1.1. Background of the Study
Education involves training the body and mind. University is a place where students receive their educational training, to develop their life skills and learn how to become more independent (Abdullah, 2017). To ensure that the standard requirements of university education are maintained, students are expected to undertake their educational activities with healthy minds and bodies in an environment devoid of chaos. Hence, university administrators developed healthcare services to meet students’ physical and mental health needs by way of university health clinics (Graf, 2015). Most university health services have extensive health infrastructures, for the provision of effective and efficient healthcare services to the students.
A school healthcare clinic is a healthful environment where nursing and other healthcare services are provided to students in different institutions of learning. Ideally, a school healthcare system offers averagely standardized counseling, and psychological and social services that promote healthy social and emotional development and remove barriers to students’ learning. It should be a part of the corporate social responsibility of the university education system both for developed and developing countries. Health services can provide an environment where the student feels safe and healthy to guarantee successful academic pursuits for the student. It should be an environment that consistently provides programs to raise the students’ sense of health and well-being. If the student is physically ill or emotionally depressed, the student’s academic activities will be affected negatively hence the need for available healthcare facility available for them within the study environment.
1.2. Literature Review
Researchers and health service administrators in the field of student health programs utilize a variety of assessment tools and national surveys to identify student health needs and health-related issues. The college and university environment needs to be conducive to safe and healthy learning opportunities. Education program planner at Florida Atlantic University claimed “College health services are pertinent to student success, and a college committed to student success is also committed to student health” (Floyd, 2003). Health issues are of concern because many students do not know how to deal with the stress of being homesick and living on their own, as well as the added stress of new classes and professors (Swinford, 2008). A path-breaking organizational theorist made the argument within the organizational or institutional cultures that there are diverse balances of influences which encourage or resist innovation. The influence that encourages and inhibits innovation is in the cultural environment/community of the institution (Hannan and Silver, 2000).
The best college health programs protect and advance the health of students in ways liberating to students’ minds. Effective college health programs are not and should never be purely clinical operations to avoid missing their primary mission (Swinford, 2012). Health programs should be placed at the heart of the institution’s mission of higher education because they are responsible for the advancement of student’s health. College health programs can strengthen and fortify the campus learning environment while supporting the development of the student cognitively, emotionally, behaviorally, and socially (Keeling, 2002). The federal government of Nigeria recently introduced the Tertiary Institutions’ Social Health Insurance Programme (TISHIP) as a means to cater for the healthcare needs of those not captured by the formal sector scheme (Anetohet al., 2017). The TISHIP is a social security system whereby the health care of students in tertiary institutions in Nigeria is paid for from funds pooled through compulsory contributions involving the students and the government. The programme promotes the health of students to create a conducive learning environment and uninterrupted academic activities due to poor health.
Shagaya (2015) Patient satisfaction is considered one of the desired outcomes of healthcare and it is directly related to the utilization of health services, it has emerged as an increasingly important parameter in the assessment of quality healthcare; hence, healthcare facility performance can be best assessed by measuring the level of patient’s satisfaction. It is measured over a wide range of health service dimensions, including availability, accessibility and convenience of services, technical competence of the providers, interpersonal skills and the physical environment where services are delivered. Prasad et al. (2013) assert that a hospital may be well organized, ideally located and well equipped but it will fail in its responsibility to provide quality care if patient satisfaction is not of a high calibre.
Moreover, changes in the healthcare industry have given healthcare providers the ongoing challenge of providing quality care to patients while maintaining cost-cutting effectiveness(Canel and Anderson, 2001). He maintained that patients feeling about the quality of care received at a clinic determine the future success or failure of the clinic. Healthcare providers must know patients' perceptions in other to help define and measure the quality of service which will create avenues to improve upon the current level of service. It therefore demands some form of sensitive advocacy and even a compulsive approach where necessary, in other to persuade universities that it is a necessary part of a student’s education processes.
Materials and Methods
The methodology adopted in this research contributed greatly to achieving the aim and objectives of the study. This chapter, however, focused on the study design, study area, study population, method of data collection and analysis of the collected data
2.1. The Study Design and Sample Size
The study was designed as a descriptive cross-sectional facilitated with a structured questionnaire administered among students of David Umahi Federal University of Health Sciences, Uburu. The students were drawn across the different faculties of the University. A desired sample size of fifty 50 students was randomly selected.
2.2. The Study Area
The study was carried out within the campus of David Umahi Federal University of Health Sciences, Uburu.
2.3. Instruments and Method of Data Collection
The researcher considered and used a structured questionnaire of five (5) point Likert scale as a veritable instrument for collecting the data. The instrument was made up of four (4) segments comprising the bio-demographic parameters, respondent’s knowledge, attitude and practice of the respondent’s utilization of the university health clinic for their routine healthcare service provisions. A convenience random sampling technique was used to recruit fifty 50 student participants who willingly accepted to participate in the study.
2.4. Method of Data Analysis
The data collected were analyzed in a table of descriptive statistics to determine the total number of respondents per question, the range, mean and median of each question gathered from respondents across the three cognate sections of the questionnaire.
Results
This study was based on fifty (50) questionnaires administered to students across different Faculties of David Umahi Federal University of Health Sciences, Uburu. The responses of these respondents to the topical questions administered are as shown in the various
Table 1,
Table 2,
Table 3 and
Table 4 representing sections A, B, C and D of the questionnaire.
-
A.
The Socio-Demographic Parameters of the Study
From the result of the socio-demographic parameters contained in
Table 1, it showed that fifty (50) student respondents specified their gender in this study. The analysis indicated that the female gender outnumbered their male counterparts by 54 and 46 per cent respectively. This explained not only that the female genders are more on campus but most importantly, shows their compliance level.
In terms of the spread of participants around the campus, virtually all the faculties were represented with Applied and Natural Sciences having 36% and followed by Health Science and Technology with 28%. It is also noteworthy that the bulk population of the study participants falls within the first year and second years 56 and 24 per cent respectively.
-
B.
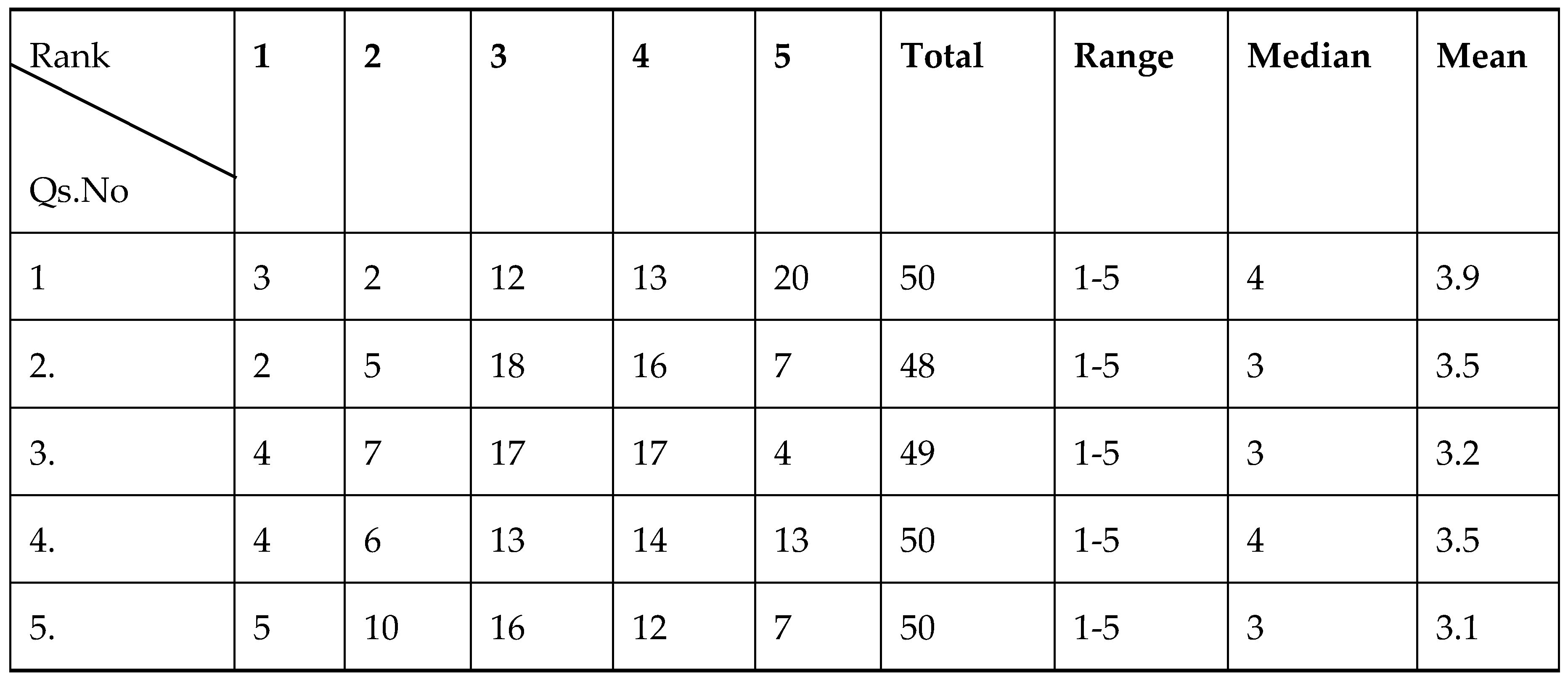
The Knowledge of DUFUHS Health Clinic
Table 2 illustrates the weighting frequencies of respondents on the various questions presented in this section to ascertain their level of knowledge of the DUFUHS healthcare clinic. It shows that the mean result for all questions 1 to 5 revolves around the fairly adequate point scale (i.e. between 3.10 – 3.9). This implies that students’ level of knowledge is not adequate to enable them to realize both the healthcare service at their disposal and what is required of them to access it. Accordingly, there is a need for more sensitization and the creation of awareness among DUFUHS students in other to draw their attention to utilising the DUFUHS clinic and improve upon their general health needs on campus at a minimally affordable rate.
-
C.
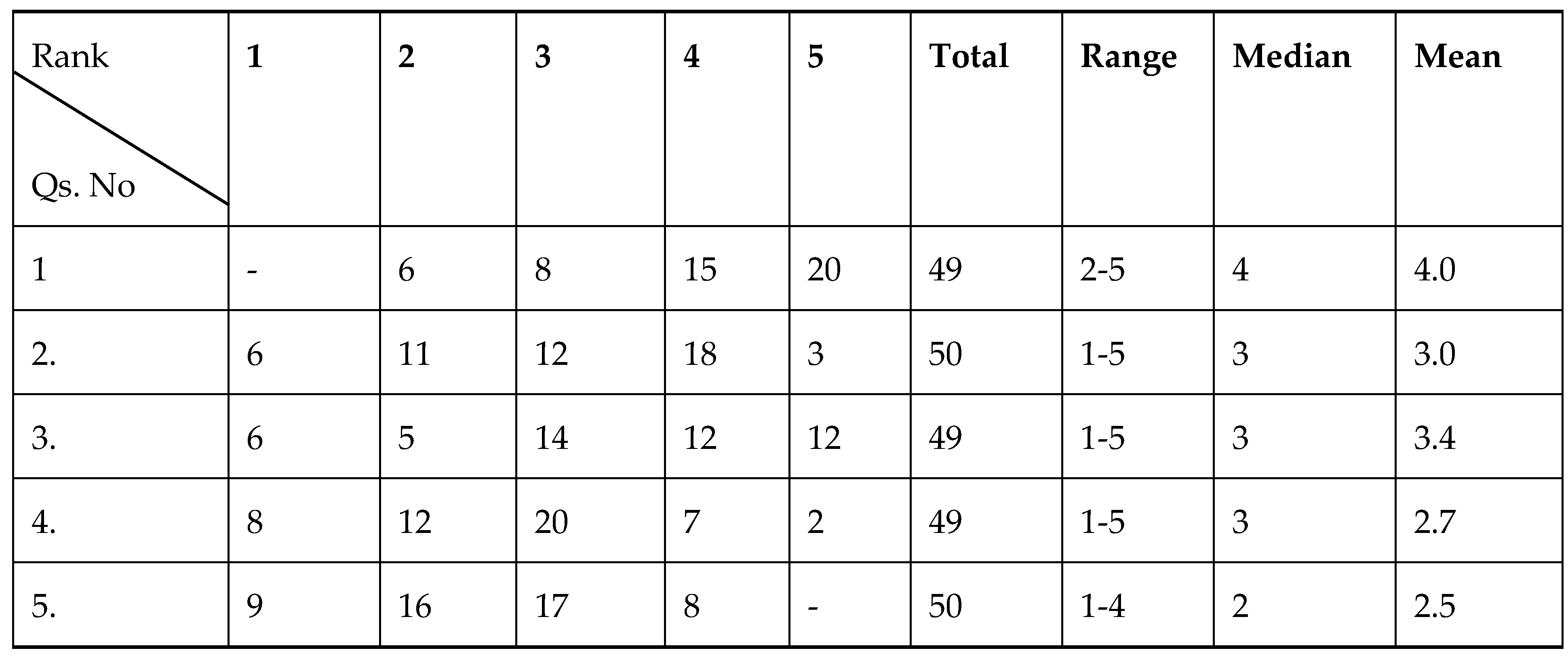
The Attitude of Students and DUFUHS Health Clinic
Table 3 displays the outcome of weighting frequencies for attitude questions posed to students in this study touching both the attitude of students and the center. The analysis indicates some variations in the mean results ranging from the least value 2.5 to the highest value 4. Accordingly, most of the issues raised require intervention to impact students' approach, as well as enhance staff-student cordial relationships for improved quality service delivery.
A more elaborate explanation of the implications of the mean values for all the questions as they affect the attitude of both students and the centre is presented in chapter four – the discussion section.
-
D.
The Practice of Students/Staff in DUFUHS Health Clinic
Table 4 is clearly shows the weighting frequencies of the results of practice of both students and staff of DUFUHS health clinic in accessing and discharging services respectively. The mean value for respondents ranges from 2.6 to 2.9 and 3.1, which indicates different levels of weaknesses in the points it represents. Given these poor mean results of the practice questions, a comprehensive intervention package will be required to address the lapses.
Further discussions on the outcome of analyzing data regarding the practice of both students and staff of DUFUHS health clinic in accessing/delivering healthcare service are as captured in chapter four of this study.
4.0. Discussions
4.1. Discussion of Results
The result of this study is intended to guide recommendations that will be geared towards reaching out and mobilizing students of DUFUHS to explore the services of the institution’s healthcare clinic.
Generally, given the overall result of this study, it is evident that DUFUHS students have poor knowledge of the existence of the university healthcare clinic in the first place, they lack good knowledge of the varieties of healthcare services accessible in the clinic and the proficiency in the clinic in terms of medical products availability and competence of her medical personnel. This is well expressed in the mean values of the knowledge questions which revolve around fairly adequate weighting (3.1 – 3.5). However, the level at which the respondents acknowledged and appreciated the dire need for healthcare clinic service in a university environment (represented with the mean value of 3.9 in the knowledge question 1), is instructive to the fact that it largely contributes to student’s academic well-being. In other to address this knowledge gap, interventions for routine awareness/enlightenment campaigns are required to get the students to know what lies in stock for them in the clinic.
In terms of attitudes, students’ responses concurred with the fact that a functional and affordable university health clinic is critical to salvaging their healthcare needs on campus. This is adduced in the resultant adequate mean value 4.0 of question 1 in the attitude section. Notwithstanding, the mean value weighting of staff attitude to students is 3.0 (fairly adequate). This is a weak point which may likely be part of why most students are not willing to seek the services of the clinic and those that once sought it are not willing to continue. Moreover, the study reveals that the rate at which students generally utilize the services of the DUFUHS health clinic is weighted at the mean value of 2.7 (inadequate/weak). Again, this is weak, poor and discouraging, a finding that portrays the clinic in a bad light with the threat of possibly going extinct with time.
A student’s willingness to access healthcare service or otherwise can be correlated with the attitude of health personnel as it has a way of affecting the quality of her service delivery. An account somewhat expressed in the mean value 2.5 (inadequate/weak) of attitude question number 5, is obnoxious and capable of turning off students’ healthcare desires. So, interventions aimed at addressing staff attitudes are required to inject a new order that is service-driven and student-centred. This would create impressions that will redirect students to resume DUFUHS health clinic services again and always.
From the result of students' practice, the mean value for most questions revolves around the “Inadequate” weighting scale (2.6, 2.8 and 2.8) indicating weakness in those issues they represent. This explains the fact that students less frequently access healthcare services from the clinic relatively due to perceived low efficacy of service, inadequate medical professionals and insufficient health facility deployment in the clinic. The cost and quality of care are also a determinant factor correlated to student affordability of the service, all these culminated in poor practices revealed in this study. Accordingly, this study infers that there is a need for interventions to address shortfalls in the practice of accessing healthcare services in DUFUHS clinics.
4.2. Conclusion
This study on assessing the knowledge, attitude and practice of accessing healthcare services in the DUFUHS health clinic among undergraduates of DUFUHS has been realized. The study revealed that operating a viable university healthcare clinic is a critical strategy for maintaining a healthy lifestyle for students and retaining most of the students admitted until graduation. A student-centred university healthcare system facilitates curbing the menace of school dropouts due to health-related challenges to the barest minimum. It serves as a central strand in achieving a robust educational system in both developing and developed economies.
4.4. Contributions to Knowledge
Findings from this study indicated that students are more disposed to embracing a comprehensive social security system incorporating programmers for their healthcare needs from the point of entry into the university until graduation. Introducing this scheme backed with enabling laws will help to derive a road map to align the DUFUHS healthcare clinic with international best practices. Moreover, there would be a rapid improvement in the quality of care in the clinic and turn, boost the confidence of both staff and students towards continued patronage of the centre.
4.5. Recommendations
The DUFUHS management/Senate should enact a law to define policy protocols for the university healthcare clinic to run a student-centred system, in other to boost the confidence of students in a healthy learning environment.
The DUFUHS management should embrace the Tertiary Institutions’ Social Health Insurance Programme (TISHIP) of the federal government with context-specific modifications. The TISHIP is a social security system (student-centred healthcare system) that pools funds from compulsory contributions involving students and the government.
University management should as a matter of duty create a routine monitoring and evaluation mechanism to help measure the level of service impact and rate of student patronage.
4.6. Policy Implication
Without students, there would not be the need for a university and students untreated health challenges pose a threat to their continued stay in school. The DUFUHS healthcare clinic systems seem not to be fair or user-friendly to her students traceable to lack of clearly defined policy direction. Policy on health is the life-wire that drives a viable healthcare system on well-established implementable protocols, hence the need for a governing law that gives students liberal access to healthcare once he/she enrol into the institution.
References
- Abdullah A. (2017). Utilisation of University Health Care Centre Services among University Students.International Journal of Health Sciences and Research.7(4); (Available at: www.ijhsr.org).
- Anetoh M. U.,Jibuaku H. C., Nduka S. O. and Uzodinma S. U. (2017).Knowledge and Implementation of Tertiary Institutions’ Social Health Insurance Programme (TISHIP) in Nigeria.The Pan African Medical Journal, 28(171).1-10. (Available: http://www.panafrican-med-journal.com/content/article/28/171/full/).
- Canel C. and Anderson E.A.F. (2001). An Analysis of Service Quality at a Student Health Care.International Journal of Health Care Quality Assurance.14(6), 260-267. http://www.emerald-library.com/ft.
- Floyd, D.L. (2003). Student health: challenges for community colleges. Community College Journal of Research and Practice, (27): pp.25-39.
- Graf L. (2015). "An Online Survey of the Healthcare Needs of Undergraduate Students at an Urban University". College of Science and Health Thesis and Dissertation.Paper 100.
- Hannan, A., & Silver, H. (2000).Innovating in higher education: Teaching, learning and institutional cultures. Philadelphia, PA: SRHE & Open University Press.
- Mccaig M. M. (2013). Importance and Effectiveness of Student Health Services at a South Texas University.
- National Center for Education Statistics, (NCES). Digest of education statistics tables and figures. Table 213.andFast Facts. Washington, DC: Available at: http://nces.ed.gov.
- Prasad, V.M (2013). Level of satisfaction in patients/attendants admitted with traumatic brain injury at an advanced ER/Casualty in a Tertiary Care Teaching Hospital. Journal of Hospital Administration, Vol. 2, No. 2; pp.89-96.
- Shagaya Y. J. (2015). Assessment of Student’s Satisfaction and Quality of Patient Care under the Nigerian Tertiary Institutions Social Health Insurance Programme. European Journal of Business and Management, 7(6).Pp.20-30.
- Swail, W. (2005).The ongoing retention challenge.Educational Policy Institute, (epi). Available at: http://www.educationalpolicy.org.
- Sweeny, S. (2005). Education update online. College of New Rochelle New York. http://www.cnr.edu.
- Tinto, V. (2012).Completing college: Rethinking Institutional Action. University of Chicago Press.
- Williams, T. (2002). Challenges in supporting student learning and success through studentservices. New Directions for Community Colleges.Spring, No.117, pp.67-76.
Table 1.
Result of the Socio-Demographic Parameters.
Table 1.
Result of the Socio-Demographic Parameters.
| Biodata: Gender |
Frequency |
Percentage |
| Male |
23 |
46% |
| Female |
27 |
54% |
| Total |
Total = 49 |
100% |
|
Age: Category |
Frequency |
Percentage |
| >25 |
34 |
75.6% |
| 25-34 |
10 |
22.2% |
| 35-44 |
1 |
2.2% |
| ≥45 |
- |
- |
| Total |
Total = 45 |
100% |
| Academic Parameter |
|
Percentage |
| Departments: |
CSC - 6
CHEMISTRY – 4
MED SURG - 7
MED LAB- 3
NURSING - 6
RADIOLOGY - 4
PHARMACY - 10
BIOMEDICAL ENG - 4
MBC - 6
Total = 50
|
12%
8%
14%
6%
12%
8%
20%
8%
12% |
| Faculty: |
APP. & NATURAL SCI -16
MEDICINE - 7
PHARMACY- 10
HEALTH SCIENCE-13
Total = 50
|
36%
14%
20%
28% |
| Level: |
100 - 28
200 - 12
300 - 10 |
56%
24%
20% |
| Total |
|
100% |
Table 2.
Result of Students Knowledge.
Table 2.
Result of Students Knowledge.
Table 3.
Result of Attitude.
Table 3.
Result of Attitude.
Table 4.
Result of Practice.
Table 4.
Result of Practice.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).