1. Introduction
Skeletal muscle is the most abundant muscle found in the body. It has a multitude of functions, including producing movement, stabilizing joints and sustaining body posture and position [
1]. While skeletal muscle is primarily reponsible for converting chemical energy into mechanical energy, it is also important for producing body heat by contracting and promoting shivering in cases of extreme cold. Additionally, these muscles serve as the storage site for carbohydrates and amino acids, therefore contributing to the basal energy metabolism [
1].
While the skeletal muscle performs many functions as discussed above, one of the other most significant functions is that of glucose uptake. Glucose is the major source of energy for a majority of the tissues of the body and the skeletal muscle is responsible for 80-90% of the insulin-stimulated glucose uptake in the body, particularly via the glucose transporter 4 (GLUT4) [
2].
More recently identified glucose and sodium co-transporters are Sodium Glucose Co-transporters (SGLT) 1 and 2. Currently, SGLT1 is expressed in not only the small intestine and the heart, but also the skeletal muscle [
3], and recently our team has shown it to be widely expressed in the retina [
4]. Unlike SGLT1, SGLT2 is particularly limited to the proximal tubules of the kidneys and areas of the eye such as the retina [
5], cornea [
6] and lens [
7]. On the other hand, one study has demonstrated that the gene for
Sglt2 (
slc5a2) is expressed at the mRNA level in skeletal muscle but it has not been shown to be expressed as protein [
3]. Future studies are warranted to ascertain if skeletal muscle is indeed a source of SGLT2 protein.
Studies addressing the clinical impact of SGLT1 and SGLT2 inhibition (SGLT1/2i) provides critical insight into the importance of regulation of these two members of the SGLT family. Inhibitors of SGLT2 were developed based on the anti-diabetic action initiated by inhibiting renal glucose reabsorption, thereby increasing glucosuria. Of great clinical significance, large-scale clinical trials utilizing a range of SGLT2 inhibitors (SGLT2i) have demonstrated both metabolic and biochemical benefits [
8] via numerous novel mechanisms, such as sympathoinhibition which has been shown by our team [
9]. One of the burning questions at present is whether utilizing a dual SGLT1/2i like Sotagliflozin (SOTAG) may be more beneficial than sole SGLT2i’s such as Empagliflozin (EMPA) when it comes to the treatment of cardiorenal disease in both patients with and without diabetes. As dual SGLT1/2i is a relatively new pharmacological therapy compared to sole SGLT2i, the breadth of research findings is limited for SGLT1/2i. Highlighting the importance of SOTAG related studies, two clinical trials utilizing SOTAG showed that in patients with Type 2 Diabetes (T2D) and Chronic Kidney Disease (CKD), the rate of hospitalization and urgent care visits for heart failure was significantly reduced when patients were administered SOTAG compared with placebo [
10,
11].
Furthermore, it is of utmost importance to examine mechanisms that regulate glucose and sodium transport in skeletal muscle. This is important because, for example, in sarcopenia, there is a loss of skeletal muscle mass and strength and both hyperglycemia (high glucose levels) and high salt intake have been associated with increased risk of sarcopenia [
12,
13]. Studies have shown that while hyperglycemia negatively affects the regenerative capability of the skeletal muscle satellite cells [
12], high salt intake may also lead to the fat accumulation due to leptin resistance [
14] and promotes the muscle weakness associated with sarcopenia [
13]. Thus, in conditions such as sarcopenia, inhibiting excessive sodium and glucose uptake in muscle is clinically relevant.
Given that Sglt2 has only been shown to be expressed at the mRNA level in skeletal muscle, our novel study aimed to determine if SGLT2 protein exists within skeletal muscle. In addition, there is currently limited literature on the regulation of SGLT1, particularly in the context of SGLT2i therapy and the Sympathetic Nervous System (SNS). In our current study, we investigate mechanisms underlying SGLT1 regulation in skeletal muscle. We hypothesise that both SGLT2 inhibition and SNS activation may upregulate SGLT1 expression. This study may ultimately highlight that either SGLT1 inhibition (SGLT1i) alone or dual SGLT1/2 inhibition (SGLT1/2i) may be beneficial to treat diseases associated with SNS activation such as diabetes and hypertension and that skeletal muscle may be a target organ for these therapies.
2. Methods
2.1. L6 Cell Culture
L6 rodent skeletal muscle cells were cultured in growth medium containing 1g/L low-glucose Dulbecco's Modified Eagle Medium (LG-DMEM) supplemented with L-glutamine (1%), streptomycin (2%) and foetal calf serum (FCS) (10%), (Thermo Fisher, Melbourne, Australia) in a 75 cm² flask until 70% confluency was achieved. At this point, the cells underwent trypsinization to allow detachment from the flask for transfer into a Corning Cell Bind 6-well plate (Corning, New York, USA) in 2 mL of growth medium.
The differentiation process started once the cells achieved 70% confluency in the growth medium. Differentiation medium contained low-glucose Dulbecco's Modified Eagle Medium (LG-DMEM) supplemented with L-glutamine (1%), streptomycin (2%) and foetal calf serum (FCS) (2%). The differentiation medium was changed every two days for seven days [
15]. At this point, the wells were treated appropriately as indicated below.
2.2. Treatment with Norepinephrine (NE)
Our team has previously published the optimal NE treatment conditions for SGLT1 and SGLT2 protein studies in HK2 cells (16). Differentiated L6 skeletal muscle cells were treated with either Vehicle (VEH, Baxter water) or 10 µM NE (Sigma-Aldrich, Sydney, Australia) in 2 ml of low glucose DMEM growth media for a period of 48 hrs. The NE was protected from light during its preparation and experiments.
2.3. Sole SGLT2 inhibitors and dual SGLT1/2 inhibitor treatment
Based on previously published literature, the SGLT2i Empagliflozin (EMPA; Ark Pharma Scientific Limited, Wuhan, China) was used at 30 µM for in vitro purposes (17, 18). Stock solutions (0.03 M) were prepared and diluted 1 in 1000 in low glucose differentiation media. Dimethyl sulphoxide (DMSO) was used to dissolve the SGLT2i’s and control cells were treated with equivalent volumes of DMSO (vehicle) compared to the SGLT2i treatment. Incubation times were chosen based on previously published data (17). To allow for comparability, SOTAG was also prepared as a 0.03 M stock solution. The stock solution was diluted at a 1 in 1000 dilution in low glucose differentiation media.
2.4. Collection of protein cell lysates
After cells were treated, they were gently placed on ice where the media was removed and discarded. This was followed by two 1X cold PBS washes of each well (2 ml per well). The monolayer was then lysed with 60 µl of lysis buffer containing 1X phosphatase inhibitor, 1X protease inhibitor and cytosolic extraction buffer (CEB). The CEB buffer consisted of 10 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) pH 7.5, 14 mM KCl, 5% glycerol, 0.2% nonidet P-40 (Igepal). After adding lysis buffer to cells, adhered HK2 cells were then scraped and transferred to a 1.5 ml eppendorf tube to be stored at -80 °C for 24 hrs. Cell lysates were thawed and centrifuged at 12 000 rpm at 4 °C for 10 minutes. Supernatants were gently transferred to a new 1.5 ml eppendorf tube for protein quantitation.
2.5. Protein quantification using the Bradford Assay
Sample protein concentrations were determined using the Bradford assay. The bovine serum albumin (BSA) protein standards were added to 96 well plates in duplicate with concentrations ranging from 0-6 µg/µl. In separate wells, 1 µl of protein sample was added in duplicate to the same 96 well plate. Then, 250 µl of Bradford protein assay reagent was prepared for each sample well (50 µl of Bio-Rad dye reagent concentrate and 200 µl of Milli-Q water) and added to each well. The absorbance of samples was then determined after reading the plate at 595 nm which gave rise to the development of a standard curve (OD versus BSA protein standard concentrations). Unknown protein sample concentrations were then calculated using the standard curve. Samples were then prepared (10 µg/100 µl) for SGLT1 determination.
2.6. Enzyme-linked Immunosorbent Assay (ELISA)
L6 lysates were analysed for SGLT1 protein expression levels using a commercially available rodent SGLT1-specific ELISA kit (Cloud clone – SEE 381Mu (Wuhan, China)) as per the manufacturer’s instructions.
2.7. SGLT1 and SGLT2 Immunocytochemistry of L6 cells
SGLT1 and SGLT2 was detected in L6 cells using the immunocytochemistry technique. Using a 6 well plate, the cells were fixed in methanol/acetone (1:1) and then endogenous peroxidases were blocked with 3% H2O2 followed by blocking with 10% FCS/Tx/PBS. The primary antibodies i) anti-SGLT1 (1:500, Rabbit antibody, Novus, NBP2.20338 Centennial, CO, USA.) and ii) anti-SGLT2 (1:500, Rabbit antibody, Santa Cruz Biotechnology, sc98975, Sydney, Australia) were diluted in 0.05% Triton X/PBS and added to each well and incubated at 4° C overnight. The following day a secondary horse-radish peroxidase conjugated anti-rabbit antibody (1:100, Santa Cruz Biotechnology, Sydney, Australia) was added to each well. Cells were washed and SGLT1 and 2 expression was detected with diaminobenzadine (DAB) prior to visualisation with a high-powered microscope.
2.8. Animal Work
Twelve week old BPN/3J (blood pressure normal) and BPH/2J (blood pressure high) male mice were obtained for experiments from Ozgene Animal Resource Centre (Ozgene ARC, Perth, Australia). Our BPH/2J Schlager mice with neurogenic hypertension [
19,
20] are a highly relevant mouse model since they mimic human disease with increased sympathetic activity [
21], elevated heart rate and heightened blood pressure [
21,
22] driven by neurogenic mechanisms [
23]. All animal experiments were carried out at the Harry Perkins Institute for Medical Research animal holding facility (Perth, WA, Australia). Animal ethics was approved by the Harry Perkins Institute for Medical Research Animal Ethics Committee (AE284).
Mice were housed individually under a 12-hour light/dark cycle, at 21
+ 2° C and were given a standard chow diet (Specialty Feeds, Glen Forrest, WA, Australia) with free access to food and drinking water. Following 7 days of acclimatization, either the dual SGLT1/2 inhibitor (SOTAG; Med Chem Express, USA; 25mg/kg/day) or Vehicle (dimethylsulfoxide [DMSO]) was administered to each mouse via drinking water for a period of 2 weeks. Drinking water containing the inhibitor or vehicle was freshly prepared and replenished weekly. The blood pressure measurements were conducted on 13, 14 and 15 week old BPH/2J mice as per our previous studies [
21] using a non-invasive computer automated multichannel blood pressure analysis system MC4000 (Hatteras Instruments, Cary, North Carolina, USA). Quadricep skeletal muscle tissue was dissected from our 15 week old BPN/3J or BPH/2J (Schlager) mice [
21,
24]. Quadricep skeletal muscle was fixed in paraformaldehyde and subsequently embedded in paraffin wax as reported by Herat et al, 2020 [
24].
2.9. SGLT1 Immunohistochemistry of Quadricep Skeletal Muscle
We performed SGLT1 immunohistochemistry in the quadricep skeletal muscle of our normotensive BPN/3J mice and hypertensive BPH/2J mice. Quadricep tissues from both our BPN/3J and BPH/2J mice were sectioned at 5 μm onto positively charged microscope slides and de-waxed in xylene and rehydrated in ethanol. Antigen retrieval was performed on slides by heating in EDTA buffer (pH 8.5; Sigma-Aldrich, Sydney, NSW, Australia). After washing twice in PBS/0.1% Tween for 5 min, tissue sections were outlined with a paraffin pen.
Sections were blocked with 3% H
2O
2 for 10 min, washed twice with PBS/0.1% Tween for 5 min and blocked with 5% FCS in PBS/0.1% Tween for 1 hr in a humidified chamber.
Sections were then incubated overnight with primary anti-SGLT1 antibodies at 4°C in a humidified chamber. SGLT1 immunohistochemical detection was done in a novel way using a combination of primary antibodies from both Abcam (Rabbit anti-SGLT1, 14685, IgG, Polyclonal, 1:180) and Novus (Rabbit anti-SGLT1, NBP2.20338, IgG, Polyclonal, 1:100) antibodies [
25]. Following overnight incubation, sections were washed three times with PBS/0.1% Tween for 5 mins and incubated with anti-rabbit (1:100, Santa Cruz Biotechnology, Sydney, Australia) secondary antibody conjugated with HRP in PBS/0.1% Tween for 1 hr. This was followed by incubation with DAB. Tissue sections were dehydrated and then mounted with DPX (Sigma-Aldrich, Sydney, Australia).
2.10. SGLT2 Immunohistochemistry of Quadricep Skeletal Muscle
We performed SGLT2 immunohistochemistry in the quadricep skeletal muscle of our normotensive BPN/3J mice and hypertensive BPH/2J mice. Quadricep tissues from both our BPN/3J and BPH/2J mice were sectioned at 5 μm onto positively charged microscope slides and de-waxed in xylene and rehydrated in ethanol. Antigen retrieval was performed on slides by heating in EDTA buffer (pH 8.5; Sigma-Aldrich, Sydney, NSW, Australia). After washing twice in PBS/0.1% Tween for 5 min, tissue sections were outlined with a paraffin pen. Sections were blocked with 3% H2O2 for 10 min, washed twice with PBS/0.1% Tween for 5 min and blocked with 5% FCS in PBS/0.1% Tween for 1 hr in a humidified chamber. Sections were then incubated overnight with primary anti-SGLT2 antibodies at 4°C in a humidified chamber. SGLT2 immunohistochemical detection was done in a novel way by using a combination of primary antibodies from both Santa Cruz (Mouse anti-SGLT2, sc393350, 1:50) and Novus (Rabbit anti-SGLT2, NBPI-92384, 1:200). Following overnight incubation, sections were washed three times with PBS/0.1% Tween for 5 mins and incubated with anti-rabbit (1:100, Santa Cruz Biotechnology, Sydney, Australia) and anti-mouse (1:100, Santa Cruz Biotechnology, Sydney, Australia) secondary antibodies conjugated with HRP in PBS/0.1% Tween for 1 hr. This was followed by incubation with DAB. Slides were dehydrated and mounted with DPX (Sigma-Aldrich, Sydney, Australia).
2.11. Tissue imaging and analysis
Images were obtained using the inverted microscopic system Nikon Eclipse Ti (Nikon, Tokyo, Japan) with a digital camera CoolSNAP HQ2 (Photometrics, Tucson, AZ, USA) linked to a computer running the image analysis software ‘NIS-Elements Advanced Research’ (Nikon, Tokyo, Japan). The mean SGLT1 staining expression intensity scores were calculated based on a scale of 0–3 (0 = absent expression; 1 = low expression; 2 = intermediate expression; 3 = high expression). Expression scores were obtained by two independent scorers to ensure results were unbiased.
2.12. Statistical analysis
All data were analyzed using two-tailed Student’s t-test or One-way ANOVA and p≤0.05 was considered as a significant threshold.
3. Results
3.1. Skeletal muscle is a novel source of SGLT2 protein.
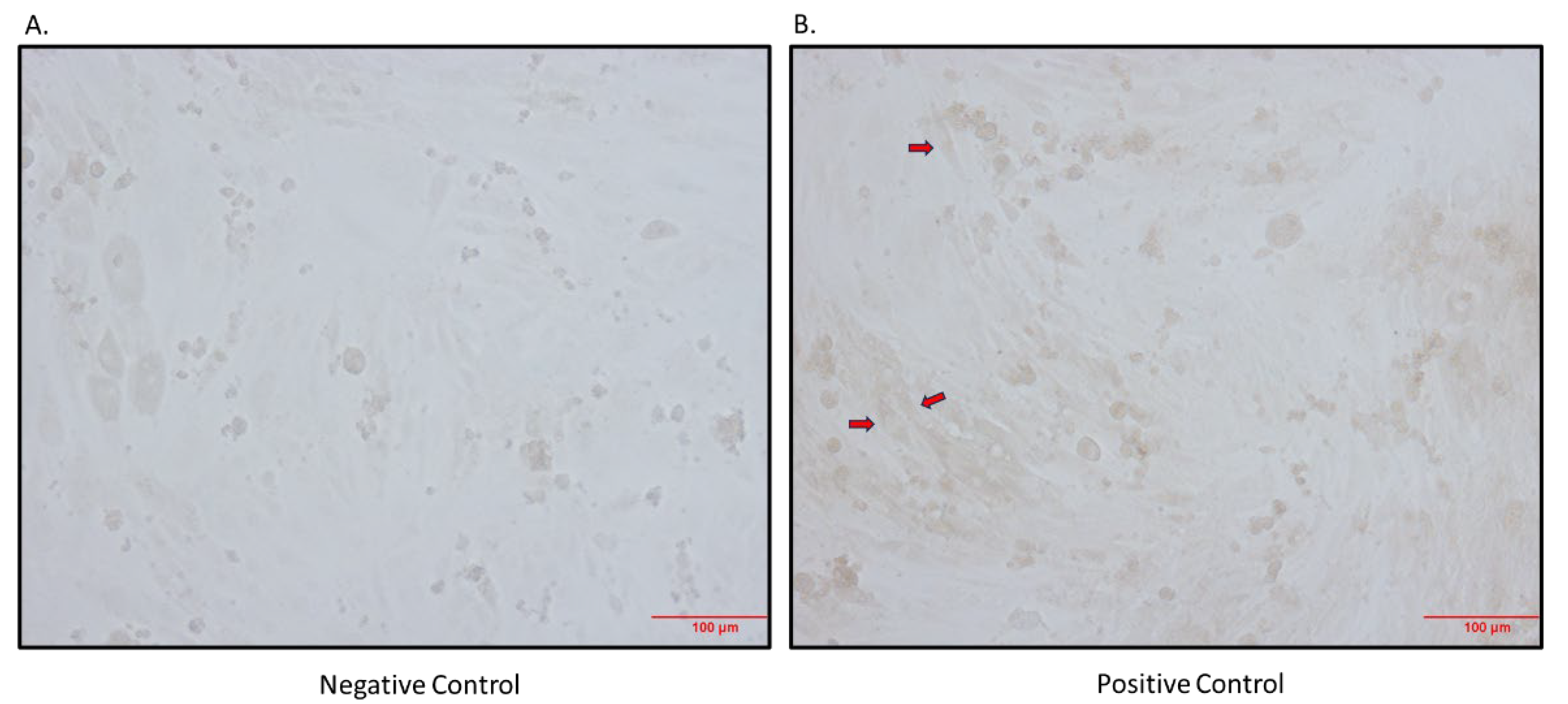
3.1.1. Immunocytochemistry staining of differentiated L6 skeletal muscle cells shows SGLT2 protein expression.
It has previously been shown that
Sglt2 mRNA is expressed in rodent skeletal muscle [
3], however it has not yet been shown to be expressed at the protein level. Further support for SGLT2 being possibly expressed at the protein level in skeletal muscle is the fact that the SGLT2i, Canagliflozin, was used in the L6 skeletal muscle cell line [
26]. Utilising the L6 cell line, we found that SGLT2 protein is indeed expressed in differentiated L6 cells (
Figure 1).
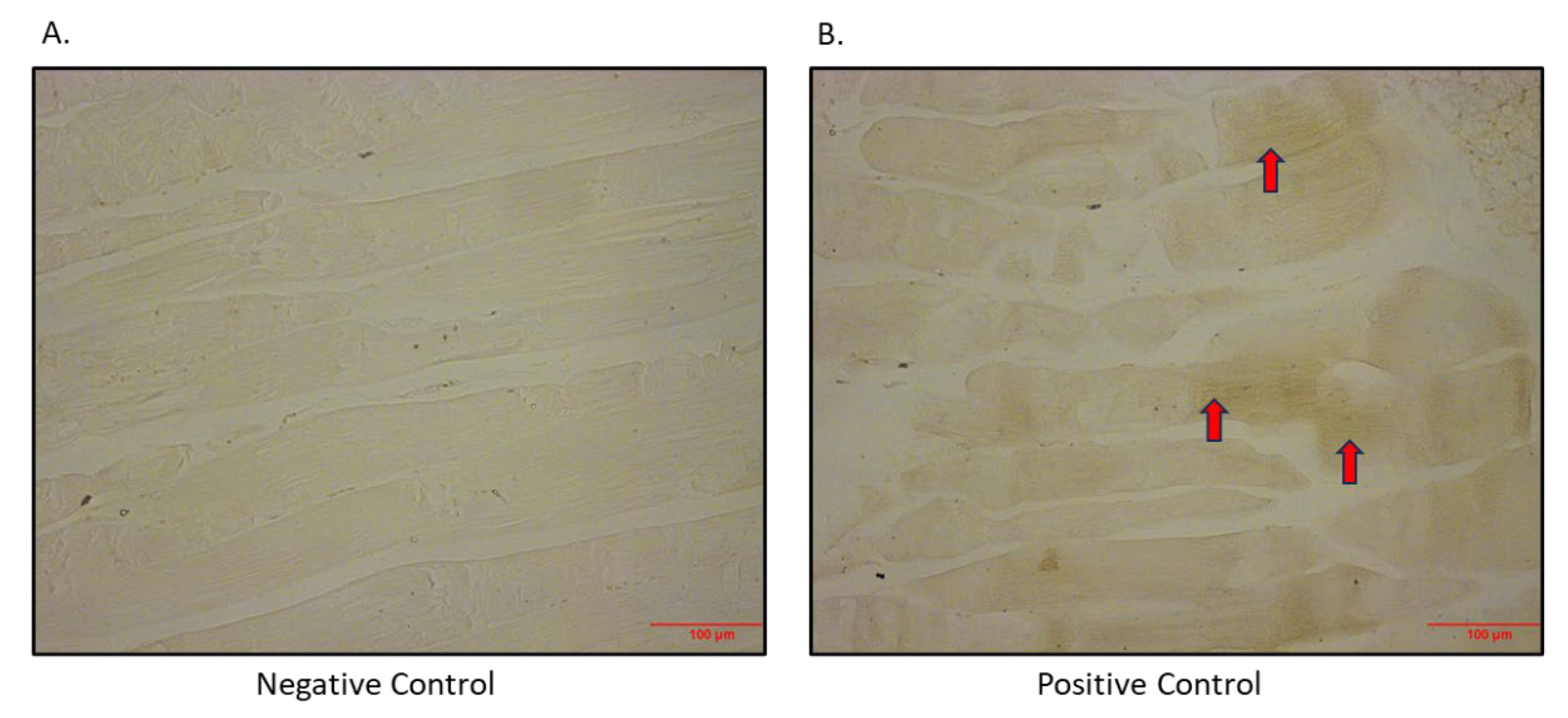
3.1.2. Skeletal Muscle expresses SGLT2 in vivo.
After determining that SGLT2 protein is expressed in the L6 skeletal muscle cell line, we also set out to show that this is an
in vivo phenomenon. The SGLT2 protein was shown to be expressed heterogeneously in quadricep skeletal muscle (
Figure 2).
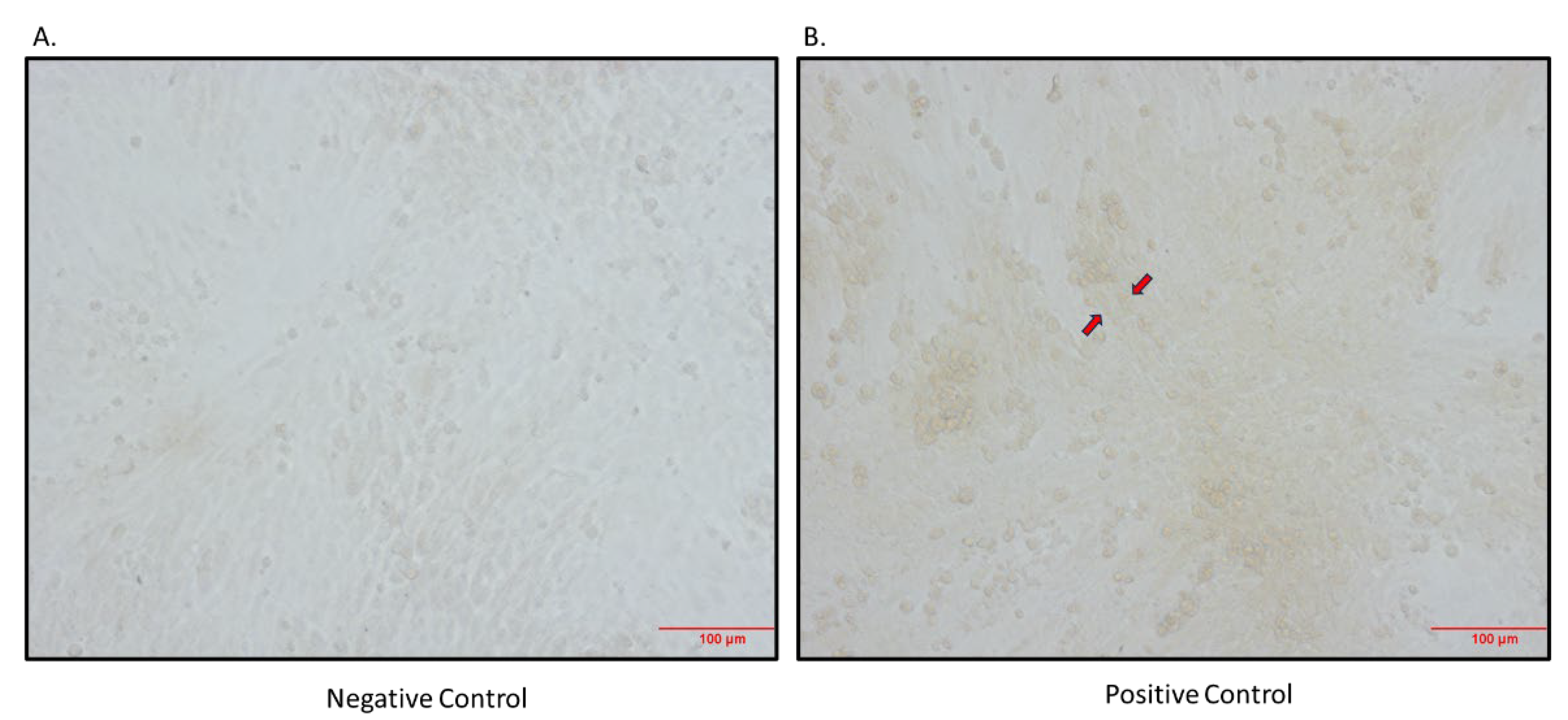
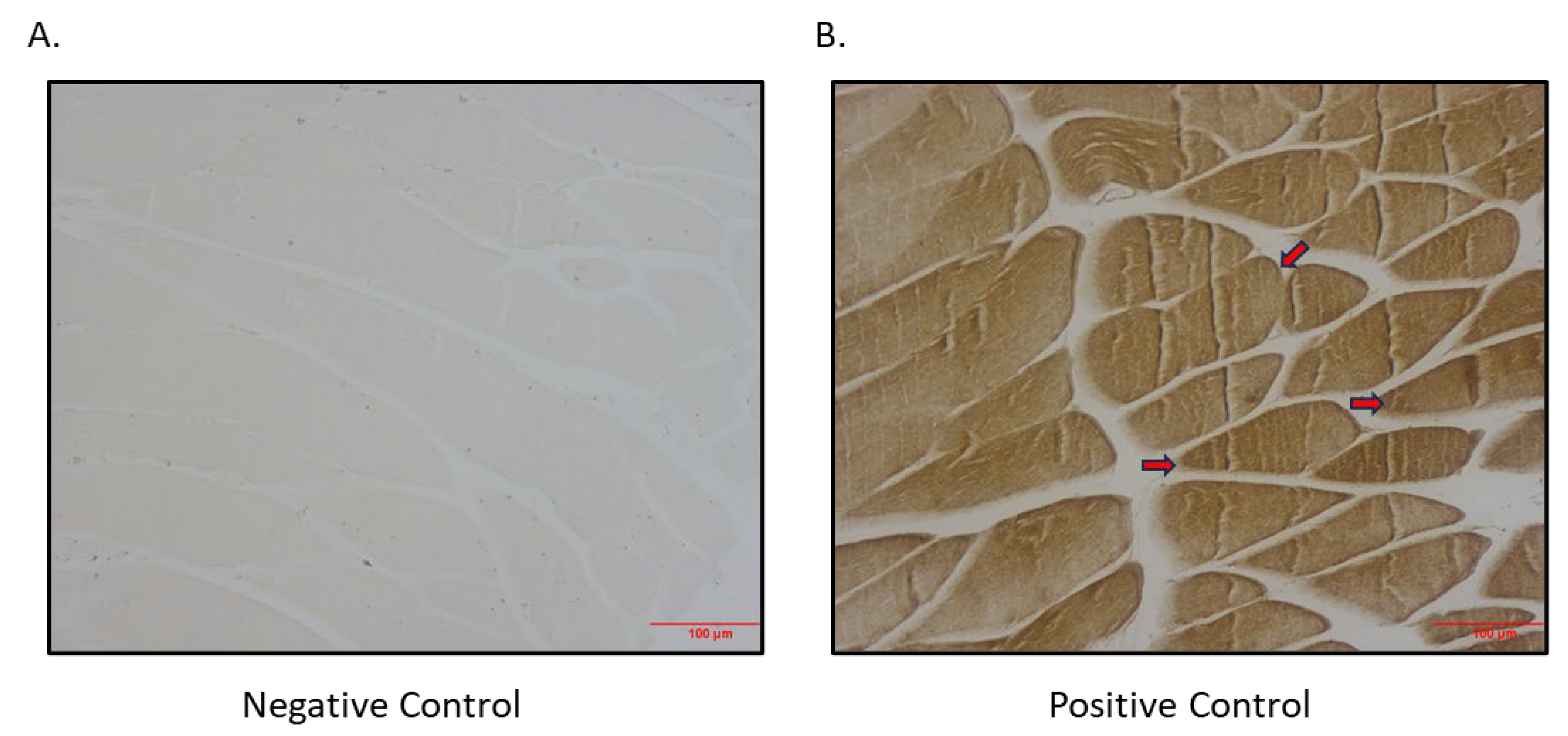
3.2. Skeletal muscle is a novel source of SGLT1 protein.
3.2.1. Immunocytochemistry staining of differentiated L6 skeletal muscle cells and quadricep muscle shows SGLT1 protein expression.
As SGLT2 is expressed in skeletal muscle, we aimed to determine if there was also SGLT1 expression in skeletal muscle. We indeed showed that SGLT1 is expressed in differentiated L6 skeletal muscle cells (
Figure 3) and also in quadricep skeletal muscle of mice (
Figure 4).
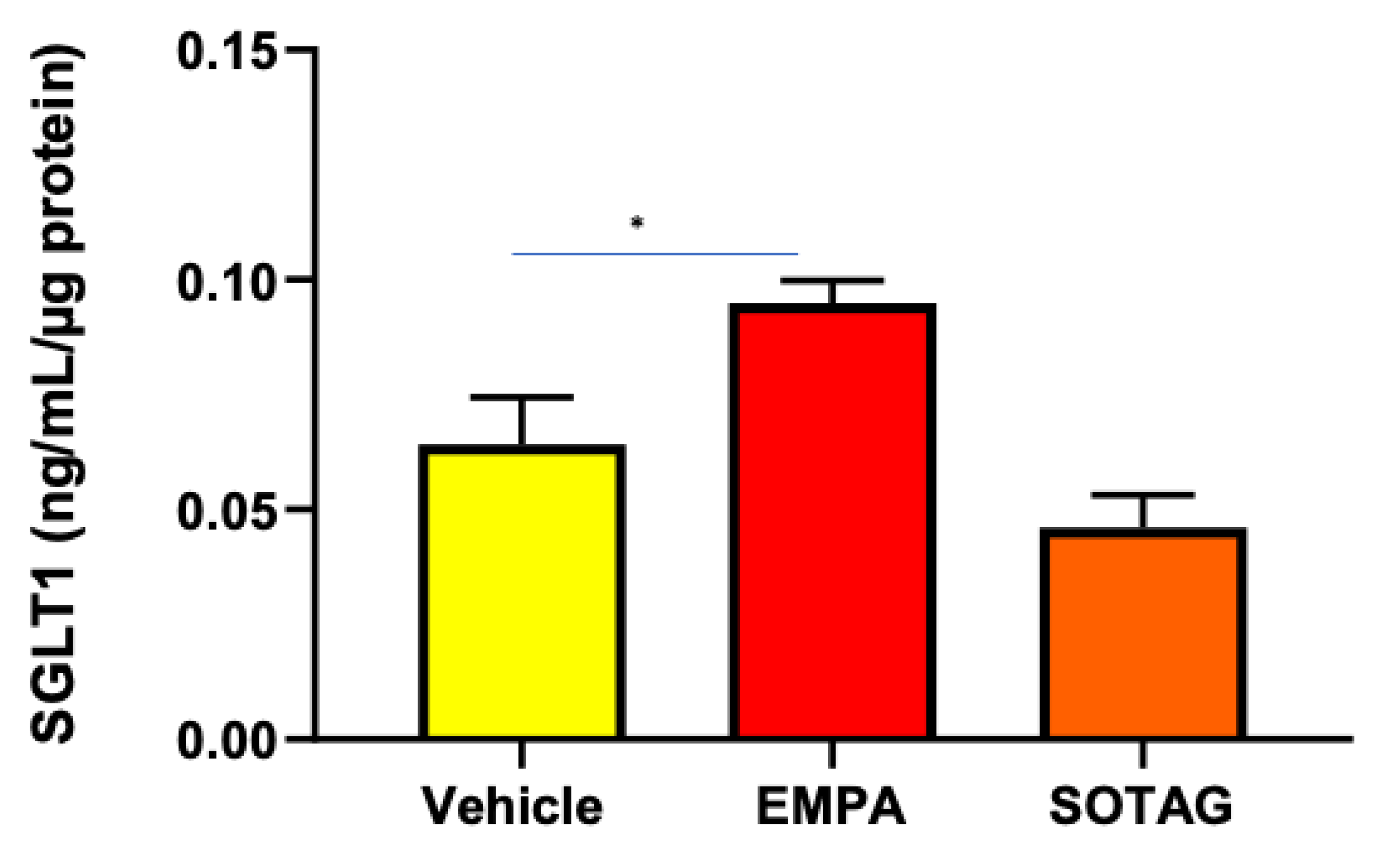
3.2.2. SGLT2 inhibition (SGLT2i) promotes SGLT1 expression in differentiated L6 skeletal muscle cells.
In previous studies, we have shown that SGLT2i produces a compensatory increase in SGLT1 expression in the eye and kidney [
4,
25]. Therefore, we wanted to ascertain if SGLT2i promotes the same phenomenon in skeletal muscle. We discovered that SGLT2i promoted SGLT1 expression in differentiated L6 skeletal muscle cells, while the SGLT1/2i, Sotagliflozin, did not (
Figure 5). The SGLT2i mediated elevation of SGLT1 warrants the utilization of an SGLT1/2i such as Sotagliflozin.
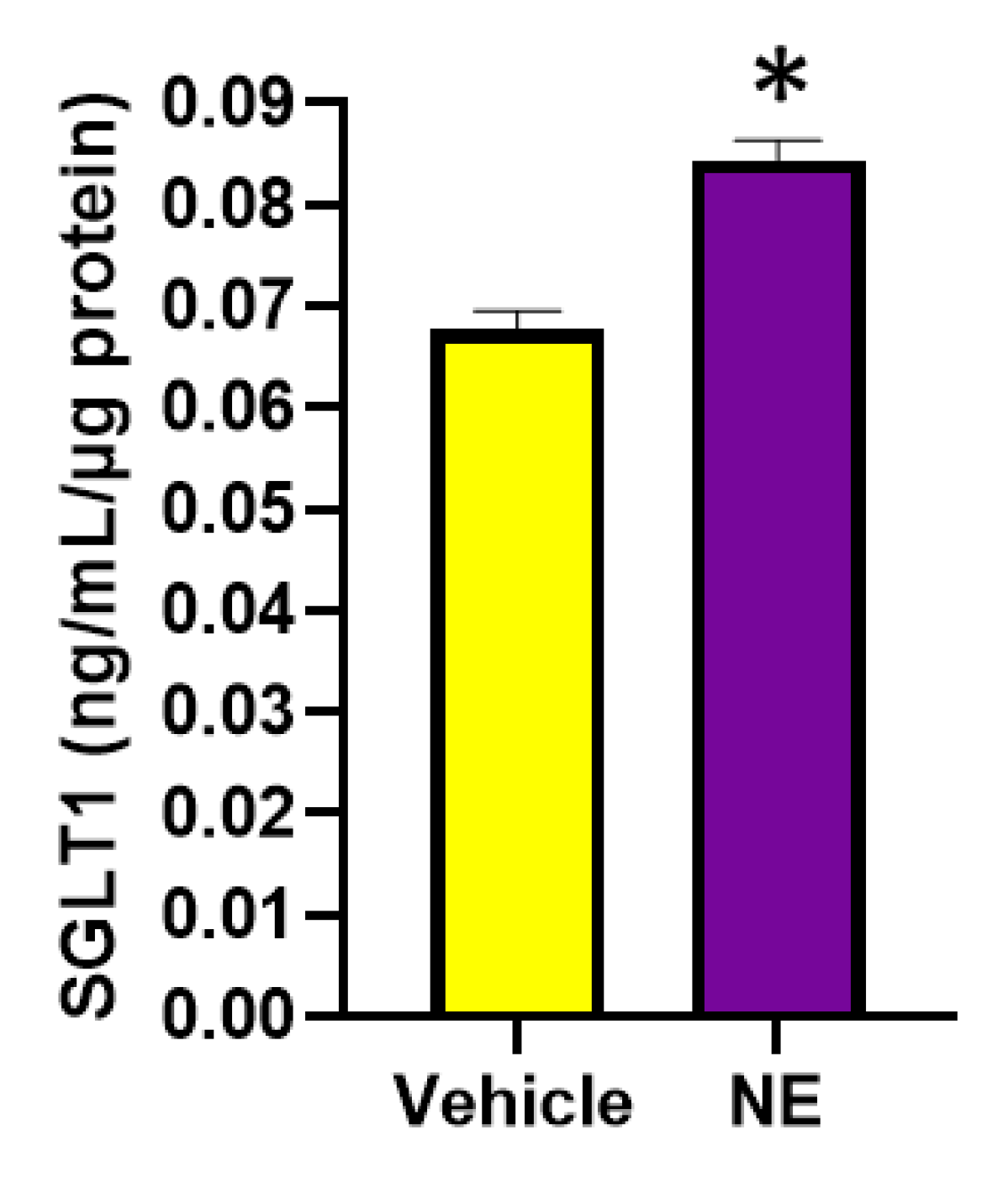
3.2.3. The major neurotransmitter of the SNS, NE, significantly increases SGLT1 levels in differentiated L6 skeletal muscle cells.
We were interested in discovering the mechanisms of SGLT1 regulation as SGLT1 is a therapeutic target in the metabolic syndrome. We aimed to ascertain whether the major neurotransmitter of the SNS, NE, which is increased in hypertension, diabetes and obesity may promote SGLT1 (
Figure 6). Excitingly, this neurotransmitter significantly promoted SGLT1 protein levels in the differentiated L6 skeletal muscle cells.
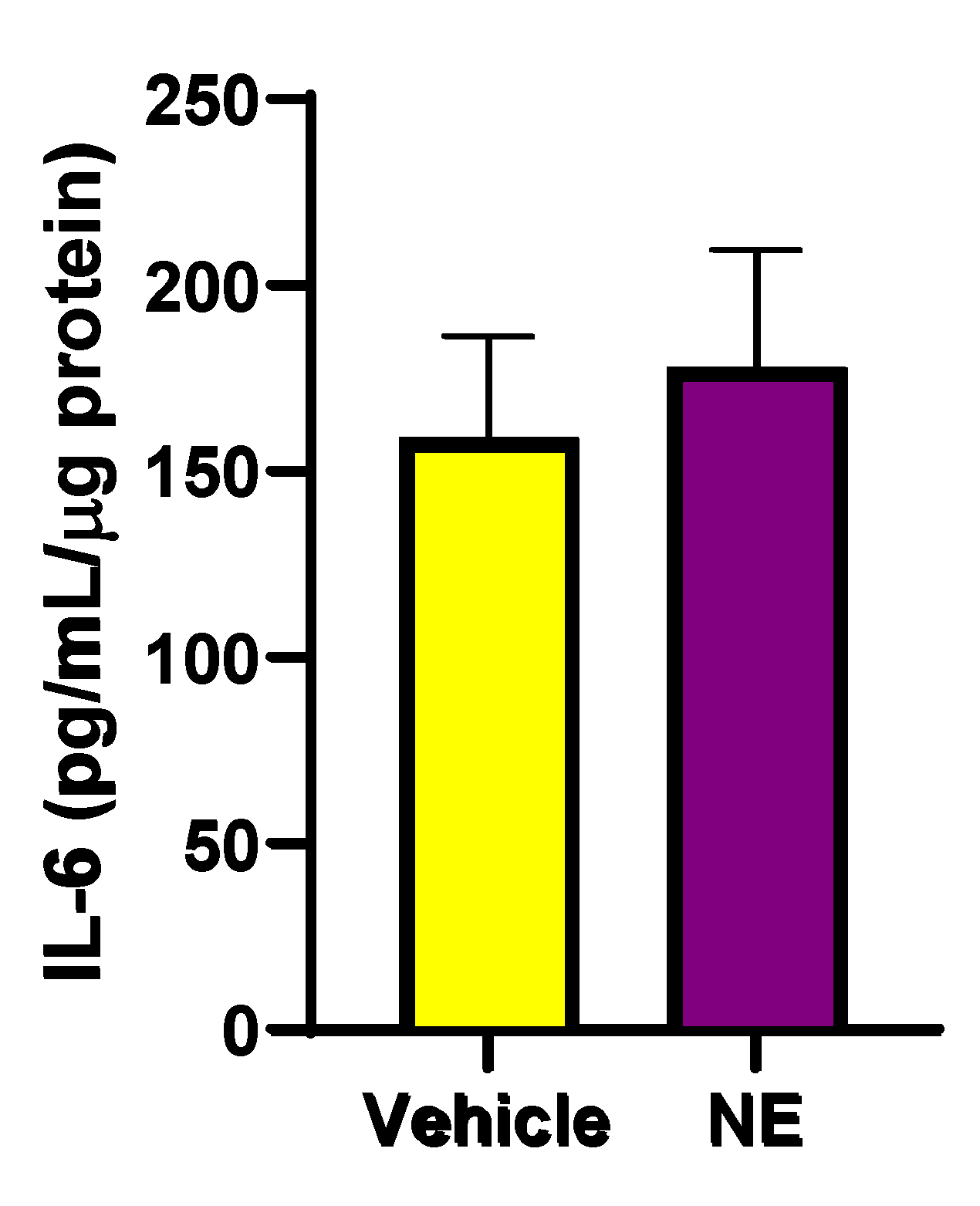
3.2.4. NE promotes an elevation in interleukin-6 (IL-6) levels in differentiated L6 cells.
Previously, it has been shown that the pro-inflammatory cytokine, IL-6, increases SNS activity [
27], which may increase SGLT1 and SGLT2 levels in human proximal tubule cells [
9,
16]. In addition, IL-6 may directly increase SGLT1 levels [
16]. We aimed to determine if NE increases IL-6 levels, which may possibly be upstream of elevated SGLT1 expression. In
Figure 7, we demonstrate that NE does result in a trend for elevated IL-6 levels in differentiated skeletal muscle cells.
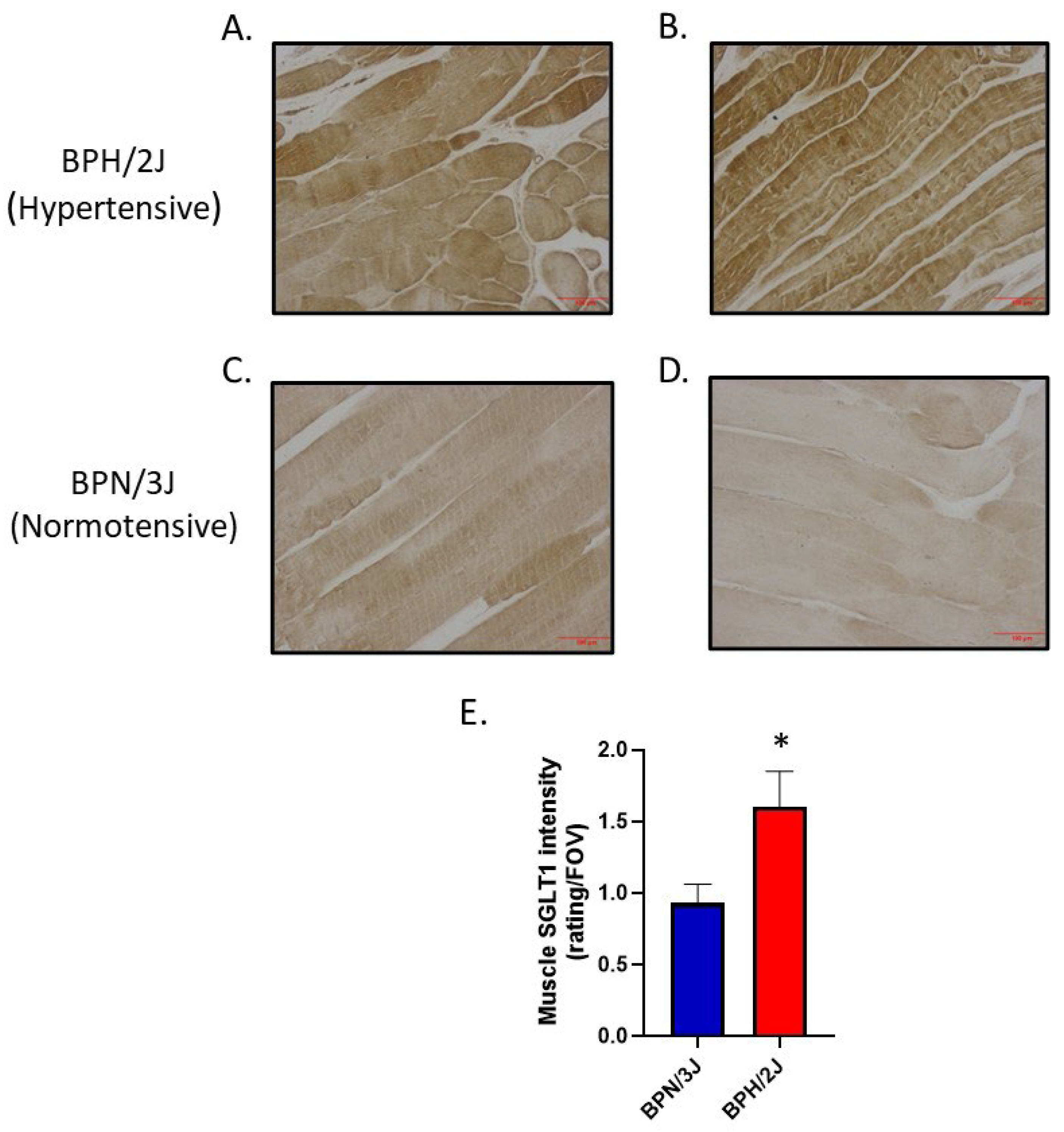
3.3. Determination of significantly increased SGLT1 in skeletal muscle of neurogenically hypertensive mice (BPH/2J): functional implications on high blood pressure.
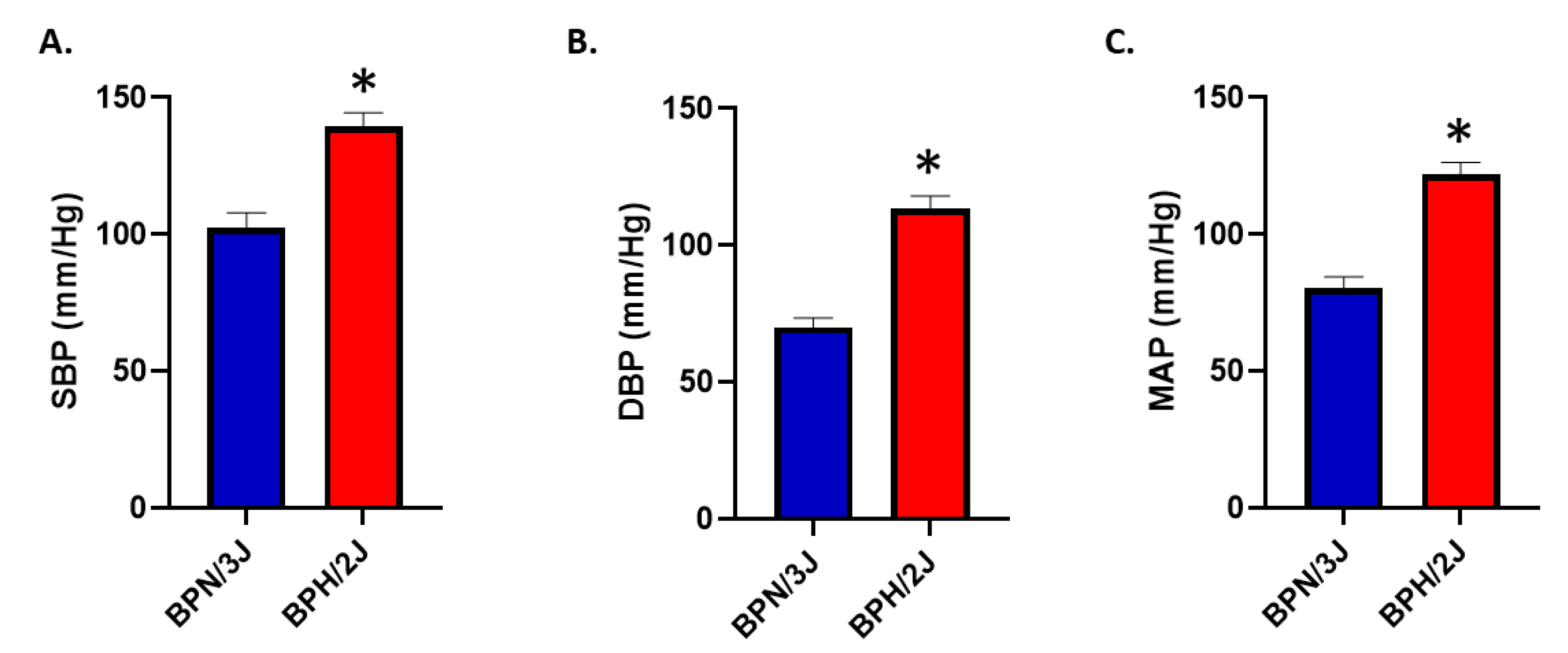
3.3.1. BPH/2J hypertensive mice have significantly higher blood pressures than BPN/3J normotensive mice.
We have previously shown that neurogenically hypertensive (BPH/2J) mice display increased SNS activation, in numerous tissues such as the heart and kidney [
24]. We confirmed in an independent cohort of normotensive (BPN/3J) and neurogenically hypertensive (BPH/2J) mice that BPH/2J mice demonstrated increased systolic blood pressure (SBP;
Figure 8A), diastolic blood pressure (DBP;
Figure 8B) and mean arterial pressure (MAP;
Figure 8C) compared to BPN/3J mice.
3.3.2. Are SGLT1 protein levels positively regulated by sympatho-excitation in skeletal muscle in vivo?
We utilised our BPH/2J (sympathoexcitation mouse) and BPN/3J (normal SNS activity) mouse model to determine if the activation of the sympathetic nervous system increases SGLT1 protein. We demonstrated that SGLT1 is significantly increased in quadricep skeletal muscle of our BPH/2J hypertensive mice compared to our normotensive BPN/3J mice (
Figure 9).
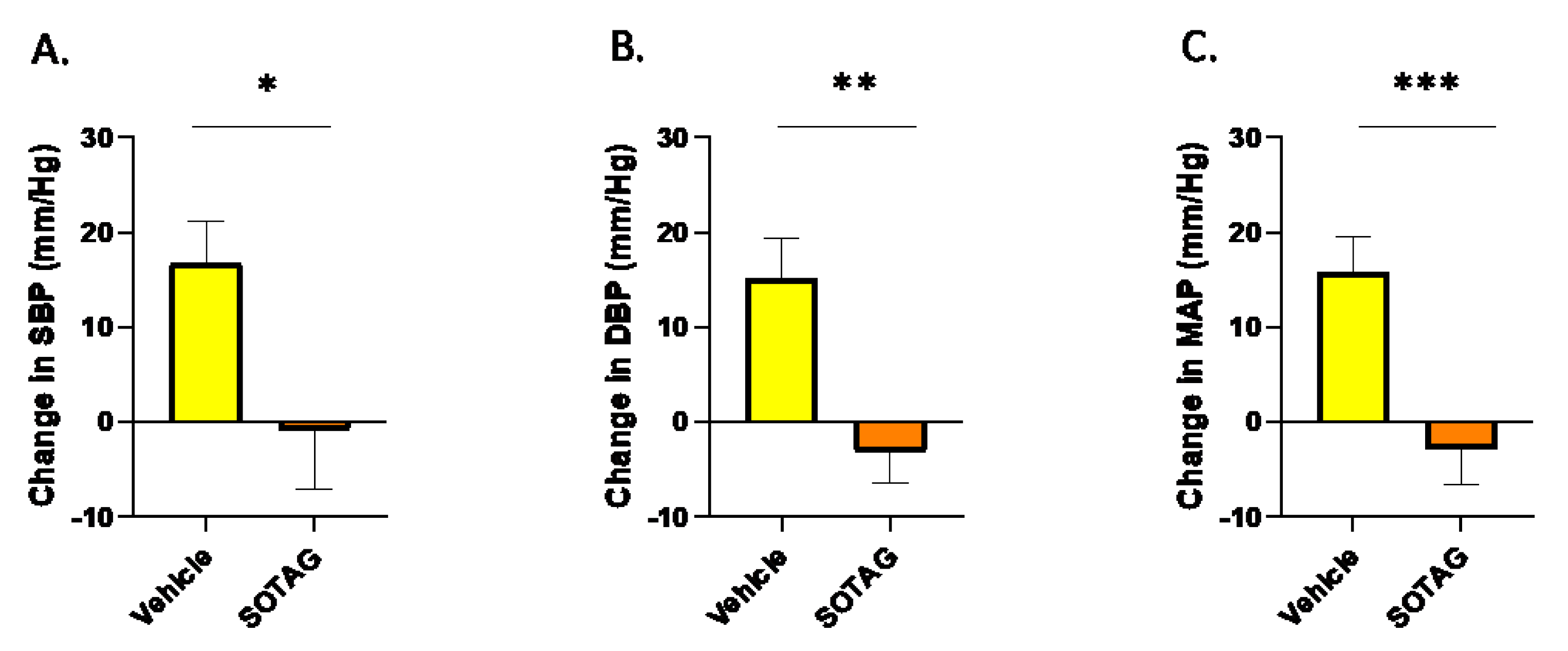
3.3.3. Inhibition of SGLT1 and 2 with Sotagliflozin lowers high blood pressure.
After determining that SGLT1 is increased in skeletal muscle of the hypertensive mouse model, we set out to ascertain the effect that the SGLT1/2 inhibitor has on high blood pressure which is evident in our neurogenically hypertensive BPH/2J mouse strain. We discovered that Sotagliflozin (SOTAG) significantly lowered the Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) and Mean Arterial Pressure (MAP) after two weeks of therapy administered in drinking water (
Figure 10).
4. Discussion
Hypertension and diabetes are chronic conditions that cumulatively affect more than 2 billion people globally every year [
28,
29]. Blood glucose levels and blood pressure are regulated by the SNS via the regulation of kidney function and peripheral vasculature tone. Hyperactivation of the SNS can lead to diabetes or hypertension as the mechanisms of regulation would be dysregulated [
30]. Similarly, the interplay between obesity and hypertension is evident since obesity dysregulates the SNS by increasing renal SNS activity [
30]. This in turn, affects the renin-angiotensin-aldosterone system and overall increases sodium retention [
31]. The high incidence, mortality rates and conditions associated with both diseases have instigated a vast amount of research regarding the management and treatment of these diseases.
It is clear that SGLT1 is expressed at a much higher level than SGLT2 in skeletal muscle. This aligns well with the tissue distribution of both proteins. Tissue distribution of SGLT1 is much greater than SGLT2. SGLT2 protein is only expressed in the proximal tubule cells of the kidneys and the eyes and we have now demonstrated for the first time it’s occurrence in the skeletal muscle at a low but biologically functional level. In contrast, SGLT1 is more widely expressed throughout the body in organs including the small intestine, eyes, kidney, heart and skeletal muscle. This difference in expression between SGLT1 and SGLT2 could be due to tighter transcriptional regulation of the
Sglt2 gene. Tissue specific nucleosome occupancy has already been shown to play an important role in the differential regulation of
Sglt2 gene expression in various tissues [
32]. This suggests that it is likely, that compared to the
Sglt1 gene in the skeletal muscle, the DNA for the
Sglt2 gene in skeletal muscle may be more tightly wound around it’s supporting proteins to form chromatin and this could affect the genes availability for transcription [
32]
. Additionally, the transcription factors for the
Sglt2 gene such as C-Maf [
33] may not be present in many tissues which may explain the limited expression of SGLT2 in the body.
There is a vast amount of evidence highlighting that the SGLT2i’s, Dapagliflozin and Empagliflozin, both promote metabolic benefits in skeletal muscle. Dapagliflozin promotes an improvement in fatty acid and ketone metabolism, as well as a reduction in glycolytic flux [
34], while Empagliflozin improves insulin sensitivity [
35] and enhances fatty acid oxidation [
36] within the skeletal muscle. Prior to our study, it may have been believed that these benefits were attributed to crosstalk between tissues. In our current study, we now show that SGLT2i is likely to be having a direct effect in skeletal muscle as the target protein SGLT2 is expressed at the protein level.
There are two main family members of the SGLT family, SGLT1 and SGLT2. When focusing on SGLT1 and SGLT2, the former is more novel and hence less is known about the regulation of this protein. Meanwhile, SGLT2 has been widely studied for decades. Research has shown that upon SNS overactivity, which may occur in conditions such as diabetes and hypertension, the function and expression of SGLT2 is dysregulated. Rafiq et al. (2015) demonstrated that NE, which is the major neurotransmitter of the SNS, may increase
Sglt2 mRNA (37). However, SGLT2 protein was not assessed. Our study, Matthews et al. (2017), displayed for the first time that SGLT2 protein expression can be positively regulated by the SNS in human proximal tubule cells (HK2) [
9]. With these findings in mind, our current study aimed to determine whether the activity of the SNS also influenced SGLT1 expression, but in the context of skeletal muscle. Our study demonstrated that neurogenically hypertensive mice possessed an elevated level of SGLT1 protein in the skeletal muscle. However, it was not known if elevated levels of NE were responsible for the increased SGLT1 in this tissue. We conducted
in vitro studies to assess whether NE may directly upregulate SGLT1 in skeletal muscle L6 cells. We did indeed show that NE promotes significantly increased SGLT1 expression in differentiated skeletal muscle L6 cells. This is not the first time that we have shown that NE can increase SGLT1. We have also demonstrated this to be the case in the context of human proximal tubule cells [
16].
Various approaches are available to treat hypertension. Moxonidine is a pharmacotherapeutic anti-hypertensive drug. It reduces peripheral sympathetic activity and thus decreases peripheral vascular resistance [
38]. Renal Denervation is a surgical procedure that utilises radiofrequency ablation to ablate renal nerves [
39]. It suppresses SNS activity, thereby decreasing blood pressure and renal glucose reabsorption [
39]. This demonstrates that the dysregulation of the SNS can be managed by appropriate medical treatment. Based on our results, it would be expected that Moxonidine would decrease both SGLT1 and SGLT2 in numerous organs as it is a systemic therapy.
As it is critical to translate our findings into humans, future studies should aim to determine whether SGLT1 and SGLT2 protein is expressed in human skeletal muscle. It would be highly informative to determine if SGLT1 and SGLT2 is upregulated in diabetic and/or hypertensive patients where the SNS is hyperactivated. If the SGLT1 and SGLT2 protein is upregulated in these conditions, it would support our current pre-clinical findings and substantiate the use of the SGLT1/2i SOTAG or Moxonidine in these conditions.
5. Conclusion
In this current paper, our findings suggest that SNS activity upregulates the therapeutic target, SGLT1 in skeletal muscle, potentially worsening cardiometabolic control. As clinical trial data suggests cardiorenal benefits with SGLT2i, future studies should aim to utilize sole SGLT1i which may offer a therapeutic strategy for conditions with heightened SNS activity, such as hypertension, diabetes and obesity.
Author Contributions
Conceptualization, J.R.M., L.Y.H., M.P.S. and V.B.M.; formal analysis, J.R.M., L.Y.H., M.P.S. and V.B.M.; funding acquisition, M.P.S., V.B.M., J.R.M. and L.Y.H.; investigation, J.R.M., L.Y.H., M.P.S. and V.B.M.; writing—original draft, J.R.M., L.Y.H., M.P.S. and V.B.M.; writing—review and editing, J.R.M., L.Y.H., M.P.S and V.B.M. All authors have read and agreed to the published version of the manuscript.
Funding
Funding from the Royal Perth Hospital Research Foundation to the Dobney Chair Professor Markus Schlaich (Dobney Chair Funds) and Dr Vance Matthews (SEED 244/2023). Royal Perth Hospital Research Foundation Fellowship to Dr Lakshini Y Herat ID CAF 133/2020.
Institutional Review Board Statement
All experimental and animal handling activities were performed at the Harry Perkins Institute for Medical Research animal holding facility (Perth, WA, Australia) according to the guidelines of the Institutional Animal Care and Use Committee. Animal ethics approval (AE284) was received from the Harry Perkins Institute for Medical Research Animal Ethics Committee.
Data Availability Statement
The data presented in this study are available on request from authors.
Acknowledgments
We thank Ozgene Animal Resources Centre (Murdoch, Western Australia) and the Bioresources, Harry Perkins Institute of Medical Research (Nedlands, Western Australia) for providing animal care services. We would like to thank Sofia Cortes Villescas for assistance with preliminary work. .
Conflicts of Interest
Prof. Schlaich has received research support from Medtronic, Abbott, Novartis, Servier, Pfizer and Boehringer Ingelheim. All other authors declare no conflict of interest.
References
- Frontera, W.; Ochala, J. Skeletal Muscle: A Brief Review of Structure and Function. Calcif Tissue Int. 2015, 96, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, B.; Young, M.; Nakamura, N.; Ha, H.; Carter, L.; Pitts, W.; Torres, D.; Noh, H.; Suk, S.; Kim, J.; Polgar, N. Disrupted glucose homeostasis and skeletal muscle-specific glucose uptake in an exocyst knockout mouse model. J Biol Chem. 2021, 296, 100482. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Williams, S.; Ho, S.; Loraine, H.; Hagan, D.; Whaley, J.; Feder, J. Quantitative PCR tissue expression profiling of the human SGLT2 gene and related family members. Diabetes Ther. 2010, 1, 57–92. [Google Scholar] [CrossRef] [PubMed]
- Herat, L.; Matthews, J.; Ong, W.; Rakoczy, E. , Schlaich, M.; Matthews, V. Determining the Role of SGLT2 Inhibition with Dapagliflozin in the Development of Diabetic Retinopathy. Front Biosci. 2022, 27, 321. [Google Scholar] [CrossRef]
- Matthews, J.; Herat, L.; Rooney, J.; Rakoczy, E.; Schlaich, M.; Matthews, V. Determining the Role of SGLT2 Inhibition with Empagliflozin in the development of diabetic retinopathy. Biosci Rep. 2022, 42. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.; Yang, P.; Chao, S.; Lee, C.; Huang, J.; Yang, S.; Lin, H. Association of sodium-glucose cotransporter 2 inhibitors with the incidence of corneal diseases in type 2 diabetes mellitus. Int J Med Sci. 2024, 21, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, C.; Wu, T.; Ho, C.; Yeh, T.; Sun, G.; Tseng, C.; Cheng, P. Attenuation of epithelial-mesenchymal transition via SGLT2 inhibition and diabetic cataract suppression by dapagliflozin nanoparticles treatment. Life Sci. 2023, 330, 122005. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.; Woerle, H.; Broedl, U.; Inzucchi, S. ; Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015, 373, 2117–28. [Google Scholar] [CrossRef]
- Matthews, VB.; Elliot, RH.; Rudnicka, C.; Hricova, J.; Herat, L.; Schlaich, MP. Role of the sympathetic nervous system in regulation of the sodium glucose cotransporter 2. J. Hypertens. 2017, 35, 2059–2068. [Google Scholar] [CrossRef]
- Bhatt, D.; Szarek, M.; Steg, P.; Cannon, C.; Leiter, L.; McGuire, D.; Lewis, J.; Riddle, M.; Voors, A.; Metra, M.; Lund, L.; Komajda, M.; Testani, J.; Wilcox, C.; Ponikowski, P.; Lopes, R.; Verma, S.; Lapuerta, P.; Pitt, B. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N Engl J Med. 2020, 384, 117–128. [Google Scholar] [CrossRef]
- Bhatt, D.; Szarek, M.; Pitt, B.; Cannon, C.; Leither, L.; McGuire, D.; Lewis, J.; Riddle, M.; Inzucchi, S.; Kosiborod, M.; Cherney, D.; Dwyer, J.; Scirica, B.; Bailey, C.; Diaz, R.; Ray, K.; Udell, J.; Lopes, R.; Lapuerta, P.; Steg, P. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. N Engl J Med. 2020, 384, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Furuichi, Y.; Kawabata, Y.; Aoki, M.; Mita, Y.; Nobuharu, F.; Manabe, Y. Excess Glucose Impedes the Proliferation of Skeletal Muscle Satellite Cells Under Adherent Culture Conditions. Front Cell Dev Biol. 2021, 1, 640399. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, Y.; Kosaki, K.; Sugasawa, T.; Matsui, M.; Yoshioka, M.; Aoki, K.; Kuji, T.; Mizuno, R.; Kuro-o, M.; Yamagata, K.; Maeda, S.; Takekoshi, K. High Salt Diet Impacts the Risk of Sarcopenia Associated with Reduction of Skeletal Muscle Performance in the Japanese Population. Nutrients. 2020, 12, 3474. [Google Scholar] [CrossRef]
- Wu, Q.; Burley, G.; Li, L.; Shu, L.; Shi, Y. The role of dietary salt in metabolism and energy balance: Insights beyond cardiovascular disease. Diabetes Obes Metab. 2023, 25, 1147–1161. [Google Scholar] [CrossRef] [PubMed]
- Saunders, B., C.; Rudnicka, A.; Filipovska, S.; Davies, N.; Ward, J.; Hricova, M.; Schlaich, V. Matthews. 2018. Shining LIGHT on the metabolic role of the cytokine TNFSF14 and the implications on hepatic IL-6 production. Immunol. Cell Biol. 2018, 96, 41–53. [Google Scholar] [CrossRef]
- Matthews, J.; Hibbs, M.; Herat, L.; Schlaich, M.; Matthews, V. The Sympathetic Nervous System Regulates Sodium Glucose Co-Transporter 1 Expression in the Kidney. Biomedicines. 2023, 11, 819. [Google Scholar] [CrossRef]
- Le, Y.; Yang, J.; Li, F.; Jiang, Y.; Wei, T.; Wang, D.; Wang, K.; Cui, X.; Lin, X.; Yang, K.; Hong, T.; Wei, R. Dapagliflozin improves pancreatic islet function by attenuating microvascular endothelial dysfunction in type 2 diabetes. Diabetes Metab Res Rev. 2023, 39, e3607. [Google Scholar] [CrossRef]
- Pirklbauer, M.; Sallaberger, S.; Staudinger, P.; Corazza, U.; Leierer, J.; Mayer, G.; Schramek, H. Empagliflozin Inhibits IL-1B-Mediated Inflammatory Response in Human Proximal Tubular Cells. Int J Mol Sci. 2021, 22, 5089. [Google Scholar] [CrossRef]
- Davern, P.; Nguyen-Huu, T.-P.; Abdelkader, A.; Head, G. Role of the sympathetic nervous system in Schlager genetically hypertensive mice. Hypertension. 2009, 54, 852–859. [Google Scholar] [CrossRef]
- Schlager, G.; Sides, J. Characterization of hypertensive and hypotensive inbred strains of mice. Lab Anim Sci 1997, 47, 288–292. [Google Scholar]
- Herat, L.; Magno, A.; Kiuchi, M.; Jackson, K.; Carnagarin, R.; Head, G.; Schlaich, M.; Matthews, V. The Schlager Mouse as a model of altered retinal phenotype. Neural Regen Res. 2020, 15, 512–518. [Google Scholar] [CrossRef]
- Chiu, C.; Jackson, K.; Hearn, N.; Steiner, N.; Head, G.; Lind, J. Identification of genes with altered expression in male and female Schlager hypertensive mice. BMC Med Genet. 2014, 15, 101–106. [Google Scholar] [CrossRef]
- Grassi, G.; Arenare, F.; Pieruzzi, F.; Brambilla, G.; Mancia, G. Sympathetic activation in cardiovascular and renal disease. J Nephrol. 2009, 22, 190–195. [Google Scholar]
- Herat, L.; Magno, A.; Rudnicka, C.; Hricova, J.; Carnagarin, R.; Ward, N.; Arcambal, A.; Kuichi, M.; Head, G.; Schlaich, M.; Matthews, V. SGLT2 Inhibitor-Induced Sympathoinhibition: A Novel Mechanism for Cardiorenal Protection. JACC Basic Transl. Sci. 2020, 5, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Herat, L.; Matthews, J.; Hibbs, M.; Rakoczy, E.; Schlaich, M.; Matthews, V. SGLT1/2 inhibition improves glycemic control and multi-organ protection in type 1 diabetes. iScience. 2023, 26, 107260. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Arakawa, K.; Ueta, K.; Matsushita, Y.; Kuriyama, C.; Martin, T.; Du, F.; Liu, Y.; Xu, J.; Conway, B.; Conway, J.; Polidori, D.; Ways, K.; Demarest, K. Effect of Canagliflozin on Renal Threshold for Glucose, Glycemia, and Body Weight in Normal and Diabetic Animal Models. PLoS One. 2012, 7, e30555. [Google Scholar] [CrossRef] [PubMed]
- Helwig, B.; Craig, R.; Fels, R.; Blecha, F.; Kenney, M. Central nervous system administration of interleukin-6 produces splenic sympathoexcitation. Auton Neurosci. 2009, 141, 104–111. [Google Scholar] [CrossRef]
- Mills, K.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Lastra, G.; Syed, S.; Kurukulasuriya, L.; Monrique, C.; Sowers, J. Type 2 diabetes mellitus and hypertension: an update. Endocrinol Metab Clin North Am. 2014, 43, 103–122. [Google Scholar] [CrossRef]
- Joyner, M.; Charkoudian, N.; Wallin, B. Sympathetic nervous system and blood pressure in humans: individualized patterns of regulation and their implications. Hypertension. 2010, 56, 10–6. [Google Scholar] [CrossRef]
- Kalil, G.; Haynes, W. Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens Rep. 2012, 35, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Takesue, H.; Hirota, T.; Tachimura, M.; Tokashiki, A.; Ieiri, I. Nucleosome Positioning and Gene Regulation of the SGLT2 Gene in the Renal Proximal Tubular Epithelial Cells. Mol Pharmacol. 2018, 94, 953–962. [Google Scholar] [CrossRef] [PubMed]
- Fujino, M.; Morito, N.; Hayashi, T.; Ojima, M.; Ishibashi, S.; Kuno, A.; Koshiba, S.; Yamagata, K.; Takahashi, S. Transcription factor c-Maf deletion improves streptozotocin – induced diabetic nephropathy by directly regulating Sglt2 and Glut2. JCI Insight. 2023, 8, e163306. [Google Scholar] [CrossRef] [PubMed]
- Kamp, Y.; Gemmink, A.; Ligt, M.; Dautzenberg, B.; Kornips, E.; Jorgensen, J.; Schaart, G.; Esterline, R.; Pava, D.; Hoeks, J.; Schrauwen-Hinderling, V.; Kersten, S.; Havekes, B.; Koves, T.; Muoio, D.; Hesselink, M.; Oscarsson, J.; Phielix, E.; Schrauwen, P. Effects of SGLT2 inhibitor dapagliflozin in patients with type 2 diabetes on skeletal muscle cellular metabolism. Mol Metab. 2022, 66, 101620. [Google Scholar] [CrossRef] [PubMed]
- Goto, Y.; Otsuka, Y.; Ashida, K.; Nagayama, A.; Hasuzawa, N.; Iwata, S.; Hara, K.; Tsuruta, M.; Wada, N.; Motomura, S.; Tajiri, Y.; Nomura, M. Improvement of skeletal muscle insulin sensitivity by 1 week of SGLT2 inhibitor use. Endocr Connect. 2020, 9, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Nagata, N.; Nagashimada, M.; Zhuge, F.; Ni, Y.; Chen, G.; Mayoux, E.; Kaneko, S.; Ota, T. SGLT2 Inhibition by Empagliflozin Promotes Fat Utilization and Browning and Attenuates Inflammation and Insulin Resistance by Polarizing M2 Macrophages in Diet-induced Obese Mice. EBioMedicine. 2017, 20, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Rafiq, K.; Fujisawa, Y.; Sherajee, S.; Rahman, A.; Sufiun, A.; Kobori, H.; Koepsell, H.; Mogi, M.; Horiuchi, M.; Nishiyama, A. Role of the renal sympathetic nerve in renal glucose metabolism during the development of type 2 diabetes in rats. Diabetologia. 2015, 58, 2885–2898. [Google Scholar] [CrossRef] [PubMed]
- Minushkina, L. Possibilities of the use of moxonidine in the treatment of arterial hypertension in patients with metabolic syndrome and diabetes. Kardiologiia. 2011, 51, 74–78. [Google Scholar] [PubMed]
- Schlaich, M.; Sobotka, P.; Krum, H.; Whitbourn, R.; Walton, A.; Esler, M. Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension. 2009, 54, 1195–1201. [Google Scholar] [CrossRef]
Figure 1.
Immunocytochemistry detection of SGLT2 protein in differentiated L6 cells. (A) Negative Control (primary antibody omitted); (B) Positive Control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale Bars: 100 μm.
Figure 1.
Immunocytochemistry detection of SGLT2 protein in differentiated L6 cells. (A) Negative Control (primary antibody omitted); (B) Positive Control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale Bars: 100 μm.
Figure 2.
Immunohistochemical detection of SGLT2 in quadricep skeletal muscle of BPH/2J mice. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining). Magnification 200x; Scale bar: 100 μm.
Figure 2.
Immunohistochemical detection of SGLT2 in quadricep skeletal muscle of BPH/2J mice. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining). Magnification 200x; Scale bar: 100 μm.
Figure 3.
Immunocytochemical detection of SGLT1 in differentiated L6 skeletal muscle cells. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale bar: 100 μm.
Figure 3.
Immunocytochemical detection of SGLT1 in differentiated L6 skeletal muscle cells. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale bar: 100 μm.
Figure 4.
Immunohistochemical detection of SGLT1 expression in quadricep skeletal muscle of BPH/2J mice. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale Bar: 100 μm.
Figure 4.
Immunohistochemical detection of SGLT1 expression in quadricep skeletal muscle of BPH/2J mice. (A) Negative control (primary antibody omitted); (B) Positive control (primary antibody added; arrows indicate brown staining); Magnification 200x; Scale Bar: 100 μm.
Figure 5.
SGLT1 protein levels are elevated in differentiated L6 skeletal cells following SGLT2i. Cells were treated with vehicle, EMPA or SOTAG after 7 days of differentiation; data represented as mean + SEM; n = 4/group; *p=0.036.
Figure 5.
SGLT1 protein levels are elevated in differentiated L6 skeletal cells following SGLT2i. Cells were treated with vehicle, EMPA or SOTAG after 7 days of differentiation; data represented as mean + SEM; n = 4/group; *p=0.036.
Figure 6.
SGLT1 protein levels are significantly elevated following NE (10μM) treatment of differentiated L6 cells. SGLT1 levels were measured in whole cell lysates, 48 hours post treatment; data represented as mean + SEM; n=3-5/group; *p<0.001.
Figure 6.
SGLT1 protein levels are significantly elevated following NE (10μM) treatment of differentiated L6 cells. SGLT1 levels were measured in whole cell lysates, 48 hours post treatment; data represented as mean + SEM; n=3-5/group; *p<0.001.
Figure 7.
IL-6 protein levels are elevated following NE (10μM) treatment of differentiated L6 cells. Whole cell lysates were used for IL-6 determination. Data is represented as mean + SEM; n=3/group.
Figure 7.
IL-6 protein levels are elevated following NE (10μM) treatment of differentiated L6 cells. Whole cell lysates were used for IL-6 determination. Data is represented as mean + SEM; n=3/group.
Figure 8.
BPH/2J mice have significantly higher blood pressures than BPN/3J mice. A. Systolic Blood Pressure (SBP), *p<0.004; B. Diastolic Blood Pressure (DBP), *p<0.001; C. Mean Arterial Pressure (MAP), *p<0.001. n=3-5 mice/group; Blood pressure was determined in 13 week old mice.
Figure 8.
BPH/2J mice have significantly higher blood pressures than BPN/3J mice. A. Systolic Blood Pressure (SBP), *p<0.004; B. Diastolic Blood Pressure (DBP), *p<0.001; C. Mean Arterial Pressure (MAP), *p<0.001. n=3-5 mice/group; Blood pressure was determined in 13 week old mice.
Figure 9.
SGLT1 is significantly elevated in quadricep skeletal muscle of BPH/2J hypertensive mice compared to BPN/3J normotensive mice. (A) and (B) representative images of 2 independent BPH/2J mice; (C) and (D) representative images of 2 independent BPN/3J mice; (E) quantitation of skeletal muscle SGLT1 intensity; 5-8 mice/group; data presented as mean + SEM; p=*0.024.
Figure 9.
SGLT1 is significantly elevated in quadricep skeletal muscle of BPH/2J hypertensive mice compared to BPN/3J normotensive mice. (A) and (B) representative images of 2 independent BPH/2J mice; (C) and (D) representative images of 2 independent BPN/3J mice; (E) quantitation of skeletal muscle SGLT1 intensity; 5-8 mice/group; data presented as mean + SEM; p=*0.024.
Figure 10.
Sotagliflozin significantly lowers high blood pressure in BPH/2J mice after two weeks of therapy. (A) Systolic blood pressure (SBP) *; p=0.044, (B) Diastolic blood pressure (DBP) **; p=0.008, (C) Mean arterial pressure (MAP) ***; p=0.006. n=5 mice per group.
Figure 10.
Sotagliflozin significantly lowers high blood pressure in BPH/2J mice after two weeks of therapy. (A) Systolic blood pressure (SBP) *; p=0.044, (B) Diastolic blood pressure (DBP) **; p=0.008, (C) Mean arterial pressure (MAP) ***; p=0.006. n=5 mice per group.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).