1. Introduction
Developmental dysplasia of the hip (DDH), also referred to as congenital dislocation of the hip, encompasses a spectrum of pathological conditions characterized by abnormal hip development in infancy. This can range from complete dislocation to bone immaturity with a stable hip [
1].
Early diagnosis of DDH plays a pivotal role in ensuring effective and straightforward treatment, fostering high family compliance and positive outcomes [
2].
However, cases that present later often require intricate surgical interventions [
2,
3].
Current protocols involve clinical examinations of newborns to assess hip stability, with the goal of preventing the need for delayed treatments linked to long-term hip deformities, gait disorders, and arthritis.
The introduction of ultrasound technology for assessing infant hip pathology stands out as a significant advancement over the past three decades. This technique allows for precise visualization of all components, both mineralized and non-mineralized, of the infant hip, facilitating early detection of joint abnormalities. Key ultrasound assessment techniques for DDH include Graf’s method [
4,
5], Harcke’s method [
6], and Morin-Terjesen’s method [
7,
8].
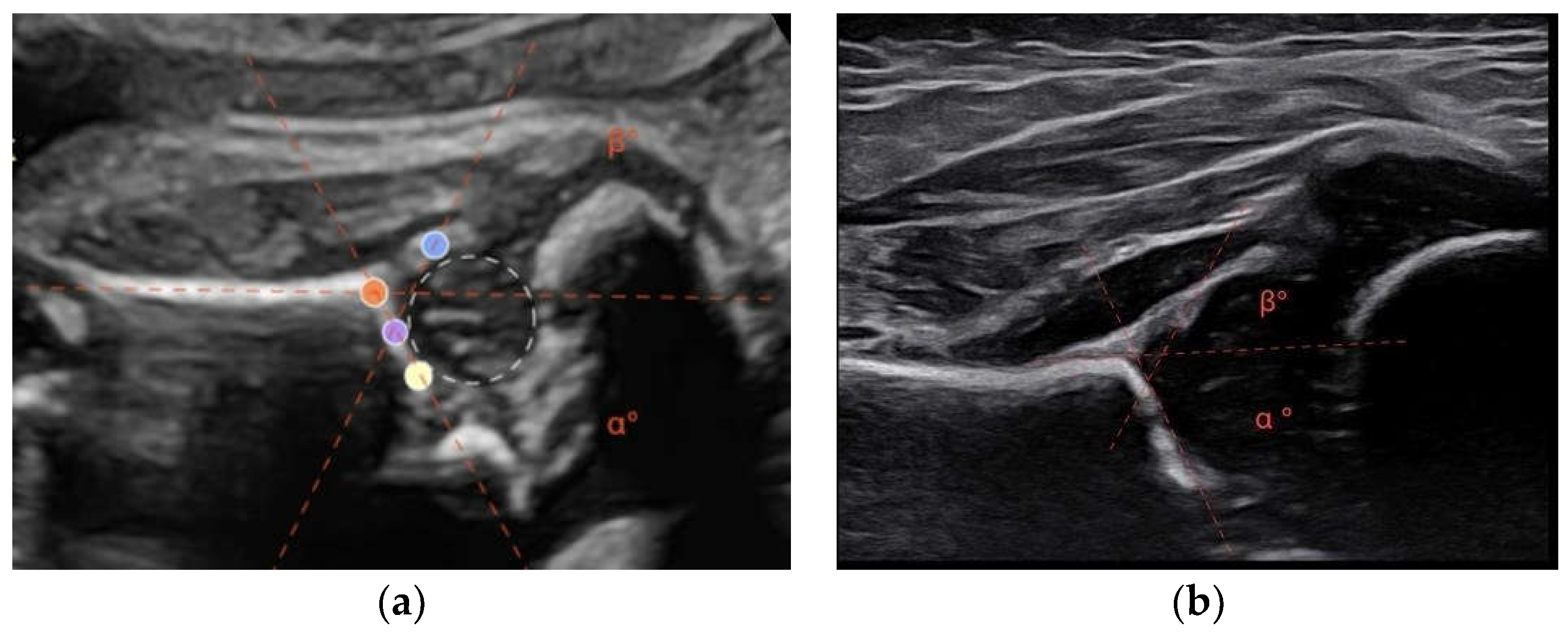
At our center, the method used is that according to Graf. The Graf method presupposes the recognition of the lateral standard sector. On this scan, the inclination angle of the osseous acetabular roof (alpha angle) and the inclination of the cartilaginous acetabular roof (beta angle) are determined. The alpha angle determines the type, and the beta angle determines the subtype in the eponymous classification (
Table 1).
To standardize the acquisition, ultrasound landmarks necessary for overcoming usability checklists must be identified, without which it is not possible to proceed with the measurement. [
4,
5,
9]
Despite the widespread use of neonatal screening protocols (combining clinical and ultrasound assessments for DDH), there remains insufficient evidence to definitively highlight the advantages and optimal timing for such examinations. A 2011 Cochrane review reported inconsistent evidence regarding universal ultrasound screening compared to targeted ultrasound or clinical examination alone. No ultrasound screening strategy has demonstrated enhanced clinical outcomes, including cases of late-diagnosed DDH requiring surgery [
10].
The early identification of patients at risk for the development of DDH could help better focus diagnostic-therapeutic attention, reducing the effort of universal screening.
The aim of this study was to verify the feasibility of diagnosing developmental dysplasia of the hip (DDH) using prenatal ultrasound and to determine the optimal gestational age for sonographic evaluation of the fetal hip.
2. Materials and Methods
This prospective observational study was conducted by the Prenatal Diagnosis Center at the Loreto Community Hospital (Italy), the Pediatric Orthopedic Clinic Department and the Pediatric Radiology Department at Salesi Hospital in Ancona (Italy), from 01/2023 to 03/2024.
Informed consent was obtained from all women and caregivers of the infants involved in the study. This study adheres to the principles outlined in the Helsinki Declaration.
100 pregnant women were recruited from the Prenatal Diagnosis Center, to undergo scheduled obstetric ultrasound examinations during the second and third trimesters.
Inclusion criteria:
Women aged 18 to 45 years;
Physiological pregnancies;
Pregnancies at term;
Complete follow-up through 18 weeks postpartum.
Exclusion criteria:
Twin or multiple pregnancies.
Suspected or diagnosed fetal abnormalities.
Mother’s pathological obesity (BMI > 30 kg/m2).
In addition to the routine examination of the fetus scheduled for the gestational week, an ultrasonographic examination of the hips was performed. The examinations were conducted by a single expert obstetrician-gynecologist. The objective of the investigation was to acquire a neutral lateral scan of the fetal hip joint, on which to measure the alpha and beta angles by adapting the method described by Graf for infants.
GE HealthCare Voluson E10 with a convex probe C2-9 (3-9 mHz) was used for the measurement. It should be noted that in most cases, it was possible to measure only one hip, as the technique allowed analyzing only the one presented towards the probe. Some maneuvers, such as changing the mother’s position or manipulating with the probe can be used to facilitate the presentation of the hip. In 10 cases, it was not possible to collect a standard scan of the fetus’s hip, so they were excluded from the evaluation and the results are referred a total of 90 cases.
A modified Graf method was performed. This involves acquiring a lateral scan of the newborn’s hip. Similarly, to the Graf method for infants, the alpha angle has been defined as the angle formed between a line tangent to the iliac wing and a line tangent to the bony roof. The angle is formed by the line tangent to the iliac wing and a line tangent to the cartilaginous roof [
9,
11] (
Figure 1).
As in the routine neonatal hip screening program, 6 weeks after birth infants underwent ultrasound examination, according to the Graf method. The ultrasound images were obtained by a GE HealthCare Logiq device with a linear ML6-15Mhz probe. The examination was performed by a single independent radiologist, separate from the physician who conducted the prenatal investigations. The values of the alpha and beta angles were determined, and based on these, the hips were classified according to the Graf classification (types Ia, Ib, IIa, IIb, IIc, IId, IIIa, IIIb, and IV). For statistical purposes, patients were divided into two subgroups: group A, including type I hips; group B, including type II, III, and IV hips.
Statistical analysis was performed to verify significant differences between the alpha and beta values between group A and group B.
The correlation between prenatal and postnatal alpha and beta angle values was also analyzed in the entire population.
Statistical Analysis
Statistical analysis of the data was performed using SPSS software version 29.0.2.0 (IBM SPSS Corp.; Armonk, NY, USA). The normal distribution of alpha and beta values was checked using the Shapiro-Wilks test. To identify if there was a statistically significant difference in prenatal alpha angles, the Mann-Whitney U test was performed. Spearman correlation coefficient was calculated to assess the relationship between the alpha angle value (in degrees) at 34 weeks of gestation and the alpha angle value (in degrees) at 6 weeks postnatal. The same methodologies were applied to the beta angles (in degrees).
3. Results
The baseline characteristics of the two groups are summarized in
Table 2.
In the second-trimester, scans showed inconclusive results because, in our experience, it was not possible to assess with accuracy the ultrasonographic findings necessary for calculating the alpha and beta angles.
In third-trimester, scans allowed the measurement of alpha and beta angles in 90 out of 100 examinations. The primary obstacles to acquiring these scans were the failure to obtain a lateral view of the hip due to the fetus positioning.
Using the Shapiro-Wilk test, data of 3rd trimester did not have a normal distribution. The Shapiro–Wilk test statistic for prenatal alpha angle values was W = 0.977, with a p-value = 0.104. The Shapiro–Wilk test statistic for prenatal beta angle values was W = 0.957, with a p-value = 0.005. The Shapiro–Wilk test statistic for postnatal alpha angle values was W = 0.933, with a p-value < 0.001. The Shapiro–Wilk test statistic for postnatal beta angle values was W = 0.907, with a p-value < 0.001. Since the p-values are less than 0.05, the data does not appear to be normally distributed.
Comparing prenatal alpha angle values between Group A and Group B using the Mann-Whitney test revealed a statistically significant difference between the two groups (U = 362.000, p < 0.001). Comparing prenatal beta angle values between Group A and Group B using the Mann-Whitney test also showed a statistically significant difference between the two groups (U = 1763.500, p < 0.001). Comparing postnatal alpha angle values between Group A and Group B using the Mann-Whitney test revealed a statistically significant difference between the two groups (U = 0.000, p < 0.001). Comparing postnatal beta angle values between Group A and Group B using the Mann-Whitney test also showed a statistically significant difference between the two groups (U = 1804.500, p < 0.001).
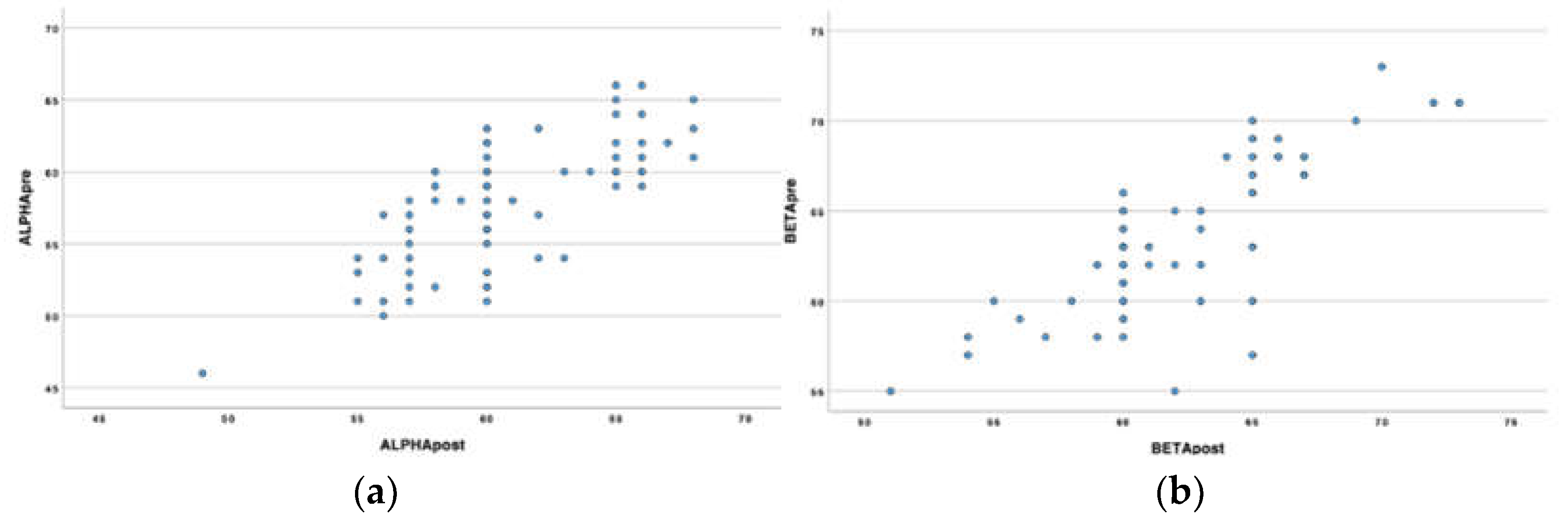
The variables (prenatal alpha/postnatal alpha and prenatal beta/postnatal beta) exhibit a positive monotonic relationship, as evidenced by scatterplots (
Figure 2).
Spearman rank correlation analyses revealed that the prenatal alpha angle value has a strong correlation with the postnatal alpha angle, rho = 0.717, p < 0.001, and the prenatal beta angle has a strong correlation with the postnatal beta angle, rho = 0.737, p < 0.001
4. Discussion
Developmental dysplasia of the hip (DDH) is among the most frequent developmental anomalies in newborns, potentially leading to significant long-term disabilities. Given the relevant social and economic impact, timely diagnosis of this condition is a goal that must be pursued not only in countries that apply universal screening but also in those that do not.
Ultrasound examinations of the fetus during the second and third trimesters are widely used in gynecological check-ups, nevertheless commonly the fetal hip joint is not investigated, and few sonographic studies are available about the evolution of the neonatal hip from fetal development to the postnatal period.
Wagner et al. reported that between the 14th and 19th week of gestation quantitative evaluation of bone structures is not possible, while from the 21st week it is feasible to measure alpha and beta angles, which become more reliable as pregnancy progresses [
12]. Stiegler et al. stated that the hip joint becomes sonographically mature at 34 weeks of gestation [
13]. Baroti et al., by a combined morphological and ultrasound examination, confirmed that alpha angle can be determined only after 18 weeks and that exact measures need a more advanced fetal development [
14].
In a cohort study from the 37th week of gestation, Contro et al. demonstrated that the application of the Graf technique, currently used in postnatal ultrasound, can also be adapted to prenatal ultrasound with good reproducibility [
15].
The results of this study are consistent with evidence from previous work in the literature. Our data indicated that ultrasound examination at the 24th week of pregnancy does not allow for accurate quantitative and qualitative assessment of alpha and beta values, conversely ultrasonographic evaluation during the 34th week of gestation proved to be a reliable and safe method for quantitative determination of alpha and beta angles.
Early ultrasound examination potentially could detect severe forms of DDH as dislocations, even if this condition generally develops in more advanced stages of fetal growth because the hip joint is less stable in the perinatal life [
14,
16,
17].
Contro et al. reported that, although there is no linear correlation between prenatal and postnatal values, the alpha angle systematically increases with development while the beta angle decreases [
15].
In the study by Stiegler et al., which evaluated by sonography fetal and newborn hip, the mean alpha angle found prenatally at 34 weeks were above the level of a mature hip joint and the values increased after birth, while there were not differences in the mean beta angles measured pre and postnatally [
13].
Finally, Komut et al. in a study of 84 patients, observed a concordance between prenatal and postnatal alpha values [
18].
In accordance with these authors, data from the present study showed at the 34th week of pregnancy a significant correlation (p<0.001) between prenatal and postnatal alpha and beta values. Specifically, the alpha angle increased between the 34th week of gestation and the postnatal period, while the beta angle decreased with fetal development.
Our analyses also revealed a significant difference in alpha and beta angle values between infants with mature (Graf I) and immature hips (Graf II) both in prenatal and in postnatal examinations. Thus, data showed a strong correspondence in the maturity level of the hip between the fetuses at the late weeks of pregnancy and the newborns. This suggests that prenatal assessment can be used to identify patients at risk of hip immaturity. In our sample, there were no dislocated or decentered hips (Graf IV) in either the prenatal or postnatal studies, so no data are available on the ultrasonographic evaluation of hips in this situation. To our knowledge, no papers with these findings were produced.
A limitation of the present study was that it showed the results of the acquisition and analysis only of the hip closer to the mother’s abdominal wall. Further studies are in course, adopting various technical measures (changing fetal and maternal position, using as needed linear, convex or even transvaginal probe), to evaluate both fetal hips and reduce the risk of missed diagnoses of DDH.
5. Conclusions
Despite the cautions due to the limited sample size and the evaluation of only one hip for each fetus, the present study confirmed that prenatal ultrasonography represents a viable and safe evaluation method of the fetal hip joint. Morphological sonographic screening of the third trimester could identify patients at risk for developing DDH, facilitating the early identification of hips that require definitive postnatal evaluation. Given these data, the presence of normal prenatal findings in absence of anamnestic or clinical concerns, could theoretically allow to avoid postnatal hip screening.
The present study lays the groundwork for potentially including hip evaluation in routine morphological ultrasonographic assessment of the fetus.
Author Contributions
Conceptualization, C.B, E.F, G.L.; methodology, C.B and V.B.; software, E.F and G.L; validation, A.P.G, A.C. and G.P. ; formal analysis, G.P.; investigation, V.B and G.P.; resources, E.F. and G.L.; data curation, E.F. and G.L.; writing—original draft preparation, C.B., E.F and G.L; writing—review and editing, C.B. and A.P.G.; visualization, S.A.; supervision, A.C.; project administration, A.P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dwan, K.; Kirkham, J.; Paton, R. W.; Morley, E.; Newton, A. W.; Perry, D. C. Splinting for the non-operative management of developmental dysplasia of the hip (DDH) in children under six months of age. Cochrane Database of Systematic Reviews. 2022, 10. [Google Scholar] [CrossRef] [PubMed]
- Dunn, P. M.; Evans, R. E.; Thearle, M. J.; Griffiths, H. E.; Witherow. P. J. Congenital dislocation of the hip: early and late diagnosis and management compared. Arch Dis Child. 1985, 60, 407–414. [CrossRef] [PubMed]
- Ning, B.; Yuan, Y.; Yao, J.; Zhang, S.; Sun, J. Analyses of outcomes of one-stage operation for treatment of late-diagnosed developmental dislocation of the hip: 864 hips followed for 3.2 to 8.9 years. BMC Musculoskelet Disord. 2014, 15, 401. [Google Scholar] [CrossRef] [PubMed]
- Graf, R. Guide to sonography of the infant hip. Thieme: New York. Stuttgart, 1987.
- Graf, R. The diagnosis of congenital hip-joint dislocation by the ultrasonic combound treatment. Archives of Orthopaedic and Traumatic Surgery. 1980, 97, 117–133. [Google Scholar] [CrossRef] [PubMed]
- Harcke, H. T.; Clarke, N. M.; Lee, M. S.; Borns, P. F.; MacEwen, G. D. Examination of the infant hip with real-time ultrasonography. Journal of Ultrasound in Medicine. 1984, 3, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.; Harcke, H. T.; MacEwen, G. D. The infant hip: real-time US assessment of acetabular development. Radiology. 1985, 3, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Terjesen, T.; Bredland, T.; Berg, V. Ultrasound for hip assessment in the newborn. J Bone Joint Surg Br 1989, 71-B, 767–773. [CrossRef] [PubMed]
- Graf, R. New Possibilities for the Diagnosis of Congenital Hip Joint Dislocation by Ultrasonography. Journal of Pediatric Orthopaedics. 1983, 3, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Shorter, D.; Hong, T.; Osborn, DA. Screening programmes for developmental dysplasia of the hip in newborn infants. Cochrane Database Syst Rev. 2011, 9. [Google Scholar] [CrossRef] [PubMed]
- Graf, R. Fundamentals of sonographic diagnosis of infant hip dysplasia. J. Pediatr. Orthop. 1984, 4, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Wagner, U.; Gembruch, U.; Schmitt, O.; Deimling, U. V.; Hansmann, M. Sonographische Untersuchungen des fetalen Hüftgelenks. Z Orthop Ihre Grenzgeb. 2008, 132, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Stiegler, H.; Hafner, E.; Schuchter, K.; Engel, A.; Graf, R. A sonographic study of perinatal hip development: from 34 weeks of gestation to 6 weeks of age. J Pediatr Orthop B. 2003, 12, 365–8. [Google Scholar] [CrossRef] [PubMed]
- Baroti, B.; Pap, Z.; Panti, Z.; Buruian, M. M.; Pavai, Z. Morphometric and ultrasonographic study of the huma fetal hip joint intrauterine development. Rom J Morphol Embryol. 2013, 54, 977–981. [Google Scholar] [PubMed]
- Contro, E.; Larcher, L.; Lenzi, J.; Benfenati, A.; Massinissa Magini, G.; Galeati, G.; Terrone, M.; Galletti, S.; Arcuri, S.; Seidenari, A.; Farina, A. Prenatal Screening for Developmental Displacement of the Hip: The BUDDHA (Pre-Birth Ultrasound for Developmental Displacement of the Hip Assessment) Study. Diagnostics (Basel). 2021, 11, 868. [Google Scholar] [CrossRef] [PubMed]
- Emerson, S.; Brown, D. L.; Mabie, B. C. Prenatal sonographic diagnosis of hip dislocation. J Ultrasound Med. 1988, 7, 687–689. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jarvis, J.; Uhthoff, H.K.; Avruch, L. The fetal acetabulum. A histomorphometric study of acetabular anteversion and femoral head coverage. Clin Ortop Relat Res. 1992, 281, 48–55. [Google Scholar]
- Komut, E.; Zehir, S. Can developmental dysplasia of the hip be identified in the prenatal period? A pilot study: Ultrasonographic evaluation and postnatal follow-up results of fetal hips in the third trimester. Acta Orthop Traumatol Turc. 2021, 55, 196–200. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).