Diabetes mellitus has posed as a life-threatening disease that affected millions of people all over the world. The high blood sugar levels over an appreciable period result in a group of metabolic disorders or diabetes mellitus. Alongside this, diabetes is caused either because of failure of the pancreas function or lower responsibility of body cells to produce insulin [
1]. In addition, research literature witnesses that type-2 diabetes may lead to increased risk of viral infections such as SAR Covid-19. Mild symptoms such as frequent urination, increased thirst, and increased appetite may lead to acute complications like diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death [
2,
3,
4]. Also, it leads to severe pathogenesis such as neuropathy, cardiomyopathy, peripheral arterial disease, coronary artery disease, stroke, and nephropathy [
5,
6,
7]. Across the globe, 463 million people are estimated to be diabetic as of 2019 wherein 90% of cases belong to type-2 diabetes. Various types of antidiabetic medications are available for diabetes treatment. For type-2 diabetes, insulin is one of the treatment options and metformin is recommended as first-line treatment (taken orally) to reduce the mortality rate [
8]. Though metformin is a first-choice antidiabetic drug, chronic administration would cause hyperlactatemia due to drug accumulation consequently resulting in lactic acidosis [
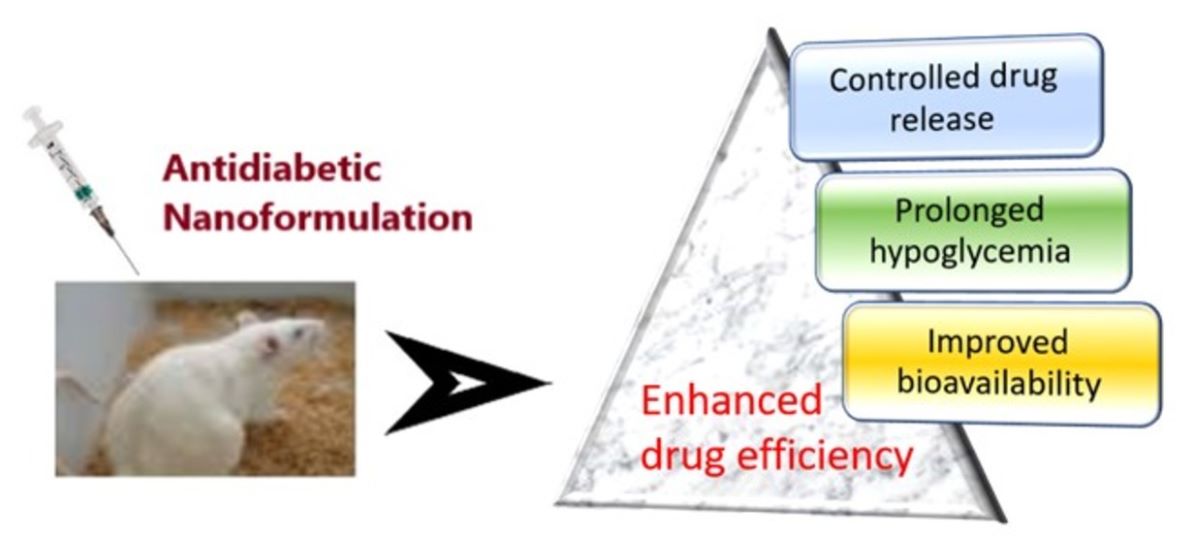
9]. A drastic change has taken place in the drug delivery system. The traditional drug delivery systems lack several useful drug properties. Since the nanoscale materials would exhibit special physical, chemical, and biological properties, they can be utilized in biomedical applications [
10]. Nanomedicine has evolved in the field of medicine that opened up several avenues in drug management and enhanced therapeutic efficacy. Nanosizing of the drug-delivering material and its constituents has a profound effect on their solubility, bioavailability, and consequently enhancing the efficacy [
11]. Alongside this, Nano-vehicles may diminish systemic adverse effects, enhance circulation times, and target precise organs [
12].
Studies indicate insulin can be delivered through nasal, rectal, buccal, ocular and oral routes employing nanotechnology and other advanced techniques [
13]. However, all these may not be equally efficient and safe for administration. Hence, a safe drug delivering vehicle is a very much essential. Besides, most of the diabetic patients require subcutaneous insulin injection that results in severe consequences such as pain, tenderness, microbial infections, local tissue necrosis, and nerve damage. Hence, oral drug delivery has become an alternative option [
14]. Having said, oral delivery of the antidiabetic drug/insulin is limited by many factors such as poor stability, low bioavailability, and short
in vivo half-lives, rapid enzymatic degradation, low permeability across intestinal epithelium, and absence of lipophilicity [
15]. Besides, studies have demonstrated that long-term use of synthetic analogs of insulin could alter mitogenic properties resulting in a risk of carcinogenicity [
16]. Hence, most of the studies focus on investigation of novel insulin-delivery systems. Herein, various nanoformulation models concerning insulin delivery and antidiabetic properties are discussed. It is broadly classified upon the type of material utilized in nanoformulation. In brief, the pharmacology (
in vitro or/and
in vivo) of the reported nanoformulations are described.
1.1. Biomolecule/Natural Product-Based Nanoformulations
In this method, the biomolecules such as chitosan, alginate, protein, cyclodextrin, embelin etc. are generally employed in fabricating or coating the antidiabetic agent, and sometimes the biomolecule used may also be an antidiabetic agent that would enhance exert synergism. The biomolecules offer minimal side effects and enhance the bioavailability and solubility. The biomolecules are also found to be non-toxic for oral administration. The biomolecules may be of a wide range of nature such as protein, vitamin, carbohydrate, or some plant extracts, etc.
Although the chitosan-based NPs greatly improve the permeability
via paracellular pathway, the mucoadhesive property limits their access to the epithelial surface since the major fraction of NPs is retained in the mucous barrier [
17]. To address this, M. Liu
et al have prepared pHPMA coated TMC-based NPs and studied drug release properties [
18]. The prepared NPs (Size, 163.1 nM) are reported to be relatively electroneutral (-3.35 mV) but possessed hydrophilic and have shown 4.56-fold higher permeability through human mucous layer revealing mucous-inert nature of pHPMA-coated NPs. Also, significant increase of internalization of drugs by the cell is noticed upon coating of NPs with pHPMA suggesting the improved access of the NPs with the epithelial cells. Further, pHPMA coating enhanced the rate of transport of encapsulated insulin across the E12 cell monolayer to 1.5-fold compared to uncoated NPs. In the
in vivo evaluation in diabetic rats, pHPMA-coated NPs displayed most promising hypoglycemic effect with the maximum blood glucose decrease of 36% at 4h and relative bioavailability (FR% = 8.56) is found to be 2.8-fold greater for pHPMA-coated NPs than uncoated NPs. Toxicity studies indicate the prepared NPs have no significant toxic property on cell viability at 50-300 µg/mL concentration.
The chemically modified cyclodextrin-based nanoparticles are designed to enhance intestinal delivery of insulin by E. Presas
et al [
19]. As the chemically-modified cyclodextrins can improve the membrane permeability through the increased interaction with biological membranes, these in combination with insulin glulisine and other two components mDSPE PEG 2000 and dextran sulfate (ratio, 1:4:4:1 for best stability) are used in preparation of insulin glulisine nanoparticles (IG-NPs: size, 109 nM). The resulting IG-NPs exhibited low polydispersity index of 0.272 and zeta potential of -25 mV. Also, high association efficiency of 71.4% and an insulin loading capacity of 10.2% are observed. Additionally, in the proteolysis studies, the IG-NPs conferred higher protection to the entrapped insulin compared to free insulin. The
in vivo jejunal instillation studies in rats indicated systemic mediation of IG-NPs in insulin absorption and further the blood glucose levels are decreased (50% after 45 min) up to 4 h. Besides, relative bioavailability of instilled insulin is found to be noteworthy (FR% = 5.46%) compared to subcutaneous administration of insulin solution.
The nanoparticulate system prepared using insulin-loaded albumin-coated alginate/dextran sulfate NPs can be stable in gastrointestinal medium, prevent premature release of insulin, and increase insulin bioavailability [
20]. These findings inspired M. Lopes
et al to evaluate biodistribution of anti-hyperglycemic activity of biopolymer-based nanoparticles (IN-AL/ALG-NPs) [
21]. The prepared nanoparticles IN-AL/ALG-NPs have been tested for oral anti-hyperglycemic activity. After 2 h of treatment hypoglycemia is observed to be 45% of basal levels, further it is reduced to 69% (
P < 0.05) with 50 IU/kg IN-AL/ALG-NPs after 10h. Biodistribution of the IN-AL/ALG-NPs is analyzed in balb-mice revealing
99mTc-ALB-NPs can significantly enhance the interactions with the small intestine. This study also indicated that the albumin is not degraded totally in the stomach that contributes to protection of insulin as well as stabilization of the NPs in the intestinal fluid.
To improve the bioavailability of insulin, A. Verma
et al have designed Vitamin B12 functionalized layer by layer calcium phosphate nanoparticles [
22] considering fact that Vitamin B12 conjugation would enhance the absorption of NPs in epithelial cells [
23,
24]. Insulin-loaded nanoparticles (IN/VitB12/CS/CP-NPs, size: 212.6 nm) possessed a loading efficiency of 7.83%. In
in-vitro release profile, a sustained insulin release (9.9%) is noticed for IN/VitB12/CS/CP-NPs while burst release (41.7%) is observed in case of NPs lacking VitB12 encapsulation. Conservation of
α-helix and
β-helix of insulin in VitB12 encapsulated NPs in 1% trypsin environment reveals, insulin is protected from enzymatic degradation. Also, the cellular uptake of these NPs is 1.43-fold higher as compared to non-VitB12 NPs, while NPs demonstrated higher uptake in ileum after 4 h that is attributed to receptor mediated endocytosis. Treatment with IN/VitB12/CS/CP-NPs reduced the TEER value to 60.40% from 100%, and further improved insulin transport (14.17%). Alongside, oral administration of IN/VitB12/CS/CP-NPs maintained much-improved relative oral bioavailability of 6.26%. It is proved by maintaining sustained blood glucose levels (197.65 mg/dl) up to 12 h in diabetic rats. VitB12/CS/CP-NPs at the concentration of 100 mg/kg have not exerted any toxicity as there is significant difference in body weight and lack of toxic symptoms.
Carboxymethyl chitosan (CMCS) in the form of nanogels (CMCS-NGs) have demonstrated transient and reversible enhancement of paracellular permeability and improved absorption [
25]. Amongst several properties of nanogels, surface charge is the most prominent factor affecting function of mucoadhesion and permeation [
26]. J. Wang
et al have studied the influence of surface charge of chitosan-based nanogels on oral insulin delivery [
27]. The two kinds of nanogels [CMCS-NGs (+) & CMCS-NGs (-)] are prepared with almost similar size and shape but differ in the surface charges. Both the positive and negatively charged nanogels have demonstrated more or less similar insulin release properties. However, the rate of insulin release at acidic pH is found to be lower than that of neutral pH suggesting suppression of insulin release from nanogels in gastro but promotion in small intestine. Also, the nanogels are safe for oral administration as no influence of nanogels is observed on cytotoxicity. The
ex vivo intestinal permeation studies indicate that the apparent permeation coefficient (
Papp) of insulin in negatively charged nanogels is 1.7-fold higher compared to positively charged nanogels. When the insulin loaded nanogels are administered orally in diabetic rats, insulin: CMCS-NGs (-) have shown maximum decrease of blood glucose level of 4.6 mmol/L comparatively higher than insulin: CMCS-NGs (+) (7.7 mmol/L) at 4 h post-injection. The blood glucose level increased with time and attained the basal level at 11-13 h. These results infer that nanogels have exerted enhanced absorption and sustained insulin release. Especially, the negatively charged nanogel has accomplished efficient and prolonged management of glucose levels. This special property might be attributed to the improved adhesion and permeation of insulin: CMCS-NGs.
Lei
et al have achieved the design of a cell-penetrating peptide-mediated chitosan nanocarriers to improve intestinal insulin delivery [
28]. The cell penetrating peptide, SAR6EW, is combined with chitosan, and insulin resulting in SAR6EW/CS/insulin-NPs (Size: 150 nM). The prepared NPs have witnessed high insulin and encapsulation efficiency of 75.36% and 7.58% respectively. The i
n vitro insulin release study reveals SAR6EW/CS/insulin-NPs have slightly higher rate of release compared to CS/insulin-NPs and it is pH dependent wherein insulin release at acidic pH is lower than at neutral condition. Also, the SAR6EW/CS/insulin-NPs offered protection to insulin from enzyme degradation and it is found that 58.6% of insulin remained after 1 h compared to insulin alone (15%). Alongside, improved transport properties of insulin across the Caco-2 cell monolayer is noticed. The cell viability (70%) for SAR6EW/CS/insulin-NPs checked on Caco-2 cells indicates that they are significantly non-toxic and safe for oral administration.
Similarly, low molecular weight polymer (LMWP) is a non-toxic cell penetrating peptide employed to enhance protein permeability across the intestinal mucosal layer [
29]. The LMWP-insulin nanoparticles have been used to improve the permeability of the intestinal mucosal layer [
30]. Further, to improve insulin oral absorption, mucoadhesive nanoparticles loaded with LMWP-linked insulin conjugates (IN-LMWP-NPs, size: 253.8 nm, ζ-potential: 47.5 mV) are prepared [
31]. The IN-LMWP-NPs have encapsulation efficiency and drug-loading capacity of 49.3% and 8.2% respectively. The LMWP-NPs demonstrated enough protection to the insulin from enzymatic degradation. Also, cell internalization implies that the drug is permeated through the mucus layer which is significantly greater for IN-LMWP-NPs compared to native insulin, while ten-fold higher cellular uptake in the epithelia cells is demonstrated by the NPs. With an eight-fold higher
Papp value of 8.90 x 10
-6 cm/s compared to native insulin, IN-LMWP-NPs have elicited remarkable insulin transport rate. In the pharmacodynamics study, oral administration of IN-LMWP-NPs has shown approx. 50% decrease in blood glucose level after 3 h and it remained at the same level up to 9 h. Besides, the IN-LMWP-NPs are non-toxic to Caco-2 cells up to the concentration of 20 µM and are safe for oral administration.
G. Erel and his coworkers have achieved preparation of insulin-loaded chitosan nanoparticles encapsulated in microemulsion for oral insulin delivery [
32]. The microemulsions containing insulin-loaded chitosan-based NPs (IN-CS-NP-ME) in the different ratios of insulin, chitosan, and TPP have a wide range of sizes.
In vitro drug release study reveals, for the formulation (INS:CS = 5:5 and CS:TPP = 6:1), at pH 6.8 the release rate after 2 h is 51.4%, while after 3 h, it is 66.1% and found to better than other formulations. In the experiment of
in vivo hypoglycemic effects in rats, the above-mentioned formulation has reduced plasma glucose level to 68.7% after 3 h and it is reported to be 66.4% after 8 h. In addition, improved oral bioavailability and better absorption of insulin in the gastrointestinal tract are observed. On Caco-2 cells, the optimized formulation is reported to be non-toxic up to a concentration of 6µl/well. Other formulations have exerted comparatively inferior activities.
Concanavalin A belonging to the Lectin class of biomolecules has been reported by several studies for its ability to bind intestinal mucosa and enhance intestinal uptake of orally administered particles [
33,
34]. Hence, taking the advantage of it, R. Sharma
et al have engineered Con A-grafted PEGylated PLGA nano-bioconjugates (Con A-PEG/PLGA-IN NCs) [
35]. The optimized formulation of Con A-PEG/PLGA-IN NCs with the size ranging from 189 nm to 254.6 nm exhibited entrapment efficiency of 46.2%. A sustained insulin release (35.85%) has been shown by the Con A-PEG/PLGA-IN NCs as compared to plain PLGA NPs (44.38%) which is attributed to the hindrance for insulin release offered by Con A conjugation. Also, the Con A-PEG/PLGA-IN NCs demonstrated greatly enhanced cellular uptake of 90% in Caco-2 cells on 12 h post-incubation. The
in vivo quantification of plasma glucose indicates, administration of NPs exhibited delayed response (2-4 h) concerning reduction in blood glucose level which is attributed to enhanced uptake and improved mucoadhesive property.
Folic acid is most often used to target cell membranes and to promote nonocarrier endocytosis
via the folate receptor [
36]. In addition, conjugation of folic acid with macromolecules enhances cellular uptake and target ability [
37]. Considering these facts, B. Xu
et al have prepared poly(lactic-
co-glycolic acid) and chitosan nanocarriers (PLGA/FA-CS-NPs, size: 204.33 nm, ζ-potential: 34.2 mV) for improved oral insulin delivery [
38]. The loading efficiency and drug-load capacity of insulin loaded nanoparticles are found to be 41% and 6.83% respectively. The cytotoxic studies reveal appreciable cell viability of 90% or higher at a concentration of 1000 µg/mL after 24 h. The encapsulation has conferred protection to the insulin from enzymatic degradation wherein 60% of insulin remains in NPs after incubation of 1 h, while almost all free insulin is degraded at this incubation period. Alongside, efficient internalization of insulin-loaded NPs by HT-29 cells and improved cellular uptake are noticed. In the study of hypoglycemic effect, oral administration of insulin-loaded NPs exhibited prolonged hypoglycemic effect, which is not observed in case of free insulin. Also, the plasma insulin concentration is increased gradually in the first 8 h followed by gradual suppression. In case of oral bioavailability, compared to insulin solution (FR%: 0.51), IN- PLGA/FA-CS-NPs expressed much higher efficacy (FR%: 7.22).
A. Bhattacharya and his coworkers reported preparation of polyurethane-alginate/chitosan nanoparticles (PU-ALG/CS-NPs) for oral insulin delivery [
39]. ζ-potential and particle size of PU-ALG/CS-NPs are determined to be 38.5 mV and 90-110 nm. Whereas encapsulation efficiency of insulin loaded nanoparticles (IN/PU-ALG/CS-NPs) is found to be 94% for optimized formulation. Initially, only 15.77% of insulin release is observed at pH 1.2 up to 1 h. However, up to 50% of insulin is released at pH 6.8 till 10
th h. Further, sustained release is noticed till 20
th h and maximum insulin release observed is 98.32%. Alongside, PU-ALG/CS-NPs demonstrated excellent adhesion properties to the mucosal layer of the intestine. In the hypoglycemia study, IN/PU-ALG/CS-NPs reduced to 98 mg/dl a dose of 100 IU/kg at 10
th h and it was maintained for several hours, reaching basal level at 18 h. The oral administration of IN/PU-ALG/CS-NPs at a dose of 50 IU and 100 IU/kg body weight resulted in relative bioavailability of approx. 9.57% and 10.36% respectively. The prepared nanoparticles are found to be non-toxic in nephron-toxicity test and hepato-toxicity test.
1.2. Antidiabetic-Natured Biomolecule-Based Nanoformulations
Apart from insulin, certain naturally extracted molecules can perform the functions of insulin. A wide range of biomolecules such as glycyrrhizin, embelin, incretin, curcumin, crocetin etc. have been reported to possess antidiabetic properties. They have demonstrated significant hypoglycemia in diabetic rats, reduced lipid profile, triglycerides and total cholesterol. Research studies also proved that nanoformulation of these biomolecules have enticing antidiabetic effects. In addition, parameters such as enhanced oral bioavailability, sustained drug-release and low cytotoxicity are accomplished through appropriate nanoparticle model designs. Results of administration of nanoformulation of such antidiabetic biomolecules is superior to plane drug suspension. Hereafter, pharmacology of a few of the nanoformulated antidiabetic molecules are discussed.
The antidiabetic property of embelin has been documented by Naik
et al and found to be associated with the inhibition of intracellular proinflammatory mediators [
40,
41]. Inspired by the antidiabetic potency of embelin, M.S. Alam
et al have aimed to prepare niosomes formulation of embelin and study their antidiabetic effects [
42]. Entrapment efficiency is found to be maximum (85.20%) for the formulation with surfactant, cholesterol, and phospholipid in the ratio of 9:1:4. The embelin-loaded niosomes of this formulation rendered 85.09% drug release at 24 h. In the antidiabetic evaluation of embelin niosomes formulation, gradual decrease in the blood glucose level is noticed and maximum hypoglycemic effect (57.79% reduction in blood glucose level) is observed after 8 h of the treatment.
It is found that ACE2/Ang-(1-7) has positive effects in metabolic regulation. For instance, mice lacking ACE2 may develop weakened glucose homeostasis [
43]. The transgenic rats with chronically increased Ang-(1-7) displayed enhanced glucose uptake in addition to other favorable factors [
44]. Besides, chronic infusion of Ang-(1-7) has been reported to reduce hyperglycemia in a rat model of type 1 diabetes mellitus [
45]. Taken together these facts, S.H.S. Santos
et al have developed hydroxypropyl-
β-cyclodextrin-based Ang-(1-7) nanoformulation in a transgenic rat model of inducible insulin resistance and diabetes type-2 [
46]. Oral treatment of TetO rats with NPs at a dose of 30 µg/kg prevented the marked elevation in blood glucose levels and reversal of hyperglycemic state is observed at a dose of 100 µg/kg, while remarkable protection from diabetic kidney fibrosis is noticed that might be attributed to decreased glycemia. The Ang-(1-7) NPs are also capable of stimulating glucose uptake in neonatal cardiomyocytes. Furthermore, administration of Ang-(1-7) has elicited a positive effect on insulin signaling through reduction of Ser612 phosphorylation on IRS-1, while increasing Akt phosphorylation in adipose tissue.
Incretin hormone, Glucagon-like peptide-1 (GLP-1) has been reported to be used for type-2 diabetes mellitus treatment. However, the activity is hindered because of its degradation by dipeptidyl peptidase-4 enzyme [
47]. To counter the issue, N. Shrestha
et al have come up with GLP-1 and DPP4 inhibitor-based nanocomposites [
48]. Here, chitosan-modified porous silicon nanoparticles are coated with hydroxypropyl methylcellulose acetate succinate MF leading to H-CSUn NPs (Size: 171.9-223.1 nM). The entrapment efficiency of the prepared NPs is 68.5% and the NPs exhibited good adhesion efficiency with intestinal epithelia. In
in vivo antidiabetic study, the GLP-1 loaded H-CSUN NPs demonstrated hypoglycemic effect and the decrease in blood glucose level is 32%. Further, results of plasma insulin level implicate the plasma level is consistent with the plasma DPP4 levels wherein H-CSUn NPs exerted 2.2-fold higher DPP4 level compared to the control
The anti-hyperglycemic property of glycyrrhizin is reported by recent studies. Considering the antidiabetic activity of glycyrrhizin [
49,
50], R. Rani
et al have prepared glycyrrhizin-loaded nanoparticles (Size: 184.1 nM) as well as metformin-loaded nanoparticles (Size: 146.5 nM) and then evaluated antidiabetic properties in diabetic rats [
51]. In the antidiabetic study, administration of glycyrrhizin-loaded NPs and metformin-loaded NPs for 21 successive days resulted in significant reduction of blood glucose levels compared to diabetic control rats which is found to be dose-dependent. It is reported that only ¼th of nanoformulated glycyrrhizin and metformin is required to produce equivalent anti-hyperglycemic activity compared to pure glycyrrhizin or metformin. Alongside, glycyrrhizin and metformin nanoformulations (40 mg/kg) have demonstrated significant increase in body weight on day 21 compared to diabetic control rats. In this activity, severity of diabetes is reduced through decreased HbA1c levels by the glycyrrhizin nanoformulations. Further administration of these formulations for 21 days led to the reduction in TC, TG, LDL, and VLDL levels and increased HDL levels compared to the control group. Besides, 20 and 40 mg/kg doses of glycyrrhizin-loaded NPs containing 4.2 mg and 8.4 mg/kg respectively of glycyrrhizin produced anti-hyperglycemic and anti-hyperlipidemic activity equivalent to pure glycyrrhizin at 20 and 40 mg/kg respectively. Similar effects are also noticed in case of metformin-loaded nanoformulation implicating encapsulation of drug molecules in nanoparticles has improved bioavailability.
Antidiabetic compound thymoquinone [
52] extracted from
Nigella sativa L. is made use in the preparation of nanoparticles in view to anticipate enhanced antidiabetic properties by R. Rani
et a [
53]
l. In presence of gum rosin, thymoquinone-loaded gum rosin (TQ-GR-NCs) (Size: 70.21 nM) and metformin-loaded gum rosin (MF-GR-NCs) (Size: 116.3 nM) nanocapsules are synthesized. The TQ-GR-NCs and MF-GR-NCs witnessed sustained drug release of 14.23 and 23.30% respectively compared to pure thymoquinone (59.60%) and metformin (76.33%) at 24
th hour. In the antidiabetic evaluation on rats, TQ-GR-NCs and MF-GR-NCs have significantly increased body weight of diabetic rats from 14
th day to 21
st day of treatment. Comparatively TQ-GR-NCs (80 mg/kg) have exhibited greater effect than that of MF-GR-NCs, thymoquinone, or metformin alone at similar concentration. Alongside, the remarkable decrease in the blood glucose levels of 58.27 and 60.28% are observed for TQ-GR-NCs and MF-GR-NCs respectively on 21
st day at the concentration of 80 mg/kg. Compared to diabetic controlled rates, a significant decrease in plasma HDL level is exerted by TQ-GR-NCs, while its oral administration has led to depression in TC, TG, LDL, and VLDL levels and increased HDL levels. Further, TQ-GR-NCs rendered a noteworthy decrease in the HbA1c level in diabetic rats compared to thymoquinone alone at various concentrations.
A combinatorial effect of rutin and silymarin towards diabetes control in rats has been demonstrated by M. M. Al-Enazi
et al [
54]. R. Rani
et al have investigated the synergistic effect of glycyrrhizin-loaded nanoparticles and thymoquinone-loaded nanoparticles (GT-NPs) [
55]. The cell viability is found to be improved (80-90%) compared to corresponding pure drugs (75-85%). The GT-NPs have expressed superior activity towards many factors. For instance, the fasting blood glucose is reduced (p < 0.01, 5.627%) compared to diabetic control, while a remarkable reduction in the total cholesterol and triglycerides is evident and found to be 7.27% and 7.86% respectively. Alongside, a profound effect on concentration of lipoproteins is noticed on administration of GT-NPs. In general, the synergism is observed when the combined nanoformulation is administered compared to individual nanoformulations.
D. Chitkara
et al developed quercetin nanoformulation (QUE-NPs) for
in vivo evaluation in diabetic rats [
56]. With drug-loading and entrapment efficiency of 20% and 72.07% respectively, particle size of QUE-NPs is found to be 278.5 nm. The QUE-NPs retained radical scavenging activity (SC
50 = 10.03 µg/mL) and anti-superoxide formation activity (IC
50 = 10.63 µg/mL). The oral administration of QUE-NPs indicates irregular quercetin plasma levels wherein 2.4 µg/mL is reached within 15 min, then a steep decline to 700 ng/mL in 2 h and further increase to 900 ng/mL after 9 h. It is followed by a gradual decrease of quercetin level over a period of 6 days. Whereas, a rapid decline in the quercetin level within 24 h is noticed in case of oral administration of quercetin suspension. A significant reduction (
P < 0.05) in the blood glucose level has occurred on QUE-NPs treatment on day 7, 10, and 15. Besides, the activity of SOD and catalase has been reduced by the QUE-NPs that might be attributed to excessive generation of ROS.
Though the quercetin is reported to possess anti-hyperglycemic properties [
57], its use in biomedical applications is limited because of poor aqueous solubility and other factors. P. Mukhyopadhyay
et al have prepared nanoformulation of quercetin with succinylated chitosan and alginate aiming at its clinical efficiency in diabetic rats [
58]. The optimized quercetin-loaded succinyl chitosan nanoparticles (QUE-SCS/ALG NPs) have possessed particle size of 91.58 nm and ζ-potential in the range of -1983 mV to -35.55 mV. It is found that smallest particle sized NPs elicited highest quercetin encapsulation and loading efficiency of 90% and 59% respectively. Quercetin release from QUE-SCS/ALG NPs is found to be pH dependent wherein an average of 16-27% of quercetin is released at pH 1.2 after 2 h, while 88-95% of the drug is released at pH 7.4 inferring the drug release is favorable in basic conditions. In the
in vivo test on diabetic rats, orally administered QUE-SCS/ALG NPs at a dose of 100 mg/kg showed significant reduction in blood glucose level compared to free quercetin. However, blank NPs could not exhibit any hypoglycemic effect indicating encapsulation of quercetin is crucial for its antidiabetic activity. Further, QUE-SCS/ALG NPs are able to maintain glucose homeostasis. Besides, lowered hyperlipidemic properties and decreased liver enzymes such as ALT, AST, and ALP are observed with QUE-SCS/ALG NPs treatment. In the cytotoxic studies, the prepared NPs are reported to be non-toxic for oral administration.
A polyphenolic flavonoid, silymarin is a non-toxic antidiabetic agent [
59] but its efficacy is hindered by its poor bioavailability, excessive damage by gastric enzymes, rapid excretion etc. [
60]. To enhance the therapeutic efficacy, Y. M. El-Far and his coworkers have developed silymarin nanoformulation with pluronic polymer [
61]. Silymarin-loaded pluronic nanoparticles (SM-PR-NPs) with encapsulation efficiency of 87.3% demonstrated cumulative drug release of 95% at 36 h and then it is found to be constant. A significant reduction in the fasting blood glucose level in STZ-induced diabetic rats is evident in the first week (p < 0.001) as well as second weak (p < 0.0001) compared to native silymarin. Also, oral administration of NPs in diabetic rats has no effect on glucose intolerance. SM-PR-NPs displayed enhanced SOD activity and elevated GSH level implicating the potential antioxidant property of NPs and playing a prominent role in decreasing oxidative stress. The triglyceride and cholesterol levels are well regulated by the administration of SM-PR-NPs. Whereas improvement in body weights of SM-PR-NPs treated diabetic rats is noticed. Besides, it is reported that SM-PR-NPs can upregulate
insulin,
Pdx-1, and
Nkx6.1 gene expression.
A naturally occurring polyphenolic compound curcumin with antidiabetic property [
62] has been utilized by Devadasu
et al in the design of antidiabetic nanoformulation with poly(lactic-co-glycolic) acid that demonstrated reduced plasma triglycerides and total cholesterol levels in streptozotocin-induced diabetic rats [
63]. This fact is made use in the preparation of curcumin-loaded pluronic nanoparticles (CUR-PR-NPs, size: 333 nm) by Y. M. El-Far
et al [
64]. The aqueous solubility of curcumin is improved upon nanoformulation. The
in vitro studies indicate the entrapment efficiency is found to be 87.8-91.2%, while cumulative drug release at 37 °C and pH 7.4 is approximately 90% after 24 h and thereafter it kept constant. Curcumin nanoparticles exhibited significant reduction in blood glucose level compared to native curcumin at the end of the second week. Administration of these nanoparticles reduced the total cholesterol (65.9%, p < 0.0001) and triglyceride level compared to native curcumin (45.4%, p < 0.01) in diabetic rats. Evaluation of oxidative stress infers a remarkable decrease in pancreatic MDA levels (33%, p < 0.05) in CUR-PR-NPs treated diabetic rats, while CUR-PR-NPs administration restored (44.4%, p < 0.0001) the activity of the antioxidant enzyme SOD as compared to diabetic control. However, there is no significant difference in body weight of diabetic rats when treated with CUR-PR-NPs or native curcumin. Whereas CUR-PR-NPs treatment has shown upregulation of insulin and
Pdx-1 gene expression (p < 0.001) as compared to native curcumin.
The studies suggest that over production of pro-inflammatory cytokines and chemokines such as TNF-α, MCP-1 are responsible for diabetic-linked renal inflammation [
65]. X. Yang
et al has designed and optimized crocetin-loaded PLGA nanoparticles (CT-PLGA-NPs) against diabetic nephropathy through suppression of inflammatory factors [
66]. The CT-PLGA-NPs have exerted inhibitory effect on α-glucosidase, α-amylase, and DPPIV with IC
50 values of 65.45 µg/mL, 43.45 µg/mL, and 35.43 µg/mL respectively. The drug-loading and encapsulation efficiency are reported as 6.51% and 75.39% respectively. The
in vitro drug-release study reveals burst release in the first 4 h, then sustained drug-release is noticed with a maximum of 75% after 48 h. Further, administration of CT-PLGA-NPs resulted in positive impact on food and water intake, body weight gain. Alongside, dose dependent down-regulation of blood glucose level is noticed, while upregulation of plasma insulin (12.10 µU/mL) is witnessed at the end of the study. A significant reduction (P < 0.001) in the inflammatory cytokines and inflammatory parameters is observed on treatment with CT-PLGA-NPs as compared to control rats. A reduction in the GSH and MDA levels indicated enhanced antioxidant property.
A glucagon-like-peptide-1 (GLP-1) derived macromolecule liraglutide has gained interest as it can maintain normoglycemia and exerts negligible hypoglycemia [
67]. To improve orally deliverable properties, N. Senduran and his team developed nanoformulation of liraglutide [
68]. The blank PLGA NPs exhibited the particle size and ζ-potential as 225.8 nm and -18.1 mV respectively. The encapsulation efficiency and drug-loading capacity of liraglutide-loaded PLGA nanoparticles (LG-PLGA-NPs) are found to be 75% and 7% respectively. The
in vitro drug-release study indicates sustained and continuous liraglutide to a total of 84.75% and 96.61% at the end of 1
st and 2
nd days respectively. Administration of LG-PLGA-NPs significantly reduced fasting blood glucose (
P < 0.05) level at 5
th week. The LG-PLGA-NPs have failed to show significant difference in fructosamine, HbA1c, and plasma levels at a dose of 75 µg/kg BD. However positive effects are observed when the NPs dose is increased to 150 µg/kg BD. Similarly, the NPs could only exert a lowering effect on serum triglycerides and total cholesterol at a higher dose.
Stevioside, a noncaloric sweetener extracted from
Stevia rebaudiana, is an FDA approved nontoxic natural substance. It has been reported for its potent antidiabetic activity [
69]. However, it is not exploited extensively because of its poor intestinal absorption, less bioavailability and metabolic degradation [
70]. I. Barwal
et al have developed antidiabetic nanomedicine using stevioside and pluronic-F-68 copolymer [
71]. The stevioside-loaded NPs have an average size of 140 nm. The
in vitro release experiment reveals initial burst release followed by sustained release. Fifty percent of the drug is released in approx. 25 h and complete release is noticed in approx. 200 h. The initial burst release is attributed to loosely associated stevioside on the surface of PLA nanoparticles.
K. Shanmugapriya
et al have developed nano-emulsion of astaxanthin and α-tocopherol with к-Carrageenan for wound healing in diabetic mice [
72] considering antidiabetic potential of astaxanthin [
73]. Based on the method of emulsification, two types of nano-emulsions KC@SENE and KC@USNE are obtained. The droplets of KC@SENE and KC@USNE have size of 216.2 nm and 214.4 nm respectively. The nano-emulsions treatment showed significant improvement in the bodyweight, water consumption and food intake in mice. Alongside, an improved blood glucose level decline is noticed after nono-emulsion treatment compared to diabetic mice. In the
in vivo wound healing study, treatment with nano-emulsions led to increased wound closure by the 5
th day and scar formation is noticed after the 15th day. Histology studies indicated regenerative changes in skin wounds on 5
th, 10
th, and 15
th days of wound induction. In addition, there is an increased tensile strength of wound tissue attributed to abundant inflammatory cells, fibroblast formation, and collagen synthesis.
LXRs are potential targets for type 2 diabetes treatment [
74]. Accumulating evidence indicates taurine can inhibit LXR, and prevent renal injury and fibrosis in diabetic animals. R. Mitra
et al attempted to improve the efficacy of taurine through nanoformulation (TU-NPs). Administration of TU-NPs demonstrated a significant decline (≈250 mg/dl) in the serum glucose level compared to disease control (≈350 mg/dl). Also, approximately twofold increase in serum albumin and 1/3
rd reduction in urinary albumin is noticed. Accordingly, TU-NPs treatment resulted in a noteworthy reduction of serum creatinine and increase in the urinary creatinine level. A lowering of serum cholesterol and serum triglyceride levels are seen. Further, a significant rise of the antioxidant enzyme GSH is noticed. In addition, histopathology reports that TU-NPs are promising in reducing the effects such as severe degeneration of tubules, increased glomerular space, and dilation of tubules. These results implicate TU-NPs play a protective role in renal damage.
1.3. Lipid-Based Nanoformulations
Lipids are employed in the preparation of antidiabetic nanoformulations. The lipid-based nanoformulations often called liposome-based NPs are highly biocompatible as compared to polymers at cellular level and may improve the permeability because of their hydrophobic nature. The liposomes may possess favorable pharmacokinetics. Most often lipid-polymer nanoformulations have possessed preferable drug-delivery properties [
75].
Since addition of bile salts to lipid bilayer reduces the detrimental activity of physiological bile salts in gastrointestinal tract [
76], M. Niu
et al developed recombinant insulin (rhINS)-loaded liposomes containing bile salt sodium glycolate (SGC) to investigate hypoglycemic activity and oral bioavailability [
77]. The size of prepared nano-liposomes is found to be in the range of 70-358 nm. rhINS-loaded liposomes with particle size 358 nm showed the entrapment efficiency of 35.0% and insulin-loaded SGC-liposomes rendered a maximum blood glucose decrease of 63% at 10 h and it took 20 h to return to basal levels. Further, the hypoglycemic effects are found to be dose dependent. The oral bioavailability of liposomes is reported as 11.0%.
Some of the plant derived sterols (cholesterol analogs) such as
β-sitosterol or stigmasterol are associated with a special property of decreasing blood plasma cholesterol [
78]. In addition, ergosterol-containing liposomes have demonstrated enhanced oral bioavailability of insulin. Tempted by these facts, M. Cui
et al engineered a drug delivery system from liposomes-containing sterols to enhance oral absorption of rhINS [
79]. The prepared liposomes containing various sterols possess particle size and ζ-potential ranging from 140.3-182.1 nm and -36.6 to -68.0 mV respectively. All the sterol-loaded liposomes exhibited a certain degree of hypoglycemia. Oral administration of
β-sitosterol-containing liposomes exhibited only 80% decrease in blood glucose level that can be correlated with stability. Whereas, ergosterol-containing liposomes (1:6) demonstrated a decrease in blood glucose level of 60% from 4-8 h after oral administration. All the sterol-liposome nanoformulations displayed higher transport of insulin across Caco-2 monolayer compared to free insulin solution which is attributed to high affinity of liposomes with cell membrane. However, P
app of ergosterol-containing liposomes is found to be maximum (6.56 x 10
-7 cm/s). The sterol-liposome nanoformulations are determined to be nontoxic to Caco-2 cells up to concentration of 2.5 mM.
F. Yu
et al have developed PLGA-lipid-PEG nanoparticles for better oral delivery of insulin [
80]. The insulin-loaded NPs (IN-PLGA-lipid-PEG-NPs) exhibited a particle size and ζ-potential of 176 nm and -31.1 mV respectively. Alongside, a remarkable drug entrapment efficiency and ideal drug loading of 92.3% and 2.4% are noticed. The NPs showed increased cellular uptake and enhanced cell internalization and better cellular permeability. Also, oral administration of insulin-loaded NPs exerted prolonged hypoglycemic effect with initial hypoglycemia as compared to subcutaneous injection. The oral administration of NPs has demonstrated a gradual increase in plasma insulin level up to 6 h, followed by gradient decrease. Besides, the NPs exhibited a better oral bioavailability of 12.42% up on oral administration.
T. Karamanidou
et al have developed DMPG incorporated mucus permeating self-nanoemulsifying drug delivery systems [
81]. The insulin-loaded DMPG SNEDDS NPs (IN/DMPG-NPs) have exhibited the particle size and ζ-potential in the range of 29.8-44.2 nm and -0.06 to 6.22 mV respectively. Whereas the insulin loading and insulin efficiency are reported to be ranging from 0.27-113 wt% and 63.84-70.89% respectively. The NPs have demonstrated sustained release without the burst release. The enzyme degradation study reveals good results wherein about 79% of insulin remains intact after 3 h of incubation with trypsin and almost similar results are observed in presence of α-chymotrypsin indicating protection of insulin from intestinal enzymes. Further, the designed nanoformulation showed low toxicity and was found to be nontoxic up to 2 mg/mL.
As an organic extract of
L. leonurus possessing antidiabetic potency [
82,
83], it is employed in the preparation of lipid-based antidiabetic nanocarriers to enhance its absorption and stability by F. Odei-Addo [
84]. Majority of Nanolipid carriers (NLCs) prepared have the particle size of 400 nm and ζ-potential of -32.7 mV in water.
L. leonurus loaded NLCs at a concentration of 10µg/mL increased glucose uptake (18%) on Chang liver cells comparatively higher than non-formulated
L. leonurus. However, the glucose uptake is comparatively inferior to that of metformin (51%). Further, the NLCs showed a significant increase (P < 0.05) in insulin stimulation in the INS-1 cells (model for β-cells) and the effect is found to be dose dependent. The results suggest that
L. leonurus formulations may be investigated further to improve the pharmacology.
To enhance the pharmacology of naturally occurring antidiabetic agent andrographolide [
85], semi-purified extract from
A. paniculata is combined with phospholipids resulting in nano-phyto vesicular carrier systems [
86]. The optimized formulation has the particle size and ζ-potential of 395.5 nm and -32.3 mV respectively, while the entrapment efficiency is found to be 79%. At a dose of 25 mg/kg, remarkable effect is noticed in the body weight of diabetic rats on oral administration. Alongside, a sustained decrease in blood glucose level is observed wherein the BGL of 87.3 mg/dl is reported after 21 days (
P < 0.01). Besides, reduction in the LDL level (38.33 mg/dL) and enhancement in the HDL level (30.83 mg/dL) is evident on oral administration of nanoformulation as compared to diabetic control (LDL: 90.83 mg/dL, HDL: 16.50 mg/dL). Additionally, approx. twofold reduction (92.17 mg/dL) in total cholesterol is seen as compared to control rats (164.80 mg/dL).
To enhance the oral bioavailability of an antidiabetic drug gliclazide, P. Patel and his team designed gliclazide-loaded lipid-based SNEDDS nanoformulation (GCZ/L-SNEDDS-NGs) [
87]. The optimized size of droplet and ζ-potential are found to be 110.4 nm and -30.1 mV respectively; self-nanoemulsifying powder (SNEP) has increased particle size of 189.2 nm. The GCZ/L-SNEDDS-NGs demonstrated higher drug release (97.84%) within 30 min compared to plain drug dispersion (15.99%) which might be due to greater availability of dissolved gliclazide. Also, SNEP exhibited slightly reduced drug release rate (95.13%), whereas the pellet form showed further lower drug release (73.76%) within 30 min. Pharmacokinetics reveal higher
Cmax value (3639.7 ng/mL) for GCZ/L-SNEDDS-NGs compared to SNEP or pellet forms. Alongside, GCZ/L-SNEDDS-NGs displayed a twofold greater extent of absorption compared to plain drug suspension. Antidiabetic activity of GCZ/L-SNEDDS-NGs, SNEP, and pellets are almost similar but better than plain drugs. Comparatively, GCZ/L-SNEDDS-NGs rendered promising effect wherein the blood glucose level is maintained in the range of 73.57-104.43 mg/dl and at the end of 24 h, the BGL is found to be 74.45 mg/dl.
M. S. El-Ridy
et al have prepared niosomes of metformin hydrochloride (MET-NIs) and then evaluated for antidiabetic effects [
88]. The particle size and ζ-potential of prepared niosomes are in the range of 380-1250 nm and -3.2 to -53.7 mV respectively. The
in vitro release profile indicates biphasic release wherein 50% of drug is released up to 8 h in controlled manner followed by slow and sustained release up to 72 h in which a maximum of 75% metformin is released. The treatment with optimized MET-NIs reduced (more than twofold compared to control) blood glucose level of diabetic rats to 174.4 and 184.6 mg/dL at 7
th and 14
th day respectively. TGF-β1 factor responsible for wound healing process is decreased in diabetic condition. Treatment with MET-NIs expressed significant increase in serum levels of TGF-β1 by 77.7%, comparatively stronger activity to oral metformin treatment (50.4%) inferring a better wound healing.