2.1. Definition and Trends of Smart Healthcare
Smart healthcare is defined by Li Jie (2018) [
4] as the trend of integrating advanced technologies such as the Internet of Things (IoT), cloud computing, and high-level analytics into existing medical processes. The application of these technologies in the field of smart healthcare is extensive, having propelled the market entry of remote healthcare, remote patient monitoring, integrated electronic medical record management systems, patient wearable devices, online medical consultations and appointments, and AI-assisted diagnostics. In this context, the prospects for the application of 5G in smart healthcare are shown to be exceptionally vast.
The concept of "Smart Earth" was first introduced in 2009, and since then, its significance has gradually been recognized globally, leading to the emergence of a series of related concepts, including "smart healthcare." With the rapid development of information technology, the integration of IT and traditional medical practices has accelerated and is now comprehensively applied within Taiwan's healthcare services. The deep integration of information technology has significantly propelled the innovation of Taiwan's medical system, enhancing both medical service models and personal health management.
At the governmental level, smart healthcare provides more scientific decision support, primarily reflected in the following aspects: firstly, the deep mining and analysis of patient medical data based on big data systems; secondly, smart healthcare technologies significantly enhance the timeliness of rational decision-making by health-related departments in Taiwan; and thirdly, the ability to establish smart emergency systems that maintain contact with large hospitals or small clinics, achieving timely and effective monitoring and management.
For businesses, smart healthcare brings substantial benefits to the development of telemedicine platforms and medical device apps. Patients can interact in real-time with data on medical information platforms through home apps or self-diagnosis platforms, providing convenient services to patients and significantly reducing the worry for their family members about needing to travel.
With continuous innovation in telemedicine technology internationally, the focus of smart healthcare technology development is shifting towards the research and development of AI-based early screening tools. Early screening gathers extensive data and, with the help of AI, assists doctors in diagnostics. This not only effectively reduces the time doctors spend reviewing cases but also alleviates the screening burden on healthcare professionals and enhances diagnostic accuracy, aiding doctors in making better medical decisions. This contributes to the early detection and treatment of diseases, reducing the waste of health insurance resources on the care of chronic diseases.
In the future, the application of smart healthcare in home remote care will become more widespread, with a sharp increase in the demand for home IoT health terminals, and the interoperability of medical information will become more comprehensive [
5]. This indicates the potential of smart healthcare technologies and their pivotal role in the future medical field.
2.2. Categories of Remote Care
Remote care is defined as the use of 5G communication network technologies and software to transmit health and medical information for patients in need of urgent treatment across different locations, and to support communication and learning among medical teams from various countries globally, thereby enhancing the quality of remote medical care services and extending them to home life support [
6]. Currently, Taiwan's remote care market can be categorized into three main types:
1. Combining 5G and AI technologies for remote medical diagnoses and even surgeries, with cases already implemented internationally. Especially after the COVID-19 pandemic in 2020, the development of remote care has accelerated significantly, driving progress in the service system. Given Taiwan's shortage of medical personnel, rising medical costs, increasing chronic disease population, and the impact of the pandemic, it is foreseeable that future care trends will evolve towards remote, non-contact applications.
2. A significant increase in community day care centers and care points, effectively promoting elderly community participation. In community smart nursing clinics, the public can use exercise equipment, measure blood pressure, etc., with related records subsequently uploaded to a cloud platform and integrated with medical imaging systems, connecting to the outpatient system of health posts, allowing physicians to monitor the physiological health data of the public in real time during the diagnostic process, thereby encouraging residents to form healthy living habits.
3. Home remote care, specifically targeting elderly individuals living alone. Considering that many elderly people's children are unable to stay nearby due to work, the placement of smart medical devices becomes particularly important to prevent emergencies from going unnoticed, leading to emergency medical situations.
These innovative remote care models not only bring revolutionary changes to Taiwan's healthcare service system but also pave new paths for global health management. The ongoing development in this field is expected to greatly enhance the efficiency and quality of medical services, especially in addressing the global aging challenge.
2.3. Home Remote Care
Shih Pei-Yu et al. (2017) [
7] pointed out that home remote care is an essential component of the long-term care system, encompassing a variety of professional services, greatly facilitating the various issues faced by patients receiving care at home [
8]. Specifically, long-term care services mainly include the following aspects:
1. Care services: Divided into home services, day care, and family hosting.
2. Respite services: Including home respite and institutional respite.
3. Home nursing: Provided by professional home nurses, including visiting patients' homes for guidance and treatment.
4. Rehabilitation services: Rehabilitation tasks performed by therapists at patients' homes.
5. Assistive device support: Involving the purchase, rental, and improvement of barrier-free home environments.
As Taiwan’s aging population continues to grow, the demand for long-term care is increasing. Therefore, developing Tele-home Care (THC) has become a significant direction in smart healthcare. The primary advantage of THC is that it enhances the capabilities of family caregivers and improves the quality of life for the entire family. For those care recipients who do not require daily medical assistance, THC facilitates convenient two-way interaction with professional medical personnel through wired or wireless transmission and equipped micro physiological parameter sensors. This not only reduces the travel burden for both parties but also enhances the mobility and disease self-management of the care recipients.
This study focuses on the categories of home remote care, exploring the use of smart electronic medical devices and 5G communication technologies to enable elderly patients or their relatives to monitor health indicators such as blood pressure and blood sugar at home, and store data in real-time on device apps, further uploading it to the smart hospital center service platform. This process not only allows medical personnel to conduct timely remote disease detection and tracking but also greatly facilitates home patients, eliminating their need to visit hospitals or clinics.
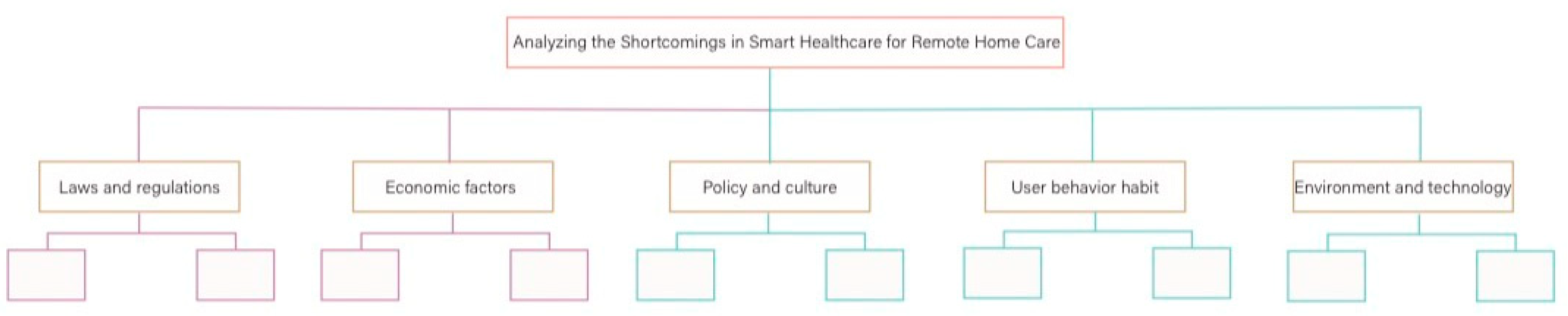
2.4. The Shortcomings in Smart Healthcare for Remote Home Care
2.4.1. Laws and regulations
Taiwan's regulations in the field of telemedicine were relatively strict until the outbreak of the COVID-19 pandemic, which saw them become more lenient. Similar to Japan's approach of easing regulations through administrative interpretation, Taiwan also adjusted its "Regulations on Telemedicine," but unlike Japan's comprehensive opening strategy, Taiwan only expanded the scope of application, mainly targeting groups under home quarantine or isolation. Additionally, prior to 2018, Taiwan's "Physician Act" stipulated that, except in remote areas, medical services in other areas required the physical presence of a physician. However, from January 10, 2018, the Ministry of Health and Welfare introduced the "Draft Regulations on Telemedicine," further broadening the scope of telemedicine. This included "follow-up treatment within three months after discharge for acute inpatients," "residents of residential long-term care facilities," among other new applicable groups, significantly expanding the target audience for telemedicine services.
The rapid development of electronic technology and the rise of the ICT industry have facilitated the widespread use of technologies such as 5G, video transmission, Bluetooth, and wireless networks, providing technical support for real-time home remote care and treatment. However, according to the current "Physician Act," telemedicine has not been fully opened to all Taiwanese people and is still awaiting further policy adjustments.
Legal responsibilities associated with telemedicine are also complex. Remote physicians may only provide professional opinions without establishing a substantial physician-patient relationship, which is referred to as "remote consultation" rather than "telemedicine." Once a physician-patient relationship is established, the lack of face-to-face examination, such as palpation or potential distortions in image transmission, introduces uncertainty into the determination of negligence liability. This uncertainty may become a psychological barrier for physicians resistant to opening telemedicine.
Moreover, when significantly opening telemedicine, other detailed issues need consideration, such as ensuring that medical actions are performed to apply for health insurance payments, which might require recording the entire process to prove informed consent. Additionally, if physicians prescribe medications, patients might still need to physically visit pharmacies to collect their prescriptions, which is not a complete solution for those with mobility issues. Thus, how to reasonably open online pharmacies and address the opposition from physical pharmacies is also a critical issue that needs to be resolved in telemedicine policies. The implementation of these measures will have a profound impact on the development direction and industry trends of telemedicine services in Taiwan.
2.4.2. Economic factors
Due to the intensifying trend of an aging population [
9] and the chronic nature of diseases resulting from advances in medical technology, along with changes in family structures and a reduction in family caregiving functions, elderly individuals face significant difficulties accessing medical care due to reduced mobility or disability. This situation leads to a significant increase in medical costs for the elderly. At the same time, Chen Wenyi et al. (2011) [
10] have noted that remote areas face severe issues with the uneven distribution of medical resources. In this context, the intervention of remote care becomes particularly necessary, but the high costs of remote care are not affordable for every family, especially as the level of service increases, which also raises the costs. Therefore, economic factors become a critical consideration for many families when choosing remote care services.
One of the primary issues facing remote care is the network connectivity of smart healthcare devices. Although 2020 marked the commercial debut year of 5G technology, there are still issues with unstable connections or interruptions under the 4G network environment. Additionally, each home smart healthcare device operates on its independent system, lacking necessary integration. While technological devices are advanced and visually appealing, their high costs and solutions that do not target core pain points limit their widespread adoption. Although 5G networks offer the possibility of real-time data transmission, their high communication costs also deter many families with limited financial resources.
If the remote care industry could nurture several teams with an ecosystem mindset to collaboratively create an interconnected working model, a new care paradigm could potentially emerge. This model would redefine the framework of remote care through technology and innovation, likely playing a significant role in enhancing care quality, reducing costs, and more broadly disseminating smart healthcare devices.
2.4.3. Policy and culture
In 2021, the head of Taiwan's Central Health Insurance Administration under the Ministry of Health and Welfare announced that the year would be designated as the inaugural year for telemedicine health insurance payments, with an allocation of 100 million New Taiwan Dollars to include telemedicine within the scope of health insurance coverage. Initially, this policy will cover ENT (Ear, Nose, and Throat), dermatology, emergency, and outpatient services in 50 townships and districts. In the emergency sector, the subsidy per patient varies from a minimum of 507 New Taiwan Dollars to a maximum of 2340 New Taiwan Dollars depending on the triage category; for outpatient teleconsultations, a uniform subsidy of 500 New Taiwan Dollars is provided. Additionally, in 2021, the Health Insurance Administration evaluated the data flow and administrative processes of telemedicine and explored the possibility of integrating home services, long-term care, and telemedicine.
However, currently only certain departments have opened up to the use of telemedicine, and not all types of diseases can receive medical services remotely. The future development of telemedicine within the health insurance system remains unclear, and whether it will be fully opened is still uncertain [
11].
In the digital health care industry, the widespread adoption of mobile devices and IoT medical equipment has become an irreversible trend. However, these devices pose data security risks during the information collection and transmission processes. For example, data may be corrupted during transmission, tampered with by humans, or hacked via Bluetooth capabilities, all of which can pose serious threats to patients receiving remote care. Consequently, the U.S. Food and Drug Administration (FDA) has issued guidelines requiring IoT-enabled medical devices to have adequate data security protections. Despite this, the rapid development of mobile device technologies, primarily smartphone apps, and their short market lifecycle mean that manufacturers aiming to quickly bring products to market may not fully consider data security and privacy protection. Since 2015, Taiwan's Ministry of Economic Affairs has implemented a voluntary security certification mechanism for apps, but further mandatory implementation could hinder this rapidly changing industry. Therefore, further development at the policy level is still needed.
From a cultural perspective, Taiwan society typically discourages leaving the elderly or patients alone at home, as any malfunction in remote care systems could pose a direct threat to their safety. This cultural characteristic adds significant socio-psychological barriers that must be overcome for the implementation of remote medical services. Therefore, future policy-making and technological innovations must take these cultural factors into account to ensure the widespread acceptance and effective implementation of remote medical services.
2.4.4. User behavior habit
Currently, user behavior habit has not fully transitioned from traditional face-to-face medical consultations to remote medical and care services. Although technological advancements allow for medical test results to be accessed via the internet or applications (Apps), many patients still prefer to be notified personally by a physician and desire the opportunity to directly ask medical personnel related questions.
Additionally, users are highly concerned about the privacy protection of their personal data. While real-time access to medical health information facilitates medical decision-making, it is also susceptible to hacker attacks. According to monitoring by the Ministry of Health and Welfare, Taiwan's government medical information system can experience up to tens of thousands of cyberattacks each night. For example, Under Armour's health application was hacked in February 2018, resulting in the leakage of approximately 150 million user records. In 2013, a hospital in Los Angeles was hacked and had to pay a significant amount of Bitcoin to ransom encrypted electronic medical records. In 2017, 47GB of medical data stored in an Amazon S3 Repository by a company was illegally accessed.
In the context of the digitalization of medical information, non-medical information and communication technology (ICT) companies may gain access to personal medical and health data. The HITECH Act, passed in the United States in 2009, established clear privacy and security regulations for collaborations between non-medical and medical institutions. However, devices such as Apple Watch smartwatches and fitness trackers, as well as data transmission on cloud platforms, may collect substantial amounts of users' physiological data without needing to cooperate with medical institutions, creating legal loopholes.
Medical devices are generally categorized into three or four risk levels for market review. Most health and medical apps are primarily used to record physiological information, but some apps claim to convert smartphones into medical devices such as stethoscopes or combine with external devices for diagnosis or treatment. If the operation of these apps involves medical professionals, safety concerns are minimal; however, if they are entirely operated by users, errors in devices that periodically record physiological information could lead to diagnostic errors.
Currently, post-market monitoring of these technological products mainly relies on product liability and consumer protection laws, with administrative regulations rarely requiring apps to collect and process safety information after market entry. The regulation becomes more challenging with apps developed by foreign companies. Strengthening continuous monitoring and improvement of these products post-market is a significant challenge in future policymaking and in changing user behavior.
2.4.5. Environment and technology
The development of smart healthcare, while full of potential, also faces significant challenges [
12]. Firstly, it encounters issues related to standardization, accuracy, and the acquisition, storage, and processing of big data. Key questions include: who has the right to benefit from this data? Which medical teams or top medical experts are needed to review this data? Moreover, the development of medical artificial intelligence relies on vast amounts of medical data, often facing high costs and poor data quality.
The development of smart healthcare information systems requires close collaboration between medical and technical professionals. However, these two types of professionals differ in their characteristics: the former excels in patient communication, while the latter communicates with machines. In most cases, achieving deep communication between the two is challenging, yet their effective collaboration is crucial for in-depth research and application of the technology.
Secondly, the high degree of specialization in healthcare and information technology, coupled with information asymmetry and the lack of a common language for deep communication, presents another challenge. While technology is crucial, it should not dominate the healthcare industry. Ignoring this point can lead to project failure.
The third challenge is discussing smart healthcare without the support of a reliable medical team. For example, there are over 500 "diabetes management platforms" available on the App Store, but very few are widely used by medical teams and patients. Even wearable devices, despite being purchased, have few continuous users. Without professional support and ongoing improvements from medical teams, these devices are easily abandoned by users.
Finally, the lack of a sustainable business model is a significant challenge. For instance, although telemedicine has played a positive role in improving care quality and preventing patient regret, the monthly fee for Changhua Christian Hospital’s telemedicine service is only 500 New Taiwan Dollars. This model is difficult to sustain. Patients often choose to stop paying for the service after experiencing noticeable short-term improvements, reflecting the issue that high-quality medical services in Taiwan's healthcare system often do not receive corresponding economic returns. Ongoing operational challenges may lead to the discontinuation of many effective medical methods, ultimately harming patient interests.