1. Introduction
Surgery is the main treatment modality for papillary thyroid carcinoma (PTC). The extent of primary surgery depends on several clinical characteristics of the disease, such as tumor size, metastases, macroscopic extrathyroidal extension, as well as the presence of microscopic vascular invasion and the morphological subtype of PTC [
1].
When tumor size is < 4.0 cm and neither regional nor distant metastases are present, patient survival is independent of extent of the surgery (total thyroidectomy or hemithyroidectomy) [
2]. Most National Comprehensive Cancer Network (NCCN) Committee members recommend performing total thyroidectomy for thyroid cancer patients having the following clinical data: T3 or T4; cytologically verified N1; presence of M1; aggressive morphological subtype; history of significant exposure to radiation within the head and neck area; and family history of cancer. The authors of the guidelines advocate for unilateral hemithyroidectomy in the group of patients having a low recurrence risk as the final treatment modality for most patients with papillary thyroid carcinoma because of low mortality and recurrence rate as well as higher rate of complications related to thyroidectomy [
3].
In some cases, it is difficult to plan surgery extent that would comply with the ATA and NCCN guidelines because of the lack of data on the morphological subtype of PTC in the cytology report. Furthermore, the potentially aggressive PTC could have possibly be diagnosed early and did not have time to manifest itself as extrathyroidal extension and vascular invasion, while no regional lymph node involvement was detected because of microscopic size of the metastases. Total thyroidectomy with central lymph node dissection followed by radioactive iodine therapy would be preferred in this case [
4]. Furthermore, for some patients with PTC at the preoperative stage, cytology report specifies “follicular neoplasm” (Bethesda category IV) or “atypia of undetermined significance” (Bethesda category III) [
5,
6]. As a result, reoperation may be needed if hemithyroidectomy is chosen as the primary surgical treatment option. Molecular testing can be used to refine indications to surgical treatment in patients with vague cytological findings [
7]. Application of molecular research in patients preoperatively diagnosed with PTC for personalizing the treatment approach remains poorly investigated.
Somatic mutations currently are the best-studied molecular markers of PTC aggressiveness. It has long been observed that early genetic events of thyroid cancer progression (e.g., BRAF mutations) are frequently found in patients with both well-differentiated thyroid cancer and poorly differentiated or anaplastic thyroid cancer because they are involved in the initiation of tumor development. In contrast, late genetic events (e.g., TP53 gene mutations) are more common in tumors that gradually lose thyroid differentiation and are therefore associated with tumor progression and an unfavorable outcome [
8]. In patients with thyroid cancer, TERT promoter mutations are classified as a late event and are found in more aggressive thyroid cancers, being more common in patients with poorly differentiated or anaplastic cancer (up to ~70% of cases) than those with well-differentiated PTC and follicular thyroid carcinoma (FTC) (~10–20%). Moreover, TERT mutations have been recognized as an independent predictor of tumor recurrence, distant metastases, poor prognosis, and mortality in patients with well-differentiated PTC and FTC [
9]. As for other types of molecular markers (assessment of expression of miRNA and various genes involved in thyroid function), the feasibility of using them to predict the development of PTC has been studied by different researchers; however, none of the new markers has become widely recognized [
10,
11,
12].
In our previous studies, we investigated the diagnostic potential of several types of molecular markers: BRAF V600E mutation, relative expression of miRNA and protein-coding genes, as well as the mitochondrial to nuclear DNA ratio for preoperative detection of thyroid cancer. Some of the results of these studies have already been published [
13]. In this work, the preoperative prognostic potential of certain markers for PTC was investigated. We analyzed 34 molecular markers in cytology specimens collected by FNAB and assessed the correlation between them, as well as the clinical and morphological features of tumors and the risk of PTC recurrence.
2. Results
Table 1 summarizes the clinical characteristics of 108 patients with PTC enrolled in the study.
Among 108 patients with PTC, there were 86 (79.6%) females and 22 (20.4%) males. The median age at diagnosis was 47.5 (37–60.25) years (the youngest patient was 22 years old; the oldest one, 85 years old). No differences in sex ratio were observed in the groups being compared. The minimal and maximum tumor diameter was 0.6 cm and 8.0 cm, respectively. Tumor was multifocal in 61 (56.5%) cases; vascular invasion was observed in 58 (53.4%) cases. Twenty-five (23.1%) patients had macroscopic extrathyroidal extension. Metastatic spread to cervical lymph nodes was detected in 53 (49.1%) cases. In accordance with the 2015 ATA Risk Stratification System, 23 (21.3%) patients were categorized into the low-risk group; 60 (55.6%), into the intermediate risk group; and 25 (23.1%) patients, into the high-risk group.
Intergroup comparative analysis of association between clinical-pathological characteristics of PTC and BRAFV660E mutation was carried out (
Table 2).
The BRAF mutation was statistically significantly more frequent in the groups of patients with intermediate (80%, p = 0.03) and high (84%, р = 0.04) ATA recurrence risk compared to the low-risk group (56.5%).
The correlation between tumor size in patients with PTC and expression level of the miRNA and genes being studied was analyzed. With adjustment for multiple comparisons, statistically significant correlation level among 34 parameters was achieved only for the expression level of the TPO gene (p = 0.00045, Spearman’s rank coefficient -0.33). Correlation between tumor size and the TPO level was negative and relatively strong: the larger the tumor size, the lower the expression level of the thyroid peroxidase gene was. There was also a correlation with expression of the SLC26A7 gene (р = 0.005, Spearman’s rank coefficient -0.26) and mtDNA level (р = 0.006, Spearman’s rank coefficient 0.26). However, the required confidence level р < 0.0015 was not achieved for these markers.
The relative expression levels of 11 miRNAs, mtDNA level, and expression of 22 genes were compared. The results are summarized in
Table 3.
Comparison of expression of molecular markers revealed differences in all the clinical-morphological groups except for the group of patients having tumors characterized by vascular invasion; weak correlation was also detected in the case of multifocal nature of cancer. No statistical significance (p > 0.05) was observed for miRNA: -199b, -223, -451a, and -21. Among the studied genes, we found no correlation with clinical manifestations of PTC for the following markers: TSHR (the TSH receptor gene playing a pivotal role in controlling the metabolism of thyrocytes) and SLC26A7 (codes for iodine receptor), whose expression is significantly downregulated in patients with anaplastic thyroid cancer [
14]; CPQ (carboxypeptidase that plays a certain role in the release of thyroxine hormone from its precursor, thyroglobulin) and RXRG (retinoic acid receptor) whose expression was found to decrease in patients with follicular thyroid cancer [
15,
16]; SPATA18 (the key regulator of mitochondrial quality) playing a role in the development of oncocytic cell carcinoma of the thyroid [
17]; APOE (apolipoprotein, a protein involved in lipid transport between organelles through plasma and interstitial fluids); ASF1B (histone chaperone) and TIMP1 (metalloproteinase inhibitor acting as a growth factor) with reduction of the overall survival in patients with thyroid cancer [
18,
19]; AFAP1L2 (transcriptional activator) whose upregulated transcription is associated with thyrocyte apoptosis [
20]; ECM1 (extracellular matrix protein stimulating proliferation of endothelial cells and promoting angiogenesis), whose expression considered to be decreased in patients with advanced forms of PTC [
21]; and DIO1 (iodothyronine deiodinase, which is responsible for deiodination of T4 to T3 and T3 to T2), which is differently expressed in patients with follicular adenoma and thyroid carcinoma [
22].
Weak statistical correlation (0.0015< р <0.05) was observed for miRNA-31, -375, -551b, -148b, -125b, for mtDNA, and for the following genes:
the TPO (thyroid peroxidase) gene; the decline in its expression is associated with resistance to radioactive iodine therapy [
23]. We detected that TPO expression depends on tumor size, while being weakly associated with extrathyroidal invasion (p = 0.01) and the high/low recurrence risk (p = 0.02). Taking into account the fact that radioactive iodine-resistant tumors are more likely to be large-sized, it appears that thyroid peroxidase activity is its consequence rather than a cause;
the CITED1 gene, which is associated with the development of follicular cancer [
22]. Differences were observed for such parameters as cervical lymph nodes metastases (p = 0.01), extrathyroidal extension (p = 0.02), and high/low recurrence risk (p = 0.004);
the HMGA2 gene: expression of this gene is believed to be associated with lymphogenic metastasis and vascular invasion [
24]. According to our data, weak differences were observed for the groups of patients with/without metastases (p = 0.02), with/without extrathyroidal extension (p = 0.01), with/without vascular invasion (p = 0.05), and with moderate/high recurrence risk (p = 0.01);
the NIS (sodium/iodine symporter) gene, whose expression level is reduced in most thyroid carcinomas [
25]. Differences were observed for the groups of patients with low/high (p = 0.05) and moderate/high (р = 0.0049) recurrence risk.
the CLU gene (clusterin alpha chain, an extracellular chaperone preventing aggregation of non native proteins) whose upregulated expression is associated with better survival prognosis [
18]. Differences were observed in groups of patients with/without metastases (p = 0.005) and multifocal/unifocal cancer (р = 0.01);
the SERPINA1 (serine protease inhibitor) gene; its association with stage and the multifocal nature of thyroid cancer has been reported [
26]. Differences were observed for the groups of patients with/without metastases (р = 0.004);
the TFF3 gene; its downregulated expression was observed in patients with follicular thyroid cancer [
15]. Differences were detected in the groups with/without metastases (p = 0.02), with/without extrathyroidal extension (p = 0.002), with high/low (p = 0.01) and moderate/high risk (р=0.003); and
the TMPRSS4 (transmembrane serine protease) gene is characterized by increased expression in patients with PTC [
21]. Differences in groups of patients with/without metastases (p = 0.04), low/intermediate (p = 0.05) and low/high (p = 0.01) recurrence risk.
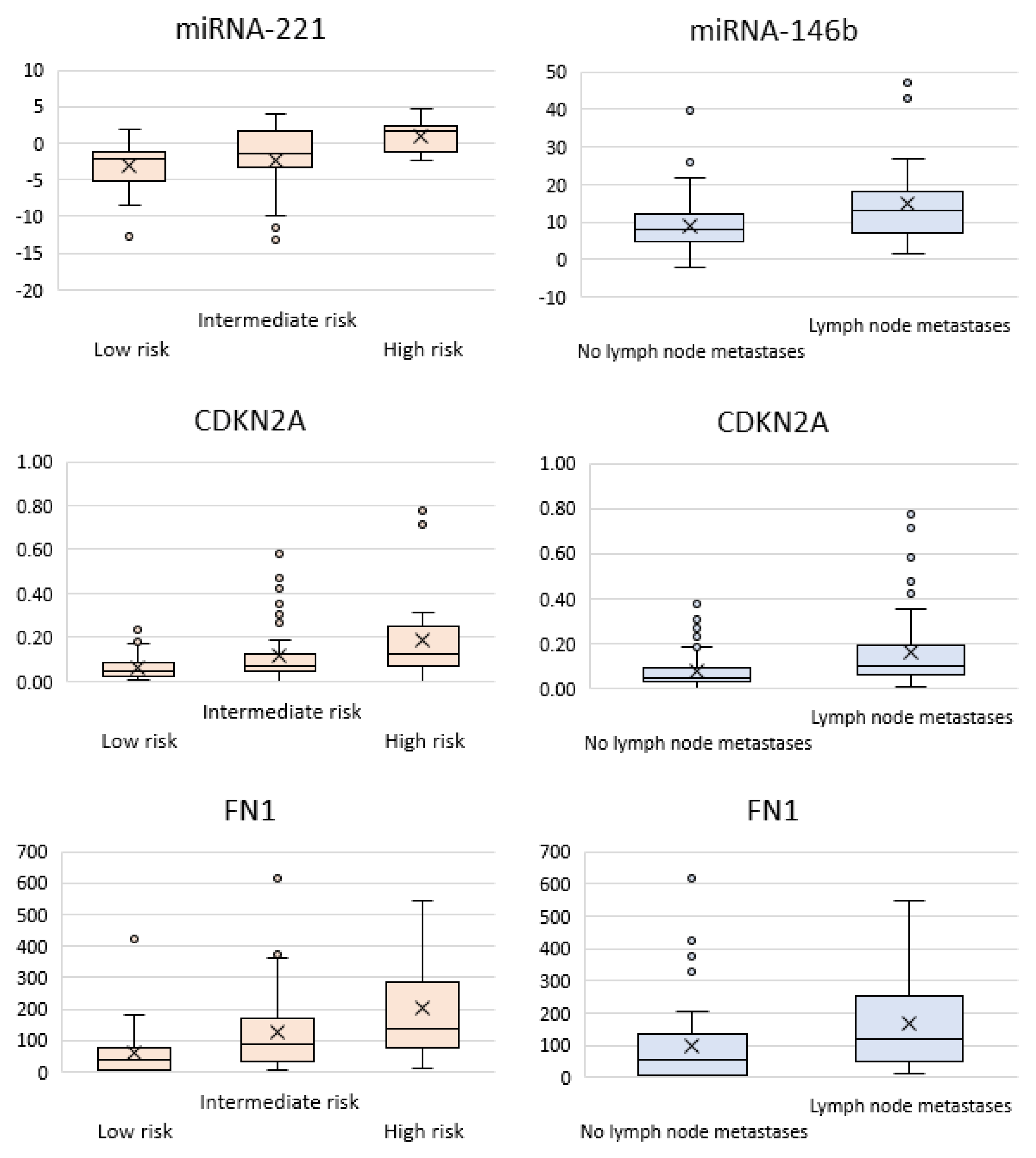
Statistically significant differences with adjustment for multiple comparisons (p < 0.0015) were obtained for four markers: miR-146b, miR-221, FN1, and CDKN2A (
Figure 1).
The miRNA-146b level was on average 1.7-fold higher in tumors with regional metastases to cervical lymph nodes than without them (p = 0.0003). The miRNA-221 level was 1.9-fold higher in patients with extrathyroidal extension (р = 0.00005), as well as 3.4-fold and twofold higher in the groups of patients with high and intermediate recurrence risk compared to the low-risk groups (р = 0.000013 and р = 0.001, respectively). Upregulated expression was observed for the FN1 (fibronectin, which is usually believed to be associated with the development of follicular cancer [
22]) gene in groups of patients having cervical lymph nodes metastases (1.7-fold higher; р = 0.0004) and with high and intermediate ATA recurrence risk (3.75-fold and 1.6-fold; р = 0.000013 and р = 0.001, respectively). Expression of the CDKN2A (cyclin-dependent kinase inhibitor 2A, which is associated with anaplastic thyroid cancer [
34]) gene was twice higher in patients with cervical lymph nodes metastases (p = 0.00014) and 3.3-fold higher in patients having a high recurrence risk than those having a low risk (р = 0.0012).
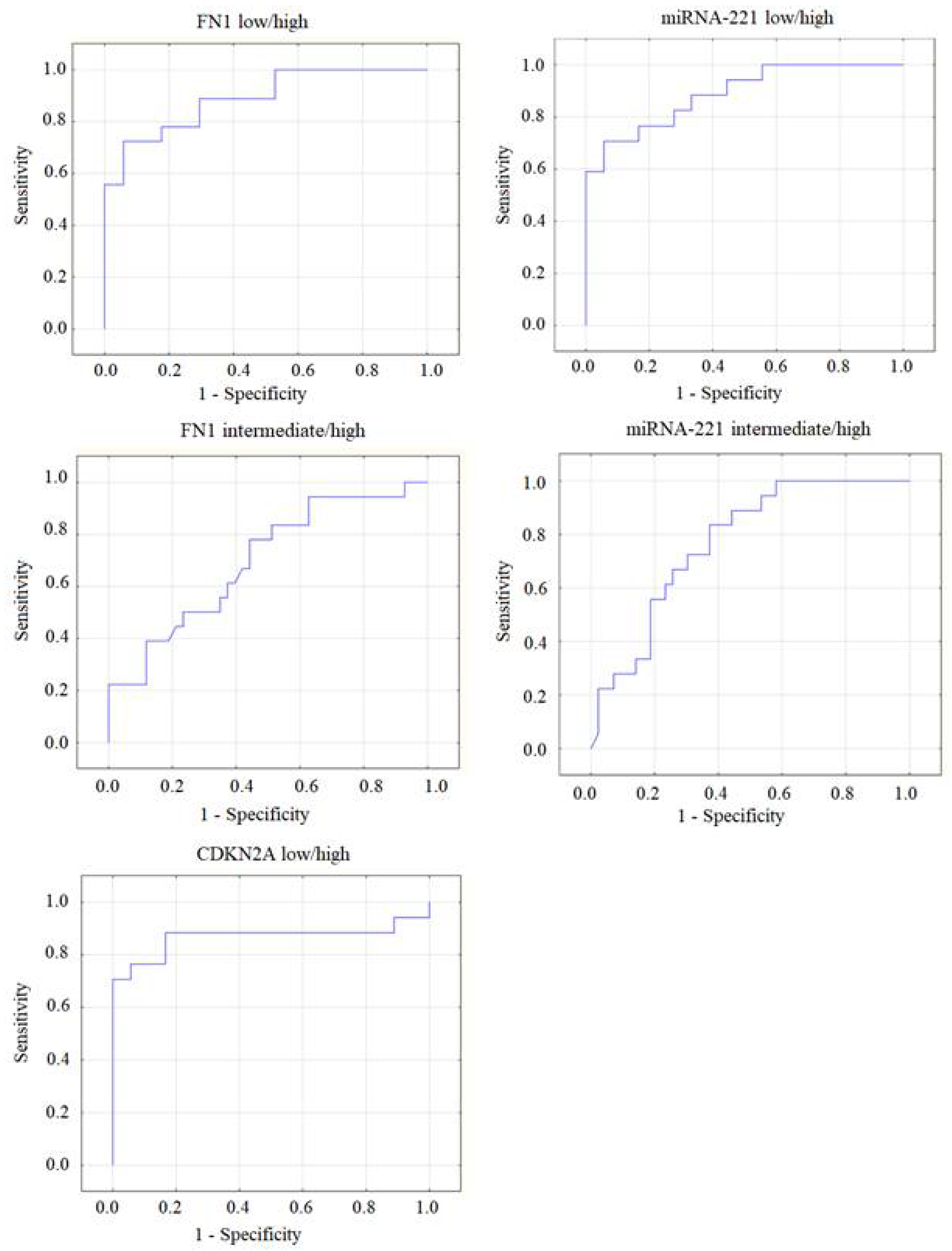
Hence, differences in recurrence risk were detected only for 3 out of the 34 studied molecular genetic factors: expression of miRNA-221, as well as the FN1 and CDKN2A genes. The areas under the ROC curves (AUC) were calculated for these markers (
Figure 2).
The highest ROC AUC values were obtained: for miRNA-221, between the low/high risk (AUC=0.88) and the intermediate/high risk (AUC=0.77) groups; for CDKN2A, the AUC between the low/high risk group was 0.87; for FN1, the AUC between the low/high risk group was 0.81 and between the intermediate/high risk group AUC = 0.69.
The calculated values of these markers gave grounds for categorizing a patient into the group of high recurrence risk according to ATA guidelines with a high sensitivity. For the CDKN2A gene, at a cut-off value of 0.044, sensitivity was 88.5% (95% CI: 69.8–97.5); specificity was 47.8% (95% CI: 26.8–69.4). For the FN1 gene, at a cut-off value of 8.5, sensitivity was 100% (95% CI: 86.7–100); specificity was 43.5% (95% CI: 23.2–65.5). The expression level of miRNA-221 > 0.47 has a 96.2% (95% CI: 80.4–99.9) prognostic sensitivity for high recurrence risk and specificity of 60.9% (95% CI: 38.5–80.3).
3. Discussion
Timely adequate surgical treatment ensures good five-year survival in most patients with PTC; metastatic spread to regional cervical lymph nodes or local cancer recurrence is detected after primary surgery in 20% of cases [
27,
28]. More accurate risk stratification of PTC recurrence is needed to avoid overtreatment of the majority of patients having a “favorable” prognosis and to ensure adequate treatment to the minority having an “aggressive” type of carcinoma.
Out of the set of molecular genetic events in patients with PTC, the ATA guidelines (2015) recommend to use only the BRAF and TERT mutations as markers of cancer with the least favorable prognosis. However, later reviews of this strategy yielded controversial conclusions. Some studies demonstrated that the BRAF mutation was associated with extrathyroidal extension of tumor and metastatic spread to cervical lymph nodes [
27], while another study did not reveal this association [
28]. In our work, the BRAF mutation was more frequent in groups of patients with intermediate and high recurrence risk according to ATA, however, statistical differences were minimal.
It is still extremely important to further search for efficient markers to perform accurate stratification of PTC recurrence [
6,
29]. MicroRNAs can be such markers; a large number of them, both oncogenic and tumor suppressor ones, have already been identified [
30]. In these studies, different miRNAs were shown to correlate with signs of tumor aggressiveness such as extrathyroidal extension, metastatic spread to lymph nodes, distant metastases, and disease recurrence. We examined 11 different miRNAs in preoperative cytology specimens and demonstrated that expression levels of two of them (miRNA-146b and miRNA-221) were significantly increased in the subgroups of patients having such features as regional metastases and extrathyroidal extension. The present work confirmed the findings of our previous study, where the expression levels of these same miRNAs were evaluated using postoperative specimens and the high risk of PTC recurrence was 9.7 times more probable (95% CI 3.1–29.5) if miR-221 level was > 1.0 [
31].
The genes responsible for various processes occurring in thyrocytes, whose activity can be determined according to their expression level, can be other candidates to act as molecular genetic markers. We can mention two out of 22 such genes that have been studied: the FN1 (fibronectin) and CDKN2A (cyclin-dependent kinase inhibitor 2A) genes. According to our findings, they turned out to be associated with metastatic spread to lymph nodes and higher recurrence risk.
For assessing the recurrence risk, one needs to understand that some patients having potentially aggressive PTC variants could be categorized into the low-risk group because of early tumor detection. However, the molecular markers may be indicative of their aggressiveness even before regional metastases and extrathyroidal extension develop. Therefore, one of the study objectives was quantifying expression of molecular genetic markers, which can be used to preoperatively predict the high risk of PTC recurrence with nearly 100% sensitivity, while specificity is not necessarily high.
These markers were as follows: relative expression of the CDKN2A gene > 0.044 (88.5% sensitivity); relative expression of the FN1 gene > 8.5 (100% sensitivity), and relative miRNA-221 expression > 0.47 (96.2% sensitivity).
4. Materials and Methods
4.1. Clinical Material
The study involved 125 patients with PTC who had been operated on at three sites (the clinical setting of the Division of General and Pediatric Surgery (Chelyabinsk, Russia), Department of Surgery at the Pirogov National Medical and Surgical Center (Moscow, Russia), and Pirogov Clinic of High Medical Technologies at St. Petersburg State University (St. Petersburg, Russia)) in 2022–2023. The clinical data and risk stratification (2015 ATA Risk Stratification System) were performed by analyzing patients’ medical records. Histology and cytology examinations were conducted by residential morphologists in the respective clinical settings. All the specimens were subsequently re-examined by two independent morphologists working at the National Center for Clinical Morphological Diagnostics (St. Petersburg, Russia); reports for cytology specimens were created in compliance with the 2023 Bethesda Systems; for histology specimens, in compliance with the Internal Histological Classification of Thyroid Tumors (5th Edition, 2022). After paucicellular cytology specimens and insufficiently informative histology specimens had been discarded, a total of 108 patients remained in the study.
4.2. Choosing the Set of Molecular Markers
Primary set of mRNA for analysis was selected according to the available literature. Protein-coding genes were chosen so that their exon–intron structure enabled detection of mRNA without preliminary purification to remove genomic DNA. The mRNA list comprised 22 genes: FN1, Geminin (GMNN), CDKN2A, TIMP1, CITED1, TPO, SLC26A7, HMGA2, CPQ, RXRG, SPATA18, APOE, ASF1B, AFAP1L2, CLU, ECM1, DIO1, NIS, SERPINA1, TFF3, TMPRSS4, and TSHR.
The set of miRNAs was selected according to our own data [
32] and analysis of the literature data; a total of 11 miRNAs were involved in experimental analysis: miR-146b-5p, miR-199b-5p, miR-221-3p, miR-223-3p, miR-31-5p, miR-375, miR-451a, miR-551b-3p, miR-148b-3p, miR-21-5p, and miR-125b-5p.
The mtDNA/nDNA ratio was used as a criterion for presence of oncocytic cells in the clinical specimen [
32]. Hence, a total of 34 molecular genetic markers have been analyzed in this study. The presence of the somatic BRAF V600E mutation was investigated separately.
4.3. Total Nucleic Acid Extraction
Nucleic acids were extracted according to the modified protocol reported in ref. [
32], namely: the dried cytology specimen was washed out into a test tube using three portions of lysis buffer (200 µL each).
4.4. Semi-Quantification of the Messenger RNA Level
Semi-quantitative assessment of the mRNA level was performed by real-time RT-PCR with specific primers and fluorescently labeled probes for detecting mRNA of the respective genes and the housekeeping gene PGK1 (phosphoglycerate kinase), which is used as a normalization gene. The RT-PCR protocol was as follows: incubation at 45°C – 30 min; heating at 95°C – 2 min, 50 cycles: denaturation at 94°C – 10 s; annealing and extension: 60°C – 20 s. The relative expression level was calculated using the 2
-ΔCq method [
33].
4.5. MicroRNA Detection
Detection of 16-miRNA by real-time RT-PCR was conducted for all tumor and lesion types. Mature miRNAs were detected by stem-loop RT-PCR [
34]. Real-time reverse transcription PCR was carried out in compliance with the procedure described in ref. [
13]. Reverse transcription PCR followed by real-time PCR was conducted individually for each miRNA. Single-replicate analysis was performed for each specimen. The miRNA level was normalized to the geometric mean of the levels of three reference miRNAs (miR-197-3p, -23a-3p, and -29b-3p) using the 2
-ΔCq method.
4.6. Quantification of the Ratio between the Mitochondrial and Nuclear DNA Copy Number (the mtDNA/nDNA Ratio)
Mitochondrial and nuclear DNA were detected by real-time PCR. The PCR protocol was as follows: pre-heating at 95°C – 2 min, 50 cycles: denaturation at 94°C – 10 s, annealing and extension: 60°C – 20 s. The ratio was determined using the 2-ΔCq method.
4.7. Detection of Somatic BRAF Mutation
All the samples were tested for somatic mutations V600E, V600K, and V600R in the BRAF gene. Somatic mutations were detected using hydrolysis probe-based allele-specific PCR. The PCR protocol was as follows: pre-heating at 95°C – 2 min, 50 cycles: denaturation at 94°C – 10 s, annealing and extension: 60°C – 15 s.
4.8. Statistical Data Analysis
Statistical data analysis was conducted using the SPSS Statistics 23 (IBM, USA) and Excel software (Microsoft, USA). The data are presented as the mean and median values, Q1 and Q3. All the statistical analyses were conducted using the Mann–Whitney test for comparing two groups. The family-wise error rate (FWER) assessed using the Bonferroni method was used to solve the multiple hypothesis testing problem. The significance level p was calculated as 0.05 divided by the number of parameters being compared. In our study, we compared 34 parameters, so р <0.05/34=0.0015 was considered statistically significant. The correlation between tumor size and miRNA and gene expression levels was evaluated using the Spearman’s rank correlation coefficient. The association between the BRAF mutation status and each clinical pathological variable was assessed using the Pearson’s chi-squared test (χ2) and Fisher’s exact test when the number of patients was < 5. If p < 0.05, the difference was considered statistically significant. The odds ratio (OR) was determined by univariate analysis; 95% confidence intervals were also calculated.
Binary classification involving plotting the ROC curves was used for objective evaluation of the predictive power for the expression levels of different miRNAs and genes to predict the risk of PTC recurrence. The ROC curve shows the dependence between the number of correctly classified positive examples (a true positive set) on the number of incorrectly classified negative examples (a false negative set). The assessed reliability score is expressed as sensitivity and specificity parameters. The tests were compared with allowance for the area under the ROC curves (AUC). It is fair to say with some assumptions that the close the AUC parameter to unity, the higher the predictive power of a test is. The following expert scale was employed for the AUC values (it can be used to assess the quality of a model): 0.9–1.0 – excellent; 0.8–0.9 – very good; 0.7–0.8 – good; 0.6–0.7 – moderate; and 0.5–0.6 – poor.
5. Conclusions
Identifying novel molecular genetic markers for predicting aggressiveness and the risk of PTC recurrence is a very important problem to be solved, since it will allow reducing the surgery extent and therefore, the number of potential postoperative complications on the one hand. On the other hand, more extensive surgical interventions, even in patients from the low recurrence risk group but having high expression of these markers, will help reduce the future risk of tumor recurrence. Furthermore, the active surveillance approach that has been recently actively discussed instead of surgical treatment, can be complemented by new molecular genetic criteria in patients with papillary thyroid microcarcinomas. Detailed understanding of the potential risks of PTC recurrence at the treatment planning stage will help ensure personalized therapy and will therefore improve patients’ quality of life and treatment outcomes.
Author Contributions
Conceptualization, SAL, SET and ESK; methodology, SET, ESK, VAZh; validation, ESK, SLV and IVS; formal analysis, PSD; investigation, YAV, DVK, TEI and NSB; resources, DVK, TEI, NSB and IVS; data curation, SET and PSD; writing—original draft preparation, SAL, SET and SLV; writing—review and editing, VAZh, IVS and SVS; supervision, SVS, VAZh and IVS; project administration, SAL, SET and ESK. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Russian Science Foundation, grant number 20-14-00074-P.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the South Ural State Medical University (Protocol No. 3 issued April 18, 2019).
Informed Consent Statement
Informed consent was obtained from all patients involved in the study, all data were depersonalized.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The cell analysis was carried out at the Center for Collective Use of Microscopic Research at the Institute of Cytology and Genetics SB RAS (supported by the IC&G budget project). The authors express their gratitude to the Center for Collective Use (CCU) "Bioinformatics" for the computational resources and their software, created within the framework of the budget project FWNR-2022-0020.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016, 26(1), 1–133. [Google Scholar] [CrossRef]
- Davies, L.; Welch, H.G. Thyroid cancer survival in the United States: observational data from 1973 to 2005. Arch Otolaryngol Head Neck Surg. 2010, 136(5), 440–444. [Google Scholar] [CrossRef] [PubMed]
- Haddad, R.I.; Bischoff, L.; Ball, D.; Bernet, V.; Blomain, E.; Busaidy, N.L.; Campbell, M.; Dickson, P.; Duh, Q.; Ehya, H.; et al. Thyroid Carcinoma, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network 2022, 20, 925–951. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.H.; Li, Y.R.; Chang, K.H.; Liou, M.J.; Lin, S.F.; Tsai, S.S.; Yu, M.C.; Hsueh, C.; Chen, S.T. Evaluation of recurrence risk in patients with papillary thyroid cancer through tumor-node-metastasis staging: A single-center observational study in Taiwan. Biomed J. 2022, 45(6), 923–930. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.N.; Angell, T.E.; Babiarz, J.; Barth, N.M.; Blevins, T.; Duh, Q.Y.; Ghossein, R.A.; Harrell, R.M.; Huang, J.; Kennedy, G.C.; et al. Performance of a genomic sequencing classifier for the preoperative diagnosis of cytologically indeterminate thyroid nodules. JAMA Surg. 2018, 153(9), 817–824. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, P.; Leon, M.E.; Centeno, B.A.; Otto, K.J.; Khazai, L.; McCaffrey, J.C.; Russell, J.S.; McIver, B. Institutional prevalence of malignancy of indeterminate thyroid cytology is necessary but insufficient to accurately interpret molecular marker tests. Eur J Endocrinol. 2016, 174(5), 621–629. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.N.; Yip, L.; Lubitz, C.C.; Grubbs, E.G.; Miller, B.S.; Shen, W.; Angelos, P.; Chen, H.; Doherty, G.M.; Fahey, T.J. 3 rd.; et al. The American Association of Endocrine Surgeons Guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020, 271(3), e21–93. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, F.; Nikitski, A.V.; Nikiforova, M.N.; Nikiforov, Y.E. Spectrum of TERT promoter mutations and mechanisms of activation in thyroid cancer. Cancer Med. 2019, 8(13), 5831–5839. [Google Scholar] [CrossRef] [PubMed]
- Melo, M.; da Rocha, A.G.; Vinagre, J.; Batista, R.; Peixoto, J.; Tavares, C.; Celestino, R.; Almeida, A.; Salgado, C.; Eloy, C.; et al. TERT promoter mutations are a major indicator of poor outcome in differentiated thyroid carcinomas. J Clin Endocrinol Metab. 2014, 99(5), E754–E765. [Google Scholar] [CrossRef] [PubMed]
- Zafon, C.; Gil, J.; Pérez-González, B.; Jordà, M. DNA methylation in thyroid cancer. Endocr Relat Cancer. 2019, 26, R415–R439. [Google Scholar] [CrossRef]
- Rogucki, M.; Buczyńska, A.; Krętowski, A.J. Popławska-Kita A. The Importance of miRNA in the Diagnosis and Prognosis of Papillary Thyroid Cancer. J Clin Med. 2021, 10(20), 4738. [Google Scholar] [PubMed]
- Nieto, H.R.; Thornton, C.E.M.; Brookes, K.; Nobre de Menezes, A.; Fletcher, A.; Alshahrani, M.; Kocbiyik, M.; Sharma, N.; Boelaert, K.; et al. Recurrence of Papillary Thyroid Cancer: A Systematic Appraisal of Risk Factors. J Clin Endocrinol Metab. 2022, 107(5), 1392–1406. [Google Scholar] [CrossRef] [PubMed]
- Titov, S.E.; Ivanov, M.K.; Demenkov, P.S.; Katanyan, G.A.; Kozorezova, E.S.; Malek, A.V.; Veryaskina, Y.A.; Zhimulev, I.F. Combined quantitation of HMGA2 mRNA, microRNAs, and mitochondrial-DNA content enables the identification and typing of thyroid tumors in fine-needle aspiration smears. BMC Cancer. 2019, 19, 1010. [Google Scholar] [CrossRef] [PubMed]
- Ravi, N.; Yang, M.; Mylona, N.; Wennerberg, J.; Paulsson, K. Global RNA Expression and DNA Methylation Patterns in Primary Anaplastic Thyroid Cancer. Cancers (Basel). 2020, 12(3), 680. [Google Scholar] [CrossRef] [PubMed]
- Wojtas, B.; Pfeifer, A.; Oczko-Wojciechowska, M.; Krajewska, J.; Czarniecka, A.; Kukulska, A.; Eszlinger, M.; Musholt, T.; Stokowy, T.; Swierniak, M.; et al. Gene Expression (mRNA) Markers for Differentiating between Malignant and Benign Follicular Thyroid Tumours. Int J Mol Sci. 2017, 18(6), 1184. [Google Scholar] [CrossRef] [PubMed]
- Poma, A.M.; Giannini, R.; Piaggi, P.; Ugolini, C.; Materazzi, G.; Miccoli, P.; Vitti, P.; Basolo, F. A six-gene panel to label follicular adenoma, low- and high-risk follicular thyroid carcinoma. Endocr Connect. 2018, 7(1), 124–132. [Google Scholar] [CrossRef] [PubMed]
- Mussazhanova, Z.; Shimamura, M.; Kurashige, T.; Ito, M.; Nakashima, M.; Nagayama, Y. Causative role for defective expression of mitochondria-eating protein in accumulation of mitochondria in thyroid oncocytic cell tumors. Cancer Sci. 2020, 111(8), 2814–2823. [Google Scholar] [CrossRef] [PubMed]
- Nan, B.Y.; Xiong, G.F.; Zhao, Z.R.; Gu, X.; Huang, X.S. Comprehensive Identification of Potential Crucial Genes and miRNA-mRNA Regulatory Networks in Papillary Thyroid Cancer. Biomed Res Int. 2021, 2021, 6752141. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Han, W.; Lu, K. Comprehensive Pan-Cancer Analysis and the Regulatory Mechanism of ASF1B, a Gene Associated With Thyroid Cancer Prognosis in the Tumor Micro-Environment. Front Oncol. 2021, 11, 711756. [Google Scholar] [CrossRef]
- Zafereo, M.; McIver, B.; Vargas-Salas, S.; Domínguez, J.M.; Steward, D.L.; Holsinger, F.C.; Kandil, E.; Williams, M.; Cruz, F.; Loyola, S.; et al. A Thyroid Genetic Classifier Correctly Predicts Benign Nodules with Indeterminate Cytology: Two Independent, Multicenter, Prospective Validation Trials. Thyroid. 2020, 30(5), 704–712. [Google Scholar] [CrossRef]
- Kebebew, E.; Peng, M.; Reiff, E.; Duh, Q.Y.; Clark, O.H.; McMillan, A. ECM1 and TMPRSS4 are diagnostic markers of malignant thyroid neoplasms and improve the accuracy of fine needle aspiration biopsy. Ann Surg. 2005, 242(3), 353–361. [Google Scholar] [CrossRef] [PubMed]
- Fryknäs, M.; Wickenberg-Bolin, U.; Göransson, H.; Gustafsson, M.G.; Foukakis, T.; Lee, J.J.; Landegren, U.; Höög, A.; Larsson, C.; Grimelius, L.; et al. Molecular markers for discrimination of benign and malignant follicular thyroid tumors. Tumour Biol. 2006, 27(4), 211–20. [Google Scholar] [PubMed]
- Colombo, C.; Minna, E.; Gargiuli, C.; Muzza, M.; Dugo, M.; De Cecco, L.; Pogliaghi, G.; Tosi, D.; Bulfamante, G.; Greco, A.; et al. The molecular and gene/miRNA expression profiles of radioiodine resistant papillary thyroid cancer. J Exp Clin Cancer Res. 2020, 39, 245. [Google Scholar] [CrossRef] [PubMed]
- Binabaj, M.M.; Soleimani, A.; Rahmani, F.; Avan, A.; Khazaei, M.; Fiuji, H.; Soleimanpour, S.; Ryzhikov, M.; Ferns, G.A.; Bahrami, A.; et al. Prognostic value of high mobility group protein A2 (HMGA2) over-expression in cancer progression. Gene. 2019, 706, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Tavares, C.; Coelho, M.J.; Eloy, C.; Melo, M.; Gaspar da Rocha, A.; Pestana, A.; Batista, R.; Bueno Ferreira, L.; Rios, E.; Selmi-Ruby, S.; et al. NIS expression in thyroid tumors, relation with prognosis clinicopathological and molecular features. Endocrine Connections. 2018, 7(1), 78–90. [Google Scholar] [CrossRef] [PubMed]
- Chai, L.; Han, D.; Li, J.; Lv, Z. The construction and analysis of gene co-expression network of differentially expressed genes identifies potential biomarkers in thyroid cancer. Transl Cancer Res. 2018, 7(5), 1235–1243. [Google Scholar] [CrossRef]
- Feng, J.; Shen, F.; Cai, W.; Gan, X.; Deng, X.; Xu, B. Survival of aggressive variants of papillary thyroid carcinoma in patients under 55 years old: a SEER population-based retrospective analysis. Endocrine. 2018, 61, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Baloch, Z.W.; Asa, S.L.; Barletta, J.A.; Ghossein, R.A.; Juhlin, C.C.; Jung, C.K.; LiVolsi, V.A.; Papotti, M.G.; Sobrinho-Simões, M.; Tallini, G.; et al. Overview of the 2022 WHO Classification of Thyroid Neoplasms. Endocr Pathol. 2022, 33(1), 27–63. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.K.; Jung, S.H.; Jeon, S.; Jeong, Y.M.; Kim, Y.; Lee, S.; Bae, J.S.; Chung, Y.J. Risk Stratifcation Using a Novel Genetic Classifer Including PLEKHS1 Promoter Mutations for Diferentiated Thyroid Cancer with Distant Metastasis. Thyroid. 2020, 30, 1589–1600. [Google Scholar] [CrossRef]
- Santiago, K.; Chen Wongworawat, Y.; Khan, S. Differential MicroRNA-Signatures in Thyroid Cancer Subtypes. J Oncol. 2020, 2020, 2052396. [Google Scholar] [CrossRef]
- Lukyanov, S.A.; Sergiyko, S.V.; Titov, S.E.; Reshetov, I.V.; Veryaskina, Y.A.; Vazhenin, A.V.; Gostimsky, A.V.; Ippolitov, L.I.; Rogova, M.O. Stratification of papillary thyroid cancer relapse risk based on the results of molecular genetic studies. Opukholi golovy i shei = Head and Neck Tumors. 2020, 10, 93–100. [Google Scholar] [CrossRef]
- Titov, S.; Ivanov, M.; Karpinskaya, E.V.; Tsivlikova, E.V.; Shevchenko, S.P.; Veryaskina, Y.A.; Akhmerova, L.G.; Poloz, T.L.; Klimova, O.A.; Gulyaeva, L.F.; et al. miRNA profiling, detection of BRAF V600E mutation and RET-PTC1 translocation in patients from Novosibirsk oblast (Russia) with different types of thyroid tumors. BMC Cancer. 2016, 16, 201. [Google Scholar] [CrossRef] [PubMed]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001, 25(4), 402–8. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Ridzon, D.A.; Broomer, A.J.; Zhou, Z.; Lee, D.H.; Nguyen, J.T.; Barbisin, M.; Xu, N.L.; Mahuvakar, V.R.; Andersen, M.R.; et al. Real-time quantification of microRNAs by stem-loop RT-PCR. Nucleic Acids Res. 2005, 33(20), e179. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).