1. Introduction
Terson’s syndrome is defined as the presence of vitreous, preretinal, intraretinal or sub-retinal haemorrhage in the setting of subarachnoid bleeding or increased intracranial pressure after traumatic or non-traumatic intracerebral haemorrhage or even after traumatic brain injury with no intracranial bleeding. [
4,
7] The most common association of Terson’s syndrome is considered to be subarachnoid haemorrhage. Occurrence of Terson’s syndrome in cases of subarachnoid haemorrhage results in worse prognosis and significantly increased mortality. [
1,
5] Terson’s syndrome is usually associated with coma, Glasgow coma scale less than 8 or with severe neurological findings. [
6]
Acquired third nerve palsies are of particular importance since they might be caused by life-threatening intracranial aneurysms. [
3] In complete oculomotor nerve palsy the eye is positioned downwards and outwards and there is also complete ptosis and dilated pupil. A pupil-involving third nerve palsy comprises a medical emergency due to the possibility of the presence of an enlarging intracranial aneurysm more frequently at the posterior communicating artery. [
14] A pupil-sparing third nerve palsy also warrants extensive investigation and internal ophthalmoplegia may also develop later during the course of the disease. However, pupil-sparing third nerve palsies due to an intracranial aneurysm have also been reported. [
9]
We describe a case of Terson’s syndrome with Roth spot resembling features accompanied by a pupil-involving third nerve palsy in a patient without any radiologically diagnosed subarachnoid haemorrhage or disturbance of consciousness that resulted in the diagnosis of a right posterior communicating artery aneurysm.
2. Detailed Case Description
A 48-year-old Caucasian female was examined at the Emergency Department of the University Hospital of Patras. The patient presented with a 9-day history of ptosis of her right eyelid followed by a sudden decrease in vision of her left eye (OS). Her previous ocular and medical history were unremarkable.
When asked, the patient mentioned an episode of short duration intense headache combined with a single vomit 11 days ago. Neurological examination revealed a pupil-involving third nerve palsy without nuchal rigidity or any other neurological signs. The Glasgow coma scale was 15/15.
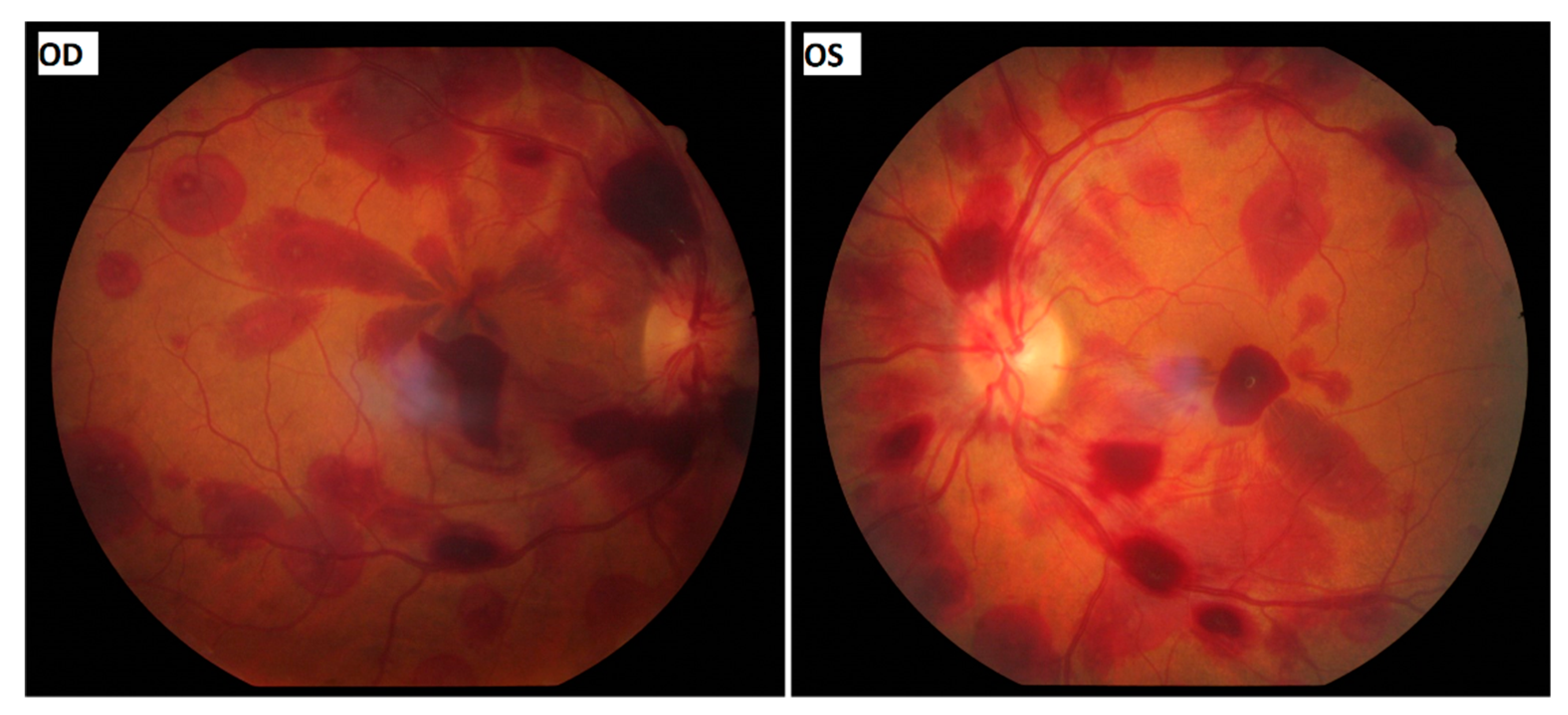
Ophthalmological examination confirmed the diagnosis of complete pupil-involving oculomotor nerve palsy, as there was ptosis of the patient’s right eyelid, the right eye (OD) was positioned downwards and outwards with inability to adduct, supraduct and infraduct and the pupil of the OD was fixed at 5.5 mm in diameter. The direct and consensual pupillary reflexes of OS were normal and the diameter of the pupil was 3 mm in photopic conditions. The patient’s best corrected visual acuity was 20/100 in OD and 20/70 in OS. The anterior segment examination was unremarkable. Dilated fundoscopy revealed multiple scattered intra- and pre-retinal haemorrhages in both eyes (
Figure 1). Several retinal haemorrhages in both eyes had a white-centered pattern resembling Roth spots. Subtle optic disk oedema was observed, especially in OD. These findings were compatible with bilateral Terson’s syndrome. Although Roth spot resembling features suggested the possibility of underlying haematological disease, the presence of a pupil-involving third nerve palsy constituted a neurosurgical emergency.
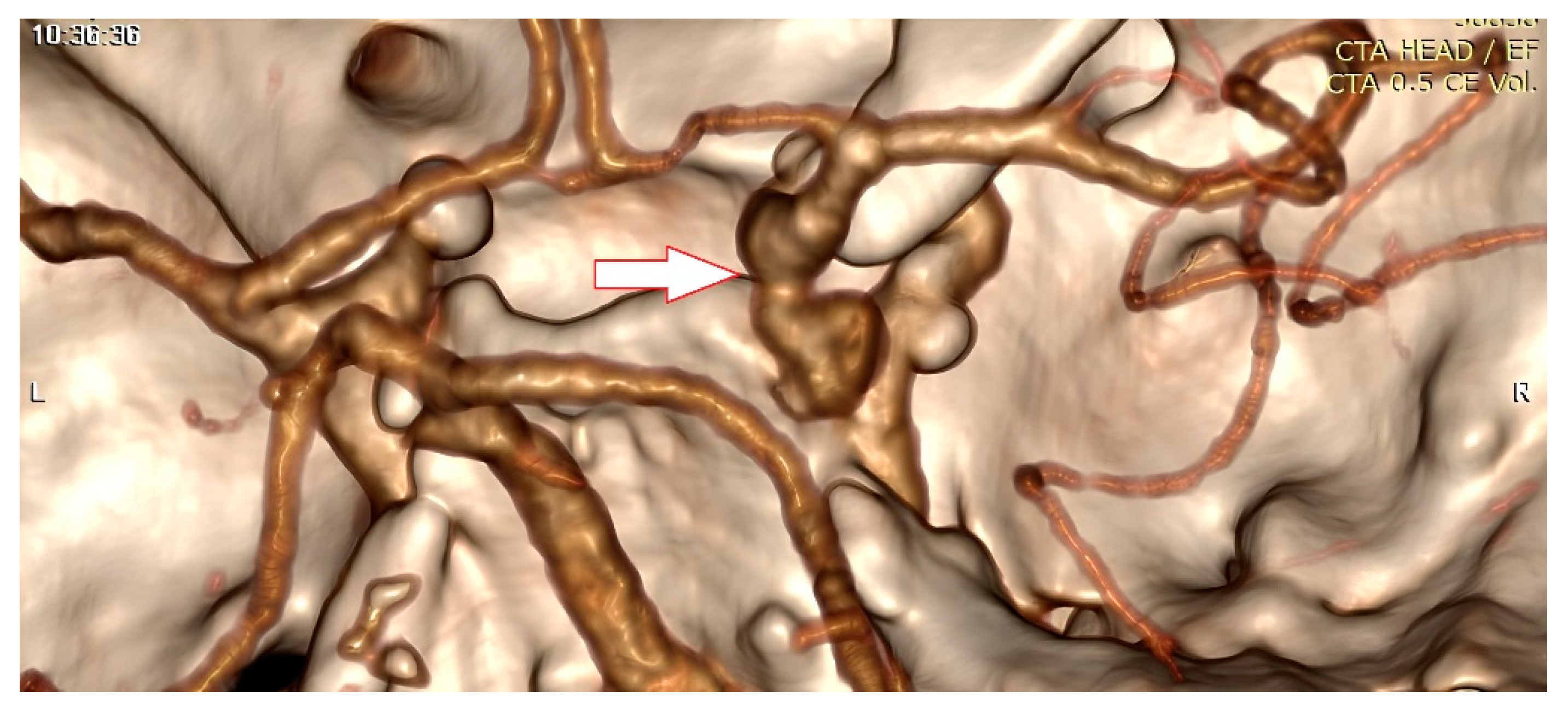
A cerebral computed tomography angiography revealed a 5 mm aneurysm of the right posterior communicating artery (
Figure 2). A lumbar puncture was also performed. The opening pressure was normal and the red blood cells count in the cerebrospinal fluid was 678 cells/mm3. The patient underwent a right pterional craniotomy and subsequent clipping of the aneurysm that compressed the right oculomotor nerve. No subarachnoid haemorrhage has been documented intraoperatively.
3. Discussion
Terson’s syndrome, although under-reported, seems to develop in almost 40% of cases with acute aneurysmal intracranial bleeds. [
6] It can be bilateral or unilateral and is characterized by the presence of any type of intraocular haemorrhage, involving several retinal layers. Vitreous haemorrhage is the most common type of intraocular haemorrhage in Terson’s syndrome and results in significant decrease in visual acuity [
6]. Several possible pathogenetic mechanisms for Terson’s syndrome have been proposed but the debate remains. The most accepted theory suggests an acute, even transient, spike in the intracranial pressure, usually due to an aneurysmal rupture, that leads to increased hydrostatic pressure in ocular venous system, decrease in venous return, venous stasis and to rupture of thin superficial retinal vessels. [
10] Terson’s syndrome is usually associated with coma, Glasgow coma scale less than 8 or with severe neurological findings. [
6] Nevertheless, there have been 2 published cases where Terson’s syndrome occurred without any neurological signs. [
11,
12]
The presence of Roth spot resembling features in our case suggested the possibility of underlying haematological disease. The presence, however, of a pupil-involving third nerve palsy constituted a neurosurgical emergency due to the possibility of the presence of an enlarging intracranial aneurysm.
The association of Terson’s syndrome with a pupil-involving third nerve palsy is well-known and has been reported before but, to our knowledge, only in the setting of radiologically diagnosed subarachnoid haemorrhage. [
13] In our case there were no radiological or intraoperative indications of subarachnoid haemorrhage, there was a normal opening pressure at lumbar puncture and the neuroimaging showed no signs of increased intracranial pressure. Only the red blood cell count in the cerebrospinal fluid was indicative of subarachnoid haemorrhage since it might have resulted from a minor leak of the aneurysm some days before [
2,
8] with an abrupt, transient increase in intracranial pressure which may have contributed to the pathogenesis of Terson’s syndrome. [
8]
4. Conclusions
We presented a case of Terson’s syndrome in which the treatment priority was the management of the aneurysm before a possible major rupture. Our case emphasizes that the ophthalmological consultation may assist the diagnosis of a life-threatening condition, as Terson’s syndrome may be indicative for minor cerebral aneurysm rupture. A high index of suspicion is required in order to recognize even the less typical cases.
Informed Consent Statement
Written informed consent was obtained from the patient involved in the study to publish this paper.
Conflicts of Interest
There are no competing interests to be declared.
References
- Czorlich P, Skevas C, Knospe V, Vettorazzi E, Richard G, Wagenfeld L, Westphal M, Regelsberger J. Terson syndrome in subarachnoid hemorrhage, intracerebral hemorrhage, and traumatic brain injury. Neurosurg Rev. 2015 Jan; 38(1):129-36; discussion 136. [CrossRef]
- Dugas C, Jamal Z, Bollu PC. Xanthochromia. [Updated 2020 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526048/.
- Fang C, Leavitt JA, Hodge DO, Holmes JM, Mohney BG, Chen JJ. Incidence and Etiologies of Acquired Third Nerve Palsy Using a Population-Based Method. JAMA Ophthalmol. 2017 Jan 1; 135(1):23-28. [CrossRef]
- Fonseca APA, Rosa Júnior M. Terson’s syndrome: an important differential diagnosis of subarachnoid hemorrhage. Radiol Bras. 2017 Sep-Oct;50(5):346-347. [CrossRef]
- Fountas KN, Kapsalaki EZ, Lee GP, Machinis TG, Grigorian AA, Robinson JS, Vergados I, Theodosiadis PG. Terson hemorrhage in patients suffering aneurysmal subarachnoid hemorrhage: predisposing factors and prognostic significance. J Neurosurg. 2008 Sep;109(3):439-44. [CrossRef]
- Hassan A, Lanzino G, Wijdicks EF, Rabinstein AA, Flemming KD. Terson’s syndrome. Neurocrit Care. 2011 Dec;15(3):554-8.
- Jing XB, Sun LQ. Terson syndrome with no cerebral hemorrhage: A case report. Exp Ther Med. 2014 Jan;7(1):251-253. [CrossRef]
- Leblanc, R. The minor leak preceding subarachnoid hemorrhage. J Neurosurg. 1987 Jan;66(1):35-9. [CrossRef]
- Lustbader JM, Miller NR. Painless, pupil-sparing but otherwise complete oculomotor nerve paresis caused by basilar artery aneurysm. Case report. Arch Ophthalmol. 1988 May;106(5):583-4. [CrossRef]
- Moraru A, Mihailovici R, Costin D, Brănişteanu D. Terson’s Syndrome - case report. Rom J Ophthalmol. 2017 Jan-Mar;61(1):44-48. [CrossRef]
- Murthy S, Salas D, Hirekataur S, Ram R. Terson’s syndrome presenting as an ophthalmic emergency. Acta Ophthalmol Scand. 2002 Dec;80(6):665-6. [CrossRef]
- Subbiah S, Wilson S, Best R. An unusual presentation of Terson’s syndrome. Eye (Lond). 2007 Jun;21(6):855-6.
- Sung W, Arnaldo B, Sergio C, Juliana S, Michel F. Terson’s syndrome as a prognostic factor for mortality of spontaneous subarachnoid haemorrhage. Acta Ophthalmol. 2011 Sep;89(6):544-7. [CrossRef]
- Woodruff MM, Edlow JA. Evaluation of third nerve palsy in the emergency department. J Emerg Med. 2008 Oct;35(3):239-46. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).