1. Introduction
The clinical management of congenital heart disease (CHD) poses significant challenges owing to its diverse morphologies that vary among individuals [
1,
2,
3,
4,
5]. A comprehensive understanding of anomalous cardiac structures is crucial for successful surgical intervention, if necessary. However, current visualization methods based on cardiac computed tomography or magnetic resonance imaging with volume rendering lack realism as they fail to depict the actual depth of the object. Over the past two decades, three-dimensional (3D) printing has emerged as an important technique in cardiovascular medicine to demonstrate the geometric associations among intra- and extra-cardiac structures [
6,
7,
8,
9,
10]. Recent research has established the utility of 3D-printed heart models (3DPHM) in aiding surgical decision-making in cases where conventional imaging provides inconclusive results [
11]. However, despite the benefits in surgical planning, training, and education, the time and cost of producing 3DPHM hinder their widespread application in the medical field [
12]. Moreover, standardization and quality control processes are required because of the novelty of the technology in medical settings [
13].
Virtual reality (VR) has transformed the medical field by offering innovative solutions for both education and patient care [
14,
15,
16]. VR technology is making a groundbreaking impact in the management and understanding of CHD [
17,
18,
19,
20]. By creating detailed, immersive 3DPHM, VR allows cardiologists and cardiac surgeons to explore the unique anatomical complexities of each patient’s heart condition in a way that was not possible with conventional imaging methods [
21,
22,
23]. This enhanced visualization aids in accurate diagnosis, surgical planning, and simulation, enabling medical professionals to visualize the heart’s structures and plan interventions with unprecedented precision [
24]. For educational purposes, VR serves as an invaluable tool for training medical students and professionals, providing them with a hands-on experience of congenital heart defects without the need for invasive procedures. In addition, VR facilitates an enhanced understanding of CHD by patients and their families, thus fostering clear communication about the condition, treatment options, and expected outcomes. By leveraging the capabilities of VR, healthcare providers can improve surgical outcomes, reduce the risks associated with complex procedures, and enhance the quality of life for patients with CHD [
25].
The introduction of 3D portable document format (PDF) technology in the medical field has revolutionized the sharing and visualization of medical information, offering considerable advantages in diagnostics, patient education, and collaborative care [
26]. Unlike conventional two-dimensional images, 3D PDFs permit the interactive visualization of complex anatomical structures directly within a PDF document. Therefore, healthcare professionals are able to manipulate and examine patient-specific models in three dimensions.
This study aimed to investigate the usefulness and clinical value of four visualization modalities in three different cases of CHD, including ventricular septal defect (VSD), double outlet right ventricle (DORV), and tetralogy of fallot (ToF). The three visualization modalities comprised DICOM (Digital Imaging and Communications in Medicine) images, 3DPHM, 3D VR, and 3D PDF. To determine the clinical value of these four visualization modalities, cardiologists and cardiac surgeons were invited to compare their usefulness in presurgical planning, medical education, and communication with patients and their families.
2. Materials and Methods
2.1. Generation of Digital Heart Models
Anonymized DICOM formats of cardiac computed tomography angiography (CCTA) images with complex CHD were collected in this study. The Mimics Innovation Suite 22.0 (Materialise, Leuven, Belgium) was used for the postprocessing and segmentation of images. DICOM images were imported into Mimics for segmentation based on thresholding and editing across multiple slices. Voxels within a certain range of Hounsfield units (HU) were isolated via thresholding by selecting different threshold ranges, allowing the creation of different masks to depict various anatomical features. The heart’s blood pool was separated from other structures, with a 2-mm thickness layer applied externally to assist in the heart model’s printing process. 3-Matic software (Materialise HQ) was utilized to repair holes in the digital model using wrap and smooth functions. The STL file was then transferred to MeshMixer for additional modifications. The 3D model was split into a two-part component to inspect the heart’s internal structure and provide a clear view and assessment of each model’s specific defect.
2.2. 3D Printing
STL files were transferred into Objet500 Connex3 (Objective 3D, Stratasys, Melbourne, Victoria, Australia) for printing. The models were printed with a flexible material, Agilus 30 (Objective 3D, Stratasys, Melbourne, Victoria, Australia), which has a shore hardness of 30 A in both clear and black color. The models were printed in two ways, as depicted in
Figure 1. The cost of the whole heart model was approximately AUD 350 each and that of the plane-cut model was approximately AUD 260 each. The printing time was approximately 5 h for each model.
2.3. VR
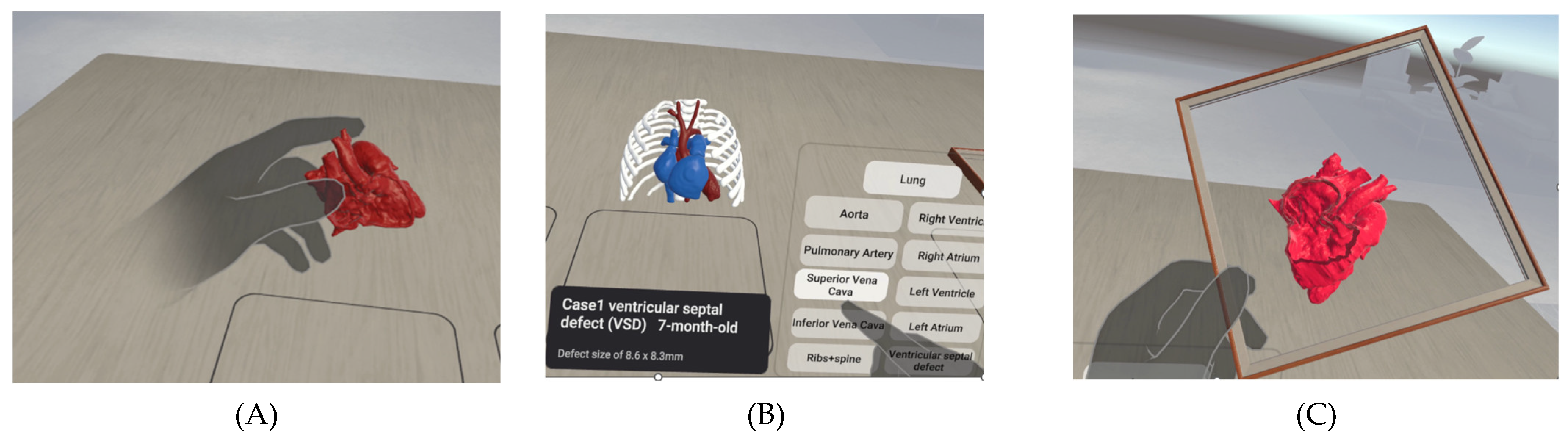
3D VR models were built using Unity 3D (Unity Technologies, San Francisco, California, USA) with C# coding for a different purpose, such as grab. Creating a VR project for the Oculus Quest 2 headset in the context of CHD using Unity involves several key steps to ensure an immersive and educational experience. Initially, the developers must install Unity with the appropriate VR development support packages and the Oculus Integration package from the Unity Asset Store, which includes essential tools, scripts, and prefabs for Oculus VR development. The digital heart model STL file can be imported using advanced 3D modelling software and then imported into Unity. Within Unity, script interactions and animations to simulate various heart conditions using VR hand tracking allows users to manipulate the view or interact with the model to better understand the heart’s structure and function. Implementing user interface elements that provide educational content, such as turning on and off the body part and performing a live plane-cut of the heart, can enhance learning. To ensure a smooth and immersive experience, the VR environment for Oculus Quest 2 must be optimized by considering its processing capabilities to maintain high performance and visual quality. The VR project, including its three main functions, is shown in
Figure 2.
2.4. 3D PDF
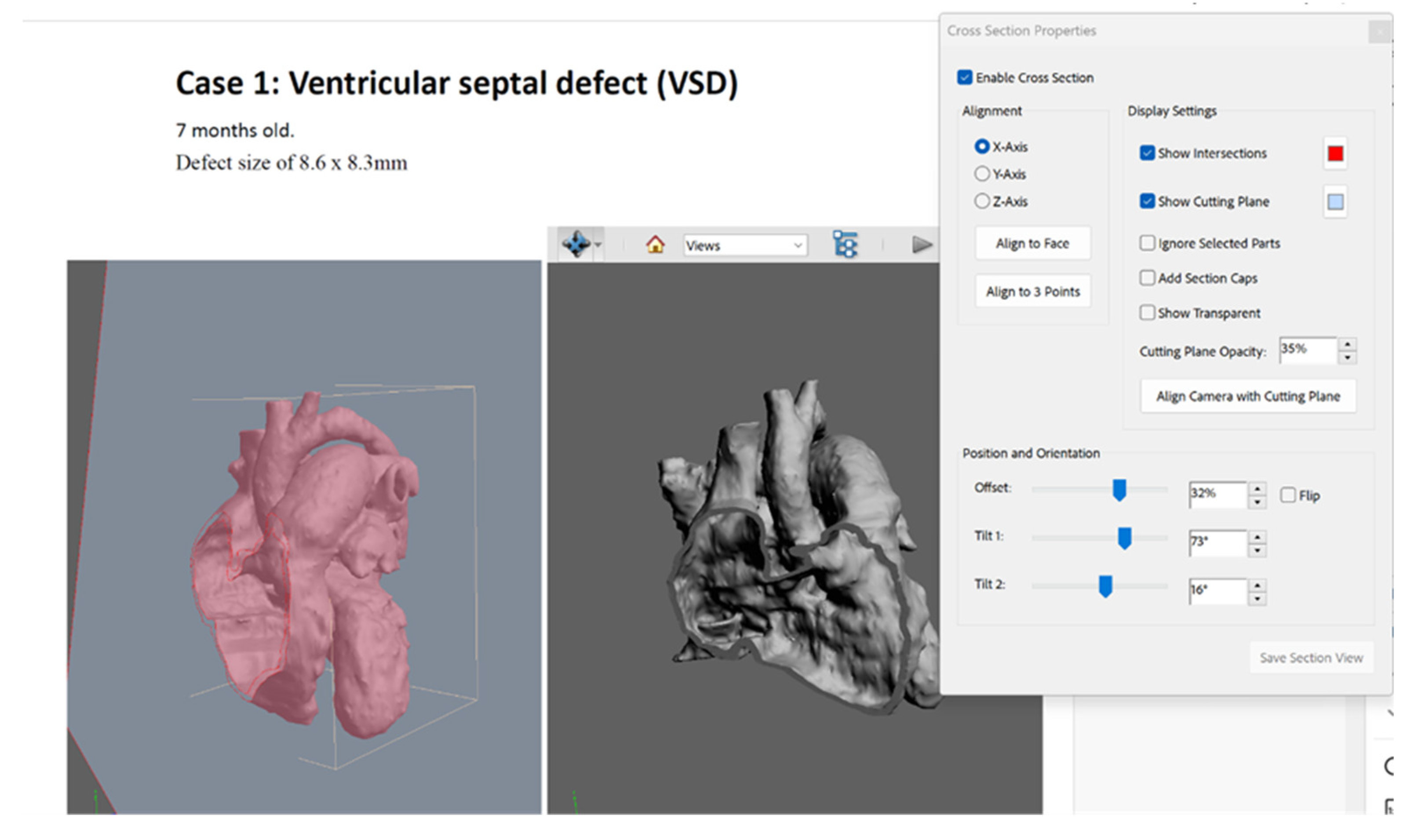
Adobe Acrobat Pro (Adobe Systems Incorporated, San Jose, California, USA) was used to create 3D PDF for the three cases of CHD. The STL file of each case was imported into the PDF file with case detail (
Figure 3), both for whole heart and plane-cut heart. The “Add Default Views” function was used to select the view that allows the participant to visualize the defect in each case. The cross-sectional property function was used to immediately display the cross-section of the 3D model, cutting it in half and looking inside, to determine the axis (x, y, or z) with which the cross-section was aligned.
2.5. Participant Recruitment and Data Collection
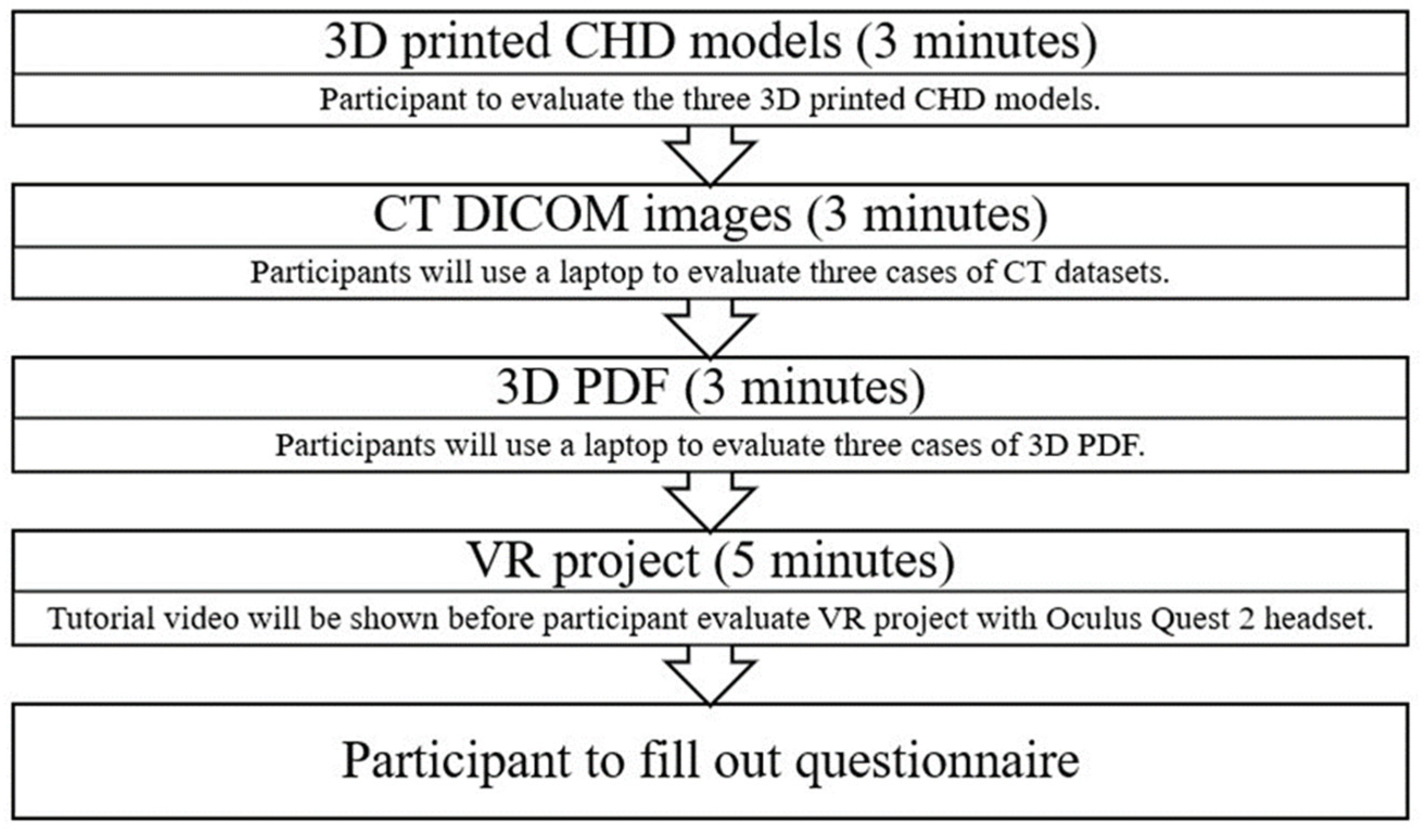
Seventeen cardiac professionals were recruited for this study from public and private hospitals in Western Australia. Each participant was involved in comparing and ranking the usefulness of the four visualization modalities across three different CHD cases, which took approximately 20 min (
Figure 4). The 3DPHMs were printed using the flexible material Agilus30. The DICOM images and 3D PDFs were displayed on a 2D flat screen, whereas the 3D VR experiences were shown via a VR headset. An open-source DICOM viewer, RadiAnt (Medixant, Poznan, Poland), was used by the participants to view the DICOM images of each case on a laptop. Before evaluating the VR project, a tutorial video was shown to provide a better understanding of how to operate it with the VR headset. Questionnaires were distributed after demonstrating the four modalities, with questions based on ranking the usefulness in three major areas, namely, presurgical planning, medical education, and communication with patients and their families. The questionnaire is furnished in Supplementary File 1. Each modality was ranked for each case, with 1 indicating the best and 4 indicating the least rank.
2.6. Statistical Analysis
Quantitative data from the questionnaire were analyzed using IBM SPSS statistical package, version 26 (IBM Corp, Armonk, NY, USA). The normality of the data was evaluated using a normal probability plot, and skewness and kurtosis of the distribution were reported. A p-value of <0.05 was considered statistically significant.
3. Results
Totally, 17 participants were included in this study, of which 12 were men and 11 had 10–20 years of working experience. There were 3 cardiac surgeons, 13 cardiologists, and 1 radiologist (
Table 1).
The mean rank of each modality for each question is presented in
Table 2. The participants were requested to rank the modalities from 1 to 4, with 1 indicating the highest preference. Hence, a mean rank approaching 1 signified a favorable perception of the modality by the participants.
VR was the best modality for assessing the anatomical location and vessels. This method exhibited the lowest mean score across all heart defects, indicating that it provides the most accurate evaluation. 3DPHM and DICOM followed, with 3D PDF being the least effective. Furthermore, VR ranked the highest in spatial association among cardiac structures, with the lowest mean scores, which signifies its superior performance in illustrating spatial relationships. 3DPHM was the most effective modality for visualizing heart defects, with the lowest mean scores. This method was followed by VR, DICOM, and 3D PDF. In learning about pathology, 3DPHM outperformed other modalities, offering the clearest insights into pathology, with the lowest mean scores.
VR was the best presurgical tool, as inferred from its lowest mean scores. 3DPHM, DICOM, and 3D PDF came next, with 3D PDF being the least preferred. For medical education, 3DPHM and VR were highly effective, and both showed lower mean scores than DICOM and 3D PDF, with 3DPHM slightly edging out in certain cases. 3DPHM stood out as the best communication tool, with significantly lower mean scores, indicating its effectiveness.
The quality of visualization is quantified by the mean score, with a rating scale from 1 (well-visualized) to 4 (non-visualized), and the standard deviation (SD) implies the variability in the scores (
Table 3). Across all anatomical structures, VR consistently showed excellent visualization capabilities, with low mean scores and minimal variability. DICOM was also effective, particularly for the aorta and pulmonary artery. 3D printing (3DP) performed well but was not as consistent as VR. 3D PDF was the least effective modality, especially for complex visualizations such as defects.
Table 4 presents the mean scores of different modalities for each question. The participants were requested to rate on a scale of 1–10 for each question, with 10 being the highest score. For presurgical planning, VR was rated as the most useful modality, with a mean score of 8.71 and an SD of 1.1. Thus, this method appears to have high average usefulness, with moderate variability in responses. 3DP followed closely, with a mean of 8.47 and a slightly lower SD of 1.07, alluding a similarly high level of usefulness but with slightly more consistent responses among the participants. In addition, DICOM demonstrated considerable usefulness, with a mean of 7.82 and the lowest SD of 0.95, indicating a more uniform perception among the respondents. 3D PDFs scored significantly lower in usefulness for presurgical planning, with a mean of 5.25 and the highest SD of 1.41, which implies both a lower perceived usefulness and a higher variability in the responses. In the context of educational tools for medical students or junior doctors, VR scored the highest at 9.12, which indicates its effectiveness in providing immersive learning experiences. 3DPHM also scored highly at 8.94, emphasizing its value in tangible learning aids. DICOM, while still useful, scored lower at 7.18, and 3D PDFs were rated the least useful at 4.65, reflecting potentially limited engagement or interactivity compared with other modalities.
Overall, VR and 3DP were consistently valued across both categories for their high engagement and effectiveness in medical education and planning, with VR having a slight advantage. Conversely, 3D PDFs were consistently rated as the least useful modality, which shows that more immersive or tangible technologies are preferred in these contexts.
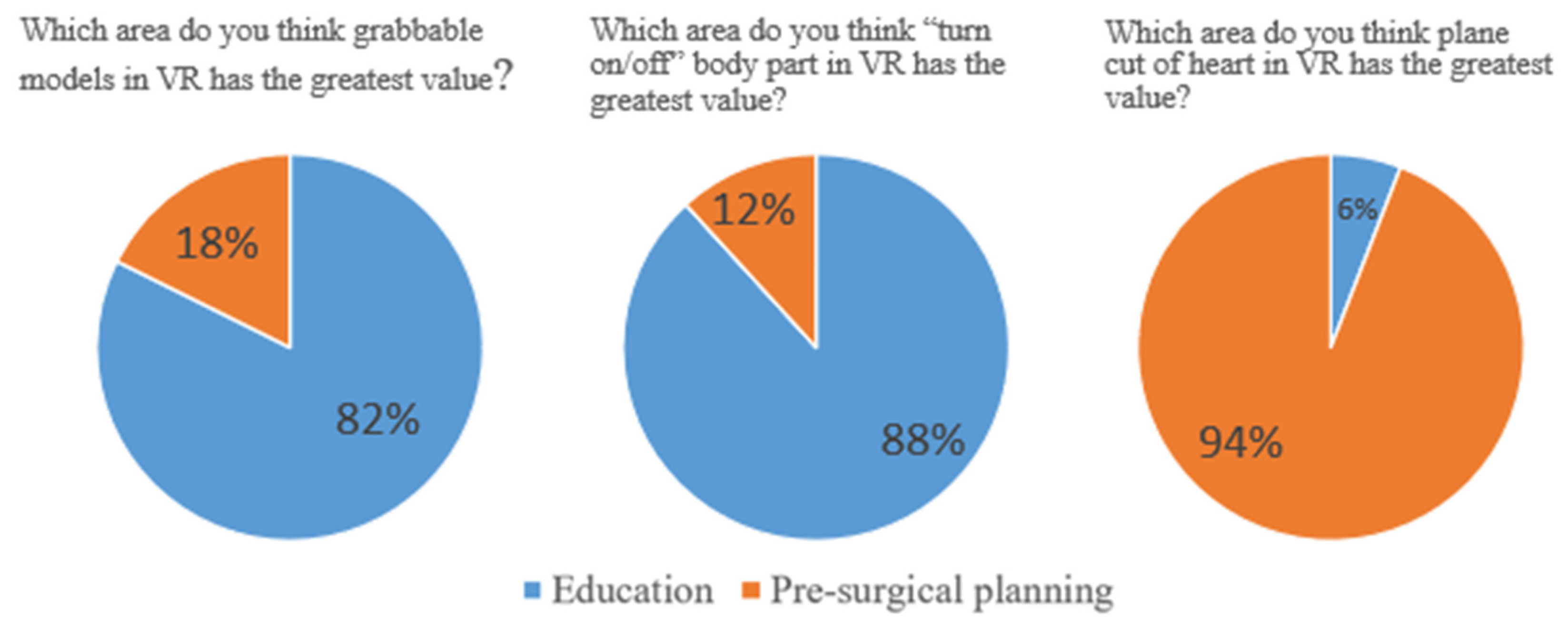
Of the 17 participants, 14 (82%) and 15(88%) opined that the grabble function and turn on/off body part in VR exhibited the greatest value in the education area, respectively. Moreover, 16 (94%) indicated that the live plane-cut function displayed the greatest value in the presurgical planning area (
Figure 5). None of the participants provided “no” as the response to all three questions, which suggests the positive inclination of the participants toward this aspect.
4. Discussion
The results of this study demonstrated the consistent superiority of 3DPHM and VR over 3D PDFs and DICOM in almost all evaluated categories. Feedback from cardiac specialists and physicians regarding the three CHD cases indicated promising outcomes for the four visualization modalities. VR emerged as the leading modality in assessing anatomical locations and vessels across all CHD types, implying its strength in providing clear and detailed visualizations for the accurate identification and understanding of complex heart structures. For comprehending the spatial associations among cardiac structures, VR exhibited superior performance, which showed its capability to offer an immersive experience that can augment the understanding of intricate spatial dynamics within the heart, which is crucial for both diagnostics and surgical planning.
Both VR and 3DPHM performed well in facilitating pathology learning, with VR having a slight edge. This finding highlights the potential of these techniques in medical education, providing interactive and engaging methods for studying and comprehending CHD pathologies. VR proved to be the most effective presurgical planning tool, which emphasizes its value in presurgical preparations owing to the benefit of 3D visualization and simulation. This capability could considerably influence surgical outcomes by enabling the use of precise and informed surgical strategies. In medical education, 3DPHM and VR showed immense promise, with 3DPHM slightly outperforming VR. 3DPHM was the best communication tool, which indicates that physical models are particularly effective in explaining complex cardiac conditions to patients and their families. This modality can enhance patient understanding and involvement in the care process.
The advent of 3DP technology has substantially transformed the landscape of CHD management and has offered innovative approaches for diagnosis, surgical planning, medical education, and patient communication. In their study, Valverde et al. demonstrated that 3DP models of complex CHD cases facilitated an in-depth understanding of anatomical structures, thereby aiding in the identification of optimal surgical pathways and potential complications. These models enable surgeons to simulate and rehearse procedures, which can potentially reduce operative times and improve the surgical precision [
27]. 3DPHM allows students and medical professionals to physically explore cardiac defects, which fosters a more intuitive understanding of congenital anomalies compared with conventional 2D imaging techniques. This interactive learning approach can improve knowledge retention and clinical skills among learners [
28]. Furthermore, 3DPHM models have emerged as a powerful tool for patient education and communication. Healthcare providers can more effectively explain the nature of the disease, the proposed surgical interventions, and the expected outcomes to the patients and their families with the aid of physical models of heart defects. This approach not only enhances patient understanding but also facilitates informed decision-making and augments patient satisfaction with the provided care [
29]. The findings from this investigation suggest that 3DPHM is the best modality for communication with patients and their family.
The ability of VR technology to enhance diagnostic accuracy and surgical planning in CHD has been increasingly recognized. VR enables clinicians to visualize complex cardiac anomalies in ways that were hitherto not possible with standard 2D imaging techniques. Studies by Priya et al. demonstrated that VR-assisted preoperative planning could significantly improve the understanding of anatomical structures, thus aiding in the strategic planning of surgical interventions to potentially reduce operative times and improve patient outcomes [
22]. In Kieu et al. established the role of VR in enhancing the educational experience for medical students and professionals. Thus, VR can facilitate a more intuitive grasp of spatial relationships and surgical techniques, which can enhance the learning outcomes [
17]. A study by Lim et al. reported that VR-based patient education can lead to higher satisfaction rates and better understanding of medical conditions and treatments [
25]. Moreover, studies documented the use of VR for preoperative planning, which allowed surgeons to explore patient-specific anatomy and devise surgical strategies for more precise and effective interventions [
30]. However, the integration of VR in CHD care has its own limitations. Technical limitations, cost implications, and the need for specialized training are some of the factors that prevent its widespread adoption. In addition, there is a growing need for standardized protocols and validation studies to ensure the reliability and accuracy of VR models. In our study, VR was considered as the best modality for presurgical planning as the live plane-cut function allows cardiac professionals to cut open the heart in any angle.
The findings of Lau et al. are similar to ours, with mixed reality models ranking the best in preoperative planning and 3DPHM being the preferred tool in communication with patients [
24]. The difference between the two studies is that our research compared 3D PDF with the other three visualization modalities. Furthermore, the headset and VR environment and function were different. While Oculus Quest 2 was used in this study, HoloLens 2 was utilized in Lau’s study.
This study has certain limitations. First, the allocated time might have been insufficient for a complete evaluation of the modality, which might have potentially led to biased responses from the participants. Second, despite receiving a brief tutorial on the use of 3D PDFs, participants faced challenges in navigating 3D heart models on a flat 2D screen. Finally, the number of participants was small, and sufficient number of cardiac surgeons were not available to assess the clinical value of these modalities. Future studies should seek opinions from more cardiac surgeons to further quantify these benefits and potentially explore the advantage of these tools in other areas of medical diagnosis and treatment for enhancing patient care.
5. Conclusions
The findings from this study have established that of the four visualization modalities, VR is the best tool for assessing the anatomical location and vessels, understanding the spatial relationship among cardiac structures, and presurgical planning. The 3DPHM models are the best tool for medical education and communication. For comprehensive and effective management of CHD, 3DPHM and VR are superior modalities, offering detailed and interactive ways to comprehend and address complex cardiac conditions. These tools hold immense promise for augmenting the outcomes in medical education, surgical planning, and patient communication.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. S1: Questionnaire.
Author Contributions
Conceptualization, S.L. and Z.S.; methodology, S.L., A.S. and Z.S.; formal analysis, S.L.; investigation, S.L., A.S. and Z.S.; data curation, S.L. and Z.S.; writing—original draft preparation, S.L. and Z.S.; writing—review and editing, all authors; visualization, S.L.; supervision, A.S. and Z.S.; project administration, Z.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Human Research Ethics Committee of CURTIN UNIVERSITY (approval number: HRE2018-0799).
Informed Consent Statement
Patient consent was waived due to use of anonymized data for 3D printing purposes with no patient’s information identified.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to express our gratitude to Carley Tillett and Curtin HIVE for their invaluable assistance with the VR project. Additionally, we extend our thanks to medical professionals from the clinical sites for their participation in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Morton, S.U.; Quiat, D.; Seidman, J.G.; Seidman, C.E. Genomic frontiers in congenital heart disease. Nat. Rev. Cardiol. 2021, 19, 26–42. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; He, J.; Shao, X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990-2017. Medicine 2020, 99, e20593. [Google Scholar] [CrossRef]
- Bhatla, P.; Tretter, J.T.; Ludomirsky, A.; Argilla, M.; Latson, L.A. Chakravarti, S.; Barker, PC.; Yoo, S.-J.; McElhinney, DB.; Wake, N. Utility and scope of rapid prototyping in patients with complex muscular ventricular septal defects or double-outlet right ventricle: does it alter management decisions? Pediatr. Cardiol. 2017, 38, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Koniordou, D.; Gasparini, M.; Capelli, C.; Leaver, L.-K.; Khambadkone, S.; Schievano, S.; Taylor, A.M.; Wray, J. Piloting the Use of Patient-Specific Cardiac Models as a Novel Tool to Facilitate Communication During Cinical Consultations. Pediatr. Cardiol. 2017, 38, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Loke, Y.-H.; Harahsheh, A.S.; Krieger, A.; Olivieri, L.J. Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ. 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Squelch, A.; Sun, Z. Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease. Biomolecules 2021, 11, 270. [Google Scholar] [CrossRef] [PubMed]
- Tarca, A.; Woo, N.; Bain, S.; Crouchley, D.; McNulty, E.; Yim, D. 3D Printed Cardiac Models as an Adjunct to Traditional Teaching of Anatomy in Congenital Heart Disease—A Randomised Controlled Study. Hear. Lung Circ. 2023, 32, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Karsenty, C.; Guitarte, A.; Dulac, Y.; Briot, J.; Hascoet, S.; Vincent, R.; Delepaul, B.; Vignaud, P.; Djeddai, C.; Hadeed, K. The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC Med. Educ. 2021, 21:1-8.
- Gomez, A.; Gomez, G.; Simpson, J.; Valverde, I. 3D hybrid printed models in complex congenital heart disease: 3D echocardiography and cardiovascular magnetic resonance imaging fusion. Eur. Hear. J. 2020, 41, 4214. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-A.; Squelch, A.; Jansen, S.; Sun, Z. Optimization of Computed Tomography Angiography Protocols for Follow-Up Type B Aortic Dissection Patients by Using 3D Printed Model. Appl. Sci. 2021, 11, 6844. [Google Scholar] [CrossRef]
- Lau, I.; Wong, Y.H.; Yeong, C.H.; Aziz, Y.F.A.; Sari, N.A.M.; Hashim, S.A.; Sun, Z. Quantitative and qualitative comparison of low- and high-cost 3D-printed heart models. Quant. Imaging Med. Surg. 2018, 9, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Paxton, NC. Navigating the intersection of 3D printing, software regulation and quality control for point-of-care manufacturing of personalized anatomical models. 3D. Print. Med. 2023, 9(1):9.
- Chen, F.-Q.; Leng, Y.-F.; Ge, J.-F.; Wang, D.-W.; Li, C.; Chen, B.; Sun, Z.-L. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef] [PubMed]
- Tene, T.; López, D.F.V.; Aguirre, P.E.V.; Puente, L.M.O.; Gomez, C.V. Virtual reality and augmented reality in medical education: an umbrella review. Front. Digit. Heal. 2024, 6, 1365345. [Google Scholar] [CrossRef] [PubMed]
- Bruno, RR.; Wolff, G.; Wernly, B.; Masyuk, M.; Piayda, K.; Leaver. S.; Erkens, R.; Oehler, R.; Afzal, S.; Heidari, H. Virtual and augmented reality in critical care medicine: the patient’s, clinician’s, and researcher’s perspective. Crit. Care. 2022, 26(1):326.
- Lau, I.; Gupta, A.; Sun, Z. Clinical Value of Virtual Reality versus 3D Printing in Congenital Heart Disease. Biomolecules 2021, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Kieu, V.; Sumski, C.; Cohen, S.; Reinhardt, E.; Axelrod, D.M.; Handler, S.S. The Use of Virtual Reality Learning on Transition Education in Adolescents with Congenital Heart Disease. Pediatr. Cardiol. 2023, 44, 1856–1860. [Google Scholar] [CrossRef] [PubMed]
- Awori, J.; Friedman, S.D.; Howard, C.; Kronmal, R.; Buddhe, S. Comparative effectiveness of virtual reality (VR) vs 3D printed models of congenital heart disease in resident and nurse practitioner educational experience. 3D Print. Med. 2023, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Galeczka, M.; Smerdzinski, S.; Tyc, F.; Fiszer, R. Virtual reality for transcatheter procedure planning in congenital heart disease. Kardiologia Polska 2023, 81, 1026–1027. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.S.; Krishnan, A.; Huang, C.Y.; Spevak, P.; Vricella, L.; Hibino, N.; Garcia, J.R.; Gaur, L. Role of virtual reality in congenital heart disease. Congenit. Hear. Dis. 2018, 13, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Loke, Y.-H.; Mass, P.; Irwin, M.R.; Capeland, C.; Olivieri, L.; Krieger, A. A Novel Virtual Reality Medical Image Display System for Group Discussions of Congenital Heart Disease: Development and Usability Testing. JMIR Cardio 2020, 4, e20633. [Google Scholar] [CrossRef]
- Priya, S.; La Russa, D.; Walling, A.; Goetz, S.; Hartig, T.; Khayat. A.; Gupta, P.; Nagpal, P.; Ashwath, R. From Vision to Reality: Virtual Reality’s Impact on Baffle Planning in Congenital Heart Disease. Pediatr. Cardiol. 2024, 45(1):165-74.
- Kiraly, L.; Shah, N.C.; Abdullah, O.; Al-Ketan, O.; Rowshan, R. Three-Dimensional Virtual and Printed Prototypes in Complex Congenital and Pediatric Cardiac Surgery—A Multidisciplinary Team-Learning Experience. Biomolecules 2021, 11, 1703. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Gupta, A.; Ihdayhid, A.; Sun, Z. Clinical Applications of Mixed Reality and 3D Printing in Congenital Heart Disease. Biomolecules 2022, 12, 1548. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.R.; Wilson, H.C.; Axelrod, D.M.; Werho, D.K.; Handler, S.S.; Yu, S.; Afton, K.; Lowery, R.; Mullan, P.B.; Cooke, J.; et al. Virtual reality curriculum increases paediatric residents’ knowledge of CHDs. Cardiol. Young- 2022, 33, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Eroğlu, F.S.; Erkan, B.; Koyuncu, S.B.; Komşal, Z.R.; Çiçek, F.E.; Ülker, M.; Toklu, M.E.; Atlan, M.; Kıyak, Y.S.; Kula, S.; et al. Effectiveness of using 2D atlas and 3D PDF as a teaching tool in anatomy lectures in initial learners: a randomized controlled trial in a medical school. BMC Med Educ. 2023, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Valverde, I.; Gomez-Ciriza, G.; Hussain, T.; Suarez-Mejias, C.; Velasco-Forte, M.N.; Byrne, N.; Ordoñez, A.; Gonzalez-Calle, A.; Anderson, D.; Hazekamp, M.G.; et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur. J. Cardio-Thoracic Surg. 2017, 52, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Wong, Y.H.; Yeong, C.H. Patient-Specific 3D-Printed Low-Cost Models in Medical Education and Clinical Practice. Micromachines 2023, 14, 464. [Google Scholar] [CrossRef] [PubMed]
- Traynor, G.; Shearn, A.I.; Milano, E.G.; Ordonez, M.V.; Forte, M.N.V.; Caputo, M.; Schievano, S.; Mustard, H.; Wray, J.; Biglino, G. The use of 3D-printed models in patient communication: a scoping review. J. 3D Print. Med. 2022, 6, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, J.M.; Barbery, D.; Yefimov, A.; Dang, P.N. Preoperative planning using virtual reality for percutaneous transseptal valve-in-valve transcatheter mitral valve replacement: a case report. Eur. Hear. J. - Case Rep. 2022, 6, ytac384. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).