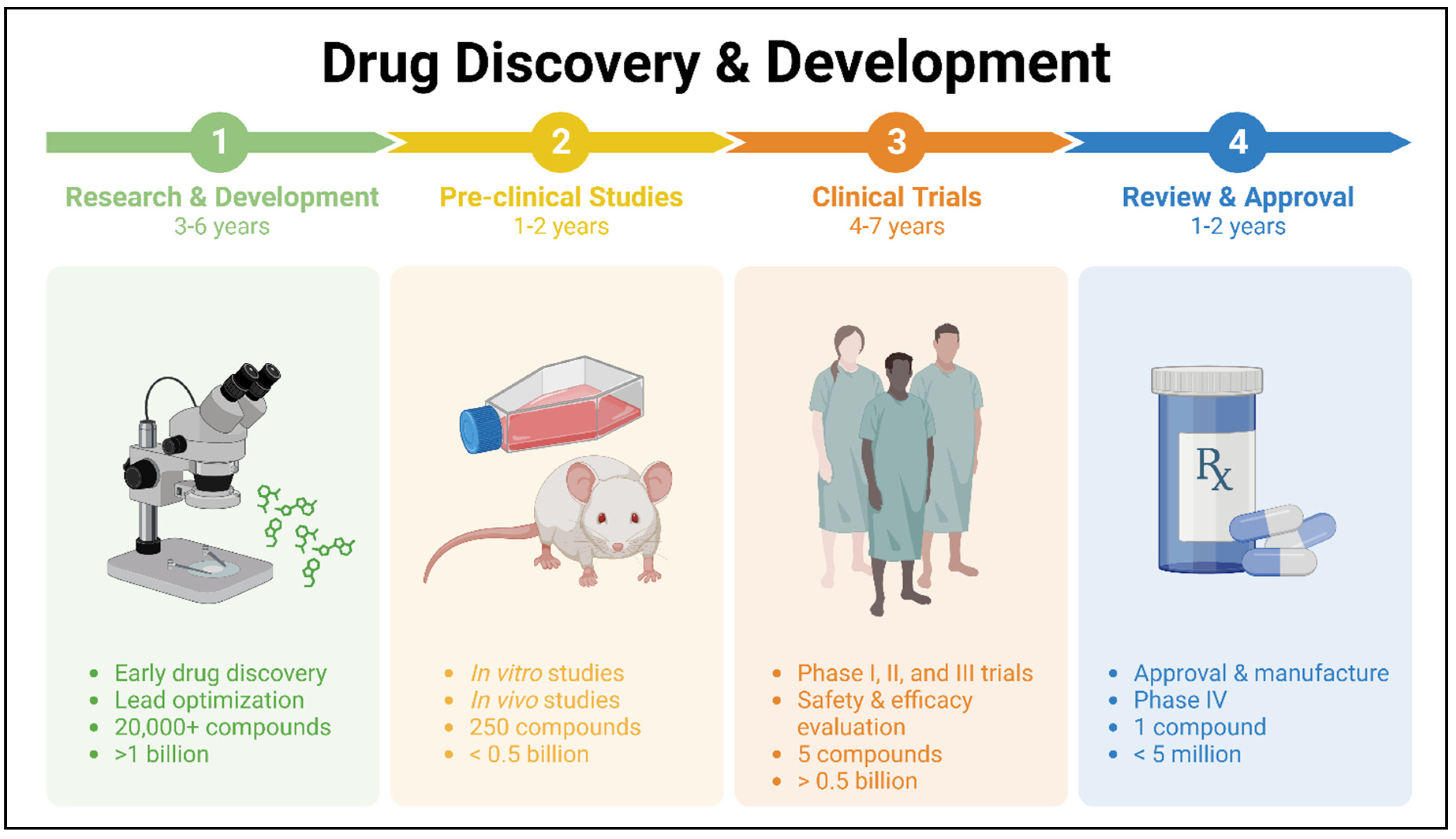
- Although there have been numerous clinical trials conducted to evaluate different approaches for treating cancer, the 5-year survival rate for individuals with MM in the US remains at a modest 55%.
- Myeloma remains a challenging malignancy to treat due to the development of drug resistance, resulting in relapse for all patients.
- There is an ongoing demand for new medications. However, the process of finding a new treatment can often be quite time-consuming. Therefore, repurposing already approved non-cancer medication for MM can aid in the discovery of new effective drugs.
- The potential for repurposing approved drugs is promising, although a thorough analysis of these agents is necessary before they can be considered for clinical trials.
- The potential of various non anti-cancer drugs as an anti-myeloma treatment was discussed.
- Thalidomide stands out as an exemplary repurposed agent for treating MM.
- There is encouraging evidence that statins, rapamycin, clarithromycin, and leflunomide can inhibit MM.
- Extensive animal studies using the MM animal model, along with phase 1 clinical studies, are necessary to thoroughly investigate these agents as potential MM therapies.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Consent for publication
References
- Yang, J., et al., Disparities in mortality risk after diagnosis of hematological malignancies in 185 countries: A global data analysis. Cancer Letters, 2024: p. 216793.
- Shameer, K., et al., Systematic analyses of drugs and disease indications in RepurposeDB reveal pharmacological, biological and epidemiological factors influencing drug repositioning. Briefings in bioinformatics, 2018. 19(4): p. 656-678.
- Ashburn, T.T. and K.B. Thor, Drug repositioning: identifying and developing new uses for existing drugs. Nature reviews Drug discovery, 2004. 3(8): p. 673-683.
- Scannell, J.W., et al., Diagnosing the decline in pharmaceutical R&D efficiency. Nature reviews Drug discovery, 2012. 11(3): p. 191-200.
- Pammolli, F., L. Magazzini, and M. Riccaboni, The productivity crisis in pharmaceutical R&D. Nature reviews Drug discovery, 2011. 10(6): p. 428-438.
- Waring, M.J., et al., An analysis of the attrition of drug candidates from four major pharmaceutical companies. Nature reviews Drug discovery, 2015. 14(7): p. 475-486.
- Beachy, S.H., et al., Drug repurposing and repositioning: workshop summary. 2014: National Academies Press Washington, DC.
- DiMasi, J.A., H.G. Grabowski, and R.W. Hansen, Innovation in the pharmaceutical industry: new estimates of R&D costs. Journal of health economics, 2016. 47: p. 20-33.
- Paul, S.M., et al., How to improve R&D productivity: the pharmaceutical industry's grand challenge. Nature reviews Drug discovery, 2010. 9(3): p. 203-214.
- Papapetropoulos, A.
- Hernandez, J.J., et al., Giving drugs a second chance: overcoming regulatory and financial hurdles in repurposing approved drugs as cancer therapeutics. Frontiers in oncology, 2017. 7: p. 273.
- Nosengo, N., Can you teach old drugs new tricks? Nature, 2016. 534(7607): p. 314-316.
- Ishida, J., et al., Repurposing of approved cardiovascular drugs. Journal of translational medicine, 2016. 14: p. 1-15.
- Cheng, F., et al., A genome-wide positioning systems network algorithm for in silico drug repurposing. Nature communications, 2019. 10(1): p. 3476.
- Rudrapal, M., S.J. Khairnar, and A.G. Jadhav, Drug repurposing (DR): an emerging approach in drug discovery. Drug repurposing-hypothesis, molecular aspects and therapeutic applications, 2020. 10.
- Rajkumar, S.V. and S. Kumar, Multiple myeloma current treatment algorithms. Blood cancer journal, 2020. 10(9): p. 1-10.
- Dehghanifard, A., et al., Various signaling pathways in multiple myeloma cells and effects of treatment on these pathways. Clinical Lymphoma Myeloma and Leukemia, 2018. 18(5): p. 311-320.
- Al-Odat, O.S., et al., Mcl-1 inhibition: managing malignancy in multiple myeloma. Frontiers in Pharmacology, 2021. 12: p. 699629.
- Hurle, M.R., et al., Computational drug repositioning: from data to therapeutics. Clinical Pharmacology & Therapeutics, 2013. 93(4): p. 335-341.
- Keiser, M.J., et al., Predicting new molecular targets for known drugs. Nature, 2009. 462(7270): p. 175-181.
- Hieronymus, H., et al., Gene expression signature-based chemical genomic prediction identifies a novel class of HSP90 pathway modulators. Cancer cell, 2006. 10(4): p. 321-330.
- Data, O., Gross domestic spending on R&D. Retrieved Mai, 2017. 14.
- Cheng, F., et al., Network-based approach to prediction and population-based validation of in silico drug repurposing. Nature communications, 2018. 9(1): p. 2691.
- Nam, Y., et al., Drug repurposing with network reinforcement. BMC bioinformatics, 2019. 20: p. 1-10.
- Zickenrott, S., et al., Prediction of disease–gene–drug relationships following a differential network analysis. Cell death & disease, 2016. 7(1): p. e2040-e2040.
- Hu, G. and P. Agarwal, Human disease-drug network based on genomic expression profiles. PloS one, 2009. 4(8): p. e6536.
- Peyvandipour, A., et al., A novel computational approach for drug repurposing using systems biology. Bioinformatics, 2018. 34(16): p. 2817-2825.
- Naylor, D.M., D. Kauppi, and J. Schonfeld, Therapeutic drug repurposing, repositioning and rescue. Drug Discovery, 2015. 57.
- Chatr-Aryamontri, A., et al., The BioGRID interaction database: 2013 update. Nucleic acids research, 2012. 41(D1): p. D816-D823.
- Szklarczyk, D., et al., STRING v10: protein–protein interaction networks, integrated over the tree of life. Nucleic acids research, 2015. 43(D1): p. D447-D452.
- Chen, J.Y., R. Pandey, and T.M. Nguyen, HAPPI-2: a comprehensive and high-quality map of human annotated and predicted protein interactions. BMC genomics, 2017. 18(1): p. 1-16.
- Kanehisa, M., et al., KEGG: new perspectives on genomes, pathways, diseases and drugs. Nucleic acids research, 2017. 45(D1): p. D353-D361.
- Croft, D., et al., Nucleic Acids Research 39 (Database issue)(2011) D691–D697. URL:< http://dx. doi. org/10.1093/nar/gkq1018.
- Wang, Z., M. Jensen, and J. Zenklusen, A Practical Guide to the Cancer Genome Atlas (TCGA). Statistical Genomics. Methods and Protocols, 2016: p. 111-141.
- Uhlén, M., et al., Tissue-based map of the human proteome. Science, 2015. 347(6220): p. 1260419.
- Uhlen, M., et al., Towards a knowledge-based human protein atlas. Nature biotechnology, 2010. 28(12): p. 1248-1250.
- Uhlén, M., et al., A human protein atlas for normal and cancer tissues based on antibody proteomics. Molecular & cellular proteomics, 2005. 4(12): p. 1920-1932.
- Barretina, J., et al., The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature, 2012. 483(7391): p. 603-607.
- Lamb, J., et al., The Connectivity Map: using gene-expression signatures to connect small molecules, genes, and disease. science, 2006. 313(5795): p. 1929-1935.
- Lamb, J., The Connectivity Map: a new tool for biomedical research. Nature reviews cancer, 2007. 7(1): p. 54-60.
- Borate, B. and A.D. Baxevanis, Searching Online Mendelian Inheritance in Man (OMIM) for information on genetic loci involved in human disease. Current protocols in bioinformatics, 2009. 27(1): p. 1.2. 1-1.2. 13.
- Goh, K.-I., et al., The human disease network. Proceedings of the National Academy of Sciences, 2007. 104(21): p. 8685-8690.
- Yang, J., et al., DNetDB: The human disease network database based on dysfunctional regulation mechanism. BMC systems biology, 2016. 10(1): p. 1-8.
- Law, V., et al., DrugBank 4.0: shedding new light on drug metabolism. Nucleic acids research, 2014. 42(D1): p. D1091-D1097.
- Andersson, M.L., et al., Evaluation of usage patterns and user perception of the drug–drug interaction database SFINX. International Journal of Medical Informatics, 2015. 84(5): p. 327-333.
- Kale, V.P., et al. Old drugs, new uses: Drug repurposing in hematological malignancies. in Seminars in cancer biology. 2021. Elsevier.
- Kuhn, M., et al., The SIDER database of drugs and side effects. Nucleic acids research, 2016. 44(D1): p. D1075-D1079.
- Siramshetty, V.B., et al., WITHDRAWN—a resource for withdrawn and discontinued drugs. Nucleic acids research, 2016. 44(D1): p. D1080-D1086.
- Kuhn, M., et al., STITCH 3: zooming in on protein–chemical interactions. Nucleic acids research, 2012. 40(D1): p. D876-D880.
- Garnett, M.J., et al., Systematic identification of genomic markers of drug sensitivity in cancer cells. Nature, 2012. 483(7391): p. 570-575.
- Lee, B.K.B., et al., DeSigN: connecting gene expression with therapeutics for drug repurposing and development. BMC genomics, 2017. 18(1): p. 1-11.
- Kumar, S., T. Witzig, and S.V. Rajkumar, Thalidomide as an anti-cancer agent. Journal of cellular and molecular medicine, 2002. 6(2): p. 160-174.
- Miller, M.T., Thalidomide embryopathy: a model for the study of congenital incomitant horizontal strabismus. Transactions of the American Ophthalmological Society, 1991. 89: p. 623.
- Grover, J., et al., Thalidomide: a re-look. The National Medical Journal of India, 2000. 13(3): p. 132-141.
- Perri III, A.J. and S. Hsu, A review of thalidomide's history and current dermatological applications. Dermatology online journal, 2003. 9(3).
- Gordon, J. and P. Goggin, Thalidomide and its derivatives: emerging from the wilderness. Postgraduate medical journal, 2003. 79(929): p. 127-132.
- Holmes, A., et al., Thalidomide Therapy for the Treatment of Hypertrophic Herpes Simplex Virus—Related Genitalis in HIV-Infected Individuals. Clinical Infectious Diseases, 2007. 44(11): p. e96-e99.
- Holland, S., Cytokine therapy of mycobacterial infections. Advances in internal medicine, 2000. 45: p. 431-452.
- Gupta, S.C., et al., Cancer drug discovery by repurposing: teaching new tricks to old dogs. Trends in pharmacological sciences, 2013. 34(9): p. 508-517.
- Locksley, R.M., N. Killeen, and M.J. Lenardo, The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell, 2001. 104(4): p. 487-501.
- Hideshima, T., et al., NF-κB as a therapeutic target in multiple myeloma. Journal of Biological Chemistry, 2002. 277(19): p. 16639-16647.
- Singhal, S. and J. Mehta, Thalidomide in cancer. Biomedicine & Pharmacotherapy, 2002. 56(1): p. 4-12.
- Kumar, V. and S. Chhibber, Thalidomide: an old drug with new action. Journal of Chemotherapy, 2011. 23(6): p. 326-334.
- Solèr, R.A., et al., Regression of AIDS-related Kaposi's sarcoma during therapy with thalidomide. Clinical infectious diseases, 1996. 23(3): p. 501-503.
- Tunio, M.A., et al., Low-dose thalidomide in patients with metastatic renal cell carcinoma. Brain, 2012. 3: p. 3.75.
- Franks, M.E., G.R. Macpherson, and W.D. Figg, Thalidomide. The Lancet, 2004. 363(9423): p. 1802-1811.
- Figg, W.D., et al., A double-blind randomized crossover study of oral thalidomide versus placebo for androgen dependent prostate cancer treated with intermittent androgen ablation. The Journal of urology, 2009. 181(3): p. 1104-1113.
- Ghobrial, I.M. and S.V. Rajkumar, Management of thalidomide toxicity. The journal of supportive oncology, 2003. 1(3): p. 194.
- Fadul, C.E., et al., A phase II study of thalidomide and irinotecan for treatment of glioblastoma multiforme. Journal of Neuro-oncology, 2008. 90: p. 229-235.
- Penas-Prado, M., et al., Randomized phase II adjuvant factorial study of dose-dense temozolomide alone and in combination with isotretinoin, celecoxib, and/or thalidomide for glioblastoma. Neuro-oncology, 2015. 17(2): p. 266-273.
- Chapman-Shimshoni, D., et al., Simvastatin induces apoptosis of B-CLL cells by activation of mitochondrial caspase 9. Experimental hematology, 2003. 31(9): p. 779-783.
- Pradelli, D., et al., Statins use and the risk of all and subtype hematological malignancies: a meta-analysis of observational studies. Cancer Medicine, 2015. 4(5): p. 770-780.
- Yi, X., et al., Statin use is associated with reduced risk of haematological malignancies: evidence from a meta-analysis. PloS one, 2014. 9(1): p. e87019.
- Afzal, A., et al., Statins reduce mortality in multiple myeloma: a population-based US study. Clinical Lymphoma Myeloma and Leukemia, 2020. 20(12): p. e937-e943.
- Brånvall, E., et al., Statin use is associated with improved survival in multiple myeloma: A Swedish population-based study of 4315 patients. American Journal of Hematology, 2020. 95(6): p. 652-661.
- Sanfilippo, K.M., et al., Statins are associated with reduced mortality in multiple myeloma. Journal of Clinical Oncology, 2016. 34(33): p. 4008.
- Epstein, M.M., et al., Statin use and risk of multiple myeloma: An analysis from the cancer research network. International journal of cancer, 2017. 141(3): p. 480-487.
- Zhang, P. and B. Liu, Statin use and the risk of multiple myeloma: A PRISMA-compliant meta-analysis. Annals of Hematology, 2020. 99: p. 1805-1812.
- Longo, J., et al., The mevalonate pathway is an actionable vulnerability of t (4; 14)-positive multiple myeloma. Leukemia, 2021. 35(3): p. 796-808.
- Juarez, D., et al., Statin-induced mitochondrial priming sensitizes multiple myeloma cells to BCL2 and MCL1 inhibitors. Cancer Research Communications, 2023.
- Cetin, M., et al., Overexpression of cyclooxygenase-2 in multiple myeloma: association with reduced survival. American journal of hematology, 2005. 80(3): p. 169-173.
- Ladetto, M., et al., Cyclooxygenase-2 (COX-2) is frequently expressed in multiple myeloma and is an independent predictor of poor outcome. Blood, 2005. 105(12): p. 4784-4791.
- Bernard, M., et al., Targeting cyclooxygenase-2 in hematological malignancies: rationale and promise. Current pharmaceutical design, 2008. 14(21): p. 2051-2060.
- Trojan, A., et al., Clinical significance of cyclooxygenase-2 (COX-2) in multiple myeloma. Swiss medical weekly, 2006. 136(25-26): p. 400-403.
- Tołoczko-Iwaniuk, N., et al., Celecoxib in cancer therapy and prevention–review. Current Drug Targets, 2019. 20(3): p. 302-315.
- Jendrossek, V., Targeting apoptosis pathways by Celecoxib in cancer. Cancer letters, 2013. 332(2): p. 313-324.
- Steinbach, G., et al., The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. New England Journal of Medicine, 2000. 342(26): p. 1946-1952.
- Scilimati, A., Patient Bone Marrow Aspiration to Explore the Cyclooxygenases (COXs) Involvement in Multiple Myeloma. J. Cancer Res. Therap. Oncol, 2021. 9: p. 1-19.
- Roy, P., U.A. Sarkar, and S. Basak, The NF-κB activating pathways in multiple myeloma. Biomedicines, 2018. 6(2): p. 59.
- Fan, L., et al., High expression of phosphorylated extracellular signal-regulated kinase (ERK1/2) is associated with poor prognosis in newly diagnosed patients with multiple myeloma. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 2017. 23: p. 2636.
- Liu, H., et al., Aspirin exerts anti-tumor effect through inhibiting Blimp1 and activating ATF4/CHOP pathway in multiple myeloma. Biomedicine & Pharmacotherapy, 2020. 125: p. 110005.
- Marinac, C.R., et al., Aspirin Use and Survival in Multiple Myeloma Patients. Blood, 2018. 132: p. 3250.
- Birmann, B.M., et al., Regular aspirin use and risk of multiple myeloma: a prospective analysis in the health professionals follow-up study and nurses' health study. Cancer prevention research, 2014. 7(1): p. 33-41.
- Sakamoto, M., et al., Effect of clarithromycin treatment of natural killer cell activity in patients with advanced non-small cell lung cancer. Gan to kagaku ryoho. Cancer & chemotherapy, 1998. 25(14): p. 2259-2266.
- Van Nuffel, A.M., et al., Repurposing Drugs in Oncology (ReDO)—clarithromycin as an anti-cancer agent. ecancermedicalscience, 2015. 9.
- Musto, P., et al., Inefficacy of clarithromycin in advanced multiple myeloma: a definitive report. Haematologica, 2002. 87(6): p. 658-659.
- Durie, B., Clarithromycin (Biaxin) as primary treatment for myeloma. Blood, 1997. 90: p. 579.
- Stewart, A., et al., Lack of response to short-term use of clarithromycin (BIAXIN) in multiple myeloma. Blood, The Journal of the American Society of Hematology, 1999. 93(12): p. 4441-4442.
- Moreau, P., et al., Lack of efficacy of clarithromycin in advanced multiple myeloma. Leukemia, 1999. 13(3): p. 490-491.
- Morris, T., et al., Phase II trial of clarithromycin and pamidronate therapy in myeloma. Medical Oncology, 2001. 18: p. 79-84.
- Coleman, M., et al., BLT-D (clarithromycin [Biaxin], low-dose thalidomide, and dexamethasone) for the treatment of myeloma and Waldenström's macroglobulinemia. Leukemia & lymphoma, 2002. 43(9): p. 1777-1782.
- Mark, T.M., et al., Thalidomide, clarithromycin, lenalidomide and dexamethasone therapy in newly diagnosed, symptomatic multiple myeloma. Leukemia & Lymphoma, 2014. 55(12): p. 2842-2849.
- Morris, T., et al., Clarithromycin with low dose dexamethasone and thalidomide is effective therapy in relapsed/refractory myeloma. British journal of haematology, 2008. 143(3): p. 349-354.
- Puig, N., et al., Lenalidomide and dexamethasone with or without clarithromycin in patients with multiple myeloma ineligible for autologous transplant: a randomized trial. Blood Cancer Journal, 2021. 11(5): p. 101.
- Klein, B., et al., Interleukin-6 in human multiple myeloma. 1995.
- Khan, A., et al., Effect of clarithromycin and azithromycin on production of cytokines by human monocytes. International journal of antimicrobial agents, 1999. 11(2): p. 121-132.
- Moriya, S., et al., Targeting the integrated networks of aggresome formation, proteasome, and autophagy potentiates ER stress-mediated cell death in multiple myeloma cells. International journal of oncology, 2015. 46(2): p. 474-486.
- Takemori, N., et al., Possible mechanisms of action of clarithromycin and its clinical application as a repurposing drug for treating multiple myeloma. ecancermedicalscience, 2020. 14.
- Sehgal, S., H. Baker, and C. Vézina, Rapamycin (AY-22, 989), a new antifungal antibiotic II. Fermentation, isolation and characterization. The Journal of antibiotics, 1975. 28(10): p. 727-732.
- Saunders, R.N., M.S. Metcalfe, and M.L. Nicholson, Rapamycin in transplantation: a review of the evidence. Kidney international, 2001. 59(1): p. 3-16.
- 1. Laplante, M. and D.M. Sabatini, mTOR signaling at a glance. Journal of cell science, 2009. 122(20): p. 3589-3594.
- Strömberg, T., et al., Rapamycin sensitizes multiple myeloma cells to apoptosis induced by dexamethasone. Blood, 2004. 103(8): p. 3138-3147.
- Gera, J. and A. Lichtenstein, The mammalian target of rapamycin pathway as a therapeutic target in multiple myeloma. Leukemia & lymphoma, 2011. 52(10): p. 1857-1866.
- Raje, N., et al., Combination of the mTOR inhibitor rapamycin and CC-5013 has synergistic activity in multiple myeloma. Blood, 2004. 104(13): p. 4188-4193.
- Kikuchi, J., et al., Histone deacetylases are critical targets of bortezomib-induced cytotoxicity in multiple myeloma. Blood, The Journal of the American Society of Hematology, 2010. 116(3): p. 406-417.
- Ichiyama, T., et al., Sodium valproate inhibits production of TNF-α and IL-6 and activation of NF-κB. Brain research, 2000. 857(1-2): p. 246-251.
- Wang, Y., et al., Valproic acid increased autophagic flux in human multiple myeloma cells in vitro. Biomedicine & Pharmacotherapy, 2020. 127: p. 110167.
- Zhang, Y., et al., Valproic acid activates autophagy in multiple myeloma cell lines RPMI8226 and U266. Zhonghua xue ye xue za zhi= Zhonghua Xueyexue Zazhi, 2016. 37(6): p. 478-483.
- Kitazoe, K.-i., et al., Valproic acid exerts anti-tumor as well as anti-angiogenic effects on myeloma. International journal of hematology, 2009. 89: p. 45-57.
- Yang, Y., et al., HIV-1 protease inhibitor induces growth arrest and apoptosis of human prostate cancer LNCaP cells in vitro and in vivo in conjunction with blockade of androgen receptor STAT3 and AKT signaling. Cancer science, 2005. 96(7): p. 425-433.
- 1. Bono, C., et al., The human immunodeficiency virus-1 protease inhibitor nelfinavir impairs proteasome activity and inhibits the proliferation of multiple myeloma cells in vitro and in vivo. Haematologica, 2012. 97(7): p. 1101.
- 2. Kawabata, S., et al., Synergistic effects of nelfinavir and bortezomib on proteotoxic death of NSCLC and multiple myeloma cells. Cell death & disease, 2012. 3(7): p. e353-e353.
- Kraus, M., et al., Nelfinavir augments proteasome inhibition by bortezomib in myeloma cells and overcomes bortezomib and carfilzomib resistance. Blood cancer journal, 2013. 3(3): p. e103-e103.
- Kalender, A., et al., Metformin, independent of AMPK, inhibits mTORC1 in a rag GTPase-dependent manner. Cell metabolism, 2010. 11(5): p. 390-401.
- Del Barco, S., et al., Metformin: multi-faceted protection against cancer. Oncotarget, 2011. 2(12): p. 896.
- Greaves, D. and Y. Calle, Epithelial Mesenchymal Transition (EMT) and Associated Invasive Adhesions in Solid and Haematological Tumours. Cells, 2022. 11(4): p. 649.
- Noto, H., et al., Cancer risk in diabetic patients treated with metformin: a systematic review and meta-analysis. PloS one, 2012. 7(3): p. e33411.
- Bodmer, M., et al., Long-term metformin use is associated with decreased risk of breast cancer. Diabetes care, 2010. 33(6): p. 1304-1308.
- Machado-Neto, J.A., et al., Metformin exerts multitarget antileukemia activity in JAK2V617F-positive myeloproliferative neoplasms. Cell death & disease, 2018. 9(3): p. 311.
- Mishra, A.K. and D. Dingli, Metformin inhibits IL-6 signaling by decreasing IL-6R expression on multiple myeloma cells. Leukemia, 2019. 33(11): p. 2695-2709.
- 1. Chang, S.-H., et al., Association between metformin use and progression of monoclonal gammopathy of undetermined significance to multiple myeloma in US veterans with diabetes mellitus: a population-based retrospective cohort study. The Lancet Haematology, 2015. 2(1): p. e30-e36.
- 2. Boursi, B., et al., Impact of metformin on the progression of MGUS to multiple myeloma. Leukemia & lymphoma, 2017. 58(5): p. 1265-1267.
- 3. LeGrand, J., et al., Global gene expression profiling in mouse plasma cell tumor precursor and bystander cells reveals potential intervention targets for plasma cell neoplasia. Blood, The Journal of the American Society of Hematology, 2012. 119(4): p. 1018-1028.
- Dalva-Aydemir, S., et al., Targeting the metabolic plasticity of multiple myeloma with FDA-approved ritonavir and metformin. Clinical Cancer Research, 2015. 21(5): p. 1161-1171.
- Mishra, R.K., et al., In silico modeling-based identification of glucose transporter 4 (GLUT4)-selective inhibitors for cancer therapy. Journal of Biological Chemistry, 2015. 290(23): p. 14441-14453.
- Zhao, Y., et al., Metformin and FTY720 synergistically induce apoptosis in multiple myeloma cells. Cellular Physiology and Biochemistry, 2018. 48(2): p. 785-800.
- Jagannathan, S., et al., Pharmacologic screens reveal metformin that suppresses GRP78-dependent autophagy to enhance the anti-myeloma effect of bortezomib. Leukemia, 2015. 29(11): p. 2184-2191.
- Berenson, J.R., Antitumor effects of bisphosphonates: from the laboratory to the clinic. Current opinion in supportive and palliative care, 2011. 5(3): p. 233-240.
- Weinstein, R.S., P.K. Roberson, and S.C. Manolagas, Giant osteoclast formation and long-term oral bisphosphonate therapy. New England Journal of Medicine, 2009. 360(1): p. 53-62.
- Mansour, A., A. Wakkach, and C. Blin-Wakkach, Emerging roles of osteoclasts in the modulation of bone microenvironment and immune suppression in multiple myeloma. Frontiers in immunology, 2017. 8: p. 954.
- 1. Tai, Y.-T., S.-F. Cho, and K.C. Anderson, Osteoclast immunosuppressive effects in multiple myeloma: role of programmed cell death ligand 1. Frontiers in immunology, 2018. 9: p. 1822.
- 2. Huang, X., et al., Diethyldithiocarbamate-copper complex (CuET) inhibits colorectal cancer progression via miR-16-5p and 15b-5p/ALDH1A3/PKM2 axis-mediated aerobic glycolysis pathway. Oncogenesis, 2021. 10(1): p. 4.
- 3. Suh, J.J., et al., The status of disulfiram: a half of a century later. Journal of clinical psychopharmacology, 2006. 26(3): p. 290-302.
- 4. Kannappan, V., et al., Recent advances in repurposing disulfiram and disulfiram derivatives as copper-dependent anticancer agents. Frontiers in Molecular Biosciences, 2021. 8: p. 741316.
- Guo, W., et al., Identification and characterization of multiple myeloma stem cell-like cells. Cancers, 2021. 13(14): p. 3523.
- Jin, N., et al., Disulfiram/copper targets stem cell-like ALDH+ population of multiple myeloma by inhibition of ALDH1A1 and Hedgehog pathway. Journal of cellular biochemistry, 2018. 119(8): p. 6882-6893.
- Chroma, K., et al., A drug repurposing strategy for overcoming human multiple myeloma resistance to standard-of-care treatment. Cell Death & Disease, 2022. 13(3): p. 203.
- Chai, J.-Y., B.-K. Jung, and S.-J. Hong, Albendazole and mebendazole as anti-parasitic and anti-cancer agents: an update. The Korean Journal of Parasitology, 2021. 59(3): p. 189.
- Wang, L.-J., et al., Non-mitotic effect of albendazole triggers apoptosis of human leukemia cells via SIRT3/ROS/p38 MAPK/TTP axis-mediated TNF-α upregulation. Biochemical Pharmacology, 2019. 162: p. 154-168.
- Yi, H., et al., Albendazole inhibits NF-κB signaling pathway to overcome tumor stemness and bortezomib resistance in multiple myeloma. Cancer Letters, 2021. 520: p. 307-320.
- Singhal, S., et al., Antitumor activity of thalidomide in refractory multiple myeloma. New England Journal of Medicine, 1999. 341(21): p. 1565-1571.
- Rajkumar, S.V., et al., Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. Journal of clinical oncology, 2006. 24(3): p. 431-436.
- Kardosh, A., et al., Multitarget inhibition of drug-resistant multiple myeloma cell lines by dimethyl-celecoxib (DMC), a non–COX-2 inhibitory analog of celecoxib. Blood, 2005. 106(13): p. 4330-4338.
- Holien, T., et al., Lymphoma and myeloma cells are highly sensitive to growth arrest and apoptosis induced by artesunate. European Journal of Haematology, 2013. 91(4): p. 339-346.
- Papanikolaou, X., et al., Artesunate overcomes drug resistance in multiple myeloma by inducing mitochondrial stress and non-caspase apoptosis. Oncotarget, 2014. 5(12): p. 4118.
- Li, S., et al., Effect of artesunate on inhibiting proliferation and inducing apoptosis of SP2/0 myeloma cells through affecting NFκB p65. International journal of hematology, 2009. 90: p. 513-521.
- Hu, G.-F., et al., Effects of Artesunate Combined with Arsenious Acid on Proliferation and Apoptosis of Multiple Myeloma Cells via PI3K/AKT Signaling Pathway. Zhongguo shi yan xue ye xue za zhi, 2021. 29(6): p. 1819-1824.
- Baumann, P., et al., Dihydroorotate dehydrogenase inhibitor A771726 (leflunomide) induces apoptosis and diminishes proliferation of multiple myeloma cells. Molecular cancer therapeutics, 2009. 8(2): p. 366-375.
- Rosenzweig, M., et al., Repurposing leflunomide for relapsed/refractory multiple myeloma: a phase 1 study. Leukemia & lymphoma, 2020. 61(7): p. 1669-1677.
- Yee, A.J., et al., Outcomes in patients with relapsed or refractory multiple myeloma in a phase I study of everolimus in combination with lenalidomide. British journal of haematology, 2014. 166(3): p. 401-409.
- Koltai, T., Nelfinavir and other protease inhibitors in cancer: mechanisms involved in anticancer activity. F1000Research, 2015. 4.
- Alodhaibi, I., et al., An Open-Label Phase I Study of Metformin and Nelfinavir in Combination With Bortezomib in Patients With Relapsed and Refractory Multiple Myeloma. Clinical Lymphoma Myeloma and Leukemia, 2024.
| Purpose | Resource | Ref. |
|---|---|---|
| Human pathways and protein-protein interaction (PPI) | BiGRID, STRING, HAPPI, KEGG, Reactome | [29,30,31,32,33] |
| Molecular classification of more than 20,000 main cancer matched normal tissue from 33 types of cancer | Cancer Genome Atlas | [34] |
| Protein expression in cancer, matched normal tissues, and cancer human cell lines | The Human Protein Atlas | [35,36,37] |
| Drug sensitivity, gene expression, and genotype for human cancer cell lines | Cancer Cell Line Encyclopedia | [38] |
| Data of genome-wide transcription expression from cultured human cancer cells with many small compounds | Connectivity Map 02 (CMap) | [39,40] |
| Disease-specific gene curation and analysis | OMIM, GEO | [41,42] |
| Disease-disease connectivity; connectivity of two genes elaborated within the same disease | The human disease network | [42] |
| Disease similarities as seen through the lens of gene regulatory mechanisms; comprehension of disease etiology and pathophysiology | Human Disease Network Database (DNetDB) | [43] |
| Drug-drug interaction; comprehensive drug-target information on tens of thousands of drugs and targets | DrugBank | [44] |
| Drug-drug interaction | SFINX | [45] |
| Database of more than 270 non-cancer drugs for potential repurposing for anti-cancer therapy | Repurposing Drugs in Oncology (ReDO) | [46] |
| Database of drugs and adverse drug reactions (ADRs) | Side Effect Resource (SIDER) | [47] |
| Withdrawn or discontinued drugs | WITHDRAWN | [48,49] |
| An inventory of main and secondary uses for repurposed pharmaceuticals | RepurposeDB | [2] |
| Chemical (including drugs)-protein interaction network | STITCH | [49] |
| Data on the sensitivity of hundreds of compounds and over a thousand cancer cell lines | Genomics of Drug Sensitivity in Cancer (GDSC) | [50] |
| Gene expression pattern-based prediction of drug effectiveness against cancer | DeSigN | [51] |
| Drug Name | Old-Indication | New-Indication | Mechanism of Action | Clinical Trials Status | Ref. |
|---|---|---|---|---|---|
| Thalidomide | Sedative, anti-nausea | MM | Inhibits IKK (also NF-κB); inhibits TNF; inhibits IL-1, IL-6, IL-12, VEGF | Approved in combination with dexamethasone | [151,152] |
| Statins | High Cholesterol | MM | HMG-CoA reductase inhibitors, upregulation of PUMA and NOXA | Smouldering MM, phase II | [74,75,76,77] |
| Celecoxib | Anti- inflammatory | MM and drug resistant MM | Inhibits COX-2, inhibits Mcl-1, Bcl-2, survivin, Akt | Not for MM, approved for FAP | [83,85,153] |
| Aspirin | Anti- inflammatory | MM | Inhibits COX-1 and COX-2, suppresses cytokines and NF-κB, inhibits EKR and Blimp1, activates ATF4/CHOP | Preclinical | [92,93] |
| Artesunate | Malaria | MM and drug resistant MM | Decreased expression of MYC and Bcl-2, triggers cleavage of caspase-3 | Preclinical | [154,155,156,157] |
| Leflunomide | Rheumatism | MM | DHODH inhibitor, cyclin D2 and pRb inhibition | Phase II NCT04508790 |
[158,159] |
| Clarithromycin | Antibiotic | MM and drug resistant MM | Inhibits IL-6 and MGFs | Phase II | [95,102] |
| Rapamycin | Fungal infections | MM | Antagonist of mTOR | Phase I | [112,113,114,160] |
| Valproic acid | Seizures, migraine, and epilepsy | MM | Block HDAC, inhibits NF-κB and cytokines | Preclinical | [115] |
| Nelfinavir | HIV Infection | MM and drug resistant MM | Inhibits 26S proteasome- disrupts Akt and STAT3, ERK1/2 | MM phase I | [121,123,161,162] |
| Metformin | Diabetes mellitus type 2 | MM | Activates AMPK (suppresses mTORC1, activates p53), inhibits EMT, regulates cell cycle proteins (ERK1/2, JAK2/STAT), IL-6 suppression | Smouldering Myeloma and Monoclonal gammopathy of undetermined significance phase II, MM phase I | [134,135,137,162] |
| Bisphosphonates | Osteoporosis | MM | HMG-CoA pathway suppression, osteoclast apoptosis | Preclinical | [140,141] |
| CuET | Alcohol-abuse drug disulfiram (DSF) |
Drug resistant MM | ALDH inhibition | Preclinical | [147] |
| Albendazole | Parasitic infections | Drug resistant MM | Microtubule system interference, p65/NF-κB pathway inhibtion | Preclinical | [150] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





