Submitted:
29 May 2024
Posted:
30 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
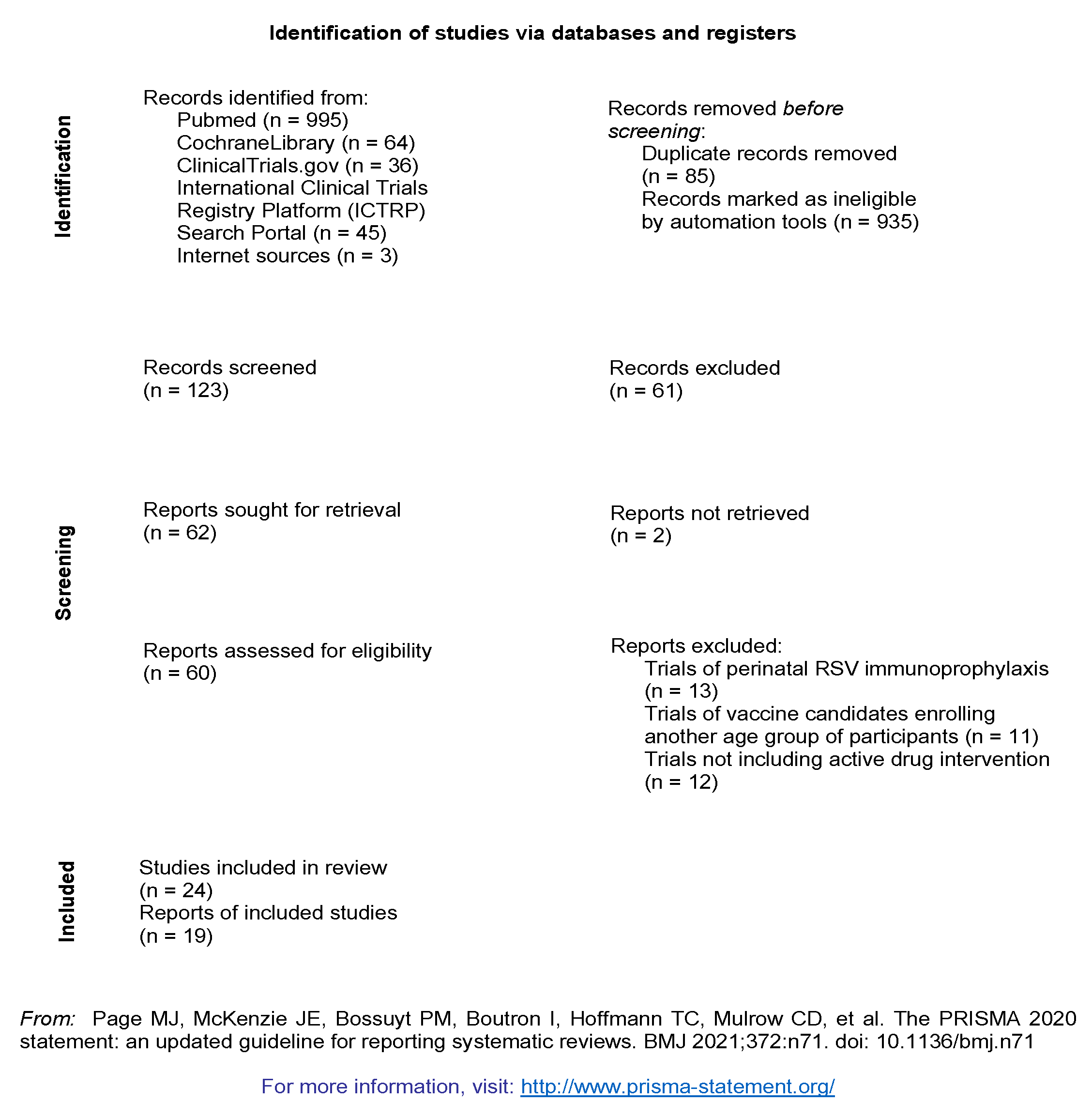
2. Materials and Methods
3. Results
3.1. Abrysvo
3.2. RSV MAT
3.3. ResVax
3.4. mRNA-1345
3.5. V-306
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Newborn Infections Available online: https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/newborn-health/newborn-infections.
- Hultquist, J.; Rios-Guzman, E.; Simons, L.; Dean, T.; Agnes, F.; Pawlowski, A.; Alisoltanidehkordi, A.; Nam, H.; Ison, M.; Ozer, E.; et al. Altered RSV Epidemiology and Genetic Diversity Following the COVID-19 Pandemic. Res. Sq. 2023. [Google Scholar] [CrossRef] [PubMed]
- RSV Surveillance & Research Available online: https://www.cdc.gov/rsv/research/index.html.
- Johannesen, C.K.; van Wijhe, M.; Tong, S.; Fernández, L. V; Heikkinen, T.; van Boven, M.; Wang, X.; Bøås, H.; Li, Y.; Campbell, H.; et al. Age-Specific Estimates of Respiratory Syncytial Virus-Associated Hospitalizations in 6 European Countries: A Time Series Analysis. J. Infect. Dis. 2022, 226, S29–S37. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; McAllister, D.A.; O’Brien, K.L.; Simoes, E.A.F.; Madhi, S.A.; Gessner, B.D.; Polack, F.P.; Balsells, E.; Acacio, S.; Aguayo, C.; et al. Global, Regional, and National Disease Burden Estimates of Acute Lower Respiratory Infections Due to Respiratory Syncytial Virus in Young Children in 2015: A Systematic Review and Modelling Study. Lancet 2017, 390, 946–958. [Google Scholar] [CrossRef] [PubMed]
- Pichler, K.; Assadian, O.; Berger, A. Viral Respiratory Infections in the Neonatal Intensive Care Unit—A Review. Front. Microbiol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, T. Vaccinations in the Newborn. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 76, 66–82. [Google Scholar] [CrossRef]
- Kollmann, T.R.; Kampmann, B.; Mazmanian, S.K.; Marchant, A.; Levy, O. Protecting the Newborn and Young Infant from Infectious Diseases: Lessons from Immune Ontogeny. Immunity 2017, 46, 350–363. [Google Scholar] [CrossRef] [PubMed]
- Niewiesk, S. Maternal Antibodies: Clinical Significance, Mechanism of Interference with Immune Responses, and Possible Vaccination Strategies. Front. Immunol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Pregnancy & Vaccines Available online: https://www.cdc.gov/vaccines/parents/by-age/pregnancy.html.
- First RSV Vaccine to Protect Infants up to 6 Months of Age and Older Adults Available online: https://www.ema.europa.eu/en/news/first-rsv-vaccine-protect-infants-6-months-age-and-older-adults.
- FDA Approves First Vaccine for Pregnant Individuals to Prevent RSV in Infants Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-vaccine-pregnant-individuals-prevent-rsv-infant.
- Walsh, E.E.; Falsey, A.R.; Scott, D.A.; Gurtman, A.; Zareba, A.M.; Jansen, K.U.; Gruber, W.C.; Dormitzer, P.R.; Swanson, K.A.; Radley, D.; et al. A Randomized Phase 1/2 Study of a Respiratory Syncytial Virus Prefusion F Vaccine. J. Infect. Dis. 2022, 225, 1357–1366. [Google Scholar] [CrossRef]
- Falsey, A.R.; Walsh, E.E.; Scott, D.A.; Gurtman, A.; Zareba, A.; Jansen, K.U.; Gruber, W.C.; Dormitzer, P.R.; Swanson, K.A.; Jiang, Q.; et al. Phase 1/2 Randomized Study of the Immunogenicity, Safety, and Tolerability of a Respiratory Syncytial Virus Prefusion F Vaccine in Adults With Concomitant Inactivated Influenza Vaccine. J. Infect. Dis. 2022, 225, 2056–2066. [Google Scholar] [CrossRef]
- Peterson, J.T.; Zareba, A.M.; Fitz-Patrick, D.; Essink, B.J.; Scott, D.A.; Swanson, K.A.; Chelani, D.; Radley, D.; Cooper, D.; Jansen, K.U.; et al. Safety and Immunogenicity of a Respiratory Syncytial Virus Prefusion F Vaccine When Coadministered With a Tetanus, Diphtheria, and Acellular Pertussis Vaccine. J. Infect. Dis. 2022, 225, 2077–2086. [Google Scholar] [CrossRef]
- Simões, E.A.F.; Center, K.J.; Tita, A.T.N.; Swanson, K.A.; Radley, D.; Houghton, J.; McGrory, S.B.; Gomme, E.; Anderson, M.; Roberts, J.P.; et al. Prefusion F Protein–Based Respiratory Syncytial Virus Immunization in Pregnancy. N. Engl. J. Med. 2022, 386, 1615–1626. [Google Scholar] [CrossRef] [PubMed]
- Package Insert - ABRYSVO Available online: https://www.fda.gov/media/168889/download.
- Schmoele-Thoma, B.; Zareba, A.M.; Jiang, Q.; Maddur, M.S.; Danaf, R.; Mann, A.; Eze, K.; Fok-Seang, J.; Kabir, G.; Catchpole, A.; et al. Vaccine Efficacy in Adults in a Respiratory Syncytial Virus Challenge Study. N. Engl. J. Med. 2022, 386, 2377–2386. [Google Scholar] [CrossRef] [PubMed]
- Kampmann, B.; Madhi, S.A.; Munjal, I.; Simões, E.A.F.; Pahud, B.A.; Llapur, C.; Baker, J.; Pérez Marc, G.; Radley, D.; Shittu, E.; et al. Bivalent Prefusion F Vaccine in Pregnancy to Prevent RSV Illness in Infants. N. Engl. J. Med. 2023, 388, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Baker, J.; Aliabadi, N.; Munjal, I.; Jiang, Q.; Feng, Y.; Brock, L.G.; Cooper, D.; Anderson, A.S.; Swanson, K.A.; Gruber, W.C.; et al. Equivalent Immunogenicity across Three RSVpreF Vaccine Lots in Healthy Adults 18–49 Years of Age: Results of a Randomized Phase 3 Study. Vaccine 2024. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, T.F.; Johnson, C.; Grigat, C.; Apter, D.; Csonka, P.; Lindblad, N.; Nguyen, T.L.-A.; Gao, F.F.; Qian, H.; Tullio, A.N.; et al. Three Dose Levels of a Maternal Respiratory Syncytial Virus Vaccine Candidate Are Well Tolerated and Immunogenic in a Randomized Trial in Nonpregnant Women. J. Infect. Dis. 2022, 225, 2067–2076. [Google Scholar] [CrossRef] [PubMed]
- Bebia, Z.; Reyes, O.; Jeanfreau, R.; Kantele, A.; De Leon, R.G.; Sánchez, M.G.; Banooni, P.; Gardener, G.J.; Rasero, J.L.B.; Pardilla, M.B.E.; et al. Safety and Immunogenicity of an Investigational Respiratory Syncytial Virus Vaccine (RSVPreF3) in Mothers and Their Infants: A Phase 2 Randomized Trial. J. Infect. Dis. 2023, 228, 299–310. [Google Scholar] [CrossRef]
- Hermida, N.; Ferguson, M.; Leroux-Roels, I.; Pagnussat, S.; Yaplee, D.; Hua, N.; van den Steen, P.; Anspach, B.; Dieussaert, I.; Kim, J.H. Safety and Immunogenicity of Respiratory Syncytial Virus Prefusion Maternal Vaccine Coadministered With Diphtheria-Tetanus-Pertussis Vaccine: A Phase 2 Study. J. Infect. Dis. 2023. [Google Scholar] [CrossRef] [PubMed]
- Glenn, G.M.; Smith, G.; Fries, L.; Raghunandan, R.; Lu, H.; Zhou, B.; Thomas, D.N.; Hickman, S.P.; Kpamegan, E.; Boddapati, S.; et al. Safety and Immunogenicity of a Sf9 Insect Cell-Derived Respiratory Syncytial Virus Fusion Protein Nanoparticle Vaccine. Vaccine 2013, 31, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Glenn, G.M.; Fries, L.F.; Thomas, D.N.; Smith, G.; Kpamegan, E.; Lu, H.; Flyer, D.; Jani, D.; Hickman, S.P.; Piedra, P.A. A Randomized, Blinded, Controlled, Dose-Ranging Study of a Respiratory Syncytial Virus Recombinant Fusion (F) Nanoparticle Vaccine in Healthy Women of Childbearing Age. J. Infect. Dis. 2016, 213, 411–422. [Google Scholar] [CrossRef] [PubMed]
- August, A.; Glenn, G.M.; Kpamegan, E.; Hickman, S.P.; Jani, D.; Lu, H.; Thomas, D.N.; Wen, J.; Piedra, P.A.; Fries, L.F. A Phase 2 Randomized, Observer-Blind, Placebo-Controlled, Dose-Ranging Trial of Aluminum-Adjuvanted Respiratory Syncytial Virus F Particle Vaccine Formulations in Healthy Women of Childbearing Age. Vaccine 2017, 35, 3749–3759. [Google Scholar] [CrossRef]
- Muňoz, F.M.; Swamy, G.K.; Hickman, S.P.; Agrawal, S.; Piedra, P.A.; Glenn, G.M.; Patel, N.; August, A.M.; Cho, I.; Fries, L. Safety and Immunogenicity of a Respiratory Syncytial Virus Fusion (F) Protein Nanoparticle Vaccine in Healthy Third-Trimester Pregnant Women and Their Infants. J. Infect. Dis. 2019, 220, 1802–1815. [Google Scholar] [CrossRef] [PubMed]
- Shaw, C.A.; Essink, B.; Harper, C.; Mithani, R.; Kapoor, A.; Dhar, R.; Wilson, L.; Guo, R.; Panozzo, C.A.; Wilson, E.; et al. Safety and Immunogenicity of an MRNA-Based RSV Vaccine Including a 12-Month Booster in a Phase 1 Clinical Trial in Healthy Older Adults. J. Infect. Dis. 2024. [Google Scholar] [CrossRef] [PubMed]
- Dieussaert, I.; Hyung Kim, J.; Luik, S.; Seidl, C.; Pu, W.; Stegmann, J.-U.; Swamy, G.K.; Webster, P.; Dormitzer, P.R. RSV Prefusion F Protein–Based Maternal Vaccine — Preterm Birth and Other Outcomes. N. Engl. J. Med. 2024, 390, 1009–1021. [Google Scholar] [CrossRef] [PubMed]
- Madhi, S.A.; Polack, F.P.; Piedra, P.A.; Munoz, F.M.; Trenholme, A.A.; Simões, E.A.F.; Swamy, G.K.; Agrawal, S.; Ahmed, K.; August, A.; et al. Respiratory Syncytial Virus Vaccination during Pregnancy and Effects in Infants. N. Engl. J. Med. 2020, 383, 426–439. [Google Scholar] [CrossRef]
- Leroux-Roels, I.; Bruhwyler, J.; Stergiou, L.; Sumeray, M.; Joye, J.; Maes, C.; Lambert, P.-H.; Leroux-Roels, G. Double-Blind, Placebo-Controlled, Dose-Escalating Study Evaluating the Safety and Immunogenicity of an Epitope-Specific Chemically Defined Nanoparticle RSV Vaccine. Vaccines 2023, 11, 367. [Google Scholar] [CrossRef]
- Walsh, E.E.; Falsey, A.R.; Zareba, A.M.; Jiang, Q.; Gurtman, A.; Radley, D.; Gomme, E.; Cooper, D.; Jansen, K.U.; Gruber, W.C.; et al. Respiratory Syncytial Virus Prefusion F Vaccination: Antibody Persistence and Revaccination. J. Infect. Dis. 2024. [Google Scholar] [CrossRef] [PubMed]
- Pipeline—Creating Tomorrow’s Vaccines Today Available online: https://www.novavax.com/science-technology/vaccine-pipeline.
- Mohr, E.; Siegrist, C.-A. Vaccination in Early Life: Standing up to the Challenges. Curr. Opin. Immunol. 2016, 41, 1–8. [Google Scholar] [CrossRef]
- Cuenca, A.G.; Wynn, J.L.; Moldawer, L.L.; Levy, O. Role of Innate Immunity in Neonatal Infection. Am. J. Perinatol. 2013, 30, 105–112. [Google Scholar] [CrossRef] [PubMed]
- 36. Yu, J.C.; Khodadadi, H.; Malik, A.; Davidson, B.; Salles, É. da S.L.; Bhatia, J.; Hale, V.L.; Baban, B. Innate Immunity of Neonates and Infants. Front. Immunol. 2018, 9. [CrossRef]
- Basha, S.; Surendran, N.; Pichichero, M. Immune Responses in Neonates. Expert Rev. Clin. Immunol. 2014, 10, 1171–1184. [Google Scholar] [CrossRef]
- Sedney, C.J.; Harvill, E.T. The Neonatal Immune System and Respiratory Pathogens. Microorganisms 2023, 11, 1597. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.R.; Jenkins, B.J.; Cronin, J.G.; Jones, N.; Thornton, C.A. A Role for Metabolism in Determining Neonatal Immune Function. Pediatr. Allergy Immunol. 2021, 32, 1616–1628. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-C.; Lin, S.-J. Neonatal Natural Killer Cell Function: Relevance to Antiviral Immune Defense. Clin. Dev. Immunol. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Strauss-Albee, D.M.; Liang, E.C.; Ranganath, T.; Aziz, N.; Blish, C.A. The Newborn Human NK Cell Repertoire Is Phenotypically Formed but Functionally Reduced. Cytom. Part B Clin. Cytom. 2017, 92, 33–41. [Google Scholar] [CrossRef]
- Hassan, J.; Reen, D.J. Human Recent Thymic Emigrants–Identification, Expansion, And Survival Characteristics. J. Immunol. 2001, 167, 1970–1976. [Google Scholar] [CrossRef]
- Jørgensen, N.; Persson, G.; Hviid, T.V.F. The Tolerogenic Function of Regulatory T Cells in Pregnancy and Cancer. Front. Immunol. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Semmes, E.C.; Chen, J.L.; Goswami, R.; Burt, T.D.; Permar, S.R.; Fouda, G.G. Understanding Early-Life Adaptive Immunity to Guide Interventions for Pediatric Health. Front. Immunol. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Siegrist, C.-A.; Aspinall, R. B-Cell Responses to Vaccination at the Extremes of Age. Nat. Rev. Immunol. 2009, 9, 185–194. [Google Scholar] [CrossRef]
- Assessment Report Abrysvo Available online: https://www.ema.europa.eu/en/documents/assessment-report/abrysvo-epar-public-assessment-report_en.pdf.
- Wang, X.; Li, Y.; Shi, T.; Bont, L.J.; Chu, H.Y.; Zar, H.J.; Wahi-Singh, B.; Ma, Y.; Cong, B.; Sharland, E.; et al. Global Disease Burden of and Risk Factors for Acute Lower Respiratory Infections Caused by Respiratory Syncytial Virus in Preterm Infants and Young Children in 2019: A Systematic Review and Meta-Analysis of Aggregated and Individual Participant Data. Lancet 2024, 403, 1241–1253. [Google Scholar] [CrossRef]
- BLA APPROVAL-ABRYSVO Available online: https://www.fda.gov/media/171492/download?attachment.
- Kenmoe, S.; Chu, H.Y.; Dawood, F.S.; Milucky, J.; Kittikraisak, W.; Matthewson, H.; Kulkarni, D.; Suntarattiwong, P.; Frivold, C.; Mohanty, S.; et al. Burden of Respiratory Syncytial Virus–Associated Acute Respiratory Infections During Pregnancy. J. Infect. Dis. 2024, 229, S51–S60. [Google Scholar] [CrossRef]
- Röbl-Mathieu, M.; Kunstein, A.; Liese, J.; Mertens, T.; Wojcinski, M. Vaccination in Pregnancy. Dtsch. Arztebl. Int. 2021. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.M.; Fleming-Dutra, K.E.; Prill, M.M.; Roper, L.E.; Brooks, O.; Sánchez, P.J.; Kotton, C.N.; Mahon, B.E.; Meyer, S.; Long, S.S.; et al. Use of Nirsevimab for the Prevention of Respiratory Syncytial Virus Disease Among Infants and Young Children: Recommendations of the Advisory Committee on Immunization Practices — United States, 2023. MMWR. Morb. Mortal. Wkly. Rep. 2023, 72, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Fleming-Dutra, K.E.; Jones, J.M.; Roper, L.E.; Prill, M.M.; Ortega-Sanchez, I.R.; Moulia, D.L.; Wallace, M.; Godfrey, M.; Broder, K.R.; Tepper, N.K.; et al. Use of the Pfizer Respiratory Syncytial Virus Vaccine During Pregnancy for the Prevention of Respiratory Syncytial Virus–Associated Lower Respiratory Tract Disease in Infants: Recommendations of the Advisory Committee on Immunization Practices — United St. MMWR. Morb. Mortal. Wkly. Rep. 2023, 72, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, D.; Wilkins, N.; van Leeuwen, E.; Watson, C.H.; Crofts, J.; Flasche, S.; Jit, M.; Atkins, K.E. Protecting Infants against RSV Disease: An Impact and Cost-Effectiveness Comparison of Long-Acting Monoclonal Antibodies and Maternal Vaccination. Lancet Reg. Heal. - Eur. 2024, 38, 100829. [Google Scholar] [CrossRef] [PubMed]
- Arora, M.; Lakshmi, R. Vaccines - Safety in Pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 76, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Kong, K.L.; Krishnaswamy, S.; Giles, M.L. Maternal Vaccinations. Aust. J. Gen. Pract. 2020, 49, 630–635. [Google Scholar] [CrossRef]
- Dauby, N.; Gagneux-Brunon, A.; Martin, C.; Mussi-Pinhata, M.M.; Goetghebuer, T. Maternal Immunization in Women Living with HIV. AIDS 2024, 38, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, J.E.; Borghans, J.A.M.; Bont, L.J.; Drylewicz, J. Disagreement FDA and EMA on RSV Maternal Vaccination: Possible Consequence for Global Mortality. Pediatr. Infect. Dis. J. 2024, 43, e1–e2. [Google Scholar] [CrossRef]
- Baral, R.; Li, X.; Willem, L.; Antillon, M.; Vilajeliu, A.; Jit, M.; Beutels, P.; Pecenka, C. The Impact of Maternal RSV Vaccine to Protect Infants in Gavi-Supported Countries: Estimates from Two Models. Vaccine 2020, 38, 5139–5147. [Google Scholar] [CrossRef]
- Willemsen, J.E.; Borghans, J.A.M.; Bont, L.J.; Drylewicz, J. Maternal Vaccination against RSV Can Substantially Reduce Childhood Mortality in Low-Income and Middle-Income Countries: A Mathematical Modeling Study. Vaccine X 2023, 15, 100379. [Google Scholar] [CrossRef]
- Koltai, M.; Moyes, J.; Nyawanda, B.; Nyiro, J.; Munywoki, P.K.; Tempia, S.; Li, X.; Antillon, M.; Bilcke, J.; Flasche, S.; et al. Estimating the Cost-Effectiveness of Maternal Vaccination and Monoclonal Antibodies for Respiratory Syncytial Virus in Kenya and South Africa. BMC Med. 2023, 21, 120. [Google Scholar] [CrossRef] [PubMed]
| Vaccine | Registration number | Phase | Population | Results |
|---|---|---|---|---|
| Completed clinical trials | ||||
| Abrysvo (Pfizer) | NCT03529773 | I/II | adults including non-pregnant female participants | -Higher titers of neutralizing antibodies in female participants, supporting the principal of maternal vaccination, levels above baseline within a year -no differences in RSV responses after coadministration with influenza vaccine (reduces responsiveness to influenza vaccination) [13,14] |
| NCT04071158 | IIb | non-pregnant female participants | -non-inferiority coadministration trial with tetanus, diphtheria and acellular pertussis vaccine (Tdap) -non-inferiority of coadministration was proved for all the pathogens except for pertussis, supporting vaccination against multiple pathogens [15] |
|
| NCT04032093 | IIb | pregnant female participants (24th -36th gestational week) | -interim analysis: maternal neutralizing antibody production and adequate infant transmission -post-hoc analysis: adequate prevention of infantile disease[16] -5.3% of preterm births in the active group compared to 2.6% in the placebo group [17] |
|
| NCT04785612 | IIa | young adults including non-pregnant female participants | -RSV challenge study -effective against symptomatic disease after RSV exposure [18] |
|
| MATISSE NCT04424316 | III | pregnant female participants (24th -36th gestational week), low-risk pregnancy | -interim analysis -avoidance of RSV-severe lower respiratory tract disease in the first 3 months of life in 81.8% -efficacy rate for lower respiratory tract illness was not statistically significant (57.1%) -protection rate against severe disease within the first 6 months after birth exceeded 69% [19] -premature births were recorded at a rate of 5.7% for the vaccine recipients and 4.7% for the placebo recipients [17] |
|
| NCT05096208 | III | adults including female participants | -consistency and safety of three different vaccine lots [20] | |
| RSV MAT (GSK) | NCT03674177 | I | non-pregnant female participants | -positive data for further evaluation of the vaccine during pregnancy [21] |
| NCT04126213 | II | pregnant female participants (28th-33rd gestational week) | -pregnancy and peripartum abnormalities in similar rates between groups, more cases of hypertension and preeclampsia in the active group without exceeding the general pregnant population rates -elevated titers of antibodies for mothers and their infants [22] |
|
| NCT04138056 | II | non-pregnant female participants | -no interference in RSV-related outcomes after coadministration with Tdap and altered responses for the Tdap pathogens with no (diphtheria and tetanus) or unknown (pertussis) clinical significancy [23] | |
| NCT05045144 | III | non-pregnant female participants | -different vaccine lots and co-administration with influenza vaccine | |
| ResVax (Novavax) | NCT01290419 | I | young male and female participants | -positive results, no association with toxicity, increase of antibody titers -supported further evaluation [24] |
| NCT01704365 | II | non-pregnant female participants | -no serious safety concerns were raised -specific antibody immunity was triggered [25] |
|
| NCT01960686 | II | non-pregnant female participants | -the high antigen dose formulation achieved high titers of antibodies remaining until 3 months post-vaccination and proved safe [26] | |
| NCT02247726 | II | pregnant female participants (33rd – 35th gestational week) | -protection against severe disease for both mothers and their infants, with high antibody titers for the infants -no significant safety issues [27] |
|
| Currently ongoing clinical trials | ||||
| mRNA-1345 | NCT04528719 | I | young adults including female participants | -promising outcomes for further development as a maternal candidate with elevated antibody titers within a 6-month period [28] |
| NCT06143046 | II | pregnant female participants (28th – 36th gestational week) | - | |
| ABRYSVO | MORISOT NCT06325657 |
III | pregnant female participants living with HIV (24th – 36th gestational week) |
- |
| RSV MAT | NCT05705440 | IIIb | participants from all previous trials | -safety monitoring |
| Discontinued clinical trials | ||||
| RSV MAT | GRACE trial NCT04605159 |
III | pregnant female participants (24th – 34th gestational week) | -high protection rates against RSV lower respiratory tract disease -Safety signals: risk of preterm birth (6.8% in the active group and 4.9% in the placebo group) [29] -termination of the study |
| NCT04980391 | III | pregnant female participants (24th – 36th gestational week), high-risk pregnancy | -premature discontinuation based on the findings of the GRACE trial | |
| NCT05229068 | III | re-vaccination trial | -withdrawn, based on the findings of the GRACE trial | |
| NCT05169905 | III | non-pregnant female participants | -early termination of the trial |
|
| Trials that did not achieve the outcome | ||||
| ResVax | NCT02624947 | III | pregnant female participants (28th – 36th gestational age) | -similar rates of pregnancy and birth adverse events between groups with no safety signals -Vaccine efficacy did not meet the primary outcome for protection against RSV lower respiratory tract infection within 3 months of age (39.4%) -VE of 58.8% for disease manifesting with severe hypoxemia [30] |
| V-306 (Virometix) | NCT04519073 | I | non-pregnant female participants | -the expected induction of antibodies and immunity was not achieved [31] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





